Abstract
Background
Dissemination of cardiopulmonary resuscitation (CPR) skills is essential for cardiac arrest survival. Virtual reality (VR)‐training methods are low cost and easily available, but to meet depth requirements adaptations are required, as confirmed in a recent randomized study on currently prevailing CPR quality criteria. Recently, the promising clinical performance of new CPR quality criteria was demonstrated, based on the optimal combination of compression depth and rate. We now study compliance with these newly proposed CPR quality criteria.
Methods and Results
Post hoc analysis of a randomized trial compared standardized 20‐minute face‐to‐face CPR training with VR training using the Lifesaver VR smartphone application. During a posttraining test, compression depth and rate were measured using CPR mannequins. We assessed compliance with the newly proposed CPR criteria, that is, compression rate within ±20% of 107/minute and depth within ±20% of 47 mm. We studied 352 participants, age 26 (22–31) years, 56% female, and 15% with CPR training ≤2 years. Among VR‐trained participants, there was a statistically significant difference between the proportions complying with newly proposed versus the currently prevailing quality criteria (52% versus 23%, P<0.001). The difference in proportions complying with rate requirements was statistically significant (96% for the new versus 50% for current criteria, P<0.001), whereas there was no significant difference with regard to the depth requirements (55% versus 51%, P=0.45).
Conclusions
Lifesaver VR training, although previously found to be inferior to face‐to‐face training, may lead to CPR quality compliant with recently proposed, new quality criteria. If the prognostic importance of these new criteria is confirmed in additional studies, Lifesaver VR in its current form would be an easily available vector to disseminate CPR skills.
Keywords: basic life support, cardiac arrest, cardiopulmonary resuscitation, education, virtual reality
Subject Categories: Cardiopulmonary Arrest
High‐quality cardiopulmonary resuscitation (CPR) is essential for survival after cardiac arrest. 1 , 2 Guidelines advise a chest compression rate of 100 to 120/minute and a depth of 50 to 60 mm. 1 , 2 In a recently performed randomized trial on virtual reality (VR) versus instructor‐led training, we found that VR training often leads to suboptimal compression depth (<50 mm), suggesting that VR training should be developed further. 3
However, current guidelines are based on studies that evaluated the impact of rate and depth separately, even though rate and depth have been shown to interact. 1 , 2 , 4 , 5 Recently, the first ever cardiac arrest study on the optimal combination of these factors was performed, identifying an optimal zone of different combinations of rate and depth associated with favorable clinical outcome. That study, on over 3500 patients treated across 150 emergency medical services, suggested that the highest survival occurs if compression rate is within ±20% of 107 compressions per minute in combination with a depth within ±20% of 47 mm. 4 These ranges markedly differ from guideline recommendations and might be easier to achieve for lay rescuers. In that context, we evaluated how often this combination of rate and depth was achieved in instructor‐led and VR‐trained adult (≥18 years) study participants.
Methods
The data that support the findings of this study are available from the corresponding author upon reasonable request.
This is a post hoc analysis of the Lowlands Saves Lives trial, a 1:1 randomized controlled trial comparing CPR quality between face‐to‐face and Lifesaver VR CPR training, as previously described. 3 , 6
Lowlands Saves Lives was performed during Lowlands Science, which was a section of the Lowlands music festival (August 16–18, 2019, Biddinghuizen, the Netherlands) dedicated exclusively to conducting scientific research. Festival attendees were eligible for participation if they were adults (≥18 years) and considered physically and mentally capable of participating in CPR training and the posttraining CPR test. The proportion of participants with previous CPR training ≤2 years was capped at 20%. After providing written informed consent, all participants completed a questionnaire regarding demographics, previous CPR training, and CPR experience. This study received approval from the research ethics committee of the Radboudumc.
Interventions
Participants were randomized to a 20‐minute face‐to‐face training or a 20‐minute training using Lifesaver VR. The latter is a free smartphone application, developed by the UK Resuscitation Council, that can be used at home for a 20‐minute CPR training using only a smartphone and commercially available VR goggles. Compressions are practiced on a pillow. The VR application provides feedback on rate and instructions, but no real‐time feedback on compression depth. This was in contrast to the participants randomized to face‐to‐face training, with an instructor actively coaching on both rate and depth.
Outcomes Measures
Following the training, all participants completed the same CPR test, of which the standardized protocol was published previously. 3 , 6 This test was supervised by assessors who were blinded to the intervention. All participants completed a uniform CPR scenario in which they demonstrated the acquired CPR skills. During this scenario, primary outcome measures (compression rate and depth) were measured objectively using CPR mannequins (Resusci Anne QCPR, Laerdal Medical, Stavanger, Norway). The information was downloaded from the mannequins for offline analysis.
