Abstract
Context
Coronavirus Disease 2019 (COVID-19) has caused unprecedented disruptions to cancer care, including through strict hospital visitation policies. Since a substantial proportion of the U.S. population report a non-English language as their primary language, it is critical that information is disseminated in multiple languages.
Objectives
To examine the availability of language translations of visitation restrictions on adult National Cancer Institute-designated comprehensive cancer centers (CCCs) Web sites.
Methods
Cross-sectional analysis of visitation policies abstracted from public-facing Web sites of CCCs in June 2020. Using U.S. Census data, CCC's city and state proportions of self-identifying Hispanic/Latinx population were categorized into three cohorts: low (<10%), moderate (10%–20%), and high (>20%).
Results
As of June 2020, all 50 CCCs published a COVID-19 visitation policy on their Web site. Of these, 33 (66%) posted policies only in English, whereas 17 (34%) included one or more non-English translations. A minority of CCCs published Spanish language resources, which did not differ based on state or city demographics: for example, only 42% (8 of 19), 10% (1 of 10), and 38% (8 of 21) of CCCs published Spanish language resources in cities with low, moderate, and high Hispanic/Latinx populations, respectively.
Conclusion
`Most CCC's did not publish non-English language translations of their visitor policies. Even in cities and states with larger Hispanic/Latinx populations, most CCCs did not publish resources in Spanish. This study highlights a key opportunity to mitigate communication barriers and deliver culturally competent, patient-centered care.
Keywords: Health disparities, translation, languages, COVID-19, visitor policies, cancer care delivery, cultural competence
Key Message
This study analyzed the availability of non-English Coronavirus Disease 2019 visitation policies at National Cancer Institute-designated comprehensive cancer centers (CCCs). The majority of CCCs, including those with locally larger Hispanic/Latinx communities, did not publish non-English resources. The results highlight the need for greater linguistic and cultural awareness in the delivery of critical health policies.
Introduction
The Coronavirus Disease 2019 (COVID-19) has magnified inequities in health outcomes among racial and ethnic minorities in the United States (U.S.).1 2 The 2019 U.S. Census American Community Survey identified that 18.5% of the U.S. population self-identifies as Hispanic/Latinx; of the 41 million Spanish-speaking persons in this survey, ∼16 million (39%) reported speaking English less than “very well.”3 Furthermore, the same survey identified that ∼25% of foreign-born persons self-identifying as Black or African American report speaking English less than “very well.”4 These findings highlight the population's linguistic diversity and the need for greater awareness of barriers that may hamper COVID-19 outreach efforts for these vulnerable populations.
Even prior to the pandemic, minority patients with cancer reported difficulties with coordination and access to care, including treatment-related information.5 6 Because most health systems adopted strict policies to mitigate COVID-19 transmission, overcoming language barriers is critical to the timely dissemination of this information to patients with cancer and their families. Although the full impact of COVID-19 on minority communities continues to be quantified, we undertook this study to characterize the accessibility of multilingual COVID-19-related visitation policies at the National Cancer Institute (NCI)-designated comprehensive cancer centers (CCCs).
Methods
N. D., E. P., C. S., and I. S. created a list of predetermined categories for data collection. Investigators (J. Y., B. T., Z. H., A. J.) abstracted COVID-19-specific visitation policies (as of June 17, 2020) from the public-facing Web sites of the 50 adult NCI CCCs. Investigators also characterized the number of non-English language translations of visitation policies available on the institutional Web site. Data abstraction and coding were performed independently by two investigators for each center, and discrepancies were discussed and resolved by consensus of the lead investigators (N. D., I. S., J. Y., C.S.). Intercoder reliability (by percent agreement) was 84% for the number of languages provided by each CCC. For CCCs with multiple affiliated sites, the flagship site, identified from the NCI Web site, was analyzed. Thematic analysis was conducted by N. D., J. Y., and I. S. Finally, state- and city-level demographics were obtained from the U.S. Census Bureau to report the proportion of CCCs offering Spanish-language resources in areas with low (<10%), moderate (10%–20%), and high (>20%) self-identifying Hispanic/Latinx populations.
