Abstract
Aims
The aim of this study was to compare robotic arm-assisted bi-unicompartmental knee arthroplasty (bi-UKA) with conventional mechanically aligned total knee arthroplasty (TKA) in order to determine the changes in the anatomy of the knee and alignment of the lower limb following surgery.
Methods
An analysis of 38 patients who underwent TKA and 32 who underwent bi-UKA was performed as a secondary study from a prospective, single-centre, randomized controlled trial. CT imaging was used to measure coronal, sagittal, and axial alignment of the knee preoperatively and at three months postoperatively to determine changes in anatomy that had occurred as a result of the surgery. The hip-knee-ankle angle (HKAA) was also measured to identify any differences between the two groups.
Results
The pre- to postoperative changes in joint anatomy were significantly less in patients undergoing bi-UKA in all three planes in both the femur and tibia, except for femoral sagittal component orientation in which there was no difference. Overall, for the six parameters of alignment (three femoral and three tibial), 47% of bi-UKAs and 24% TKAs had a change of < 2° (p = 0.045). The change in HKAA towards neutral in varus and valgus knees was significantly less in patients undergoing bi-UKA compared with those undergoing TKA (p < 0.001). Alignment was neutral in those undergoing TKA (mean 179.5° (SD 3.2°)) while those undergoing bi-UKA had mild residual varus or valgus alignment (mean 177.8° (SD 3.4°)) (p < 0.001).
Conclusion
Robotic-assisted, cruciate-sparing bi-UKA maintains the natural anatomy of the knee in the coronal, sagittal, and axial planes better, and may therefore preserve normal joint kinematics, compared with a mechanically aligned TKA. This includes preservation of coronal joint line obliquity. HKAA alignment was corrected towards neutral significantly less in patients undergoing bi-UKA, which may represent restoration of the pre-disease constitutional alignment (p < 0.001).
Cite this article: Bone Joint J 2020;102-B(11):1511–1518.
Keywords: Knee arthroplasty, Robotics, Bi-unicompartmental, Kinematic, Mechanical, Alignment, Implant positioning
Introduction
Cemented total knee arthroplasty (TKA) accounts for 85% of TKAs performed in the UK,1 with the vast majority implanted using mechanical alignment techniques. Patient satisfaction lags behind that of total hip arthroplasty, and TKA usually requires resection of the anterior cruciate ligament (ACL), which fundamentally alters the joint kinematics.2,3 Various implant designs have been developed, in addition to different alignment techniques, with the aim of improving functional outcomes and patient satisfaction.
In a mechanically aligned TKA, both the distal femur and proximal tibia are aligned perpendicular to a neutral mechanical axis of the lower limb. As a result, the femoral component is required to be placed in slight external rotation to balance the ligaments in knee flexion.4 Neutral obliquity of the joint line of the knee, however, is not the most common alignment observed constitutionally.5-7 There are many reasons for dissatisfaction following TKA, and over-correction of varus knees into neutral mechanical alignment might be one which results from the extensive capsular and ligamentous releases which are sometimes required.8
The kinematic alignment technique in TKA uses femoral and tibial condylar anatomy to determine the orientation of the components. This usually yields a hip-knee-ankle angle (HKAA) which is similar to mechanical alignment, but with varying obliquity of bony cuts.9-11 However, concerns have been raised about implanting components beyond 3° perpendicular to the mechanical axis because of the risk of cantilever loading leading to early loosening, particularly on the tibial side, and of increased polyethylene wear leading to early failure.12-15 Furthermore, restoring pre-disease joint alignment, while keeping within 3° parameters, can be difficult using a kinematic technique in the presence of severe varus or valgus deformities, particularly with manual implantation, when the accuracy of bone cuts cannot be assured.8
Unicompartmental knee arthroplasty (UKA) is suitable for patients with single-compartment osteoarthritis (OA), in the absence of gross deformity or ligamentous deficiency. Resurfacing the degenerative compartment while retensioning its respective collateral ligament restores constitutional alignment. It has been shown that patients with a UKA and a contralateral TKA tend to favour the UKA, which maintains a more natural gait.16-18 UKA also offers faster recovery, less postoperative pain, and lower rates of thromboembolism, cerebrovascular events and 30-day mortality, compared with TKA.19
Bi-unicompartmental knee arthroplasty (bi-UKA) replaces the medial and lateral joint surfaces separately, retensioning the collateral ligament on the more affected side, and sparing both cruciate ligaments.20 It aims to deliver the advantages of decreased morbidity and mortality associated with UKA to patients with bicompartmental OA. The literature on bi-UKAs is limited, but it has been shown that manually implanted bi-UKAs do not correct HKAA to neutral as much as TKA.21 Improved early function and promising implant survivorship of UKAs with robotic assistance also makes this approach more attractive than previously.22,23
The aim of this study was to determine whether robotic-assisted bi-UKA maintains constitutional joint line anatomy compared with mechanically aligned TKA, and to analyze differences in postoperative HKAA. We also present a method of determining lower limb and knee alignment using CT, whether in the presence of a normal knee, bi-UKA, or TKA.
