Abstract
Firearm storage method is a potentially modifiable risk factor for suicide. Using data from a large, multi-state survey, we sought to determine whether there is an association between mental health and household firearm storage practices, and characterize that association by state of residence. Participants who endorsed the presence of a household firearm and answered the mental health questions in the 2016-2017 Behavioral Risk Factor Surveillance System from eight states were included (n=26,949). Exposures were recent poor mental health (≥14 vs. 0-13 days/past month), and diagnosis of depression. Outcomes were household firearm storage practices (loaded, and both loaded and unlocked). Using Poisson regression, we calculated adjusted prevalence ratios (aPR) overall and stratified by state of residence. Of adults endorsing a household firearm, 35.1% reported storing a firearm loaded, and of those, 53.4% reported that the firearm was both loaded and unlocked. Neither recent poor mental health nor depression was associated with loaded (aPR 1.14 [95% CI: 0.95-1.37] and aPR 0.94 [95% CI 0.80-1.09], respectively) or loaded and unlocked (aPR 1.08 [95% CI 0.88-1.42] and aPR 1.04 [95% CI 0.88-1.22], respectively) firearm storage. In the setting of highly prevalent loaded firearm storage, no differences in storage practices by mental health indicators were observed across eight states despite disparate firearm policies and local culture. The lack of difference in storage practices by mental health indicators across several states highlights an opportunity to improve means safety counseling practices, and the need for dedicated evaluation of state-level firearm storage policies.
Keywords: Injury prevention, firearm, means safety, suicide, mental health
INTRODUCTION
According to the Centers for Disease Control and Prevention (CDC), suicide was the 10th leading cause of death in the United States with 47,173 deaths in 2017.[1] Over 50% of deaths by suicide involve a firearm.[2] Firearm availability (the presence or absence of a firearm in the household)[3–5] and firearm storage practices [6–9] are both potentially modifiable risk factors for death by suicide.[3,9–11] Multiple studies have demonstrated no association between indicators of poor mental health and firearm availability[5,12,13]; however, the relationship between mental health status and firearm storage practices is less well-characterized.
Ecologic studies have demonstrated decreased rates of suicide death or firearm-related mortality associated with more stringent firearm legislation by state[14–16]. While there is evidence that specific state-level policies impact the rates of suicide and homicide by firearm[11,16–19], the mechanisms for these associations are unclear. Examining differences in firearm storage practices in those with and without markers of poor mental health may provide opportunities for suicide prevention. One study found no association between indicators of poor mental health and firearm storage practices [12], but as a single-state assessment, this may have limited generalizability to a broader population. Overall, little is known about the association between firearm storage practices and mental health across different states.
The relationship between mental health and firearm storage practices is made more complex by the presence of both overt mental health diagnoses, such as depression, and undiagnosed or sub-clinical poor mental health status that may contribute to increased risk of suicide death. Further, individuals reporting a diagnosis of depression may have well-controlled symptoms, and as such may not report recent poor mental health, which may impact their firearm storage choices.
Ideally, public policy could address firearm storage practices in households with both diagnosed and undiagnosed at-risk members in order to decrease suicide deaths by firearm. Individual states, however, differ widely in their attitudes and legislative approach to firearm availability and storage practices in the context of mental health. For example, by 2016 individual states differed widely in policies related to universal background checks, mandatory mental health reporting to a national database, safe storage regulations, child access prevention laws, firearm safety training, or risk-based (i.e., “red flag”) laws which allow family, law enforcement, and/or medical professionals to petition the court for removal of a firearm from an individual deemed to be a substantial danger to themselves or others.[20] Firearm safety training could encompass more of the at-risk population; however, mandatory training may only be required for a subset of firearm classes (as in Washington state), [20] and the content of the training program may not include education addressing suicide prevention and firearm storage practices.[21] In addition, though optional firearm safety courses are widely offered in states without mandatory training, uptake is limited and their utility is unclear.[21,22]
Given differences in state-level policy, unmeasured population characteristics, and cultural norms, it is possible that the association between mental health and firearm storage practices may differ based on state of residence. However, no study to our knowledge has characterized the association between mental health status and firearm storage across multiple states using statewide representative data.
Using data from the Behavioral Risk Factor Surveillance System (BRFSS), we sought to expand on findings from prior studies of mental health and firearm storage practices to include current data from multiple states, and characterize that relationship based on state of residence. The primary objective of this study was to determine whether the prevalence of firearm storage practices differs between those who do and do not report poor mental health or a depression diagnosis. As a secondary analysis, we sought to characterize this association by state of residence. Characterizing firearm storage practices in the context of both recent poor mental health and depression diagnosis allows for evaluation of firearm storage practices across a more complete spectrum of those at risk of firearm death. In addition, broad state-level characterizations may provide insight into state-level cultural and political landscapes which impact the local population.
