Abstract
Objectives
Latinos are 1.5 times as likely to develop Alzheimer’s dementia as non-Latino Whites. This health disparity may arise from multiple influences with culturally relevant factors receiving increasing attention. Models of acculturation stress the importance of considering acculturation-related factors within the context of socioenvironmental factors to better capture the Latino experience in the United States.
Methods
We measured 10 acculturation and contextually-related variables in 199 Latinos (age 69.7 years) without dementia participating in Rush Alzheimer’s Disease Center studies. We tested the relationship between these variables via Principal Component Analysis (PCA), then investigated how resulting components associated with level of and longitudinal change in global and domain-specific cognition using separate linear mixed-effects models adjusted for relevant confounders and their interactions with time.
Results
The PCA revealed a 3-factor unrotated solution (variance explained ~70%). Factor 1, representing acculturation-related aspects of nativity, language- and social-based acculturation, was positively associated with level, but not change, in global cognition, semantic memory, and perceptual speed. Factor 2, representing contextually-related socioenvironmental experiences of discrimination, social isolation, and social networks, was negatively associated with level of global cognition, episodic and working memory, and faster longitudinal decline in visuospatial ability. Factor 3 (familism only) did not associate with level or change in any cognitive outcome.
Discussion
Acculturation- and contextually-related factors differentiated from each other and differentially contributed to cognition and cognitive decline in older Latinos. Providers should query acculturation and lived experiences when evaluating cognition in older Latinos.
Keywords: Acculturation, Memory, Social interaction, Working memory
The Latino community is one of the fastest growing minority populations in the United States (Greenberg, 2009). In addition to being at the forefront of the Alzheimer’s epidemic (Greenberg, 2009), a sizable proportion of Latinos also have adverse major cardiovascular disease (CVD) risk factors (Daviglus et al., 2012). While great strides have been made to document how these and other modifiable risk factors negatively affect cognition and brain aging in Latinos (Gonzales et al., 2019; Lamar et al., 2019; Ramirez et al., 2007), they do not fully account for age-related health disparities between Latinos and non-Latino Whites. Furthermore, there is evidence that other established risk factors for cognitive decline and dementia in non-Latino Whites, including sex and Apolipoprotein E epsilon 4 status, may not confer the same level of risk among Latinos (Haan et al., 2003; O’Bryant et al., 2013). Thus, investigating more culturally relevant contributors to cognitive decline in Latinos is a logical next step.
Acculturation, the process of adapting to a new environment and potentially adopting its values and practices, is an important contributor to overall health in Latinos, in both positive and negative ways. For example, higher levels of acculturation have been associated with higher levels of health insurance, preventative care utilization, and self-perceived health (Lara et al., 2005). In contrast, acculturation also predicts negative health behaviors including substance abuse, smoking, unhealthy eating (Lara et al., 2005), and CVDs (Daviglus et al., 2016; Lutsey et al., 2008) thought to negatively affect cognition. Directed studies of acculturation and cognition, much like acculturation and overall health, are mixed (Xu et al., 2017 for review). Some studies reported that Latinos with lower levels of acculturation were more likely to show cognitive impairment (Ramirez et al., 2007; Simpao et al., 2005) and higher dementia risk (Haan et al., 2003), while others did not report significant associations (Farias et al., 2011; Flores et al., 2017). These inconsistencies may be due, in part, to overreliance on global cognitive screeners and/or a limited number of cognitive tests. They may also be due to an overemphasis on language-based measures of acculturation (Lara et al., 2005) as opposed to a more comprehensive approach that considers contextual factors that may influence the acculturation process (Abraído-Lanza et al., 2006, 2016; Lara et al., 2005; Lopez-Class et al., 2011; Schwartz, Weisskirch et al., 2010).
The theoretical framework of “acculturation in context” moves beyond acculturation as a static, individualized process to include the dynamic exchange between new and host members of society that emerges from, and is reinforced by broader contextual, socioenvironmental factors (Abraído-Lanza et al., 2016). This framework draws from the model of segmented assimilation (Portes & Zhou, 1992) which suggests that acculturation is based on differential relationships with the “core” culture determined by contextual constraints faced by minority groups. These constraints involve characteristics of the individual (e.g., education, occupation, and English abilities), the social context that receives them (e.g., attitudes of the “core” culture that too often involving obstacles like racism and discrimination), and the family context in which they live (e.g., social support systems). Thus, contextual socioenvironmental factors including experiences of discrimination, family and social support, and cultural stressors need to be integrated into acculturation-related research with Latinos (Abraído-Lanza et al., 2006, 2016; Lara et al., 2005; Lopez-Class et al., 2011; Schwartz, Unger et al., 2010).
There is evidence that contextual socioenvironmental factors contribute to cognition in other minority populations, and emerging work attests to their importance in Latino health. For example, smaller social networks (Barnes et al., 2004) and higher levels of self-reported experiences of discrimination (Barnes et al., 2012) have independently been associated with lower levels of global cognition, episodic memory, executive functioning, and perceptual speed, as well as cognitive decline in non-Latino Blacks. While higher levels of self-reported experiences of discrimination have been associated with higher counts of chronic conditions in Latinos (Molina & Simon, 2014), investigators have suggested that levels of perceived discrimination may vary based on time in the United States (Abraído-Lanza et al., 2016), generational status, and/or social networks of exposure (Viruell-Fuentes, 2007). No studies to date have examined these contextually-related factors with acculturation-related factors to determine whether and how they associate with each other and how they relate to cognition in older Latinos.
This study explored the inclusion of contextual, socioenvironmental factors in the conceptualization of acculturation to better characterize acculturation in context and its relationship with level and change in cognition in older Latinos without dementia at baseline participating in Rush Alzheimer’s Disease Center studies. We subjected acculturation- and contextually-related variables to Principal Component Analysis (PCA) to determine the relationship between these variables. We used the results of this PCA to investigate how subsequent factor score(s) related to level and change in cognition. Based on prior theoretical literature (Abraído-Lanza et al., 2006, 2016; Lara et al., 2005; Lopez-Class et al., 2011; Schwartz, Unger et al., 2010), we hypothesized that acculturation-related variables and contextually-related variables would load on separate factors. Given work investigating individual aspects of these variables in Latinos and other minority populations (Barnes et al., 2004, 2012; Molina & Simon, 2014), we hypothesized that higher acculturation would be associated with higher levels and slower declines in cognition while higher adverse socioenvironmental constraints would be associated with lower levels and faster declines in cognition.
