Highlights
-
•
Burn mass casualty events can and do occur across the globe, often in environments where health systems are already fragile and under resourced.
-
•
The World Health Organisation Emergency Medical Teams initiative was developed to improve local, national and international response to disasters.
-
•
Clear, simple recommendations can help planning bodies and burn service providers with establishing a timely and appropriate response to burn mass casualty events.
-
•
The following recommendations are based on extensive literature review, expert opinion and feedback from frontline staff involved in providing a response.
-
•
These recommendations cover the initial response from the scene to the first receiving hospital and referral to specialist services, including clinical and logistical aspects.
Keywords: Burns, Mass casualty incidents, Emergency medical teams (EMTs), Recommendations
Abstract
Health and logistical needs in emergencies have been well recognised. The last 7 years has witnessed improved professionalisation and standardisation of care for disaster affected communities – led in part by the World Health Organisation Emergency Medical Team (EMT) initiative.
Mass casualty incidents (MCIs) resulting in burn injuries present unique challenges. Burn management benefits from specialist skills, expert knowledge, and timely availability of specialist resources. With burn MCIs occurring globally, and wide variance in existing burn care capacity, the need to strengthen burn care capability is evident. Although some high-income countries have well-established disaster management plans, including burn specific plans, many do not – the majority of countries where burn mass casualty events occur are without such established plans. Developing globally relevant recommendations is a first step in addressing this deficit and increasing preparedness to deal with such disasters.
Global burn experts were invited to a succession of Technical Working Group on burns (TWGB) meetings to:
1) review literature on burn care in MCIs; and
2) define and agree on recommendations for burn care in MCIs.
The resulting 22 recommendations provide a framework to guide national and international specialist burn teams and health facilities to support delivery of safe care and improved outcomes to burn patients in MCIs.
1. Introduction
Health and logistical needs in emergencies have been well recognised [1]. The last seven years has witnessed an improving professionalization and standardisation of care for disaster affected communities – a change which has been brought about in part by the World Health Organization Emergency Medical Team (WHO EMT) initiative [2]. Since its origin in 2013, this initiative has provided a platform for the evolution and development of specialist EMTs, strengthening specific health and logistical response in emergencies. National capacity strengthening has been a focus, with particular resources targeted to building National EMT specialist teams. The initiative supports and encourages trained and appropriately skilled teams of national and international personnel to deliver a co-ordinated approach to targeted health needs whilst adhering to minimum standards of care. The evolving nature, and changing definition, of humanitarian emergencies has highlighted the need for a widened scope of practice for EMTs. In addition to EMT’s influential role in outbreaks, conflict and chronic complex disasters, smaller scale but high impact emergencies have also brought to attention a need for specialist EMTs able to target specific health needs [3,4].
MCIs resulting in burn injuries present some unique challenges [5,6]. Accounting for at least 200,000 deaths annually, burn injuries and the resultant morbidity, mortality, and disability rank high as a global public health problem [7,8]. With high prevalence in low and middle-income countries, non-fatal burns are among the leading causes of Disability Adjusted Life Years (DALY) lost [9]. Burn management of those injured requires specialist skills, expert knowledge, and timely availability of specialist resources. Lack of immediate (on-scene) patient care and the consequences of poor early decision-making in patient management can impact significantly on patient outcome and capability of health facilities to deliver good burns care [10]. MCIs with multiple burn injured patients have demonstrated the extensive demands placed on health care workers and local health facilities and the resultant high morbidity and mortality rates. With burn MCIs occurring globally, and the wide variance in existing burn care capacity in different parts of the world, the need to strengthen burn care capability is evident.
1.2. International technical working group on burns (TWGB)
In accordance with the processes used to create minimum standards of care amongst the emerging EMT specialist teams, a number of global burn and EMT experts were invited to participate in a succession of Technical Working Group on burns consensus meetings (TWGB). All EMT working groups are convened by WHO under the auspices of the Strategic Advisory Group (SAG) of the EMT Initiative. This SAG assists the WHO EMT secretariat to identify gaps and priorities for work and is made up of representatives from Ministries of Health. Opinions from each of the 6 regions, as well as UN and representatives from Non Government Organisations (NGOs) and the Red Cross and Red Crescent movement, are represented.
The TWGB was given terms of reference and a time bound period to complete its work of two years. Experts came from a range of countries and geographic regions, were gender balanced, and represented national health authorities, academic institutions, professional bodies, NGOs and the Red Cross Red Crescent movement, WHO and militaries.
The aims of this work were:
1) Review the literature on burn injuries and management in MCIs; and
2) define and achieve agreement amongst the EMT and global burns community on recommendations for burn care in MCIs.
The resulting recommendations are meant to provide a framework to guide national and international specialist burn teams and health facilities to ensure delivery of safe, appropriate, and relevant care to burn patients in the context of a mass casualty.
A three-staged approach was undertaken:
-
1
A comprehensive literature search was performed using a number of search terms. In addition, relevant cited papers from citation lists were sourced .
-
2
A series of TWGB consensus meetings were held to facilitate discussion and consensus building. In total four TWGB meetings were held over an 18 month period .
-
3
A two-phase survey was conducted detailing each of the proposed draft recommendationsand circulated to the EMT and wider burns community for feedback. The results of the survey can be found at https://interburns.org/survey.
1.3. TWGB consensus process
Step 1
Members of the TWGB undertook a comprehensive literature search. Evidence was collated from both published and ‘grey’ literature. In addition, guidelines and technical documents across the humanitarian sector were consulted.
Step 2
Burn experts from a variety of contexts, and with significant roles in the clinical care of burn-injured patients, were invited to join the first TWGB meeting at The Centre for Global Burn Injury Policy & Research in Swansea, December 2017. The main deliverables included drafting an initial set of recommendations based on experiential practice and evidence from the literature on burn care in MCIs. TWGB representatives included those involved in burn care nursing, rehabilitation, surgical care and community-based care with extensive working practice both within their home countries and in emergency response. Expert opinion was weighted heavily when drafting the recommendations.
Step 3
Led by the TWGB consultant, a technical document stating the recommendations and rationale for each was drafted and circulated to TWGB members for comment. In addition, a comprehensive survey detailing the recommendations and rationale was distributed to the wider EMT community with a request to ‘agree; partially agree; or disagree’ on each recommendation. Comments were invited to provide rationale for each answer provided, and to help contribute to onward discussions.
Step 4
Ahead of the 2nd TWGB meeting (July 2018, WHO, Geneva), results from the survey were collated and revisions to the technical document from TWGB member feedback and the survey were made. Further discussions and consensus was undertaken, with particular focus on views and comments captured in the survey.
Step 5
A revised survey, retaining the same format but reflecting the changes after the 2nd TWGB discussions, was circulated to the wider EMT community and international burn organisations for comment.
Step 6
The third TWGB meeting was hosted in New Delhi (November 2018). Results from the revised survey were presented and discussed in addition to revision of a number of draft recommendations. Following the TWGB meeting, a penultimate iteration of the technical document was circulated to TWGB members.
Step 7
The final TWGB meeting was hosted in meeting Bergen, Norway (Nov 2019) to address any points requiring clarification and agree final recommendations, in addition to discussions around implementation and training.
2. Background and overview
2.1. Aetiology of mass casualty incidents with burn injuries
Burn injury frequency following a MCI should not be underestimated. The nature of burn injuries often results in a protracted clinical journey for the patient, commonly resulting in long-term health consequences affecting functioning, quality of life and mental health. Burn patients also risk being stigmatised by communities [7,11]
Table 1 captures some of the most recent global MCIs resulting in burn injuries [[12], [13], [14], [15], [16], [17], [18], [19]]. The end column highlights the constraints and challenges identified during the MCI response and from which anecdotal evidence was considered when evolving the recommendations presented in this paper.
Table 1.
Constraints and challenges identified from MCIs resulting in burn injuries.
| Mass casualty incident | Aetiology | Estimated no of burn injured | Identified constraints and challenges |
|---|---|---|---|
| ‘White Island’ volcanic eruption; New Zealand; 2019 | Volcanic Eruption | 47 (21 dead) |
|
| MBUBA gas tanker explosion, 2018, DRC [12] | Truck caught fire post collision and siphoning of gasoline | 125 |
|
| Fuego Volcano eruption, Guatemala, 2018 [13] | Volcanic eruption | >200 |
|
| Grenfell Tower Fire, 2017, UK [14] | Origin of fire electrical fault refrigerator – fire spread secondary to poor fire retardant external cladding | 140 |
|
| Formosa Fun Coast Park Colour Party, 2015, Taiwan SAR [15] | Ignition of coloured powder | 499 |
|
| Kunshan factory aluminium dust explosion, China [16] | Flame in dust filled workshop used to polish car wheel hubs | 230 |
|
| Colectiv nightclub fire, 2015, Romania [17] | Fireworks released inside club | 144 (64 died) |
|
| Tazreen Fashions factory, 2013, Bangladesh [18] | Faulty electrical installations; poor electrical safety | >200 (112 died) |
|
| Mount Merapi volcano, Yogyakarta 2010 and 1994 [19] | Volcano eruption | >200 |
|
2.2. Setting standards in burn care
Standard setting has proven a crucial strategy for health care system strengthening, improving patient safety and improving quality of care [20]. As burn care capability across health facilities varies globally, providing guidance to standardise and define levels of burn care available or required within a health facility helps provide a platform for strengthening response to burns care in MCIs
In 2012 Interburns (International Network for Training, Education & Research in Burns) hosted an international consensus meeting to define basic, intermediate and advanced levels of burn care in terms of knowledge, skills facilities and equipment. These levels of care reflect those most often found across the globe, but in low resource environments there is a significant lack of both intermediate and advanced levels of care which further hamper the ability to respond to a burn MCI. The role of specialist burns teams is to bolster the capacity of burns care to meet local needs in an emergency scenario [20].
2.3. Evolving specialist burn teams
The TWGB identified the need for two types of specialist burn teams to reflect the phases of response following a burn MCI:
-
˗
Burn Rapid Response Team (BRRT); and
-
˗
Burn Specialist Team (BST).
Countries may have capability to support development of one or both types of team, with BRRTs likely to be more prevalent and have a stronger national presence than specialist teams.
2.3.1. Burn rapid response team (BRRT)
A small team of senior burn experienced health care workers and logisticians aiming to deploy within 6−12 h. The timeliness required for the BRRT supports a national presence offering home and regional response. The role of BRRTs is to support the immediate and early phase of burn care, specifically definitive triage, clinical assessment, and the co-ordination of patient distribution to hospitals within the country. Supportive roles may also include: resource and clinical assessment; clinical advice and support; decision making; technical advice; co-working with local authorities and the Health Emergency Operations Centre (H-EOC) to support referral and transfer of patients; resource assessment and distribution; and liaison communication.
BRRTs are expected to work cohesively with health care workers at the receiving hospitals and with local health emergency managers to support co-ordination of the burn response and patient distribution. BRRTs are recommended to remain in-situ for only a short period of time, with integration into the burn specialist team (BST) if required. A large burn incident would likely benefit from more than one BRRT.
2.3.2. Burn specialist team (BST)
A comprehensive burns team comprised of a broader mix of experienced burn healthcare workers and logisticians. The BST may be national or international, aiming to provide a longer duration of support to the burn response and supplement the support provided by the BRRT. Arrival in country may be 48−72 h (or longer) after the initial incident and BSTs are recommended to remain in-situ for up to 6 weeks. The role of BSTs is to provide direct clinical assistance in managing the high caseload. BSTs are likely to be tasked to an advanced burn service, if one exists, or to the hospital where the majority of patients are being treated. Very rarely it may be necessary to establish an entirely separate field hospital to support the BST.
BRRTs and BSTs should be self–sufficient, and adhere to minimum standards and core principles of care as defined in the ‘Blue Book’ (Classification and Minimum Standards for Foreign Medical Teams in Sudden Onset Disasters, [1]).
