Abstract
While fear and anger have been extensively studied as emotions involved in posttraumatic stress disorder, shame is an important emotion to examine in those who have experienced a traumatic event, as it is often associated with treatment avoidance and treatment resistance. Compared to guilt, which is associated with having participated in something that violates social/cultural norms or expectations, shame is associated with a negative perception of the self. The current paper sought to examine the role of shame proneness and guilt proneness, as it relates to posttraumatic cognitions and posttraumatic stress symptoms (PTSS) among women reporting a history of sexual trauma. Seventy-two community-recruited women with a history of sexual trauma completed self-report measures of shame and guilt proneness and negative posttraumatic cognitions as well as a semi-structured interview assessing PTSS. There was an indirect effect of shame proneness on PTSS, through its positive association with negative cognitions about the self but not others or the world. Guilt proneness was not significantly related to PTSS or negative posttraumatic cognitions. The current paper outlines the importance of these findings and future directions for continuing to better understand the relations between shame and posttraumatic stress disorder symptoms and treatment.
Keywords: sexual trauma, posttraumatic stress, shame, guilt, negative cognitions
Posttraumatic stress disorder (PTSD) is comprised of re-experiencing, avoidance, negative alterations in beliefs and feelings, and hyperarousal symptoms (American Psychiatric Association [APA], 2013). Those who have experienced an interpersonal trauma have demonstrated rates of PTSD as high as 50% (Chivers-Wilson, 2006; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995), and increased anger, fear, shame, or guilt often follows interpersonal victimization (Beck et al., 2011; Lee & Scragg, 2001). To date, there has been extensive research on fear and anger in PTSD (Olatunji, Ciesielski, & Tolin, 2010; Shvil, Rusch, Sullivan, & Neria, 2013; Zuj, Palmer, Lommen, & Felmingham, 2016). However, shame and guilt are two emotions that are in need of more research in the context of PTSD (Saraiya & Lopez-Castro, 2016). Advanced understanding of shame and guilt in the context of posttraumatic stress symptomatology is particularly important, as people who develop PTSD and are experiencing shame or guilt have the tendency to avoid treatment (Foa, Keane, & Friedman, 2000), and shame has been identified as an important mediator of symptom change among patients who do receive PTSD treatment (Saraiya & Lopez-Castro, 2016).
Shame has been defined as a negative evaluation of the self with associated feelings of distress, worthlessness, and powerlessness (Tangney & Dearing, 2002). In contrast, guilt has been defined as a self-conscious emotion that relates to a sense of responsibility for one’s behavior during a negative event generally, and even victimization specifically (Lee, Scragg & Turner, 2001; Street & Arias, 2001; Tangney & Dearing, 2002). While guilt is associated with having done something that violates social/cultural norms or expectations, shame is associated with the perception that the person is a terrible, unlovable, or unworthy person (Tracy & Robins, 2004). Guilt is typically associated with actions aimed at repairing a perceived transgression, while shame is linked to behavioral avoidance and social withdrawal (Dickerson, Gruenewald, & Kemeny, 2004; Saraiya & Lopez-Castro, 2016). Compared to guilt, shame appears to be more strongly linked to the development and maintenance of posttraumatic stress symptoms (PTSS) following exposure to trauma (Beck et al., 2011; Ginzburg et al., 2009; Leskela, Dieperink, & Thuras, 2002; Pineles, Street, & Koenen, 2006; Street & Arias, 2001) and has been described as a more painful and potentially maladaptive emotion compared to guilt (Tangney, Stuwig, & Mashek, 2007).
Several studies have specifically linked shame-proneness, or the trait-like vulnerability or likelihood of experiencing shame in response to situations with ambiguous culpability (Tangney, Stuewig, & Mashek, 2007; Tangney, Wagner, & Gramzow, 1992), to more severe PTSS following exposure to trauma (Beck et al., 2015; Harman & Lee, 2010; Leskela, et al., 2002; Pineles et al., 2006; Semb et al., 2011; Street & Arias, 2001; Vidal, & Petrak, 2007); although some work has failed to document this association (Ojserkis et al., 2014; Shin et al., 2014). Considerably less is known regarding the specific role of shame-proneness in understanding the development, maintenance, and treatment of PTSS. In one cross-sectional study, Semb and colleagues (2011) found that shame-proneness was positively related to PTSS severity among recent victims of violent crime, in part through increased event-related shame (i.e., current feelings of shame when thinking about the trauma). There is also some evidence to suggest that shame-proneness may lead to negative alterations in self-referential cognitions that have been linked to worsened PTSS following traumatic event exposure (Beck et al., 2015; Harman & Lee, 2010).
