Abstract
Background
Children have been less affected by the COVID-19 pandemic, but its repercussions on pediatric illnesses may have been significant. This study examines the indirect impact of the pandemic on a population of critically ill children in the United States.
Research Question
Were there significantly fewer critically ill children admitted to PICUs during the second quarter of 2020, and were there significant changes in the types of diseases admitted?
Study Design and Methods
This retrospective observational cohort study used the Virtual Pediatric Systems database. Participants were 160,295 children admitted to the PICU at 77 sites in the United States during quarters 1 (Q1) and 2 (Q2) of 2017 to 2019 (pre-COVID-19) and 2020 (COVID-19).
Results
The average number of admissions was similar between pre-COVID-19 Q1 and COVID-19 Q1 but decreased by 32% from pre-COVID-19 Q2 to COVID-19 Q2 (20,157 to 13,627 admissions per quarter). The largest decreases were in respiratory conditions, including asthma (1,327 subjects in pre-COVID-19 Q2 (6.6% of patients) vs 241 subjects in COVID-19 Q2 (1.8%; P < .001) and bronchiolitis (1,299 [6.5%] vs 121 [0.9%]; P < .001). The percentage of trauma admissions increased, although the raw number of trauma admissions decreased. Admissions for diabetes mellitus and poisoning/ingestion also increased. In the multivariable model, illness severity-adjusted odds of ICU mortality for PICU patients during COVID-19 Q2 increased compared with pre-COVID-19 Q2 (OR, 1.165; 95% CI, 1.00-1.357; P = .049).
Interpretation
Pediatric critical illness admissions decreased substantially during the second quarter of 2020, with significant changes in the types of diseases seen in PICUs in the United States. There was an increase in mortality in children admitted to the PICU during this period.
Key Words: COVID-19, epidemiology, pediatric critical care
Abbreviations: PIM2, Pediatric Index of Mortality-2; Q1, quarter 1; Q2, quarter 2; SMR, standardized mortality rate; VPS, Virtual Pediatric Systems
FOR EDITORIAL COMMENT, SEE PAGE 396
Since COVID-19 was first detected in the United States in January 2020, more than 500,000 American adults have died of this disease.1, 2, 3 Children have been less directly affected by the disease, accounting for < 5% of cases and rarely requiring hospitalization, developing critical illness, or dying of COVID-19.2 , 4, 5, 6, 7, 8, 9 However, the indirect impact of the COVID-19 pandemic on children’s overall health and on the development of critical illness is unclear.
During the first months of the pandemic, states issued stay-at-home orders, mandated mask use, and closed schools in efforts to control the pandemic, with the federal government announcing nationwide restrictions on March 13, 2020. These public health efforts to mitigate the spread of the virus may have had both positive and negative effects on acute and chronic pediatric illnesses. Transmission of common viral infections and incidence of accidental trauma may have decreased due to these measures.10, 11, 12, 13 However, children’s health may have been negatively affected by reduced access to school-based nutritional and health services, postponement of elective surgical procedures, and delays in seeking care. Psychosocial stressors may have led to an increase in child abuse, intentional ingestions, and suicide attempts.2 Severe infections, traumatic injuries, perioperative conditions, and acute exacerbations of chronic illnesses such as asthma and diabetes are among the most common causes of admission to a PICU; thus, the epidemiology of pediatric critical illness was likely sensitive to the indirect effects of COVID-19.
The goal of the current study was to examine the indirect impact of the COVID-19 pandemic on children by comparing the epidemiology and outcomes of patients admitted to a large network of US PICUs during the first months of the pandemic compared with the same months in previous years. We hypothesized that there would be significantly fewer critically ill children admitted and significant changes in the types of diseases admitted to PICUs during the second quarter of 2020.
Materials and Methods
This retrospective observational cohort study was conducted by using the Virtual Pediatric Systems database (VPS, LLC). VPS is a validated and quality-controlled clinical database dedicated to standardized outcome data sharing among PICUs. Data included in the database have an interrater reliability of > 95% and include patient-level variables for all admissions to the participating PICU. This study was reviewed by the Institutional Review Board of Connecticut Children’s Medical Center and determined to be non-human subject research.
Creation of the Study Database
The VPS database was queried for children admitted to a US PICU in either quarter 1 (Q1, January-March) or quarter 2 (Q2, April-June) of the years 2017 to 2020 to compare the pre-COVID-19 (2017-2019) era vs 2020. Only centers with complete 2020 data and at least 1 full year worth of pre-COVID-19 data were included.
For this study, we abstracted demographic characteristics, primary diagnosis, Pediatric Index of Mortality-2 (PIM2) risk of mortality, interventions (eg, mechanical ventilation by endotracheal tube or tracheostomy tube), patient type (scheduled vs unscheduled admission; surgical vs medical), PICU length of stay, and survival to PICU discharge.14 The primary diagnosis was initially collected as the STAR code, which is the proprietary diagnosis classification of VPS. The 2,153 individual STAR codes were organized into 73 primary diagnoses by combining related STAR codes (eg “asthma with status asthmaticus” and “asthma with acute exacerbation”) using a system detailed in e-Appendix 1; seven authors (J. E. Z.-C., C. K. M., M. C. S., A. T. R., S. L. S., K. E. R., and C. L. C.) reviewed the proposed categorization, and disagreements were resolved by consensus.
