Abstract
Background
Sex differences in the trends for control of cardiovascular disease (CVD) risk factors have been described, but temporal trends in the age at which CVD and its risk factors are diagnosed and sex‐specific differences in these trends are unknown.
Methods and Results
We used the Medical Expenditure Panel Survey 2008 to 2017, a nationally representative sample of the US population. Individuals ≥18 years, with a diagnosis of hypercholesterolemia, hypertension, coronary heart disease, or stroke, and who reported the age when these conditions were diagnosed, were included. We included 100 709 participants (50.2% women), representing 91.9 million US adults with above conditions. For coronary heart disease and hypercholesterolemia, mean age at diagnosis was 1.06 and 0.92 years older for women, compared with men, respectively (both P<0.001). For stroke, mean age at diagnosis for women was 1.20 years younger than men (P<0.001). The mean age at diagnosis of CVD risk factors became younger over time, with steeper declines among women (annual decrease, hypercholesterolemia [women, 0.31 years; men 0.24 years] and hypertension [women, 0.23 years; men, 0.20 years]; P<0.001). Coronary heart disease was not statistically significant. For stroke, while age at diagnosis decreased by 0.19 years annually for women (P=0.03), it increased by 0.22 years for men (P=0.02).
Conclusions
The trend in decreasing age at diagnosis for CVD and its risk factors in the United States appears to be more pronounced among women. While earlier identification of CVD risk factors may provide opportunity to initiate preventive treatment, younger age at diagnosis of CVD highlights the need for the prevention of CVD earlier in life, and sex‐specific interventions may be needed.
Keywords: age of diagnosis, cardiovascular disease, risk factors, sex differences
Subject Categories: Primary Prevention, Risk Factors, Women, Epidemiology
Nonstandard Abbreviations and Acronyms
- MEPS
Medical Expenditure Panel Surveys
Clinical Perspective
What Is New?
This study suggests that there is a trend of decreasing age at diagnosis of cardiovascular disease (CVD) and CVD risk factors, which appears to be more pronounced among women.
This could be a reflection of improved screening and detection of CVD and its risk factors at younger ages, or that the US population has been getting sicker at younger ages over time.
Younger age at the time of diagnosis of clinical CVD has significant public health implications, as this could potentially translate to greater disability; loss of productivity; reduction in the quality of life; and excessive financial burden on patients, their families, and the US healthcare system.
What Are the Clinical Implications?
The results from this study support more aggressive, high‐impact, and proactive strategies for the primary prevention of CVD and its risk factors, particularly among the younger population in the outpatient setting.
Cardiovascular disease (CVD) remains the leading cause of morbidity and mortality worldwide and is a major cause of lost productivity in the United States. 1 , 2 Mortality rates from CVD in the United States had been steadily declining from 1990 through 2010, but there has been stagnation in this progress over the past decade, particularly among young adults and especially women. 3 , 4 , 5 , 6 , 7 , 8 In fact, death rates from heart disease have been on the rise for middle‐aged women 45 to 64 years of age. 5 Even though advancing age is the strongest risk factor for CVD, over 60% of individuals living with CVD are <65 years old. 2 Sex differences in trends of control of CVD risk factors such as hypertension and dyslipidemia have been described, with better control of hypertension noted among women but not with dyslipidemia. 9 However, the temporal trends in the age at which CVD or its risk factors are diagnosed in the United States and whether there are sex‐specific differences in these trends is unknown.
Younger age at the time of diagnosis of clinical CVD has significant public health implications, as this could potentially translate to greater loss of productivity; disability years lived; reduction in the quality of life; and excessive financial burden on patients, their families, and the US healthcare system. 7 , 8 On the other hand, younger age at diagnosis of risk factors for CVD could be an opportunity for earlier and better control of these risk factors to delay the onset of the disease, which will be beneficial in the long run. 8 , 10 It is also important to know whether there are sex‐specific differences in the age of CVD onset, as this may support the implementation of sex‐specific interventions for the improvement of cardiovascular outcomes. 11 , 12
The current study was designed to describe the overall and sex‐specific trends in age at diagnosis of CVD and its risk factors, using data from a nationally representative sample of the US adult civilian population from 2008 to 2017. We hypothesized that the mean age at diagnosis of CVD and its risk factors has decreased over time and that women have experienced steeper declines in the age at diagnosis of CVD, compared with men.
Transparency and Openness Policy
The Medical Expenditure Panel Surveys (MEPS) are publicly available data sets available from the Agency for Healthcare Research and Quality. While we are not directly providing data sets, our study findings should be easily reproducible from the methods described in paper.
Methods
Data for this study were obtained from the MEPS from January 1, 2008 to December 31, 2017. The MEPS is a cross‐sectional data set, cosponsored by the National Center for Health Statistics and the Agency for Healthcare Research and Quality. 13 , 14 , 15 , 16 , 17 It contains nationally representative samples of the US civilian noninstitutionalized population. The MEPS collects data of individuals and families using an overlapping panel design where new households are included yearly, and detailed information is collected for each person in the household in several rounds of interviews. 13 , 14 , 15 , 16 , 17 Information collected includes sociodemographic characteristics, health conditions, health resource use and expenditure, health insurance coverage, access to care, and patient satisfaction with health care. Informed consent was obtained by the Agency for Healthcare Research and Quality researchers. More detailed information on the background and data collection process of the MEPS is available in Data S1.
