Abstract
Background
Timely use of Sacubitril/Valsartan has the potential to significantly improve cardiac function and dramatically reduce secondary mitral regurgitation (MR) severity even in patients presenting with acute decompensated heart failure (HF), not only in compensated chronic HF patients. The outstanding impact of echocardiography is obvious in monitoring improvement of cardiac function and MR severity in patients with HF with reduced ejection fraction (HFrEF).
Case summary
We report a relevant case of an elderly patient who presented with acute decompensated HF and severe MR. He was symptomatic despite being on maximally tolerated doses of ACEI, beta-blockers, and diuretics. Left ventricular ejection fraction (LVEF) improved from 15% to 35% 2 weeks following initiation of Sacubitril/Valsartan during second HF hospitalization. There was a dramatic improvement of patient’s symptoms from New York Heart Association (NYHA) Class IV to NYHA I. N-terminal pro B-type natriuretic peptide reduced from 9000 pg/mL to 800 pg/mL. Coronary angiography depicted three-vessel coronary artery disease. The patient was advised to undergo coronary artery bypass graft surgery with mitral valve repair, then followed by implantation of a cardiac resynchronization therapy-defibrillator device (CRT-D) if no LV function improvement is observed after revascularization. The electrocardiogram showed Q waves in inferior leads with QRSd ≥ 125 ms, hence a good candidate for CRT. Following an elective percutaneous coronary intervention, LVEF further improved to 50%. The patient became asymptomatic with preserved LVEF on follow-up for 18 months later.
Discussion
This case report documents the swift echocardiographic and symptom improvement in a decompensated end-stage HF patient when Sacubitril/Valsartan initiated during acute setting.
Keywords: Angiotensin receptor-neprilysin inhibitor, Sacubitril/Valsartan, CRT-D, Echocardiography, heart failure with reduced ejection fraction, Coronary artery disease, NT-proBNP, Case report
Learning points
Dramatic reduction in secondary mitral regurgitation severity is possible when using angiotensin receptor-neprilysin inhibitor even in patients with acute decompensated heart failure (HF).
The outstanding impact of multimodality imaging is obvious in monitoring the improvement of cardiac function and deciding for revascularization.
It is necessary to make a change in clinical practice to early implement this lifesaving therapy in acute decompensated HF patients.
There was an obvious role of Sacubitril/Valsartan in improving symptoms and New York Heart Association class with the dramatic swift improvement of left ventricular ejection fraction (LVEF) in acute decompensated HF with reduced ejection fraction patients when started during hospital admission and the acute setting.
Apart from the improvement of LV function, there is a significant reduction of secondary mitral regurgitation severity, pulmonary hypertension, and normalization of right ventricular function after starting Sacubitril/Valsartan.
Introduction
Sacubitril/Valsartan is a first-in-class combination of angiotensin receptor blocker (ARB) and neprilysin inhibitor. It is now recommended as the first line for the treatment of chronic heart failure with reduced ejection fraction (HFrEF). It is also recommended in cases that remain symptomatic despite optimal medical therapy.1
Compared with enalapril, sacubitril/valsartan reduced the composite endpoint of cardiovascular death or HF hospitalization and is recommended as an alternative for angiotensin‐converting enzyme inhibitors (ACEI) and (ARB) in patients with HFrEF and New York Heart Association (NYHA) Class II–III symptoms.2,3
Timeline
| Time intervals | Clinical status | Echo findings | Treatment | Investigations |
|---|---|---|---|---|