Methods
Patients on the waiting list for knee arthroplasty at Glasgow Royal Infirmary were screened for possible recruitment to the Total versus Robotic assisted bi-UniCompartmental Knee (TRUCK) trial (ISRCTN 12151461).20 Patients were eligible for inclusion if they presented with medial and lateral compartment OA suitable for treatment with a standard unconstrained TKA, with clinically intact cruciate and collateral ligaments. Exclusion criteria comprised patients with rheumatoid arthritis or other inflammatory arthropathies, those with varus or valgus deformities > 15°, a fixed flexion contracture > 10°, single-compartment OA suitable for an isolated UKA, or patellofemoral OA greater than Kellgren and Lawrence grade III.24 Patients who had undergone previous surgery to the knee which might affect the outcome of an arthroplasty, or those with significant disease in other joints, which might alter their gait, were also excluded.
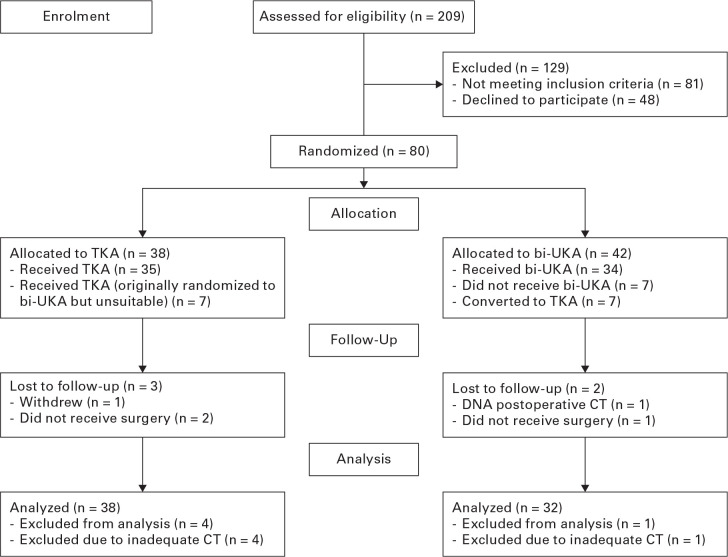
From a total of 209 screened patients, 80 were recruited to the TRUCK trial. The Consolidated Standards of Reporting Trials (CONSORT) diagram for this study is shown in Figure 1, and demographic data are shown in Table I. Patients were randomized to one of two treatment arms using a web-based system, with all procedures sub-randomized to be undertaken by one of three orthopaedic surgeons (BGJ, ADM, MJGB), with extensive experience in both TKA and robotic-assisted UKA.
Fig. 1.
Consolidated Standards of Reporting Trials (CONSORT) diagram, showing the flow of patients through the Total versus Robotic assisted bi-UniCompartmental Knee (TRUCK) trial. Bi-UKA, bi-unicompartmental arthroplasty; TKA, total knee arthroplasty.
Table I.
Preoperative demographic data.
| Characteristic | TKA (n = 38) | Bi-UKA (n = 32) | p-value |
|---|---|---|---|
| Mean age, yrs (SD) | 70.5 (7.1) | 68.7 (7.8) | 0.316* |
| Operated side (R:L) | 16:22 | 14:18 | 0.889† |
| Sex (M:F) | 18:20 | 15:17 | 0.967† |
| Mean BMI, kg/m2 (SD) | 32.6 (5.8) | 31.7 (17) | 0.497* |
Paired t-test.
Chi-squared test.
BMI, body mass index.
Patients in the TKA group underwent this procedure using the NexGen LPS implant (Zimmer, Warsaw, Indiana, USA), a fixed-bearing bicruciate-sacrificing total condylar implant (Figure 2). Patellar resurfacing was not carried out. Traditional instrumentation, without the aid of robotics, was used to perform the bony cuts, aiming for a neutral HKAA, with femoral and tibial components being implanted perpendicular to the mechanical axis.
Fig. 2.
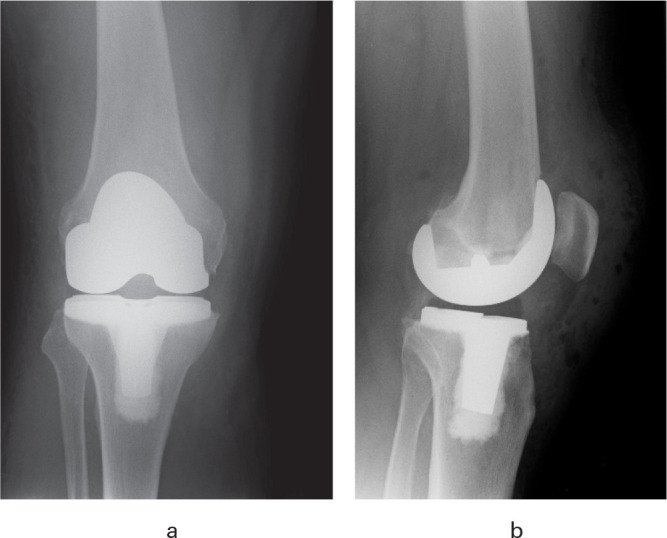
a) Anteroposterior and b) lateral postoperative radiographs showing a NexGen LPS-Flex total knee arthroplasty.