Information from the MEPS are saved in different files. For instance, demographic information is available in the MEPS full‐year consolidated file, information on medical diagnoses are saved in the medical conditions file, medication data are available in the prescribed medicines file. We merged the full‐year consolidated and the medical conditions file from 2008 to 2017, to obtain all necessary information on the participants included in this study. Of note, starting from 2016, the MEPS upgraded from the International Classification of Diseases, Ninth Revision (ICD‐9), to the Tenth Revision (ICD‐10) codes for medical conditions.
Participants, CVD, and Its Risk Factors and Definitions
For the purpose of these analyses, the term CVD is used to include coronary heart disease (CHD) and stroke. CVD risk factors described here includes hypertension and hypercholesterolemia. The diagnosis of CVD and its risk factors was based on self‐report or ICD diagnosis. The ICD codes used include CHD (ICD‐9: 410, 413, and 414; ICD‐10: I20, I21, and I25), stroke (ICD‐9: 433–437; ICD‐10: I163–I167), hypertension (ICD‐9: 401; ICD‐10: I10), and hypercholesterolemia (ICD‐9: 278; ICD‐10: E78). The MEPS questionnaire contains questions asking if participants had ever been diagnosed as having CHD, hypertension, stroke, or high cholesterol, and these questions remained the same over the study period. Individuals with any of the above medical conditions were asked at what age the diagnosis was made, and this information was included in the full‐year consolidated file. The age of diagnosis for CHD, stroke, hypertension, and hypercholesterolemia was top‐coded at 85 years. 18 Per guidelines from the Department of Health and Human Services, this study did not require approval from an institutional review board since the MEPS contains only a deidentified, publicly available data set. 19
Other Study Variables
Some of the sociodemographic variables used in this study include current age groups (18–39, 40–64, and ≥65 years), race/ethnicity (non‐Hispanic White, Black, Asian, and Hispanic), health insurance (uninsured, Medicaid, private, Medicare), level of education (less than high school, high school/Graduate Educational Development, and some college or higher), and geographic region (Northeast, Midwest, South, and West). Family income was categorized on the basis of the federal poverty level; <125% of the federal poverty level was classified as very low income/poor, 125% to <200% of the federal poverty level as low income, 200% to <400% of the federal poverty level as middle income, ≥400% of the federal poverty level as high income. An individual's comorbidity burden was estimated using the Charlson comorbidity index. 20 , 21
Statistical Analysis
MEPS data from 2008 to 2017 were combined to calculate the mean age at diagnosis for CHD, stroke, hypertension, and hypercholesterolemia for men and women. The mean age at diagnosis was calculated for each of the above medical conditions for each year from 2008 to 2017, for the total population, and then for men and women separately. We also combined CHD and stroke to generate a single variable and averaged the age at diagnosis for these 2 conditions for each survey year. The trend in the mean age at diagnosis for CHD, stroke, hypertension, hypercholesterolemia, and a combination of CHD and stroke was calculated from the annual change overall and by sex, using a linear regression model. This same trend analysis was repeated for each medical condition, with further stratification by current age group, race/ethnicity, level of income, type of health insurance, and region. We also used linear regression to estimate the mean difference in the age at diagnosis of women compared with men for CHD, stroke, hypertension, and hypercholesterolemia, adjusted for the covariates mentioned above.
All statistical analyses were conducted using Stata version 14 (StataCorp LLC, College Station, TX) in April 2020. We used the svy command in Stata to declare the data set used as survey data. All weighted regression analyses were adjusted for current age, race/ethnicity, level of income, educational status, health insurance, and comorbid conditions. P values were 2‐tailed, and the level of significance was set at <0.05.
Results
From 2008 to 2017, a total of 100 709 participants (50.2% women), representing 91.9 million US civilian adults with CHD, hypertension, hypercholesterolemia, or stroke, who reported an age at diagnosis for these conditions were included. As shown in Table 1, over 40% of both men and women included were between 40 and 64 years of age at the time of MEPS survey. The majority of the patients studied were non‐Hispanic White individuals, with 69.7% and 72.5% of the women and men being non‐Hispanic White individuals, respectively. About 45% of the women and 54% of the men had private insurance. Additional sociodemographics by sex are as follows: completed at least high school education or its equivalent (53.5% women and 53.3% men), earned high income (36.6% women and 46.8% men), and resided in the southern region of the country (39.6% women and 38.2% men).
Table 1.