One way in which shame-proneness may be associated with development and/or maintenance of PTSS is indirectly, through its negative influence on the way people think about or relate to themselves or the world following a traumatic event. Indeed, trauma-related negative alterations in cognitions and beliefs predict persistence of PTSS following exposure to trauma (Dekel, Peleg, & Solomon, 2013; Dunmore, Clark, & Ehlers, 2001; Scher, Suvak, & Resick, 2017), and change in negative cognitions is associated with greater improvement in other PTSS during treatment (Holliday, Link-Malcom, Morris, & Surís, 2014; Kumpula et al., 2017; Zalta et al., 2014). The importance of negative trauma-related cognitions for understanding psychopathology following exposure to trauma is underscored by the move to include two new symptoms in the updated diagnostic criteria for PTSD in the 5th edition of the Diagnostic and Statistical Manual for Mental Disorders (DSM-5; APA, 2013): 1) persistent and exaggerated beliefs about the self, other people, or the world as the result of a traumatic event(s); and 2) persistent and distorted cognitions involving self- or other-blame for the causes or consequences of the traumatic event.
Taken together, extant research and theory underscore the need to examine how shame-proneness (and guilt-proneness) are related to posttraumatic cognitions and PTSS. The current study aimed to advance understanding of how shame-proneness may relate to PTSS following sexual trauma. Studying these associations among female survivors of sexual assault is a useful first step, as elevated levels of shame, guilt, and PTSS have been observed in this population (Street & Arias, 2001). We hypothesized that shame-proneness, but not guilt-proneness, would evidence an indirect effect on PTSS, via negative posttraumatic cognitions about the self, the world, and self-blame.
Method
Participants
Participants were community-recruited adult women (Mage = 29.91, SD = 12.44) who took part in a larger study (N = 72) examining specific emotional responses to sexual assault (Badour & Feldner, 2016). The present investigation included all participants from the parent study with complete data on relevant study measures (N = 64). All participants reported an index trauma involving sexual victimization that satisfied the definition of a traumatic event as specified in criterion A for the diagnosis of PTSD in the 4th edition text revision of the DSM (DSM–IV–TR; APA, 2000). Participants endorsed at least one of the following acts: exposing of sexual organs (18.7%), touching/fondling of sexual organs (50.0%), vaginal intercourse (35.9%), oral intercourse (20.4%), anal intercourse (3.1%), and other sexual acts (6.3%). Participants’ relationship to the assailant included relative (36.0%), acquaintance (12.5%), stranger (12.5%), friend (9.4%), intimate partner/spouse (9.4%), date (4.7%), and other (14.1%). One participant did not indicate the relationship of her assailant. Fifty-three individuals (82.8%) reported experiencing more than one sexual trauma, and the average age at the time of the index trauma was 13.64 years old. Of the total sample, 17.2% met criteria for a current diagnosis of PTSD.
Measures
Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995).
The CAPS is a semi-structured interview that assesses DSM-IV-TR-defined PTSD diagnosis and provides an index of the frequency and severity of past-month posttraumatic stress symptoms. With strong interrater reliability (Blake et al., 1995), test-retest reliability (Weathers et al., 1991), and convergent validity with other measures of PTSD (Keane, Caddell, & Taylor, 1988), the CAPS is considered a gold standard in the assessment of PTSS and PTSD (Weathers, Keane, & Davidson, 2001). For the present study, the CAPS was used to collect details about participants’ index traumatic event, past-month PTSS (sum of frequency and intensity of 17 symptoms), and past-month diagnosis of PTSD using the 1, 2 scoring rules recommended by Weathers, Ruscio, and Keane (1999). For the purposes of the current study, PTSS severity was examined continuously due to research suggesting that symptoms are better represented by a continuum of symptom severity, with the PTSD diagnosis falling at the upper end of this continuum (Ruscio, Ruscio, & Keane, 2002). Accordingly, a PTSS severity score was computed by summing the frequency and intensity scores obtained for the 17 symptoms on the CAPS. Additionally, diagnostic status was obtained for descriptive purposes.
Posttraumatic Cognitions Inventory (PTCI; Foa, Ehlers, Clark, Tolin, & Orsillo, 1999).
The PTCI is a 36-item questionnaire designed to measure a range of trauma-related cognitions that are rated on a 7-point scale from 1 (Totally disagree) to 7 (Totally agree). The PTCI includes 3 subscales: Negative Cognitions about the Self (e.g., “There is something wrong with me as a person”), Negative Cognitions about the World (e.g., “People can’t be trusted”), and Self-Blame (e.g., “The event happened because of the way I acted”). The total score and the subscale scores have shown high internal consistency, with Cronbach’s α = .97 for the full measure and α = .86 to .97 for the subscales in previous studies (Foa et al., 1999). High test-retest reliability has been reported after both a 1-week (Spearman’s ρ = .74 - .89) and a 3-week interval (ρ = .80 - .85; Foa et al., 1999). Strong correlations between the PTCI and other measures of trauma-related cognitions (e.g., Personal Beliefs and Reactions Scale [Resick, Schnicke, & Markway, 1991] and World Assumptions Scale [Janoff-Bulman, 1989]) provide evidence of convergent validity. The PTCI has also shown good sensitivity and high specificity with regard to identifying individuals with and without PTSD in a traumatic event-exposed sample (Foa et al., 1999).
Test of Self-Conscious Affect-3 Short-Form (TOSCA-3 Short-Form; Tangney, Dearing, Wagner, & Gramzow, 2000).
