Abstract
Background
The incidence of cardiovascular disease among pregnant women is rising in the United States. Data on racial disparities for the major cardiovascular events during pregnancy are limited.
Methods and Results
Pregnant and post‐partum women hospitalized from January 2007 to December 2017 were identified from the Nationwide Inpatient Sample. The outcomes of interest included: in‐hospital mortality, myocardial infarction, stroke, pulmonary embolism, and peripartum cardiomyopathy. Multivariate regression analysis was used to assess the independent association between race and in‐hospital outcomes. Among 46 700 637 pregnancy‐related hospitalizations, 21 663 575 (46.4%) were White, 6 302 089 (13.5%) were Black, and 8 914 065 (19.1%) were Hispanic. The trends of mortality and stroke declined significantly in Black women, but however, were mostly unchanged among White women. The incidence of mortality and cardiovascular morbidity was highest among Black women followed by White women, then Hispanic women. The majority of Blacks (62.3%) were insured by Medicaid while the majority of White patients had private insurance (61.9%). Most of Black women were below‐median income (71.2%) while over half of the White patients were above the median income (52.7%). Compared with White women, Black women had the highest mortality with adjusted odds ratio (aOR) of 1.45, 95% CI (1.21–1.73); myocardial infarction with aOR of 1.23, 95% CI (1.06–1.42); stroke with aOR of 1.57, 95% CI (1.41–1.74); pulmonary embolism with aOR of 1.42, 95% CI (1.30–1.56); and peripartum cardiomyopathy with aOR of 1.71, 95 % CI (1.66–1.76).
Conclusions
Significant racial disparities exist in major cardiovascular events among pregnant and post‐partum women. Further efforts are needed to minimize these differences.
Keywords: cardiovascular mortality, disparities in care, health inequities, pregnancy
Subject Categories: Quality and Outcomes, Pregnancy, Race and Ethnicity
Nonstandard Abbreviation and Acronyms
- NIS
Nationwide Inpatient Sample
Clinical Perspective
What Is New?
There are known disparities in maternal morbidity and mortality outcomes in the United States, however, the maternal cardiovascular outcomes have limited data evaluating racial disparities.
Pregnant and postpartum women in the United States of Black origin, as well as other minority groups, have worse cardiovascular outcomes compared with women of White origin even when adjusting for socioeconomic factors and medical comorbidities.
What Are the Clinical Implications?
Compared with White women, Black women had a higher risk of mortality, myocardial infarction, stroke, pulmonary embolism, and peripartum cardiomyopathy with odds ratio of 1.45, 1.23, 1.57, 1.42, and 1.71, respectively.
The United States is witnessing an increasing maternal mortality rate that increased from as low as 9.8 per 100 000 live births at the start of the cenury to 26.4 in 2015 then declined to 17.4 in 2018. 1 , 2 , 3 The Global Burden of Disease study estimates that in 2015, the United States had a maternal mortality rate of 26.4 per 100 000 live births which is significantly higher compared with other high sociodemographic index countries, with a mortality rate of 15.0 per 100 000 live births, close to 4‐fold the rate in Canada or Western Europe; 7.3, and 7.2 per 100 000 live births, respectively. Furthermore, it is higher than East Asia and comparable with central Asia with rates of 18.8 and 28.4 per 100 000 live births, respectively. 4 Moreover, US maternal mortality has shown a startling rise with an annual percent change of +1.8 compared with an observed decline globally, in high‐sociodemographic index countries, and low‐ sociodemographic index counties; –1.5, –2.1, and –1.0, respectively. Thus, a better understanding of the underlying etiologies causing this rise is warranted to halt and potentially begin to reverse the inclining trends. 4
Multiple studies attempted to understand the perplexing numbers reported in the United States with studies showing that maternal mortality and morbidities with geographic and economic factors playing a significant role. Studies showed differences from one state to another, with California reporting a decline while the rates in Texas doubled, between different socioeconomic groups, with Black women having considerably higher rates compared with White pregnant women, and based on the level of access to medical care with studies showing that uninsured and rural populations suffer from worse outcomes. 5 , 6 , 7 , 8 A possible cause may be related to data capturing and collection as some states collect information related to pregnancy, childbirth, and the puerperium in vital statistics related to mortality while other states have not implemented routine collection of pregnancy‐related information. 9
Cardiovascular morbidity and mortality in pregnant women are a matter of concern with heart disease, stroke, and pregnancy‐related complications ranking amongst the top 10 leading causes of death in women aged 20 to 44 years. 10 The US Department of Health and Human Services set a goal of eliminating health disparities and achieving equity as a part of healthy people 2020 initiative, and understanding the disparities in cardiovascular pregnancy‐related health outcomes plays a pivotal role in alleviating the healthcare disparities and achieving equity between different groups, most importantly different racial groups. 11
A better understanding of the socioeconomic determinant, traditional cardiovascular risk factors in pregnancy, and racial factors are warranted as policymakers attempt to implement interventions to counter the stern trends noted. 12 The current study aims to explore disparities in cardiovascular disease in pregnancy and its associations with race, socioeconomic status, or medical comorbidities. The findings from this study may shed further light on actionable plans that can be targeted by policy makers as well as healthcare administrators to improve healthcare systems, equity, and access to health care, and reduce financial and social burden of pregnancy‐related cardiovascular morbidity and mortality in the United States.