Sociodemographic Characteristics of Individuals With Cardiovascular Disease or Its Risk Factors by Sex: MEPS 2008 to 2017
| Women | Men | Total | |
|---|---|---|---|
| N | 50 556 | 50 153 | 100 709 |
| Weighted sample | 46 161 722 | 45 793 899 | 91 955 621 |
| Current age groups in y (weighted %) | |||
| 18–39 | 12.4 | 15.5 | |
| 40–64 | 49.3 | 53.3 | |
| ≥65 | 38.3 | 31.2 | |
| Race/Ethnicity (weighted %) | |||
| Non‐Hispanic White | 69.7 | 72.5 | |
| Non‐Hispanic Black | 14.1 | 10.8 | |
| Asian | 4.2 | 4.6 | |
| Hispanic | 12.0 | 12.1 | |
| Insurance status (weighted %) | |||
| Uninsured | 7.5 | 8.9 | |
| Private | 45.5 | 54.5 | |
| Medicaid | 11.0 | 8.0 | |
| Medicare | 36.0 | 28.7 | |
| Education (weighted %) | |||
| Less than high school | 18.3 | 16.7 | |
| High school/General Education Development (GED) | 53.5 | 53.3 | |
| Some college or higher | 28.2 | 30.0 | |
| Level of income (weighted %) | |||
| High income | 36.6 | 46.8 | |
| Middle income | 29.2 | 28.4 | |
| Low income | 15.1 | 11.9 | |
| Poor/very low income | 19.1 | 12.9 | |
| Region (weighted %) | |||
| Northeast | 17.9 | 18.1 | |
| Midwest | 21.7 | 21.5 | |
| South | 39.6 | 38.2 | |
| West | 20.8 | 22.2 | |
MEPS indicates Medical Expenditure Panel Survey.
Figure 1 shows the mean age at diagnosis for CHD, stroke, hypertension, and hypercholesterolemia for men and women (CHD: men, 57.4 years versus women, 59.3 years; P<0.001; stroke: men, 58.7 years versus women 57.6 years; P<0.001; hypercholesterolemia: men, 48.7 years versus women, 51.6 years; P<0.001; hypertension: men, 46.8 years versus women, 48.8 years; P=0.05).
Figure 1. Mean age at diagnosis of cardiovascular disease/risk factors among US adults, by sex: 2008 to 2017.
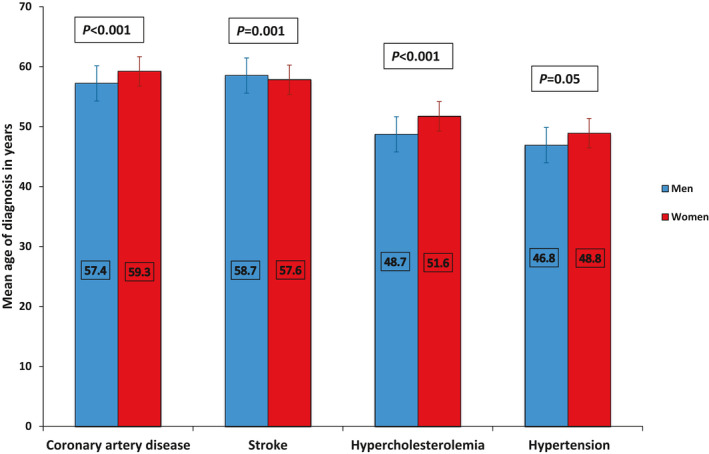
Table 2 shows the adjusted mean difference in the age at diagnosis of CVD and its risk factors in women compared with men. For CHD, the mean age at diagnosis was 1.06 years older for women compared with men (P<0.001). Regarding hypercholesterolemia, the mean age at diagnosis was 0.92 years older for women compared with men (P<0.001). Women were also diagnosed with hypertension at an older age compared with men, but this finding was not statistically significant. For stroke, the mean age at diagnosis for women was 1.20 years younger compared with men (P<0.001).
Table 2.
Adjusted Mean Difference in the Age of Diagnosis (in Years) of Cardiovascular Disease and Its Risk Factors Among US Adults, Stratified by Sex: MEPS 2008 to 2017
| Age of Diagnosis (in y) of CVD/CVD Risk Factors | Men | Women | P Value |
|---|---|---|---|
| β (95% CI) in y | |||
| Coronary heart disease | Ref | 1.06 (0.48 to 1.63)* | <0.001* |
| Hypercholesterolemia | Ref | 0.92 (0.70 to 1.15)* | <0.001* |
| Hypertension | Ref | 0.28 (−0.01 to 0.57) | 0.05 |
| Stroke | Ref | −1.20 (−1.89 to −0.49)* | 0.001* |
The beta‐coefficients and their 95% CIs were obtained from linear regression models. All models compared women with men and were adjusted for current age, race/ethnicity, level of income, health insurance, educational status, and Charlson comorbidity index. MEPS indicates Medical Expenditure Panel Survey.
Results are statistically significant with P<0.05.
