Abstract
Objective:
To examine the distinctiveness and significance of two body image constructs, dissatisfaction with weight and shape and overvaluation of weight and shape, with respect to eating disorder psychopathology, weight, and depression in White and Latinx/Hispanic men and women.
Methods:
Participants were White (n=1941) and Latinx/Hispanic (n=568) adults living in the United States who completed an online battery of established measures of body image, eating disorder psychopathology and behaviors, and depression.
Results:
Two body image constructs, dissatisfaction with weight and shape and overvaluation of weight and shape, were related to each other but showed some important distinctions in their associations with eating/weight-related variables. Significantly greater proportions of White than Latinx/Hispanic individuals reported co-occurring dissatisfaction and overvaluation, and significantly greater proportions of Latinx/Hispanic than White individuals reported dissatisfaction alone. Ethnicity moderated the association of dissatisfaction and overvaluation with BMI, and the association of overvaluation with depression; ethnicity also had a main effect on binge eating frequency.
Conclusions:
Dissatisfaction and overvaluation were distinct among both Latinx/Hispanic and White individuals. However, associations with eating/weight-related variables varied between ethnicities, suggesting a need for further research on the influence of cultural variables on body image and eating disorder psychopathology.
Keywords: body image, eating disorders, obesity, disordered eating, ethnicity, gender, Latinx/Hispanic
Introduction
Body image is a complex cognitive schema for how individuals perceive their appearance (Cash, 2004) and body image disturbance is a key driver of maladaptive eating and weight-related behaviors (Fairburn, Cooper, & Shafran, 2003). Body image disturbance consists of several unique facets, including dissatisfaction and overvaluation of weight and shape (Lydecker, White, & Grilo, 2017). Dissatisfaction refers to negative attitudes about one’s weight or shape (Fairburn & Cooper, 1993) and is commonly observed across age, gender, race, ethnicity, and weight status, although women and individuals with overweight/obesity experience the most body dissatisfaction (Schwartz & Brownell, 2004; Tiggemann, 2004; Wildes, Emery, & Simons, 2001). Body dissatisfaction is positively associated with several adverse psychosocial comorbidities, including depression (Ohring, Graber, & Brooks-Gunn, 2002), anxiety (Friederich et al., 2010), and disordered eating (Mond & Hay, 2011). Overvaluation occurs when shape or weight has an excessive influence on self-evaluation. Overvaluation is considered to be core cognitive psychopathology across eating disorders and is reliably positively associated with psychosocial impairment (Fairburn et al., 2003; Grilo et al., 2008; Tabri et al., 2015).
Dissatisfaction and overvaluation are distinct concepts (Grilo, 2013). For example, Mitchison and colleagues (2017) demonstrated that in boys, dissatisfaction and overvaluation have similar positive associations with psychological distress, while in girls, overvaluation is more strongly, positively associated with psychological distress than dissatisfaction. Previous research has also described some gender differences, with greater body dissatisfaction and overvaluation in girls than boys (Feingold & Mazzella, 1998; Mitchison et al., 2017; Schwartz & Brownell, 2004; Van den Berg et al., 2007). Emerging research supports that overvaluation and dissatisfaction are positively associated with different facets of eating disorder psychopathology among individuals with binge-eating disorder (Lydecker et al., 2017; Masheb & Grilo, 2003), anorexia nervosa (Calugi & Dalle Grave, 2019; Grilo, Crosby, & Machado, 2019), bulimia nervosa (Grilo, Crosby, et al., 2019; Grilo, Ivezaj, Lydecker, & White, 2019) and overweight/obesity (Dalle Grave, Misconel, Fasoli, & Calugi, 2020; Grilo, Ivezaj, et al., 2019). Grilo, Ivezaj and colleagues (2019) demonstrated a severity gradient in the degree of reported dissatisfaction and overvaluation between people with bulimia nervosa, binge-eating disorder, and overweight/obesity. Specifically, individuals with bulimia nervosa reported the greatest dissatisfaction and overvaluation, followed by individuals with binge-eating disorder, followed by individuals with overweight or obesity. Across the different groups, dissatisfaction was associated most strongly with body mass index (BMI), while overvaluation was associated most strongly with depression. Overvaluation was not associated significantly with BMI in patients with anorexia nervosa (Grilo, Crosby, et al., 2019), but this may be attributed to a restricted range of BMIs. In a clinical-research sample of patients seeking treatment for binge-eating disorder (Lydecker et al., 2017), neither overvaluation nor dissatisfaction were associated significantly with BMI, although both were positively associated with poor self-esteem, depressive symptoms, and eating concerns. Longitudinally, overvaluation has been shown to have a prospective association with binge-eating frequency across eating disorder diagnoses and in community samples, whereas dissatisfaction did not have any significant associations in clinical samples (Askew et al., 2020; Sharpe et al., 2018). Moreover, among patients with binge-eating disorder, changes over treatment in body dissatisfaction have been associated with changes in depressive symptomatology and self-esteem, whereas changes in overvaluation have been associated with only changes in self-esteem (Masheb & Grilo, 2003). This suggests that associations of dissatisfaction and overvaluation with eating/weight-related variables vary across clinical conditions, but it remains relatively unknown whether associations vary across other patient characteristics, including ethnicity.