Methods
Data Source and Study Population
Using the Nationwide Inpatient Sample (NIS) database between January 2007 and December 2017, we identified any pregnancy or post‐partum‒related hospitalization. The NIS is made publicly available by the Agency for Healthcare Research and Quality for the Healthcare Cost and Utilization Project. 13 The NIS represents the largest publicly available all‐payer database and contains discharge‐level administrative data on inpatient diagnoses and procedures from a stratified sample of ≈ 20% of US hospitals through 2012. Starting from 2012, the NIS represents a sample of 20% of discharges from all hospitals. The NIS provides a weight variable for establishing an estimate of national statistics in the design of a complex survey sample using a stratum variable and a clustering variable. Women who were hospitalized during pregnancy, labor, and the post‐partum period for pregnancy‐related causes were identified by using the appropriate administrative codes (Table S1). The need for an institutional review board approval was waived for this study because of the anonymized and de‐identified nature of the publicly available data.
Patient and Hospital Characteristics
Baseline characteristics included demographics (age, race, length of hospital stay, elective admission to the hospital, patient disposition, primary payer information, and percentile of home income by residential zip code as provided by Healthcare Cost and Utilization Project), and medical/pregnancy‐related comorbidities were identified with the corresponding International Classification of Diseases, Ninth Revision, Clinical Modification (ICD‐9‐CM) (until September 2015) and International Classification of Diseases, Tenth Revision, Clinical Modification (ICD‐10‐CM) codes (starting from October 2015) (Table S1). The hospital‐related characteristics included bed size, location, hospital region, and teaching status.
Outcome Measure
The primary outcome of the study was the difference in in‐hospital mortality and cardiovascular events, defined as acute myocardial infarction (AMI), stroke, pulmonary embolism (PE), and peripartum cardiomyopathy between the different racial group. Cardiovascular events were chosen as they could be fatal and catastrophic for the mother and the family and play a major role in maternal mortality rates. The null hypothesis of the current study was that no difference in mortality and cardiovascular morbidity existed between pregnant women of different ethnicities in the United States. The secondary pre‐specified outcomes included the temporal trends of in‐hospital mortality and cardiovascular morbidity by race, and adjusted odds ratio of adverse events by race. Further subgroup analyses were performed based on patient baseline comorbidities and socioeconomic status.
Statistical Analysis
The patient baseline characteristics and demographics, as well as outcomes, were compared between different races/ethnicities. Categorical variables were compared with the Mantel Haenszel Chi‐square test, and continuous variables were compared with ANOVA testing. The linear Chi‐square test was used to evaluate current temporal trends of outcomes and risk factors. The rates were expressed as a percentage, or per 100 000 pregnancy‐related hospitalizations, as appropriate. We used bivariate and multivariate regression models to estimate odds of outcomes by race, and adjusted for insurance information and socioeconomic status. All statistical analyses were performed by using the weighted values, hospital clusters, and strata of observations as provided by the NIS to measure national estimates. Statistical analyses were conducted using RStudio software (RStudio, Boston, Massachusetts). P values were corrected using Bonferroni correction to avoid multiple comparisons causing type I error. A 2‐sided value of P<0.05 was set for statistical significance. Odds ratios and the 95% CIs were used.
Results
Population Demographics
Among 46 700 637 hospitalizations of pregnant or post‐partum women, 46.4% were White, 13.5% were Black, 19.1% were Hispanic, 4.8% were Asian/Pacific Islander, 0.7% were Native American, 4.3% other races/multiple races, and 11.2% unknown race (results not shown). Black and Hispanic pregnant and post‐partum women were younger with 39.9% and 34.8%, respectively aged between 18 and 24 years compared with 25.9% of White women. Approximately 1 in 200 pregnancies in Hispanic and Black women were aged <18 years compared with 1 in 500 pregnancies in White women.
Further information on demographics for each race is shown in Table 1.
Table 1.