3. Recommendations
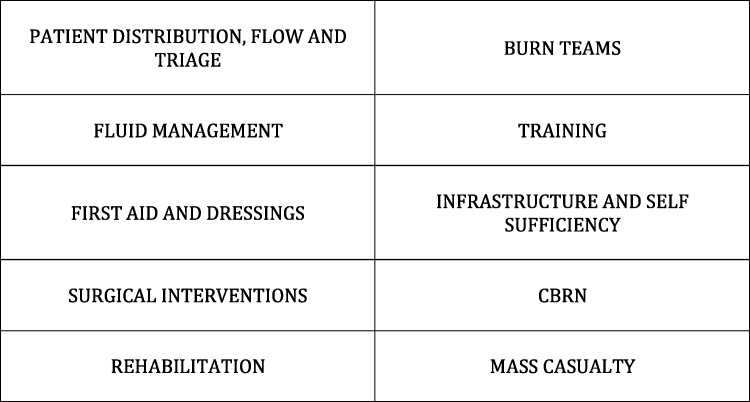
The recommendations, finalised after consensus from both the TWGB discussions and results of the surveys, are categorised under a number of key themes. Each recommendation is detailed comprehensively with rationale provided for each. The themes have been identified by the TWGB as being crucial to effective burn care in MCIs and where minimum standards of care should be delivered (Fig. 1).
Fig. 1.
TWGB Recommendation themes.
Part 1: Patient distribution, flow and triage
Patient distribution from the scene, and onward patient flow, has been clearly evidenced as being integral to efficient use of health resources and improved patient outcome in MCIs [21,22].
A simple and applicable patient flow diagram, capturing the points detailed below and for use in the event of a MCI with burn injured, was constructed by the TWBG. This can be viewed in the ‘infographic’ developed by the TWGB members in 2019 reflecting all of the recommendations: : https://interburns.org/assessment/#consultancy.
On-Scene (the site of the incident):
-
•
First responders may include passers-by, local community members, emergency service personnel and healthcare workers.
-
•
Immediate first aid and ‘on-scene’ triage should occur.
-
•
Patients should be moved from scene to the first receiving hospital/s. Patients may be moved by any form of transport available.
-
•
A health post (local clinic) should be considered an extension of the scene and not judged a hospital. Immediate first aid and ‘on-scene’ triage is recommended followed by transfer of patient to a first receiving hospital.
-
•
Patients may self-present (immediately or delayed) to a health post or hospital.
First receiving Hospital/s
-
•
Is defined as the hospital/s receiving patients from the scene or patients who self-present.
-
•
On-going clinical care, ‘on-arrival’, and ‘definitive triage’ should occur at the first receiving hospital prior to any decision about patient onward referral being made.
-
•
Designated first receiving hospitals should be either a district level (preferential) or a tertiary level hospital.
-
•
Burn care capability within first receiving hospitals will vary. To help standardise the level of burn care a first receiving hospital can deliver, and support the facility in achieving this, tasking of BRRT and BST can occur.
-
•
Decisions regarding referral and transfer of patients who meet the defined clinical criteria should occur at the first receiving facility once definitive triage has been undertaken.
-
•
Patients who have self presented or been moved from scene to a tertiary hospital in the first instance, and who have sustained burn injuries which do not require specialist burn centre care, should be re-distributed to other non specialist facilities. This process supports decongestion of specialist burn facilities (e.g. availability of burn beds; intensive care beds).
-
•
Any transfer of a patient between hospitals should only occur once the patient is clinically stable enough for transfer, and appropriate communication between referring and receiving hospital has been undertaken.
-
•
Decision-making regarding transfer of patients can be difficult. BRRT and BSTs are well placed to support this process.
Referral Hospitals (those receiving referred patients)
-
•
Referral Hospitals can be tertiary or district hospitals. Tertiary hospitals are recommended to receive patients who will benefit from specialist and higher acuity burns care. District hospitals however may also act as referral hospitals and support a decongestion mechanism by receiving patients (from tertiary hospitals) who do not require specialist burn services but on-going lower acuity burn care is indicated.
An important role of BRRT and BSTs is to help implement a scale up of resources (surge capacity) and help support an advanced burn care capability, particularly in referral hospitals.
Triage (On-scene)
Recommendation 1
On Scene: Conventional triage systems should be utilised on scene to determine life –threatening trauma injuries.
Recommendation 2
On Scene: Estimation of burn severity should focus mainly on Total Burn Surface Area (TBSA) estimation and not include depth assessment.
In a MCI involving fire or explosion, both trauma and/or burn injuries may result and a rapid assessment and triage of injuries is indicated [23]. The first responder pool will be varied in their experience of assessing injured patients and thus guidance should be familiar, simple and practical in its approach.
Existing and conventional triage systems (such as START or MIMMS Triage) should be implemented in the first instance to identify life-threatening injuries (Priority 1) such as those compromising the airway (including inhalational burns as well as head and neck injuries), breathing (such as circumferential full thickness chest burns), or injuries causing massive haemorrhage, and patients assigned an appropriate triage category [22].
Following conventional triage, assessment of burn injury severity can occur. On-scene assessment of burn severity should be determined from Total Body Surface Area (TBSA) estimation as scene responders may not be experienced nor trained in comprehensive burn injury assessment. Depth of a burn will change over time and can be difficult to assess even by burns specialists in the first 24 hours [24].
Estimation of TBSA on scene supports a simple but early effective approach to initial burn triage. However, over and underestimation of TBSA is likely on-scene, and environmental and cultural constraints may impact on how easily TBSA estimation can occur [6]. Thus, reassessment and re-triage on arrival at the first receiving hospital, and subsequently by burn-experienced staff, is essential.
Mortality from burns is multifactorial, although the relationship between TBSA and survival is well known and was first noted in 1902 [25].· Survivability factors such as age, depth and site of burn, and patient co-morbidities should be considered in conjunction with TBSA estimation from the first receiving facility onwards.
Recommendation 3
On scene: the following categories are recommended for burn injury triage: (Table 2).
Table 2.
On scene: the following categories are recommended for burn injury triage.
| Triage category | Estimated TBSA (%) | Additional comments |
|---|---|---|
| Green (P3) | <20 | |
| Yellow (P2) | 20–40 | Circumferential limb burns and special area burns can be considered here. |
| Red (P1) | >40 | Symptomatic inhalational injuries must be categorised as RED. Circumferential chest wall burns irrespective of TBSA % should be categorised as RED |
Recommendation 3 is applicable to low, middle and high-income countries in an approach to standardise and simplify on-scene triage of burn injuries across all contexts, and with consideration to local resource availability. As over and underestimation of TBSA is likely to occur on scene Recommendation 3 supports a cautious approach to allocation into Green (P3), Yellow (P2) and Red (P1) categories [6].
Inhalation injury
First responders, and those at the initial receiving health facility, are advised to be observant for the early signs and symptoms of a thermal inhalational injury. Inhalational injuries can cause significant morbidity and mortality [26]. Early recognition and intervention of likely airway compromise or respiratory failure is an important step in helping improve patient outcome. Signs of inhalational injury include soot in the mouth, facial burns, stridor, hoarseness and confusion.
The type of incident and mechanism of burn injury will also provide additional indications to risk of inhalational injury. Evidence suggests that failure to recognise actual or pending airway compromise from inhalational burns early increases mortality rate significantly [6,27]. Findings from a three staged mix methods study following the burn MCI in Taiwan (2015) identified that patients with inhalational injuries were prone to be under-triaged when first responders used the Simple and START triage tools and no burn injury specific triage tool was used. Those with inhalational burns rapidly developed airway obstruction and hypoxia whilst awaiting transportation. The authors recommended that evaluation of inhalational injury be an integral part of triage procedures and evaluation of inhalational injury the most critical step in the triage process [6].
Consideration should also be given to the possibility of chemical inhalational injuries such as those resulting from mustard gas, phosphorus and chlorine following MCIs. Appropriate personal protective equipment is advised when managing patients suspected of being victims of a chemical incident and an awareness of the often delayed effects of the agent is important (e.g. Mustard agents) [28]. Industrial accidents can also give rise to inhalational injuries – for example cyanide poisoning from acrylics [29].
Inhalational injury impacts significantly on patient outcome [6,30].· However, early and appropriate interventions and referral of such patients to specialised burn centres can help support improved outcome. Early interventions include airway protection, oxygenation and cautious fluid management. Advanced airway management (intubation and ventilation) is resource intense and thus consideration at the earliest possible phase of care should be given to onward planning of patient care. Considering the complexity of positively diagnosing inhalation injury even in specialised settings, it is likely that first responders will often miss the condition. Careful re-assessment at the first receiving hospital is therefore paramount.
Recommendation 4
On Scene: ‘Non-survivable’ triage category should not be implemented on scene, only at the first receiving hospital.
Due to the dynamic nature of TBSA estimation and potential on-scene TBSA estimation error, decision-making regarding survivability of a burn injury is recommended to occur at the first receiving health facility, ideally under expert guidance. Survivability factors such as patient age, patient co-morbidities, depth and site of burn, and availability of local and international resources should be considered in addition to TBSA estimation. Such factors are likely to be determined only once the patient has undergone definitive triage.
The decision to assign a patient to the ‘non-survivable’ triage category is a difficult and sensitive one within all cultures and communities, but more so in some contexts others. Support for such decision- making is recommended and can be offered by the BRRT. Once a decision has been made by the treating healthcare team, implementation of palliative care interventions are essential to ensure the patient’s dignity and comfort. Consideration should also be given to the needs of the patient’s family.
Patients with non-survivable injuries should be nursed at the health facility they have been initially received in. However this decision should be at the discretion of the treating clinicians and may be influenced by availability of nursing care and locality of patient family.
Recommendation 5
On Scene: the tool first responders and / or healthcare workers are most familiar with should be used to determined TBSA. However if none exist, the Rule of Nines TBSA estimation tool for adults and the modified Rule of Nines for children should be used.
The TBSA estimation tool utilised on scene should reflect the tool most familiar to the first responder. This is likely to reduce error and support an easy to use assessment for first responders to determine TBSA.
Each of the burn estimation tools have their own merits, and variation in accuracy is accountable to expertise, experience and patient body type [31,32]. On arrival at the first receiving health facility, additional tools and burn experienced health care workers may be available to re-estimate TBSA as part of the overall re-assessment and triage of the patient.
If guidance is indicated, use of the Rule of Nines is recommended. This method is simple, applicable across a variety of contexts and is a commonly used burn estimation tool used in pre-hospital environments [32].
Modern technology (for example mobile ‘Apps’) has greatly increased the options available to clinicians and strengthened accuracy of TBSA assessment [32]. However, resources enabling the use of such devices are likely to be very limited in low and middle-income countries particularly during the early phases of response. Many of the mobile technology applications supporting burn assessment are targeted to high-income countries and the resources available within these.
It should be noted that across all contexts paediatric burns are routinely difficult to assess. A 2017 retrospective study of 123 paediatric burns patients demonstrated that approximately 40% of cases received an initial overestimation of TBSA by the early referring hospital. The study concluded that significant differences were observed between the TBSA assessment of referring hospitals and that made by a specialist burns unit. This discrepancy impacted on transfer decisions to specialist facilities [31]. Regular re-assessment and re-triage supported by burns expertise is thus recommended.
Recommendation 6
Triage should be a dynamic process repeated at a minimum of three stages following a MCI involving burns. Additional factors impacting survivability and TBSA estimation should be considered during ‘Arrival’ and ‘Definitive’ triage.
3 stage triage recommendations:
-
▪
On-Scene
-
▪
On-Arrival (at first receiving hospital)
-
▪
Definitive (after scrub/wound cleaning by experienced burns healthcare workers)
Triage assessment for burn injuries should be dynamic and sequential. A three-phased approach is recommended to help guide health-care workers in patient assessment and decision-making.