| Day 1 of admission | Acute decompensated CHF-dyspnoea New York Heart Association (NYHA) Class IV for the past 10 days | Severe Bi-ventricular dysfunction. Left ventricular ejection fraction (LVEF) 15–20%, severe mitral regurgitation (MR), severe tricuspid regurgitation, severe pulmonary hypertension, right ventricular systolic pressure (RVSP) 70 mmHg. Frequent B-lines on lung us | Previous non-optimal medical treatment: bisoprolol 2.5 mg o.d. and ramipril 1.25 mg o.d. Bisoprolol stopped on admission. |
NT-pro BNP > 9000 pg/mL (normal <450 pg/mL for patients aged 75–99 years) Creatinine Cl. 45 mL/min (normal 107–139 mL/min), S. Potassium 3.8 mmol/L (normal 3.5–5.0 mmol/L), Haemoglobin 14 gm/dL (normal 13.8–17.2 g/dL) |
| Day 5 of admission | Dyspnoea NYHA Class III after starting diuretics | Same as before, however no B lines on lung us | Furosemide infusion, aspirin 100 mg o.d., spironolactone 25 mg o.d., Ramipril 2.5 mg b.i.d., Rosuvastatin 20 mg o.d., Empagliflozin 10 mg o.d. | Coronary angiogram: severe triple coronary artery disease |
| Day 1 of discharge after 10 days of hospitalization | Dyspnoea NYHA Class II–III | Same as before | Same as before plus added on top carvedilol 6.25 mg b.i.d. (Bisoprolol 5 mg o.d. stopped due to hypotension). Discharged on Lasix 40 mg oral b.i.d. | |
| Week 2 post-discharge (in outpatient clinic) | Recurrent clinic visits due to dyspnoea NYHA Class III and poor effort tolerance | Mild LV function improvement to 25% | Enalapril 5 mg bd, up-titrated carvedilol to 12.5 mg b.i.d., up-titrated spironolactone to 50 mg o.d.- received Lasix 40 mg IV bolus injection – Enalapril changed to Valsartan 160 mg o.d. due to ACEI intolerance |
NT-pro-BNP >6000 pg/ml Creatinine Cl. 47 ml/min, S. Potassium 4.2 mmol/L |
| Day 1 of re-admission (4 weeks post-discharge) | Recurrent hospitalization due to acute decompensated heart failure. | Same as before | Sacubitril/Valsartan 24 mg/26 mg b.i.d. with 36 h wash-out period. Up titrated Furosemide to 80 mg b.i.d. Metoprolol 50 mg b.i.d. added on discharge due to hypotension with carvedilol. | |
| Week 1 post-discharge after 2 weeks of 2nd hospitalization | Improvement to dyspnoea NYHA class I–II | LVEF improved to 35–40%, MR severity to Grade II, TR severity to Grade I. Marked RVSP reduction to 25 mmHg | Sacubitril/Valsartan dose then increased to 49 mg/51 mg BD | NT-pro-BNP 800 pg/ml |
| Week 3 post-discharge |
Asymptomatic. Improved quality of life |
Reduced Furosemide to 40 mg OD | Myocardial perfusion scan: viable left anterior descending (LAD) and left circumflex (LCX)/optimal medical (OM) territories. | |
|
Week 5 post-discharge |
Asymptomatic. Improved quality of life |
LVEF 50% | Percutaneous coronary intervention to LAD and LCX/OM arteries, angiotensin receptor-neprilysin inhibitor, Aspirin + Clopidogrel, Metoprolol 50 mg b.i.d., Empagliflozin 25 mg o.d., Rosuvastatin 20 mg o.d., stopped diuretics | Creatinine Cl. 56 mL/min |
| Follow-up visit 18 months later |
Asymptomatic Improved quality of life |
LVEF 50% | Sacubitril/Valsartan 49 mg/51 mg b.i.d., Metoprolol 50 mg b.i.d., Aspirin o.d., Empagliflozin 25 mg o.d., Rosuvastatin 20 mg o.d. |
Case presentation
Herein, we describe a case report of a low body weight 74-year-old Asian male patient with a body mass index of 17.2 kg/m2 who presented with acute decompensated HF with both end-stage systolic and diastolic HF including right ventricular (RV) failure.
He is known to have type II diabetes mellitus, hypertension, and a previous presumed diagnosis of dilated cardiomyopathy (DCM) in another facility on non-optimal medical therapy (OMT) for the past 2 years.
On presentation, the patient was dyspnoeic (NYHA functional Class IV) for the previous 10 days.
Physical examination revealed wide-spread coarse inspiratory crepitations extending till mid-zonal area of both lungs with III/IV harsh systolic murmur and S3 gallop heard over the apex.
Vitals were as follows normal temperature, blood pressure 120/80 mmHg, heart rate 87 beats/minute, respiratory rate 30/minute, SpO2 at room air 90%.