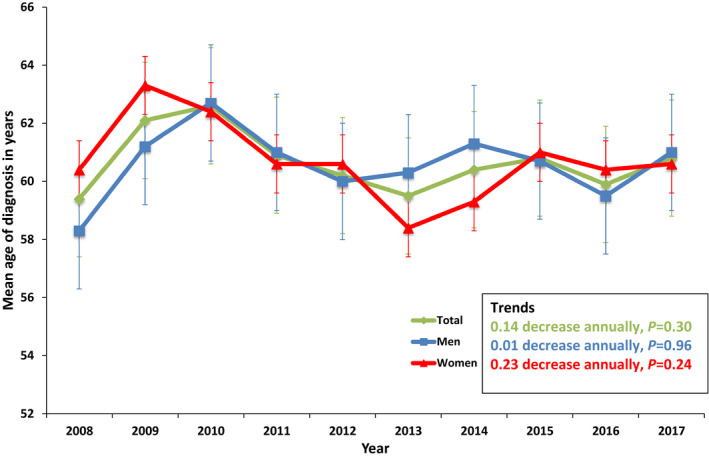
Figures 2, 3, 4, 5, 6 show the sex‐specific trends in the adjusted mean age at diagnosis for CVD and its risk factors from 2008 to 2017. Over this 10‐year period, there was an average annual decrease in the age at diagnosis of CHD for men and women, but this was not statistically significant (Figure 2). For stroke, the age at diagnosis decreased by 0.19 years annually for women (P=0.03), but increased by 0.22 annually for men (P=0.02) (Figure 3). Figure 4 shows a decreasing trend in the mean age at diagnosis for hypercholesterolemia from 2008 to 2017. Overall, there was a decrease of 0.28 years annually in the age at diagnosis for hypercholesterolemia (P<0.001), reflecting an average yearly decrease of 0.31 and 0.24 years for women and men, respectively (both P<0.001). Similar trends are seen in the age at diagnosis of hypertension from 2008 to 2017; there was an annual decrease of 0.21, 0.23, and 0.20 years in the age at diagnosis of hypertension for overall, and for women and men, respectively (all P<0.001) (Figure 5). There was an annual decrease in the age at diagnosis of CHD and stroke combined for men, women, and the total population, but this was not statistically significant (Figure 6).
Figure 2. Adjusted* mean age (95% CI) of diagnosis of coronary heart disease among US adults for overall and by sex: trends from 2008 to 2017.
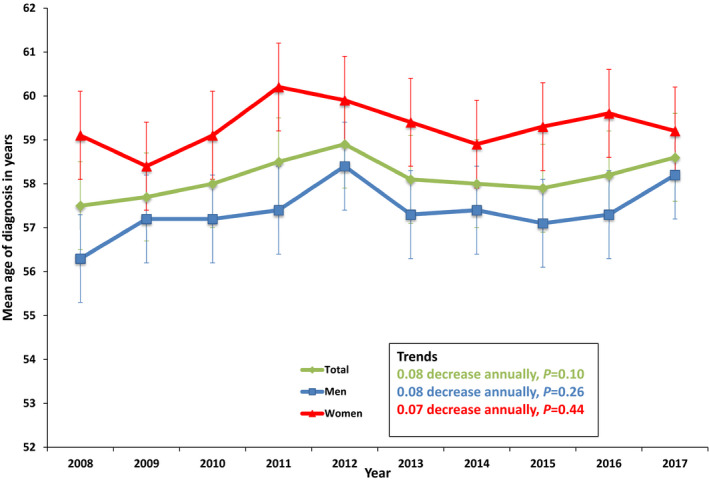
*Adjusted for current age group, race/ethnicity, level of income, type of health insurance, and Charlson comorbidity index.
Figure 3. Adjusted* mean age (95% CI) of diagnosis of stroke among US adults for overall and by sex: trends from 2008 to 2017.
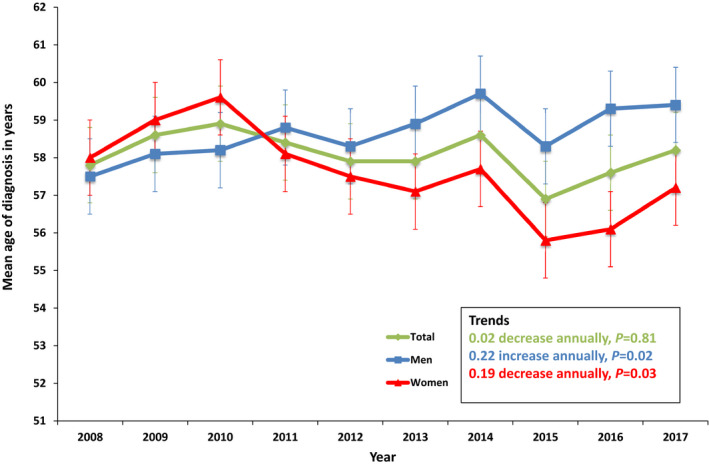
*Adjusted for current age group, race/ethnicity, level of income, type of health insurance, and Charlson comorbidity index.
Figure 4. Adjusted* mean age (95% CI) of diagnosis of hypercholesterolemia among US adults for overall and by sex: trends from 2008 to 2017.
