Acute myocardial infarction (AMI) remains the leading cause of death worldwide. 1 As “time is muscle”, major efforts were undertaken to address patient and system delays and facilitate early diagnosis and revascularization in as many patients with AMI as possible. 2 , 3 Little is known about the impact of medical factors on patient delay. As patient education and patient empowerment to appropriately react to acute chest pain suggestive of AMI are key components in post‐AMI cardiac rehabilitation programs, we hypothesized that because of the impact of these educational programs on actual patient behavior, patients with prior AMI would have shorter delays when again presenting with suspected AMI compared with patients without prior AMI. 4
This hypothesis was tested in a prospective, multicenter study, including patients presenting with acute chest discomfort to 12 emergency departments (EDs) in 5 countries (ClinicalTrials.gov registry, NCT00470587). The study was approved by local ethic committees. Written informed consent was obtained from all patients. 2 Times of chest pain onset (CPO) and chest pain maximum were prospectively assessed by study physicians. Patient delay, as quantified by time from CPO to the ED (CPO‐ED) was the primary outcome measure. Time from chest pain maximum to ED presentation was the secondary outcome measure. Time of ED presentation was the time of first vital sign documentation in the ED. Two independent cardiologists adjudicated the final diagnosis, according to the universal definition of AMI. 2 , 3 Patients on long‐term dialysis were excluded, according to the study protocol. Sensitivity analyses explored the impact of a history of coronary artery disease (CAD) with or without prior AMI, the impact of sex, and the final adjudicated diagnosis underlying acute chest discomfort (AMI versus other causes). Differences between groups were assessed using Kruskal‐Wallis rank‐sum test for continuous variables and χ2 or Fisher exact test for categorical variables. The 95% CIs of proportions were constructed using bootstrap. The data have not been made publicly available, but are available from the authors on reasonable request.
From April 2006 to April 2018, 6649 patients, 33% women, were eligible for this analysis. Of these patients, 1515 (23%) had a history of prior AMI, and 606 (9%) had a history of CAD, but no prior AMI.
CPO‐ED was comparable in patients with and without prior AMI (median, 5.0 [interquartile range {IQR}, 2.5–13.0] hours versus 5.8 [IQR, 2.0–17.5] hours; P=0.86; Figure [A]). Similarly, time from chest pain maximum to ED presentation was comparable in patients with and without prior AMI (median, 3.0 [IQR, 1.5–6.0] hours versus 3.0 [IQR, 1.5–6.0] hours; P=0.99; Figure [B]). Also, both patient groups with and without prior AMI had comparable rates of ED admission by the ambulance (17% [95% CI, 15.0%–18.8%] versus 16% [95% CI, 14.5%–16.5%]; P=0.23). Sensitivity analysis revealed similar findings for the comparisons of patients with a history of CAD (with or without prior AMI) versus patients without CAD (eg, CPO‐ED was comparable in patients with prior CAD versus patients without prior CAD (median, 5.5 [IQR, 3.0–13.0] hours versus 5.5 [IQR, 2.0–18.0] hours). Similarly, sensitivity analysis addressing the possible impact of sex (eg, CPO‐ED in women with prior AMI [median, 6.0 {IQR, 3.0–14.0} hours] versus women without prior AMI [median, 6.0 {IQR, 2.0–18.0} hours]) and the final adjudicated diagnosis on CPO‐ED, restricting the analysis to patients with an adjudicated diagnosis of AMI, confirmed the main findings. In this subgroup, CPO‐ED was comparable in patients with prior AMI versus patients without AMI (median, 5.0 [IQR, 2.5–12.0] hours versus 5.5 [IQR, 2.0–14.0] hours; Figure [C]).
Figure 1. Cumulative distribution curve of patient delay of patients with vs without prior acute myocardial infarction (AMI), quantified as time from chest pain onset (CPO) to presentation to the emergency department (ED) (A), time from chest pain maximum (CPM) to presentation to the ED (B), and time from CPO to presentation to the ED in the subgroup of patients with an adjudicated final diagnosis of AMI (C).
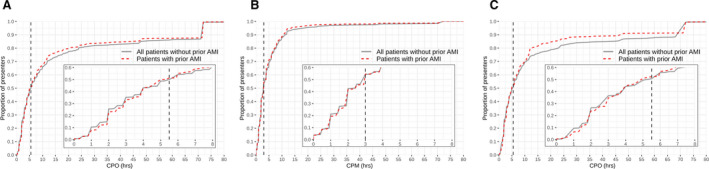
*Vertical line denotes the overall median.
Quantifying the overall impact of an extensive list of medical factors on CPO‐ED, multivariable binary logistic regression, including all univariable significant medical factors for the prediction of late presentation (defined as above the median of 5.5 hours in this study), showed low accuracy (area under the receiver‐operating characteristic curve of 0.66 [95% CI, 0.65–0.67]).