Patients in the bi-UKA group (Figure 3) underwent this procedure with medial and lateral Restoris MCK (MultiCompartmental Knee) fixed-bearing onlay implants (Stryker, Kalamazoo, Michigan, USA), performed with the aid of the Mako Robotic-Arm Assisted Technology (Stryker). The aim for the bi-UKA group was to resurface both the medial and lateral compartments (Figure 4), reconstructing each patient’s constitutional joint alignment. This involved retensioning the collateral ligament on the more affected side of the joint (medial collateral ligament for a varus knee; lateral collateral ligament for a valgus knee). The less affected side of the knee was then resurfaced in situ without requiring ligament balancing. Neither the trochlea nor the patella was resurfaced in this procedure.
Fig. 3.
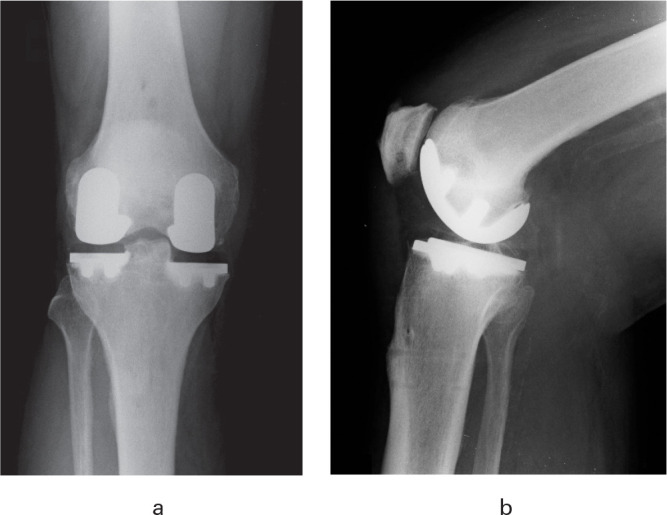
a) Anteroposterior and b) lateral postoperative radiographs showing a bi-unicompartmental knee arthroplasty with medial and lateral Restoris MCK implants.
Fig. 4.

Intraoperative photograph showing a bi-unicompartmental knee arthroplasty, with both medial and lateral compartments resurfaced separately; the cruciate ligaments remain intact. The procedure is performed through a midline incision and medial parapatellar approach, as for a total knee arthroplasty.
The bi-UKA technique, simultaneously replacing both medial and lateral sides of the joint, was an off-label use of the Mako System at the time of registration of the trial. Permission for this specific use of the robotic system was obtained via Clinical Trials Notification (CI/2014/0032) with the Medicines and Healthcare products Regulatory Agency. Ethical approval for the trial was obtained from the West of Scotland Research Ethics Committee (14/WS/0134).20
All patients had weight-bearing anteroposterior (AP) and lateral radiographs of the knee and CT scans of the lower limb preoperatively and at three months postoperatively.
The primary outcome measure used in the TRUCK trial was the percentage of patients with a bi-phasic (normal) moment curve during gait (level walking) at one year following surgery. This study analyzes the secondary outcome of component positioning, assessing the anatomy of the knee joint in all three planes on both the femoral and tibial sides, in addition to the overall HKAA.
Both pre- and postoperative CT scans followed those stipulated in the Mako partial knee arthroplasty (PKA) CT scanning protocol. Hip and ankle regions were scanned with 2 mm to 5 mm interval scans and the knee regions at 0.5 mm to 1 mm interval scans. Images were converted to Digital Imaging and Communications in Medicine (DICOM) and analyzed using Mimics and 3-Matic software (Materialise NV, Leuven, Belgium) to determine the parameters of alignment (Supplementary Table i).
Anatomical points were chosen to define the same bone reference frames from both pre- and postoperative scans (Supplementary Table i). Additional points, on both native anatomy and implants, were chosen to determine the orientation of the femoral and tibial condyles relative to the bone reference frames. (Supplementary Table i). From these derived points and reference frames, the relative angles could be calculated (Supplementary Table ii) to generate the measurements of alignment pre- and postoperatively (Table II).
Table II.
Pre- and postoperative lower limb and knee alignment, according to the type of implant.