Statistical Analysis
We calculated the proportions of participants who met the recently proposed, new criteria for optimal CPR quality, defined using the aforementioned criteria (rate 86–128/minute and depth 38–56 mm). 4 We also reported on the proportions of participants meeting the current guideline criteria and compared proportions meeting the newly proposed and currently prevailing quality criteria. Furthermore, we compared baseline demographics and characteristics between participants who did or did not comply with the newly proposed criteria. Categorical variables were reported as numbers (percentages) and compared between groups using a χ2 test or a Fisher's exact test, whichever was appropriate. Continuous variables were analyzed for gaussian distribution and reported as means± SD or medians (interquartile ranges), whichever was appropriate. Comparisons between groups were performed accordingly, with either a Student's t test or a Mann‐Whitney U test. All analyses were performed with SPSS (Version 25, IBM, Armonk, NY, USA). A P value of <0.05 was considered statistically significant.
Results
In the Lowlands Saves Lives study, 381 participants were randomized. In the present analyses, we studied 352 participants, as 29 participants did not complete the training and/or CPR test, mainly because of long waiting lines. Median age was 26 (interquartile range 22–31) years, 56% were female and 15% had recent (≤2 years) CPR training.
Figure displays the achieved CPR quality of all participants, Lifesaver VR‐trained participants, and face‐to‐face trained participants, using a heat map. 4 Optimal CPR quality according to the new criteria was achieved by 40% of all participants.
Figure . Heat maps of the achieved CPR quality.
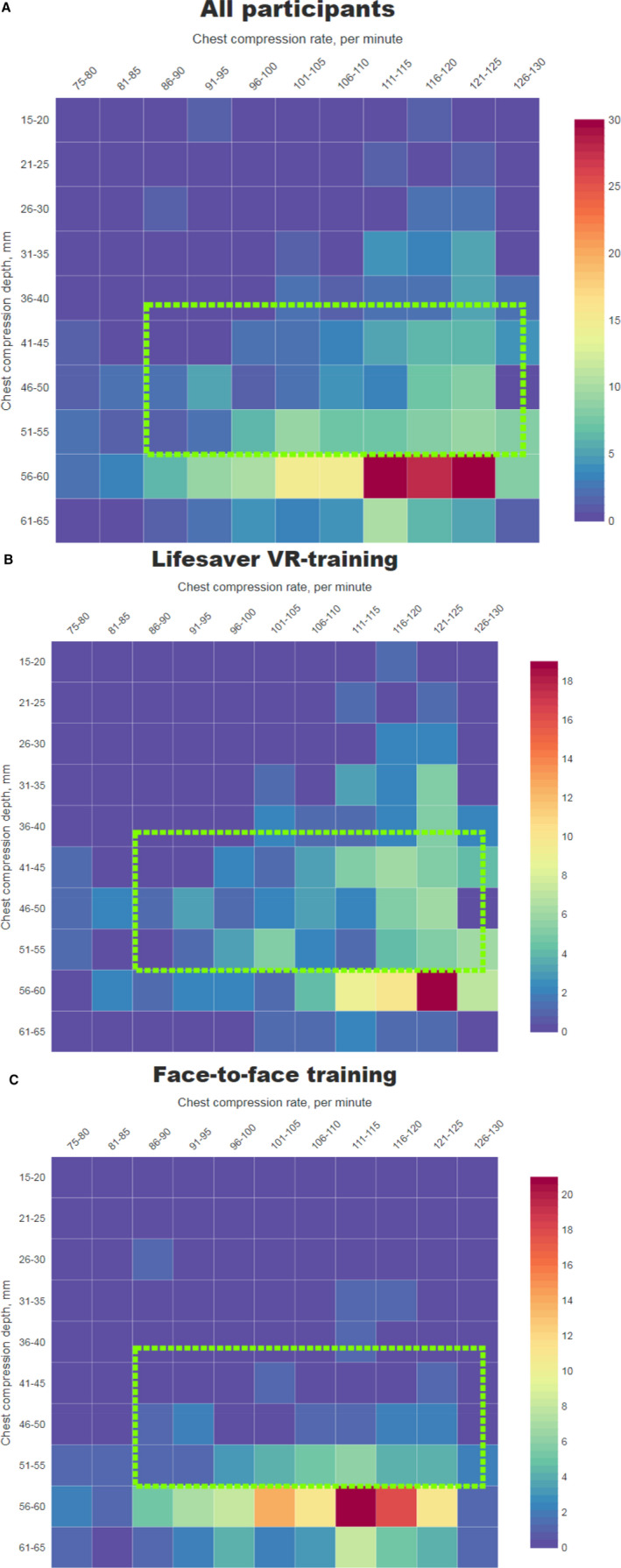
A, CPR quality of all study participants; (B) CPR quality of VR‐trained participants; (C) CPR quality of face‐to‐face trained participants. Chest compression depth (y‐axis) and rate (x‐axis). Colors toward dark blue indicate a lower number of participants with that specific combination of rate and depth. The green dashed rectangle indicates the range for the newly proposed criteria for optimal CPR quality. Overall, 40% of the participants complied with these criteria; 52% were in the VR group and 28% in the face‐to‐face group. CPR indicates cardiopulmonary resuscitation; and VR, virtual reality.