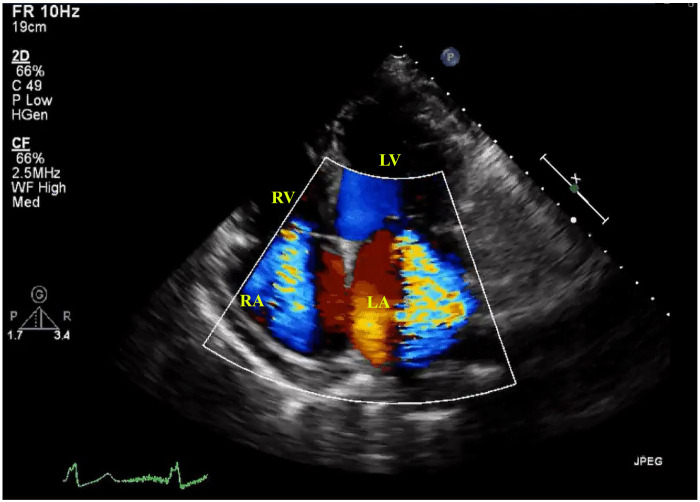
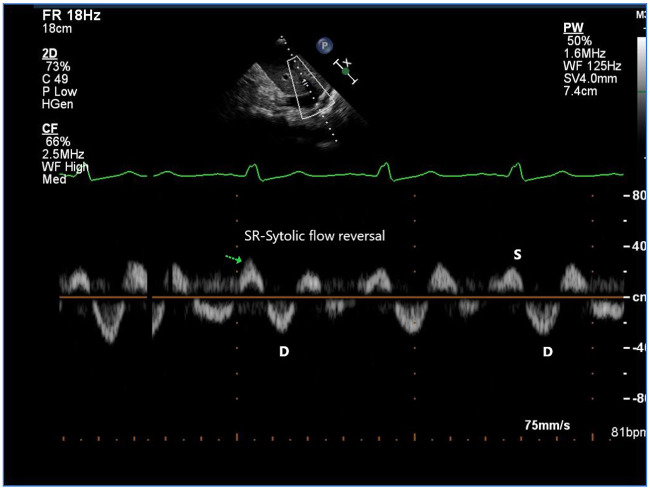
Initial work up included 2D echocardiography (Echo) which showed severe LV dysfunction with an estimated LVEF of 15–20% (Video 1), with global hypokinesia, apical and inferolateral wall akinesia, suggestive of ischaemic dilated cardiomyopathy. There was severe RV dysfunction with interventricular septal flattening in diastole suggesting RV volume overload (Video 2). There was also severe tricuspid regurgitation (TR) with high right ventricular systolic pressures (RVSP) of 70 mmHg suggesting severe pulmonary hypertension (PH). There was severe grade IV mitral regurgitation (MR) (Video 3) and Grade IV TR (Figure 1) with hepatic vein systolic flow reversal on pulsed wave Doppler (PWD) (Figure 2). Mitral regurgitation severity was quantified by a vena contracta area of 0.8 cm, an effective regurgitant orifice area (EROA) by proximal isovelocity surface area (PISA) method of 0.4 cm2, peak velocity of the MR jet of 5 m/s by continuous-wave Doppler, in addition to the presence of PH derived from TR jet velocity and a dominant early filling (E velocity 1.5 m/s) by PWD of mitral inflow.
Figure 1.
2D transthoracic echocardiogram with colour Doppler on admission, A4C view demonstrating severe grade IV TR and severe grade IV MR. LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.
Figure 2.
Transthoracic echocardiogram with pulsed wave Doppler (PWD) interrogation across hepatic vein on admission illustrating hepatic vein systolic flow reversal due to severe TR. D wave, atrial diastole; S wave, ventricular systole; SR, systolic atrial flow reversal.
Furthermore, there was a restrictive pattern Grade III diastolic dysfunction with elevated LV filling pressure by tissue Doppler imaging.
Lung ultrasound demonstrated frequent B-lines on both lungs denoting pulmonary interstitial oedema.
The patient was hospitalized and started on Frusemide infusion at a rate of 10 mg/h after an IV bolus dose of 40 mg, besides Spironolactone 25 mg o.d., Ramipril 1.25 mg o.d., Rosuvastatin 20 mg o.d., Empagliflozin 10 mg o.d., and Aspirin 100 mg o.d.