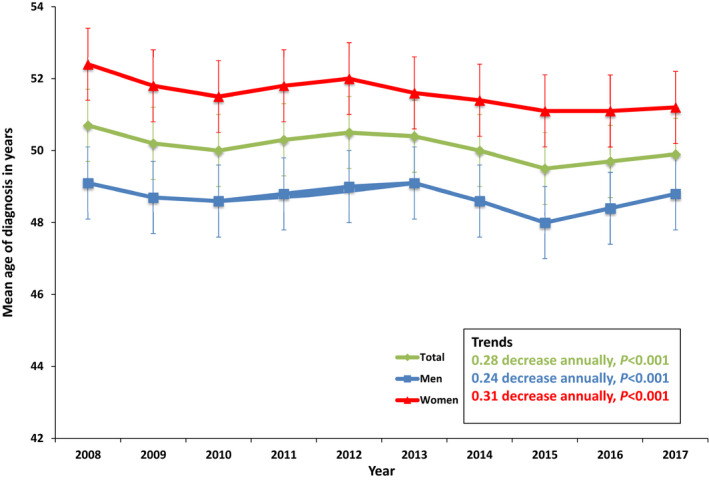
*Adjusted for current age group, race/ethnicity, level of income, type of health insurance, and Charlson comorbidity index.
Figure 5. Adjusted* mean age (95% CI) of diagnosis of hypertension among US adults for overall and by sex: trends from 2008 to 2017.
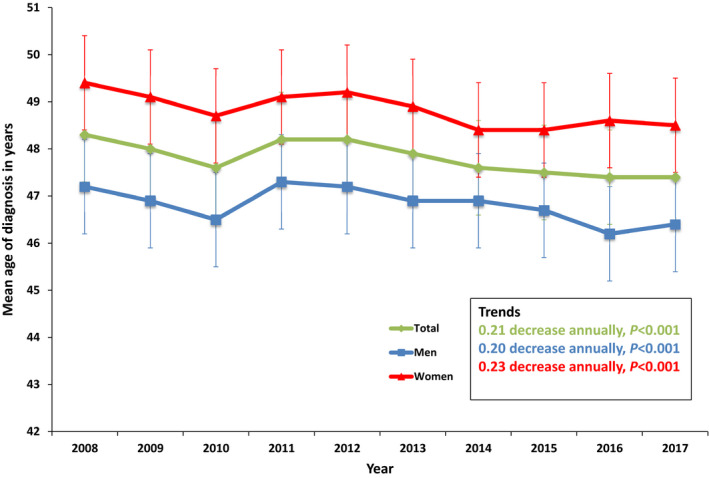
*Adjusted for current age group, race/ethnicity, level of income, type of health insurance, and Charlson comorbidity index.
Figure 6. Adjusted* mean age (95% CI) of diagnosis of coronary artery disease+stroke combined among US adults for overall and by sex: trends from 2008 to 2017.
*Adjusted for current age group, race/ethnicity, level of income, type of health insurance, and Charlson comorbidity index.
A subanalysis showing the sex‐specific trends in the mean age at diagnosis of CVD and its risk factors from 2008 to 2017, stratified by various sociodemographic factors, is shown in Tables S1 through S19: Tables S1 through S4 are stratified by race/ethnicity, Tables S5 through S7 are stratified by age groups, Tables S8 through S11 are stratified by income, Tables S12 through S15 are stratified by insurance, and Tables S16 through S19 are stratified by region.
Among non‐Hispanic White individuals, the mean age at diagnosis of hypercholesterolemia decreased from 51.7 years in 2008 to 50.5 years in 2017 (P=0.004) overall, and from 53.5 years in 2008 to 51.7 years in 2017 for women (P=0.001) (Table S1). There was no statistically significant change in the age at diagnosis for hypercholesterolemia among non‐Hispanic White men (Table S1). Among Black, Asian, and Hispanic individuals, there was no statistically significant change in the age of diagnosis of CVD and its risk factors over the study period (Table S2 through S4). Among young women (age 18–39 years) with hypertension, the mean age at diagnosis decreased from 28.5 years in 2008 to 26.9 years in 2017 (P=0.007) (Table S5).
Among high‐income‐earning men, the age of diagnosis for CHD increased from 55.2 years in 2008 to 58.6 years in 2017 (P=0.03), but not so for women within the same income class (Table S8). Among individuals with middle income, for women, the age at diagnosis of CHD decreased from 61.8 years in 2008 to 58.0 years in 2017 (P=0.01) (Table S9). There was no statistically significant change in the age at diagnosis for CHD among men with middle income (Table S9). Among women with very low income, the age at diagnosis for stroke decreased from 56.9 years in 2008 to 54.7 years in 2017 (P=0.005) (Table S11). There was an increase in the age at diagnosis for stroke among men with very low income, but this was not statistically significant (Table S11).
Among individuals with private insurance, the age of diagnosis of hypercholesterolemia has become younger for both men and women, and age of diagnosis of hypertension younger for women (Table S12). Among uninsured individuals, the age of diagnosis of stroke has become older for women and the age of diagnosis of hypercholesterolemia younger for women (Table S13). For Medicaid insurance, the age of hypertension diagnosis in women has become older (Table S14). For Medicare insurance, the age of diagnosis for stroke was older in men, the age of diagnosis of hypertension younger in men, and the age of diagnosis of hypercholesterolemia was younger in both women and men (Table S15).