Positive associations between body image disturbance and eating disorder psychopathology and depression can be explained by the sociocultural model of body image disturbance (Thompson, Heinberg, Altabe, & Tantleff-Dunn, 1999; Thompson & Stice, 2001), which suggests that negative consequences arise when an individual’s perceived body shape or size differs from internalized cultural messages regarding ideal body shape or size. At present, the majority of studies examining the distinctiveness of body image facets have focused primarily on differences between individuals with eating disorder diagnoses and consisted of primarily White samples (Cash & Smolak, 2011), although there is some diversity in nationality (e.g., Grilo, Crosby, et al., 2019). It is unknown whether there are differential associations between body image constructs and eating disorder psychopathology, weight, and depression among individuals of various ethnic groups, including White and Latinx or Hispanic individuals. This understanding is critical to understand associations with eating- and health-related behaviors, which might help to refine intervention targets and to ensure diverse populations receive appropriate treatments. Aspects of Latinx/Hispanic identity, such as acculturation or ethnic identity, might influence facets of body image disturbance and eating pathology. For instance, acculturation, which refers to adopting elements of a majority culture, has been linked to higher body mass index (Abraido-Lanza, Chao, & Flórez, 2005), greater body image concerns (Menon & Harter, 2012), and loss of control eating in Latinx/Hispanic populations (Alegria et al., 2007). Ethnic identity (i.e., attitudes toward and a sense of commitment to one’s ethnic group) is associated with increased well-being in Latinx/Hispanic populations (Smith & Silva, 2011), reduced loss of control eating in Latinx/Hispanic men (Williamson, Guidinger, & Kelly, 2020), and less frequent negative body talk in Latina women (Sladek, Salk, & Engeln, 2018). While research generally suggests that there are no differences in body dissatisfaction between White and Latina/Hispanic women (Cash & Smolak, 2011; Grabe & Hyde, 2006), it is important to note that overvaluation has been less commonly examined and men have been excluded from most research in this area. Further, distinctiveness in body dissatisfaction’s and overvaluation’s association with eating- and health-related domains between these groups remains unexamined. Thus, the present study bridges an important gap in the literature by testing whether clinical levels of body dissatisfaction and overvaluation differ by ethnicity, and by examining and comparing associations of body dissatisfaction and overvaluation with eating/weight-related variables by ethnicity.
Methods
Procedures
Survey respondents (N=2509) were recruited from Amazon’s Mechanical Turk website to complete an online survey on opinions about weight and eating. Individuals responded to an advertisement to “share your opinions about eating, weight, and health” (“encuesta sobre la alimentación, el peso y la salud”) and were eligible to participate if they spoke Spanish or English, were adults, and currently resided in the United States. Data were collected between August 2015 and January 2017. Consistent with similar studies during our data collection period, participants were paid between $0.50 and $1.00 to complete the survey. This study was approved by Yale’s institutional review board. All participants consented to study participation prior to completing measures.
