Abstract
Background:
Preterm birth is the most important in children under 5 yr mortality. In this study, we used the Global Burden of Disease Data (GBD) to evaluate the trend of preterm infant mortality rate for all countries from 1990 to 2017 and to assess the effect of development factors on this trend.
Methods:
The preterm infant mortality rate data from 196 countries of the world, from 1990 to 2017, were extracted from the GBD database. To study the trend of preterm infant mortality rate, a mixed-effects log-linear regression model was fitted separately for each IHME super-region. In the next step of data analysis, the development factor was included in the model to determine its effect on this trend for all countries under study.
Results:
The average rate mortality rate has declined about 2% per year throughout the world over the mentioned period. The highest and lowest decreasing trends were observed in high-income countries (about 4.0%) and Sub-Saharan Africa (about 1.0%), respectively. Including the effect of development factor in the mentioned model revealed that in 1990, the rate of preterm infant mortality in developed countries was 2.2 times of this rate in developing countries and this rate ratio has increased to 2.69 in year 2017.
Conclusion:
Although the preterm infant mortality rate were decreasing in all super regions, there is a remarkable gap in this rate between developing and developed countries yet. Therefore, preventative strategies are needed to reduce preterm birth and its burden, especially in the developing world.
Keywords: Global burden of disease, Preterm, Trend, Mixed-effects model, Log-linear regression
Introduction
Preterm, defined as childbirth happening before 37 completed weeks of gestational age, is one of the serious perinatal health problems worldwide (1, 2). It is the second leading cause of death among children under 5 yr old as well as a common cause of infant death in the first 12 h after birth (2,3). The neonate born at fewer than 37 weeks of this stage is known as preterm. Preterm birth is classified into three categories: mild pre-term (32–36 wk), very preterm (28–31 weeks) and extremely preterm (<28 wk) (4). The importance of this categorization is because of its direct association with disability of neonate, intensity of required neonatal care and the related costs. Variety of reasons such as medical conditions of mother or fetus, genetic influences, environmental exposure, infertility treatments, behavioral and socioeconomic factors and iatrogenic immaturity are attributed to the preterm birth (1). Preterm neonates are believed to have higher risk for long-term disorders like respiratory distress, apnea, seizures, jaundice and kernicterus than normal infants (5).
According to the WHO reports in 2012, 15 million babies are born preterm annually, and this is more than one in ten of all newborns (6). Based on a systematic review in 2009 the worldwide incidence of preterm birth brought the highest-burden for developing communities, especially African and Southern Asian regions. Surprisingly preterm birth has a high rate in North America too (1). Preterm birth is associated with over 75% of all perinatal mortality and more than 50% of perinatal and long-term morbidity. As it was estimated in 2010, complications of preterm birth cause almost 1.1 million death in children annually, and this trend is increasing according to the WHO reports (6,7).
The mortality rates (such as infant mortality rates) are varying at different times in different countries and geographical regions. Thus, evaluating this trend and its related factors seem to be crucial. To assess the trend of change in mortality rates, the data should be gathered repeatedly at different time points (longitudinally). Accordingly, appropriate statistical models should be utilized for analyzing these kinds of data sets. In this context, generalized mixed-effects models (GLMMs) are among the most common approaches due to their flexibility in accounting different levels within subject variability and considering different types of outcome variables including normal and non-normal response data (8). Although our literature review showed that there were several published papers about preterm infant birth and its mortality rate in different countries, the researchers could not find any published manuscript on assessing the trend of preterm infant mortality rate in the last two decades. Therefore, we aimed to assess the trend of mortality rates of preterm children under 5 yr old in all countries from 1990 to 2017 using the data from the GBD database.