These findings reject our hypothesis and have important clinical implications. The impact of post‐AMI educational programs specifically, and medical factors in general, on CPO‐ED during subsequent acute chest discomfort episodes seems much smaller than previously thought. 4 These findings also extend and support observations that many patients with prior AMI do not perceive themselves as being at an increased risk of having another AMI. In addition, nonmedical factors, including sociodemographic aspects, seem to play an important role in the decision of seeking medical help. 5
Two main consequences emerge from these findings. First, post‐AMI educational programs need to intensify efforts aiming at increasing the implementation efficacy of the theoretical content of AMI symptom recognition and the “time is muscle” concept. This likely should include methods to better address symptom denial. Second, as nonmedical factors seem to be important contributors to CPO‐ED, efforts aiming to explore and possibly mitigate them should be intensified.
In conclusion, patients with prior AMI do not present earlier to the ED when having a subsequent acute chest pain episode suggestive of AMI compared with patients without prior AMI, irrespective of sex and the final adjudicated diagnosis (AMI versus other diagnoses).
Appendix
APACE Investigators
Joan Walter, MD (Cardiovascular Research Institute Basel and Department of Cardiology, University Hospital Basel, University of Basel, Basel, Switzerland; GREAT Network); Ana Yufera Sanchez, MD (Cardiovascular Research Institute Basel and Department of Cardiology, University Hospital Basel, University of Basel, Basel, Switzerland; GREAT Network); Christian Puelacher, MD (Cardiovascular Research Institute Basel and Department of Cardiology, University Hospital Basel, University of Basel, Basel, Switzerland; GREAT Network; Department of Internal Medicine, University Hospital Basel, University of Basel, Basel, Switzerland); Jeanne du Fay de Lavallaz (Cardiovascular Research Institute Basel and Department of Cardiology, University Hospital Basel, University of Basel, Basel, Switzerland; GREAT Network); Samyut Shrestha, MD; (Cardiovascular Research Institute Basel and Department of Cardiology, University Hospital Basel, University of Basel, Basel, Switzerland; GREAT Network); Beatriz López, MD (Emergency Department, Hospital Clinic, Barcelona, Catalonia, Spain); Esther Rodriguez Adrada, MD (Servicio de Urgencias, Hospital Clínico San Carlos, Madrid, Spain); Piotr Muzyk, MD (GREAT Network; 2nd Department of Cardiology, Medical University of Silesia, Zabrze, Poland); Beata Morawiec, MD (GREAT Network; 2nd Department of Cardiology, Medical University of Silesia, Zabrze, Poland); Jens Lohrmann, MD (Cardiovascular Research Institute Basel and Department of Cardiology, University Hospital Basel, University of Basel, Basel, Switzerland); Michael Christ, MD (Emergency Department Cantonal Hospital of Luzerne, Luzerne, Switzerland); Paul David Ratmann, MD (Cardiovascular Research Institute Basel and Department of Cardiology, University Hospital Basel, University of Basel, Basel, Switzerland; GREAT Network); Patrick Badertscher, MD (Cardiovascular Research Institute Basel and Department of Cardiology, University Hospital Basel, University of Basel, Basel, Switzerland; GREAT Network); Ketina Arslani, MD (Cardiovascular Research Institute Basel and Department of Cardiology, University Hospital Basel, University of Basel, Basel, Switzerland; GREAT Network); Tobias Zimmermann, MD (Cardiovascular Research Institute Basel and Department of Cardiology, University Hospital Basel, University of Basel, Basel, Switzerland; GREAT Network; Department of Internal Medicine, University Hospital Basel, University of Basel, Basel, Switzerland); Michael Freese, RN (Cardiovascular Research Institute Basel and Department of Cardiology, University Hospital Basel, University of Basel, Basel, Switzerland; GREAT Network); Karin Wildi, MD (Cardiovascular Research Institute Basel and Department of Cardiology, University Hospital Basel, University of Basel, Basel, Switzerland; GREAT Network); Desiree Wussler, MD (Cardiovascular Research Institute Basel and Department of Cardiology, University Hospital Basel, University of Basel, Basel, Switzerland; GREAT Network; Department of Internal Medicine, University Hospital Basel, University of Basel, Basel, Switzerland); Danielle M. Gualandro, MD (Cardiovascular Research Institute Basel and Department of Cardiology, University Hospital Basel, University of Basel, Basel, Switzerland; GREAT Network); Simon Frey, MD (Cardiovascular Research Institute Basel and Department of Cardiology, University Hospital Basel, University of Basel, Basel, Switzerland; GREAT Network); Nicolas Geigy, MD (Blood Transfusion Centre, Swiss Red Cross, Basel, Switzerland).
Sources of Funding
APACE was supported by research grants from the Swiss National Science Foundation, the Swiss Heart Foundation, the European Union, the Cardiovascular Research Foundation Basel, the University Hospital Basel, the University of Basel, Abbott, Beckman Coulter, Roche, Ortho Clinical Diagnostics, Quidel, Siemens, and Singulex.