Baseline Demographics of Included Patients, Baseline Medical Comorbidities, and Pregnancy‐Related Comorbidities
| White (n = 21 663 575) | Black (n = 6 302 089) | Hispanic (n = 8 914 065) | Asian/Pacific Islander (n = 2 251 824) | P Value | |
|---|---|---|---|---|---|
| 46.4% | 13.5% | 19.1% | 4.8% | ||
| Age group, (%) | <0.001 | ||||
| Under 18 y | 0.2% | 0.5% | 0.5% | 0.1% | |
| 18–24 y | 25.9% | 39.9% | 34.8% | 11.1% | |
| 25–29 y | 29.6% | 27.4% | 28.0% | 26.3% | |
| 30–34 y | 27.9% | 19.4% | 22.1% | 36.3% | |
| 35–39 y | 13.2% | 10.0% | 11.6% | 21.1% | |
| 40–44 y | 2.8% | 2.5% | 2.8% | 4.7% | |
| ≥45 y | 0.3% | 0.3% | 0.2% | 0.4% | |
| Income | <0.001 | ||||
| 0–25th percentile | 21.4% | 48.6% | 36.8% | 12.5% | |
| 26th–50th percentile | 25.9% | 22.6% | 25.5% | 16.2% | |
| 51st–75th percentile | 26.6% | 17.6% | 23.1% | 25.0% | |
| 76th–100th percentile | 26.1% | 11.3% | 14.6% | 46.3% | |
| Primary payer | <0.001 | ||||
| Medicare | 0.9% | 1.7% | 0.5% | 0.3% | |
| Medicaid | 31.9% | 62.3% | 63.6% | 26.9% | |
| Private insurance | 61.9% | 30.7% | 28.3% | 65.3% | |
| Self‐pay | 1.9% | 2.9% | 5.4% | 5.5% | |
| No charge | 0.1% | 0.2% | 0.4% | 0.1% | |
| Other | 3.4% | 2.2% | 1.8% | 2.0% | |
| Comorbidities | |||||
| Known cardiovascular risk factors | 0.8% | 1.2% | 0.5% | 0.6% | <0.001 |
| Hypertension | 2.3% | 5.8% | 2.1% | 1.8% | <0.001 |
| Heart failure | 0.1% | 0.4% | 0.1% | 0.1% | <0.001 |
| Cardiomyopathy | 0.1% | 0.2% | 0.0% | 0.0% | <0.001 |
| Congenital heart disease | 0.1% | 0.1% | 0.1% | 0.1% | <0.001 |
| Atrial fibrillation | 0.0% | 0.1% | 0.0% | 0.0% | <0.001 |
| Valvular disease | 0.3% | 0.3% | 0.1% | 0.2% | <0.001 |
| Dyslipidemia | 0.2% | 0.2% | 0.2% | 0.3% | <0.001 |
| Diabetes mellitus | 1.0% | 2.0% | 1.5% | 1.0% | <0.001 |
| Obstructive sleep apnea | 0.1% | 0.2% | 0.0% | 0.0% | <0.001 |
| Obesity | 8.8% | 14.6% | 10.2% | 4.5% | <0.001 |
| Smoking | 4.9% | 4.0% | 1.7% | 1.8% | <0.001 |
| Alcohol abuse | 0.1% | 0.2% | 0.1% | 0.0% | <0.001 |
| Drug abuse | 3.2% | 3.6% | 1.3% | 0.4% | <0.001 |
| Peripheral vascular disorders | 0.0% | 0.0% | 0.0% | 0.0% | <0.001 |
| Rheumatoid arthritis/collagen vascular diseases | 0.4% | 0.4% | 0.3% | 0.3% | <0.001 |
| Deficiencies anemia | 6.9% | 13.3% | 9.4% | 8.3% | <0.001 |
| Chronic blood loss anemia | 11.6% | 21.5% | 15.2% | 13.6% | <0.001 |
| Chronic pulmonary disease | 5.0% | 7.9% | 3.7% | 2.7% | <0.001 |
| Pregnancy‐related complications | |||||
| Gestational hypertension | 4.3% | 4.3% | 2.8% | 2.2% | <0.001 |
| Preeclampsia | 3.7% | 5.1% | 3.8% | 2.6% | <0.001 |
| Eclampsia | 0.1% | 0.2% | 0.1% | 0.1% | <0.001 |
| Gestational diabetes mellitus | 2.3% | 3.3% | 3.3% | 4.3% | <0.001 |
| Hospitalization during delivery and puerperium | 90.1% | 84.3% | 88.7% | 93.6% | <0.001 |
| C‐section | 30.2% | 30.7% | 29.9% | 30.9% | <0.001 |
Black women had higher prevalence of cardiovascular risk factors including hypertension, heart failure, cardiomyopathy, atrial fibrillation, diabetes mellitus, and obesity compared with White women while Hispanic women tended to have lower prevalence. Further information on baseline comorbidities for each race is shown in Table 1. Table S2 provides further information about hospital and demographics characteristics.
Hospital Complications and Cardiovascular Events
Black women had a higher risk of bleeding, cardiac tamponade, cardiac arrest, acute kidney injury, and sepsis compared with other races/ethnicities.
Further information on complications for each race is shown in Table 2.
Table 2.