Statistical Analysis
For each center, baseline patient characteristics were calculated by summing data from 2017 to 2019 and dividing by the number of years of available data. These center-level averages were then summed together to create weighted average totals for “pre-COVID-19.” Pre-COVID-19 Q1 data were compared with Q1 data from 2020 (COVID-19 Q1), and pre-COVID-19 Q2 data were compared with Q2 data from 2020 (COVID-19 Q2). Categorical variables were compared by using the χ2 test, and continuous variables were compared with the Wilcoxon rank sum test. The frequency of each primary diagnosis was compared between pre-COVID-19 years and 2020 using the χ2 test with P values adjusted for multiple comparisons using the Bonferroni correction.
For each quarter, the standardized mortality rate (SMR) was calculated by dividing the actual number of deaths by the number of deaths predicted using PIM2, which uniquely incorporates diagnoses into mortality risk prediction.14 To compare the SMR for pre-COVID-19 vs COVID-19 for each quarter, a Z-test was performed to determine if the SMRs were significantly different from each other. SMRs are presented with 95% CIs.15 , 16 Finally, a multivariable logistic regression model for factors associated with mortality was created using variables chosen a priori: PIM2, age, race, medical vs surgical, scheduled vs unscheduled, and study year. Analyses were conducted by using SAS/STAT software version 9.4 (SAS Institute, Inc.). Reported P values < .05 were deemed statistically significant and were adjusted for multiple comparisons when appropriate, as described earlier. Data are shown as number (%) and median (interquartile range).
Results
Demographic Characteristics
In the first two quarters of 2017 to 2020, there were a total of 160,295 children admitted to the 77 participating PICUs, 69 of which had data for all three baseline years. The number of admissions in COVID-19 Q1 was 1% less than in pre-COVID-19 Q1 (22,895 vs 23,197 admissions per quarter), but there was a 32% decrease in admissions in COVID-19 Q2 compared with pre-COVID-19 Q2 (13,627 vs 20,157 admissions per quarter) (Table 1 ). Age, sex, race, and patient origin differed significantly between pre-COVID-19 Q2 and COVID-19 Q2 (e-Table 1), and a higher fraction of COVID-19 Q2 patients were surgical (30.5% vs 29.0%; P = .003). PIM2 scores were not significantly different between baseline and COVID-19 Q1 but increased significantly from pre-COVID-19 Q2 to COVID-19 Q2.
Table 1.
Demographic Characteristics and Treatments Received
| Variable | All Dataa (N = 160,295) | Pre-COVID-19 Q1 Weighted Annual Averagesb (n = 23,197) | COVID-19 Q1 (n = 22,895) | P Valuec | Pre-COVID-19 Q2 Weighted Annual Averagesb (n = 20,157) | COVID-19 Q2 (n = 13,627) | P Valuec |
|---|---|---|---|---|---|---|---|
| Age | .11 | < .0001 | |||||
| Neonate birth to 29 d | 5,444 (3.4) | 883 (3.8) | 788 (3.4) | 573 (2.8) | 512 (3.8) | ||
| Infant 29 d to < 2 y | 55,953 (34.9) | 9,011 (38.8) | 8,975 (39.2) | 6,254 (31.0) | 3,578 (26.3) | ||
| Child 2 y to < 6 y | 31,630 (19.7) | 4,478 (19.3) | 4,459 (19.5) | 4,191 (20.8) | 2,369 (17.4) | ||
| Child 6 y to < 12 y | 28,624 (17.9) | 3,851 (16.6) | 3,675 (16.1) | 3,904 (19.4) | 2,641 (19.4) | ||
| Adolescent 12 y to < 18 y | 38,644 (24.1) | 4,976 (21.5) | 4,998 (21.8) | 5,235 (26.0) | 4,527 (33.2) | ||