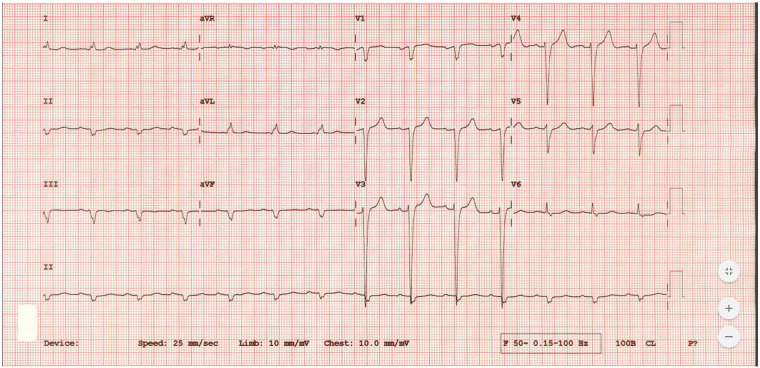
Electrocardiogram showed a sinus rhythm with interventricular conduction delay and QRS duration ≥ 125 ms. Q waves seen in inferior leads (Figure 3).
Figure 3.
Baseline 12-leads electrocardiogram showing sinus rhythm with wide QRS complex and interventricular conduction delay with increased duration of QRS complex ≥ 125 ms. Q waves seen in inferior leads.
Chest X-ray showed signs of pulmonary congestion.
N-terminal pro B-type natriuretic peptide (NT-proBNP) was over 9000 pg/mL (normal <450 pg/mL). Serum potassium 3.8 mmol/L (normal 3.5–5.0 mmol/L), serum sodium 141 mmol/L (normal 135–145 mmol/L), haemoglobin 14 g/dL (normal 13.8–17.2 g/dL), and creatinine clearance of 45 mL/min (normal 107–139 mL/min).
Consequently, the patient improved on medical therapy. Coronary angiography (CAG) was done during hospitalization and revealed triple vessel disease with 90% diffuse tight lesions in proximal to mid-left anterior descending (LAD) artery, 90% significant lesion in both obtuse marginal (OM) branches of left circumflex (LCX) artery, and chronic total occlusion (CTO) of right coronary artery (RCA) with retrograde filling from the left system (Supplementary material online,Videos S1 andS2).
In view of severe MR, triple vessel disease and severe LV and RV dysfunction; accordingly we recommended coronary artery bypass graft (CABG) surgery combined with mitral valve repair (MVr), then followed by implantation of a cardiac resynchronization therapy defibrillator (CRT-D) device if no LV function improvement achieved after coronary revascularization.
Awaiting myocardial viability stress test before revascularization and with efforts to improve LV function, we started maximally tolerated dose of ACEI using Ramipril 2.5 mg b.i.d., however, the patient developed mild hypotension with dizziness even with reducing diuretic dose from 40 mg b.i.d. to 20 mg b.i.d. of Frusemide. We then shifted the patient to Enalapril 5 mg b.i.d. that was stopped due to ACEI intolerance in the form of dry tickling cough. Eventually, we started valsartan with 80 mg o.d. then titrated to 160 mg o.d. Additionally, we had to change to different classes of beta-blockers. After hypotension with Bisoprolol 5 mg o.d. it was stopped and then the patient was started on Carvedilol 6.25 mg b.i.d. that resulted as well in hypotension after gradually increasing its dose to 12.5 mg b.i.d., with complaints of generalized weakness and fatigue. Finally, we shifted the patient on slowly increasing the dose of Metoprolol up to 50 mg b.i.d. with no resulting adverse effects. Patient was maintained as well on mineralocorticoid receptor antagonists (MRA) (Spironolactone 25 mg o.d.), sodium-glucose cotransporter-2 (SGLT-2) inhibitors (Empagliflozin 10 mg o.d.), aspirin 100 mg OD, and Furosemide 40 mg b.i.d.
Patient could not financially afford Sacubitril/Valsartan.
He experienced recurrent hospitalization due to acute decompensated HF. After hospital discharge, the patient showed up every other day in the hospital for Furosemide injection to alleviate his HF symptoms.
Three weeks later during a re-admission with heart failure, Sacubitril/Valsartan in a dose of 24 mg/26 mg PO b.i.d. was offered to the patient. A dramatic improvement in symptoms from NYHA Class IV to Class II was observed 5 days after starting Sacubitril/Valsartan. NYHA class also improved to NYHA I 2 weeks after treatment initiation. Following discharge, the patient was walking 4 km everyday with good exercise tolerance. N-terminal pro-B-type natriuretic peptide also decreased to 800 pg/mL after 2 weeks.