Patients’ Complications and Cardiovascular Outcomes
| White (n = 21 663 575) | Black (n = 6 302 089) | Hispanic (n = 8 914 065) | Asian/Pacific Islander (n = 2 251 824) | P Value | |
|---|---|---|---|---|---|
| 46.4% | 13.5% | 19.1% | 4.8% | ||
| Complications | |||||
| Bleeding | 0.7% | 1.0% | 1.0% | 0.9% | <0.001 |
| Cardiac arrest | 0.0% | 0.0% | 0.0% | 0.0% | <0.001 |
| Acute kidney injury | 0.1% | 0.2% | 0.1% | 0.1% | <0.001 |
| Sepsis | 0.2% | 0.2% | 0.2% | 0.2% | <0.001 |
| Outcomes | |||||
| In‐hospital mortality | 0.01% | 0.03% | 0.01% | 0.01% | <0.001 |
| Acute myocardial infarction | 0.01% | 0.02% | 0.01% | 0.01% | 0.015 |
| Stroke | 0.04% | 0.07% | 0.04% | 0.03% | <0.001 |
| Pulmonary embolism | 0.02% | 0.04% | 0.01% | 0.01% | <0.001 |
| Peripartum cardiomyopathy | 0.1% | 0.3% | 0.1% | 0.1% | <0.001 |
Compared with White women, Black women had the highest in‐hospital mortality with adjusted odds ratio (aOR) of 1.45, 95% CI (1.21–1.73); AMI with aOR of 1.23, 95% CI (1.06–1.42); stroke with aOR of 1.57, 95% CI (1.41–1.74); PE with aOR of 1.42, 95% CI (1.30–1.56); and peripartum cardiomyopathy with aOR 1.71, 95% CI (1.66–1.76) when adjusted for socioeconomic status, access to health care, and medical comorbidities. Hispanic women had aOR of mortality 1.23, 95% CI (1.02–1.49); AMI with aOR of 1, 95% CI (0.84–1.19); stroke with aOR of 1.23, 95% CI (1.10–1.38); PE with aOR of 0.66, 95% CI (0.58–0.74); and peripartum cardiomyopathy with aOR of 0.69, 95% CI (0.67–0.72). Pacific Islander/Asian women had aOR of mortality 2.00, 95% CI (1.53–2.61); AMI with aOR of 0.77, 95% CI (0.56–1.07); stroke with aOR of 1.08, 95% CI (0.90–1.31); PE with aOR of 0.34, 95% CI (0.25–0.45); and peripartum cardiomyopathy with aOR of 1.11, 95% CI (1.08–1.15) (Table 3).
Table 3.
Baseline Comorbidities*, Socioeconomic Status, and Access to Health Care Adjusted Odds Ratio of Mortality and Cardiovascular Morbidity
| In‐hospital mortality | Acute Myocardial Infarction | Stroke | Pulmonary Embolism | Peripartum Cardiomyopathy | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Race/ethnicity | ||||||||||
| White women | Reference | Reference | Reference | Reference | Reference | |||||
| Black women | 1.45 | <0.001 | 1.23 | 0.006 | 1.57 | <0.001 | 1.42 | <0.001 | 1.71 | <0.001 |
| (1.21–1.73) | (1.06–1.42) | (1.41–1.74) | (1.30–1.56) | (1.66–1.76) | ||||||
| Hispanic women | 1.23 | 0.031 | 1 | 0.979 | 1.23 | <0.001 | 0.66 | <0.001 | 0.69 | <0.001 |
| (1.02–1.49) | (0.84–1.19) | (1.10–1.38) | (0.58–0.74) | (0.67–0.72) | ||||||
| Pacific Islander or Asian women | 2 | <0.001 | 0.77 | 0.119 | 1.08 | 0.401 | 0.34 | <0.001 | 1.11 | <0.001 |
| (1.53–2.61) | (0.56–1.07) | (0.90–1.31) | (0.25–0.45) | (1.08–1.15) | ||||||
Adjusted for comorbidities; including age, diabetes mellitus, cardiomyopathy, obesity, hyperlipidemia, heart failure, hypertension, smoking, pre‐eclampsia/eclampsia, gestational hypertension, gestational diabetes mellitus, and cesarean section, socioeconomic status (income levels), and access to health care (healthcare insurance). OR indicates odds ratio.
Temporal Trends
Over the study duration, the incidence of in‐hospital mortality in Black women decreased (from 38.1 in 2007 to 21.9 in 2017 per 100 000 hospitalizations) as well as the rates of stroke (from 85.5 in 2007 to 54.2 in 2017 per 100 000 hospitalizations). But the rates of AMI (from 24.2 in 2007 to 36.4 in 2017 per 100 000 hospitalizations), PE (from 29.3 in 2007 to 60.7 in 2017 per 100 000 hospitalizations), and peripartum cardiomyopathy increased (from 236.4 in 2007 to 296.2 in 2017 per 100 000 hospitalizations), P‐trend <0.001 (Figure and Table S3).
Figure 1. Temporal trends of incidence of mortality and cardiovascular events in pregnant and post‐partum women by race/ethnicity.