| Weight, kg | 15.9 (8.70, 39.20) | 14.1 (8.0, 34.5) | 14.0 (8.1, 35.0) | .43 | 17.7 (9.6, 42.0) | 22.4 (10.2, 51.3) | < .0001 |
| Female sexd | 71,640 (44.7) | 10,362 (44.7) | 10,232 (44.7) | .96 | 8,987 (44.6) | 6,227 (45.7) | .043 |
| Race White (vs non-White) | 63,119 (39.4) | 9,242 (39.8) | 8,728 (38.1) | .0002 | 7,916 (39.3) | 5,286 (38.8) | .37 |
| Region | .0021 | < .0001 | |||||
| Midwest | 41,543 (25.9) | 5,930 (25.6) | 6,153 (26.9) | 5,265 (26.1) | 3,564 (26.2) | ||
| Northeast | 9,826 (6.1) | 1,369 (5.9) | 1,227 (5.4) | 1,265 (6.3) | 698 (5.1) | ||
| South | 40,361 (25.2) | 5,708 (24.6) | 5,603 (24.5) | 5,193 (25.7) | 3,765 (27.6) | ||
| West | 68,565 (42.8) | 10,190 (43.9) | 9,912 (43.3) | 8,435 (41.9) | 5,600 (41.1) | ||
| PIM2 | 0.80 (0.20, 1.29) | 0.78 (0.20, 1.21) | 0.78 (0.20, 1.20) | .94 | 0.83 (0.21, 1.44) | 0.87 (0.31, 1.54) | < .0001 |
| Physical length of stay, d | 1.74 (0.94, 3.77) | 1.84 (0.96, 4.0) | 1.83 (0.97, 3.9) | .91 | 1.63 (0.91, 3.6) | 1.49 (0.88, 3.1) | < .0001 |
| Unscheduled patient type | 127,082 (79.3) | 18,942 (81.7) | 19,290 (84.3) | < .0001 | 15,412 (76.5) | 10,345 (75.9) | .25 |
| Post-operative | 41,192 (25.7) | 5,254 (22.7) | 4,676 (20.4) | < .0001 | 5,848 (29.0) | 4,157 (30.5) | .0032 |
| Intubated | 33,056 (20.6) | 4,739 (20.4) | 4,425 (19.3) | .0031 | 4,191 (20.8) | 2,920 (21.4) | .16 |
| Mechanical ventilation | 39,841 (24.9) | 5,604 (24.2) | 5,365 (23.4) | .068 | 5,151 (25.6) | 3,470 (25.5) | .85 |
| ECMO | 993 (0.6) | 156 (0.7) | 143 (0.6) | .53 | 116 (0.6) | 76 (0.6) | .85 |
| ICU mortality | 3,301 (2.1) | 442 (1.9) | 434 (1.9) | .95 | 429 (2.1) | 350 (2.6) | .0081 |
Data are presented as No. (%) = frequency (column percentage), median (25th percentile, 75th percentile). ECMO = extracorporeal membrane oxygenation; PIM2 = Pediatric Index of Mortality-2.
Raw counts.
Weighted averages weighted by the number of quarters the center submitted data (from 2017, 2018, and 2019), rounded to the nearest whole number.
P values for categorical data are based on the χ2 test, whereas continuous variables are based on the Wilcoxon signed-rank test.
Two patients listed as “Ambiguous” were treated as missing because they did not specify male or female; percentages are out of the total nonmissing.
Treatments and Outcomes
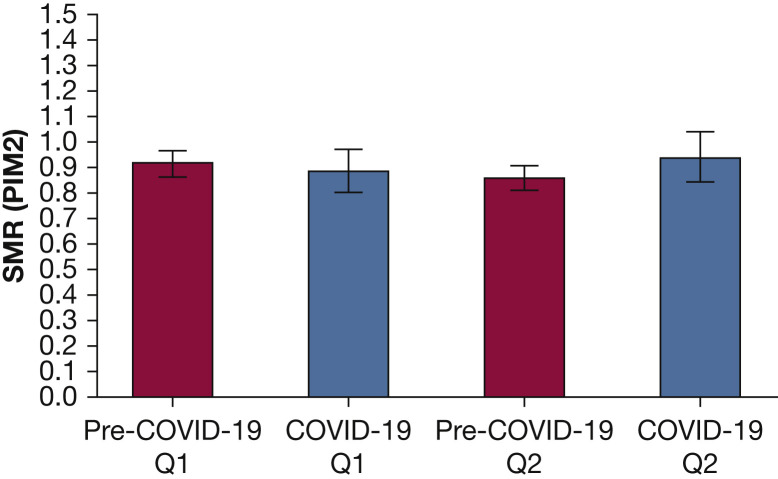
Frequency of intubation was lower in pre-COVID-19 Q1 compared with COVID-19 Q1 but did not differ between pre-COVID-19 Q2 and COVID-19 Q2, although the raw number of children requiring intubation in Q2 decreased markedly, from 4,191 (20.8% of subjects) to 2,920 (21.4%) (Table 1). Use of mechanical ventilation (including via tracheostomy) and extracorporeal membrane oxygenation did not change between baseline and 2020 for either Q1 or Q2. PICU length of stay did not differ between baseline and COVID-19 Q1 but was significantly shorter in COVID-19 Q2 compared with pre-COVID-19 Q2 (1.49 [0.88, 3.10] vs 1.63 [0.91, 3.60] days; P < .001). Raw mortality rate did not differ between pre-COVID-19 Q1 and COVID-19 Q1 but was higher in COVID-19 Q2 than baseline (2.6% vs 2.1%; P = .008). When adjusted for PIM2 score, the SMR did not differ between baseline pre-COVID-19 Q1 and COVID-19 Q1 (0.91 [0.86, 0.96] vs 0.89 [0.80, 0.97]; P = .56). Comparing pre-COVID-19 Q2 and COVID-19 Q2, the SMR was modestly higher in COVID-19 Q2, although this finding was not significant (0.86 [0.81, 0.91] vs 0.94 [0.84, 1.04]; P = .15) (Fig 1 ).
Figure 1.