The short form of the TOSCA-3 was used to measure shame-proneness and guilt-proneness. This questionnaire includes 11 negative vignettes (e.g., “While out with a group of friends, you make fun of a friend who’s not there.”) and asks respondents to indicate the degree to which they would be likely to experience each of four different cognitive/affective responses if faced with the situations detailed in the vignettes. Responses are recorded on a 0 (Not likely) to 5 (Very likely) scale. This measure includes four subscales (shame-proneness, guilt-proneness, externalization, detachment/unconcern), but only the shame- and guilt-proneness subscales were used in the present study. Good internal consistency has been reported for shame-proneness (α = .76 - .88), and adequate internal consistency for guilt-proneness (α = .57 - .83; Fedewa, Burns, & Gomez, 2005; Rusch et al., 2007; Tangney et al., 2000). Evidence of convergent and divergent validity has also been reported for both subscales (Fedewa et al., 2005).
Procedure
Participants were recruited from the Northwest Arkansas community via paper and electronic flyers, which advertised for a larger study examining specific emotional responses to sexual assault (Badour & Feldner, 2016). In order to decrease participant burden during the laboratory visit, participants were given the option to complete the TOSCA-3 as well as several other questionnaires not relevant to the present investigation online prior to their scheduled laboratory visit. After arriving at the lab and providing written consent, participants completed the CAPS interview and the PTCI. In addition to these measures, participants completed several other questionnaires and then engaged in a lab task, none of which is relevant to the present study.
Data Analytic Approach
First, zero-order correlations were examined. Two multiple indirect effects models with simultaneous entry were then conducted in SPSS 22 using the PROCESS custom dialog (Hayes, 2012) to test the hypotheses that shame-proneness, should relate to PTSS through associations with maladaptive posttraumatic cognitions (i.e., negative cognitions about the self, negative cognitions about the world, and self-blame). Specificity tests were conducted to examine the same model substituting shame-proneness with guilt-proneness. Variables were standardized (M = 0; SD = 1) to aid in interpretation of path coefficients. Bootstrapping with 5000 samples was employed to assess for the presence of indirect effects, as well as to contrast the size of individual indirect effects (Hayes, 2009; Williams & MacKinnon, 2008). A bias-corrected (BC) 95% confidence interval (CI) was used as the criterion for evaluating significance of the indirect effects. Indirect effects were considered statistically significant if zero was not included in the confidence interval (CI) generated based on the established sampling distribution. Additional models were run with age and age at index traumatic event exposure included as covariates. Inclusion of these covariates did not change the primary results of the process models described below.
Results
Descriptive Information and Zero-Order Correlations
Table 1 includes additional descriptive information and zero-order correlations among all variables, including Cronbach’s alphas corresponding to each measure. Current age negatively correlated with negative cognitions about the world. Guilt-proneness was positively correlated with age at index traumatic event exposure. Posttraumatic stress symptom severity was positively correlated with shame-proneness, negative cognitions about the self, negative cognitions about the world, and self-blame. Shame-proneness also was positively correlated with guilt-proneness, as well as with negative cognitions about the self, negative cognitions about the world, and self-blame. Of note, guilt-proneness was not significantly related to PTSS or any of the domains of posttraumatic cognitions.
Table 1.
Descriptive Data and Zero-Order Relations among Continuous Predictor and Criterion Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | M (SD) | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Current age | - | 29.91 (12.44) | |||||||
| 2. Age of index trauma | .19 | - | 13.64 (8.77) | ||||||
| 3. PTSS | −.17 | .04 | .92 | 31.78 (19.46) | |||||
| 4. Shame proneness | .07 | −.00 | .47* | .79 | 30.73 (7.55) | ||||
| 5. Guilt proneness | .22 | .25* | .14 | .36** | .56 | 48.67 (4.28) | |||
| 6. Negative cognitions about the self | −.16 | .09 | .75** | .55** | .10 | .96 | 2.30 (1.31) | ||
| 7. Negative cognitions about the world | −.25* | .06 | .52** | .37** | .14 | .55** | .91 | 4.05 (1.60) | |
| 8. Self-blame | −.04 | .14 | .35** | .25* | .16 | .54** | .37** | .80 | 2.80 (1.56) |
Note. N = 64; PTSS = posttraumatic stress symptoms; values in the diagonal represent Cronbach’s alphas.
p < .05
p < .01
Primary Hypothesis Tests
Shame-proneness.
