Since initial reports documenting an increase in midlife U.S. mortality rates were first published,1 numerous studies have examined the resulting demographic, economic, and policy implications. Fewer studies have examined trends for the two major drivers of U.S. mortality: heart disease and cancer. Here, we used two decades (1999-2018) of death certificate data to further inform understanding of contemporary U.S. cancer and heart disease mortality trends overall and by sex, race, ethnicity, and age group.
Publicly available death certificates listing cancer (ICD-10 codes C00-C97) or heart disease (ICD-10 codes I00-I09, I11, I13, and I20-I51) as the underlying cause of death (N=50,163,483 decedents) were obtained from the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research database.2 Age-adjusted mortality rates (AAMRs) in the overall population and by sex, race, and ethnicity were calculated using the direct method with the 2000 U.S. Census as the standard population. Annual relative rates of change in AAMRs were estimated using Poisson regression allowing for overdispersion and including a piecewise linear spline with one knot at 2011. These modeling decisions were informed by prior research,3 the limited number of data points (20), and the need for a common analytic strategy that enabled comparisons of cancer and heart disease mortality trends in the overall population and when stratified by sex, race, age group, and ethnicity. Because annual age-specific population size estimates were unavailable for decedents 85+ years of age, crude mortality rates were calculated for age-specific analyses, again using Poisson models allowing for overdispersion and including a piecewise linear spline with a knot at 2011. Sensitivity analyses that adjusted for age in decedents <85 years were consistent with findings based on crude mortality rates.
Decedents <25 years of age were excluded from age-specific analyses given small numbers of deaths. The institutional review board of the University of North Carolina at Chapel Hill determined this study did not represent human subjects research.
From 1999-2018, the proportion of deaths listing cancer or heart disease as the underlying cause decreased from 53.6% (1999) to 44.4% (2018). For heart disease, annual estimated relative rates of change in AAMRs slowed from −3.80 [95% CI: (−3.66, −3.93)] in 1999-2011 to −0.72 (95% CI: −0.45, −0.99) in 2011-2018. For cancer, estimated declines in relative AAMR annual change observed from 1999-2011 (annual AAMR relative change: −1.48 (95% confidence interval (CI): −1.43, −1.52) accelerated during 2011-2018 [annual AAMR relative change: −1.77 (95% CI: −1.67, −1.86)]. In 2018, these trends culminated in heart disease mortality continuing to exceed cancer mortality overall (163.1 vs. 148.8 per 100,000 person years) and among males, all racial groups except non-Hispanic Asians, and Hispanics. For females, cancer mortality (AAMR=147.2, 95% CI: 146.7, 147.8) exceeded heart disease mortality (AAMR=146.3, 95% CI: 145.8, 146.8) beginning in 2009.
In contrast to trends seen in the overall population, cancer mortality equaled or exceeded heart disease mortality for all age groups except decedents 85+ years of age (Figure). The greatest difference in mortality was observed for 85+ year old decedents, where annual heart disease crude mortality rates were 2.4 to 3.4 times higher than cancer crude mortality rates. These differences narrowed over time. For decedents 75-84 years of age, cancer and heart disease crude mortality rates were approximately equivalent beginning in 2006, with an estimated 25 more cancer than heart disease deaths per 100,000 person-years in 2018. Among decedents 45-74 years of age, cancer crude mortality was 16-42% higher than heart disease crude mortality in 2018. There also was evidence that heart disease crude mortality rates increased after nadir years in 2011 (182.5/100,000) and 2014 (383.0/100,000) for decedents 55-64 years and 65-74 years of age, respectively. Finally, for decedents 25-44 years of age, stagnation in crude heart disease mortality rates combined with declines in cancer crude mortality rates resulted in equivalent crude mortality rates by 2018.
Figure.