‘Arrival’ and ‘Definitive’ triage are processes that can be supported by a BRRT in collaboration with local healthcare workers.
A three-phased triage approach is important in part to ensure accurate patient assessment following an evolving injury, but also to ensure patients are provided the most suitable interventions for their burn injury in a timely manner. The three-phase triage approach also helps target national and international resources to needs - for example higher acuity burn care resources (e.g. specialist beds; intensive care capability) can be appropriately allocated.
‘On-arrival’ and definitive triage
‘On-arrival’ and ‘definitive’ triage should include assessment of burn depth and confirm site of burn. Other survivability factors (e.g. patient age and co-morbidities) should also be considered during these phases of triage. Decisions regarding onward clinical care and re-distribution of patients can then be considered once a more accurate patient assessment has been completed.
Part 2: Fluid management
Unlike trauma injuries resulting in massive haemorrhage and where early ‘fluid’* (*in recent years packed red cells and clotting agents rather than saline or equivalent) is required to preserve life, the fluid shifts resulting from burn injuries is somewhat slower thus giving time for appropriate delayed fluid management.
Fluid replacement therapy in the management of burn casualties promoted extensive discussion within the TWGB, and survey responders. There is clear evidence demonstrating the need for intravenous fluids as part of the management of the systemic inflammatory response and capillary leak syndrome following a severe burn injury, with complications such as acute renal failure secondary to burns injuries being partly preventable with early administration of fluids [[33], [34], [35]]. However, broad evidence also exists detailing the complications of excessive fluid administration in patients with burn injuries [[36], [37], [38]]. Reported complications include abdominal compartment syndrome, pulmonary oedema, interstitial tissue leakage and airway compromise amongst others. Fluid creep is a well recognised term used for excessive fluid resuscitation in the first 24 h after a burn injury. It increases the chances of developing many of the complications listed above [36,37,39,40].
Inaccurate TBSA assessment is most likely to occur in the early response phase, and the resultant fluid formula based on this assessment can be extremely detrimental to the patient [41]. In a high-income multi-centre study in 2007, the authors observed that for every 5 L increase in fluid received by the patient, the risk of developing pneumonia, bloodstream infection, multi-organ failure and death was significantly increased [33].
Recommendation 7
On scene: in the event of a MCI, oral fluid should be encouraged (as appropriate) on-scene. Burn injured patients should not routinely receive intravenous burn resuscitation fluid at the scene.
TWGB experts reflected on their own extensive experiences from managing multiple burns patients (a recent example being drawn from the Senegalese burn speciality team responding to the oil tanker crash in Democratic Republic of Congo [12]) and concluded that intravenous fluid replacement therapy for burns victims should not be delivered on scene but once further clinical assessment of the patient has been undertaken at the first receiving hospital. A number of points were highlighted:
-
•
There are likely to be multiple, competing demands for first responders time on scene of a MCI. The accuracy of administration of intravenous fluid may easily be overlooked (for example ensuring an appropriate volume of fluid is titrated via a drip) and the attention to detail lacking. The risk of administering an inappropriate volume of intravenous fluid to a patient is thus high and the resultant fluid related complications increased. This would be particularly hazardous in the pre-hospital environment to all patients but particularly those sustaining inhalational injuries.
-
•
If extended delays in transporting the patient from the scene to a health facility are likely however fluids may be considered, including judicious intravenous fluids using the formulas suggested in Recommendation 8a in cases of >40% TBSA. The risks of fluid creep and other complications from over resuscitation by intravenous fluid must be considered and mitigated for, especially as a consequence of an overestimated TBSA.
-
•
In patients with concurrent trauma injuries, on scene intravenous fluids should be considered on a case-by-case basis as per standard trauma protocols according to type of injury, injury severity and the clinical status of the patient.
-
•
Concerns were raised in the survey from the wider burn community regarding the risk of organ hypo-perfusion and subsequent complications when on-scene intravenous fluids are not given. These concerns are justified. However, field experiences following mass casualty burn incidents have supported the TWGB consensus that on-scene fluid resuscitation for burn injury is not only impractical in this setting, but that its individual and collective risk/benefit ratio is likely to be unfavourable [42]. This is mostly due to the loss of efficiency brought by implementing any complex intervention on-scene, to the difficulty of managing potential complications of overly active fluid resuscitation, and to the high probability of such over resuscitation related to aforementioned inaccuracy of on-scene TBSA assessment.
-
•
Logistically the sheer volume and weight of intravenous fluid that would need to be transported by first responders or brought to scene if intravenous fluids were instigated during this phase is highly impractical. If intravenous fluid is provided per ‘normal regime’ (such as modified Parkland Formula, 2 mL/kg/%TBSA in the first 8 h) in the pre-hospital phase to 50 patients with an average 40% TBSA and an average 70 kg body weight, the estimated overall weight of transporting the estimated fluid volume is around 280 kg for 8 h.
Recommendation 8a
At the first receiving hospital: The following initial fluid regimes are recommended: (Table 3).
Table 3.
TWGB recommend fluid regime: At the first receiving hospital: the following initial fluid regimes are recommended.
| %TBSA | Fluid recommended |
|---|---|
| <20% | Oral fluids to thirst. No intravenous fluids recommended |
| 20–40% | Support with Oral Rehydration Solution as soon as is practicable at a volume of 100mls/kg/24 h Consider IV fluid as appropriate* |
| *Consider the need for more fluids in children < 15 kg | |
| >40% | 100mls/kg/24 h intravenous crystalloids and drink as able |
| *Consider the need for more fluids in children < 15 kg |
Following extensive discussions and review of literature the TWGB concluded that a specific, simple, practical and effective fluid formula should be recommended for this particular context and cohort of patients - i.e. where there are multiple burn injured patients for whom timely burn care management and where resources are likely to be stretched.
Oral fluids
Therapeutic efficacy with the use of enteral fluids in the management of severe burns was first documented by Fox in 1944 [43]. Chilled isotonic 1.75% sodium lactate solution was administered enterally (10–15% of body weight in first 24 hours), and subsequently adjusted in its volume to maintain a urine output of 1–2 litres daily. A number of adult and paediatric patients with extensive full thickness burns received the oral therapy with good effect [43]. In the 1960s, Sorenson sought a simple and effective way to treat mass casualties from thermal nuclear warfare. Over a 16 month period all patients admitted to a burns unit were permitted to drink ‘ad libitum’, aiming for approximately 15% of body weight per 24 hours to be drunk.. For each litre consumed, a 5g salt tablet was also given. Sorenson found that 80% of patients with burns not exceeding 45% TBSA drank adequately and required no additional fluid therapy for ‘anti-shock’ treatment [44].
Subsequent studies exploring the efficiency of enteral fluids (in the form of ORS) rather than intravenous fluids as an effective approach to fluid management of burn injured patients have been undertaken [45,46]. Observations from these studies highlighted the importance of considering the use of enteral fluids as a suitable alternative to intravenous fluids up to a certain TBSA burn.
The TWGB recommend that, when able, oral fluids be started on-scene with burn injured patients encouraged to drink to thirst. Oral fluid can be provided as potable drinking water supplemented with Oral Rehydration Salts. This approach to patient fluid management should be continued beyond arrival at the first receiving hospital and guided by the patient’s clinical response. If intravenous fluids are indicated, oral supplementation can continue.
Intravenous fluid
There are a number of recognised guidelines and formulae for fluid management in burns care, primarily focused on care of the individual burns patient [[47], [48], [49], [50]]. Little evidence however exists detailing the impact of minimal fluid administration in the early phase of response to a burn casualty and whether this would cause harm or be of benefit especially in the event of a MCI. A 2017 review identified that due to the challenges of austere environments fluid resuscitation can be delayed or restricted in burns up to 40% TBSA provided the patient is quickly transported to a treatment facility [51]. The complications of aggressive fluid resuscitation however are well documented [36,37,39,40]. In addition to clinical complications, logistical considerations should also be taken into account.
The recommendation detailed above suggests, when indicated, intravenous crystalloids (lactated Ringer, supplemented with dextrose in children) should be given at a volume and rate of 100mls/kg/24 h (TBSA > 40%). Burned surface area (%TBSA) however forms no part of the calculation unlike in other burn fluid formulae. This supports a more simplified yet fully individualised approach whereby fluid volume administered should be routinely adjusted in accordance with patient’s clinical response and not adhered to in a strict formulaic manner.
If a patient needs a high volume of fluid due to deteriorating clinical course, early advanced airway intervention should be considered in conjunction with the increased resource need for on-going patient care.
Recommendation 8b
The recommended administered fluid regime should be calculated from time of arrival at the first receiving health facility and not the time of burn. Fluid status of the patient should be assessed regularly (urine output; capillary refill time; heart rate; respiratory rate) and fluid regime adjusted accordingly.
In accordance with a more judicious overall approach to intravenous fluid therapy for burns patients in the context described, the TWGB recommend that the volume of intravenous fluid administered to patients should not include any ‘catch up’ fluid. – This approach to intravenous fluid management may help mitigate the risks of fluid over resuscitation and enables more accurate recording of fluid volume given.
The patient’s clinical response to intravenous and oral fluids is the most important determinant of patient fluid / hydration status in a MCI and can help dictate on-going fluid estimates. Goal directed fluid therapy has been a long recognised important concept in fluid resuscitation of burn patients particularly in the initial phase [48,[52], [53], [54]]. However invasive monitoring to help measure response to fluid (such as cardiac output monitoring) is not likely to be available within many contexts, nor be a suitable tool to be utilised as part of a mass casualty response.
Part 3: Immediate first aid and dressings
Recommendation 9
Potable/drinking water can be used to cool and clean burn wounds.
Recommendation 10a
On scene: the following management of burn wounds is recommended:
-
•
Cool burn wound if less than 3 h since injury with (running) potable water if available (avoid hypothermia).
-
•
If available, provide pain relief to patient.
-
•
Remove debris / irritant from the wound and clean as thoroughly as possible with potable/drinking water.
-
•
Cover burn with a light clean dressing or plastic wrap (non-circumferential).
-
•
Avoid non evidenced based practices such as applying eggs, butter, toothpaste or similar on the burn.
Recommendations 10b
At first receiving hospital: on arrival the following burn wound care is recommended:
-
•
Cool burn wound if less than 3 h since injury with (running) potable/drinking water if available (avoid hypothermia).
-
•
Provide analgesia to patient.
-
•
Re-triage patient (on-arrival triage).
-
•
Clean wound /scrub.
-
•
Re-estimate TBSA.
-
•
Determine burn depth.
-
•
Confirm site of burn.
-
•
Re-assess for other injuries including inhalational injury.
-
•
Re-triage after wound clean/scrub (definitive triage).
-
•
Confirm tetanus status (and give booster and/or Immunoglobulin if indicated).
-
•
Determine appropriate dressing.
At the first receiving hospital: recommendations for:
the early management of inhalational injury include:
-
•
Sit patient up if no suspicion of other trauma injuries (i.e. burn injuries only);
-
•
Avoid excess fluid;
-
•
Consider early intubation and ventilation.
Patients with <20% TBSA and no ‘special area’ burns
-
•
Consider early discharge with out-patient follow up if <20% TBSA and superficial /partial thickness or non-special area burns.
-
•
Ensure adequate out-patient support for those discharged (e.g. wound care, social and community support and clear care pathway communicated).
Patients with >20% TBSA and/or deep dermal or ‘special area’ burns
-
•
Patients should be reviewed by an experienced burn clinician.
-
•
Such patients are likely to benefit from on-going in-patient care.
-
•
Ensure comprehensive documentation of TBSA estimation, burn depth and burn site in addition to standard clinical history and examination.
-
•
Patients with burns in ‘special areas’ such as across/near joints, hands, face or feet, and those with large burns to benefit from grafting and subsequent scar management, should be reviewed by a rehabilitation specialist.