Method
Participants
Participants were self-identified Latinos enrolled in the Rush Memory and Aging Project (MAP; Bennett et al., 2012) or the Rush Alzheimer’s Disease Center (RADC) Latino Core (Marquez et al., in press), two ongoing longitudinal cohort studies at the RADC. First begun in 1997, MAP is a community-based clinical–pathological cohort study of aging in older adults of all races and ethnicities. The Latino Core began in 2015 as a similar longitudinal community-based cohort study of aging with an exclusive focus on older Latinos. Identical in essential details (e.g., a harmonized cognitive protocol, acculturation in context measures, plus overlapping and standardized evaluations of CVD risk factors), older Latinos enroll free of known dementia at baseline and agree to annual, in-home, evaluations. Participants in the MAP also agree to brain donation as a condition of entry.
Latinos in both studies are recruited from a variety of settings in and around Chicago including senior centers, community centers, churches, senior housing, health centers and clinics, social activity fairs, and consulates that cater to ethnic minority seniors. These cohort studies are conducted by the same bilingual investigators with a single population studies team to ensure data can be efficiently merged and compared across cohorts. An Institutional Review Board of Rush University Medical Center approved both studies, and participants gave written informed consent in accordance with the Declaration of Helsinki.
At the time of analyses, 340 Latinos had completed a baseline evaluation and were alive and active for longitudinal follow-up. Of these 340 participants, we excluded 5 participants who had a diagnosis of dementia (Bennett, Schneider, Aggarwal et al., 2006) at the time of their baseline evaluation based on a uniform structured clinical evaluation (Bennett, Schneider, Tang et al., 2006) and following the NINDS/ADRDA criteria (National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association criteria) (McKhann et al., 1984). Of the remaining 335 participants, 89 were missing data on ≥50% of our acculturation in context metrics (many added relatively recently) or lacked key demographic information; an additional 52 participants had not yet reached their first longitudinal follow-up visit. This left 199 individuals for our analyses with a mean follow-up of 3.7 years.
Acculturation in Context
Metrics used in the current research reflected acculturation- and contextually-related factors outlined in the literature as important to research with Latinos (Abraído-Lanza et al., 2006, 2016; Lara et al., 2005; Lopez-Class et al., 2011; Schwartz, Unger et al., 2010). Single-item metrics included language preference for testing (0 = English, 1 = Spanish), nativity status based on country of origin (0 = US, 1 = non-US), and parents’ nativity status based on maternal and paternal country of origin (0 = neither parent, 1 = one parent, 2 = both parents born outside the mainland United States). The Short Acculturation Scale for Hispanics (SASH) quantified domain-specific language- and social-based acculturation levels and provided a total SASH score combining these two domain-specific subscales (Marín et al., 1987). The six-item version of the Sabogal Familism Measure (Sabogal et al., 1987) assessed the level of identification/attachment of individuals with their family, a key aspect of cultural identity in Latino communities. The Williams Everyday Discrimination Scale (Williams et al., 1997) measured self-reported experiences of unfair treatment. Social network size was quantified using standard questions about the number of children, family, and friends each participant had and how often they interacted with them with the final metric representing the number of these individuals seen at least once a month (Bennett, Schneider, Tang et al., 2006). Social isolation was assessed with a five-item version of the de Jong Gierveld Loneliness Scale with higher values indicating more isolation (Wilson, Krueger et al., 2007).
Cognitive Assessment
All participants underwent a cognitive evaluation administered in an identical fashion at annual evaluations (Marquez et al., in press). Tests have been translated into Spanish, back-translated into English, and validated (Marquine et al., 2012). Participants were tested in their preferred language, English or Spanish. Nineteen tests assessed five specific cognitive domains. Episodic memory consisted of scores from immediate and delayed recall of story A from Logical Memory, immediate and delayed recall of the East Boston Story, CERAD Word List Memory, Recall, and Recognition. Semantic memory consisted of performance on a 15-item Boston Naming Test, Verbal Fluency, and a 15-item reading test. Working memory comprises scores for Digit Span Forward and Backward, and Digit Ordering while perceptual speed consisted of performance on Symbol Digit Modalities Test, Number Comparison, and two indices from a modified version of the Stroop Neuropsychological Screening Test. Visuospatial ability was represented by a 15-item Judgment of Line Orientation and a 16-item Standard Progressive Matrices.
Raw scores on each of the individual tests were converted to standard z-scores using the baseline mean (SD) of the entire cohort, and the z-scores of all tests for each domain were then averaged for the five cognitive domains outlined above. A global cognitive function score was also derived averaging a person’s standard scores across all 19 test scores. Psychometric information on these summary scores has been deemed adequate and is contained in previous publications (Wilson et al., 2002).
Potential Covariates
In addition to age, sex, and education, we considered the following as potential confounders of the association between acculturation in context and cognition: vascular disease burden, CVD risk factors, body mass index (BMI), depressive symptomatology, and income.
Vascular disease burden was based on questions probing the presence or absence of claudication, heart attack, congestive heart failure, and stroke by self-report or clinician diagnosis based on neurological exam. Each item was given a value of 0 or 1 with the cumulative disease burden score ranging from 0 to 4 (Boyle et al., 2009). To calculate the CVD risk factor burden, participants were queried for the current or past history of hypertension, diabetes, and/or smoking (max score = 3; higher score = higher burden). BMI was calculated based on height and weight determined by direct measurement to the nearest inch and pound, respectively. A 10-item version of the Center for Epidemiological Studies-Depression scale (CES-D; Wilson et al., 2002) assessed depressive symptoms. Income was measured by asking participants to select one of 10 levels of total income, using a show-card, that represented their personal income for the past month or year including income from sources such as wages, salaries, social security or retirement benefits, help from relatives, rent from property, and so forth (Wilson, Scherr et al., 2007).
Statistical Analysis
Analyses were conducted using SAS/STAT software, version 9.4 of the SAS System for Linux (SAS Institute, Cary, NC) and significance was set at p < .05.
Descriptive summaries of all variables including potential covariates were conducted for the analytic sample. We conducted a PCA including data from all 10 acculturation in context measures at baseline. Fifty-six participants were missing the Sabogal Familism Measure and thus were not included in the PCA. We created individual composite scores for the entire analytic sample based on the resulting factor loadings with raw scores converted to standard z-scores using the baseline mean (SD) of the entire sample; some z-scores were multiplied by −1 to ensure that a higher score reflected higher levels of acculturation and/or contextual socioenvironmental resources.