Disclosures
Dr Nestelberger has received research support from the Swiss National Science Foundation (P400PM_191037/1), the Prof. Dr. Max Cloëtta Foundation, the Margarete und Walter Lichtenstein‐Stiftung (3MS1038), and the University Hospital Basel as well as speaker honoraria/consulting honoraria from Siemens, B. Braun, Beckman Coulter, Bayer, Ortho Clinical Diagnostics, and Orion Pharma, outside the submitted work. Dr Boeddinghaus has received research grants from the University of Basel, the University Hospital of Basel, the Division of Internal Medicine, the Swiss Academy of Medical Sciences, and the Gottfried and Julia Bangerter‐Rhyner‐Foundation; and has received speaker honoraria and/or consulting honoraria from Siemens, Roche Diagnostics, Ortho Clinical Diagnostics, and Quidel Corporation. Dr Koechlin received a research grant from the University of Basel, the Swiss Academy of Medical Sciences, and the Gottfried and Julia Bangerter‐Rhyner Foundation, as well as the “Freiwillige Akademische Gesellschaft Basel.” Dr Rubini has received research grants from the Swiss Heart Foundation and Swiss National Science Foundation (P400PM_180828) as well as speakers/consulting honoraria from Abbott, Ortho Diagnostic, Roche, and Siemens. Dr Twerenbold received research support from the Swiss National Science Foundation (P300PB_167803), the Swiss Heart Foundation, the Swiss Society of Cardiology, the University Hospital of Basel, the University of Basel, and the Cardiovascular Research Foundation Basel as well as speaker honoraria/consulting honoraria from Abbott, Amgen, Brahms, Roche, Singulex, and Siemens. Dr Mueller has received research support from the Swiss National Science Foundation, the Swiss Heart Foundation, Swiss Commission for Technology and Innovation, the European Union, the University of Basel, the University Hospital Basel, the Stiftung für kardiovaskuläre Forschung Basel, Abbott, Beckman Coulter, Biomerieux, Idorsia, Ortho Cinical Diagnostics, Quidel, Roche, Siemens, Singulex, and Sphingotec, as well as speaker honoraria/consulting honoraria from Acon, Amgen, Astra Zeneca, Boehringer Ingelheim, Bayer, BMS, Idorsia, Novartis, Osler, Roche, and Sanofi, outside of the submitted work. The remaining authors have no disclosures to report.
Acknowledgments
We thank the patients who participated in the study, the staff of the emergency departments, the research coordinators, and the laboratory technicians for their most valuable efforts. The authors designed the study, gathered and analyzed the data, vouch for the data and analysis, wrote the letter, and decided to publish. All authors have read and approved the letter. The sponsors had no role in designing or conducting the study and no role in gathering or analyzing the data or writing the letter. The letter and its contents have not been published previously and are not being considered for publication elsewhere in whole or in part in any language, including publicly accessible websites or e‐print servers.
(J Am Heart Assoc. 2021;10:e017829. DOI: 10.1161/JAHA.120.017829.)
Registration: URL: https://www.clinicaltrials.gov; Unique identifier: NCT00470587.
For Sources of Funding and Disclosures, see page 3.
Contributor Information
Christian Mueller, Email: christian.mueller@usb.ch.
for the APACE Investigators:
Joan Walter, Ana Yufera Sanchez, Christian Puelacher, Jeanne du Fay de Lavallaz, Samyut Shrestha, Beatriz López, Esther Rodriguez Adrada, Piotr Muzyk, Beata Morawiec, Jens Lohrmann, Michael Christ, Paul David Ratmann, Patrick Badertscher, Ketina Arslani, Tobias Zimmermann, Michael Freese, Karin Wildi, Desiree Wussler, Danielle M Gualandro, Simon Frey, and Nicolas Geigy
References
- 1. Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, et al. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137:e67–e492. DOI: 10.1161/CIR.0000000000000558. [DOI] [PubMed] [Google Scholar]
- 2. Nestelberger T, Boeddinghaus J, Wussler D, Twerenbold R, Badertscher P, Wildi K, Miró Ò, López B, Martin‐Sanchez FJ, Muzyk P, et al. Predicting major adverse events in patients with acute myocardial infarction. J Am Coll Cardiol. 2019;74:842–854. DOI: 10.1016/j.jacc.2019.06.025. [DOI] [PubMed] [Google Scholar]
- 3. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli‐Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, et al. ESC guidelines for the management of acute myocardial infarction in patients presenting with ST‐segment elevation. Eur Heart J. 2018;39:119–177. DOI: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 4. Naegeli B, Radovanovic D, Rickli H, Erne P, Seifert B, Duvoisin N, Pedrazzini G, Urban P, Bertel O. Impact of a nationwide public campaign on delays and outcome in Swiss patients with acute coronary syndrome. Eur J Prev Cardiol. 2011;18:297–304. DOI: 10.1177/1741826710389386. [DOI] [PubMed] [Google Scholar]
- 5. Lichtman JH, Leifheit EC, Safdar B, Bao H, Krumholz HM, Lorenze NP, Daneshvar M, Spertus JA, D'Onofrio G. Sex differences in the presentation and perception of symptoms among young patients with myocardial infarction. Circulation. 2018;137:781–790. DOI: 10.1161/CIRCULATIONAHA.117.031650. [DOI] [PMC free article] [PubMed] [Google Scholar]