Results
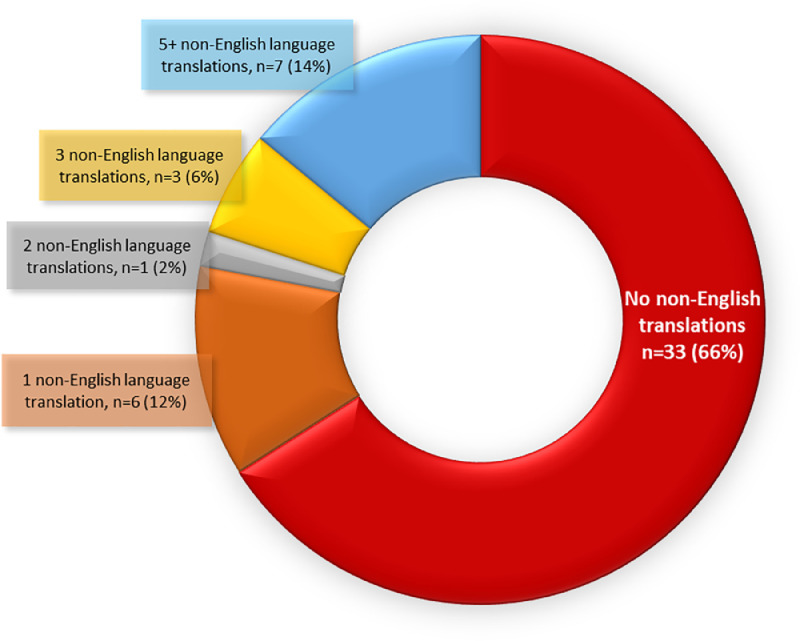
All 50 centers included in the analysis published COVID-specific visitor policies on their public site by June 17, 2020 with most centers (n = 43, 86%) posting their initial policy by April 15, 2020. At the time of review in June 2020, the majority of CCCs (n = 33, 66%) did not post non-English translations of their hospital or health system-specific visitor policies (Fig. 1 ). One-third of the CCCs (n = 17, 34%) included one or more non-English language translations of their visitor policies on their public-facing Web site, with the median number of non-English languages being 3 (range 1–9). About one-fourth of the centers (n = 11, 22%) provided policies in two or more non-English languages, and seven CCCs (14%) provided policies in five or more non-English translations. Two CCCs embedded an online language translation platform with over 100 languages (Google Translate) within their visitation policy site. However, there was no indication that the third-party translations were reviewed by the institution for accuracy and consequently were not included as accepted translations.
Fig. 1.
Proportions of primary language and translations of visitor policies at NCI-designated comprehensive cancer centers.
Among the non-English translations posted directly on a CCC Web site (as opposed to through a translation platform), the most commonly available languages were Spanish (n = 17, 34%), Arabic (n = 9, 18%), Chinese (n = 9, 18%), Vietnamese (n = 4, 8%), Russian (n = 4, 8%), Korean (n = 3, 6%), Somali (n = 3, 6%), Nepali (n = 2, 4%), and Portuguese (n = 2, 4%). Other languages represented (at one center each) were French, Swahili, Kinyarwanda, Khmer, Thai, Amharic, Italian, Polish, and Turkish.
CCCs located in states or cities with larger self-identifying Hispanic/Latinx populations were not more likely to publish Spanish language resources. For example, CCCs located in states with <10%, 10%–20%, and >20% Hispanic/Latinx populations only published Spanish language resources 35% (6 of 17), 29% (5 of 17), and 38% (6 of 16) of the time, respectively. Even on a local level, CCCs located in cities with <10%, 10%–20%, and >20% Hispanic/Latinx populations only published Spanish language resources 42% (8 of 19), 10% (1 of 10), and 38% (8 of 21) of the time, respectively.