Figure 1 presents results of the process analysis examining the association between shame-proneness and PTSS. The omnibus regression model accounted for 57.89% of the total variance in PTSS [F(4, 59) = 20.28, p < .001]. As predicted, the total effect (path c) of shame-proneness on PTSS was significant (β = .47, SE = .11, p < .001). Similarly, shame-proneness was positively related to negative cognitions about the self (path a1: β = .55, SE = .11, p < .001), negative cognitions about the world (path a2: β = .37, SE = .12, p = .003), and self-blame (path a3: β = .25, SE = .12, p = .04). Negative cognitions about the self were positively related to PTSS when accounting for both shame-proneness and negative cognitions about the world and self-blame (path b1: β = .67, SE = .13, p < .001). However, paths b2 (negative cognitions about the world: β = .15, SE = .10, p = .13) and b3 (self-blame: β = −.08, SE = .10, p = .42) were non-significant. Bootstrapping analysis revealed an indirect effect of shame-proneness on PTSS, through its positive association with negative cognitions about the self (path ab1: β = .37, SE = .12, BC 95% CI [0.17, 0.63]). Examination of the ratio of the indirect to total effect indicated that this indirect effect accounted for 79.7% of the total effect of shame-proneness on PTSS. The indirect effects of negative cognitions about the world (path ab2: β = .05, SE = .05, BC 95% CI [−0.02, 0.17]) and self-blame (path ab2: β = −.02, SE = .03, BC 95% CI [−0.12, 0.02]) were non-significant. Planned contrasts revealed that the ab1 path was significantly larger than the ab2 (β = .31, SE = .13, BC 95% CI [0.09, 0.61]) and ab3 paths (β = .39, SE = .13, BC 95% CI [0.17, 0.67]). The difference between the ab2 and ab3 paths was non-significant (β = .08, SE = .06, BC 95% CI [−0.02, 0.23]). Finally, the direct effect of shame-proneness on PTSS was no longer significant after accounting for the indirect effects (path c’: β = .06, SE = .10, p = .57).
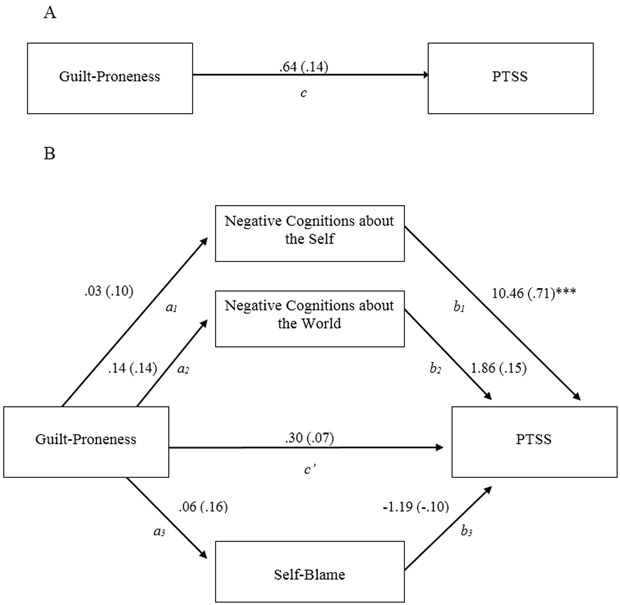
Figure 1.
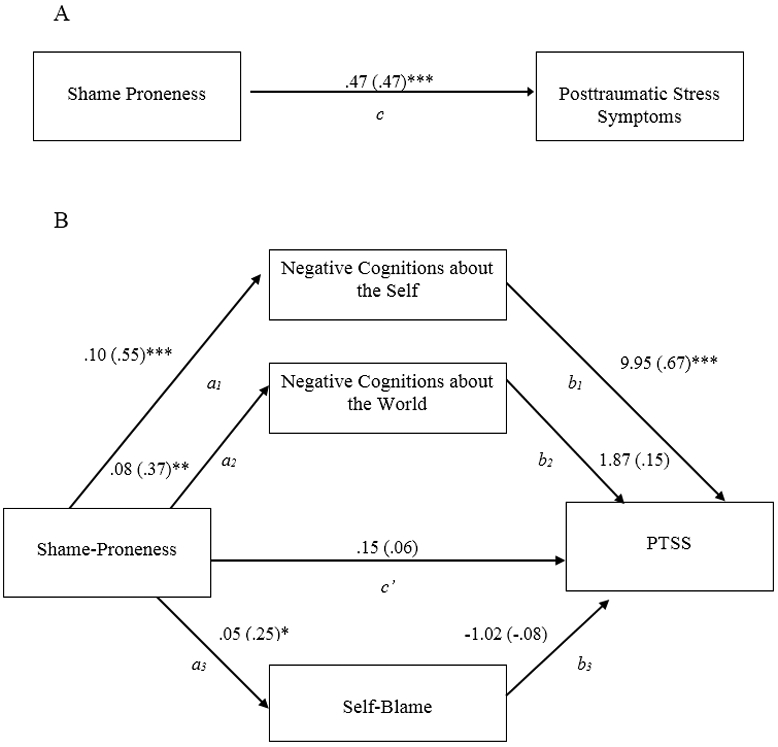
A diagram of the hypothesized indirect effects model. A: The total effect of shame proneness on posttraumatic stress symptoms. B: The indirect effects model with posttraumatic cognitions examined as possible factors accounting for the relation between shame proneness and posttraumatic stress symptoms. Unstandardized path coefficients are displayed, with corresponding standardized coefficients in parentheses. PTSS = posttraumatic stress symptoms
Guilt-proneness.