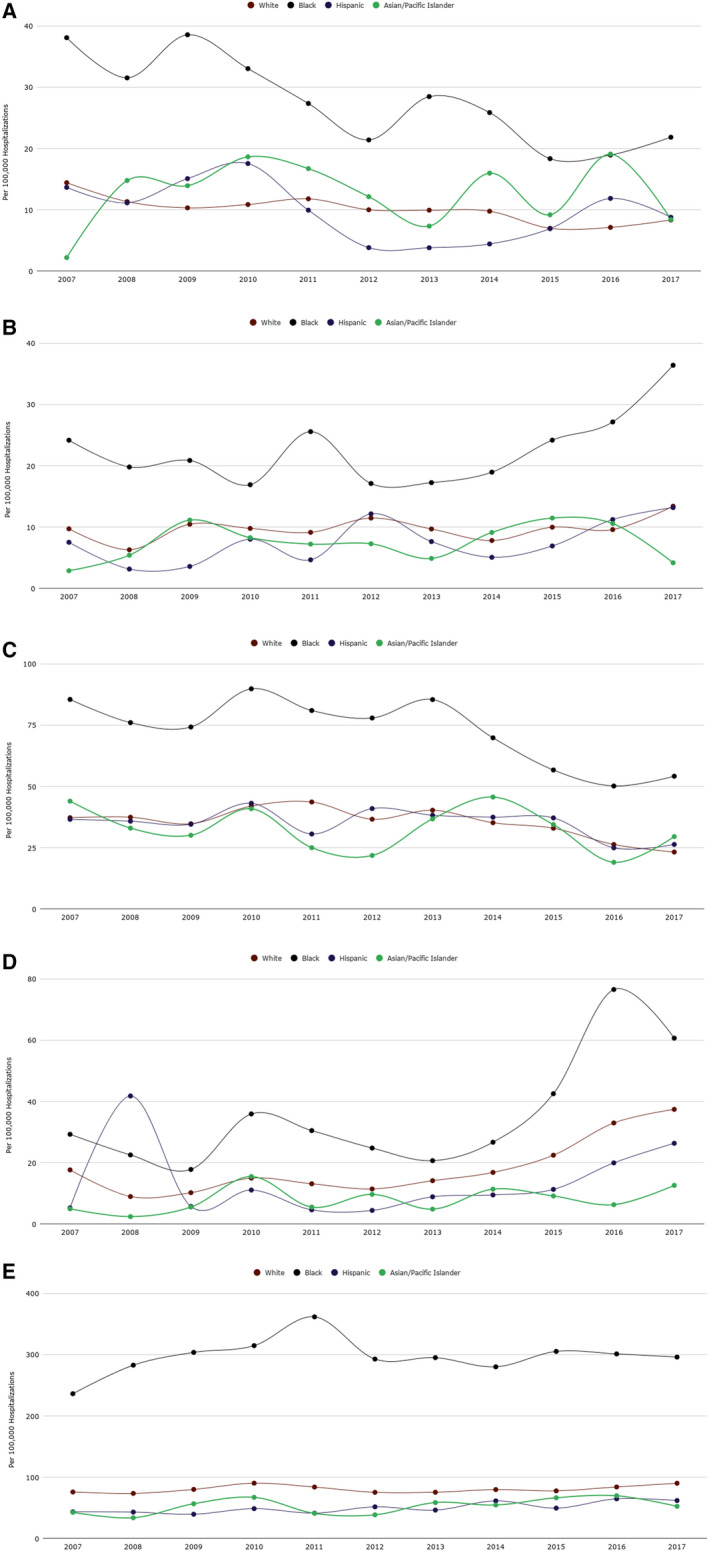
A, In‐hospital mortality, B, acute myocardial infarction, C, stroke, D, pulmonary embolism, and E, peripartum cardiomyopathy
Subgroup Analyses
Among women with diabetes mellitus, Black women had mortality, AMI, stroke, and PE rates of 129.8, 171.0, 203.7, and 120.5 per 100 000 hospitalizations compared with White women with rates of 67.6, 121.2, 131.1, and 65.3 per 100 000 hospitalizations, respectively, P value <0.001.
Among patients with history of known cardiovascular disease Black women had mortality, AMI, stroke, and PE rates of 0.7%, 1.3%, 1.5%, and 0.6% compared with White women with rates of 0.3%, 0.8%, 1.0%, and 0.3%, respectively, P value <0.001.
When comparing White women with below‐median socioeconomic status to Black women with similar socioeconomic status, Black women had higher odds of AMI, stroke, and PE outcomes with OR of 2.26 (2.08–2.46), 1.87 (1.78–1.96), and 1.74 (1.63–1.85), respectively. When Black women with highest socioeconomic quartile status were compared with White women of the lowest quartile, Black women had persistently higher odds of AMI, stroke, and PE outcomes with OR of 1.62 (1.34–1.97), 2.38 (2.18–2.6), and 1.35 (1.19–1.54), respectively. When comparing White women with no affordable access to health care, as defined by self‐paying as insurance, to Black women with private insurance, Black women persistently had worse AMI, and stroke outcomes with OR of 1.32 (1.01–1.71), 1.61 (1.38–1.87), but better PE outcome of 0.77 (0.66–0.90).