Methods
In this study, the preterm infant mortality rates (per 100,000) were regarded as the main outcome under study for both gender and age-standardized groups from each country in all different regions from 1990 to 2017. The mortality rates were based on the online available database of GBD from the Institute for Health Metrics and Evaluation (IHME) Website estimated using various sources like vital registration systems, sample registration systems, household surveys (complete birth histories, summary birth histories, sibling histories), censuses (summary birth histories, household deaths), and Demographic Surveillance Sites. The world countries are classified into seven distinct parts, called super regions (Table 1) based on the IHME classification. To estimate the sex-specific probability of death, a spatiotemporal Gaussian process regression model (ST-GPR) is applied. This mixed effects model merges different data sources to get unified estimates of levels and trends by borrowing information across age, time, and locations. Besides, the developing factor (based on GBD database classification) was considered as the most important explanatory variable for preterm mortality rate in the statistical modelling process. Those countries with higher average level of well-being, are called developed countries. Classification of developing factor was based on World Bank that is by gross national income (GNI) per capita (9,10).
Table 1:
Estimates from the mixed effects log-linear regression model by IHME super regions adjusting for sex
| Region | Number of Countries | Intercept(SEa) | Slope(SE) | Random term variance (SE) |
|---|---|---|---|---|
| Southeast Asia, East Asia and Oceania | 23 | 2.710(0.125)* | −0.027(0.0009)a | 0.356(0.108)a |
| Central Europe, Eastern Europe and Central Asia | 29 | 2.030(0.138)* | −0.030(0.001)a | 0.528(0.145)a |
| High-income | 33 | 1.289(0.096) * | −0.035(0.001)a | 0.279(0.072)a |
| Latin America and Caribbean | 29 | 2.513(0.090) * | −0.027(0.0009)a | 0.230(0.062)a |
| North Africa and Middle East | 19 | 2.966(0.124) * | −0.039(0.0009)a | 0.289(0.097)a |
| South Asia | 6 | 3.279(0.170) * | −0.031(0.001)a | 0.171(0.109)a |
| Sub-Saharan Africa | 49 | 2.907(0.047) * | −0.018(0.0005)a | 0.105(0.022)a |
| Total | 188 | 2.384(0.059) * | −0.026(0.0003)a | 0.684(0.069)a |
P-value<0.05
Standard Error of the Estimate
The main objectives of this study were to assess the trend of the preterm mortality rate in all world countries and different IHME super regions, during the last two decades of the century, and to evaluate the effect of developing factor on this outcome during the years under study (11,12). According to the literature, since the mortality rate in boys appears to be higher than girls, the gender factor was included in the models as a predictor variable.
Statistical Approaches
The Generalized Linear Models (GLMs) have been proposed to unify the regression approaches for a wide variety of discrete and continuous longitudinal data. The GLMMs are extensions of GLMs in which the linear predictor contains random terms as well as the usual fixed effects. Inclusion of these two distinct parts in the model allows the data analysts to consider both the between-subject and within-subject sources of variation in the longitudinal responses (8).
Suppose Yij is the response for the ith sampling unit in jth occasion, β is a (p×1) vector of fixed effects, bi is a (q×1) vector of random effects, Xi is a (ni×p) matrix of covariates, Zi is a (ni×q) matrix of covariates, with q≤p and g(.) is the appropriate link function. The general form of a GLMM can be written as follows:
For a count response variable considering a log link function, the most common form of GLMMs is as follows:
To achieve the first objective of this study, (assessing the trend of the preterm mortality rate), the following random intercept GLMMs was utilized, separately for each super region and for all super regions:
where Pij is the population at risk in each country. Furthermore, to determine the effect of development on mortality rate from 1990 to 2017 in all 196 countries (second objective), the fitted GLMMs was as follows:
The statistical analyses were performed using the SAS Software, version 9.3.
Results
In general, annually preterm infant mortality rates (per 100,000) for 196 world countries from 1990 to 2017 were studied. A decreasing trend (slope) with different starting points in 1990 (intercepts) was seen in the trajectory plot of these countries, separately for each gender. Moreover, assessing the trend of changes in death rate for each gender and in each IHME super region revealed that South Asia had the highest intercept and slope and the high-income countries and North Africa and the Middle East had the lowest intercept and slope of preterm infant mortality rate during these years, respectively. Generally, a decreasing trend exists over this time in all regions.
To assess the trend of preterm infant mortality rate, a mixed-effects log-linear regression model was fitted separately for each IHME super region adjusting for sex (Table 1).