Immediate first aid for burn injury influences the clinical course and severity of the burn [52,53,55]. Basic first aid should include cooling, pain relief, cleaning and application of a simple clean dressing to the burn wound. Cooling of the burn wound should occur up to three hours after the injury was sustained and thus can be continued from scene into the first receiving hospital. Evidence has demonstrated benefit in burn care, and a reduction in future complications, from both good effective basic first aid delivered by first responders and in the cooling of a burn within this 3 hour time period [[56], [57], [58], [59], [60], [61]].
First aid treatment should continue from scene to first receiving health facility.
Recommendation 10c
Following a burns MCI, antibiotics should not routinely be given prophylactically to burns patients unless specifically clinically indicated (e.g. compound fracture) [62].
Dressings
The effectiveness, practicality and cost of dressings must be taken into account when evaluating what would be the most suitable for a burn MCI. There is, however, little available evidence on any of these considerations. One recent paper estimating the cost impact of dressing choice in the context of a mass burn casualty event did find increased costs associated with the use of silver dressings. Importantly however time savings were also identified - savings that might help optimise burns management by minimising the time nurses spent doing dressing changes [63].
There are now a number of dressings available that are designed to be left in place for a longer duration than the more traditional daily or alternate day dressings. However, the former are considerably more expensive.
Two options for dressings should be considered:
-
•
The traditional dressings used routinely at the health facility; and/or
-
•
the more specialist dressings likely to be externally sourced.
Recommendation 11
There is no overwhelming evidence of one type of dressing over another, therefore the TWGB do not recommend any superior dressing regime. Dressing type should be chosen according to:
-
•
The wound characteristics (e.g. infected versus non-infected; donor site).
-
•
Point of application (on-scene or health facility).
-
•
Availability of dressings.
-
•
Cost-benefit implications and resource requirements (e.g. staffing); and ability of patient to return for follow up.
In a MCI, availability of staff to regularly change dressings and dressing availability (potentially affected by lack of local and international re-supply) are likely to be compromised. Consideration also needs to be given to the logistical requirement of transporting dressings if brought to the facility by a BRRT (i.e. packaging weight and volume; air transport costs; clinical waste disposal requirements, and local transportation).
Silver impregnated dressings, as opposed to silver ointment, are often used to help prevent infection and promote healing. However evidence of their clinical and cost effectiveness remains controversial [64]. In low and middle-income countries, access to silver based dressings and availability of funding to support their use is likely to be restricted. This limitation will be magnified in the event of a high number of patients receiving burn care at any one time.
Various anti-septic agents have been used for burns management including povidine-iodine, alcohol, chlorhexidine, and honey as well as more non-evidenced practices [65,66]. Silver however has remained one of the most popular due to its perceived benefits.
Dressing type and duration may need to be adjusted depending on the type and character of the wound dressed (e.g. donor site wound; infected burn) and staff availability.
Part 4: Surgical interventions
Recommendation 12
Surgical intervention capacity for the care of burns patients at the first receiving hospital should include escharotomy and scrub provided the facilities, infrastructure (e.g. operating theatre) and local skill set is available. Additional expertise via a BRRT and/or BST can support these procedures in addition to further interventions as indicated.
Surgical care should be implemented at the first receiving hospital. Procedures the local surgical team are unfamiliar or inexperienced in should be supported by clinical expertise from a BRRT and, if required, a BST, in addition to the provision and use of written procedural guidance and checklists.
Procedures that may be performed by non-burn surgeons include wound clean and scrub, escharotomy and fasciotomy. Excision and grafting procedures must be performed by surgeons skilled in burns care and/or by surgeons supported by clinical expertise [67].
If early excision and grafting is undertaken at the first receiving hospital, the patient’s care should continue at that facility and no transfer of the patient undertaken unless clinical course deteriorates. As a life saving intervention, escharotomies and/or fasciotomies were deemed to be an important part of the initial management and stabilisation approach to burn patients arriving at the first receiving hospital [[68], [69], [70]].
TBSA estimation, depth assessment and burn site confirmation should be revised following scrub to help guide definitive triage and aid decision making regarding transfer. Patients with >20% TBSA after scrub and/or ‘special area burns’ are recommended for referral and transfer to a more specialist facility. Patients with <20% TBSA with on-going surgical care, and those with superficial ‘special area’ burns should remain at the first receiving health facility. This supports rationing of resources by ensuring capacity of specialist hospitals is preserved for the more complex and extensive burns [71].
Early and late burns care
As part of strategies for burns care, the definition of early versus late burns management was also considered with agreement within the TWGB that full thickness burns should ideally be managed within the first week (early excision) and partial thickness burns beyond week one (late excision) to permit healing of those areas that might heal with dressings alone [48,[72], [73], [74], [75], [76]].
Following discussions within the TWGB, it was considered appropriate for a local surgical team in a non-specialist hospital (e.g. district) to perform scrub and excision on TBSA estimated up to 20% in adults and 10% in children. However, a staged approach to this intervention is advised and, where possible, supported by burn expertise. Skilled burn surgeons (supporting a district or tertiary hospital) would be required to undertake excision in patients with >20% TBSA (adult) and >10% TBSA (children) [77].
Paediatric burns >10% TBSA (determined after definitive triage); inhalational; and specific chemical burns should be triaged to and managed in a tertiary hospital when possible [71].
Early rehabilitation for all patients with burn injuries with support from rehabilitation specialists should be encouraged [78]. Rehabilitation specialists are potentially also well suited to take over the care of burns patients once surgical intervention and wound care has been completed.
Part 5: Rehabilitation
Recommendation 13
When indicated, rehabilitation - including active and passive exercises and functional retraining - should commence at the earliest phase of care, once vital functions are stable and with precuations considered. Precautions to consider include related trauma, wound breakdown/graft frailty, k-wires, low blood pressure, or infection.
Early access to rehabilitation can have a significant impact on patient outcomes and reduce the risk of secondary complications, such as immobility and contractures [79,80]. In the context of burns injury, the focus of rehabilitation is on:
-
•
Minimising the impact of scarring on range of movement;
-
•
Reducing disfigurement; and
-
•
Supporting functional recovery.
Rehabilitation specialists have specific skills to target these objectives. However, improving patient outcome from burn injury through effective rehabilitation strategies remains the responsibility of the entire treating team in collaboration with the patient [81].
Rehabilitation recommendations should be considered for all patients (based on burn severity and location of burn) on their arrival at the first receiving hospital [78,80,82]. Depending on need, rehabilitation interventions may include:
-
•
Scar management;
-
•
Respiratory physiotherapy;
-
•
Anti-contracture positioning;
-
•
Range of movement exercises;
-
•
Splinting;
-
•
Stretching;
-
•
Ambulation;
-
•
Strength and coordination exercises; and
-
•
Activity of daily living/functional retraining.
Scar maturation can continue for 12–18 months and complications can arise for years following discharge from acute care [83,84]. Thus identification and coordination with local rehabilitation providers and disability organizations is an important aspect of discharge planning particularly in a MCI. This is especially critical for paediatric patients who will benefit from on-going intervention due to the impact of growth on scar tissue.
Adequate analgesia should be administered prior to rehabilitation interventions as pain can reduce participation and performance. Early mobilisation is encouraged, including as part of patient self-care.
Active and passive exercises and functional retraining:
The hyper-metabolic response from severe burns, coupled with prolonged bed-rest, make patients vulnerable to deconditioning and secondary complications [48,85]. Rehabilitation supports the cardiorespiratory system, reduces oedema, reduces the risk of pressure areas and contractures, as well as readying the patient for discharge [79]. This is especially critical in the context of limited inpatient bed availability characteristic of MCI [86].
Recommendation 14
When burns are grafted (deep partial or full thicknes:) position the burnt/grafted skin so as to counteract contractile forces, using splints when indicated, to prevent contracture and manage oedema.
Splinting can be used after skin grafting to immobilise the limb. The typical regime after skin graft is to continually immobilize the affected joint area(s) for five to seven days, followed by night-wear of splints. However this should be decided in consultation with the surgeon. Splints may be applied in theatre whilst the patient is under anaesthesia or during post-operative recovery to minimise discomfort. The indication for splinting is based on the severity and location of the burn, and the patient’s ability to move actively [48,80]. Splinting should be particularly considered for young children and sedated patients who may not be able to actively participate in stretching and exercises. Photographs or pictures can be used to illustrate ideal positioning.
Splinting and anti-contracture positioning should be considered for conservatively managed wounds that do not heal within two weeks as the risk of scarring increases in these incidences. Thermoplastic is the ideal splinting material as it can be remoulded over time and can achieve good conformity but alternative materials, such as Plaster of Paris and PVC piping, may also be considered in more resource-limited settings [87]. Innovative resources can also be used for mouth and neck splints.
Burn contractures can develop rapidly (within weeks). Splinting and positioning are essential for maintaining tissue length during wound healing and to maximise functioning [48]. Oedema after burn injury can be aggravated by limb dependency and can restrict wound healing and movement, as well as exacerbate pain. Elevated positioning facilitates lymphatic drainage and, along with massage and compression, can be used to effectively manage oedema.
Recommendation 15
Compression therapy and massage should be used to minimize scarring and manage oedema.
Compression can be achieved with bandaging, tubular elastic stockings, and pressure garments. While customised compression garments may not be available in resource-limited settings, compression should aim to achieve a pressure of 24 mmHg [83]. Compression bandages or garments should be worn 23 h a day, with regular monitoring, until scar maturation [83]. As patients with severe burns will continue to use compression and massage well beyond discharge, education in correct use/technique is critical in addition to education about on-going scar care. Encouraging participation during inpatient stay improves chances of continuity after discharge.
In the context of moderate and severe burns, compression therapy can reduce scar height and can alleviate some of the discomfort of immature scars, such as blood rush and itching. Scar massage similarly works to soften scars and can improve skin movement and reduce hypersensitivity [48,85].
Recommendation 16
Where an inhalation injury is suspected, early advice and respiratory care should be commenced.
Respiratory complications from inhalation injuries will affect each patient differently. Early respiratory rehabilitation and optimal early patient positioning can help alleviate symptoms and prevent future complications in addition to ensuring the patient is equipped to manage their symptoms on discharge [82]. Where possible, early mobilisation should be encouraged to enable the patient to clear secretions and maintain cardiorespiratory system function [79]. For children this may take the form of play. A programme of breathing exercises and manual techniques should be used to support the patient to maximise lung function and chest expansion [79].
Part 6: Burn teams
The role of Burn Rapid Response Teams and Burn Specialist Teams are distinct but complimentary.
Burn Rapid Response Teams (BRRTs)
BRRTs should play a pivotal role in the early phase of response to a burns MCI to support the local health system. Often national or regional teams, and likely to be familiar with local context, the main roles of a BRRT can be categorised into:
-
•
Assessing
-
•
Clinical
-
•
Co-ordination
Assessing:
-
•
Early assessment of the current situation with estimates of patient numbers.
-
•
Provision of a comprehensive check on resource availability in the first receiving health facility and specialist burn facilities if feasible.
Clinical:
-
•
Support to local health care workers with the clinical assessment, re-triage and on-going care of patients at the first receiving health facility.
-
•
Support and guidance to local health care workers, once triage and relevant transfer has occurred, in the delivery of surgical interventions for burn care (e.g. early debridement and grafting).
-
•
Support the care of patients receiving palliative care.
Co-ordination:
-
•
If requested, support to local co-ordinating teams in hospitals and centrally.
-
•
Part of the decision-making team regarding patient transfer and patient re-distribution.
-
•
Assisting the H-EOC to determine the need for additional expertise in the form of BSTs.
Once requested, national BRRT teams should ideally deploy immediately (within 6–12 h) following a request from the affected local health authority. BRRTs are not expected to assist on-scene and are best placed focusing their support on the first non-specialist receiving hospitals. This mechanism also helps preserve the country’s local and national burn expertise at their relevant specialist hospitals (those individuals who are not part of the BRRT).