| TKA (n = 38) | Bi-UKA (n = 32) | ||||||
|---|---|---|---|---|---|---|---|
| Variable | Preop | Postop | Delta | Preop | Postop | Delta | p-value* |
| Mean femoral coronal angle (MDFA), ° (SD) | 92.5 (2.2) | 89.8 (2.1) | 2.6 (2.2) | 92.2 (2.8) | 91.3 (2.1) | 0.9 (1.6) | 0.001 |
| Mean femoral sagittal angle, ° (SD) | -0.5 (2.2) | 2.2 (3.4) | -2.7 (2.9) | 0.0 (2.6) | 3.1 (5.4) | -3.1 (6.6) | 0.650 |
| Mean femoral axial angle, ° (SD) | 2.7 (2.4) | -1.6 (2.5) | 4.3 (2.9) | 2.4 (2.1) | 2.2 (2.4) | 0.2 (2.2) | < 0.001 |
| Mean tibial coronal angle (MPTA), ° (SD) | 85.4 (2.5) | 89.6 (1.7) | -4.3 (2.8) | 86.0 (2.5) | 86.6 (2.9) | -0.6 (2.5) | < 0.001 |
| Mean tibial sagittal angle – medial, ° (SD) | 7.1 (3.3) | 3.2 (2.1) | 3.9 (3.6) | 6.0 (3.6) | 4.4 (2.7) | 1.6 (2.4) | 0.006 |
| Mean tibial sagittal angle – lateral, ° (SD) | 4.6 (4.8) | 3.2 (2.1) | 1.4 (4.6) | 5.4 (4.4) | 5.4 (3.2) | 0.1 (3.6) | 0.159 |
| Mean tibial axial angle, ° (SD) | -12.9 (7.1) | -5.2 (6.1) | -7.7 (9.2) | -10.7 (5.5) | -12.1 (4.6) | 1.4 (7.1) | < 0.001 |
| HKAA, ° (SD) | 177.8 (3.1) | 179.5 (3.2) | -1.6 (2.7) | 178.2 (4.2) | 177.8 (3.4) | 0.3 (2.4) | 0.001 |
Mann-Whitney U test.
HKAA, hip-knee-ankle angle; MDFA, medial distal femoral angle; MPTA, medial proximal tibial angle.
As an example, the centre of the tibia is typically defined as the midpoint between the tibial spines,25 but these structures were removed in the postoperative TKA scan, hence a novel geometrical centre of the tibia was used (Figure 5). While this method has limitations due to the natural variation seen in native knees, we were unable to use other methods to define a consistent point, as it is resected in TKAs, and can be difficult to identify due to implant-generated artefacts in the case of bi-UKAs.
Fig. 5.
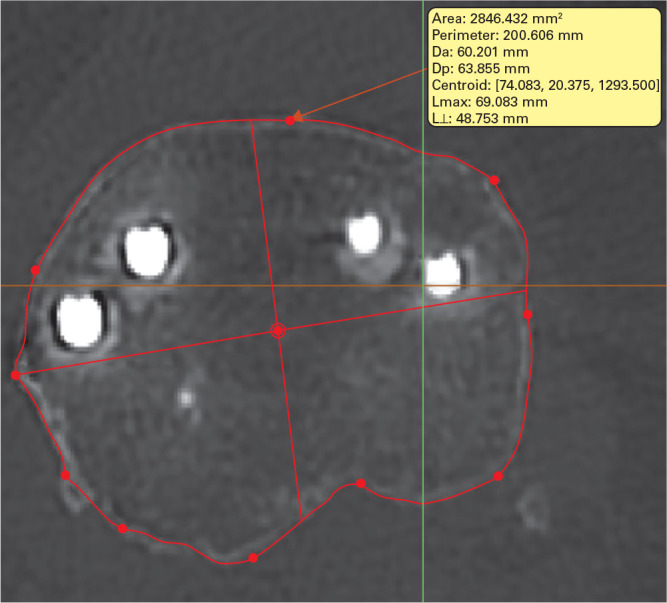
Example of measurement on axial CT, using Mimics software (Materialise NV, Leuven, Belgium), of the centre of the tibia following bi-unicompartmental knee arthroplasty.
Statistical analysis
A per protocol analysis of differences between bi-UKA and TKA groups in terms of the anatomy of the knee and the alignment of the lower limb was undertaken with two-sample non-parametric tests (Mann-Whitney U test) using statistical software (MATLAB Version 9.5.0 (R2018b); MathWorks, Natick, Massachusetts, USA). A p-value of < 0.05 was considered significant. The primary outcome power calculation for the presence of a biphasic knee flexion moment during gait required 36 patients per group, with a 30% loss to follow-up, totalling 96 recruits. Following slow recruitment, this was changed to a 10% loss to follow-up, with permission of the overview groups, leading to a final recruitment target of 80 patients, which was achieved. A post-hoc power calculation of this secondary outcome, based on a 2° difference in the change of HKAA, medial distal femoral angle (MDFA), and medial proximal femoral angle (MPTA), at 80% power, would require a sample of 55, 21, and 47, respectively.
Intraobserver correlation was assessed with an investigator (WDJ) analyzing the CT scans on two separate occasions, while interobserver correlation was examined by a second investigator (NR) analyzing the scans separately. The intraclass correlation coefficient (ICC) was calculated using statistical software (SPSS v. 25; IBM, Armonk, New York, USA).
Results
The ICC between all sets of measurements was > 0.99, indicating excellent intra- and interobserver reliability.
The pre- to postoperative change in joint anatomy was significantly less in patients undergoing bi-UKA in all three planes in both the femur and tibia, except for femoral sagittal component orientation, in which there was no difference (Table II). Overall, for the six parameters of alignment (three femoral and three tibial), 47% of bi-UKAs and 24% of TKAs had a pre- to postoperative change of < 2° (p = 0.045). The change in HKAA towards neutral in varus and valgus knees was significantly less in patients undergoing bi-UKA compared with TKA (p < 0.001). Alignment was neutral in those who underwent TKA (mean 179.4° (SD 3.2°)) while those who underwent bi-UKA had mild residual varus or valgus alignment (mean 177.8° (SD 3.4°)) (p < 0.001 ).