SMRs. Using PIM2 with 95% CIs, reference line at 1 indicates that the number of observed deaths is equal to the number of expected deaths. PIM2 = Pediatric Index of Mortality-2; Q1 = quartile 1; Q2 = quartile 2; SMR = standardized mortality ratios.
Diagnoses
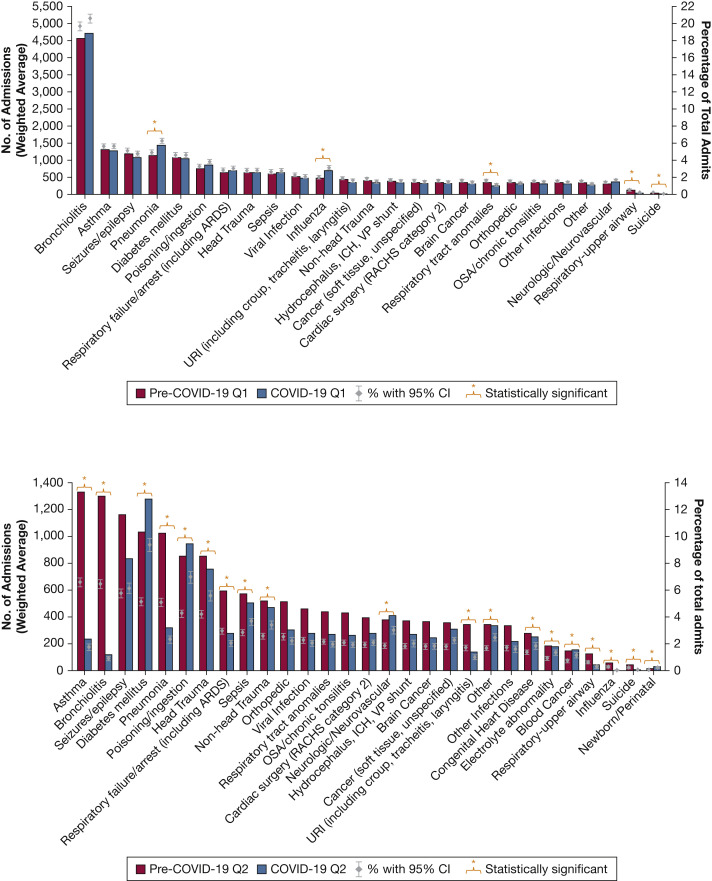
Among the 73 primary diagnoses, the frequency differed significantly between pre-COVID-19 Q1 and COVID-19 Q1 in only five diagnoses (e-Table 2, Fig 2 A, Table 2 ). There were increases in influenza (2.0% vs 3.1%) and pneumonia (4.9% vs 6.3%), and decreases in upper airway disease (0.6% vs 0.2%), respiratory tract anomalies (1.6% vs 1.2%), and suicide (0.2% vs 0.1%) (all, P < .003).
Figure 2.
Diagnostic categories in Q1 and Q2 pre-COVID-19 (2017-2019) and during COVID-19 (2020). For each diagnosis, the bars represent the weighted annual average of the number of children admitted to a participating ICU. The diamond and whiskers represent the percentage of admissions due to each diagnosis, which were compared between pre-COVID-19 years and 2020 by using the χ2 test with P values adjusted for multiple comparisons using the Bonferroni correction. Only diagnoses with ≥ 2,500 admissions in the entire dataset or statistically significant differences (Table 2) are shown. ICH = intracerebral hemorrhage; Q1 = quartile 1; Q2 = quartile 2; RACHS = risk adjustment for congenital heart surgery; URI = upper respiratory tract infection; VP = ventriculoperitoneal.
Table 2.
Diagnostic Categories With Significant Changes Between Pre-COVID-19 and COVID-19 Quarters
| Category | Pre-COVID-19 Q1 (n = 23,197) | COVID-19 Q1 (n = 22,895) | P Value | Pre-COVID-19 Q2 (n = 20,157) | COVID-19 Q2 (n = 13,627) | P Value |
|---|---|---|---|---|---|---|
| Asthma | 1,299 (5.6%) | 1,292 (5.6%) | > .99 | 1,327 (6.6%) | 241 (1.8%) | < .0001 |
| Blood cancer | 143 (0.6%) | 147 (0.6%) | > .99 | 146 (0.7%) | 158 (1.2%) | .003 |
| Bronchiolitis | 4,564 (19.7%) | 4,707 (20.6%) | > .99 | 1,299 (6.5%) | 121 (0.9%) | < .0001 |
| Congenital heart disease | 256 (1.1%) | 249 (1.1%) | > .99 | 278 (1.4%) | 253 (1.9%) | .037 |
| Diabetes mellitus | 1,072 (4.6%) | 1,054 (4.6%) | > .99 | 1,033 (5.1%) | 1,276 (9.4%) | < .0001 |
| Electrolyte abnormality | 189 (0.8%) | 203 (0.9%) | > .99 | 186 (0.9%) | 183 (1.3%) | .018 |
| Head trauma | 649 (2.8%) | 645 (2.8%) | > .99 | 853 (4.2%) | 757 (5.6%) | < .0001 |
| Influenza | 465 (2.0%) | 717 (3.1%) | < .0001 | 56 (0.3%) | 3 (0.0%) | < .0001 |
| Neurologic/neurovascular | 328 (1.4%) | 378 (1.7%) | > .99 | 375 (1.9%) | 411 (3.0%) | < .0001 |
| Newborn/perinatal, all | 13 (0.1%) | 13 (0.1%) | > .99 | 20 (0.1%) | 34 (0.3%) | .039 |
| Other | 347 (1.5%) | 286 (1.3%) | > .99 | 343 (1.7%) | 338 (2.5%) | < .0001 |
| Pneumonia | 1,137 (4.9%) | 1,436 (6.3%) | < .0001 | 1,027 (5.1%) | 318 (2.3%) | < .0001 |