BRRTs should ideally to be self-sufficient, carrying their own specialised equipment, consumables, communication tools, food, water and habitat (i.e. self sufficient for their own needs and in order to perform their function) for a minimum of 3 days to undertake core activities around triage and patient distribution. If circumstances permit, BRRTs can stay on longer to assist with direct clinical care.
Burns MCIs are unlikely to have damaged all local infrastructure, thus large caches of tents and logistical equipment are not required, rather teams should be light and portable to facilitate rapid deployment. Self-sufficiency in terms of food, water and habitat for teams can be through the use of local accommodation if these are not affected by the incident. The teams should expect to be self-sufficient in terms of paying for their own local bills or have this covered through their deploying agency and not be a burden on the local system.
The development of BRRTs is encouraged within all countries and guidance for training and evolution of teams will be provided as part of the EMT toolkit.
Should a country have few burns specialists, or prefer to retain these at the national referral centres, then BRRTs may be sought from surrounding countries. These teams would need to comply with international EMT standards and be self-sufficient/self-caring for up to two weeks., International BRRTs should be aware they will likely be deployed into a hospital lacking much of a burns service and thus include within their kit burn care equipment and consumables to perform their task.
Recommendation 17a
Recommended composition of Burn Rapid Response Teams (BRRT): (Table 4).
-
•
The BRRT is recommended to be a national team with capability to deploy quickly and efficiently to support a number of roles.
-
•
BRRTs are not recommended to attend the scene of the incident but provide their expertise at the first receiving health facilities.
Table 4.
Recommended composition of Burn Rapid Response Teams (BRRT).
| Number per team | Skill requirement | |
|---|---|---|
| Team Leader | 1 | e.g. emergency response manager experience (this is a non clinical role) |
| Burns specialist surgeon | 1 | Minimum 5 years experience in burns care across various contexts; |
| Burns experienced Anaesthetist | 1 | Minimum 5 years experience in burns care across various contexts; |
| Burns experienced nurse | 1 | Minimum 5 years experience in burns care across various contexts |
| Logistician | 1 | With WASH and waste management experience |
Burn Specialist Teams (BST)
BSTs are larger teams comprised of a multidisciplinary healthcare workers with extensive burn experience. Whether nationally or internationally based teams, BST’s have a number of important roles:
-
•
Support the on-going clinical care of burn patients.
-
•
Provide additional experienced personnel to provide support, advice and guidance to local healthcare teams.
-
•
Support surge capacity in burns care and act as a ‘force-multiplier’ by bolstering the capacity of local health facilities in managing burn injuries.
-
•
Provide expertise particularly regarding rehabilitation and long-term treatment plans for patients.
BSTs are expected to deploy following invitation from the local health authority or H-EOC after initial assessment by the BRRTs. International BSTs are not likely to arrive in country for several days after the initial incident but should remain for a minimum of 6 weeks.
In line with BRRTs and the minimum standards and core principles for EMTS, BSTs must be self sufficient for a minimum of 2 weeks prior to re-supply. BRRTs and BSTs are not expected to provide their own field infrastructure as teams are most likely to be co-located with an existing facility.
All countries should consider creating a BRRT or having bilateral or regional agreements to request BRRTs from neighbours as part of their national EMT system and their national emergency response plan. BSTs are potentially less likely to be deployed, more difficult to put together (especially for long deployments) and may be best shared regionally among multiple countries - either sourced from one larger country, and/or with contributions of experts and resources from nearby countries within the region.
Much of the discussion within the TWGB regarding BST capacity revolved around the specific placement of expertise. The main role of a BST has been recognised as capacity building particularly for an existing health facility. It may be preferable to keep national healthcare staff and expertise in their existing place of work where familiarity resides rather than re-distribute personnel to support other facilities – a role that could be supported by a BST. Resource allocation is recommended to be determined on a case-by-case basis dependent on local context and resources, BST availability and type of incident.
Recommendation 17b
Recommended composition of Burn Specialist Teams (BST): (Table 5)
-
•
Along with BRRT, BSTs should be registered by local authorities to work for a time-limited period in the affected country and be tasked by the H-EOC, to work in support of relevant facilities and local health teams.
-
•
Minimum recommended deployment of a BST is 6 weeks given the complexity of burns care and long inpatient stays. Staff may be rotated within specialty teams (as is practised within other forms of EMTs), but ideally this would be infrequent, and careful handover would be indicated .
-
•
BSTs should support strategies to ensure smooth handover of patients with on-going care and follow-up.
-
•
BSTs are recommended to help provide training and mentorship to local specialists.
-
•
BSTs and BRRTs should ensure weekly activities are reported to relevant authorities throughout their deployment and a final exit report.
Table 5.
Recommended composition of Burn Specialist Teams (BST).
| Skill Set | Essential experience/Core Skills | Number per team | Desirable experience |
|---|---|---|---|
| Team Leader | Experience working in health emergency response co-ordination (this is a non clinical role) | 1 | Experience in disaster management |
| Burns specialist surgeons | >5 years burns experience with general trauma experience | 2 | Experience working in trauma ± mass burns or mass casualty across various contexts |
| Anaesthetist | With burns experience (>5 years) and ICU experience | 2 | Experience or training in various contexts |
| Nurses | With burns experience ± paediatric experience (2−5 years). Nurses should have experience in burns dressings, autoclaving, operating theatre nursing and 1−2 with clinical leadership experience | 5 | Burns training, if possible across various contexts |
| Medical logistician | For management of consumables and pharmacy | 1 | Experience in emergency health deployments, managing medical stock etc. specific for burns care |
| General logistician | 1 | Experience in emergency deployments including managing team self sufficiency, as well as ability to support power, water | |
| Rehabilitation specialist | With >3 years burns experience including splinting and respiratory care | 2 |
Part 7: Training
Recommendation 18
All BRRT and BST personnel should have completed generic EMT training and safety and security training (either as part of an EMT training or separately) prior to being eligible to join a burns team. In particular, all members should complete training focusing on adaptation of clinical care according to context - including in resource-limited settings - and team focused training. Successful completion of this training is recommended as a pre-requisite for selection to a BRRT or BST.
Additional specific training for BRRTs and BSTs should include:
-
•
Assessment, co-ordination and leadership in MCIs with burn injuries.
-
•
Clinical care including resuscitation and safe burn patient transfer.
-
•
Decision making regarding the management of multiple burn patients.
-
•
Local and national co-ordination mechanisms and patient transfers.
-
•
Surge capacity management.
-
•
‘Lesson Learnt’ from burn MCIs.
The target audience for burns specialist training are practising clinicians and members of local co-ordination systems (for example personnel from the H-EOC).
Recommendation 19
All burns team personnel should complete specialised training in burns care specifically focusing on MCI, whilst team leaders and clinicians should also have training in coordination and emergency management.
Globally, utilisation should be made of existing courses which meet the expected learning outcomes, ensuring training is regionally accessible, open access and economically viable.
Personnel with the relevant burns and training experience are encouraged to provide a mentorship role to emerging teams and support delivery of training as expert faculty.
Training should encompass a blended modular approach to learning and knowledge acquisition (for example workshop-based activities, immersive simulation, classroom based sessions). Consideration should also be given to supporting community education programmes around on scene first responder burn care. Training for teams in low resource contexts should be sensitive and responsive to local and cultural needs, relevant to the type of healthcare professional working with burns patients and tailored to meet the basic, intermediate and advanced levels of burn care [2,7].
The WHO EMT Toolkit will provide an open access virtual platform for supporting curriculum material and training guidance.
-
•
Guidance on EMT training curriculum, content and delivery can be accessed via the virtual EMT Toolkit.
-
•
Guidance on a standardised mass casualty burn response curriculum, course content and delivery of specific training will be available via the virtual EMT toolkit.
-
•
Training for BRRTs is recommended to be delivered at a national level.
-
•
Training specific for BSTs can be delivered centrally at a regional level.
Part 8: Infrastructure and self-sufficiency
Recommendation 20
All BRRTs and BSTs are expected to be self-sufficient for their own needs and for the equipment and consumables required for the surgical and burns care capacity they will provide. However national teams may be partially supplied by local hospitals through a pre-established collaborative agreement.
In accordance with recommendations in the ‘Blue Book’, BRRTs and BSTs are expected to be self-sufficient for a minimum of 3 days for national teams and a minimum of 2 weeks for international teams [1]. However, teams are likely to co-locate with an existing facility and thus are not required to deploy with their own field infrastructure or accommodation tents..
Recommendations regarding the equipment teams should deploy will be made available in the EMT Toolkit. Following initial situational assessment by incoming BRRTs, any additional resources can be sourced and provided by tasked BSTs.
Consideration should also be given to the tasking of other specialist EMTs such as those supporting logistics (i.e. logistics specialist team). The need for such teams can be determined by BRRTs once assessment of the situation and resources available has been completed.
Surge Response Capability
BRRTs and BSTs should support efficient and timely scaling up (and down) of resources to help ensure resources are used appropriately and with optimal impact across health facilities managing the patient influx and on going care. Strengthening surge response capability benefits from collaboration, cohesiveness and clear communication amongst all involved and is an important role for both types of team.
Equipment
A modularised approach to equipment is recommended. A modular system such as that detailed below helps supports a standardised and simplified framework for burns equipment and expedite re-supply (Table 6).
Table 6.
Recommended equipment modules.
|
1. Infrastructure Module
Burns teams are expected to co-locate with an existing facility and, although self-sufficiency of burns teams is required, they are not expected to be self-sufficient in the same manner as EMTs 1−3. MCIs resulting in burn injuries are, in general, not likely to damage health facility infrastructure on a large scale (e.g. oil tanker explosion). However, there are exceptions to this and consideration should be given to self-sufficiency in such incidences. These include:
-
•
Conflict resulting in thermal and non-thermal (e.g. chemical) burns to a large population. Infrastructural damage may exist due to conflict, especially if health facilities are specifically targeted.
-
•
Explosion within a health facility. Surrounding health facilities may however not be impacted and, with external support, able to provide the burns care needed and where burns teams can co-locate.
-
•
Gas plumes or other forms of contamination (e.g. radiation) may make it unsafe to use nearby health facilities and temporary EMT facilities may have to be erected in another safer area.
-
•
A burn MCI as a consequence of a sudden onset disaster. Local and regional functioning health facilities and EMTs (national and international) will provide an infrastructural platform for delivery of health care. BRRT and BSTs can co-locate with either.
Guidance on the recommended equipment burns teams should carry for infrastructural support including equipment needed for operating theatre infrastructure will be available on the EMT Toolkit. Equipment requirements can be adjusted according to identified needs following initial assessment by BRRTs, and should be targeted to support large scale burns response and replenishment of depleted local burn resources.
Additional infrastructural support, for example in the form of a specialist logistical team with a ward module, can be requested by BRRTs should this be identified as a need.
2. Laboratory module
Burn teams should aim to augment the laboratory equipment available locally. Information on the receiving hospitals existing laboratory capability should be determined by BRRTs and equipment to augment laboratory capability communicated to BSTs prior to their arrival in country.
Standard questions regarding the availability of blood transfusion services, basic lab, autoclave and radiology (CXR in particular) are required and if not present teams should bring.
3. Pharmacy module
Quantity is estimated based on a two-week re-supply and thus in line with recommendations for EMTs in the Blue Book. Adjustments can be made to quantity and items according to local needs. Logistical measures should be in place amongst burns teams for ensuring cold chain transport and storage if required.
Analgesics
Consideration should be given to augmenting the analgesics commonly used within local hospitals and available locally. This may vary across contexts. Transportation of any controlled pharmaceutical agents (such as opiates) must follow international custom and country guidelines.
Antibiotics
Unless specifically clinically indicated, antibiotics should not routinely be given prophylactically to burn patients after a mass casualty incident [62]. However, antibiotics may be indicated to treat secondary infections. Teams should consider bringing appropriate burns specific antibiotics to commence therapy in the case of infection.