Figure 2 presents results of the process analysis examining the association between guilt-proneness and PTSS. The omnibus regression model accounted for 58.06% of the total variance in PTSS [F(4, 59) = 20.42, p < .001]. The total effect (path c) of guilt-proneness on PTSS was non-significant (β = .14, SE = .13, p = .27). Similarly, guilt-proneness was unrelated to negative cognitions about the self (path a1: β = .10, SE = .13, p = .43), negative cognitions about the world (path a2: β = .14, SE = .13, p = .27), and self-blame (path a3: β = .16, SE = .13, p = .20). Given the non-significant total effect (path c), and non-significant associations between guilt-proneness and negative posttraumatic cognitions (paths a1 – a3), an indirect effects analysis was not conducted.
Figure 2.
A diagram of the hypothesized indirect effects model. A: The total effect of guilt proneness on posttraumatic stress symptoms. B: The indirect effects model with posttraumatic cognitions examined as possible factors accounting for the relation between guilt proneness and posttraumatic stress symptoms. Unstandardized path coefficients are displayed, with corresponding standardized coefficients in parentheses. PTSS = posttraumatic stress symptoms
Discussion
To the best of our knowledge, this was the first study to examine associations among shame- and guilt-proneness, negative cognitions, and PTSS among sexually assaulted women. As hypothesized and consistent with previous research (Beck et al., 2011; Ginzburg et al., 2009; Leskela, Dieperink, & Thuras, 2002; Pineles, Street & Arias, 2011; Street, & Koenen, 2006; Tangney & Dearing, 2002), shame-proneness, but not guilt-proneness, was positively associated with PTSS. More specifically, shame-proneness was indirectly associated with PTSS via increased negative cognitions about the self; however, the paths via negative cognitions about the world and self-blame were not significant.
It is not surprising that shame-proneness would be more strongly linked to PTSS via negative cognitions about the self as compared to negative cognitions about the world, given that shame is inherently an ego-centric emotion (Tangney et al., 2007). Negative cognitions about the self, as measured by the PTCI, refers to not only a general negative view of the self, but also includes items measuring hopelessness, the perception of permanent change as a result of the trauma, and negative interpretation of symptoms (Foa et al., 1999). Although preliminary, these findings suggest that individuals who are more shame-prone may be more likely to experience negative cognitions about the self following sexual trauma, which may then in turn lead to the development or maintenance of PTSS. However, it will be critical to replicate these findings using a prospective design, as it is possible that the presence of PTSS may lead to a worsening of maladaptive self-focused cognitions over time.
While it may seem that self-blame should produce a similar result to negative cognitions about the self, other studies have also failed to document a correlation between the self-blame scale of the PTCI and PTSS (Beck et al., 2004; Shin et al., 2014), and questions have been raised regarding the validity of the self-blame scale (Beck et al., 2004). It has been suggested that this scale does not adequately discriminate between perceived characterological self-blame (i.e., the traumatic event occurred because of uncontrollable or unchangeable aspects of the self, such as personality characteristics) versus behavioral self-blame (i.e., the traumatic event occurred because of controllable or modifiable factors of the self, such as specific actions or behaviors; Startup, Makgekgenene, & Webster, 2007). It stands to reason that cognitions regarding characterological self-blame would be more likely to be influenced by shame-proneness, while behavioral self-blame would be more likely to be influenced by guilt-proneness. However, a more discriminative measure of posttraumatic self-blame cognitions is needed to test this prediction.
It is also possible that the nature of the sample included in this study influenced the results. Although nearly 20% of the sample met criteria for a current diagnosis of PTSD, and evidence suggests that PTSS is best represented by a dimensional construct (Ruscio et al., 2002), the findings may have differed among a clinical or treatment seeking sample of women with a history of sexual trauma. Furthermore, including women exposed to varying traumatic event types in order to compare links between shame-proneness and negative posttraumatic cognitions across traumatic event types would be a useful extension to extant research.
Consistent with findings from other studies (Leskela et al., 2002; Street & Arias, 2001), guilt-proneness was not directly or indirectly related to PTSS. It is possible that previously observed associations between PTSS and guilt were driven primarily by the closely related construct of shame. Accordingly, when an assessment approach that disentangles shame and guilt is adopted, shame emerges as the key factor related to PTSS (Bannister, Colvonen, Angkaw, & Norman, 2019).
Limitations of the current study need to be considered when drawing inferences based on these results. First, the sample was limited to women who reported a history of sexual assault. Consequently, the current results cannot be generalized to men or to populations suffering from PTSS related to other trauma types. In addition, the cross-sectional and correlational nature of the study design also constrains inferences that can be drawn. Although these types of designs can be useful initial steps in a research program aiming to inform ultimate longitudinal and experimental studies, they do not allow for inferences regarding temporal patterning or cause-and-effect relations (Kraemer, Yesavage, Taylor, & Kupfer, 2000; Rutter, 1994). This study does, however, support extending examination of links between shame, negative cognitions about the self, and sexual assault to longitudinal research, which will significantly advance our understanding of the role of shame in the development of negative cognitions and PTSD. Further, reliance on retrospective self-report measures introduces measurement error (via, for example, memory biases) and other biases (e.g., reporting biases). Accordingly, inferences drawn based on the current results are necessarily cautious. Finally, PTSS in this study was assessed via criteria outlined in the DSM-IV-TR (APA, 2000). This is notable, as 1) maladaptive posttraumatic cognitions about the self, others, or the world, and 2) persistent distorted blame of the self or others for the causes or consequences of a traumatic event were determined in DSM-5 to be characteristic features of the PTSD diagnosis and are included as specific symptoms within the negative alterations in cognitions and mood symptom cluster of PTSD (Cluster D). It will thus be increasingly important for future studies to consider the time course of symptom development within the symptoms that comprise the PTSD diagnosis to determine whether the development of negative posttraumatic cognitions occurs immediately following traumatic event exposure, or if maladaptive posttraumatic cognitions emerge following other symptoms of PTSD, such as intrusive reexperiencing or hypervigilance.