The PCA-derived composite score(s) were used as separate predictors in a series of linear mixed-effects models to examine the associations of the score(s) with baseline level and longitudinal change in global cognition and the five cognitive domains (separately). Models included terms for age, sex, education, time-in-study, and interactions of each demographic variable with time (core model) with additional adjustments for covariates determined via bivariate Pearson and/or Spearman correlations (as appropriate) between potential covariates (i.e., vascular disease burden, CVD risk factors, BMI, CES-D, and income), PCA-derived composite score(s), and global cognition at baseline.
Results
Participants (N = 199) were on average 70 years of age, primarily female, with an average education at nearly 11 years. The majority of participants (69%) self-identified their country of origin outside of the United States and its territories; named countries included Mexico (41%), Guatemala and Honduras (3% Central American), Colombia, Ecuador, and Peru (~5% South American) or Cuba (<1%). Participants reported an average of 40 years living in the mainland United States. The average SASH score, roughly 2 points, suggested lower levels of acculturation using the recommended cut-point of ≥2.9 as a threshold for higher levels of acculturation (Marín et al., 1987). Additional information may be found in Table 1.
Table 1.
Participant Characteristics at Baseline
| N = 199 | |
|---|---|
| Key demographics | |
| Age (years) | 69.7 (6.6) |
| Sex (male:female ratio) | 38:161 |
| Education (years) | 10.8 (4.7) |
| Years in mainland United States (available for n = 161) | 40.8 (14.0) |
| CES-D | 1.73 (2.19) |
| CVD risk factor burden | 1.2 (0.83) |
| Acculturation in context | |
| Tested in Spanish (n, %) | 140, 70.3 |
| Nativity status (non-US, n, %) | 161, 80.9 |
| Parents’ nativity status (both non-US, n, %) | 131, 92.9 |
| SASH social | 2.2 (0.59) |
| SASH language | 1.9 (1.0) |
| SASH total | 2.1 (0.76) |
| Familism | 20.9 (2.8) |
| Self-report of discrimination | 1.7 (2.0) |
| Social network | 6.6 (5.1) |
| Social isolation | 2.5 (0.70) |
| Cognitive composite scores | |
| Global cognition | −0.28 (0.57) |
| Episodic memory | −0.09 (0.62) |
| Semantic memory | −0.17 (0.80) |
| Working memory | −0.72 (0.72) |
| Perceptual speed | −0.41 (0.99) |
| Visuospatial ability | −0.29 (0.79) |
Notes: CES-D = Center for Epidemiological Studies-Depression; CVD = cardiovascular disease; SASH = Short Acculturation Scale for Hispanics. All values are mean (SD) unless otherwise noted.
PCA of Individual Metrics Reflecting Acculturation in Context
An unrotated PCA of the 10 acculturation in context metrics revealed distinct factor loadings accounting for approximately 70% of the total variation (Table 2). Given the orthogonal nature of the unrotated factor loadings, we did not perform varimax rotation.
Table 2.
Principal Component Analysis of Variables Reflecting Acculturation in Context
| Factor 1 | Factor 2 | Factor 3 | |
|---|---|---|---|
| Tested in Spanish | 0.894 | −0.016 | −0.002 |
| Nativity status (non-US) | 0.802 | −0.127 | −0.195 |
| Parents’ nativity status (both non-US) | 0.563 | −0.315 | −0.356 |
| SASH social | −0.695 | −0.009 | −0.070 |
| SASH language | −0.953 | −0.007 | −0.006 |
| SASH total | −0.967 | −0.008 | −0.025 |
| Self-report of discrimination | 0.004 | 0.665 | 0.101 |
| Social network | 0.011 | −0.664 | 0.437 |
| Social isolation | 0.395 | 0.711 | 0.136 |
| Familism | 0.264 | −0.014 | 0.839 |
| Variance explained | 43.136 | 15.083 | 10.957 |
Notes: SASH = Short Acculturation Scale for Hispanics. Factor loadings are unrotated with bold values representing the primary loading for each study variable.
Factor 1, accounting for 43.1% of the variation explained, represented negative loadings for all three SASH scores, a positive loading for preferred (Spanish) language for testing, and positive loadings for both participant (non-US) and parental (both non-US) nativity. When creating the Factor 1 acculturation-related composite score, z-scores for both nativity status variables and preferred language for testing were multiplied by −1 so that higher scores reflected higher levels of acculturation to the United States. Factor 2 (15.0% of the variation explained) included a positive loading for self-reported experiences of discrimination and social isolation combined with a negative loading for social network size. When creating the contextually-related socioenvironmental Factor 2 composite score, social network size was multiplied by −1 in keeping with the direction of the other variables loading on Factor 2. Factor 3 (10.9% of the variation explained) consisted of a sole positive loading for familism. Given that Factor 3 comprises the one metric that was missing in 56 participants, we created composite scores from Factor 1 and Factor 2 loadings for all 199 participants and allowed the sample size for analyses including Factor 3 to fluctuate thus, maximizing our sample for all other analyses that did not require this metric.
Bivariate correlations (Table 3) revealed that none of the potential vascular covariates (i.e., vascular burden, CVD risk factors, BMI) significantly correlated with our PCA-derived composite scores (p values ≥.07). Only the CVD risk factor score significantly and negatively correlated with global cognition. CES-D was significantly associated with the contextually-related socioenvironmental and global cognitive composite scores (p values ≤.0004). Income was significantly associated with acculturation- and contextually-related composite scores and global cognition (Table 3). Education, an a priori covariate in all models, also correlated with PCA-derived composite scores (p values ≤.002) and income (r (193) = 0.44, p < .0001). Given that education is often included when estimating SES, we did not include income as an additional covariate. Thus, in addition to age, sex, and education, we adjusted for CES-D and CVD risk factors in fully adjusted cognitive analyses outlined below.
Table 3.
Correlation of Potential Covariates, Predictors, and Global Cognitive Outcome
| Acculturation-related composite | Contextually-related composite | Familism | Global cognition | |
|---|---|---|---|---|
| Cumulative vascular disease burden | −0.01 (.85) | −0.12 (.07) | −0.005 (.95) | 0.004 (.94) |
| Cumulative CVD risk factors | −0.11 (.12) | 0.06 (.40) | 0.07 (.35) | −0.18 (.009) |
| Body mass index | −0.06 (.39) | −0.03 (.60) | 0.03 (.60) | −0.05 (.47) |
| CES-D | −0.04 (.57) | 0.44 (<.0001) | −0.09 (.28) | −0.25 (.0004) |
| Income | 0.31 (<.0001) | −0.34 (<.0001) | −0.11 (.20) | 0.39 (<.0001) |
Notes: CES-D = Center for Epidemiological Studies-Depression; CVD = cardiovascular disease. Values are Pearson correlation coefficient (p value) with the exception of the Spearman correlation coefficient (p value) for analyses involving income. Bolded values met significance set at p < .05.