Discussion
In this nationwide analysis of pregnancy‐related hospitalizations from 2007 to 2017, we aimed to characterize the racial and socioeconomic disparities among pregnant and post‐partum women on in‐hospital mortality, and cardiovascular events. We found that racial disparities that persisted after adjusting for socioeconomic factors and access to health care. Our study showed that Black women are at a significant risk of mortality and cardiovascular events with certain cardiovascular events, AMI and PE increasing over the study duration disproportionately compared with White women. Many studies entreat socioeconomic differences as the leading contributor to racial disparities as the average Black female has a lower household income, educational attainment, and access to health care. 14 , 15 , 16 , 17 , 18 While our findings substantiate those observations, we observe persistent disparities with further adjustment for socioeconomic factors, which was observed in studies evaluating racial disparities in pregnancy and infant outcomes with documented racial differences within the same socioeconomic strata. Our study found startling worse pregnancy‐related cardiovascular events among high socioeconomic status Black women when compared with low socioeconomic status White women. These disparities appear to have been persisted since the 1990s with Singh et al. reporting that infants born to Black women of higher socioeconomic status suffered from worse outcomes compared with White women of lower socioeconomic status. 19 Thus, those findings are alarming as long‐standing disparities appear to be more complex and persistent than to be attributed to socioeconomic factors. Another attributable factor was identified as a lack of access to affordable health care resulting in delayed or inadequate medical care, 20 either prenatal or perinatal care, however; our findings indicate that Black women remained at higher risk when adjusted for insurance type, as a proxy to access to health care, and found a startling increase in myocardial infarction and stroke in Black women with private insurance; OR of 1.32 and 1.60, compared with White women without insurance. Those findings are troubling and alarming as they show persistently worse outcomes in Black women with the highest income and insurance levels when compared with White women with the lowest levels. Our findings indicate that most Black pregnant women were of below‐median income (71.2%) and insured by Medicaid (62.3%) compared with White pregnant women who were of above‐median income (52.7%) and had private insurance (61.9%). However, the percentage of uninsured Black women significantly trended down over the study period from 4.3% in 2007 to 2.3% in 2017, highlighting increased insurance access. However, those findings are not without drawbacks, as private insurance coverage for Black women declined from 33.1% to 29.9%, and Medicaid insurance trended up from 57.9% to 64.0% which sheds light at reduced and limited access to employer‐funded insurance yet highlight increasing state efforts to provide coverage as 34 states expanded Medicaid to improve eligibility criteria for pregnant women increasing the income threshold for Medicaid coverage from 134% of the federal poverty level to >200%. 21 , 22
Our results show a disparity in the prevalence of risk factors contributing to potential mortality and morbidity during pregnancy. Significant risk factors previously associated with poor pregnancy outcomes are trending up in Black women and significantly higher than White women. Prior history of cardiovascular disease was found in 1.1% of Black women compared with 0.7% in White women. Obesity in Black women went up from 4.1% in 2007 to 13.8% in 2017 and was overall 8.9% compared with 4.9% in White women. Depression and smoking in Black women increased ≈ 3‐fold and 11‐folds over the study duration as well, highlighting significant differences in risky maternal behaviors, psychologic, and medical comorbidities that are likely driving the persistent gap in outcomes. Further studies highlighted similar findings and attempted to understand the underlying causes that may cause such disparities. A number of studies highlighted the disparities in food access in Black women with more food deserts in predominantly Black neighborhoods and restricted access to healthy nutritional options worsening obesity and malnutrition. 23 , 24 Another interesting study that focused on Black women of school age found a disturbingly increased consumption of sweetened beverages and low step count, particularly in low‐income women during summertime; no school provided nutrition or mandated activities that highlight a concerning increase in obesity prevalence. 25 To understand the potential reasons why Black women may be at an increased risk of poor dietary habits, Acheampong et al. conducted a study with that question in mind and found that Black women had sufficient awareness of healthy food options; however, the most constant limitation was unaffordability of nutritious food elements. 26 Our results show increasing depression in pregnant women, and poor outcomes have been shown to be related to increased maternal psychological distress, depression, and anxiety with studies showing elevated norepinephrine and cortisol elevation in stress that may contribute to worse cardiovascular outcomes. Further studies have shown that anxiety and stress were correlated with altered immune function and increased risk of infections and overall increased morbidity and mortality. 27
Our results show that the outcomes in Black women seem to be improving over the study duration; however, the outcomes are consistently worse compared with White women. However, Hispanic pregnant women appear to have a persistent pattern of poor cardiovascular outcomes and are projected to overtake Black women as the population at the highest risk of adverse cardiovascular morbidity and mortality in the next few years. Those findings are concerning as Hispanic women are the most substantial portion of minority births in the United States with the highest birth rate and constitute the fastest‐growing minority in the United States. 28 Thus, further understanding of potential causes and possible interventions to reduce cardiovascular morbidity and mortality are warranted. Several studies looked into cardiovascular risk factors in Hispanic women and found concerning findings of increased prevalence of cardiovascular risk factors as the incidence of type 2 diabetes mellitus was increased in Hispanic women as well as Hispanic women being at a higher risk of entering pregnancy being overweight or obese, as well as gain an excessive amount of weight during pregnancy. 29 , 30 More studies investigated those findings and found significant differences in dietary habits with increased levels of processed meats, soft drinks, fatty food consumption in the Hispanic population, which reinforce the importance of dietary modifications and understanding of different nutritional ingredients. Another identified concern was food insecurity, which raises levels of anxiety and depression in addition to the established poor nutritional status. 31 Those identifiable risk factors are essential to intervene to lower cardiovascular morbidity and mortality in the fastest‐growing minority in the United States.