Mechanical Turk is an online recruitment platform that yields high-quality and convenient data and has been used in psychological and psychiatric research (Thorstad & Wolff, 2018), including research on ethnicity (e.g., Villicana, Delucio, & Biernat, 2016) and disordered eating (e.g., Cummings & Tomiyama, 2019). Psychometric properties of measures completed by participants recruited from Mechanical Turk do not differ from participants recruited using traditional sources (Behrend, Sharek, Meade, & Wiebe, 2011). Mechanical Turk samples have greater demographic variability and are more geographically diverse than undergraduate samples (Behrend et al., 2011; Buhrmester, Kwang, & Gosling, 2011; Hauser & Schwarz, 2016), although they tend to be younger and are more likely to have a college education than nationally-representative samples (Yank, Agarwal, Loftus, Asch, & Rehkopf, 2017). Mechanical Turk allows for quality control from the platform as well as validity checks from within the survey to review response quality. In the current study, we required that each participant’s approval rating on Mechanical Turk exceeded 85%, and also included three items throughout the survey to assess effort and attention, in line with recommendations to use multiple response formats (we used multiple choice, true/false, and open-ended) (Buhrmester et al., 2011). Participants were excluded if they did not provide correct answers to validity items. In addition, participants were excluded for providing contradictory information, for example, reporting a birth date and an age that were discrepant. In sum, approximately 32.6% of participants were excluded for suspected invalid responding. Of the total 3025 participants with valid responses, a subset was included in the current study as described below.
Participants
Participants were included in the current study if they completed body image measures and self-identified as Latinx/Hispanic (n=568; n=362 White Hispanic, n=9 Black Hispanic, n=13 Asian Hispanic, n=20 American Indian/Native Hawaiian Hispanic, n=44 Multiracial Hispanic, n=120 Other race Hispanic) or non-Hispanic White (n=1941). Among participants who self-identified as Latinx/Hispanic, 67.3% chose to complete surveys in Spanish; 5.3% of participants who self-identified as non-Hispanic White chose to complete surveys in Spanish. All other surveys were completed in English.
Participants were between 19 and 74 years old (White: M=36.26, SD=11.95; Latinx/Hispanic: M=31.65, SD=9.04, p<.001). Participants were male (White: n=613, 31.6%; Latino/Hispanic: n=239, 42.1%, p<.05), female (White: n=1321, 68.1%; Latina/Hispanic: n=328, 57.7%, p<.05), transgender (White: n=5, 0.3%; Latinx/Hispanic: n=1, 0.2%), or “other” (White: n=2, 0.1%; Latinx/Hispanic: n=0). Education did not differ significantly between White and Latinx/Hispanic participants (p=.101): high school or less (White: n=285, 14.7%; Latinx/Hispanic: n=72, 12.7%), some college (White: n=628, 32.4%; Latinx/Hispanic: n=215, 37.9%), college degree (White: n=687, 35.4%; Latinx/Hispanic: n=188, 33.1%), or more than a college degree (White: n=341, 17.6%; Latinx/Hispanic: n=93, 16.4%). Sexual orientation also did not differ significantly between White and Latinx/Hispanic participants (p=.329): heterosexual (White: n=1725, 88.9%; Latinx/Hispanic: n=503, 88.6%), gay or lesbian (White: n=64, 3.3%; Latinx/Hispanic: n=27, 4.8%), bisexual (White: n=135, 7.0%; Latinx/Hispanic: n=33, 5.8%), or other (White: n=17, 0.9%; Latinx/Hispanic: n=5, 0.9%).
Measures
Body Mass Index (BMI).
BMI (kg/m2) was calculated using participants’ self-reported weight and height.
Eating/Weight-Related Psychopathology.