PCA-Derived Composite Scores and Cognition
Acculturation-related composite
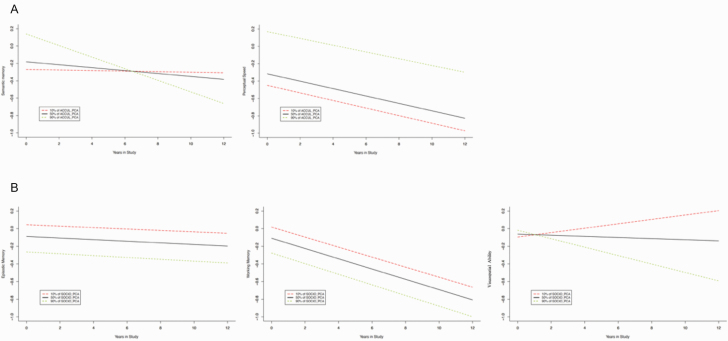
Regardless of adjustments, results of linear mixed-effects models revealed that the acculturation-related composite score was positively associated with the baseline level of but not change in global cognition (Table 4). Similarly, regardless of adjustments, there was a significant positive association between this composite score and levels of semantic memory and perceptual speed (Figure 1A), but not change in these domains over time (Table 4). The acculturation-related composite score was not related to level of or change in episodic memory, working memory, or visuospatial abilities (Table 4).
Table 4.
Fully Adjusted Models for Global Cognition and the Five Cognitive Domains by PCA-Derived Composite Scores
| Global cognition | Episodic memory | Semantic memory | Working memory | Perceptual speed | Visuospatial ability | |
|---|---|---|---|---|---|---|
| Factor 1 composite | ||||||
| Acculturation-related | 0.10 (0.04, p = .03) | 0.03 (0.05, p = .50) | 0.16 (0.06, p = .01) | 0.07 (0.05, p = .23) | 0.25 (0.06, p = .0002) | 0.05 (0.05, p = .36) |
| Time × Acculturation-related | −0.01 (0.01, p = .37) | −0.01 (0.01, p = .35) | −0.02 (0.02, p = .20) | 0.008 (0.01, p = .45) | 0.002 (0.01, p = .89) | 0.02 (0.01, p = .09) |
| Factor 2 composite | ||||||
| Contextually-related | −0.15 (0.05, p = .005) | −0.17 (0.06, p = .007) | −0.14 (0.08, 0.08) | −0.17 (0.07, p = .01) | −0.21 (0.08, p = .01) | 0.04 (0.07, 0.54) |
| Time × Contextually-related | 0.001 (0.01, p = .96) | −0.001 (0.02, 0.95) | 0.01 (0.03, 0.65) | −0.002 (0.02, 0.92) | 0.02 (0.02, 0.38) | −0.04 (0.02, 0.06) |
| Factor 3 | ||||||
| Familism | 0.01 (0.04, p = .71) | 0.06 (0.05, p = .17) | −0.04 (0.06, 0.48) | −0.03 (0.05, 0.48) | 0.01 (0.06, 0.77) | −0.05 (0.06, 0.38) |
| Time × Familism | −0.005 (0.01, p = .69) | −0.01 (0.02, p = .60) | 0.03 (0.02, 0.15) | 0.007 (0.02, 0.72) | −0.01 (0.02, 0.45) | −0.01 (0.03, 0.60) |
Notes: PCA = Principal Component Analysis. Fully adjusted models included adjustment for the following: age, sex, education, Center for Epidemiological Studies-Depression score, cumulative cardiovascular disease risk factor burden, and their individual interactions with time (data not shown). Values are unstandardized coefficient (standard error, p value) from linear regression models with significance corrected for multiple comparisons at p < .01 for the five cognitive domain score models. Bolded terms and values denote statistical significance.
Figure 1.
Representation of the separate associations of PCA-derived composite scores of (A) acculturation-related variables (ACCUL_PCA) with level of and change in semantic memory and perceptual speed and (B) contextually-related socioenvironmental variables (SOCIO_PCA) with level of and change in episodic and working memory as well as visuospatial abilities in fully adjusted models accounting for age, sex, education, time-in-study, CES-D, CVD risk factor burden, and interactions of each variable with time. Figures divide each composite into percentiles, i.e., 10%, 50%, and 90%, for ease of interpretation. CES-D = Center for Epidemiological Studies-Depression; CVD = cardiovascular disease; PCA = Principal Component Analysis.
Contextually-related socioenvironmental composite
Regardless of adjustments, linear mixed-effects models revealed that the contextually-related composite score inversely associated with level of but not change in global cognition (Table 4). Similarly, this composite score, reflecting higher levels of self-reported experiences of discrimination and social isolation as well as smaller social networks, was associated with lower baseline levels of episodic and working memory, and slower perceptual speed, regardless of adjustments (Figure 1B). This contextually-related composite score was also inversely associated with change in (but not level of) visuospatial ability (core estimate = −0.06, SE = 0.02, p = .001); additional adjustment for CES-D and CVD risk factors did not reduce beta estimates but did alter p values (Table 4, Figure 1B). Lastly, while the contextually-related composite score was inversely associated with level of semantic memory in core models (estimate = −0.20, SE = 0.07, p = .005), additional adjustments for CES-D and CVD risk factors reduced estimates to −0.14 and increased p values to .08.
Familism
Familism did not associate with level of or change in global cognition or any of the five cognitive domains, regardless of adjustments (Table 4).
Comprehensive Models of PCA-Derived Composite Scores and Cognition
We repeated fully adjusted models by adding all three PCA-derived composite scores as independent predictors in the same model based on mutual significant results above. The acculturation- and contextually-related socioenvironmental composite scores associated with level of (acculturation-related estimate = 0.12, SE = 0.05, p = .01; contextually-related estimate = −0.15, SE = 0.05, p = .004) but not change in (p values ≥.14) global cognition. Higher levels of acculturation associated with faster perceptual speed at baseline (estimate = 0.29, SE = 0.08, p = .0007), while higher levels of self-reported experiences of discrimination and social isolation and smaller social networks associated with slower perceptual speed at baseline (estimate = −0.21, SE = 0.08, p = .0.01); familism was not associated with level of or change in global cognition or perceptual speed.