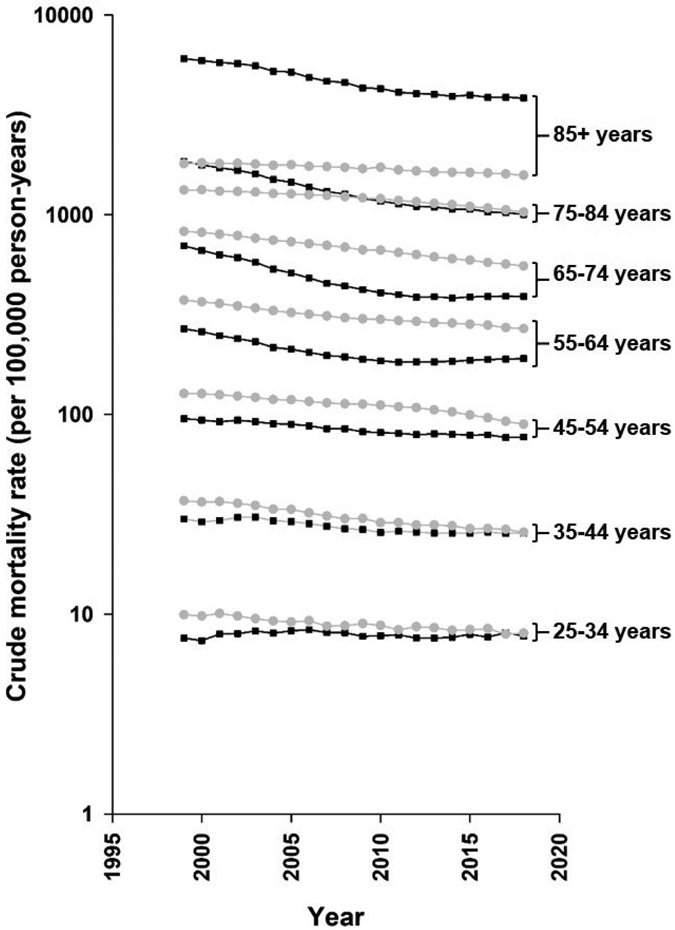
Crude cancer and heart disease mortality rates by age group in the United States, 1999–2018. Annual cancer crude mortality rates are shown by gray circles, with heart disease crude mortality rates shown by black squares.
Despite many strengths, there are limitations that merit consideration, chief of which is reliance on mortality data. Although cancer incidence estimates are available through broad, population-based surveillance programs, parallel data for heart disease incidence are unavailable.4 As an alternative, the death certificate provides a standardized source of health-related data at national, state, and local levels. Several studies have examined the accuracy of death certificates to classify heart disease mortality, reporting overestimates of heart disease mortality, particularly for elderly decedents.5 However, deaths in younger decedents were less prone to misclassification.5 These observations emphasize the need to examine mortality trends within age groups, as potential increases in heart disease mortality in younger populations may signal a very high future disease burden as the cohort ages.
In conclusion, cancer and heart disease mortality trends are complex and vary across population subgroups. Whether future years will see other inflection points or subgroup-specific developments that contribute to the changing epidemiology of cancer and heart disease mortality deserves further study.
Acknowledgments
Funding Sources
None
Footnotes
Conflict of Interest Disclosures
None
REFERENCES
- 1.Case A and Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112:15078–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention National Center for Health Statistics. Underlying cause of death, 1999-2018. Last accessed: November 11, 2019. https://wonder.cdc.gov/ucd-icd10.html [Google Scholar]
- 3.Sidney S, Quesenberry CP Jr., Jaffe MG, Sorel M, Nguyen-Huynh MN, Kushi LH, Go AS and Rana JS. Recent Trends in Cardiovascular Mortality in the United States and Public Health Goals. JAMA cardiology. 2016;1:594–9. [DOI] [PubMed] [Google Scholar]
- 4.Ford ES, Roger VL, Dunlay SM, Go AS and Rosamond WD. Challenges of ascertaining national trends in the incidence of coronary heart disease in the United States. J Am Heart Assoc. 2014;3:e001097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lloyd-Jones DM, Martin DO, Larson MG and Levy D. Accuracy of death certificates for coding coronary heart disease as the cause of death. Ann Intern Med. 1998;129:1020–6. [DOI] [PubMed] [Google Scholar]