METHODS
Data Sources and Study Population
The BRFSS is a state-administered survey supported by the CDC, which completes interviews with over 400,000 non-institutionalized adults age ≥ 18 years annually through random digit dialing including cell phone and land-line telephones. Responses are weighted using an iterative proportional fitting method to produce national and state representative samples.[23] We utilized BRFSS survey data from eight states that included an optional or state-added module regarding firearm availability and storage practices in either 2016 (Washington and New Mexico) or 2017 (Texas, Oregon, Idaho, Kansas, California, and Utah).[23] Participants who answered both the firearm and mental health questions in the BRFSS survey and reported a household firearm were included in the study. Participants who answered “Don’t know” or refused to answer the firearm, poor mental health days, or depression diagnosis questions were excluded.
Exposures and Outcomes
The exposures of interest were recent poor mental health (categorized as ≥ 14 days vs. 0–13 days in the past month)[12,24] and a prior diagnosis of depression (yes vs. no). The BRFSS question on recent poor mental health states, “Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?” The question on a diagnosis of depression states, “Has a doctor, nurse, or other health professional ever told you that you have a depressive disorder (including depression, major depression, dysthymia, or minor depression)?”
We defined two binary (yes vs. no) outcomes among participants: (1) presence of a loaded firearm in the household and (2) presence of a loaded and unlocked firearm in the household. The specific questions asked in the optional 2017 BRFSS Firearm Safety Module, the 2016 New Mexico State Firearm Safety Module, and the 2016 Washington State Firearm Safety Module are given in Figure S1. If respondents refused to answer or answered “No” to a question, then no further questions in the firearm module were asked.
Statistical Analysis
We used STATA/SE version 14 for data analysis (StataCorp LP, College Station, TX). Data were analyzed in 2019. BRFSS survey weights were applied for all analyses. Complete case analysis was used because missingness was less than 2% in all covariates. We calculated weighted percentages to describe demographic characteristics of groups categorized by recent mental health status and by depression diagnosis.
For the primary analysis assessing the association of mental health status with storage practices, we used univariable and multivariable Poisson regression models with robust standard errors to determine the crude and adjusted prevalence ratios and 95% CIs for each outcome. Covariates were chosen a priori based on reported associations with mental health status and firearm availability.[4,8,25–27] Adjusted analyses included the following covariates: age (18-24, 25-34, 35-44, 45-54, 55-64, ≥65 years), sex (male, female), race/ethnicity (white, Hispanic, black, Asian, American Indian/Alaskan Native, other), education level (less than a high school degree, high school degree, some college but no degree, college graduate), employment status (unemployed, employed, elective unemployment—students, homemakers, or retirees, unable to work), marital status (married or part of an unmarried couple, divorced or separated, widowed, never married), veteran status (yes, no), health care coverage (yes, no), and presence of at least one child in the household (yes, no). State of residence was included as a fixed effect in the models to account for potential differences in unmeasured confounders. In a secondary analysis, we further characterized the relationship between mental health status and firearm storage practices by stratifying on state of residence.
Per the University of Washington Human Subjects Division, this study did not involve human subjects research and therefore did not require IRB review.
RESULTS
Among the eight states that used the BRFSS firearm module in 2016 or 2017, there were 82,666 respondents, of whom 1,634 (2.0%) individuals refused to answer or answered “Don’t know/Not sure” to the questions on number of recent poor mental health days and/or diagnosis of depression (Figure 1). An additional 17,083 (20.7%) did not have a response to at least one firearm question; in this group, 897 (5.3%) answered “Don’t know/Not sure”, 3,743 (21.9%) refused to answer, and 12,443 (72.8%) were not selected for this module or discontinued the survey prior to reaching the module, leaving 63,949 participants who answered both the mental health questions and the firearm modules. Those who responded to the firearm module were slightly older, more likely to be female, and more likely to be white, compared to non-responders (Table S1). Amongst participants answering these modules, household firearms were common (weighted prevalence: 31.0% overall and ranging from 20.6% in California to 55.8% in Idaho).
Figure 1.