Discussion
In this cohort study of approximately 200 older Latinos without dementia at baseline, we measured acculturation-related factors within the context of socioenvironmental factors to investigate the association of acculturation in context on cognition. An unrotated PCA revealed orthogonal factor loadings for acculturation-related (Factor 1), contextually-related socioenvironmental (Factor 2), and familism (Factor 3) variables. Consistent with our hypotheses, resulting PCA-derived composite scores revealed that acculturation-related variables including nativity, language- and social-based acculturation were positively associated with level of global cognition as well as semantic memory and perceptual speed performance. The contextually-related socioenvironmental composite score reflecting higher levels of self-reported experiences of discrimination and social isolation, and smaller social networks, was associated with lower baseline levels of global cognition, more specifically episodic memory, working memory, and slower perceptual speed as well as faster rates of decline in visuospatial abilities. Familism, the Latino-specific measure of family identification/attachment (Sabogal et al., 1987), did not associate with any cognitive score. When placed in the same model, acculturation- and contextually-related composite scores independently contributed, albeit in different directions, to global cognition and perceptual speed at baseline. Taken together, results suggest that acculturation in context represents a multifaceted concept, aspects of which differentially contribute to level more so than change in cognition in older Latinos.
Although acculturation-related and contextually-related socioenvironmental composites were both associated with global cognition, there were differences in the direction of these associations as well as their associations with domain-specific cognition, providing a unique opportunity to consider life milieu as it relates to cognition. For example, while SASH scores suggest our participants report lower levels of language- and social-based acculturation than participants from other studies (Marín et al., 1987), our participants also reported approximately 40 years of living in a US state. Within this context, the association of higher acculturation with higher baseline levels of global cognition, more specifically, semantic memory and perceptual speed, may reflect known associations between higher levels of acculturation and higher levels of education, health insurance, and/or access to care including preventative care and health-related medications (Daviglus et al., 2016; Lara et al., 2005; Padilla et al., 2011). Evidence in support of these potential mechanisms includes the fact that our semantic memory domain includes a reading task often thought of as a proxy for educational quality, as well as the fact that previous work from our group has shown that lower semantic memory and slower processing speed are associated with uncontrolled CVD risk factors (Arvanitakis et al., 2006; Kazlauskaite et al., 2020). In contrast, higher levels of self-reported experiences of discrimination and social isolation, as well as smaller social networks, were associated with lower levels of baseline global cognition, more specifically, episodic memory, working memory, and slower perceptual speed, as well as a faster decline in visuospatial abilities (abilities that may rely not only on visuospatial processing, but working memory already reduce at baseline secondary to these same socioenvironmental factors). While higher acculturation has been associated with greater medication adherence, it does not necessarily translate to greater health (Padilla et al., 2011); and adverse social interactions including experiences of discrimination have long been associated with exacerbated CVD and associated risk (Lewis et al., 2009).
When taken together, results suggest that older Latinos’ cognitive starting point in specific domains may be bolstered by higher levels of acculturation-related factors including nativity and language, while other cognitive domains may be undermined both at baseline and over time by negative contextually-related factors of the socioenvironmental milieu in which they live. Thus, acculturation, a multifaceted process, may exert both beneficial and detrimental effects on health, including cardiovascular health (Daviglus et al., 2016), and our results suggest the same may be said for cognitive health. In fact, when combined within the same model, both acculturation-related and contextually-related factors of acculturation in context were significant contributors to cognition. Thus, providers working with older Latinos may wish to expand beyond interview questions of nativity and/or language preference to include socioenvironmental factors reflective of Latinos’ lived experiences in the United States. Furthermore, outreach and policies to change the social context in which older Latinos experience the United States may prove useful intervention targets for protecting cognitive aging in this population.
Results of this study contribute to the literature in several ways. First, through the results of the unrotated PCA, we found statistically independent factor loadings that outline aspects of acculturation in context. These empirically determined composite measures build upon theories and models acknowledging the multifaceted nature of acculturation (Abraído-Lanza et al., 2006, 2016; Lara et al., 2005; Lopez-Class et al., 2011; Portes & Zhou, 1992; Schwartz, Unger et al., 2010) and lay the groundwork for future larger-scale studies of the interplay of these factors using advanced statistics. Second, while acculturation-related factors including preferred language of testing, nativity, and years lived in a US state have been associated (separately) with higher scores on the Modified Mini-Mental State (3MS) test (Farias et al., 2011), slower cognitive decline (Hill et al., 2012), lower prevalence of Mini-Mental State Examination-defined (Simpao et al., 2005) or Medicare/Medicaid documented (Ramirez et al., 2007) cognitive impairment, and lower dementia risk (Haan et al., 2003), we extended these individual results to include broader socioenvironmental factors of acculturation in context and more specific cognitive domains. Unlike these previous studies, however, our acculturation-related composite did not relate to longitudinal cognitive change; this may be due in part to the more inclusive nature of our metric. For example, Hill et al. (2012) reported slower cognitive decline primarily in men who migrated in midlife while lower dementia risk was related to an acculturation-related metric probing language-, media-, and social-based Spanish/English preferences (Haan et al., 2003) as opposed to considering other factors like self or parental nativity. It should be noted that when considered individually, only language used for testing was associated with change in cognition over time in our study (data not shown). In contrast, work to date investigating contextually-related socioenvironmental factors like family networks (Simpao et al., 2005) or social support and social activities (Howrey et al., 2015) in isolation reported mixed results related to cognition and cognitive decline in older Mexican Americans. Our study provides a more comprehensive assessment of these and other socioenvironmental factors reporting associations with level of and change in cognition in a more diverse Latino cohort.
While beyond the scope of this study, potential underlying mechanisms to explain the associations between acculturation in context and level of and change in cognition may be found in the literature. In addition to the discussion of potential lifestyle and health behavior mechanisms by which acculturation-related variables may operate as outlined above (Daviglus et al., 2016; Lara et al., 2005; Padilla et al., 2011), the high rate of Spanish language preference and lower SASH scores in our analytic sample combined with positive associations between acculturation and levels of cognition may suggest a selective path of acculturation that allows for the maintenance of important cultural ideals (Portes & Zhou, 1992) and hence, lower levels of acculturation-related stress. Lower stress is associated with lower levels of circulating cortisol (Lenze et al., 2011) that are otherwise, when elevated, detrimental to cognition (Gomez-Gallego & Gomez-Garcia, 2019); thus, lower stress and/or cortisol levels may underlie our acculturation-related composite score results. In contrast, contextually-related socioenvironmental factors have been shown to negatively affect levels of inflammation directly (Heffner et al., 2011; Lewis et al., 2010) and, as previously stated, indirectly through adverse cardiovascular health (Lewis et al., 2009) in other minority populations. Thus, older Latinos reporting discrimination, isolation, and/or smaller social networks may have simultaneously experienced increases in inflammatory processes and/or adverse cardiovascular health outcomes detrimental to brain health and associated cognition (Nilsson et al., 2011). More work is needed to verify these hypothesized links.