Oral and intravenous fluids
A large quantity of Oral Rehydration Salts is recommended as nearly all burn patients will receive oral fluids. Ringers Lactate and/or Hartmanns intravenous fluid is recommended for intravenous fluids although consideration should be given to the logistics required for the weight and volume carried as deployed kit. Oral and intravenous fluids may be available locally – the deploying team should try and determine prior to deployment if oral/intravenous fluid is available and, if so, the quantity available for use.
Tetanus
Tetanus vaccination is likely to be available in some quantity at local hospitals. Teams should also deploy with tetanus vaccine and immunoglobulin surge supplies if local stocks are not available.
Nutritional supplements
Nutritional supplements should form an essential part of the pharmaceutical equipment. Recommendations include: multi-vitamins; zinc; Vitamin C; supplementary feed options. A guide to calculating nutritional recommendations in major burns can be found in the ICRC War Surgery Manual (Annex 15, page 297). Equipment supporting a nutritional focus should include MUAC tape; weighing scales and hanging paediatric scales.
Prophylaxis after exposure
As per EMT staff safety requirements, teams are recommended to carry a short course of HIV PEP for team members inadvertently exposed.
4. Blood module
A blood module may be indicated. The BRRT as part of their initial assessment should help determine the availability of ‘safe’ blood for use and confirm the likely need for deployment of a blood module. Procedures to reduce risk of bleeding are encouraged (for example use of lignocaine adrenaline on harvesting site and incision).
5. Surgical module
The estimates in Table 7 are based on the predicted activity of a BRRT (in particular time for scrub and definitive grafting). Although a BST will deploy with enough personnel to technically support a second operating theatre it is more likely that the additional team members will be delivering on a wide range of roles including supporting ward work, post-operative care, complex cases, outpatients or resting.
These estimates can be used to support decision-making regarding requests for additional resources and burn teams (Table 7).
Table 7.
Estimated resource times for care of burns patients: based on 10-12 h working day; approx. 50 beds.
| <20% TBSA | Approx. 20−30 minutes per patient. 2–3 patients managed per hour |
| >20% TBSA | Approx. 60 min per patient for assessment, initial management and surgical scrub. |
| Per day approx. 10–12 scrubs. | |
| Per day approx. 3−4 excision grafts. | |
Part 9: Chemical, Biological, Radiological and Nuclear
Recommendation 21
BRRT’s and BSTs should have the capability to support the initial and definitive clinical care respectively of burns patients resulting from a Chemical, Biological or Radio-Nuclear (CBRN) incident. They are not however expected to treat casualties in a ‘Hot Zone’ but should have provision to provide an early basic package of care.
The general principles of burn care offered by BRRTs and BSTs can be applied to CBRN incidents and thus the recommendations applied in the same manner as for a thermal burn incident.
Consideration should be given to the use of self-administered CBRN treatment kits provided by BRRTs to affected patients (for example analgesia, ORS and water bottle, antibiotic cream and dressing) [88].
Team members should have a good awareness and basic training in CBRN but do not require specialist higher-level training.
Specific knowledge on chemical burns, thermo-nuclear and radiation burns is recommended.
Part 10: Mass Casualty Planning
Recommendation 22
All Member States should have a national mass casualty burns plan ideally as a sub-plan under its mass casualty and disaster plan, and one which should be drafted following collaboration with the burn specialist community.
As part of their mass casualty and disaster plan, Member States are recommended to include a Burns MCI plan. Plans should be drafted in collaboration with members of the burn specialist community and tabletop scenarios exercised on a regular basis. Close collaboration and communication with the relevant burn specialist community to harness their expertise is essential to developing and implementing a mass casualty burns plan.
To ensure an effective response from specialist burn teams co-ordination should be centralised and engage all relevant stakeholders.
A clear and concise communication pathway should exist between the transferring and receiving health facilities to optimise patient care and resource allocation.
Focus of co-ordination should include strategies to decompress specialist centres and harness additional resources where available.
Consideration should be given to the support and use of local and regional trauma teams (not burn specialised) in augmenting some of the clinical work. The integration of such teams is likely in the event of a mixed blast incident.
The burns MCI plan should include:
-
•
types of possible burns and predicted number likely;
-
•
response pillars (including coordination);
-
•
systems in place to mobilise national teams personnel and to receive international teams personnel;
-
•
approaches to care including transferring and receiving health facilities;
-
•
written procedures; and
-
•
resources available.
The plan should be tested with the relevant stakeholders - notably coordination mechanisms at national, regional and local levels and BRRT and BST
All BST personnel should also be aware of the likely inequity in access to health resources which may emerge and be visible between those patients from separate incidents contributing financially to their treatment and those victims of an MCI receiving funded specialist care
Part 10: General EMT capabilities in mass casualty burn care
General EMTs refer to the classic Type 1 (Mobile and fixed) Type 2 and Type 3 teams that respond to disasters. Specialist teams (such as burns, outbreak response) are designed to fit within general EMTs or into local hospitals [1]. Depending on their composition, expertise and infrastructure, general EMTs will have capability to deliver a basic (EMT Type 1) to intermediate (EMT Type 2 and 3) level of burns care [1]. However, general EMTs are not specialist burns teams and are recommended to support the care of a burn injured patient only to within their existing capability. EMTs are very well placed to host BRRTs and BSTs should a need arise, and if local hospitals are overwhelmed or unable to support a burns response. This situation is most likely to arise following a mass casualty burn incident following a sudden onset disaster when EMTs may already be in-country, or following an MCI resulting in extensive burn and non-burn trauma injuries where there is a requirement for both EMT and specialist burn team support. In the presence of a BRRT and/or BST, burn care capability of an EMT Type 2 or 3 can be strengthened, in a similar manner to the resultant increased capability of a local first receiving or specialist hospital.
Final conclusions
A clear need has been recognised for the development of EMT burn specialist teams, alongside standardised recommendations for the care of burn injured in mass casualty incidents.
By implementing simple yet effective standardised approaches to burn care in MCIs, and in supporting the capability of healthcare systems globally to meet and deliver the resources and expertise to manage multiple burn injured patients, patient outcome can be improved and the associated disability adjusted life years reduced.
Specialist burn teams working to recommendations of care are therefore well placed to help target specific needs which arise, in particular in building local burn resource capacity and capability. These recommendations are for guidance only, and clinical application will depend on local context, resources and availability of skilled workforce.
Declaration of interests
No conflict of interest declared by any authors.
Acknowledgements
WHO Technical Working Group on Burns contributors (alphabetical). NIHR Global Health Research Group on Burn Trauma (Grant 16/137/110); Norwegian Directorate of Health; Haukeland University Hospital Health Trust; World Health Oganization Health Emergencies Programme (EMT Unit).
Acknowledgments
Contributors: WHO TWB contributors
All authors have approved the final article.
| Contributor | Affiliations |
| Dr Roger Alcock | Consultant in Emergency Medicine and Paediatric Emergency Medicine Member of UK-EMT, UK |
| Dr. Calin Alexandru | General Director Department for Emergency Situations, Ministry of Internal Affairs ROMANIA |
| Dr. Stian Kreken Almeland | M.D. Plastic Surgeon and Burn Surgeon, National Burn Centre in Norway Haukeland University Hospital, Jonas Lies vei 65, 5021 Bergen NORWAY |
| Dr Nikki Allorto | President, Pan African Burn Society Head Pietermaritzburg Burns Service South Africa SOUTH AFRICA |
| Dr Opoku Ware Ampomah | Consultant Plastic and Burn surgeon Director, National Reconstructive Plastic Surgery and Burn Centre Korle-Bu Teaching Hospital Accra. GHANA |
| Amanda Baumgartner | Chief Nurse and Hospital Services Program Coordinator ICRC |
| Margaret Brennan | Burns clinical nurse consultant National Critical Care and Trauma Response Centre Darwin; AUSTRALIA |
| Delphine Chedorge | Medical department, coordinator for drafting of MSF-OCP Guideline for burn care MSF |
| Resa Crestani | Emergency coordinator MSF Belgium |
| Dr Alle Baba Dieng | Operations Unit Chief Senegal Ministry of Health and Social Action’s Health Emergency Operations Centre Senegal |
| Janecke Dyvi, | Intensive care nurse Norwegian Burn Unit IFRC |
| Merete Ellefsen | Senior Adviser Norwegian Directorate of Health, P.O.box 7000 St Olavs plass, 0130 Oslo NORWAY |
| Mansour Fall | Service de réanimation chirurgicale – brûlés, Hôpital principal de Dakar, Hôpital d’instruction des armées, Dakar, Sénégal |
| Prof Josef Haik | Chief The Burn Unit Department of Plastic & Reconstructive Surgery Sheba Medical Center, Tel Hashomer; Sackler Faculty of Medicine; Tel aviv University, Israel Institute of Health Research; University of Notre Dame, western Australia; College of Health and Medicine, University of Tasmania |
| Dr Kai v.Harbou | Health Emergency Officer World Health Organization, Regional Office for South-East Asia New Delhi, India |
| Dr Minoru Hayashi | Japanese Society for Burn Injuries The Academic Committee Japan |
| Dr Amy Hughes | Clinical Lecturer in Emergency Response; Humanitarian and Conflict Response Institute; University of Manchester; Interburns, Consultant for WHO Working Group on Burns Care in Mass Casualty Incidents; Paediatric ICU Fellow, Addenbrookes Hospital, Cambridge UK |
| Prof Thomas Leclerc | Médecin en chef (COL) Professeur agrégé, anesthésiste réanimateur Chef du Centre de traitement des brûlés, HIA Percy |
| Dr Khaled Mansour | Plastic surgeon Department of burns Damascus Hospital, Syria |
| Emily McMullen | Global Emergency Rehabilitation Specialist Humanity and Inclusion UK |
| Jody-Anne Mills | Rehabilitation Programme Department of Noncommunicable Diseases World Health Organization John Walsh Centre for Rehabilitation Research; Northern Clinical School, Faculty of Medicine and Health, University of Sydney, Australia |
| Prof Naiem Moiemen | Consultant Burn and Plastic Surgeon Professor, University of Birmingham School of Medicine Director, Scar Free Foundation Burn Research Centre, Birmingham. President, International Society for Burn Injury (ISBI) UK |
| Prof R P Narayan | Professor Consultant & Head, Department Of Burns,Plastic & Maxillofacial Surgery, Vardham Mahavir Medical College and Safdarjung Hospital, New Delhi - 110029 |
| Dr. Richard E. Nnabuko | Consultant Burns and Plastic Consultant Burns and Plastic Surgery Department, National Orthopaedic Hospital. Enugu, NIGERIA |
| Dr Ian Norton | Emergency Medical Team Unit, World Health Organization Health Emergencies Program; WHO, Geneva, Switzerland (2013-2019) |
| Dr Takayuki Ogura | Japanese Society for Burn Injuries; The Disaster Network Committee Japan |
| Nelson Olim | Technical Officer WHO |
| Prof Tom Potokar | Director Interburns Co-Chair WHO-EMT Technical Working Group on Burns Chair in Global Burn Injury Policy & Research Director NIHR Global Health Research Group on Burn Trauma Swansea University Swansea, Wales , UK |
| Michael Roriz | Physiotherapist in Humanitarian Emergencies Humanity and Inclusion |
| Anne-Constance Sartiaux | Nurse anesthetist in high and low resources countries, Burn Care Advisor MSF France |
| Dr. Remy Zilliox | MSF Burn and Plastic Surgery Advisor MSF France |
Contributor Information
Amy Hughes, Email: amy.hughes@manchester.ac.uk.
Stian Kreken Almeland, Email: stian.almeland@gmail.com.
Thomas Leclerc, Email: thomas.leclerc@m4x.org.
Takayuki Ogura, Email: alongthelongestway2003@yahoo.co.jp.