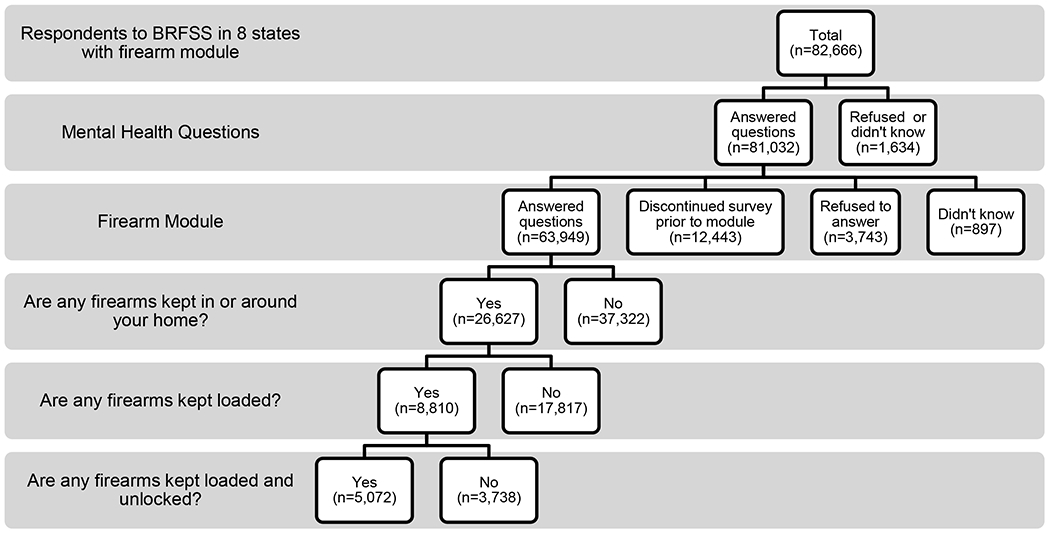
Number of respondents who answered each of the firearm module questions, Behavioral Risk Factors Surveillance System (BRFSS), 2016-2017. Per the BRFSS questionnaire, those who responded “No” to a question in the firearm module were asked no further questions in the module.
Respondent Demographics
Participants reporting recent poor mental health tended to be younger; predominantly female; unemployed or unable to work; and divorced, separated, or never married compared to those not reporting recent poor mental health. Those reporting a diagnosis of depression were more often middle-aged; predominantly female; white; unemployed or unable to work; and divorced or separated compared to those without a depression diagnosis (Table 1).
Table 1.
Demographic characteristics of U.S adults with household firearm access by mental health status, BRFSS, 2016-2017, n=26,627.
| Respondent Demographics | 0-13 Poor Mental Health Days, weighted percenta n=24,169 |
≥14 Poor Mental Health Days, weighted percenta n=2,458 |
No Depression Diagnosis, weighted percenta n=21,660 |
Depression Diagnosis, weighte percenta n=4,967 |
All, weighted percenta n=26,627 |
|---|---|---|---|---|---|
| Age, years | |||||
| 18-24 | 8.2 | 14.7 | 9.1 | 7.9 | 8.9 |
| 25-34 | 13.5 | 13.4 | 14.2 | 10.8 | 13.5 |
| 35-44 | 14.7 | 19.6 | 14.6 | 17.7 | 15.2 |
| 45-54 | 17.0 | 15.2 | 16.3 | 19.0 | 16.8 |
| 55-64 | 21.6 | 23.3 | 21.1 | 24.7 | 21.8 |
| ≥65 | 25.0 | 13.9 | 24.7 | 20.0 | 23.8 |
| Female | 58.8 | 54.2 | 38.3 | 61.1 | 42.6 |
| Race/Ethnicity | |||||
| White | 74.8 | 65.3 | 73.6 | 74.8 | 73.8 |
| Hispanic | 15.7 | 17.0 | 16.3 | 13.6 | 15.8 |
| Black | 4.6 | 7.2 | 4.7 | 5.5 | 4.9 |
| Asian | 1.8 | 3.8 | 2.1 | 1.6 | 2.0 |
| American Indian/Alaskan Native | 0.9 | 1.5 | 0.9 | 1.5 | 1.0 |
| Other | 2.2 | 5.2 | 2.4 | 3.1 | 2.5 |
| Education Level | |||||
| Less than high school | 5.5 | 6.2 | 5.6 | 5.3 | 5.5 |
| Completed high school or GED | 22.7 | 33.5 | 24.1 | 22.9 | 23.9 |
| Some college | 33.4 | 38.0 | 31.8 | 42.7 | 33.9 |
| Completed college | 38.4 | 22.3 | 38.5 | 29.1 | 36.7 |
| Employment Status | |||||
| Unemployed | 3.7 | 6.9 | 3.2 | 7.9 | 4.1 |
| Employed | 62.0 | 48.2 | 63.6 | 47.0 | 60.5 |
| Elective unemploymentb | 31.6 | 25.1 | 30.9 | 30.8 | 30.9 |
| Unable to work | 2.7 | 19.8 | 2.3 | 14.3 | 4.5 |
| Marital Status | |||||
| Married/Unmarried couple | 67.9 | 54.2 | 66.5 | 66.5 | 66.5 |