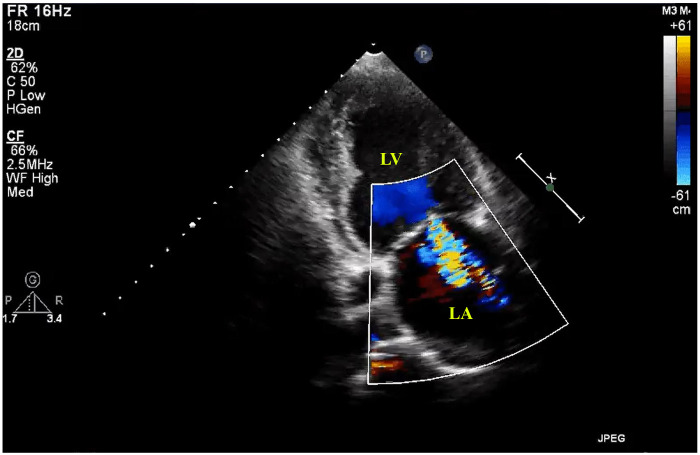
Screening 2D echo on hospital discharge showed dramatic improvement of LVEF to 35–40% with significant reversal of LV remodelling. MR improved to Grade II (Figure 4,Supplementary material online,Video S3) and TR improved to Grade I (Supplementary material online,Video S4). Moreover, RVSP was reduced to 30 mmHg (Supplementary material online,Figure S1). Additionally, the diastolic function improved to Grade I (Supplementary material online,Figure S2).
Figure 4.
2D transthoracic echocardiogram, A2C view showing reduction of MR severity to grade II after 2 weeks of starting Sacubitril/Valsartan. LA, left atrium; LV, left ventricle.
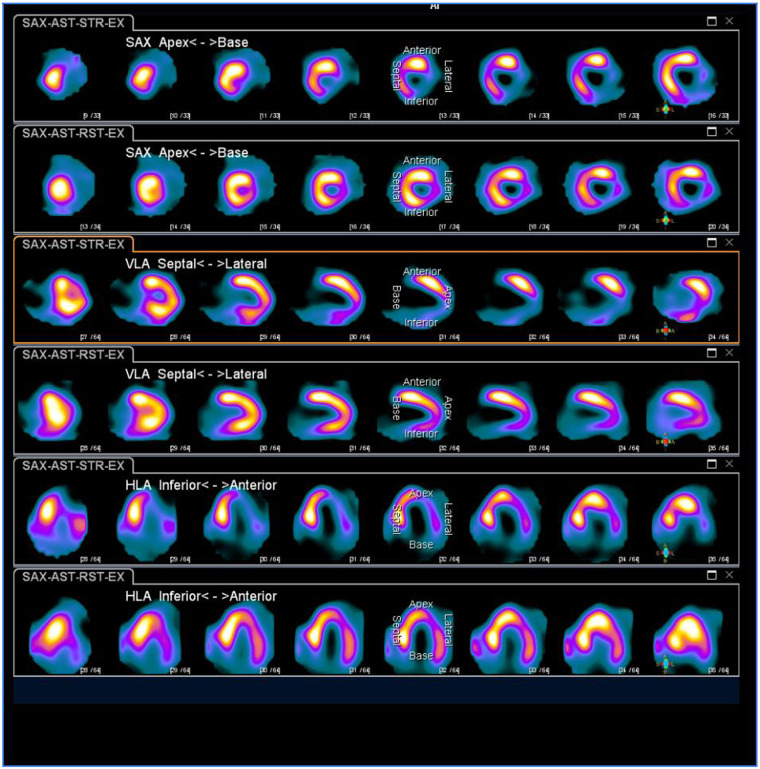
Sacubitril/Valsartan dose was then increased to 49 mg/51 mg PO b.i.d. A myocardial perfusion scintigraphy scan 3 weeks later showed evidence of viable LAD and LCX/OM territories with non-viable RCA territory (Figure 5).
Figure 5.
Gated cardiac SPECT images after IV injection of Tc-Sestamibi for Regadenoson stress and rest studies showing almost absent tracer uptake in Apex, apical lateral, and infero-apical regions of left ventricle (LV) after stress. There is moderate to severe reduction of tracer uptake in the rest of the lateral and inferior wall. Perfusion to the anterior wall and septum is well preserved. Following re-distribution, there is improvement in the lateral, mid-inferior, infero-apical, and apical region of the LV with evidence of inducible myocardial ischemia (and hence a reversible defect) in the same previously mentioned territories. Possible partial thickness infarct in the apical lateral region and basal lateral wall with superimposed ischaemia was noted.