The Eating Disorder Examination-Questionnaire (EDE-Q) measures eating disorder psychopathology including eating disordered behaviors over the past 28 days (Fairburn & Beglin, 1994). The Spanish version has been validated in a nonclinical sample of Latinx/Hispanic individuals (Elder & Grilo, 2007; Grilo, Crosby, & White, 2012). The current study used a brief version of the EDE-Q, which uses seven items from the full version to derive three subscales (Dietary Restraint [3 items], Overvaluation [2 items], and Dissatisfaction [2 items]; higher scores are indicative of greater severity). The brief version has been shown to demonstrate superior psychometric properties in nonclinical and clinical studies compared with those from the original measure (Grilo, Crosby, et al., 2012; Grilo, Reas, Hopwood, & Crosby, 2015; Machado, Grilo, & Crosby, 2018; Machado, Grilo, Rodrigues, Vaz, & Crosby, 2020). In the current sample, items yielded internally consistent scales for both White (α=.89) and Latinx/Hispanic (α=.88) participants. Overvaluation and dissatisfaction variables were dichotomized into clinical and subclinical levels to examine distinctiveness, but continuous scores were used for correlations and regressions. Individuals who endorsed a score of 4 (“moderately”) or higher on either the overvaluation of weight or the overvaluation of shape item were categorized as having clinical levels of overvaluation, which corresponds to criteria applied in previous work (e.g., Grilo et al., 2008). Similarly, participants who responded with a score of 4 (“moderately”) or higher on either the dissatisfaction with weight or the dissatisfaction with shape item were categorized as having clinical levels of dissatisfaction, which corresponds to criteria applied in previous work (e.g., Lydecker et al., 2017). Frequency of objective overeating episodes (eating an unusually large amount of food without perceiving loss of control while eating), objective binge-eating episodes (eating an unusually large amount of food and feeling a subjective sense of loss-of-control while eating), and purging behaviors (vomiting, laxative misuse, and/or driven exercise; combined due to low frequency) were also assessed.
Depression.
Participants completed the Patient Health Questionnaire (PHQ-2), which assesses depressive mood during the past two weeks (Kroenke, Spitzer, & Williams, 2003). Specifically, the PHQ-2 is the first two items of the PHQ-9 (Kroenke, Spitzer, & Williams, 2001). Scores range from 0 to 6. The Spanish version of the PHQ, developed and validated by Wulsin and colleagues (Wulsin, Somoza, & Heck, 2002), was used for participants who chose to complete measures in Spanish.
Statistical Analyses
Because of non-normality, three variables (objective overeating episodes, objective binge-eating episodes, purging episodes) were log-transformed prior to analyses. Chi-square tests evaluated overlap between clinical levels of dissatisfaction and overvaluation of weight and shape as a test of their distinctiveness (i.e., whether overvaluation and dissatisfaction co-occur in individuals, whether only one is present, or whether neither is present). Correlations and regressions used the continuous variable forms of body image constructs. Descriptive statistics and Pearson correlation coefficients determined associations between body image constructs (overvaluation and dissatisfaction with weight and shape) and between each construct and each eating/weight-related variable: overeating frequency, binge-eating frequency, purging frequency, dietary restraint, and depression. Fisher’s r-to-z test compared correlations between White and Latinx/Hispanic participants. Multiple regression analyses included the body image constructs, and ethnicity as independent variables, the interaction of ethnicity with each body image construct (i.e., ethnicity as a moderator), and eating/weight-related variables as dependent variables. Results were considered significant at p<.05. To account for multiple comparisons, Z-tests evaluating correlation magnitudes (between body image constructs and between ethnicities) were considered significant at p<.025.
Results
Distinctiveness of Dissatisfaction and Overvaluation
Chi-square tests evaluated overlap between clinical levels of dissatisfaction and overvaluation of weight and shape as a test of their distinctiveness. In both Latinx/Hispanic (χ2(1, N=568)=114.28, p<.001) and White (χ2(1, N=1941)=567.84, p<.001) individuals, constructs were distinct. Among Latinx/Hispanic individuals: 40.3% reported clinical levels of both dissatisfaction and overvaluation, 15.3% reported clinical dissatisfaction but not overvaluation, 12.1% reported clinical overvaluation but not dissatisfaction, and 32.2% reported neither. Among White individuals: 44.5% reported clinical levels of both dissatisfaction and overvaluation, 12.3% reported clinical dissatisfaction but not overvaluation, 10.4% reported clinical overvaluation but not dissatisfaction, and 32.8% reported neither. Proportions did not significantly differ between White and Latinx/Hispanic individuals.