| Divorced/Separated | 11.2 | 15.2 | 11.2 | 13.5 | 11.7 |
| Widowed | 4.9 | 7.2 | 4.9 | 6.0 | 5.1 |
| Never married | 16.0 | 23.4 | 17.4 | 13.9 | 16.8 |
| Veteran | 17.2 | 17.8 | 17.7 | 15.5 | 17.3 |
| Any health insurance | 91.6 | 83.3 | 90.5 | 91.7 | 90.7 |
| At least one child in household | 33.6 | 37.0 | 33.6 | 35.6 | 34.0 |
| State of residence | |||||
| California | 31.0 | 33.8 | 31.4 | 30.6 | 31.3 |
| Idaho | 4.2 | 3.6 | 4.1 | 4.3 | 4.1 |
| Kansas | 5.9 | 4.7 | 5.8 | 5.7 | 5.8 |
| New Mexico | 1.2 | 1.3 | 1.2 | 1.1 | 1.2 |
| Oregon | 7.0 | 8.4 | 6.7 | 8.7 | 7.1 |
| Texas | 40.0 | 38.7 | 40.2 | 38.3 | 39.8 |
| Utah | 6.9 | 5.6 | 6.6 | 7.3 | 6.7 |
| Washington | 3.9 | 4.0 | 3.9 | 3.9 | 3.9 |
Weighted percentages exclude missing values. All covariates with 0-2% missingness. Number of missing values were: age, 0; female, 12; race/ethnicity, 0; education level, 49; employment status, 131; marital status, 76; veteran, 21; health insurance, 71; child in the household, 55; and state residence, 0.
Includes students, homemakers, and retirees.
Association of mental health status with firearm storage practices
Of adults who reported presence of a household firearm, 35.1% reported storing a firearm loaded. Of those who reported storing a firearm loaded, 53.4% reported that the firearm was both loaded and unlocked. There were no associations between recent poor mental health or depression diagnosis with household presence of a loaded firearm (Figure 2, Table S2) or presence of a loaded and unlocked firearm (Figure 3, Table S3) after adjusting for potential confounders. There was no evidence that the association between reported recent poor mental health or depression diagnosis, and storing a firearm loaded, or unlocked and loaded varied by state of residence as shown in figures 2 and 3, respectively (Table S2 & S3).
Figure 2.
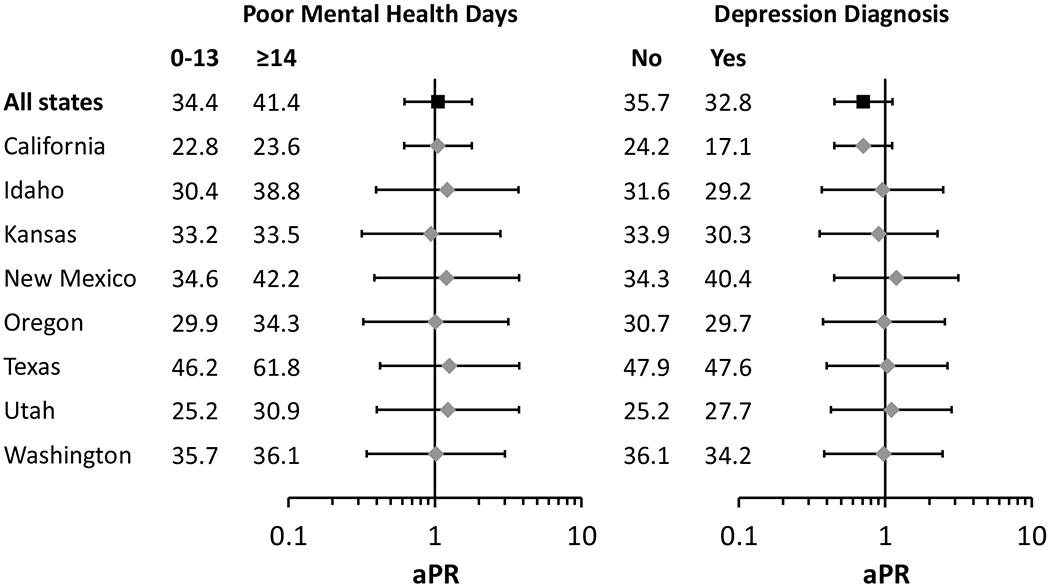
Association of recent poor mental health and depression diagnosis with presence of a loaded household firearm (n=26,627), Behavioral Risk Factors Surveillance System, 2016-2017. Numbers represent weighted prevalence of individuals reporting the presence of a loaded household firearm for each exposure group. Prevalence ratios (aPR) adjusted for age, sex, race/ethnicity, education level, employment status, marital status, veteran status, health insurance status, and presence of at least one child in the household.
Figure 3.