In terms of CPR quality in the Lifesaver VR group, 52% met the newly proposed optimal combination of depth and rate. When studied separately, the rate range was met by 96% and the depth range by 55% of study participants. For reference, according to the current guideline criteria, 23% of the Lifesaver VR‐trained participants met both the rate and depth ranges. When considered separately, 50% met the rate range and 51% met the depth range of prevailing CPR quality guidelines. 3
For comparisons of CPR quality within the Lifesaver group, the difference between the proportion complying with the newly proposed citeria (52%) and the proportion meeting both rate and depth requirements according to the current quality criteria (23%) was statistically significant (P<0.001). The difference in proportions meeting the new versus current rate criteria was statistically significant as well (P<0.001), whereas the comparison between new versus current depth criteria was not (P=0.45).
In the face‐to‐face trained group, 28% met the newly proposed CPR quality criteria. The depth range was met by 30% and the rate range by 97%. For reference, 49% of these participants met the current guideline quality criteria, with 75% meeting the depth range and 63% meeting the guideline rate range. 3
The Table shows a comparison between participants with and without optimal CPR quality according to the newly proposed criteria. There were no statistically significant differences in median age (25 [22–32] versus 26 [22–31], P=0.61), or proportions of female sex (61% versus 54%, P=0.17), university education (43% versus 45%, P=0.65), healthcare professionals (18% versus 22%, P=0.37), and previous CPR course ≤2 years (15% versus 17%, P=0.64) between participants with or without optimal CPR quality according to the new criteria. The median weight was significantly lower in participants complying with the newly proposed CPR quality criteria than in those not complying with the newly proposed criteria (69 kg [62–78] compared with 73 kg [64–80], P=0.02).
Table 1.
Participants' Characteristics According to Newly Proposed CPR Quality Criteria
| CPR Quality Optimal (n=141) | CPR Quality Not Optimal (n=211) | P Value | |
|---|---|---|---|
| Baseline characteristics | |||
| Female sex (n=350) | 86 (61%) | 112 (54%) | 0.17 |
| Age, y (n=352) | 25 (22–32) | 26 (22–31) | 0.61 |
| Weight, kg (n=352) | 69 (62–78) | 73 (64–80) | 0.02 |
| University education (n=352) | 60 (43%) | 95 (45%) | 0.65 |
| Healthcare professional (n=351) | 26 (18%) | 47 (22%) | 0.37 |
| Previous CPR course ≤2 y (n=332) | 20 (15%) | 33 (17%) | 0.64 |
| Ever witnessed a cardiac arrest (n=352) | 22 (16%) | 34 (16%) | 0.90 |
| Breath alcohol level ≥0.5‰ (n=352) | 26 (18%) | 27 (13%) | 0.15 |
| Drugs or narcotics ≤24 h (n=342) | 37 (26%) | 48 (24%) | 0.58 |
| Allocated to Lifesaver virtual reality (n=352) | 91 (65%) | 84 (40%) | <0.001 |
Comparison of baseline characteristics and intervention between participants with optimal CPR quality and participants with no optimal CPR quality according to the newly proposed criteria. CPR indicates cardiopulmonary resuscitation.
Discussion
In this post hoc analysis of a randomized trial, we demonstrate that 52% of VR‐trained individuals meet the newly proposed CRP quality criteria, which is twice as high as according to prevailing CPR criteria. These improvements are mainly related to better compliance with the newly proposed criteria for compression rate. Our findings provide important input for future educational developments and future clinical studies on assessment of criteria for optimal CPR quality.