This study has several strengths. The comprehensive nature of not only our conceptualization of acculturation, but also our cognitive assessment allowed us to discuss the effect of domain-specific culturally relevant factors on domain-specific cognition in Latinos. We studied multiple aspects of acculturation in context particularly relevant for older Latinos comprehensively and examined them as they related to cognition at baseline and over time providing results across a mean of 3.7 years of follow-up. While we revealed several trends toward relationships between our composite scores and cognitive decline, most of these results did not meet our threshold for significance suggesting additional follow-up time may be needed to detect more robust associations. Although our cohort mainly comprises self-identified Mexicans and Puerto Ricans, we did have representation from Cuba, Central and South America making this a relatively diverse group.
This study also has several limitations. While we adjusted for several variables thought to confound our effect of interest, additional variables such as acculturation-related stress were not accounted for and may help to explain our results. Likewise, our CVD risk factor covariate was based on self-report which inherently relies on awareness of vascular health, the awareness that may be reduced in some Latinos (Sorlie et al., 2014). Additionally, we did not include neighborhood-level socioenvironmental factors thought to be associated with acculturation in context (Abraído-Lanza et al., 2016). Such information may help place familism within the larger conceptual model through a better understanding of extended family networks (Sabogal et al., 1987) secondary to communalism (Schwartz, Weisskirch et al., 2010) or ethnic enclaves (Weden et al., 2017). We also lacked information on the age of migration and only had information on overall time in the United States for approximately 80% of our sample. Lastly, while regression analysis allows for the assessment of direct associations, mediators as well as moderators of effects, the use of structural equation models and/or path analyses may further our understanding of the complex relationships between acculturation-related constructs. Future larger-scale studies are needed that incorporate additional aspects of acculturation in context and more advanced statistical approaches with cognition in Latinos.
Acknowledgments
We thank all the participants in the Memory and Aging Project and the Rush Alzheimer’s Disease Center’s (RADC) Latino Core as well as the research assistants, Outreach and Recruitment staff as well as the Statistics and Data Management Core of the RADC. More information regarding obtaining data from the Rush Memory and Aging Project for research use can be found at the RADC Research Resource Sharing Hub (www.radc.rush.edu). Please note, this study was not preregistered.
Funding
This work was supported by the National Institute on Aging (grant numbers R01 AG062711, R01 AG17917, and P30 AG010161).
Conflict of Interest
None declared.
References
- Abraído-Lanza, A F, Armbrister, A N, Flórez, K R, & Aguirre, A N. (2006). Toward a theory-driven model of acculturation in public health research. American Journal of Public Health, 96(8), 1342–1346. doi: 10.2105/AJPH.2005.064980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraído-Lanza, A F, Echeverría, S E, & Flórez, K R. (2016). Latino immigrants, acculturation, and health: Promising new directions in research. Annual Review of Public Health, 37, 219–236. doi: 10.1146/annurev-publhealth-032315-021545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arvanitakis, Z, Wilson, R S, Li, Y, Aggarwal, N T, & Bennett, D A. (2006). Diabetes and function in different cognitive systems in older individuals without dementia. Diabetes Care, 29(3), 560–565. doi: 10.2337/diacare.29.03.06.dc05-1901 [DOI] [PubMed] [Google Scholar]
- Barnes, L L, Lewis, T T, Begeny, C T, Yu, L, Bennett, D A, & Wilson, R S. (2012). Perceived discrimination and cognition in older African Americans. Journal of the International Neuropsychological Society, 18(5), 856–865. doi: 10.1017/S1355617712000628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes, L L, Mendes de Leon, C F, Wilson, R S, Bienias, J L, & Evans, D A. (2004). Social resources and cognitive decline in a population of older African Americans and whites. Neurology, 63(12), 2322–2326. doi: 10.1212/01.wnl.0000147473.04043.b3 [DOI] [PubMed] [Google Scholar]
- Bennett, D A, Schneider, J A, Aggarwal, N T, Arvanitakis, Z, Shah, R C, Kelly, J F, Fox, J H, Cochran, E J, Arends, D, Treinkman, A D, & Wilson, R S. (2006). Decision rules guiding the clinical diagnosis of Alzheimer’s disease in two community-based cohort studies compared to standard practice in a clinic-based cohort study. Neuroepidemiology, 27(3), 169–176. doi: 10.1159/000096129 [DOI] [PubMed] [Google Scholar]
- Bennett, D A, Schneider, J A, Buchman, A S, Barnes, L L, Boyle, P A, & Wilson, R S. (2012). Overview and findings from the rush Memory and Aging Project. Current Alzheimer Research, 9(6), 646–663. doi: 10.2174/156720512801322663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett, D A, Schneider, J A, Tang, Y, Arnold, S E, & Wilson, R S. (2006). The effect of social networks on the relation between Alzheimer’s disease pathology and level of cognitive function in old people: A longitudinal cohort study. The Lancet. Neurology, 5(5), 406–412. doi: 10.1016/S1474-4422(06)70417-3 [DOI] [PubMed] [Google Scholar]