Overall, the mean postoperative MDFA and MPTA for TKAs were 89.8° (SD 2.1°) and 89.6° (SD 1.7°), respectively, indicating orientation of femoral and tibial components perpendicular to the mechanical axis. The mean postoperative MDFA and MPTA for bi-UKAs were 91.3° (SD 2.1°) and 86.6° (SD 2.9°), respectively, indicating a more oblique joint line – valgus on the femoral side and varus on the tibial side.
The mean pre- to postoperative change in tibial sagittal alignment laterally was not significantly different between different types of implant (0.1° bi-UKA (SD 3.6°) vs 1.4° TKA (SD 4.6°); p = 0.159). However, the mean pre- to postoperative change in sagittal alignment medially was significantly greater for TKAs than bi-UKAs (1.6° bi-UKA (SD 2.4°) vs 3.9° TKA (SD 3.6°); p = 0.006). The TKA sagittal slope was equal on medial and lateral sides (mean, 3.2°) due to the monoblock nature of the component. The mean pre- to postoperative change in tibial axial alignment was significantly different between implant types, with TKAs being significantly more externally rotated (1.4° bi-UKA (SD 7.1°) vs -7.7° (SD 9.2°) TKA; p < 0.001).
Discussion
A fundamental principle of conventional TKA has been to achieve a neutral mechanical axis, with components implanted perpendicular to this axis.12 This has been supported by studies which have shown lower revision rates in patients in whom the coronal alignment of the component was within 3° of neutral.14,15 However, this concept overlooks the variable natural alignment seen by Bellemans et al6 in the pre-disease knee of adolescents and young adults. Implanting components perpendicular to the mechanical axis may be beneficial for implant survivorship, but risks altering the patient's bony anatomy and may require more aggressive capsular and ligament releases to obtain soft tissue balancing. The concept of kinematic alignment in TKA attempts to address this concern by allowing placement of components based on joint anatomy.10 Although some studies have suggested that postoperative coronal lower limb and knee alignment (HKAA, MDFA, and MPTA) outside 3° from neutral does not predict implant failure,26–28 most existing literature advocates keeping within this ‘safe zone’.12–15,29 The effectiveness of kinematically aligned TKA may therefore be limited for patients with constitutional varus or valgus beyond 3° from neutral.
The concept of bi-UKA surgery to treat both medial and lateral tibiofemoral arthritis is not new, but the technique is demanding, particularly when using traditional instrumentation. Multicompartmental small implants were developed around the same time as TKAs,30 but variable results have been reported with bi-UKAs. Parratte et al31 reported a survivorship of 78% at 17 years, with aseptic loosening being the predominant cause of failure at a mean of 6.5 years. In contrast, Biazzo et al32 reported no failures and better functional outcomes with 19 bi-UKAs, when compared with 18 TKAs at a mean follow-up of 15 years.32
A previous randomized controlled trial at our institution showed that conventional UKAs were within 2° of their coronal, sagittal, and axial alignment targets in a significantly lower proportion of patients, compared with robotic-assisted UKAs, for both femoral and tibial components.33 These findings were supported by a recent meta-analysis of seven studies, which showed that robotic assistance significantly improved the accuracy of implanting UKA components.34 Although the meta-analysis found that robotic-assisted UKA takes about 16 minutes longer on average than conventional UKA, there was no increase in adverse events.
Robotic assistance has therefore given us the opportunity to revisit the bi-UKA concept, delivering a multiplanar surgical plan with greater sensitivity to the native knee. Decoupling the medial and lateral sides of the joint removes the concerns about cantilever loading on monoblock components used in TKA, meaning fewer theoretical limits on the amount of varus or valgus to which the femoral and tibial components can be aligned. Bi-UKA surgery can therefore be considered a true kinematic procedure, allowing retensioning of the soft tissue envelope back towards to the pre-disease constitutional varus or valgus.
Confalonieri et al21 undertook a matched cohort study comparing 22 manually implanted bi-UKAs with 22 navigated TKAs. The mean postoperative HKAA alignment of TKAs (179.4°) was significantly closer to neutral (p < 0.01), compared with that of bi-UKAs (176.8°), which are similar to our results. However, the bi-UKA group had significantly better function at a minimum follow-up of four years (p < 0.05).
In some ways, the results of this study are self-evident, showing that robotic-assisted bi-UKA surgery alters joint anatomy to a lesser extent than conventional TKA, as the position of the components is patient-specific and not predetermined by values on a mechanical jig (Figure 6). To our knowledge, however, this has not previously been quantified in the literature. This was demonstrated on both the femoral and tibial sides of the joint, but was especially noticeable on the tibial side, where proximal tibial varus was maintained in constitutionally varus knees. This has the potential to provide kinematic function closer to that of a normal knee, although currently there are no data to support this view.
Fig. 6.