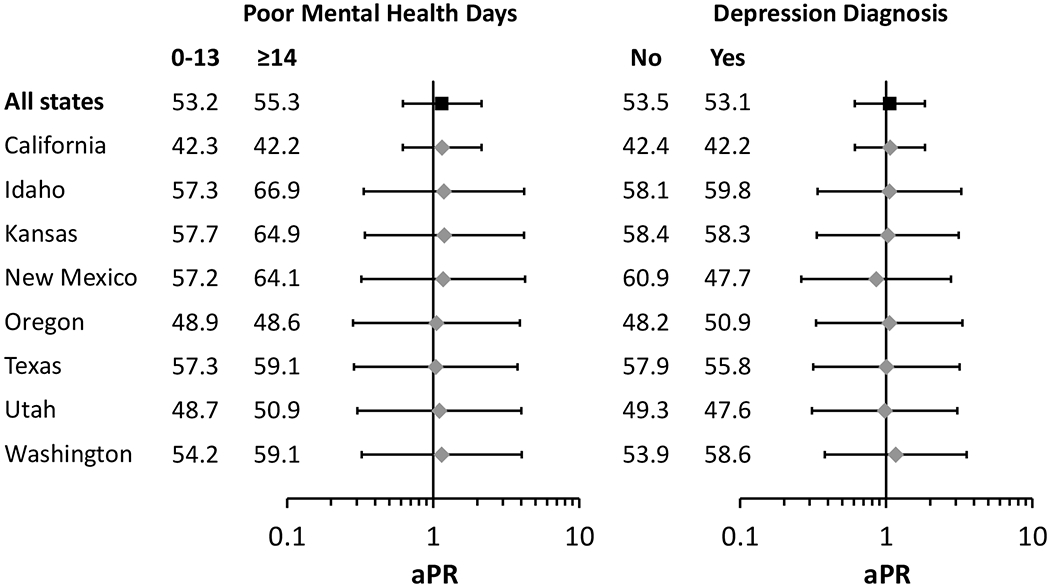
Association of recent poor mental health and depression diagnosis with presence of a loaded and unlocked household firearm, among those reporting presence of a loaded household firearm (n=8,810), Behavioral Risk Factors Surveillance System, 2016-2017. Numbers represent weighted prevalence of individuals reporting the presence of a loaded and unlocked household firearm for each exposure group. Prevalence ratios (aPR) adjusted for age, sex, race/ethnicity, education level, employment status, marital status, veteran status, health insurance status, and presence of at least one child in the household.
DISCUSSION
To our knowledge, this is one of the first multi-state studies to evaluate the relationship between mental health and firearm storage practices using contemporary BRFSS data. In our eight-state sample, we found no differences in household firearm storage practices between those with poor mental health or a depression diagnosis and those without either in aggregate or when stratified by state of residence. This is particularly concerning in the setting of the high proportion of household firearms stored loaded, or loaded and unlocked.
Our findings echo the single-state analysis of firearm storage practices and suicide risk factors in Washington.[12] It expands upon the existing literature by including a multi-state assessment and by elucidating firearm storage practices in the specific subset of those with poor mental health and with depression diagnoses. The lack of difference in the association between storage practices and mental health between states is similar to a separate study focusing on households with small children.[28] Though Prickett et al found no difference in storage practices when comparing households in states with and without child access prevention laws, they did note differences in firearm safety practices among a subset of states that had both stringent firearm legislation and child access prevention laws.[28] This highlights the complexity of the role of unmeasured state-level characteristics and relevant policy in this type of analysis.
Both the American Academy of Child and Adolescent Psychiatry[29] and the American Psychiatric Association[30] guidelines on suicide assessment and management recommend screening for presence of a firearm and counseling on lethal means safety, defined as reducing access to, or increasing safe storage of, potentially lethal methods for suicide. Given that an individual must have been evaluated by a mental health or medical provider to receive a diagnosis of depression and in light of these recommendations, we expected to find differences in firearm storage practices in households with versus without individuals reporting that they had been evaluated for a mental health concern and received a diagnosis of depression. Conversely, those experiencing recent poor mental health may not have the opportunity to undergo evaluation by a mental health or medical provider but may still be at increased of risk of firearm death.
