Atherosclerosis is widely recognized to be a chronic inflammatory disease. Monocytes and macrophages are key elements in initiation and progression of atherosclerosis 1 and express the NLRP3 inflammasome, a multiprotein complex that forms in response to “danger signals” and serves as a platform for activation of the protease caspase‐1. 1 Caspase‐1 cleaves pro–interleukin (IL)‐1β to its active form, IL‐1β, the proinflammatory cytokine that drives the proatherosclerotic IL‐6 signaling pathway. 1 , 2 Oxidative stress is one of the danger signals sensed by toll‐like receptors in monocytes, which, in turn, leads to increased transcription of NLRP3 inflammasome proteins. 1 Tobacco cigarette (TCIG) smoking is the most prevalent modifiable risk factor for atherosclerosis. We recently reported that monocytes from TCIG smokers have increased intracellular oxidative stress compared with nonsmokers. 3 Importantly, many preclinical and clinical studies support the notion that the toll‐like receptor 4 (TLR4)‐inflammasome–IL‐6 signaling axis is critical to the initiation and progression of inflammatory atherosclerosis. 1 , 2 It is not surprising, then, that this axis has become a therapeutic target in cardiovascular disease. Canakinumab, a monoclonal antibody against IL‐1β, the caspase‐1 substrate, was found to significantly reduce recurrent cardiovascular events in survivors of myocardial infarction. 2
Although TCIG smoking is at an all‐time low in the United States, electronic cigarette (ECIG) vaping is markedly increasing. It is unknown whether vaping carries the same risk for atherosclerosis as smoking, a determination with significant public health implications. We reasoned that measuring expression of key proteins of the TLR4–inflammasome–IL‐6 signaling axis in otherwise healthy young individuals without other known cardiac risk factors, except that they smoke or vape, would provide insights into the relative cardiac risk of smoking and vaping.
The data that support the findings of this study are available from the corresponding author on reasonable request. H.R.M. and T.K. had full access to all of the data in the study and take responsibility for its integrity and the data analysis. We conducted studies in immune cells in 33 otherwise healthy young individuals (mean age, 24.4±3.5 years), including 9 long‐term (>1 year) TCIG smokers, 12 long‐term ECIG vapers, and 12 nonsmokers. 3 Former TC smokers were eligible if >1 year had elapsed since quitting. Baseline characteristics of the 3 groups have been published and did not differ. 3 All participants were healthy, with no known medical problems or prescription medications (oral contraceptives allowed). Importantly, TCIG smokers and ECIG vapers had similar, and relatively light, smoking burdens as estimated by plasma cotinine levels (58.0±39.5 versus 85.0±126.2 ng/mL, P=0.34). 3 After abstaining from tobacco product use for at least 12 hours, as confirmed by nondetectable plasma nicotine levels at the time of blood collection, blood was drawn for cell isolation. Cryopreserved peripheral blood mononuclear cells were processed for flow cytometry analysis. In peripheral blood monocytes, we used multicolor flow 3 to determine expression of key TLR4–inflammasome–IL‐6 signaling axis proteins, including: (1) caspase‐1, which cleaves pro–IL‐1β to active IL‐1β; (2) TLR4, which senses danger (eg, oxidative stress) and then primes the NLRP3 inflammasome; and (3) IL‐6 receptor α (IL‐6R‐α), a major downstream cytokine implicated in cardiovascular disease. 1 , 2 The experimental protocol was approved by the institutional review board at the University of California, Los Angeles, and written informed consent was obtained from each participant.
Caspase‐1 levels were markedly and significantly increased in monocytes from TCIG smokers, but not ECIG vapers, compared with nonsmokers (Figure). Interestingly, caspase‐1 levels were significantly reduced in ECIG vapers compared with nonsmokers. Similarly, TLR4 levels were markedly and significantly increased only in TCIG smokers but not in ECIG vapers (Figure) compared with nonsmokers. Finally, IL‐6R‐α levels were markedly increased in TCIG smokers but not ECIG vapers (Figure) compared with nonsmokers.
Figure 1. Protein levels of toll‐like receptor 4 (TLR4), caspase 1, and interleukin 6 receptor α (IL‐6R‐α) in CD14+ monocytes among smoker groups.
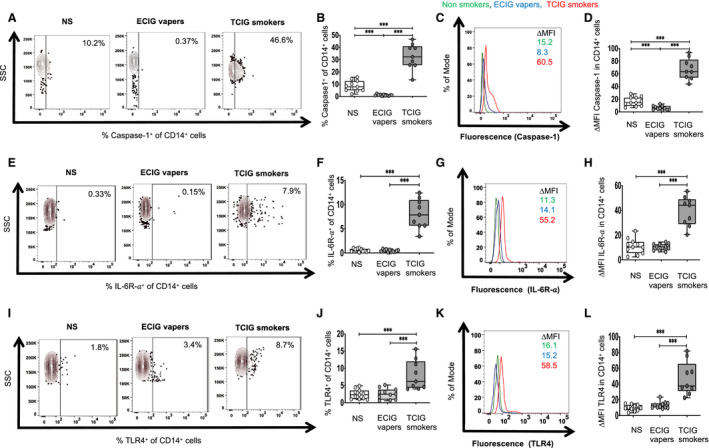
A through L, Flow cytometry was used to determine membrane protein levels of TLR4 and IL‐6R‐α and intracellular protein levels of caspase‐1. Fluorescence intensity of a positive cell population was compared with a negative cell population (fluorescence minus 1 negative control for staining) (∆MFI). The compared groups were nonsmokers (NS, white), electronic‐cigarette vapers (ECIG vapers, light grey), and tobacco cigarette smokers (TCIG smokers, dark grey). Representative data of percentage of CD14+ monocytes that had positive staining for each protein between compared groups are shown for caspase 1 (A), IL‐6R‐α (E), and TLR4 (I). Summary of data for caspase 1 (B), IL‐6R‐α (F), and TLR4 (J) are shown. Representative data of ∆MFI of caspase 1 (C), IL‐6R‐α (G), and TLR4 (K) in CD14+ monocytes. Summary of data for ∆MFI of caspase 1 (D), IL‐6R‐α (H), and TLR4 (L) are shown. Kruskal‐Wallis ANOVA was used to compare the 3 groups and, if the results were statistically significant (P<0.05), then the Mann‐Whitney test was used to compare individual 2 groups (***P<0.001).