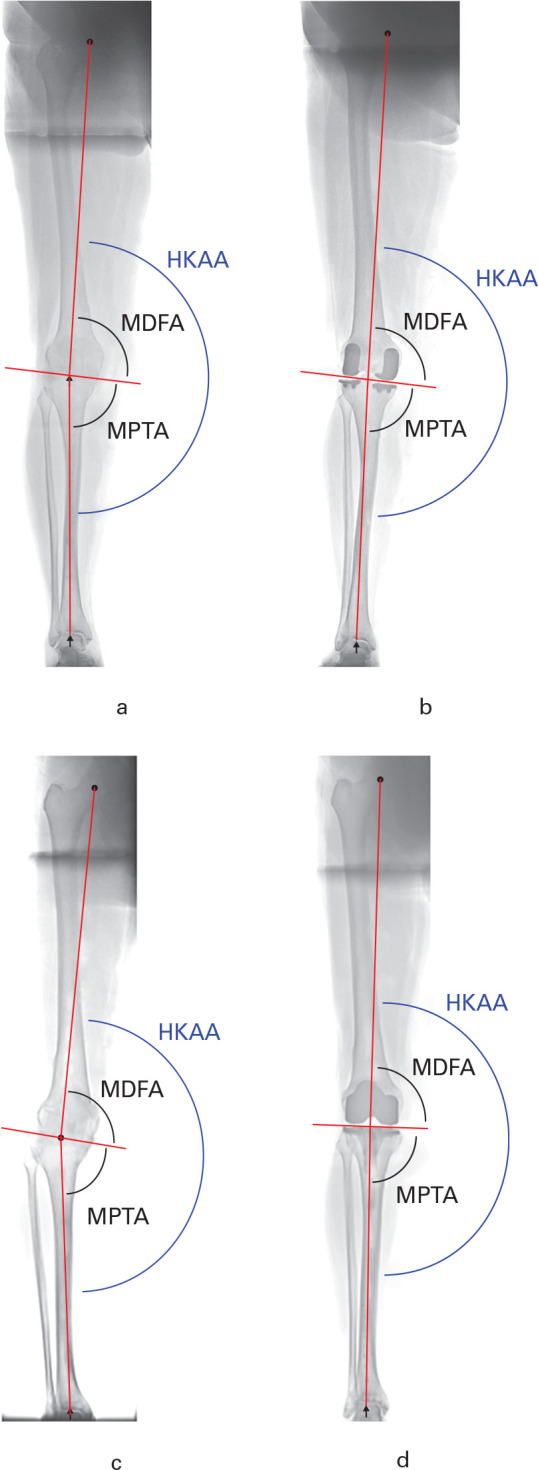
a) Pre- and b) postoperative long-leg standing radiographs showing correction of hip-knee-ankle angle (HKAA), while the obliquity of the joint line is maintained, following bi-unicompartmental knee arthroplasty. c) Pre- and d) postoperative long-leg standing radiographs showing correction of HKAA and alteration of the obliquity of the joint line following total knee arthroplasty.
The range of varus in postoperative MPTA in patients who underwent bi-UKA, with a maximum of 81.3°, was of particular interest. Overall, there were 13 knees with proximal tibial varus of > 3° following bi-UKA, compared with only three knees following TKA. It is perhaps these patients, with severe proximal tibia vara, for whom the bi-UKA technique will be most suitable, either because a mechanically aligned TKA would necessitate much larger soft tissue releases, or a kinematically aligned TKA may incompletely restore the native joint anatomy or require an increased obliquity with the associated concerns of possible early failure. Furthermore, the tissue-sparing nature of a bi-UKA would permit easier revision surgery, should it be required.21
It will be interesting to observe the clinical outcome with the passage of time and whether the bi-UKA technique, recreating preoperative joint anatomy and kinematics, results in improved function in the short term. It will also be interesting to see the effect of joint line obliquity on survivorship in the long term. Although joint reaction forces lie parallel to the mechanical axis in standing, they are between 2° and 3° of varus from the mechanical axis during normal gait, because heel strike occurs closer to the midline than the hip joint.2 An oblique joint line therefore lies more perpendicular to the joint reaction force than a neutral TKA joint line. Given that peak joint reaction force occurs at heel strike, this may translate into better wear and implant survivorship in patients who undergo bi-UKA.
We recognize that this study has limitations. First, despite successfully undergoing surgery, four patients who underwent TKA and two who underwent bi-UKA could not be included in the analysis due to inadequate CT scans. This was mainly due to failing to capture the required anatomy due to inadequate resolution with metal artefact. Nevertheless, determining alignment using CT scans is far more accurate than with plain radiographs, and overcomes the possibility of errors in rotational positioning. Secondly, it is likely that a dynamically loaded knee behaves differently to an unloaded knee. It was not possible to obtain weight-bearing CT scans to ensure a close-packed joint and accurate measurement of overall lower limb alignment; however, our method of determining HKAA with the sum of the MDFA and the MPTA should eliminate any errors from lift-off. In addition, both the intra- and interobserver reliability of the CT measurements showed that our method was consistent and reproducible.
In conclusion, we found that robotic arm-assisted bi-UKA maintains the anatomy of the knee in all three planes and alters the overall HKAA much less than a mechanically aligned TKA. Although it remains to be seen whether this will translate into improved long-term outcomes, the results offer the exciting prospect of restoring the pre-disease joint anatomy and producing a kinematic performance which is closer to that of the normal knee.