The above limitations notwithstanding, there is significant potential for research on links among shame, negative posttraumatic cognitions, and PTSS for improving the health of survivors of sexual assault. For example, Cognitive Processing Therapy (Resick, Nishith, Millie, Catherine, & Feuer, 2002) is an empirically supported treatment for PTSD that targets the modification of cognitions thought to maintain posttraumatic stress symptoms. Advancing our understanding of how shame may systematically relate to posttraumatic cognitions has potential for improving such cognitive therapies’ ability to specifically target types of posttraumatic cognitions that maintain PTSS associated with certain traumatic events. Moreover, contemporary approaches to reducing shame-proneness, including interventions aimed at increasing self-compassion (Au et al., 2017; Cȃndea & Szentágotai-Tătar, 2018; Gilbert & Procter, 2006), may serve as a useful adjunctive or alternative intervention to traditional PTSD treatment. Furthermore, understanding how proneness to shame increases the likelihood that a person may develop relatively elevated PTSS following sexual assault will enhance our currently limited ability to deliver brief preventive interventions (e.g., brief education in cognitive restructuring) to women at particularly elevated risk for developing problems following sexual assault. Taken together, it appears women who are particularly prone to experiencing shame are also likely to experience elevated negative posttraumatic cognitions about the self, and both of these are related to relatively elevated levels of sexual assault-related posttraumatic stress symptoms.
Acknowledgments
This research was supported by a National Research Service Award (F31 MH092994) from the National Institute of Mental Health (NIMH) awarded to Dr. Badour. The expressed views do not necessarily represent those of NIMH
Contributor Information
Christal L. Badour, University of Kentucky
Courtney E. Dutton, Durham VA Healthcare System
Jessica J. Wright, University of Arkansas
Alyssa C. Jones, University of Kentucky
Matthew T. Feldner, University of Arkansas, Canopy Growth
References
- American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author [Google Scholar]
- Au T, Sauer-Zavala S, King M, Petrocchi N, Barlow D, & Litz B (2017). Compassion-based therapy for trauma-related shame and posttraumatic stress: Initial evaluation using a multiple baseline design. Behavior Therapy, 48, 207–221. [DOI] [PubMed] [Google Scholar]
- Badour CL, & Feldner M (2016). Disgust and imaginal exposure to memories of sexual trauma: Implications for the treatment of posttraumatic stress. Psychological Trauma: Theory, Research, Practice, and Policy, 8, 267–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bannister JA, Colvonen PJ, Angkaw AC, & Norman SB (2019). Differential relationships of guilt and shame on posttraumatic stress disorder among veterans. Psychological Trauma: Theory, Research, Practice, and Policy, 11(1), 35–42. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, & Keane TM (1995). The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress, 8, 75–90. [DOI] [PubMed] [Google Scholar]
- Beck J, Coffey S, Palyo S, Gudmundsdottir B, Miller L, & Colder C (2004). Psychometric properties of the Posttraumatic Cognitions Inventory (PTCI): A self-protective cognition? Behaviour Research and Therapy, 45, 395–403. [DOI] [PubMed] [Google Scholar]
- Beck JG, McNiff J, Clapp JD, Olsen SA, Avery ML, & Hagewood JH (2011). Exploring negative emotion in women experiencing intimate partner violence: shame, guilt, and PTSD. Behavior Therapy, 42, 740–750. [DOI] [PubMed] [Google Scholar]
- Beck J, Reich C, Woodward M, Olsen S, Jones J, & Patton S (2015). How do negative emotions relate to dysfunctional posttraumatic cognitions? An examination of interpersonal trauma survivors. Psychological Trauma: Theory, Research, Practice, and Policy, 7, 3–10. [DOI] [PubMed] [Google Scholar]
- Cȃndea D-M, & Szentágotai-Tătar A (2018). The impact of self-compassion on shame-proneness in social anxiety. Mindfulness, 9, 1816–1824. [Google Scholar]
- Chivers-Wilson KA (2006). Sexual assault and posttraumatic stress disorder: A review of the biological, psychological and sociological factors and treatments. McGill Journal of Medicine, 9, 111–118. [PMC free article] [PubMed] [Google Scholar]
- Dekel S, Peleg T, & Solomon Z (2013). The relationship of PTSD to negative cognitions: A 17-year longitudinal study. Psychiatry, 76, 241–255. [DOI] [PubMed] [Google Scholar]
- Dickerson SS, Gruenewald TL, & Kemeny ME (2004). When the social self is threatened: Shame, physiology, and health. Journal of Personality, 72(6), 1191–1216. [DOI] [PubMed] [Google Scholar]
- Dunmore E, Clark DM, & Ehlers A (2001). A prospective investigation of the role of cognitive factors in persistent posttraumatic stress disorder (PTSD) after physical or sexual assault. Behaviour Research and Therapy, 39, 1063–1084. [DOI] [PubMed] [Google Scholar]