| Poisoning/ingestion | 761 (3.3%) | 867 (3.8%) | .23 | 856 (4.3%) | 946 (6.9%) | < .0001 |
| Respiratory, upper airway | 129 (0.6%) | 38 (0.2%) | < .0001 | 127 (0.6%) | 38 (0.3%) | .0004 |
| Respiratory failure/arrest (including ARDS) | 651 (2.8%) | 699 (3.1%) | > .99 | 594 (3.0%) | 280 (2.1%) | < .0001 |
| Respiratory tract anomalies | 373 (1.6%) | 264 (1.2%) | .0022 | 440 (2.2%) | 269 (2.0%) | > .99 |
| Sepsis | 612 (2.6%) | 639 (2.8%) | > .99 | 573 (2.8%) | 501 (3.7%) | .0013 |
| Suicide | 53 (0.2%) | 15 (0.1%) | .0004 | 46 (0.2%) | 9 (0.1%) | .020 |
| Non-head trauma | 417 (1.8%) | 344 (1.5%) | .97 | 520 (2.6%) | 466 (3.4%) | .0005 |
| URI (includes croup, tracheitis, laryngitis) | 438 (1.9%) | 361 (1.6%) | .77 | 3,445 (1.7%) | 139 (1.0%) | < .0001 |
Frequencies calculated from total samples and for weighted averages; N rounded to nearest whole number. Full dataset is presented in e-Table 2. P values are resulting from 2 × 2 χ2 tests and are adjusted for multiple comparisons using the Bonferroni adjustment. The χ2 test compares each individual diagnosis vs all other diagnoses; for example, pneumonia vs all other non-pneumonia diagnoses. Q1 = quartile 1; Q2 = quartile 2; URI = upper respiratory tract infection.
The frequency of 19 diagnoses differed significantly between pre-COVID-19 Q2 and COVID-19 Q2 (Fig 2B). The largest decreases in patient volume were observed in respiratory conditions, including asthma (1,327 subjects at baseline [6.6% of patients] vs 241 subjects in COVID-19 Q2 [1.8%]; P < .0001), bronchiolitis (1,299 [6.5%] vs 121 [0.9%]; P < .001), pneumonia (1,027 [5.1%] vs 318 [2.3%]; P < .001), influenza (56 [0.3%] vs 3 [0.0%]; P < .001), and respiratory failure/arrest (594 [3.0%] vs 280 [2.1%]; P < .0001). The frequency of brain trauma (4.2% vs 5.6%; P < .001) and general trauma (2.6% vs 3.4%; P < .001) increased, whereas attempted suicide (0.2% vs 0.1%; P = .02) decreased in COVID-19 Q2, although raw patient volumes decreased in all three diagnoses. Only five primary diagnoses had both a significant increase in frequency and an increase in raw patient volume, including diabetes mellitus (1,033 [5.1%] vs 1,276 [9.4%]; P < .001), poisoning/ingestion (856 [4.3%] vs 946 [6.9%]; P < .001), blood cancer (146 [0.7%] vs 158 [1.2%]; P = .003), and neurologic/neurovascular disease (375 [1.9%] vs 411 [3.0%]; P < .0001).
Factors Associated With Mortality
A multivariable logistic model was created to calculate OR estimates for PICU mortality in Q1 and Q2 (Table 3 ). Mortality was not associated with study year using Q1 data. However, the OR for mortality in COVID-19 Q2 was 1.17 (95% CI, 1.0-1.36; P = .047) compared with pre-COVID-19 Q2 while controlling for PIM2, age, race, and patient type. Non-White children and neonates also had increased odds of mortality.
Table 3.