Among men living in the Northeast region of the country, there was an average yearly increase in the age of diagnosis for stroke by 0.86 years (P=0.005), a trend that was not noted among women (Table S16). Among women living in the South, there was an average yearly decrease in the age of diagnosis for stroke by 0.39 years (P=0.04), but not so for men (Table S18).
Discussion
In a nationally representative sample of the US adult population from 2008 to 2017, women are first diagnosed with CHD, hypertension, and hypercholesterolemia at a slightly older age compared with men. For stroke, women are diagnosed at a younger age when compared with men. When examining 10‐year trends, there was a trend toward diagnosis at a younger age for these conditions, and this appeared to be more pronounced among women. The mean age at diagnosis for stroke decreased over the 10‐year period for women but not so for men.
The burden of established CVD risk factors at 50 years of age is thought to be a predictor for lifetime risk of developing CVD. 22 Even the presence of a single major CVD risk factor before the age of 50 is associated with an increased lifetime risk of CVD and a decrease in median survival. 23 Other recent data from MEPS have shown that the prevalence of poor cardiovascular health status has been increasing in the US population over the past decade, and this adverse trend was noted across age groups. 17 A longer period of exposure to CVD risk factors may accelerate the development of CVD in younger individuals. 24 This is alarming when put in context with the findings from this study showing a trend toward younger age at diagnosis for hypertension and hypercholesterolemia, which were also found to be more pronounced among women. Recent studies also suggests that women exhibit steeper increases in blood pressure compared with men, as early as in their 30s, and this persists throughout their lifetime. 25
On one hand, this trend toward a younger age at diagnosis of CVD and its risk factors might be favorable, suggesting improved preventive screening and detection efforts. Given that there has been an increase in awareness of CVD and its risk factors among women over the past decades, 26 one could argue that this has made women more proactive regarding their health care. Earlier detection of CVD risk factors provides an opportunity to initiate CVD prevention strategies as early as possible. 22 On the other hand, the progressive younger ages at time of diagnosis of CVD risk factors may indicate that the US population is getting unhealthier over time, which is supported by other national data. 2 , 17 , 27
With the evidence‐based recommendations for CVD prevention among women, 12 findings from the current study could help galvanize our approach to targeted age‐group and sex‐specific risk factor modification for the prevention of CVD. 11 However, it is important to note that irrespective of sex, a more aggressive approach needs to be adopted regarding promotion of cardiovascular health, CVD prevention, and risk factor modification for all adults, as described in the 2019 American College of Cardiology/American Heart Association Guideline for the Primary Prevention of CVD. 22
In addition to younger age at diagnosis for CVD risk factors, our study also showed a trend toward younger age at diagnosis of clinical CVD, particularly for stroke. Mortality from CVD has been stagnant within the past decade and might have actually increased among middle‐aged adults 55 to 64 years. 2 , 5 , 28 Some of the prior progress made in reducing mortality from heart disease was attributed to advances in care, early use of an invasive approach for CHD to improve survival, and better control of CVD risk factors. 28 However, over the past decade, optimal control of hypertension has plateaued (or worsened), 27 coincident with the prevalence of CHD and stroke, which interestingly appears to be on the rise among middle‐aged adults. 28 , 29
CVD commonly presents at an older age among women compared with men. 2 However, the prevalence of CVD is on the rise among middle‐aged women. 4 , 5 , 30 Even though it is thought that the vasodilatory and antioxidant properties of endogenous estrogen provide some protection from CVD in younger premenopausal women, this may not be the case in the setting of other CVD risk factors. 11 The trends toward younger age at diagnosis of CVD in women as shown in this current study, with the increase in mortality within this population, requires further attention. 30 The results from this study also suggest that the mean age at diagnosis for stroke among women is younger and down‐trending compared with men, a finding that is worrisome. It is unclear from our study whether a younger age of diagnosis of clinical CVD was from better detection of these disorders that might have been missed in the younger population in years past or attributed to other non‐CVD causes, or whether there has been a true increase in the prevalence of these medical conditions among younger population.
The national Million Hearts 2022 program was created to address these alarming trends toward a younger CVD population and reduce preventable cardiovascular events. 29 This is a framework that was revised in 2017 and co‐led by the Centers for Disease Control and Prevention and the Centers for Medicare and Medicaid Services with the goal of preventing 1 million heart attacks and strokes in the United States over 5 years, by implementing proven, effective, and high‐impact strategies to improve CVD risk factors, particularly among the younger population. 29 The Million Hearts strategy adopts a concerted effort led by clinicians that involves the identification of at‐risk individuals and the implementation of cardiovascular preventive efforts by various federal and private partner organizations to ensure that these vulnerable individuals get the cardiovascular preventive services they need.