The burden of pregnancy on the US economy and healthcare expenditure increased by 67% over the past 2 decades from 149.56 USD per capita in 2000 to 248.83 USD per capita in 2017. 32 Thus, pregnancy‐related costs cause a significant burden on the US economy, and as the Institute of Medicine estimates that most of the pregnancy‐associated expenses are directly related to medical care, we underestimate the financial burden associated with poor neonatal health, long‐term morbidity in mothers, and loss of productivity in the workforce in a young population. Moreover, in light of an estimated burden of cardiovascular disease on women to be 1.1 trillion USD in 2035, 33 , 34 , 35 interventions directed at reducing cardiovascular events can help alleviate immense indirect costs that burden the US economy. Programs targeted at reducing racial disparities should consider cultural factors affecting certain behaviors and disease prevalence as culturally tailored interventions influence behaviors in a more favorable way preventing modifiable risk factors. Further studies are needed to provide a cost‐benefit analysis demonstrating the impact of primary and secondary preventive measures on direct and indirect financial costs associated with cardiovascular events and mortality in pregnancy.
The findings of this study should be interpreted with certain limitations. This is a retrospective, non‐randomized study with inherent limitations intrinsic to the retrospective nature of the study. Our study is derived from an administrative database relying on ICD‐9 and 1 ICD‐10 codes. It is thus subject to coding errors, in addition to that, administrative codes were designed for billing purposes and lack granularity of details in regard to the severity of the disease. In addition to that, the NIS database lacks crucial clinical and demographic information such as patient educational level, size of household, imaging data, and medications. NIS provides significant inpatient information; however, it lacks follow‐up beyond the index hospitalization, and that limits peripartum follow up as well as the lack of timing of admission after delivery. In addition to that, obtaining further information on temporal follow‐up of the same patient through multiple hospitalizations during 1 or multiple pregnancies is not possible because of the de‐identified nature of the data set. Despite these limitations, our study is derived from a national representative sample and provides a large sample size with generalizable results to the US population.
Conclusions
Significant racial disparities exist in regard to in‐hospital mortality and major cardiovascular events among pregnant and post‐partum women. AMI and PE rates are trending up significantly in all racial groups, particularly in Black women. Our current observations and estimates provide policy makers as well as healthcare administrators with needed evidence to allocate funds to social and medical programs that can help reduce health disparities and inequities in pregnant women.
Sources of Funding
None.
Disclosures
None.
Supporting information
Table S1–S3
(J Am Heart Assoc. 2021;10:e017832. DOI: 10.1161/JAHA.120.017832.)
Supplementary Materials for this article are available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.120.017832.
For Sources of Funding and Disclosures, see page 9.
This manuscript was sent to Elizabeth A. Jackson, MD, MPH, Guest Editor, for review by expert referees, editorial decision, and final disposition.
References
- 1. MacDorman MF, Declercq E, Cabral H, Morton C. Recent increases in the U.S. Maternal mortality rate: disentangling trends from measurement issues. Obstet Gynecol. 2016;128:447–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Centers for disease control and prevention . Compressed mortality file 1999–2014 on CDC wonder online data base. http://wonder.cdc.gov/mortsql.html. Accessed March 1, 2020.
- 3. CDC . National center for health statistics. 2020. https://www.cdc.gov/nchs/maternal‐mortality/index.htm
- 4. Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388:1775–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Carroll AE. Why is us maternal mortality rising? JAMA. 2017;318:321. [DOI] [PubMed] [Google Scholar]
- 6. Kozhimannil KB, Interrante JD, Henning‐Smith C, Admon LK. Rural‐urban differences in severe maternal morbidity and mortality in the US, 2007–15. Health Aff (Millwood). 2019;38:2077–2085. [DOI] [PubMed] [Google Scholar]
- 7. Kuehn B. Disparities in maternal mortality. JAMA. 2019;322:1545. [DOI] [PubMed] [Google Scholar]
- 8. McCarthy M. Maternal mortality varies sevenfold across the US, report finds. BMJ. 2016;354:i5327. [DOI] [PubMed] [Google Scholar]
- 9. National center for health statistics . Center for disease control (CDC). 2020. https://www.cdc.gov/nchs/data/nvsr/nvsr69/nvsr69_02‐508.pdf
- 10. CDC . Leading causes of death females all races/origins. [online] centers for disease control and prevention. 2020. https://www.cdc.gov/women/lcod/2017/all‐races‐origins/index.htm. Accessed March 1, 2020.
- 11. CDC . Healthy people ‐ healthy people 2020 [internet]. Centers for disease control. https://www.cdc.gov/nchs/healthy_people/hp2020.htm. Accessed March 1, 2020.
- 12. Elgendy IY, Gad MM, Mahmoud AN, Keeley EC, Pepine CJ. Acute stroke during pregnancy and puerperium. J Am Coll Cardiol. 2020;75:180–190. [DOI] [PubMed] [Google Scholar]
- 13. Nis, hcup nationwide inpatient sample. Healthcare cost and utilization project (hcup). https://www.hcup‐us.ahrq.gov/nisoverview.jsp. Accessed March 10, 2020.