With the marked improvement in EF and MR severity following the initiation of angiotensin receptor-neprilysin inhibitor (ARNI), the revascularisation strategy was re-discussed with the team and the patient. Percutaneous coronary intervention was thought to be a better option in this scenario as the peri-operative risks associated with CABG were substantially lower in this elderly low body weight individual. There was also no surgical indication for MV intervention at this point. Elective PCI was successfully performed to the LAD and LCX/OM arteries (Supplementary material online,Videos S5 andS6), with the EF increasing to 50% on the follow-up Echo (Supplementary material online,Video S7). The patient subsequently reported improved exercise tolerance. The improved LVEF persisted during the 18 months follow-up period whilst on Sacubitril/Valsartan.
Discussion
This case demonstrates the tremendous effect of ARNI on LV function and reverse remodelling.
In 2016, the U.S. Food and Drug Administration (FDA) approved a new drug for the treatment of heart failure, the scientific evidence that has supported the approval of this new drug was mainly obtained from the results of the PARADIGM-HF trial which was a prospective comparison of ARNI with ACEI to determine the impact on mortality and morbidity in patients with heart failure.2
The PIONEER-HF trial by Velazquezet al. in 2019 showed that patients with acute decompensated heart failure treated with ARNI had a greater reduction in NT-proBNP levels compared to standard care.4
Many case reports and case series reports have been published with similar observation of the improved ejection fraction after using ARNI, one of them was published by Pandeyet al in 2017 where he included 60 HFrEF individuals and noticed the improvement of their EF from 27.3% to 37.5% after a period of 1 year (P < 0.001).5
In the randomized controlled trial Pharmacological Reduction of Functional, Ischaemic Mitral Regurgitation (PRIME) sacubitril/valsartan treatment resulted in a greater reduction of MR associated with HF compared to valsartan alone.6
Conclusion
Appropriate and timely use of Sacubitril/Valsartan has the potential to improve LV function even significantly and swiftly in patients with acute decompensated HF, not only in chronic HF patients.
Echocardiography is the most useful tool in evaluating progress in a heart failure patient being optimized on medical therapy.
Lead author biography

Dr Fady Gerges, Cardiovascular imaging specialist and clinical cardiologist. His main areas of interests are TTE, TEE, cardiovascular CT and clinical cardiology. He has a master's degree in Cardiology and Critical Care Medicine. He has had international publications as the first Author in peer-reviewed journals . He has been a speaker and abstract presenter in International congresses. He is a regular reviewer in international peer-reviewed journals in both imaging and interventional cardiology. Editorial board member for the Internatonal Journal of the Cardiovascular Academy. He has EACVI Accreditation in adult TTE and Level 1 & 2 certification in Cardiovascular CT from SCCT, UK. He is the President of the medical Board of International Young Academy of Cardiology.
Supplementary material
Supplementary material is available atEuropean Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online asSupplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Funding: none declared.
Supplementary Material
References
- 1.Ponikowski P,Voors AA,Anker SD,Bueno H,Rutten FH,van der Meer P,. et al. ;ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC.Eur Heart J 2016;37:2129–2200. [DOI] [PubMed] [Google Scholar]
- 2.McMurray JJ,Packer M,Desai AS,Gong J,Lefkowitz MP,Rizkala AR. et al. angiotensin-neprilysin inhibition versus enalapril in heart failure.N Engl J Med 2014;371:993–1004. [DOI] [PubMed] [Google Scholar]
- 3.Yancy CW,Jessup M,Bozkurt B,Butler J,Casey DE Jr,Colvin MM. et al. 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for heart failure: an update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines and the Heart Failure Society of America.J Am Coll Cardiol 2016;68:1476–1488. [DOI] [PubMed] [Google Scholar]
- 4.Velazquez EJ,Morrow DA,DeVore AD,Duffy CI,Ambrosy AP,McCague K. et al. Angiotensin-neprilysin inhibition in acute decompensated heart failure.N Engl J Med 2019;380:539–548. [DOI] [PubMed] [Google Scholar]
- 5.Pandey A,Clarus S,Pandey A,Verma S.. The impact of ARNI therapy on LV systolic function as measured by 2-D echocardiography: a 1 year case series.Can J Card 2017;33:S161–S162. Volume issue supplement, [Google Scholar]
- 6.Kang D-H,Park S-J,Shin S-H,Hong G-R,Lee S,Kim M-S. et al. Angiotensin receptor neprilysin inhibitor for functional mitral regurgitation.Circulation 2019;139:1354–1365. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.