Strengths and Limitations of the Study
Our findings should be considered in the context of several limitations. First, conclusions from this study can be applicable only to the population from which the sample was drawn, and this does not include the military, incarcerated individuals, or any institutionalized individuals. Second, given that the age at diagnosis for CVD and its risk factors were self‐reported (24% of the diagnosis of hypertension and 34% of the diagnosis of hypercholesterolemia did not have ICD confirmation), we cannot exclude the possibility of recall bias. Third, differences in healthcare‐seeking behavior may contribute to some of the sex‐specific differences observed in the age at diagnosis of CVD and its risk factors, which we could not account for in this study. Fourth, although we adjusted for the severity of an individual's other medical conditions, using a combination of their comorbidities as a metric, there remains a chance for residual confounding, given the lack of detailed clinical information on each participant in the MEPS data set. Fifth, since report on the age at diagnosis for the components of CHD; subtypes of stroke; and other CVD risk factors such as diabetes mellitus, obesity, and smoking is not available in the MEPS data set, that information is lacking in our study. Sixth, about 40% of the participants included in this study lived in the South region, which is known to have a high incidence of CVD, especially stroke, and although our findings reflect the US population in aggregate, this may have an impact on the generalizability of results to specific US regions. However, our findings remain essentially the same on further stratification by region. Seventh, given that this was a large‐sized population‐based study, small differences may meet a level of statistical significance, but its clinical significance may be difficult to evaluate. In lieu of this, we therefore placed more emphasis on results with larger effect estimates. Finally, the trends in the age at diagnosis of CVD and its risk factors could have been affected by changes in temporal patterns over the years such as the mean age of men and women recruited for the survey yearly. Although the impact of these changes would be random on both men and women, some may be nonrandom.
Despite these limitations, our study has a number of strengths, including the overlapping survey design of MEPS to be able to track national trends over a time period and the application of survey weights to make the results representative of the status of the civilian adult US population.
Conclusions
In a nationally representative sample of the US adult population from 2008 to 2017, there is a decreasing trend in the age at diagnosis for CVD and its risk factors, which appears to be more pronounced among women. These findings may reflect improved screening and detection of CVD and its risk factors at younger ages; or more worrisome, it could mean the US population is getting unhealthier over time. While earlier identification of CVD risk factors may provide an opportunity to initiate preventive treatments, younger age at diagnosis of CVD highlights the need for the prevention of CVD at the earliest opportunity, and sex‐specific interventions may be needed.
Sources of Funding
Dr Michos is supported by the Amato Fund for Women's Cardiovascular Health Research at Johns Hopkins University. Dr Virani is supported by the Department of Veterans Affairs, World Heart Federation, Tahir and Jooma Family Honorarium: American College of Cardiology (Associate Editor for Innovations, acc.org). He is a member of the Steering Committee: PALM (Patient and Provider Assessment of Lipid Management) registry at the Duke Clinical Research Institute (no financial remuneration). Dr Volgman's research is supported by National Institutes of Health studies, Apple Inc stock ownership, and Novartis. Dr Leucker's research is supported by an American Heart Association Career Development Grant, National Institutes of Health studies, and Amgen.
Disclosures
Dr Leucker has received grant funding from Amgen. Dr Volgman has Apple Inc stock ownership and funding from Novartis. The remaining authors have no disclosures to report.
Supporting information
Data S1
Tables S1–S19
(J Am Heart Assoc. 2020;9:e018764. DOI: 10.1161/JAHA.120.018764.)
Supplementary Material for this article is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.120.018764
This work was presented as an abstract at the American Heart Association's Scientific Sessions, November 13 to 17, 2020.
For Sources of Funding and Disclosures, see page 10.
References
- 1. Mensah GA, Brown DW. An overview of cardiovascular disease burden in the United States. Health Aff (Millwood). 2007;26:38–48. [DOI] [PubMed] [Google Scholar]
- 2. Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, et al. Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation. 2020;141:e139–e596. [DOI] [PubMed] [Google Scholar]
- 3. Khan SU, Bashir ZS, Khan MZ, Khan MS, Gulati M, Blankstein R, Blumenthal RS, Michos ED. Trends in cardiovascular deaths among young adults in the United States, 1999 to 2018. Am J Cardiol. 2020;128:216–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Arora S, Stouffer GA, Kucharska‐Newton AM, Qamar A, Vaduganathan M, Pandey A, Porterfield D, Blankstein R, Rosamond WD, Bhatt DL, et al. Twenty year trends and sex differences in young adults hospitalized with acute myocardial infarction. Circulation. 2019;139:1047–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Curtin SC. Trends in cancer and heart disease death rates among adults aged 45–64: United States, 1999–2017. Natl Vital Stat Rep. 2019;68:1–8. [PubMed] [Google Scholar]
- 6. Gupta A, Wang Y, Spertus JA, Geda M, Lorenze N, Nkonde‐Price C, D'Onofrio G, Lichtman JH, Krumholz HM. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol. 2014;64:337–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Li C, Baek J, Sanchez BN, Morgenstern LB, Lisabeth LD. Temporal trends in age at ischemic stroke onset by ethnicity. Ann Epidemiol. 2018;28:686–690.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Michos ED, Choi AD. Coronary artery disease in young adults: a hard lesson but a good teacher. J Am Coll Cardiol. 2019;74:1879–1882. [DOI] [PubMed] [Google Scholar]
- 9. Peters SAE, Muntner P, Woodward M. Sex differences in the prevalence of, and trends in, cardiovascular risk factors, treatment, and control in the United States, 2001 to 2016. Circulation. 2019;139:1025–1035. [DOI] [PubMed] [Google Scholar]
- 10. Martin SS, Michos ED. Mapping hyperlipidemia in young adulthood to coronary risk: importance of cumulative exposure and how to stay young. Circulation. 2015;131:445–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Elder P, Sharma G, Gulati M, Michos ED. Identification of female‐specific risk enhancers throughout the lifespan of women to improve cardiovascular disease prevention. Am J Prev Cardiol. 2020;2:100028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cho L, Davis M, Elgendy I, Epps K, Lindley KJ, Mehta PK, Michos ED, Minissian M, Pepine C, Vaccarino V, et al. Summary of updated recommendations for primary prevention of cardiovascular disease in women: JACC State‐of‐the‐Art Review. J Am Coll Cardiol. 2020;75:2602–2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Agency for Healthcare Research and Quality . MEPS‐HC panel design and data collection process. https://meps.ahrq.gov/mepsweb/survey_comp/hc_data_collection.jsp. Accessed July 25, 2019.