- Boyle, P A, Buchman, A S, Wilson, R S, Leurgans, S E, & Bennett, D A. (2009). Association of muscle strength with the risk of Alzheimer’s disease and the rate of cognitive decline in community-dwelling older persons. Archives of Neurology, 66(11), 1339–1344. doi: 10.1001/archneurol.2009.240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daviglus, M L, Pirzada, A, Durazo-Arvizu, R, Chen, J, Allison, M, Aviles-Santa, L, Cai, J., Gonzalez, H. M., Kaplan, R. C., Schniderman, N., Sorlie, P. D., Talavera, G. A., Wassertheil-Smoller, S., & Stamler, J. (2016). Prevalence of low cardiovascular risk profile among diverse Hispanic/Latino adults in the United States by age, sex, and level of acculturation: The Hispanic community health study/study of Latinos. Journal of the American Heart Association, 5(8), 1–17. doi: 10.1161/JAHA.116.003929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daviglus, M L, Talavera, G A, Avilés-Santa, M L, Allison, M, Cai, J, Criqui, M H, Gellman, M, Giachello, A L, Gouskova, N, Kaplan, R C, LaVange, L, Penedo, F, Perreira, K, Pirzada, A, Schneiderman, N, Wassertheil-Smoller, S, Sorlie, P D, & Stamler, J. (2012). Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. Journal of the American Medical Association, 308(17), 1775–1784. doi: 10.1001/jama.2012.14517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farias, S T, Mungas, D, Hinton, L, & Haan, M. (2011). Demographic, neuropsychological, and functional predictors of rate of longitudinal cognitive decline in Hispanic older adults. The American Journal of Geriatric Psychiatry, 19(5), 440–450. doi: 10.1097/JGP.0b013e3181e9b9a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores, I, Casaletto, K B, Marquine, M J, Umlauf, A, Moore, D J, Mungas, D, Gershon, R C, Beaumont, J L, & Heaton, R K. (2017). Performance of Hispanics and non-Hispanic whites on the NIH toolbox cognition battery: The roles of ethnicity and language backgrounds. The Clinical Neuropsychologist, 31(4), 783–797. doi: 10.1080/13854046.2016.1276216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gómez-Gallego, M, & Gómez-García, J. (2019). Stress and verbal memory in patients with Alzheimer’s disease: Different role of cortisol and anxiety. Aging & Mental Health, 23(11), 1496–1502. doi: 10.1080/13607863.2018.1506741 [DOI] [PubMed] [Google Scholar]
- Gonzales, M M, Durazo-Arvizu, R A, Sachdeva, S, Unterman, T G, O’Brien, M J, Gallo, L C, Talavera, G A, Kaplan, R C, Cai, J, Schneiderman, N, Espinoza Giacinto, R A, González, H M, Daviglus, M L, & Lamar, M. (2019). Associations of insulin resistance with cognition in individuals without diagnosed diabetes: Results from the Hispanic Community Health Study/Study of Latinos. Diabetes Research and Clinical Practice, 150, 38–47. doi: 10.1016/j.diabres.2019.01.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg, S. (2009). A profile of older Americans: 2009. Retrieved from http://www.aoa.gov/AoAroot/Aging_Statistics/Profile/2009/docs/2009profile_508.pdf;2009
- Haan, M N, Mungas, D M, Gonzalez, H M, Ortiz, T A, Acharya, A, & Jagust, W J. (2003). Prevalence of dementia in older Latinos: The influence of type 2 diabetes mellitus, stroke and genetic factors. Journal of the American Geriatrics Society, 51(2), 169–177. doi: 10.1046/j.1532-5415.2003.51054.x [DOI] [PubMed] [Google Scholar]
- Heffner, K L, Waring, M E, Roberts, M B, Eaton, C B, & Gramling, R. (2011). Social isolation, C-reactive protein, and coronary heart disease mortality among community-dwelling adults. Social Science & Medicine (1982), 72(9), 1482–1488. doi: 10.1016/j.socscimed.2011.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill, T D, Angel, J L, Balistreri, K S, & Herrera, A P. (2012). Immigrant status and cognitive functioning in late-life: An examination of gender variations in the healthy immigrant effect. Social Science & Medicine (1982), 75(12), 2076–2084. doi: 10.1016/j.socscimed.2012.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howrey, B T, Raji, M A, Masel, M M, & Peek, M K. (2015). Stability in cognitive function over 18 years: Prevalence and predictors among older Mexican Americans. Current Alzheimer Research, 12(7), 614–621. doi: 10.2174/1567205012666150701102947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazlauskaite, R, Janssen, I, Wilson, R S, Appelhans, B M, Evans, D A, Arvanitakis, Z, El Khoudary, S. M., & Kravitz, H M. (2020). Is midlife metabolic syndrome associated with cognitive function change? The study of women’s health across the nation. The Journal of Clinical Endocrinology and Metabolism, 105(4), e1093–e1105. doi: 10.1210/clinem/dgaa067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamar, M, Durazo-Arvizu, R A, Sachdeva, S, Pirzada, A, Perreira, K M, Rundek, T, Gallo, L C, Grober, E, DeCarli, C, Lipton, R B, Tarraf, W, González, H M, & Daviglus, M L. (2019). Cardiovascular disease risk factor burden and cognition: Implications of ethnic diversity within the Hispanic Community Health Study/Study of Latinos. PLoS One, 14(4), e0215378. doi: 10.1371/journal.pone.0215378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara, M, Gamboa, C, Kahramanian, M I, Morales, L S, & Bautista, D E. (2005). Acculturation and Latino health in the United States: A review of the literature and its sociopolitical context. Annual Review of Public Health, 26, 367–397. doi: 10.1146/annurev.publhealth.26.021304.144615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenze, E J, Mantella, R C, Shi, P, Goate, A M, Nowotny, P, Butters, M A, Andreescu, C, Thompson, P A, & Rollman, B L. (2011). Elevated cortisol in older adults with generalized anxiety disorder is reduced by treatment: A placebo-controlled evaluation of escitalopram. The American Journal of Geriatric Psychiatry, 19(5), 482–490. doi: 10.1097/JGP.0b013e3181ec806c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis, T T, Aiello, A E, Leurgans, S, Kelly, J, & Barnes, L L. (2010). Self-reported experiences of everyday discrimination are associated with elevated C-reactive protein levels in older African-American adults. Brain, Behavior, and Immunity, 24(3), 438–443. doi: 10.1016/j.bbi.2009.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis, T T, Barnes, L L, Bienias, J L, Lackland, D T, Evans, D A, & Mendes de Leon, C F. (2009). Perceived discrimination and blood pressure in older African American and white adults. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 64(9), 1002–1008. doi: 10.1093/gerona/glp062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Class, M, Castro, F G, & Ramirez, A G. (2011). Conceptions of acculturation: A review and statement of critical issues. Social Science & Medicine (1982), 72(9), 1555–1562. doi: 10.1016/j.socscimed.2011.03.011 [DOI] [PubMed] [Google Scholar]
- Lutsey, P L, Diez Roux, A V, Jacobs, D RJr, Burke, G L, Harman, J, Shea, S, & Folsom, A R. (2008). Associations of acculturation and socioeconomic status with subclinical cardiovascular disease in the multi-ethnic study of atherosclerosis. American Journal of Public Health, 98(11), 1963–1970. doi: 10.2105/AJPH.2007.123844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marín, G, Sabogal, F, VanOss Marín, B, Otero-Sabogal, F, & Pérez-Stable, E J. (1987). Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Sciences, 9, 183–205. doi: 10.1177/07399863870092005 [DOI] [Google Scholar]