Take home message
- Bi-unicompartmental knee arthroplasty (bi-UKA) alters overall hip-knee-ankle angle alignment towards neutral less than conventional total knee arthroplasty (TKA), although it remains to be seen whether this will translate into improved long-term outcomes.
- Robotic-arm assisted bi-UKA maintains coronal, sagittal, and axial knee joint anatomy, compared with a mechanically aligned TKA.
Author contributions
M. S. Banger: Designed the study, Collected and analyzed the data, Prepared and approved the manuscript.
W. D. Johnston: Designed the study, Collected and analyzed the data, Prepared and approved the manuscript.
N. Razii: Collected and analyzed the data, Prepared and approved the manuscript.
J. Doonan: Analyzed the data, Prepared and approved the manuscript.
P. J. Rowe: Analyzed the data, Prepared and approved the manuscript.
B. G. Jones: Performed the operations, Collected and analyzed the data, Prepared and approved the manuscript.
A. D. MacLean: Performed the operations, Collected and analyzed the data, Prepared and approved the manuscript.
M. J. G. Blyth: Designed the study, Performed the operations, Collected and analyzed the data, Prepared and approved the manuscript.
Funding statement
The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article. In addition, benefits have been or will be directed to a research fund, foundation, educational institution, or other non- profit organization with which one or more of the authors are associated.This project (project reference 12/12/12) is funded by the Efficacy and Mechanism Evaluation (EME) Programme, an MRC and NIHR partnership. The views expressed in this publication are those of the author(s) and not necessarily those of the MRC, NIHR or the Department of Health and Social Care. In kind support was received from a commercial party related to the subject of this article in the form of surgical implants and the robotic-arm system.
ICMJE COI statement
All authors declare an institutional grant from Stryker, related to this study. M. Banger, W. Johnston, and M. Blyth also declare support for travel from Stryker, related to this study. M. Banger, J. Doonan, P. Rowe, and M. Blyth all declare institutional grants from Stryker, unrelated to this study. B. Jones declares personal payments for lectures from Zimmer Biomet and travel support from Stryker, unrelated to this study. M. Blyth declares personal payments from Stryker for consultancy, speaking fees, and support for travel, all unrelated to this study.
Acknowledgements
The authors would like to thank Glasgow Clinical Research Facility, Georgia Tarfali, Janet Johnstone, Elizabeth Lennon, Jane Ireland, Dario Salutous and John Alexander for their contribution to the collection of data. The authors would also like to thank Iona Donnelly and Sinead O’Donnell for their contribution to supporting the project and maintaining the research database.
Ethical review statement
Ethical approval for the trial was obtained from the West of Scotland Research Ethics Committee (14/WS/0134).
Open access statement
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/
Trial registration number
ISRCTN 12151461
Follow M. S. Banger @MatthewBanger
Follow J. Doonan @DoonanJames
Follow the Institute of Infection, Immunity & Inflammation @iiiglasgow
Follow the University of Glasgow @UofGlasgow
Follow the Glasgow Clinical Research Facility @GlasgowCRF
Follow the University of Strathclyde @UniStrathclyde
Follow Strathclyde Biomedical Engineering @StrathBiomedEng
Supplementary material
Definitions of anatomical points, and definition of axes and angles used in determining coronal, sagittal and axial alignment.
This article was primary edited by J. Scott.
References
- 1.No authors listed . NJR 16th Annual Report. 2019. https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2016th%20Annual%20Report%202019.pdf (date last accessed 24 June 2020).
- 2.Cherian JJ, Kapadia BH, Banerjee S, et al. . Mechanical, anatomical, and kinematic axis in TKA: concepts and practical applications. Curr Rev Musculoskelet Med. 2014;7(2):89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hutt JRB, LeBlanc M-A, Massé V, Lavigne M, Vendittoli P-A. Kinematic TKA using navigation: surgical technique and initial results. Orthop Traumatol Surg Res. 2016;102(1):99–104. [DOI] [PubMed] [Google Scholar]
- 5.Fahlman L, Sangeorzan E, Chheda N, Lambright D. Older adults without radiographic knee osteoarthritis: knee alignment and knee range of motion. Clin Med Insights Arthritis Musculoskelet Disord. 2014;7:CMAMD.S13009–.13011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat Award: is neutral mechanical alignment normal for all patients? the concept of constitutional varus. Clin Orthop Relat Res. 2012;470(1):45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hsu RW, Himeno S, Coventry MB, Chao EY. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;255:215–227. [PubMed] [Google Scholar]
- 8.Rivière C, Iranpour F, Auvinet E, et al. . Alignment options for total knee arthroplasty: a systematic review. Orthop Traumatol Surg Res. 2017;103(7):1047–1056. [DOI] [PubMed] [Google Scholar]