Minoru Hayashi, Email: mokkox2@yahoo.co.jp.
Jody-Ann Mills, Email: millsj@who.int.
Ian Norton, Email: ian.norton@respondglobal.com.
Tom Potokar, Email: tom.potokar@interburns.org.
References
- 1.Norton I., von Schreeb J., Aitken P., Herard P., Lajolo C. 2013. Classification and Minimum Standards for Foreign Medical Teams in Sudden Onset Disasters. [Google Scholar]
- 2.Amat Camacho N., Hughes A., Burkle F.M., Ingrassia P.L., Ragazzoni L., Redmond A. Education and training of emergency medical teams: recommendations for a global operational learning framework. PLoS Curr. 2016;8 doi: 10.1371/currents.dis.292033689209611ad5e4a7a3e61520d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ravi S.J., Snyder M.R., Rivers C. Review of international efforts to strengthen the global outbreak response system since the 2014–16 West Africa Ebola Epidemic. Health Policy Plan. 2019;34:47–54. doi: 10.1093/heapol/czy102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gostin L.O. The future of the world health organization: lessons learned from ebola. Milbank Q. 2015;93:475–479. doi: 10.1111/1468-0009.12134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McGregor J.C. Major burn disasters: lessons to be learned from previous incidents and a need for a national plan. Surgeon. 2004;2:249–250. doi: 10.1016/S1479-666X(04)80092-1. [DOI] [PubMed] [Google Scholar]
- 6.Lin C.-H., Lin C.-H., Tai C.-Y., Lin Y.-Y., Shih F.F.-Y. Challenges of burn mass casualty incidents in the prehospital setting: lessons from the Formosa fun coast park color party. Prehosp Emerg Care. 2019;23:44–48. doi: 10.1080/10903127.2018.1479473. [DOI] [PubMed] [Google Scholar]
- 7.Haagsma J.A., Graetz N., Bolliger I., Naghavi M., Higashi H., Mullany E.C. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev. 2016;22:3–18. doi: 10.1136/injuryprev-2015-041616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization . 2018. Burns. WwwWhoInt.https://www.who.int/news-room/fact-sheets/detail/burns (accessed May 19, 2020) [Google Scholar]
- 9.Alonge O., Agrawal P., Talab A., Rahman Q.S., Rahman A.F., Arifeen S.E. Fatal and non-fatal injury outcomes: results from a purposively sampled census of seven rural subdistricts in Bangladesh. Lancet Glob Health. 2017;5:e818–27. doi: 10.1016/S2214-109X(17)30244-9. [DOI] [PubMed] [Google Scholar]
- 10.Newberry J.A., Bills C.B., Pirrotta E.A., Barry M., Rao G.V.R., Mahadevan S.V. Timely access to care for patients with critical burns in India: a prehospital prospective observational study. Emerg Med J. 2019;36:176–182. doi: 10.1136/emermed-2018-207900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agbenorku P. Burns functional disabilities among burn survivors: a study in Komfo Anokye Teaching Hospital, Ghana. Int J Burns Trauma. 2013;3:78–86. [PMC free article] [PubMed] [Google Scholar]
- 12.Associated Press . 2018. Dozens killed after oil tanker catches fire in DRC. The Guardian.https://www.theguardian.com/world/2018/oct/06/oil-tanker-truck-fire-leaves-at-least-50-dead-100-injured-in-drc (Accessed May 19, 2020) [Google Scholar]
- 13.Global Volcanism Program, 2013. Fuego (342090) in Volcanoes of the World, v. 4.9.0 (04 Jun 2020). Venzke, E (ed.). Smithsonian Institution. (https://volcano.si.edu/volcano.cfm?vn=342090). 10.5479/si.GVP.VOTW4-2013 (Accessed June 9, 2020). [DOI]
- 14.Gaut J. Lessons learned from the grenfell tower fire. Fire Eng. 2018 https://www.fireengineering.com/2018/04/01/252530/lessons-learned-from-the-grenfell-tower-fire/ (Accessed June 9, 2020) [Google Scholar]
- 15.Lin C.-H., Lin C.-H., Tai C.-Y., Lin Y.-Y., Shih F.F.-Y. Challenges of burn mass casualty incidents in the prehospital setting: lessons from the Formosa fun coast park color party. Prehosp Emerg Care. 2019;23:44–48. doi: 10.1080/10903127.2018.1479473. [DOI] [PubMed] [Google Scholar]
- 16.Tan Q. Challenges for rescue and treatment of mass burns: the experience of rescue and treatment for casualties in August 2nd Kunshan factory aluminum dust explosion accident. Zhonghua Shao Shang Za Zhi Zhonghua Shaoshang Zazhi Chin J Burns. 2018;34:329–331. doi: 10.3760/cma.j.issn.1009-2587.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 17.Pirii L.E., Friedrich A.W., Rossen J.W.A., Vogels W., Beerthuizen G.I.J.M., Nieuwenhuis M.K. Extensive colonization with carbapenemase-producing microorganisms in Romanian burn patients: infectious consequences from the Colectiv fire disaster. Eur J Clin Microbiol Infect Dis Off Publ Eur Soc Clin Microbiol. 2018;37:175–183. doi: 10.1007/s10096-017-3118-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burke J., Hammadi S. Bangladesh textile factory fire leaves more than 100 dead. The Guardian. 2012 [Google Scholar]
- 19.Baxter P.J., Jenkins S., Seswandhana R., Komorowski J.-C., Dunn K., Purser D. Human survival in volcanic eruptions: thermal injuries in pyroclastic surges, their causes, prognosis and emergency management. Burns J Int Soc Burn Inj. 2017;43:1051–1069. doi: 10.1016/j.burns.2017.01.025. [DOI] [PubMed] [Google Scholar]
- 20.Potokar T., Moghazy A., Peck M., Bendell R., Fanstone R. Interburns; 2013. Setting Standards for Burn Care Services in Low and Middle Income Countries.https://aidstream.org/files/documents/Interburns%20Standards%20Report%202013.pdf [Google Scholar]
- 21.Khajehaminian M.R., Ardalan A., Hosseini Boroujeni S.M., Nejati A., Keshtkar A., Foroushani A.R. Criteria and models for the distribution of casualties in trauma-related mass casualty incidents: a systematic literature review protocol. Syst Rev. 2017;6:141. doi: 10.1186/s13643-017-0538-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization . World Health Organization; Geneva: 2007. Mass Casualty Management Systems: strategies and guidelines for building health sector capacity. [Google Scholar]
- 23.Atiyeh B., Gunn S.W.A., Dibo S. Primary triage of mass burn casualties with associated severe traumatic injuries. Ann Burns Fire Disasters. 2013;26:48–52. [PMC free article] [PubMed] [Google Scholar]
- 24.Monstrey S., Hoeksema H., Verbelen J., Pirayesh A., Blondeel P. Assessment of burn depth and burn wound healing potential. Burns. 2008;34:761–769. doi: 10.1016/j.burns.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 25.Capek K.D., Sousse L.E., Hundeshagen G., Voigt C.D., Suman O.E., Finnerty C.C. Contemporary burn survival. J Am Coll Surg. 2018;226:453–463. doi: 10.1016/j.jamcollsurg.2017.12.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Badulak Jh, Schurr M., Sauaia A., Ivashchenko A., Peltz E. Defining the criteria for intubation of the patient with thermal burns. Burns. 2018;44:531–538. doi: 10.1016/j.burns.2018.02.016. [DOI] [PubMed] [Google Scholar]
- 27.Sabri A., Dabbous H., Dowli A., Barazi R. The airway in inhalational injury: diagnosis and management. Ann Burns Fire Disasters. 2017;30:24–29. [PMC free article] [PubMed] [Google Scholar]
- 28.Seth R., Chester D., Moiemen N. A review of chemical burns. Trauma. 2007;9:81–94. doi: 10.1177/1460408607083960. [DOI] [Google Scholar]
- 29.Reade M.C., Davies S.R., Morley P.T., Dennett J., Jacobs I.C. Review article: management of cyanide poisoning. Emerg Med Australas. 2012;24:225–238. doi: 10.1111/j.1742-6723.2012.01538.x. [DOI] [PubMed] [Google Scholar]
- 30.Walker P.F., Buehner M.F., Wood L.A., Boyer N.L., Driscoll I.R., Lundy J.B. Diagnosis and management of inhalation injury: an updated review. Crit Care. 2015;19:351. doi: 10.1186/s13054-015-1077-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Face S., Dalton S. Consistency of total body surface area assessment in severe burns: implications for practice. Emerg Med Australas. 2017;29:429–432. doi: 10.1111/1742-6723.12806. [DOI] [PubMed] [Google Scholar]
- 32.Thom D. Appraising current methods for preclinical calculation of burn size – a pre-hospital perspective. Burns. 2017;43:127–136. doi: 10.1016/j.burns.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 33.Klein M.B., Hayden D., Elson C., Nathens A.B., Gamelli R.L., Gibran N.S. The association between fluid administration and outcome following major burn: a multicenter study. Ann Surg. 2007;245:622–628. doi: 10.1097/01.sla.0000252572.50684.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barrow R.E., Jeschke M.G., Herndon D.N. Early fluid resuscitation improves outcomes in severely burned children. Resuscitation. 2000;45:91–96. doi: 10.1016/s0300-9572(00)00175-1. [DOI] [PubMed] [Google Scholar]
- 35.Guilabert P., Usúa G., Martín N., Abarca L., Barret J.P., Colomina M.J. Fluid resuscitation management in patients with burns: update. Br J Anaesth. 2016;117:284–296. doi: 10.1093/bja/aew266. [DOI] [PubMed] [Google Scholar]
- 36.Pruitt B.A., Jr Protection from excessive resuscitation: “pushing the pendulum back.”. J Trauma. 2000;49:567–568. doi: 10.1097/00005373-200009000-00030. [DOI] [PubMed] [Google Scholar]
- 37.Peeters Y., Lebeer M., Wise R., Malbrain M.L.N.G. An overview on fluid resuscitation and resuscitation endpoints in burns: Past, present and future. Part 2 - avoiding complications by using the right endpoints with a new personalized protocolized approach. Anaesthesiol Intensive Ther. 2015;47(Spec No):s15–26. doi: 10.5603/AIT.a2015.0064. [DOI] [PubMed] [Google Scholar]
- 38.Chung K.K., Wolf S.E., Cancio L.C., Alvarado R., Jones J.A., McCorcle J. Resuscitation of severely burned military casualties: fluid begets more fluid. J Trauma. 2009;67:231–237. doi: 10.1097/TA.0b013e3181ac68cf. discussion 237. [DOI] [PubMed] [Google Scholar]
- 39.Saffle J.R. Fluid creep and over-resuscitation. Crit Care Clin. 2016;32:587–598. doi: 10.1016/j.ccc.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 40.Ivy M.E., Atweh N.A., Palmer J., Possenti P.P., Pineau M., D’Aiuto M. Intra-abdominal hypertension and abdominal compartment syndrome in burn patients. J Trauma. 2000;49:387–391. doi: 10.1097/00005373-200009000-00001. [DOI] [PubMed] [Google Scholar]
- 41.Parvizi D., Kamolz L.-P., Giretzlehner M., Haller H.L., Trop M., Selig H. The potential impact of wrong TBSA estimations on fluid resuscitation in patients suffering from burns: things to keep in mind. Burns. 2014;40:241–245. doi: 10.1016/j.burns.2013.06.019. [DOI] [PubMed] [Google Scholar]
- 42.Little M., Cooper J., Gope M., Hahn K.A., Kibar C., McCoubrie D. ‘Lessons learned’: A comparative case study analysis of an emergency department response to two burns disasters. Emerg Med Australas. 2012;24:420–429. doi: 10.1111/j.1742-6723.2012.01578.x. [DOI] [PubMed] [Google Scholar]
- 43.Fox C.L. Oral Sodium Lactate in the Treatment of Burn Shock. J Am Med Assoc. 1944;124:207–212. doi: 10.1001/jama.1944.02850040007002. [DOI] [Google Scholar]