Comparisons of Correlation Magnitudes between Latinx/Hispanic and White Participants
Descriptive statistics for the eating/weight-related variables and body image constructs are summarized in Table 1. Correlations between body image constructs and eating/weight-related variables within each group are summarized in Table 2. Correlations were all significant at p<.001. The correlation between dissatisfaction and overvaluation was higher among White individuals (r=.71) than Latinx/Hispanic individuals (r=.65, Z=2.36, p=.018). The correlation between depression and overvaluation was stronger among White individuals (r=.41) than Latinx/Hispanic individuals (r=.31, Z=2.26, p=.024). The magnitudes of other correlations did not differ significantly between Latinx/Hispanic and White individuals.
Table 1.
Means and standard deviations of body image constructs and clinical variables.
| Latinx/Hispanic | White | |||||
|---|---|---|---|---|---|---|
| N | M | SD | N | M | SD | |
| Dissatisfaction with Weight and Shape | 568 | 3.09 | 1.93 | 1941 | 3.29 | 1.92 |
| Overvaluation of Weight and Shape | 568 | 2.99 | 1.89 | 1941 | 3.09 | 1.90 |
| Body Mass Index | 568 | 27.97 | 6.86 | 1941 | 27.99 | 7.15 |
| Overeating Frequency | 568 | 3.21 | 5.86 | 1940 | 2.61 | 5.21 |
| Binge-eating Frequency* | 568 | 2.04 | 4.46 | 1940 | 1.40 | 3.94 |
| Purging Frequency* | 568 | 3.24 | 7.91 | 1941 | 2.37 | 6.97 |
| Dietary Restraint | 568 | 2.52 | 2.07 | 1941 | 2.57 | 2.12 |
| Depression | 568 | 1.74 | 1.71 | 1941 | 1.74 | 1.78 |
Note. As missing data were minimal, the participant who did not provide overeating or binge eating data was excluded from those analyses, but not others where data were available.
67.6% of individuals reported zero binge eating episodes; 65.5% of individuals reported zero purging episodes. These variables were log-transformed for analyses with the assumption of normality.
Table 2.
Correlations Between Body Image Constructs and Eating/Weight-related Variables in Latinx/Hispanic and White Individuals
| Latinx/Hispanic | White | ||||
|---|---|---|---|---|---|
| Dissatisfaction | Overvaluation | Dissatisfaction | Overvaluation | ||
| r | r | r | r | Z | |
| Body Mass Index | 0.428 | 0.273 | 0.462 | 0.255 | ns |
| Overeating Frequency† | 0.266 | 0.248 | 0.238 | 0.245 | ns |
| Binge-eating Frequency† | 0.331 | 0.278 | 0.331 | 0.325 | ns |
| Purging Frequency† | 0.197 | 0.258 | 0.145 | 0.234 | ns |
| Dietary Restraint | 0.407 | 0.534 | 0.43 | 0.493 | ns |
| Depression | 0.379 | 0.311 | 0.404 | 0.405 | OVW>OVL |
Note. All correlations were significant, p<.001. Z-tests compared strength of correlations between Latinx/Hispanic and White individuals. OV=overvaluation.
Variable used a log transformation.
Comparisons of Overvaluation/Dissatisfaction Correlation Magnitudes within Latinx/Hispanic Participants and White Participants
Correlations between body image constructs and eating/weight-related variables were all significant (see Table 2). Among Latinx/Hispanic individuals, BMI (Z=2.98, p=.003) had a significantly stronger association with dissatisfaction than overvaluation, whereas dietary restraint (Z= −2.759, p=.006) had a significantly stronger association with overvaluation than dissatisfaction. Among White individuals, BMI had a significantly stronger association with dissatisfaction than overvaluation (Z= 7.44, p<.001). Purging (Z= −2.88, p=.004) and dietary restraint (Z= −2.492, p=.013) both had significantly stronger associations with overvaluation than dissatisfaction. Correlations of other eating/weight-related variables and dissatisfaction and overvaluation did not differ significantly.
Dissatisfaction and Overvaluation: Moderator Analyses
Multiple regression analyses tested overvaluation, dissatisfaction, and ethnicity as independent variables for each of the outcome variables, and also tested moderation using the interaction of overvaluationXethnicity and dissatisfactionXethnicity. Regression analyses for each eating/weight-related variable are presented in Table 3.