Limitations
This study is subject to some of the limitations inherent to the use of large-scale survey data. Key considerations include the potential for recall and social desirability bias, especially in the setting of a high percentage of non-respondents to the firearm module. The firearm module was one of the last modules on the BRFSS questionnaire; as a result, most non-respondents likely did not respond due to survey fatigue, rather than refusing to answer questions on firearms. However, some survey participants specifically refused to answer the firearm module, which may have introduced response bias. In a study on responses to firearm questionnaires, female respondents were less likely to report household firearm availability or unsafe storage.[27] In our analysis, we controlled for sex in order to mitigate this effect, though some residual bias may remain, particularly given the higher proportion of female respondents reporting recent poor mental health and depression diagnoses. The effect of firearm ownership attitudes is also thought to reduce response rate overall and to be associated with underreporting in surveys, though data are somewhat limited.[31] It is unclear what effect this would have on responses to storage-specific questions. In addition, BRFSS asks about presence of a household firearm, and the individual completing the survey may not be aware of a household firearm or the method of storage; similarly, BRFSS focuses specifically on the mental health of the individual completing survey, while the mental health of other household members may influence firearm storage, which we were unable to account for. Additionally, the questionnaire item format in the BRFSS firearm module limits analysis of storage practices, as it does not provide the ability to distinguish between all permutations of storing a firearm unlocked or loaded. Changing the question format to better delineate these categories (as has been implemented in the Washington State questionnaire) could allow for a more specific analysis of policy and intervention effects in the future.
Both recent poor mental health and depression diagnosis were used as surrogates for mental health status, however, accurate ascertainment of mental health via surveys is challenging. In particular, BRFSS data have been shown to underestimate the prevalence of severe depression.[32] This may be in part due to those with a diagnosis of depression or more severe symptoms being less likely to participate in general. Both self-reported recent poor mental health and depression diagnoses may be subject to underreporting due to social desirability bias—this may be more pronounced in those with a household firearm or unsafe storage practices. Additionally, results from mental health-related questions differ between self-administered and telephone administered questionnaires with lower endorsement of depression and depressive symptoms in interviewer-administered settings.[33] This may lead to further under-reporting of poor mental health in our study. This survey data also does not address the potential for poor mental health of other household members who, if affected, may also be at higher risk of death by firearm.[3]
Though this study is more generalizable than other studies which focus on a single state, the states that asked the firearm modules are predominately in the western United States and may not be generalizable to populations outside of those surveyed. Encouraging more states to include the firearm module in future editions of the BRFSS or including it as a core module would aid in improved generalizability. In addition, the study was not adequately powered to formally test differences in storage practices by mental health status across different states. However, the point estimates for that association across states were quite similar suggesting no meaningful differences.
There are complex population characteristics that contribute to a community’s attitudes toward both mental health and firearms. With regard to policy, our findings highlight an opportunity to further evaluate the efficacy of current policies and practices relating to mental health and firearm storage. At the time this survey was completed, state-level legislation specifically addressing means safety in the setting of poor mental health was limited and often only tangentially related (i.e. mandatory firearms training which included means safety in the setting of at-risk persons). It should be noted that the policies highlighted here reflect legislation at the time the surveys were conducted, and policies have continued to evolve. The stringency of state level firearm legislation may be a surrogate for more ingrained firearm attitudes and culture. Other studies have suggested that only select firearm laws are associated with reduced firearm mortality including suicide death. Our study highlights a need to further evaluate and strengthen policies surrounding firearm storage practices. Assessment of not only firearms deaths, but of the intermediate step of firearm storage is important to better understand the impacts of targeted interventions at state, community, and individual levels.
Our findings are particularly concerning for those with a depression diagnosis as a formal assessment by a medical provider is necessary to obtain the diagnosis, and clinical practice recommendations include screening for and counseling regarding firearm availability and storage.[29,30,34] The lack of difference in storage practices between those with and without a diagnosis of depression suggests the need for further research evaluating both the receipt and effectiveness of means safety assessment and education for patients diagnosed with depression.
This study provides impetus for refinement of BRFSS firearm questions to include separate questions on presence of unlocked or loaded firearms in the household allowing for more specific analysis of firearm storage practices. Our study also suggests the need for critical assessment of current practices surrounding mental health diagnosis and firearm means safety counseling. It provides a model for analysis of firearm storage as an intermediate step to firearm death in a population of those with poor mental health and demonstrates a potential application for this type of model in state-level policy development and assessment. Most importantly, this study speaks to the need for comprehensive regular assessments of household firearm storage practices, particularly in those with poor mental health, to create data-driven policy and practical solutions.
Supplementary Material
ACKNOWLEDGEMENTS
Dara L. Horn was supported by the National Institutes of Health T-32 Postdoctoral Research Fellowship in Trauma and Burns [5T32GM121290].
Elissa K. Butler was supported by the National Institutes of Health T-32 Pediatric Injury Research Training Program [5T32HD057822-10].
Jessica L. Stahl was supported by the National Institutes of Health T-32 Pediatric Nephrology Training Program [5T32DK007662-28].
Ali Rowhani-Rahbar has no conflict of interests or financial disclosures.
Alyson J. Littman has no conflict of interests or financial disclosures.
Footnotes
The research and conclusions presented in this paper are those of the authors and do not reflect the official policy of the NIH. The authors attest that this study has not been previously presented elsewhere.