There is a natural heterogeneity among the countries within each IHME super regions in terms of their baseline rate of preterm infant mortality since the variance of random component was strongly significant in all super regions (P<0.001). The high-income countries had the lowest mean rate (e1.289=3.62) and the South Asian countries had the highest mean rate (e3.279=26.54) in the starting point of the study (year 1990). The negative sign for the estimates of all world slopes indicates a reduction in the preterm infant mortality rate over time from the starting tear of the study in all super regions. In Sub-Saharan Africa, for instance, the annual mean decrease in preterm infant mortality rate is less than 1% (e−0.018=0.98), which is the lowest decreasing slope and the highest decreasing slope was observed in North Africa and the Middle East (annual decrease of %4 or e−0.039=0.96). In other super regions, this trend had a relatively similar decreasing pattern, regions ranged %3 (e−0.027=.97) to %4 (e−0.035=.96) per year. The annual decline in preterm infant mortality rate was %3 (e−0.026=.97) from total world countries during this time.
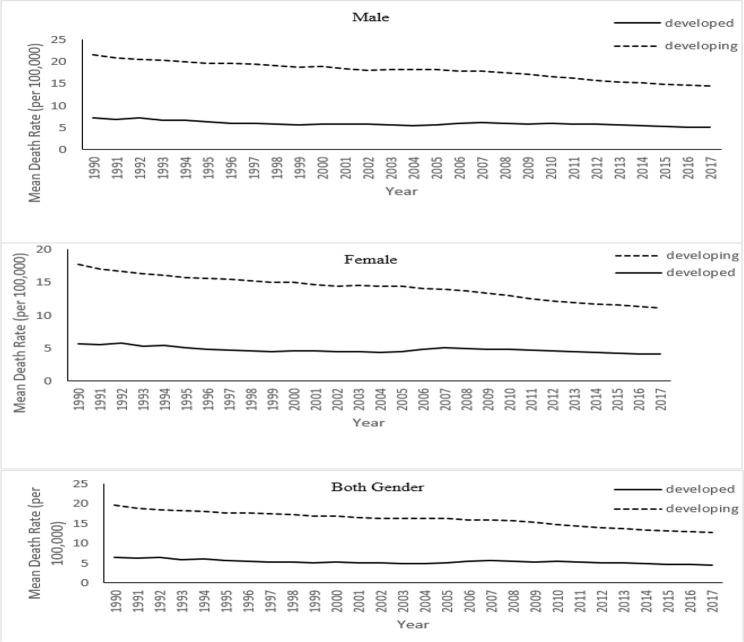
In the next step of data analysis, we aimed to assess the effect of developing on preterm infant mortality rate. Figure 1 displays the trend of pre-term infant mortality rate from 1990 to 2017 by sex, separately for the developing and developed countries. This figure gives us an intuitive justification for potential effect of developing factor on preterm infant mortality rate in this time. In the next step of data analysis, the effect of developing factors on preterm infant mortality rate was assessed by including this factor in a mixed-effects log-linear regression model (Equation 4).
Fig. 1:
Mean preterm infant mortality rate trajectories from 1990 to 2017 by developing factor for both genders
The significant variance of random term shows a remarkable heterogeneity in preterm mortality rates among these countries at the starting point of the study (Table 2).
Table 2:
Estimates from the mixed effects log-linear regression model
| Parameters | Estimate | Standard Error | P-value |
|---|---|---|---|
| Intercept | 2.479 | 0.062 | |
| Year | −0.034 | 0.001 | <0.001 |
| Sex | 0.227 | 0.005 | <0.001 |
| Development | −0.074 | 0.023 | 0.001 |
| Year * Development | 0.011 | 0.001 | <0.001 |
| Random term variance | 0.644 | 0.068 | <0.001 |
At the first glance, one can observe that the interaction between year and development factor was significant at 0.05 level (P<0.001). We report the rate ratio of preterm infant mortality rate in the developed to developing countries, separately for each year under study. Table 3 shows these rate ratios. Comparing the trend of preterm infant mortality rate shows that this trend was decreasing during the years under study both in the developed and developing countries. However, the reported rate ratios in Table 3 tell us that the gap between the developed and developing countries had an increasing trend during this time [from 2.2 in 1990 to 2.69 in 2017].