- 44.Sørensen B. Management of burns occurring as mass casualties after nuclear explosion. Burns. 1979;6:33–36. doi: 10.1016/0305-4179(79)90035-4. [DOI] [Google Scholar]
- 45.Michell M.W., Oliveira H.M., Kinsky M.P., Vaid S.U., Herndon D.N., Kramer G.C. Enteral resuscitation of burn shock using world health organization oral rehydration solution: a potential solution for mass casualty care. J Burn Care Res. 2006;27:819–825. doi: 10.1097/01.BCR.0000245422.33787.18. [DOI] [PubMed] [Google Scholar]
- 46.Moghazy A.M., Adly O.A., Elbadawy M.A., Hashem R.E. Evaluation of who oral rehydration solution (ORS) and salt tablets in resuscitating adult patients with burns covering more than 15% of total body surface area (TBSA) Ann Burns Fire Disasters. 2016;29:43. [PMC free article] [PubMed] [Google Scholar]
- 47.Malic C.C., Karoo R.O.S., Austin O., Phipps A. Resuscitation burn card—a useful tool for burn injury assessment. Burns. 2007;33:195–199. doi: 10.1016/j.burns.2006.07.019. [DOI] [PubMed] [Google Scholar]
- 48.ISBI Practice Guidelines Committee, Ahuja R.B., Gibran N., Greenhalgh D., Jeng J., Mackie D. ISBI practice guidelines for burn care. Burns. 2016;42:953–1021. doi: 10.1016/j.burns.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 49.Pham T.N., Cancio L.C., Gibran N.S. American Burn Association practice guidelines burn shock resuscitation. J Burn Care Res. 2008;29:257–266. doi: 10.1097/BCR.0b013e31815f3876. [DOI] [PubMed] [Google Scholar]
- 50.Legrand M., Barraud D., Constant I., Devauchelle P., Donat N., Fontaine M. Management of severe thermal burns in the acute phase in adults and children. Anaesth Crit Care Pain Med. 2020;39:253–267. doi: 10.1016/j.accpm.2020.03.006. [DOI] [PubMed] [Google Scholar]
- 51.King B.T., Peterson W.C. The Care of Thermally Injured Patients in Operational, Austere, and Mass Casualty Situations. Wilderness Environ Med. 2017;28:S103–8. doi: 10.1016/j.wem.2017.03.011. [DOI] [PubMed] [Google Scholar]
- 52.Read D.J., Tan S.C., Ward L., McDermott K. Burns first aid treatment in remote Northern Australia. Burns. 2018;44:481–487. doi: 10.1016/j.burns.2017.07.013. [DOI] [PubMed] [Google Scholar]
- 53.Wood F.M., Phillips M., Jovic T., Cassidy J.T., Cameron P., Edgar D.W. Water first aid is beneficial in humans post-burn: evidence from a Bi-National cohort study. PLoS One. 2016;11 doi: 10.1371/journal.pone.0147259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Paratz J.D., Stockton K., Paratz E.D., Blot S., Muller M., Lipman J. Burn resuscitation-hourly urine output versus alternative endpoints: a systematic review. Review]. Shock. 2014;42:295–306. doi: 10.1097/SHK.0000000000000204. [DOI] [PubMed] [Google Scholar]
- 55.Fiandeiro D., Govindsamy J., Maharaj R.C. Prehospital cooling of severe burns: experience of the emergency department at Edendale Hospital, KwaZulu-Natal, South Africa. S Afr Med J. 2015;105:457. doi: 10.7196/SAMJ.8705. [DOI] [PubMed] [Google Scholar]
- 56.Read D.J., Tan S.C., Ward L., McDermott K. Burns first aid treatment in remote Northern Australia. Burns. 2018;44:481–487. doi: 10.1016/j.burns.2017.07.013. [DOI] [PubMed] [Google Scholar]
- 57.Nguyen N.L., Gun R.T., Sparnon A.L., Ryan P. The importance of initial management: a case series of childhood burns in Vietnam. Burns. 2002;28:167–172. doi: 10.1016/S0305-4179(01)00079-1. [DOI] [PubMed] [Google Scholar]
- 58.Wood F.M., Phillips M., Jovic T., Cassidy J.T., Cameron P., Edgar D.W. Water first aid is beneficial in humans post-burn: evidence from a Bi-National cohort study. PLoS One. 2016;11 doi: 10.1371/journal.pone.0147259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cuttle L., Kempf M., Liu P.-Y., Kravchuk O., Kimble R.M. The optimal duration and delay of first aid treatment for deep partial thickness burn injuries. Burns. 2010;36:673–679. doi: 10.1016/j.burns.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 60.Lam N.N., Dung N.T. First aid and initial management for childhood burns in Vietnam—an appeal for public and continuing medical education. Burns. 2008;34:67–70. doi: 10.1016/j.burns.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 61.Fadeyibi I.O., Ibrahim N.A., Mustafa I.A., Ugburo A.O., Adejumo A.O., Buari A. Practice of first aid in burn related injuries in a developing country. Burns. 2015;41:1322–1332. doi: 10.1016/j.burns.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 62.Stewart B.T., Gyedu A., Agbenorku P., Amankwa R., Kushner A.L., Gibran N. Routine systemic antibiotic prophylaxis for burn injuries in developing countries: a best evidence topic (BET) Int J Surg Lond Engl. 2015;21:168–172. doi: 10.1016/j.ijsu.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lowin J., Winfield T., Price P., Anderson P., Potokar T. Estimating the cost impact of dressing choice in the context of a mass burns casualty event. Ann Burns Fire Disasters. 2019;32:222–226. [PMC free article] [PubMed] [Google Scholar]
- 64.Kearney L., Francis E.C., Clover A.J. New technologies in global burn care - a review of recent advances. Int J Burns Trauma. 2018;8:77–87. [PMC free article] [PubMed] [Google Scholar]
- 65.Hussain S., Ferguson C. Silver sulphadiazine cream in burns. Emerg Med J EMJ. 2006;23:929–932. doi: 10.1136/emj.2006.043059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Aziz Z., Abdul Rasool Hassan B. The effects of honey compared to silver sulfadiazine for the treatment of burns: A systematic review of randomized controlled trials. Burns. 2017;43:50–57. doi: 10.1016/j.burns.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 67.Orgill D.P. Excision and skin grafting of thermal burns. N Engl J Med. 2009;360:893–901. doi: 10.1056/NEJMct0804451. [DOI] [PubMed] [Google Scholar]
- 68.Burd A., Noronha F.V., Ahmed K., Chan J.Y.W., Ayyappan T., Ying S.Y. Decompression not escharotomy in acute burns. Burns. 2006;32:284–292. doi: 10.1016/j.burns.2005.11.017. [DOI] [PubMed] [Google Scholar]
- 69.Orgill D.P., Piccolo N. Escharotomy and decompressive therapies in burns. J Burn Care Res. 2009;30:759–768. doi: 10.1097/BCR.0b013e3181b47cd3. [DOI] [PubMed] [Google Scholar]
- 70.Oda J., Ueyama M., Yamashita K., Inoue T., Harunari N., Ode Y. Effects of escharotomy as abdominal decompression on cardiopulmonary function and visceral perfusion in abdominal compartment syndrome with burn patients. J Trauma. 2005;59:369–374. doi: 10.1097/01.ta.0000174917.90514.4a. [DOI] [PubMed] [Google Scholar]
- 71.Ahuja R.B., Bhattacharya S. Burns in the developing world and burn disasters. BMJ. 2004;329:447–449. doi: 10.1136/bmj.329.7463.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Janzekovic Z. The burn wound from the surgical point of view. J Trauma. 1975;15:42–62. [PubMed] [Google Scholar]
- 73.Herndon D.N., Barrow R.E., Rutan R.L., Rutan T.C., Desai M.H., Abston S. A comparison of conservative versus early excision. Therapies in severely burned patients. Ann Surg. 1989;209:547–552. doi: 10.1097/00000658-198905000-00006. discussion 552-553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ahuja R.B., Bhattacharya S. An analysis of 11,196 burn admissions and evaluation of conservative management techniques. Burns J Int Soc Burn Inj. 2002;28:555–561. doi: 10.1016/s0305-4179(02)00069-4. [DOI] [PubMed] [Google Scholar]
- 75.Puri V., Khare N.A., Chandramouli M.V., Shende N., Bharadwaj S. Comparative analysis of early excision and grafting vs delayed grafting in burn patients in a developing country. J Burn Care Res Off Publ Am Burn Assoc. 2016;37:278–282. doi: 10.1097/BCR.0b013e31827e4ed6. [DOI] [PubMed] [Google Scholar]
- 76.Goswami P., Sahu S., Singodia P., Kumar M., Tudu T., Kumar A. Early excision and grafting in burns: an experience in a tertiary care industrial hospital of Eastern India. Indian J Plast Surg Off Publ Assoc Plast Surg India. 2019;52:337–342. doi: 10.1055/s-0039-3402707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Atiyeh B., Masellis A., Conte C. Optimizing burn treatment in developing low-and middle-income countries with limited health care resources (Part 2) Ann Burns Fire Disasters. 2009;22:189–195. [PMC free article] [PubMed] [Google Scholar]
- 78.Hundeshagen G., Suman O.E., Branski L.K. Rehabilitation in the acute versus outpatient setting. Clin Plast Surg. 2017;44:729–735. doi: 10.1016/j.cps.2017.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Porter C., Hardee J.P., Herndon D.N., Suman O.E. The role of exercise in the rehabilitation of patients with severe burns. Exerc Sport Sci Rev. 2015;43:34–40. doi: 10.1249/JES.0000000000000029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jacobson K., Fletchall S., Dodd H. Starnes C. Current concepts burn rehabilitation, part I: care during hospitalization. Clin Plast Surg. 2017;44:703–712. doi: 10.1016/j.cps.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 81.Gosselin R.A., Kuppers B. Open versus closed management of burn wounds in a low-income developing country. Burns. 2008;34:644–647. doi: 10.1016/j.burns.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 82.Edgar D., Brereton M. Rehabilitation after burn injury. BMJ. 2004;329:343–345. doi: 10.1136/bmj.329.7461.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bloemen M.C.T., van der Veer W.M., Ulrich M.M.W., van Zuijlen P.P.M., Niessen F.B., Middelkoop E. Prevention and curative management of hypertrophic scar formation. Burns. 2009;35:463–475. doi: 10.1016/j.burns.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 84.Finnerty C.C., Jeschke M.G., Branski L.K., Barret J.P., Dziewulski P., Herndon D.N. Hypertrophic scarring: the greatest unmet challenge after burn injury. Lancet Lond Engl. 2016;388:1427–1436. doi: 10.1016/S0140-6736(16)31406-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.European Burns Association . 2015. European practice guidelines for burn care. [Google Scholar]
- 86.Bricknell Julie, Chan Wai, Darton Anne, Edmondson Rachel, Iddamalgoda Tanya, Katsu Akane. 2017. Burn physiotherapy and occupational therapy guidelines. [Google Scholar]
- 87.Young A.W., Graves C., Kowalske K.J., Perry D.A., Ryan C.M., Sheridan R.L. Guideline for burn care under austere conditions: special care topics. J Burn Care Res Off Publ Am Burn Assoc. 2017;38:e497–509. doi: 10.1097/BCR.0000000000000369. [DOI] [PubMed] [Google Scholar]
- 88.Burkle F.M., Potokar T., Gosney J.E., Dallas C. Justification for a Nuclear Global Health Workforce: multidisciplinary analysis of risk, survivability & preparedness, with emphasis on the triage management of thermal burns. Confl Health. 2017;11:13. doi: 10.1186/s13031-017-0116-y. [DOI] [PMC free article] [PubMed] [Google Scholar]