- 14. Okunrintemi V, Valero‐Elizondo J, Patrick B, Salami J, Tibuakuu M, Ahmad S, Ogunmoroti O, Mahajan S, Khan SU, Gulati M, et al. Gender differences in patient‐reported outcomes among adults with atherosclerotic cardiovascular disease. J Am Heart Assoc. 2018;7:e010498. DOI: 10.1161/JAHA.118.010498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Okunrintemi V, Spatz ES, Di Capua P, Salami JA, Valero‐Elizondo J, Warraich H, Virani SS, Blaha MJ, Blankstein R, Butt AA, et al. Patient‐provider communication and health outcomes among individuals with atherosclerotic cardiovascular disease in the United States: Medical Expenditure Panel Survey 2010 to 2013. Circ Cardiovasc Qual Outcomes. 2017;10:e003635. [DOI] [PubMed] [Google Scholar]
- 16. Cohen JW, Monheit AC, Beauregard KM, Cohen SB, Lefkowitz DC, Potter DE, Sommers JP, Taylor AK, Arnett RH III. The Medical Expenditure Panel Survey: a national health information resource. Inquiry. 1996;33:373–389. [PubMed] [Google Scholar]
- 17. Tibuakuu M, Okunrintemi V, Savji N, Stone NJ, Virani SS, Blankstein R, Thamman R, Blumenthal RS, Michos ED. Nondietary cardiovascular health metrics with patient experience and loss of productivity among US adults without cardiovascular disease: the Medical Expenditure Panel Survey 2006 to 2015. J Am Heart Assoc. 2020;9:e016744. DOI: 10.1161/JAHA.120.016744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. "Medical Expenditure Panel Survey". http://meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp. Accessed July 20, 2019.
- 19. "IRB Exemption". http://www.hhs.gov/ohrp/regulations‐and‐policy/decision‐trees/‐c2. Accessed July 20, 2019.
- 20. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 21. de Groot V, Beckerman H, Lankhorst GJ, Bouter LM. How to measure comorbidity. a critical review of available methods. J Clin Epidemiol. 2003;56:221–229. [DOI] [PubMed] [Google Scholar]
- 22. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd‐Jones D, McEvoy JW, et al. 2019 ACC/AHA Guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:e596–e646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lloyd‐Jones DM, Leip EP, Larson MG, D'Agostino RB, Beiser A, Wilson PW, Wolf PA, Levy D. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–798. [DOI] [PubMed] [Google Scholar]
- 24. Pletcher MJ, Bibbins‐Domingo K, Liu K, Sidney S, Lin F, Vittinghoff E, Hulley SB. Nonoptimal lipids commonly present in young adults and coronary calcium later in life: the CARDIA (Coronary Artery Risk Development in Young Adults) study. Ann Intern Med. 2010;153:137–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ji H, Kim A, Ebinger JE, Niiranen TJ, Claggett BL, Bairey Merz CN, Cheng S. Sex differences in blood pressure trajectories over the life course. JAMA Cardiol. 2020;15:19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mosca L, Mochari‐Greenberger H, Dolor RJ, Newby LK, Robb KJ. Twelve‐year follow‐up of American women’s awareness of cardiovascular disease risk and barriers to heart health. Circ Cardiovasc Qual Outcomes. 2010;3:120–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Muntner P, Hardy ST, Fine LJ, Jaeger BC, Wozniak G, Levitan EB, Colantonio LD. Trends in blood pressure control among US adults with hypertension, 1999–2000 to 2017–2018. JAMA. 2020;324:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ritchey MD, Wall HK, George MG, Wright JS. US trends in premature heart disease mortality over the past 50 years: where do we go from here? Trends Cardiovasc Med. 2020;30:364–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wright JS, Wall HK, Ritchey MD. Million Hearts 2022: small steps are needed for cardiovascular disease prevention. JAMA. 2018;320:1857–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bybee KA, Stevens TL. Matters of the heart: cardiovascular disease in U.S. women. Mo Med. 2013;110:65–70. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1
Tables S1–S19