VR‐Assisted CPR Training
VR training is an emerging CPR training modality, with several studies showing promising results in terms of usability and outcomes of training. 7 , 8 , 9 , 10 , 11 , 12 , 13 It is considered to hold promising potential according to a recent survey among resuscitation experts (members of national resuscitation councils, educators, and instructors), as this application may reach a broad target population of all ages, in particular young people, with the possibility of at‐home CPR training. 14
Besides Lifesaver VR, several other technological innovations in CPR training have recently been developed. For example, a VR‐enhanced mannequin is a device that uses VR in combination with a traditional mannequin to teach CPR. 9 , 10 Using a professional mannequin has the potential advantage of teaching high‐quality chest compressions, but the downside is that such trainings require considerable investments in training equipment. With Lowlands Saves Lives, we specifically focused on CPR training that can be performed at every location at minimal costs, with the potential advantage to sensitize a larger audience for CPR training. 3 , 6 Another previous study on VR training focused on advanced cardiac life support, in contrast to our study, in which we specifically focused on basic life support and automated external defibrillator use. 15
CPR Quality
A major downside that should be addressed in further studies is chest compression depth, which has repeatedly been shown to be lower in VR training compared with face‐to‐face training. 3 , 8 In a previous study on short VR training, pressing a button was used to practice chest compressions. In that study, mean compression depth was 38 mm, which is markedly lower than in our Lifesaver VR group, who used a pillow to practice chest compressions. 8 Notably, compression depth following VR training was still significantly lower than that following face‐to‐face training, demonstrating the value of instructor‐led training and suggesting the need to adapt the VR training. 3
However, with the newly proposed criteria, VR training in its current form shows promising results. This low‐cost, easily available, 20‐minute training could result in a widespread dissemination of resuscitation skills, with potentially about half of its users acquiring high‐quality CPR skills. These findings also underscore the need to investigate the newly proposed criteria in additional cardiac arrest cohorts, as it may provide important information for the development and adaptation of educational tools.
Notably, the primary goal of this post hoc analysis is to demonstrate the promising results of the Lifesaver VR in its current form, which should not be interpreted in terms of superiority to face‐to‐face training. Participants in this latter group received active feedback on compression depth, targeted to the current guideline criteria. Importantly, in the derivation study of the newly proposed CPR quality criteria, data refer to in‐field resuscitations by professionals, also trained according to prevailing guidelines. Notably, the Lifesaver VR outcomes reflect the controlled setting of a posttraining CPR test and it is unknown how this translates into actual in‐field CPR performance. 3 , 4 Finally, as study participants were trained to comply with current guidelines, and not with the newly proposed quality criteria, it is uncertain what outcomes would be after specific training on the new criteria.
Conclusions
Whereas our previous analyses suggested the need for adaptation of Lifesaver VR, the present analysis shows more promising results, as over 50% of recently trained individuals complied with newly proposed CPR quality criteria. If the prognostic importance of these criteria is confirmed in additional cardiac arrest populations, Lifesaver VR in its current form would be an easily available vector to further disseminate CPR skills.
Sources of Funding
None.
Disclosures
Dr van Geuns reports grants from Abbott Vascular, Boston Scientific, and Amgen and personal fees from Abbott Vascular outside the submitted work. Dr van Royen received research grants from Abbott, Biotronik, AstraZeneca, and Philips and professional fees from Abbott, MicroPort, Amgen, and Medtronic. The remaining authors have no disclosures to report.
Acknowledgments
We would like to thank Lowlands Science for providing the opportunity to perform this study during the Lowlands festival. We are greatly indebted to our face‐to‐face instructors, and all festival attendees that participated in the trial.
(J Am Heart Assoc.2021;10:e017367. DOI: 10.1161/JAHA.120.017367.)
For Sources of Funding and Disclosures, see page 6.
Registration: URL: www.clinicaltrials.gov; Unique identifier: NCT04013633.