Multivariable Logistic Model OR Estimates for ICU Mortality
| Effect | OR Estimate | 95% Wald Confidence Limits |
P Value | |
|---|---|---|---|---|
| Pre-COVID-19 Q1 vs COVID-19 Q1a | ||||
| Neonate (birth to 29 d) vs infant (29 d to < 2 y) | 2.25 | 1.78 | 2.83 | < .0001 |
| Child (2 y to < 6 y) vs infant (29 d to < 2 y) | 1.11 | 0.94 | 1.32 | .23 |
| Child (6 y to < 12 y) vs infant (29 d to < 2 y) | 1.28 | 1.08 | 1.52 | .0053 |
| Adolescent (12 y to < 18 y) vs infant (29 d to < 2 y) | 1.42 | 1.22 | 1.66 | < .0001 |
| Postoperative (yes vs no) | 0.63 | 0.54 | 0.75 | < .0001 |
| COVID-19 Q1 vs pre-COVID-19 Q1 | 0.93 | 0.81 | 1.06 | .25 |
| PIM2 | 1.11 | 1.10 | 1.11 | < .0001 |
| Pre-COVID-19 Q2 vs COVID-19 Q2b | ||||
| White vs non-White (race) | 0.86 | 0.76 | 0.99 | .030 |
| Neonate (birth to 29 d) vs infant (29 d to < 2 y) | 1.84 | 1.41 | 2.39 | < .0001 |
| Child (2 y to < 6 y) vs infant (29 d to < 2 y) | 0.86 | 0.72 | 1.04 | .12 |
| Child (6 y to < 12 y) vs infant (29 d to < 2 y) | 1.04 | 0.87 | 1.25 | .64 |
| Adolescent (12 y to < 18 y) vs infant (29 d to < 2 y) | 0.92 | 0.78 | 1.09 | .33 |
| Postoperative (yes vs no) | 0.55 | 0.47 | 0.65 | < .0001 |
| COVID-19 Q2 vs pre-COVID-19 Q2 | 1.17 | 1.00 | 1.36 | .047 |
| PIM2 | 1.11 | 1.10 | 1.11 | < .0001 |
The rate of the missing values for variables in the multivariable regression model was 0% in both the Q1 and Q2 mortality models. There were 88,176 observations in pre-Q1 + COVID-19-Q1 and all of them had complete data for the mortality model variables. The same was true for the Q2 model. PIM2 = Pediatric Index of Mortality-2; Q1 = quartile 1; Q2 = quartile 2.
N = 88,176, Akaike information criterion = 11,884.46, area under the curve = 0.86 (95% CI, 0.85-0.87).
N = 72,119, Akaike information criterion = 10,011.64, area under the curve = 0.88 (95% CI, 0.87-0.89).
Discussion
Using quality-controlled data from 77 PICUs across the United States, we observed a 32% decrease in critically ill children admitted to the PICU in April to June of 2020 compared with the same time frame during the preceding 3 years, predominantly due to marked reductions in common infection-related respiratory conditions. Diabetes and poisoning/ingestion were notable outliers that increased both in frequency and patient volume. Mortality rate was higher in COVID-19 Q2 compared with baseline, even after adjusting for demographic characteristics and the increase in illness severity at PICU admission, suggesting that the COVID-19 pandemic negatively affected children despite the low incidence of direct illness.
Our observed decrease in non-COVID-19 patient volume is similar that of adult patients in New York City (38%).17 A larger relative decrease in admissions (59%) was reported from the medical services of a single tertiary children’s hospital, although that study included general ward patients.13 A decrease in PICU admissions was unsurprising given that elective surgeries were deferred in many regions and the predictable effects of mask mandates and stay-at-home orders on transmission of pathogens that cause common PICU conditions (eg, bronchiolitis, pneumonia). Observing that PICU medical and surgical admissions decreased by approximately 30% may help leaders prepare during future pandemics, and the disproportionate effects on specific diagnoses provide unique information about the causative factors underlying pediatric critical illnesses. For example, the marked reduction in critical asthma suggests that infections contribute substantially to severe exacerbations, although reduced allergen exposure and increased parental supervision may also have influenced this finding.
Diabetes mellitus was the primary diagnosis with the largest increase in raw patient volume, increasing by > 200 admissions per quarter compared with the pre-COVID-19 years in Q2. Similarly, in the United Kingdom, an increase in the proportion of patients with diabetic ketoacidosis was reported for March to April 2020 compared with the previous 2 years.18 , 19 COVID-19 may contribute to the development of diabetes and/or ketoacidosis, as coronaviruses bind to angiotensin-converting enzyme 2 receptors that are expressed on multiple organs and tissues, including pancreatic beta cells.19 Alternatively, lack of access to school-based health care may account for a decrease in compliance with diabetes management. Future studies should endeavor to better understand if COVID-19 infection increases the likelihood of diabetic ketoacidosis among children with diabetes or increases the chances that a child develops diabetes in the first place.
Financial stressors, school closures, social distancing, and sick family members may have a negative impact on the emotional well-being of children and their parents, but the changes in the epidemiology of trauma and self-harm in our cohort are unclear. The raw numbers of critically injured children decreased, but their relative frequency increased significantly, suggesting that traumatic injuries were less affected by the pandemic than other causes of PICU admission. Encouragingly, both the frequency and raw number of children requiring PICU care after attempting suicide decreased. Further study is needed to understand the relative contributions of intentional and accidental causes to the increase in observed poisonings.
Perhaps our most troubling findings were that severity of illness and raw mortality rates were higher in COVID-19 Q2. The approximately 15% increase in mortality was statistically reliable in the logistic regression model, but the contributing factors are unclear and warrant additional exploration and external validation. Parents may have had a reluctance to bring children to medical facilities, as evidenced by decreases in rates of routine childhood vaccination and ED visits during the pandemic, which could have led to delayed care and more severe illness at presentation.20 Hospital systems were strained during Q2 of 2020 while dealing with the first pandemic in more than a century. Care protocols changed frequently, supply shortages occurred, and health care workers dealt with unprecedented levels of stress; cardiac arrest in the PICU during COVID-19 has been attributed to such factors.21, 22, 23, 24, 25 All these factors may have potentially contributed to our findings.