Table 3:
Estimated rate ratio (Developing countries/Developed countries) of preterm infant mortality from 1990 to 2017
| Year | 1990 | 1997 | 2004 | 2011 | 2017 |
|---|---|---|---|---|---|
| Rate ratio | 2.20 | 2.31 | 2.43 | 2.55 | 2.69 |
Discussion
About 13 million infants are born annually before 37 completed weeks of gestation worldwide. This may be the main reason for about one million neonatal deaths annually (13–15). These worrying statistics inspire the researchers to conduct more studies about preterm labor and its consequences. Although there are numerous published research about the prevalence and risk indicators of pre-term labor in different parts of the world, few articles are available about the long-term trend of infant mortality related to this health concern (1, 13–15).
We used the reported data from the GBD to present more detailed information about the trends of preterm infant mortality rate and compared these trends in the developed and developing countries in the last two decades. The obtained results from the present study comprise pleasant and unpleasant news. The good news is that the average rate of preterm infant mortality appeared to have a decreasing trend in the years under study (about 2% per year), whereas the presence of a considerable gap in preterm infant mortality rate between developed and developing countries is the bad news of this research (The rate ratio was 2.69 for both sex in 2017). Our findings of the decreasing trend of preterm infant mortality rate is in agreement with another study, conducted in year 2015, in which the researchers used the vital registration data reported by WHO and UN Inter-Agency Group for Child Mortality Estimation. The results of this study showed a decrease of 20%–30% in death from preterm labor in 2000–2013 although the preterm birth complications were the most important leading causes of neonatal mortality in that time (16). Despite the considerable promotion in the level of knowledge and practice of the mother and infant health care and medical technology development led to reduction in preterm infant mortality rate in recent years, it is still a major health problem in several parts of the world. More than 60% of preterm infant were born in South Asia and Sub-Saharan Africa from 1990 to 2010 (2). The high rates of preterm birth in these regions may be attributed to intrauterine infection and lack of access to primary medication such as tocolytic (1). Preterm birth rate is one of the indicators that highlight the apparent gap in maternal and peri-natal health care between developed and developing countries. In some developed countries, the preterm birth rate has a range differing from 5% to 7% in live births. Although this rate is substantially higher in developing countries, an unexpected upward trend could be seen in some developed countries, such as the United Kingdom, the United States and the Scandinavian countries during the last 20 years. This dramatic increasing rate may be attributed to some factors such as increasing rates of multiple births, higher rate of birth using the assisted reproductive techniques, increase in the proportion of births among women over 34 yr of age, and changes in clinical practices including the request for elective cesarean section and changes in the definitions of fetal loss, stillbirth and early neonatal death (1). In most developed countries, due to planned pregnancies and easy access to neonatal care, only very preterm babies are at risk of dying, and the survival rate of infants born at 32 weeks is similar to that of infants born at term (1, 11, 12); however, preterm birth has a destructive effect even at late gestational ages in developing countries (12). In the present study, the results obtained from the mixed-effects log-linear regression model showed 19% further reduction in girls' preterm infant mortality rate. In many parts of the world, the mortality rate in boys under 5 yr is higher than girls, except for some areas such as China, India, Nepal and Pakistan (17). The observed difference may be due to differences in genetic and biological structure, as boys are weaker biologically and at higher risk for diseases and preterm death (18).
In general, the observed decreasing trend of pre-term infant mortality rate in developed and developing countries in the period under study could be attributed to improvement in medical resources and rising the level of mothers' and health care providers' knowledge about the consequences of preterm labour all around the world.
Preterm infant mortality rate varies in different countries. More than 90% of babies who born extremely soon die within the first few days of life in low-income countries, and the majority of them die due to a lack of feasible and cost-effective care, while more than 75% of these pre-term babies can be saved with proper care. On the contrary, almost all of the preterm babies survive in high-income countries. The low-income countries should improve antenatal care for reducing preterm birth rates and they need to improve postnatal care for reducing preterm infant mortality rate. In addition, all pregnant women need to receive care that is more professional before, between and during pregnancies from healthcare facilities for safe delivery and having healthy baby (6).