- Fedewa BA, Burns LR, & Gomez AA (2005). Positive and negative perfectionism and the shame/guilt distinction: Adaptive and maladaptive characteristics. Personality and Individual Differences, 38, 1609–1619. [Google Scholar]
- Foa EB, Ehlers A, Clark DM, Tolin DF, & Orsillo SM (1999). The posttraumatic cognitions inventory (PTCI): Development and validation. Psychological Assessment, 11, 303–314. [Google Scholar]
- Foa EB, Keane TM, & Friedman MF (2000). Guidelines for treatment of PTSD. Journal of Traumatic Stress, 13, 539–588. [DOI] [PubMed] [Google Scholar]
- Gilbert P, & Proctor S (2006). Compassionate mind training for people with high shame and self-criticism: Overview and pilot study of a group therapy approach. Clinical Psychology and Psychotherapy, 13, 353–379. [Google Scholar]
- Ginzburg K, Butler L, Giese-Davis J, Cavanaugh C, Neri E, Koopman C,…Spiegel D (2009). Shame, guilt, and posttraumatic stress disorder in adult survivors of childhood sexual abuse at risk for human immunodeficiency virus: Outcomes of a randomized clinical trial of group psychotherapy treatment. Journal of Nervous and Mental Disease, 197, 536–542. [DOI] [PubMed] [Google Scholar]
- Harman R, & Lee D (2010). The role of shame and self-critical thinking in the development and maintenance of current threat in post-traumatic stress disorder. Clinical Psychology and Psychotherapy, 17, 13–24. [DOI] [PubMed] [Google Scholar]
- Hayes A (2009). Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs, 76, 408–420. [Google Scholar]
- Holliday R, Link-Malcom J, Morris E, & Surís A (2014). Effects of cognitive processing therapy on PTSD-related negative cognitions in military veterans with military sexual trauma. Military Medicine, 179, 1077–1082. [DOI] [PubMed] [Google Scholar]
- Janoff-Bulman R (1989). Assumptive worlds and the stress of traumatic events: Applications of the schema construct. Social Cognition, 7, 113–136. [Google Scholar]
- Keane TM, Caddell JM, & Taylor KL (1988). Mississippi Scale for Combat-Related Posttraumatic Stress Disorder: three studies in reliability and validity. Journal of Consulting and Clinical Psychology, 56, 85–90. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, & Nelson CB (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048–1060. [DOI] [PubMed] [Google Scholar]
- Kraemer H, Yesavage J, Taylor J, & Kupfer D (2000). How can we learn about developmental processes from cross-sectional studies, or can we? American Journal of Psychiatry, 157, 163–171. [DOI] [PubMed] [Google Scholar]
- Kruger LE (2014). Is there more to the experience of war trauma that PTSD? The development of moral injury and its impact on soldiers. Journal of Military and Government Counseling, 2, 136–145. [Google Scholar]
- Kubany ES, Abueg FR, Owens JA, Brennan JM, Kaplan AS, & Watson SB (1995). Initial examination of a multidimensional model of trauma-related guilt: Applications to combat veterans and battered women. Journal of Psychopathology and Behavioral Assessment, 17, 353–376. [Google Scholar]
- Kumpula M, Pentel K, Foa E, LeBlanc N, Bui E, McSweeney L, Knowles K,…Rauch S (2017). Temporal sequencing of change in posttraumatic cognitions and PTSD symptom reduction during prolonged exposure therapy. Behavior Therapy, 48, 156–165. [DOI] [PubMed] [Google Scholar]
- La Bash H, & Papa A (2014). Shame and PTSD symptoms. Psychological Trauma, Theory, Research, Practice, and Policy, 6, 159–166. [Google Scholar]
- Lee DA, Scragg P, & Turner S (2001). The role of shame and guilt in traumatic events: A clinical model of shame-based and guilt-based PTSD. British Journal of Medical Psychology, 74, 451–466. [DOI] [PubMed] [Google Scholar]
- Leskela J, Dieperink M, & Thuras P (2002). Shame and posttraumatic stress disorder. Journal of Traumatic Stress, 15, 223–226. [DOI] [PubMed] [Google Scholar]
- Olatunji B, Ciesielski B, & Tolin D (2010). Fear and loathing: A meta-analytic review of the specificity of anger in PTSD. Behavior Therapy, 41, 93–105. [DOI] [PubMed] [Google Scholar]
- Ojserkis R, McKay D, Badour C, Feldner M, Arocho J, & Dutton C (2014). Alleviation of moral disgust, shame, and guilt in posttraumatic stress reactions: An evaluation of comprehensive distancing. Behavior Modification, 38, 801–836. [DOI] [PubMed] [Google Scholar]
- Pineles S, Street A, & Koenen K (2006). The differential relationships of shame-proneness and guilt-proneness to psychological and somatization symptoms. Journal of Social and Clinical Psychology, 25, 688–704. [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, & Feuer CA (2002). A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology, 70, 867–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Schnicke MK, & Markway BG (1991, November). The relationship between cognitive content and posttraumatic stress disorder. Paper presented at the annual meeting of the Association for Advancement of Behavior Therapy, New York. [Google Scholar]