Table 3.
Regression models evaluating the moderating role of ethnicity.
| Eating/Weight Variable | Independent Variable | R2 | β | t | p |
|---|---|---|---|---|---|
| Body Mass Index | 21.6% | ||||
| Dissatisfaction | 0.579 | 20.09 | <.001 | ||
| Overvaluation | −0.156 | −5.41 | <.001 | ||
| Ethnicity | 0.032 | 0.88 | .378 | ||
| Dissatisfaction X Ethnicity | −0.131 | −2.79 | .005 | ||
| Overvaluation X Ethnicity | 0.117 | 2.53 | .012 | ||
| Overeating Frequency† | 7.6% | ||||
| Dissatisfaction | 0.128 | 4.10 | <.001 | ||
| Overvaluation | 0.153 | 4.91 | <.001 | ||
| Ethnicity | 0.063 | 1.61 | .108 | ||
| Dissatisfaction X Ethnicity | 0.042 | 0.82 | .410 | ||
| Overvaluation X Ethnicity | −0.020 | −0.39 | .694 | ||
| Binge-eating Frequency† | 13.5% | ||||
| Dissatisfaction | 0.195 | 6.44 | <.001 | ||
| Overvaluation | 0.177 | 5.87 | <.001 | ||
| Ethnicity | 0.116 | 3.08 | .002 | ||
| Dissatisfaction X Ethnicity | 0.068 | 1.37 | .171 | ||
| Overvaluation X Ethnicity | −0.051 | −1.05 | .293 | ||
| Purging Frequency† | 6.4% | ||||
| Dissatisfaction | −0.045 | −1.41 | .157 | ||
| Overvaluation | 0.259 | 8.26 | <.001 | ||
| Ethnicity | 0.026 | 0.66 | .510 | ||
| Dissatisfaction X Ethnicity | 0.080 | 1.57 | .117 | ||
| Overvaluation X Ethnicity | −0.014 | −0.27 | .788 | ||
| Dietary Restraint | 26.3% | ||||
| Dissatisfaction | 0.160 | 5.74 | <.001 | ||
| Overvaluation | 0.380 | 13.65 | <.001 | ||
| Ethnicity | −0.006 | −0.19 | .853 | ||
| Dissatisfaction X Ethnicity | −0.051 | −1.11 | .267 | ||
| Overvaluation X Ethnicity | 0.065 | 1.44 | .149 | ||
| Depression | 18.3% | ||||
| Dissatisfaction | 0.237 | 8.05 | <.001 | ||
| Overvaluation | 0.240 | 8.19 | <.001 | ||
| Ethnicity | 0.064 | 1.73 | .083 | ||
| Dissatisfaction X Ethnicity | 0.048 | 1.00 | .315 | ||
| Overvaluation X Ethnicity | −0.108 | −2.27 | .023 |
Note. Bolded values are significant (p < .05) independent variables and interactions (moderations). Ethnicity used non-Hispanic White as the reference group (0=White, 1=Latinx/Hispanic).
Variable used a log transformation.
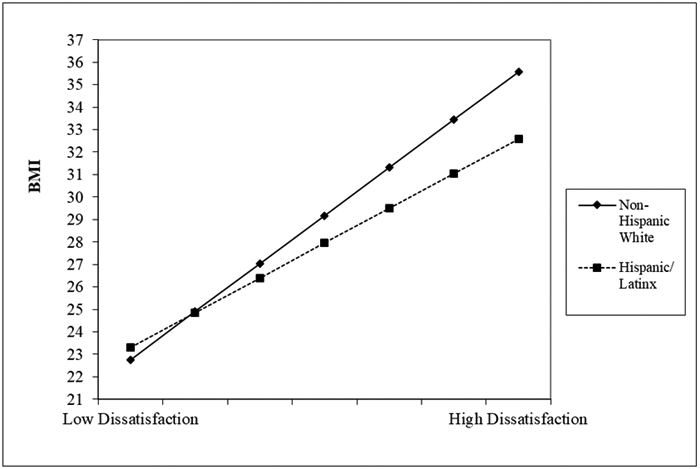
The overall regression model for BMI was significant (F(5,2503)=138.09, p<.001). Ethnicity moderated the association of overvaluation and BMI (β=.117, t=2.53, p=.012) such that among non-Hispanic White participants, those who reported higher overvaluation had lower BMIs than those who reported lower overvaluation (t=−5.31, p<.001), but the relationship between overvaluation and BMI was not significant among Hispanic/Latinx (t=−0.23, p=.816), see Figure 1A. Likewise, ethnicity moderated the association of dissatisfaction and BMI (β= −.131, t= −2.80, =.005) such that dissatisfaction and BMI were positively associated among both non-Hispanic White (t=20.36, p<.001) and Hispanic/Latinx (t=8.53, p<.001) participants, with a steeper slope amongst non-Hispanic White participants see Figure 1B.