- 14. Metcalf PA, Sharrett AR, Folsom AR, Duncan BB, Patsch W, Hutchinson RG, Szklo M, Davis CE, Tyroler HA. African American‐white differences in lipids, lipoproteins, and apolipoproteins, by educational attainment, among middle‐aged adults: the atherosclerosis risk in communities study. Am J Epidemiol. 1998;148:750–760. [DOI] [PubMed] [Google Scholar]
- 15. Hibbs SD, Rankin KM, DeSisto C, Collins JW Jr. The age‐related patterns of preterm birth among urban African‐American and non‐latina white mothers: the effect of paternal involvement. Soc Sci Med. 2018;211:16–20. [DOI] [PubMed] [Google Scholar]
- 16. Mazul MC, Salm Ward TC, Ngui EM. Anatomy of good prenatal care: perspectives of low income African‐American women on barriers and facilitators to prenatal care. J Racial Ethn Health Disparities. 2017;4:79–86. [DOI] [PubMed] [Google Scholar]
- 17. McDaniel A, DiPrete TA, Buchmann C, Shwed U. The black gender gap in educational attainment: historical trends and racial comparisons. Demography. 2011;48:889–914. [DOI] [PubMed] [Google Scholar]
- 18. Wood D, Kaplan R, McLoyd VC. Gender differences in the educational expectations of urban, low‐income African American youth: the role of parents and the school. J Youth Adolesc. 2007;36:417–427. [Google Scholar]
- 19. Singh GK, Yu SM. Infant mortality in the United States: trends, differentials, and projections, 1950 through 2010. Am J Public Health. 1995;85:957–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Copeland VC. African Americans: disparities in health care access and utilization. Health Soc Work. 2005;30:265–270. [DOI] [PubMed] [Google Scholar]
- 21. Georgetown university center for children and families. Medicaid and chip eligibility, enrollment, renewal, and cost sharing policies as of January 2017: findings from a 50‐state survey [internet]. Ccf.Georgetown.Edu. 2020. https://ccf.georgetown.edu/wp‐content/uploads/2017/01/report‐medicaid‐and‐chip‐eligibility‐as‐of‐jan‐2017‐1.Pdf. Accessed March 1, 2020.
- 22. Trends in medicaid and chip eligibility over time –section 3: eligibility trends by medicaid expansion status – 2016 update – 8762–02 [internet]. The henry j. Kaiser family foundation. 2020. https://www.kff.org/report‐section/trends‐in‐medicaid‐and‐chip‐eligibility‐over‐time‐section‐3‐eligibility‐trends‐by‐medicaid‐expansion‐status‐2016‐update/. Accessed March 1, 2020.
- 23. Byrd AS, Toth AT, Stanford FC. Racial disparities in obesity treatment. Curr Obes Rep. 2018;7:130–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kleine CE, Moradi H, Streja E, Kalantar‐Zadeh K. Racial and ethnic disparities in the obesity paradox. Am J Kidney Dis. 2018;72:S26–S32. [DOI] [PubMed] [Google Scholar]
- 25. Cullen KW, Liu Y, Thompson D. Diet and physical activity in African‐American girls: seasonal differences. Am J Health Behav. 2017;41:171–178. [DOI] [PubMed] [Google Scholar]
- 26. Acheampong I, Haldeman L. Are nutrition knowledge, attitudes, and beliefs associated with obesity among low‐income Hispanic and African American women caretakers? J Obes. 2013;2013:123901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wadhwa PD, Entringer S, Buss C, Lu MC. The contribution of maternal stress to preterm birth: issues and considerations. Clin Perinatol. 2011;38:351–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lindsay AC, Machado MMT, Wallington SF, Greaney ML. Sociocultural and interpersonal influences on Latina women's beliefs, attitudes, and experiences with gestational weight gain. PLoS One. 2019;14:e0219371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Aguayo‐Mazzucato C, Diaque P, Hernandez S, Rosas S, Kostic A, Caballero AE. Understanding the growing epidemic of type 2 diabetes in the hispanic population living in the united states. Diabetes Metab Res Rev. 2019;35:e3097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hromi‐Fiedler A, Bermudez‐Millan A, Segura‐Perez S, Perez‐Escamilla R. Nutrient and food intakes differ among Latina subgroups during pregnancy. Public Health Nutr. 2012;15:341–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hromi‐Fiedler A, Bermudez‐Millan A, Segura‐Perez S, Perez‐Escamilla R. Household food insecurity is associated with depressive symptoms among low‐income pregnant Latinas. Matern Child Nutr. 2011;7:421–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Medical services expenditures per capita by disease: complications of pregnancy; childbirth; and the puerperium, meps account basis [internet]. Fred.Stlouisfed.Org. 2020. https://fred.stlouisfed.org/series/coprchpcmeps. Accessed March 17, 2020.
- 33. Beam AL, Fried I, Palmer N, Agniel D, Brat G, Fox K, Kohane I, Sinaiko A, Zupancic JAF, Armstrong J. Estimates of healthcare spending for preterm and low‐birthweight infants in a commercially insured population: 2008–2016. J Perinatol. 2020;40:1091–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Institute of medicine (US) committee on understanding premature birth and assuring healthy outcomes; Behrman re, butler as, editors. Preterm birth: causes, consequences, and prevention. Washington (dc): National academies press (us); 2007. 12, societal costs of preterm birth. https://www.ncbi.nlm.nih.gov/books/nbk11358/. [PubMed]
- 35. American heart association CVD burden report [internet]. Healthmetrics.Heart.Org. 2020. https://healthmetrics.heart.org/wp‐content/uploads/2017/10/cardiovascular‐disease‐a‐costly‐burden.pdf. Accessed March 1, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1–S3