REFERENCES
- 1.Centers for Disease Control. 10 Leading Causes of Death by Age Group , United States – 2009. https://www.cdc.gov/injury/images/lc-charts/leading_causes_of_death_by_age_group_2017_1100w850h.jpg. Published 2009. Accessed April 3, 2020.
- 2.Center for Health Statistics N. National Vital Statistics Reports Volume 67, Number 5, July 26, 2018.; 2016. https://www.cdc.gov/nchs/data/nvsr/nvsr67/nvsr67_05.pdf. Accessed April 6, 2020.
- 3.Anglemyer A, Horvath T, Rutherford G. The Accessibility of Firearms and Risk for Suicide and Homicide Victimization Among Household Members. Ann Intern Med. 2014;160(2):101–110. doi: 10.7326/M13-1301 [DOI] [PubMed] [Google Scholar]
- 4.Miller M, Warren M, Hemenway D, Azrael D. Firearms and suicide in US cities. Inj Prev. 2015;21:e116–e119. doi: 10.1136/injuryprev-2013-040969 [DOI] [PubMed] [Google Scholar]
- 5.Miller M, Barber C, Azrael D, Hemenway D, Molnar BE. Recent psychopathology, suicidal thoughts and suicide attempts in households with and without firearms: Findings from the National Comorbidity Study Replication. Inj Prev. 2009;15(3):183–187. doi: 10.1136/ip.2008.021352 [DOI] [PubMed] [Google Scholar]
- 6.Khazem LR, Houtsma C, Gratz KL, Tull MT, Green BA, Anestis MD. Firearms matter: The moderating role of firearm storage in the association between current suicidal ideation and likelihood of future suicide attempts among united states military personnel. Mil Psychol. 2016;28(1):25–33. doi: 10.1037/mil0000099 [DOI] [Google Scholar]
- 7.Shenassa ED, Rogers ML, Spalding KL, Roberts MB. Safer storage of firearms at home and risk of suicide: A study of protective factors in a nationally representative sample. J Epidemiol Community Health. 2004;58(10):841–848. doi: 10.1136/jech.2003.017343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Horwitz AG, Smith DL, Held P, Zalta AK. Characteristics of Veteran and Civilian Suicide Decedents: A Sex-Stratified Analysis. Am J Prev Med. 2019;56(5):e163–e168. doi: 10.1016/j.amepre.2018.11.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grossman DC, Mueller BA, Riedy C, et al. Gun storage practices and risk of youth suicide and unintentional firearm injuries. J Am Med Assoc. 2005;293(6):707–714. doi: 10.1001/jama.293.6.707 [DOI] [PubMed] [Google Scholar]
- 10.Monuteaux MC, Azrael D, Miller M. Association of Increased Safe Household Firearm Storage with Firearm Suicide and Unintentional Death among US Youths. JAMA Pediatr. 2019;173(7):657–662. doi: 10.1001/jamapediatrics.2019.1078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anestis MD, Anestis JC. Suicide rates and state laws regulating access and exposure to handguns. Am J Public Health. 2015;105(10):2049–2058. doi: 10.2105/AJPH.2015.302753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morgan ER, Gomez A, Rowhani-Rahbar A. Firearm Ownership, Storage Practices, and Suicide Risk Factors in Washington State, 2013–2016. Am J Public Health. 2018;108(7):882–888. doi: 10.2105/AJPH.2018.304403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sorenson SB, Vittes KA. Mental Health and Firearms in Community-Based Surveys. Eval Rev. 2008;32(3):239–256. doi: 10.1177/0193841X08315871 [DOI] [PubMed] [Google Scholar]
- 14.Anestis MD, Houtsma C, Daruwala SE, Butterworth SE. Firearm legislation and statewide suicide rates: The moderating role of household firearm ownership levels. Behav Sci Law. May 2019:bsl.2408. doi: 10.1002/bsl.2408 [DOI] [PubMed] [Google Scholar]
- 15.Madhavan S, Taylor JS, Chandler JM, Staudenmayer KL, Chao SD. Firearm Legislation Stringency and Firearm-Related Fatalities among Children in the US. J Am Coll Surg. 2019;229(2):150–157. doi: 10.1016/j.jamcollsurg.2019.02.055 [DOI] [PubMed] [Google Scholar]
- 16.Siegel M, Pahn M, Xuan Z, Fleegler E, Hemenway D. The Impact of State Firearm Laws on Homicide and Suicide Deaths in the USA, 1991–2016: a Panel Study. J Gen Intern Med. March 2019. doi: 10.1007/s11606-019-04922-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stanley IH, Hom MA, Rogers ML, Anestis MD, Joiner TE. Discussing Firearm Ownership and Access as Part of Suicide Risk Assessment and Prevention: “Means Safety” versus “Means Restriction.” Arch Suicide Res. 2017;21(2):237–253. doi: 10.1080/13811118.2016.1175395 [DOI] [PubMed] [Google Scholar]