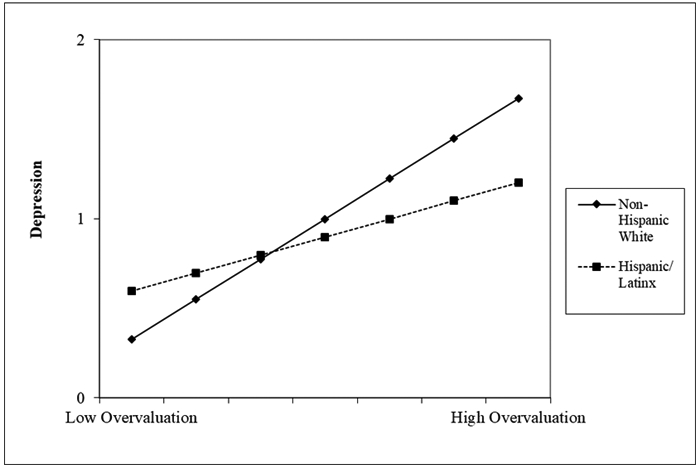
Figure 1. Depictions of Significant Interactions.
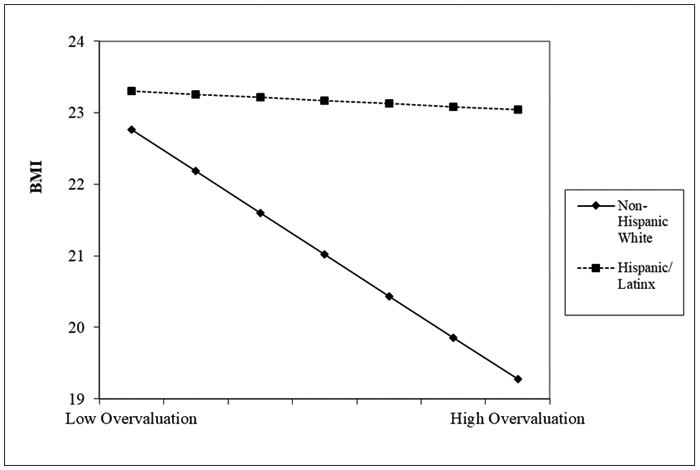
A: Ethnicity moderated the association between overvaluation and BMI. Overvaluation (x-axis) is graphed from 0 through 6, corresponding to possible scores on the subscale.
B: Ethnicity moderated the association between dissatisfaction and BMI. Dissatisfaction (x-axis) is graphed from 0 through 6, corresponding to possible scores on the subscale.
C: Ethnicity moderated the association between overvaluation and depression. Overvaluation (x-axis) is graphed from 0 through 6, corresponding to possible scores on the subscale.
The overall regression model for overeating frequency was significant (F(5,2502)=41.00, p<.001). Ethnicity did not moderate overvaluation (t=−.39, p=.69) nor dissatisfaction (t=.82, p=.41), nor did ethnicity have a main effect on overeating frequency (t=1.61, p=.11). Both overvaluation (t=4.91, p<.001) and dissatisfaction (t=4.11, p<.001) had significant main effects on overeating frequency.