There are several limitations to the current study. First, this was an observational cohort study conducted through retrospective analysis of a large quality-benchmarking dataset. Database studies such as ours carry an inherent risk of inaccurate data entry. However, the VPS database uses strict quality control measures to reduce the likelihood of data entry errors, has low frequency of missing data and high interrater reliability, and has been used for many observational studies of pediatric critical illness.26 , 27 Second, not all 77 centers had all 3 years of baseline data (four had 1 year and four had 2 years), but this was accounted for by averaging 2017 to 2019 data according to center. Third, because we only included the 77 centers that contributed data to the VPS database during the periods of interest, our data may not be representative of all PICUs in the United States. However, we believe that by including multiple centers with diverse characteristics from every region of the country, our findings are likely generalizable beyond the current study sample and thus representative of the changes in PICU admissions throughout the country.
Interpretation
During the second quarter of 2020, in the midst of the COVID-19 pandemic, we observed a 32% decrease in PICU admissions (particularly infection-related respiratory conditions, with diabetes mellitus a notable outlier), a modest increase in severity of illness, and a 16.5% increase in the odds of mortality. Similar reductions in patient volume may be planned for when large-scale public health measures are next needed. The disproportionate impact on specific conditions provides unique insight on the causative factors underlying pediatric critical illness and should be further investigated. Pending external validation, the observed increase in mortality risk warrants consideration to avoid indirect harms to children from this pandemic that predominantly affects adults.
Take-home Points.
Study Question: Were there significantly fewer critically ill children admitted to PICUs during the second quarter of 2020, and were there significant changes in the types of diseases admitted?
Results: During the second quarter of 2020, in the midst of the COVID-19 pandemic, we observed a 32% decrease in PICU admissions (particularly infection-related respiratory conditions, with diabetes mellitus a notable outlier), a modest increase in severity of illness, and a 16.5% increase in the odds of mortality.
Interpretation: Pediatric critical illness admissions decreased substantially during the second quarter of 2020, with significant changes in the types of diseases seen in PICUs in the United States.
Acknowledgments
Author contributions: J. E. Z.-C. is the guarantor for the content of the manuscript, including the data and analysis. All authors conceptualized and designed the study. J. Z.-C., C. L. C., and C. K. M. wrote the initial manuscript, edited and reviewed subsequent manuscript drafts, and prepared the manuscript for publication; M. J. K. performed all formal data analysis and created tables and figures, and edited and reviewed manuscript drafts; M. C. S. performed project administration, assisted with methodology, and edited and reviewed manuscript drafts; A. T. R. performed project administration, assisted with methodology, and edited and reviewed manuscript drafts; S. L. S. curated and maintained data, developed initial methodology, and edited and reviewed manuscript drafts; K. E. R. performed project administration, assisted with methodology, and edited and reviewed manuscript drafts; J. A. P. maintained data, assisted with methodology and data analysis, and edited and reviewed manuscript drafts.
Financial/nonfinancial disclosures: None declared.
Other contributions: The authors greatly acknowledge the work of Nicholas Huff, MD, in helping to develop the methodology used to simplify the STAR code diagnoses.
Additional information: The e-Appendix and e-Tables can be found in the Supplemental Materials section of the online article.
Footnotes
FUNDING/SUPPORT: The authors have reported to CHEST that no funding was received for this study.