- 9.Howell S, Hull M, Mahfouz M. Kinematically Aligned Total Knee Arthroplasty. Insall & Scott Surgery of the Knee. 6th. Philadelphia PA, 2020. [Google Scholar]
- 10.Spencer BA, Mont MA, McGrath MS, Boyd B, Mitrick MF. Initial experience with custom-fit total knee replacement: intra-operative events and long-leg coronal alignment. Int Orthop. 2009;33(6):1571–1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nogler M, Hozack W, Collopy D, et al. . Alignment for total knee replacement: a comparison of kinematic axis versus mechanical axis techniques. A cadaver study. Int Orthop. 2012;36(11):2249–2253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73(5):709–714. [DOI] [PubMed] [Google Scholar]
- 13.Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty. 2009;24(6 Suppl):39–43. [DOI] [PubMed] [Google Scholar]
- 14.Berend ME, Ritter MA, Keating EM, Faris PM, Meding JB. Tibial component failure mechanisms in total knee replacement. J Arthroplasty. 2004;19(2):262. [DOI] [PubMed] [Google Scholar]
- 15.Park J-K, Seon J-K, Cho K-J, Lee N-H, Song E-K. Is immediate postoperative mechanical axis associated with the revision rate of primary total knee arthroplasty? A 10-year follow-up study. Clin Orthop Surg. 2018;10(2):167–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Watanabe T, Abbasi AZ, Conditt MA, et al. . In vivo kinematics of a robot-assisted uni- and multi-compartmental knee arthroplasty. J Orthop Sci. 2014;19(4):552–557. [DOI] [PubMed] [Google Scholar]
- 17.Chassin EP, Mikosz RP, Andriacchi TP, Rosenberg AG. Functional analysis of cemented medial unicompartmental knee arthroplasty. J Arthroplasty. 1996;11(5):553–559. [DOI] [PubMed] [Google Scholar]
- 18.Wiik AV, Nathwani D, Akhtar A, et al. . The unicompartmental knee is the preferred side in individuals with both a unicompartmental and total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liddle AD, Judge A, Pandit H, Murray DW. Adverse outcomes after total and unicompartmental knee replacement in 101 330 matched patients: a study of data from the National Joint Registry for England and Wales. The Lancet. 2014;384(9952):1437–1445. [DOI] [PubMed] [Google Scholar]
- 20.Blyth M, Anthony I, Jones B, et al. . Explanatory comparative study of conventional total knee arthroplasty versus robotic assisted Bi-UniCompartmental knee arthroplasty. 2020. https://w3.abdn.ac.uk/hsru/TRUCK/Public/Download.aspx?ID=7 (date last accessed 24 June 2020).
- 21.Confalonieri N, Manzotti A, Cerveri P, De Momi E. Bi-unicompartmental versus total knee arthroplasty: a matched paired study with early clinical results. Arch Orthop Trauma Surg. 2009;129(9):1157–1163. [DOI] [PubMed] [Google Scholar]
- 22.Blyth MJG, Anthony I, Rowe P, et al. . Robotic arm-assisted versus conventional unicompartmental knee arthroplasty: Exploratory secondary analysis of a randomised controlled trial. Bone Joint Res. 2017;6(11):631–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Banger M, Blyth M, Jones B, MacLean A, Rowe P. 5 year results of a randomised trial of robotic arm assisted vs. manual unicompartmental knee arthroplasty [abstract]. 20th EFORT Annual Congress, Lisbon. 2019. https://congress.efort.org/documents/6862319/7471674/N2461.pdf (date last accessed 3 July 2020).
- 24.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jamali AA, Meehan JP, Moroski NM, et al. . Do small changes in rotation affect measurements of lower extremity limb alignment? J Orthop Surg Res. 2017;12(1):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML. Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res. 2013;471(3):1000–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Howell SM, Papadopoulos S, Kuznik KT, Hull ML. Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2271–2280. [DOI] [PubMed] [Google Scholar]
- 28.Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010;92-A(12):2143–2149. [DOI] [PubMed] [Google Scholar]
- 29.Abdel MP, Oussedik S, Parratte S, Lustig S, Haddad FS. Coronal alignment in total knee replacement: historical review, contemporary analysis, and future direction. Bone Joint J. 2014;96-B(7):857–862. [DOI] [PubMed] [Google Scholar]
- 30.Gunston FH. Polycentric knee arthroplasty. prosthetic simulation of normal knee movement. J Bone Joint Surg Br. 1971;53(2):272–277. [PubMed] [Google Scholar]
- 31.Parratte S, Pauly V, Aubaniac J-M, Argenson J-NA. Survival of bicompartmental knee arthroplasty at 5 to 23 years. Clin Orthop Relat Res. 2010;468(1):64–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Biazzo A, Manzotti A, Confalonieri N. Bi-unicompartmental versus total knee arthroplasty: long term results. Acta Orthop Belg. 2018;84(3):237–244. [PubMed] [Google Scholar]
- 33.Bell SW, Anthony I, Jones B, et al. . Improved accuracy of component positioning with robotic-assisted Unicompartmental knee arthroplasty: data from a prospective, randomized controlled study. J Bone Joint Surg Am. 2016;98-A(8):627–635. [DOI] [PubMed] [Google Scholar]
- 34.Fu J, Wang Y, Li X, et al. . Robot-assisted vs. conventional unicompartmental knee arthroplasty: Systematic review and meta-analysis. Orthopade. 2018;47(12):1009–1017. [DOI] [PubMed] [Google Scholar]