- 18.Anestis MD, Houtsma C, Daruwala SE, Butterworth SE. Firearm legislation and statewide suicide rates: The moderating role of household firearm ownership levels. Behav Sci Law. 2019;37(3):270–280. doi: 10.1002/bsl.2408 [DOI] [PubMed] [Google Scholar]
- 19.Alban RF, Nuño M, Ko A, Barmparas G, Lewis A V, Margulies DR. Weaker gun state laws are associated with higher rates of suicide secondary to firearms. J Surg Res. 2018;221:135–142. doi: 10.1016/j.jss.2017.08.027 [DOI] [PubMed] [Google Scholar]
- 20.Cherney S, Morral A, Schell T, Smucker S. RAND State Firearm Law Database. RAND State Firearm Law Database. doi: 10.7249/tl283-1 [DOI] [Google Scholar]
- 21.Rowhani-Rahbar A, Lyons VH, Simonetti JA, Azrael D, Miller M. Formal firearm training among adults in the USA: Results of a national survey. Inj Prev. 2018;24(2):161–165. doi: 10.1136/injuryprev-2017-042352 [DOI] [PubMed] [Google Scholar]
- 22.Berrigan J, Azrael D, Hemenway D, Miller M. Firearms training and storage practices among US gun owners: A nationally representative study. Inj Prev. 2019:injuryprev-2018-043126. doi: 10.1136/injuryprev-2018-043126 [DOI] [PubMed] [Google Scholar]
- 23.CDC - About BRFSS. https://www.cdc.gov/brfss/about/index.htm. Accessed April 10, 2020.
- 24.Borawski E, Wu G, Jua H. Substance Abuse and Mental Health Services Administration, Centers for Disease Control and Prevention: Self-reported frequent mental distress among adults--United States, 1993–1996. MMWR. 1998;47(16):325–331. [Google Scholar]
- 25.Li Z, Page A, Martin G, Taylor R. Attributable risk of psychiatric and socio-economic factors for suicide from individual-level, population-based studies: A systematic review. Soc Sci Med. 2011;72:608–616. doi: 10.1016/j.socscimed.2010.11.008 [DOI] [PubMed] [Google Scholar]
- 26.Miller M, Lippmann SJ, Azrael D, Hemenway D. Household Firearm Ownership and Rates of Suicide Across the 50 United States. J Trauma Inj Infect Crit Care. 2007;62(4):1029–1035. doi: 10.1097/01.ta.0000198214.24056.40 [DOI] [PubMed] [Google Scholar]
- 27.Azrael D, Miller M, Hemenway D. Are household firearms stored safely? It depends on whom you ask. Pediatrics. 2000;106(3):E31. [DOI] [PubMed] [Google Scholar]
- 28.Prickett KC, Martin-Storey A, Crosnoe R. State firearm laws, firearm ownership, and safety practices among families of preschool-aged children. Am J Public Health. 2014;104(6):1080–1086. doi: 10.2105/AJPH.2014.301928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dunnt JE, Arnold V, Scott Benson R, et al. Summary of the Practice Parameters for the Assessment and Treatment of Children and Adolescents With Suicidal Behavior. J Am Acad Child Adolesc Psychiatry. 2001;40(4):495–499. doi: 10.1097/00004583-200104000-00024 [DOI] [PubMed] [Google Scholar]
- 30.Practice Guideline for the Assessment and Treatment of Patients With Suicidal Behaviors. In: APA Practice Guidelines for the Treatment of Psychiatric Disorders: Comprehensive Guidelines and Guideline Watches. Arlington, VA: American Psychiatric Association; 2007. doi: 10.1176/appi.books.9780890423363.56008 [DOI] [Google Scholar]
- 31.Rafferty AP, Thrush JC, Smith PK, McGee HB. Validity of a household gun question in a telephone survey. Public Health Rep. 110(3):282–288. [PMC free article] [PubMed] [Google Scholar]
- 32.Frankel MR, Battaglia MP, Balluz L, Strine T. When data are not missing at random: implications for measuring health conditions in the Behavioral Risk Factor Surveillance System. BMJ Open. 2012;2(4):e000696. doi: 10.1136/bmjopen-2011-000696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hoebel J, von der Lippe E, Lange C, Ziese T. Mode differences in a mixed-mode health interview survey among adults. Arch Public Heal. 2014;72(1):46. doi: 10.1186/2049-3258-72-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Steele IH, Thrower N, Noroian P, Saleh FM. Understanding Suicide Across the Lifespan: A United States Perspective of Suicide Risk Factors, Assessment & Management. J Forensic Sci. 2018;63(1):162–171. doi: 10.1111/1556-4029.13519 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