Discussion
Healthcare facilities enacted policies restricting visitation as a part of broad efforts to limit person-to-person COVID-19 transmission. Although timely execution of risk mitigation strategies was prioritized amid this historic pandemic, our findings suggest these policies may amplify already extant healthcare disparities disproportionately impacting minority populations. In our study, we report that most NCI-designated CCCs did not provide readily accessible, COVID-19-specific hospital policies in a non-English language despite the diverse populations served by these major centers. As it is difficult to precisely describe the patient demographics of a CCC's catchment area, we used city- and state-level demographics as a surrogate. This study revealed that CCCs located in cities or states with larger (>20%) self-identified Hispanic/Latinx populations were not more likely to publish Spanish language visitor policies. Meanwhile, New Hampshire, with a relatively homogenous population (∼90% self-identifying as non-Hispanic White) housed an institution which provided visitor policies in eight languages, including Spanish.
Disproportionately higher case and mortality rates of COVID-19 are well documented in areas with high populations of Hispanic/Latinx and non-Hispanic Black populations.2 7 One study that characterized COVID-19 transmission within Latinx communities reported high rates of diagnosis in counties with ≥17.8% Latinx population, greater number of persons in the household, and a greater proportion of monolingual Spanish-speaking or bilingual inhabitants.8
Limitations of this study include its observational design and data source (public-facing Web sites at one time point). However, the study was intentionally designed to simulate patients and caregivers’ experiences in seeking would undergo to obtain this critical, hospital-specific information at the height of the pandemic.
In summary, our results show that non-English language translations were not available on the Web sites of most CCCs, suggesting that non-English-speaking families likely had to take additional steps to obtain critical information on visitation policies, through alternate modalities such as telephone calls to the clinic or hospital, or word of mouth. These challenges are significant because each individual's cancer journey is often marked by important milestones, such as discovering disease progression, weighing future lines of treatment, and discussing goals of care. These real-world scenarios require high-quality communication, and may involve communal medical decision-making for patients from cultures that value allocentrism and familism. Visitation restrictions can hamper this decision-making process, thus impacting the way that patients and families confront serious illness during the COVID-19 pandemic. Providing these policies in a linguistically aware and accessible way is crucial for delivering culturally competent, patient-centered care.
Research Support
The authors received no financial support for this work.
Disclosures
The authors have no relevant conflicts of interest to disclose.
References
- 1.U.S. Census Bureau . 2019. Quick facts—population estimates, July 1, 2019, (V2019)https://www.census.gov/quickfacts/fact/table/US/PST045219 Available at: Accessed October 2, 2020. [Google Scholar]
- 2.Centers for Disease Control and Prevention . 2020. Demographic trends of COVID-19 cases and deaths in the US reported to CDC.https://covid.cdc.gov/covid-data-tracker/#demographics Available at: Accessed October 2, 2020. [Google Scholar]
- 3.U.S. Census Bureau . 2019. Languages spoken at home by ability to speak English for the population 5 years and over.https://data.census.gov/cedsci/table?q=language&tid=ACSDT1Y2019.B16001&hidePreview=false Available at: Accessed October 2, 2020. [Google Scholar]
- 4.U.S. Census Bureau . 2019. Nativity by language spoken at home by ability to speak English for the population 5 years and over (Black of African American alone)https://data.census.gov/cedsci/table?q=black%20language&d=ACS%201-Year%20Estimates%20Detailed%20Tables&tid=ACSDT1Y2019.B16005B&hidePreview=false Available at: Accessed October 2, 2020. [Google Scholar]
- 5.Timmins CL. The impact of language barriers on the health care of Latinos in the United States: a review of the literature and guidelines for practice. J Midwifery Womens Health. 2002;47:80–96. doi: 10.1016/s1526-9523(02)00218-0. [DOI] [PubMed] [Google Scholar]
- 6.Ayanian JZ, Zaslavsky AM, Guadagnoli E. Patients' perceptions of quality of care for colorectal cancer by race, ethnicity, and language. J Clin Oncol. 2005;23:6576–6586. doi: 10.1200/JCO.2005.06.102. [DOI] [PubMed] [Google Scholar]
- 7.Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020;323:2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodriguez-Diaz CE, Guilamo-Ramos V, Mena L. Risk for COVID-19 infection and death among Latinos in the United States: examining heterogeneity in transmission dynamics. Ann Epidemiol. 2020;52:46–53.e2. doi: 10.1016/j.annepidem.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]