- Rüsch N, Corrigan PW, Bohus M, Jacob GA, Brueck R, & Lieb K (2007). Measuring shame and guilt by self-report questionnaires: A validation study. Psychiatry Research, 150, 313–325. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Ruscio J, & Keane TM (2002). The latent structure of post-traumatic stress disorder. A taxometric investigation of reactions to extreme stress. Journal of Abnormal Psychology, 111, 290–301. [PubMed] [Google Scholar]
- Rutter M (1994). Beyond longitudinal data: Causes, consequences, changes, and continuity. Journal of Consulting and Clinical Psychology, 62, 928–940. [DOI] [PubMed] [Google Scholar]
- Saraiya T, & Lopez-Castro T (2016). Ashamed and afraid: A scoping review of the role of shame in post-traumatic stress disorder. Journal of Clinical Medicine, 5, 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scher C, Suvak M, & Resick P (2017). Trauma cognitions are related to symptoms up to 10 years after cognitive behavioral treatment for posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy, 9, 750–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semb O, Stromsten L, Sundbom E, Fransson P, & Henningsson M (2011). Distress after a single violent crime: How shame-proneness and event-related shame work together as risk factors for post-victimization symptoms. Psychological Reports, 109, 3–23. [DOI] [PubMed] [Google Scholar]
- Shin K, Cho S-M, Lee S, & Chung Y (2014). A pilot prospective study of the relationship among cognitive factors, shame, and guilt proneness on posttraumatic stress disorder symptoms in female victims of sexual violence. Journal of Korean Medical Science, 29, 831–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shvil E, Rusch H, Sullivan G, & Neria Y (2013). Neural, psychophysiological, and behavioral markers of fear processing in PTSD: A review of the literature. Current Psychiatry Reports, 15, 358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Startup M, Makgekgenene L, & Webster R (2007). The role of self-blame for trauma as assessed by the Posttraumatic Cognitions Inventory (PTCI): A self-protective cognition? Behavior Research and Therapy, 45, 395–403. [DOI] [PubMed] [Google Scholar]
- Street AE, & Arias I (2001). Psychological abuse and posttraumatic stress disorder in battered women: Examining the roles of shame and guilt. Violence and Victims, 16, 65–78. [PubMed] [Google Scholar]
- Tangney JP (1993) Shame and guilt. In Costello CG (Ed.), Symptoms of Depression (pp.161–180). New York: John Wiley. [Google Scholar]
- Tangney JP, & Dearing RL (2002). Shame and Guilt. New York: Guilford. [Google Scholar]
- Tangney JP, Dearing RL, Wagner PE, & Gramzow R (2000). The test of self-conscious affect-3 (TOSCA-3). Fairfax, VA: George Mason University. [Google Scholar]
- Tangney J, Stuewig J, & Mashek D (2007). Moral emotions and moral behavior. Annual Review of Psychology, 58, 345–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tangney JP, Wagner PE, & Gramzow R (1992). Proneness of shame, proneness to guilt, and psychopathology. Journal of Abnormal Psychology, 103, 469 – 478. [DOI] [PubMed] [Google Scholar]
- Tracy J, & Robins R (2004). Putting the self into self-conscious emotions: A theoretical model. Psychological Inquiry, 15, 103–125. [Google Scholar]
- Vidal M, & Petrak J (2007). Shame and adult sexual assault: A study with a group of female survivors recruited from an East London population. Sexual and Relationship Therapy, 22, 159–171. [Google Scholar]
- Weathers FW, Blake DD, & Litz BT (1991, August). Reliability and validity of a new structured interview for PTSD. In Keane TM (Chairperson), Advances in psychometric assessment of combat-related post-traumatic stress disorder. Symposium presented at the meeting of the American Psychological Association, San Francisco, CA. [Google Scholar]
- Weathers FW, Keane TM, & Davidson JR (2001). Clinician-administered PTSD scale: A review of the first ten years of research. Depression and Anxiety, 13(3), 132–156. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Ruscio AM, & Keane TM (1999). Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychological Assessment, 11, 124–133. [Google Scholar]
- Williams J, & MacKinnon DP (2008). Resampling and distribution of the product methods for testing indirect effects in complex models. Structural Equation Modeling, 15, 23–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalta A, Gillihan S, Fisher A, Mintz J, McLean C, Yehuda R, & Foa E (2014). Change in negative cognitions associated with PTSD predicts symptom reduction in prolonged exposure. Journal of Consulting and Clinical Psychology, 82, 171–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuj D, Palmer M, Lommen M, & Felmingham K (2016). The centrality of fear extinction in linking risk factors to PTSD: A narrative review. Neuroscience & Biobehavioral Reviews, 69, 15–35. [DOI] [PubMed] [Google Scholar]