- Marquez, D X, Glover, C M, Lamar, MLeurgansS E, Shah, R C, Barnes, L L, Aggarwal, N TBuchmanA S, & Bennett, D A(2020). Representation of older Latinxs in cohort studies at the Rush Alzheimer’s Disease Center. Neuroepidemiology. Advance online publication. doi: 10.1159/000509626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquine, M J, Segawa, E, Wilson, R S, Bennett, D A, & Barnes, L L. (2012). Association between cognitive activity and cognitive function in older Hispanics. Journal of the International Neuropsychological Society, 18(6), 1041–1051. doi: 10.1017/S135561771200080X [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKhann, G, Drachman, D, Folstein, M, Katzman, R, Price, D, & Stadlan, E M. (1984). Clinical diagnosis of Alzheimer’s disease: Report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology, 34(7), 939–944. doi: 10.1212/wnl.34.7.939 [DOI] [PubMed] [Google Scholar]
- Molina, K M, & Simon, Y. (2014). Everyday discrimination and chronic health conditions among Latinos: The moderating role of socioeconomic position. Journal of Behavioral Medicine, 37(5), 868–880. doi: 10.1007/s10865-013-9547-0 [DOI] [PubMed] [Google Scholar]
- Nilsson, K, Gustafson, L, & Hultberg, B. (2011). C-reactive protein level is decreased in patients with Alzheimer’s disease and related to cognitive function and survival time. Clinical Biochemistry, 44(14–15), 1205–1208. doi: 10.1016/j.clinbiochem.2011.07.011 [DOI] [PubMed] [Google Scholar]
- O’Bryant, S E, Johnson, L, Reisch, J, Edwards, M, Hall, J, Barber, R, Devous, M DSr, Royall, D, & Singh, M. (2013). Risk factors for mild cognitive impairment among Mexican Americans. Alzheimer’s & Dementia, 9(6), 622–631.e1. doi: 10.1016/j.jalz.2012.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padilla, R, Steiner, J F, Havranek, E P, Beaty, B, Davidson, A J, & Bull, S. (2011). A comparison of different measures of acculturation with cardiovascular risk factors in Latinos with hypertension. Journal of Immigrant and Minority Health, 13(2), 284–292. doi: 10.1007/s10903-010-9434-5 [DOI] [PubMed] [Google Scholar]
- Portes, A, & Zhou, M. (1992). Gaining the upper hand: Economic mobility among immigrant and domestic minorities. Ethnic and Racial Studies, 15, 491–522. doi: 10.1080/01419870.1992.9993761 [DOI] [Google Scholar]
- Ramírez, M, Teresi, J A, Holmes, D, Martínez, V, & Lantigua, R. (2007). Prevalence estimates and health-related correlates of cognitive impairment from a probability sample of community-residing Latino elders. Journal of Aging and Health, 19(4), 559–574. doi: 10.1177/0898264307304321 [DOI] [PubMed] [Google Scholar]
- Sabogal, F, Marin, G, & Otero-Sabogal, R. (1987). Hispanic familism and acculturation: What changes and what doesn’t?. Hispanic Journal of Behavioral Sciences, 9(4), 397–412. doi: 10.1177/07399863870094003 [DOI] [Google Scholar]
- Schwartz, S J, Unger, J B, Zamboanga, B L, & Szapocznik, J. (2010). Rethinking the concept of acculturation: Implications for theory and research. The American Psychologist, 65(4), 237–251. doi: 10.1037/a0019330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz, S J, Weisskirch, R S, Hurley, E A, Zamboanga, B L, Park, I J K, Kim, S Y, Umaña-Taylor, A, Castillo, L G, Brown, E, & Greene, A D. (2010). Communalism, familism, and filial piety: Are they birds of a collectivist feather? Cultural Diversity & Ethnic Minority Psychology, 16(4), 548–560. doi: 10.1037/a0021370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpao, M P, Espino, D V, Palmer, R F, Lichtenstein, M J, & Hazuda, H P. (2005). Association between acculturation and structural assimilation and Mini-Mental State Examination-assessed cognitive impairment in older Mexican Americans: Findings from the San Antonio Longitudinal Study of Aging. Journal of the American Geriatrics Society, 53(7), 1234–1239. doi: 10.1111/j.1532-5415.2005.53364.x [DOI] [PubMed] [Google Scholar]
- Sorlie, P D, Allison, M A, Avilés-Santa, M L, Cai, J, Daviglus, M L, Howard, A G, Kaplan, R, Lavange, L M, Raij, L, Schneiderman, N, Wassertheil-Smoller, S, & Talavera, G A. (2014). Prevalence of hypertension, awareness, treatment, and control in the Hispanic Community Health Study/Study of Latinos. American Journal of Hypertension, 27(6), 793–800. doi: 10.1093/ajh/hpu003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viruell-Fuentes, E A. (2007). Beyond acculturation: Immigration, discrimination, and health research among Mexicans in the United States. Social Science & Medicine (1982), 65(7), 1524–1535. doi: 10.1016/j.socscimed.2007.05.010 [DOI] [PubMed] [Google Scholar]
- Weden, M M, Miles, J N V, Friedman, E, Escarce, J J, Peterson, C, Langa, K M, & Shih, R A. (2017). The Hispanic paradox: Race/ethnicity and nativity, immigrant enclave residence and cognitive impairment among older US Adults. Journal of the American Geriatrics Society, 65(5), 1085–1091. doi: 10.1111/jgs.14806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams, D R, Yu, Y, Jackson, J S, & Anderson, N B. (1997). Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology, 2(3), 335–351. doi: 10.1177/135910539700200305 [DOI] [PubMed] [Google Scholar]
- Wilson, R S, Barnes, L L, Mendes de Leon, C F, Aggarwal, N T, Schneider, J S, Bach, J, Pilat, J., Becket, L. A., Arnold, S. E., Evans, D. A., & Bennett, D A. (2002). Depressive symptoms, cognitive decline, and risk of AD in older persons. Neurology, 59(3), 364–370. doi: 10.1212/WNL.59.3.364 [DOI] [PubMed] [Google Scholar]
- Wilson, R S, Krueger, K R, Arnold, S E, Schneider, J A, Kelly, J F, Barnes, L L, Tang, Y., & Bennett, D A. (2007). Loneliness and risk of Alzheimer’s disease. Archives of General Psychiatry, 64(2), 234–240. doi: 10.1001/archpsyc.64.2.234 [DOI] [PubMed] [Google Scholar]
- Wilson, R S, Scherr, P A, Schneider, J A, Tang, Y, & Bennett, D A. (2007). Relation of cognitive activity to risk of developing Alzheimer’s disease. Neurology, 69(20), 1911–1920. doi: 10.1212/01.wnl.0000271087.67782.cb [DOI] [PubMed] [Google Scholar]
- Xu, H, Zhang, Y, & Wu, B. (2017). Association between migration and cognitive status among middle-aged and older adults: A systematic review. BMC Geriatrics, 17(1), 184. doi: 10.1186/s12877-017-0585-2 [DOI] [PMC free article] [PubMed] [Google Scholar]