Conclusion
There is a considerable gap in the preterm infant mortality rate between developing and developed countries. Due to the burden of preterm birth, postpartum care for mother and neonatal is needed with more care and intensity. Therefore, preventative strategies and health policies are needed to reduce preterm birth and its burden, especially in the developing world.
Acknowledgements
The authors appreciate the Institute for Health Metrics and Evaluation (IHME) for providing the data.
Footnotes
Conflict of interest
The authors declare that there is no conflict of interests.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
References
- 1.Beck S, Wojdyla D, Say L, et al. (2010). The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity Bull World Health Organ, 88(1):31–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blencowe H, Cousens S, Oestergaard MZ, et al. (2012). National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications Lancet, 379(9832):2162–72 [DOI] [PubMed] [Google Scholar]
- 3.Patel RM, Kandefer S, Walsh MC, et al. (2015). Causes and timing of death in extremely premature infants from 2000 through 2011 N Engl J Med, 372(4):331–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moutquin JM. (2003). Classification and heterogeneity of preterm birth. BJOG, 110 Suppl 20:30–3. [DOI] [PubMed] [Google Scholar]
- 5.Saigal S, Doyle LW. (2008). An overview of mortality and sequelae of preterm birth from infancy to adulthood Lancet, 371(9608):261–9 [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization (2012). 15 Million babies born too soon. Available from: https://www.who.int/mediacentre/news/releases/2012/preterm_20120502/en/
- 7.Simmons LE, Rubens CE, Darmstadt GL, et al. (2010). Preventing preterm birth and neonatal mortality: exploring the epidemiology, causes, and interventions, Semin Perinatol, 34(6):408–15. [DOI] [PubMed] [Google Scholar]
- 8.Fitzmaurice GM, Laird NM, Ware JH. (2012). Applied longitudinal analysis. 2nd ed. John Wiley & Sons, pp.: 395–401. [Google Scholar]
- 9.GBD 2017 Mortality Collaborators (2018). Global, regional, and national age-sex-specific mortality and life expectancy, 1950–2017: a systematic analysis for the Global Burden of Disease Study 2017 Lancet, 392(10159):1684–1735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.GBD 2016 Disease and Injury Incidence and Prevalence Collaborators (2017). Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016 Lancet, 390(10100):1211–1259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kramer MS. (2003). The epidemiology of adverse pregnancy outcomes: an overview J Nutr, 133(5):1592S–1596S. [DOI] [PubMed] [Google Scholar]
- 12.Ngoc NTN, Merialdi M, Abdel-Aleem H, et al. (2006). Causes of stillbirths and early neonatal deaths: data from 7993 pregnancies in six developing countries Bull World Health Organ, 84(9):699–705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chang HH, Larson J, Blencowe H, et al. (2013). Preventing preterm births: analysis of trends and potential reductions with interventions in 39 countries with very high human development index Lancet, 381(9862):223–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blencowe H, Cousens S, Chou D, et al. (2013). Born too soon: the global epidemiology of 15 million preterm births Reprod Health, 10(Suppl 1):S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lawn JE, Gravett MG, Nunes TM, et al. (2010). Global report on preterm birth and stillbirth (1 of 7): definitions, description of the burden and opportunities to improve data BMC Pregnancy and Childbirth, 10(Suppl 1):S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu L, Oza S, Hogan D, et al. (2015). Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: an updated systematic analysis Lancet, 385(9966):430–40 [DOI] [PubMed] [Google Scholar]
- 17.Gaimard M. (2013). Population and health in developing countries. Springer Science & Business Media, pp.: 48. [Google Scholar]
- 18.Pongou R. (2013). Why is infant mortality higher in boys than in girls? A new hypothesis based on preconception environment and evidence from a large sample of twins Demography, 50(2):421–44 [DOI] [PubMed] [Google Scholar]