References
- 1. Kleinman ME, Brennan EE, Goldberger ZD, Swor RA, Terry M, Bobrow BJ, Gazmuri RJ, Travers AH, Rea T. Part 5: adult basic life support and cardiopulmonary resuscitation quality: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S414–S435. 10.1161/CIR.0000000000000259 [DOI] [PubMed] [Google Scholar]
- 2. Perkins GD, Handley AJ, Koster RW, Castrén M, Smyth MA, Olasveengen T, Monsieurs KG, Raffay V, Gräsner J‐T, Wenzel V, et al. European Resuscitation Council Guidelines for Resuscitation 2015: section 2. Adult basic life support and automated external defibrillation. Resuscitation. 2015;95:81–99. 10.1016/j.resuscitation.2015.07.015 [DOI] [PubMed] [Google Scholar]
- 3. Nas J, Thannhauser J, Vart P, van Geuns R‐J, Muijsers HEC, Mol J‐Q, Aarts GWA, Konijnenberg LSF, Gommans DHF, Ahoud‐Schoenmakers SGAM, et al. Effect of face‐to‐face vs virtual reality training on cardiopulmonary resuscitation quality: a randomized clinical trial. JAMA Cardiol. 2019;5:328–335. 10.1001/jamacardio.2019.4992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Duval S, Pepe PE, Aufderheide TP, Goodloe JM, Debaty G, Labarere J, Sugiyama A, Yannopoulos D. Optimal combination of compression rate and depth during cardiopulmonary resuscitation for functionally favorable survival. JAMA Cardiol. 2019;4:900–908. 10.1001/jamacardio.2019.2717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Idris AH. The sweet spot: chest compressions between 100–120/minute optimize successful resuscitation from cardiac rest. JEMS. 2012;37:4–9. [PMC free article] [PubMed] [Google Scholar]
- 6. Nas J, Thannhauser J, Vart P, van Geuns RJ, van Royen N, Bonnes JL, Brouwer MA. Rationale and design of the Lowlands Saves Lives trial: a randomised trial to compare CPR quality and long‐term attitude towards CPR performance between face‐to‐face and virtual reality training with the Lifesaver VR app. BMJ Open. 2019;9:e033648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cerezo Espinosa C, Segura Melgarejo F, Melendreras Ruiz R, García‐Collado ÁJ, Nieto Caballero S, Juguera Rodríguez L, Pardo Ríos S, García Torrano S, Linares Stutz E, Pardo RM. Virtual reality in cardiopulmonary resuscitation training: a randomized trial. Emergencias. 2019;31:43–46. [PubMed] [Google Scholar]
- 8. Leary M, McGovern SK, Chaudhary Z, Patel J, Abella BS, Blewer AL. Comparing bystander response to a sudden cardiac arrest using a virtual reality CPR training mobile app versus a standard CPR training mobile app. Resuscitation. 2019;139:167–173. 10.1016/j.resuscitation.2019.04.017 [DOI] [PubMed] [Google Scholar]
- 9. Semeraro F, Frisoli A, Bergamasco M, Cerchiari EL. Virtual reality enhanced mannequin (VREM) that is well received by resuscitation experts. Resuscitation. 2009;80:489–492. 10.1016/j.resuscitation.2008.12.016 [DOI] [PubMed] [Google Scholar]
- 10. Semeraro F, Frisoli A, Loconsole C, Banno F, Tammaro G, Imbriaco G, Marchetti L, Cerchiari EL. Motion detection technology as a tool for cardiopulmonary resuscitation (CPR) quality training: a randomised crossover mannequin pilot study. Resuscitation. 2013;84:501–507. 10.1016/j.resuscitation.2012.12.006 [DOI] [PubMed] [Google Scholar]
- 11. Semeraro F, Frisoli A, Loconsole C, Mastronicola N, Stroppa F, Ristagno G, Scapigliati A, Marchetti L, Cerchiari E. Kids (learn how to) save lives in the school with the serious game Relive. Resuscitation. 2017;116:27–32. 10.1016/j.resuscitation.2017.04.038 [DOI] [PubMed] [Google Scholar]
- 12. Semeraro F, Ristagno G, Giulini G, Gnudi T, Kayal JS, Monesi A, Tucci R, Scapigliati A. Virtual reality cardiopulmonary resuscitation (CPR): comparison with a standard CPR training mannequin. Resuscitation. 2019;135:234–235. 10.1016/j.resuscitation.2018.12.016 [DOI] [PubMed] [Google Scholar]
- 13. Wong M, Chue S, Jong M, Benny HWK, Zary N. Clinical instructors' perceptions of virtual reality in health professionals' cardiopulmonary resuscitation education. SAGE Open Med. 2018;6:2050312118799602. 10.1177/2050312118799602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Semeraro F, Scapigliati A, Ristagno G, Luciani A, Gandolfi S, Lockey A, Müller MP, Wingen S, Böttiger BW. Virtual reality for CPR training: how cool is that? Dedicated to the "next generation". Resuscitation. 2017;121:e1–e2. 10.1016/j.resuscitation.2017.09.024 [DOI] [PubMed] [Google Scholar]
- 15. Khanal P, Vankipuram A, Ashby A, Vankipuram M, Gupta A, Drumm‐Gurnee D, Josey K, Tinker L, Smith M. Collaborative virtual reality based advanced cardiac life support training simulator using virtual reality principles. J Biomed Inform. 2014;51:49–59. 10.1016/j.jbi.2014.04.005 [DOI] [PubMed] [Google Scholar]