Supplementary Data
References
- 1.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaplan L.J., Kleinpell R., Maves R.C., Doersam J.K., Raman R., Ferraro D.M. Critical care clinician reports on coronavirus disease 2019: results from a national survey of 4,875 ICU providers. Crit Care Explor. 2020;2(5) doi: 10.1097/CCE.0000000000000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ghinai I., McPherson T.D., Hunter J.C. First known person-to-person transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA. Lancet. 2020;395(10230):1137–1144. doi: 10.1016/S0140-6736(20)30607-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee P.I., Hu Y.L., Chen P.Y., Huang Y.C., Hsueh P.R. Are children less susceptible to COVID-19? J Microbiol Immunol Infect. 2020;53(3):371–372. doi: 10.1016/j.jmii.2020.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shekerdemian L.S., Mahmood N.R., Wolfe K.K. Characteristics and outcomes of children with coronavirus disease 2019 (COVID-19) infection admitted to US and Canadian pediatric intensive care units. JAMA Pediatr. 2020;174(9):868–873. doi: 10.1001/jamapediatrics.2020.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Badruddin S.S., Clayton J.A., McKee B.P. Prevalence of reintubation within 24 hours of extubation in bronchiolitis: retrospective cohort study using the Virtual Pediatric Systems Database [published online ahead of print October 8, 2020]. Pediatr Crit Care Med. https://doi.org/10.1097/PCC.0000000000002581 [DOI] [PubMed]
- 7.Devulapalli C.S. COVID-19 is milder in children possibly due to cross-immunity. Acta Paediatr. 2020;109(11):2422. doi: 10.1111/apa.15407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta S., Jawanda M.K. The impacts of COVID-19 on children. Acta Paediatr. 2020;109(11):2181–2183. doi: 10.1111/apa.15484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ranabothu S., Onteddu S., Nalleballe K., Dandu V., Veerapaneni K., Veerapandiyan A. Spectrum of COVID-19 in children. Acta Paediatr. 2020;109(9):1899–1900. doi: 10.1111/apa.15412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vasquez-Hoyos P., Diaz-Rubio F., Monteverde-Fernandez N. Reduced PICU respiratory admissions during COVID-19 [published online ahead of print October 7, 2020]. Arch Dis Child. https://doi.org/10.1136/archdischild-2020-320469 [DOI] [PubMed]
- 11.Ow Z.G.W., Cheong C.K., Chin Y.H., Chin B.Z. A look at the global impact of SARS CoV-2 on orthopedic services. J Clin Orthop Trauma. 2021;12(1):33–39. doi: 10.1016/j.jcot.2020.10.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chavasse R.J. Covid-19: reduced asthma presentations in children. BMJ. 2020;370 doi: 10.1136/bmj.m2806. [DOI] [PubMed] [Google Scholar]
- 13.Wilder J.L., Parsons C.R., Growdon A.S., Toomey S.L., Mansbach J.M. Pediatric hospitalizations during the COVID-19 pandemic. Pediatrics. 2020;146(6) doi: 10.1542/peds.2020-005983. [DOI] [PubMed] [Google Scholar]
- 14.Slater A., Shann F., Pearson G. Paediatric Index of Mortality Study Group. PIM2: a revised version of the Paediatric Index of Mortality. Intensive Care Med. 2003;29(2):278–285. doi: 10.1007/s00134-002-1601-2. [DOI] [PubMed] [Google Scholar]
- 15.Lilienfeld D.E., Stolley P.D., Lilienfeld A.M. 3rd ed. Oxford University Press; New York, NY: 1994. Foundations of Epidemiology. [Google Scholar]
- 16.Rothman K.J., Greenland S., Lash T.L. 3rd ed. Wolters Kluwer Health/Lippincott Williams & Wilkins; Philadelphia, PA: 2008. Modern Epidemiology. [Google Scholar]
- 17.Blecker S., Jones S.A., Petrilli C.M. Hospitalizations for chronic disease and acute conditions in the time of COVID-19. JAMA Intern Med. 2021;181(2):269–271. doi: 10.1001/jamainternmed.2020.3978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dayal D., Gupta S., Raithatha D., Jayashree M. Missing during COVID-19 lockdown: children with onset of type 1 diabetes. Acta Paediatr. 2020;109(10):2144–2146. doi: 10.1111/apa.15443. [DOI] [PubMed] [Google Scholar]
- 19.Rubino F., Amiel S.A., Zimmet P. New-onset diabetes in Covid-19. N Engl J Med. 2020;383(8):789–790. doi: 10.1056/NEJMc2018688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Santoli J.M., Lindley M.C., DeSilva M.B. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration—United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(19):591–593. doi: 10.15585/mmwr.mm6919e2. [DOI] [PubMed] [Google Scholar]
- 21.Greenberg N., Docherty M., Gnanapragasam S., Wessely S. Managing mental health challenges faced by healthcare workers during Covid-19 pandemic. BMJ. 2020;368:m1211. doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- 22.Gonzalez-Dambrauskas S., Vasquez-Hoyos P., Camporesi A. Pediatric critical care and COVID-19. Pediatrics. 2020;146(3) doi: 10.1542/peds.2020-1766. [DOI] [PubMed] [Google Scholar]
- 23.Ng Y., Li Z., Chua Y.X. Evaluation of the effectiveness of surveillance and containment measures for the first 100 patients with COVID-19 in Singapore-January 2-February 29, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(11):307–311. doi: 10.15585/mmwr.mm6911e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuehn B.M. COVID-19 precautions helped limit cases linked to Milwaukee primary. JAMA. 2020;324(10):929. doi: 10.1001/jama.2020.16103. [DOI] [PubMed] [Google Scholar]
- 25.Gravina N., Nastasi J.A., Sleiman A.A., Matey N., Simmons D.E. Behavioral strategies for reducing disease transmission in the workplace. J Appl Behav Anal. 2020;53(4):1935–1954. doi: 10.1002/jaba.779. [DOI] [PubMed] [Google Scholar]
- 26.Clayton J.A., McKee B., Slain K.N., Rotta A.T., Shein S.L. Outcomes of children with bronchiolitis treated with high-flow nasal cannula or noninvasive positive pressure ventilation. Pediatr Crit Care Med. 2019;20(2):128–135. doi: 10.1097/PCC.0000000000001798. [DOI] [PubMed] [Google Scholar]
- 27.Gupta P., Tang X., Gossett J.M. Association of center volume with outcomes in critically ill children with acute asthma. Ann Allergy Asthma Immunol. 2014;113(1):42–47. doi: 10.1016/j.anai.2014.04.020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.