To our knowledge, this is the first study in humans to demonstrate a marked and significant increase in key proteins in the TLR4–inflammasome–IL‐6 signaling axis, including caspase‐1 and TLR4, in monocytes of TCIG smokers but not ECIG vapers compared with nonsmokers. This novel finding is consistent with the notion that ECIGs would be less likely to promote inflammation, including inflammatory atherosclerosis, compared with TCIGs. These data are similar to data reported by Tsai et al 4 who showed increased inflammasome proteins in bronchoalveolar lavage fluid in TCIG smokers, intermediate levels in ECIG vapers, and lowest levels in nonsmokers. 4 In our study, the plasma cotinine levels were not different between ECIG vapers and TCIG smokers, implicating the non‐nicotine pro‐oxidant toxicants in TCIG smoke as the mediators of increased transcription of these proteins. Surprisingly, caspase‐1 levels were slightly but significantly lower in ECIG vapers compared with nonsmokers. We speculate that in TCIG smokers, an anti‐inflammatory nicotine effect on activation of nuclear factor‐kB and caspase‐1 in response to danger signals 1 is overwhelmed by the increased oxidative stress burden carried by the >7000 non‐nicotine constituents in TCIG smoke.
We also found that TLR4 levels are significantly increased in monocytes from TCIG smokers compared with ECIG vapers and nonsmokers. TLR4 is a pattern recognition receptor that senses danger and leads to priming of the NLRP3 inflammasome. This finding is consistent with the report by Buscetta et al 5 in which cigarette smoke extract was found to upregulate the TLR4 pathway. 5
The markedly increased IL‐6R‐α on monocytes in TCIG smokers is of concern. This finding would be expected to render monocytes more susceptible to activation by the cytokine IL‐6. IL‐6 is a cytokine strongly implicated in atherosclerosis in humans. 2
TCIGs but not ECIGs are associated with increased expression of key proteins in the TLR4–inflammasome–IL‐6 signaling axis, supporting the notion that ECIGs may represent a harm reduction approach to those addicted to TCIGs who are unwilling or unable to quit. The increased IL‐6R‐α in monocytes in smokers provides urgency to smoking cessation efforts.
Sources of Funding
This work was supported by the Tobacco‐Related Disease Research Program (TRDRP) under the contract number TRDRP 28IR‐0065 (H.R.M.), by UCOP under the contract number R00RG2749 Emergency COVID‐19 Research Seed Funding (H.R.M.), and by the National Institutes of Health (NIH) National Center for Advancing Translational Science (NCATS) UCLA CTSI grant number L1TR001881. This work was also supported in part by NIH grants R01AG059501 and R03AG059462 (to T.K.). The flow cytometry machine used in the study was purchased through the UCLA Center for AIDS Research (P30AI28697) grant.
Disclosures
None.
Acknowledgments
Author contributions: Kelesidis: design of the study, flow cytometry experiments, supervision of experiments, data analysis, interpretation of data, writing of the article (with H.R.M.), revision of the article, and financial support. Zhang: data collection, processing of biospecimens, and performance of flow cytometry experiments. Tran: data collection and revision of the article. Sosa: data collection and revision of the article. Middlekauff: design of the study, interpretation of data, writing of the article (with T.K.), revision of the article, and financial support.
(J Am Heart Assoc. 2021;10:e019324. DOI: 10.1161/JAHA.120.019324.)
For Sources of Funding and Disclosures, see page 3.
REFERENCES
- 1. Karasawa T, Takahashi M. Role of NLRP3 inflammasomes in atherosclerosis. J Atheroscler Thromb. 2017;24:443–451. DOI: 10.5551/jat.RV17001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker SD, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377:1119–1131. DOI: 10.1056/NEJMoa1707914. [DOI] [PubMed] [Google Scholar]
- 3. Kelesidis T, Tran E, Arastoo S, Lakhani K, Heymans R, Gornbein J, Middlekauff HR. Elevated cellular oxidative stress in circulating immune cells in otherwise healthy young people who use electronic cigarettes in a cross‐sectional single‐center study: implications for future cardiovascular risk. J Am Heart Assoc. 2020;9:e016983. DOI: 10.1161/JAHA.120.016983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tsai M, Song MA, McAndrew C, Brasky TM, Freudenheim JL, Mathe E, McElroy J, Reisinger SA, Shields PG, Wewers MD. Electronic versus combustible cigarette effects on inflammasome component release into human lung. Am J Respir Crit Care Med. 2019;199:922–925. DOI: 10.1164/rccm.201808-1467LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Buscetta M, Di Vincenzo S, Miele M, Badami E, Pace E, Cipollina C. Cigarette smoke inhibits the NLRP3 inflammasome and leads to caspase‐1 activation via the TLR4‐TRIF‐caspase‐8 axis in human macrophages. FASEB J. 2020;34:1819–1832. DOI: 10.1096/fj.201901239R. [DOI] [PubMed] [Google Scholar]