The overall regression model for binge eating frequency was also significant (F(5,2502)=78.28, p<.001). Ethnicity did not moderate dissatisfaction (t=1.37, p=.17) nor overvaluation (t=−1.05, p=.29) but had a significant main effect on binge eating frequency (t=3.08, p=.002); Latinx/Hispanic individuals reported more binge-eating episodes than White individuals. Both overvaluation (t=6.44, p<.001) and dissatisfaction (t=5.87, p<.001) also had significant main effects on binge eating frequency.
The overall regression model for purging was also significant (F(5, 2503)=34.45, p<.001). Ethnicity did not moderate overvaluation (t=−.27, p=.79) nor dissatisfaction (t=1.57, p=.12), nor did it have a main effect on purging frequency (t=.66, p=.51). Overvaluation (t=8.26, p<.001) but not dissatisfaction (t=−1.41, p=.16) had a significant main effect on purging frequency.
The overall regression model for dietary restraint was significant (F(5, 2503)=178.53, p<.001. Overvaluation (t=13.65, p<.001) and dissatisfaction (t=5.74, p<.001), but not ethnicity (t=−.186, p=.85), had significant main effects. Ethnicity did not moderate overvaluation (t=1.44, p=.15) nor dissatisfaction (t=−1.11, p=.27).
The overall regression model was also significant for depression (F(5, 2503=111.82, p<.001). Ethnicity moderated overvaluation (t=−2.27, p=.02) but not dissatisfaction (t=1.00, p=.32) see Figure 1C. Overvaluation and depression were significantly, positively associated among both Hispanic/Latinx (t=2.26, p=.024) and non-Hispanic White (t=7.08, p<.001) participants, with a more pronounced association amongst non-Hispanic White participants. Overvaluation (t=8.19, p<.001) and dissatisfaction (t=8.05, p<.001), but not ethnicity (t=1.73, p=.08), had significant main effects on depression.
Discussion
This study found that dissatisfaction and overvaluation were distinct body image constructs in Latinx/Hispanic and White individuals, aligning with prior research highlighting that they are distinct constructs in individuals across a range of different eating and weight disorders, as well as across age groups (Grilo, Crosby, et al., 2019; Grilo, Ivezaj, et al., 2019; Lydecker et al., 2017; Masheb, Grilo, Burke-Martindale, & Rothschild, 2006; Mitchison et al., 2017). Results indicated there were not significant ethnic differences in clinical levels of body image concerns, aligning with previous research suggesting that White and Latinx/Hispanic adults generally don’t differ in levels of body dissatisfaction (Cash & Smolak, 2011; Grabe & Hyde, 2006). Further support of the distinctiveness of body dissatisfaction and overvaluation, independent of ethnicity, is found in the pattern of correlations. In both Latinx/Hispanic and White individuals, dissatisfaction was more strongly associated with BMI whereas overvaluation was more strongly associated with dietary restraint. Again in both Latinx/Hispanic and White individuals, associations did not differ significantly between overvaluation and dissatisfaction and overeating episode frequency, binge-eating episode frequency, and depression. This pattern mirrors findings in adults categorized with eating and weight disorders (Grilo, Ivezaj, et al., 2019), as well as research in adolescents (Mitchison et al., 2017). The positive association of overvaluation with purging, a behavior reported at a low frequency in our sample yet a clear indicator of psychopathology (Favaro & Santonastaso, 1996; Franko & Keel, 2006), is especially notable as prior research indicates that overvaluation is an important distinguishing feature underlying eating disorders and not simply a reaction to one’s weight, although research with patients with bulimia nervosa indicates overvaluation is not independently associated with purging (Grilo, Crosby, et al., 2019; Grilo et al., 2009; Grilo et al., 2008). Taken together, these findings suggest that overvaluation may signal eating disorder psychopathology across ethnicity, whereas dissatisfaction may be more of a reflection of weight.
Although most of the correlations had similar magnitudes between Latinx/Hispanic and White individuals, depression was more strongly associated with overvaluation among White than Latinx/Hispanic individuals. Parallel findings emerged from the regression model for depression, in which ethnicity moderated the association of overvaluation (but not dissatisfaction) and depression. Prior research has highlighted overvaluation as particularly relevant to psychological distress and depression (Grilo, Masheb, & White, 2010; Grilo, White, & Masheb, 2012) and our findings suggest that higher levels of overvaluation might signal elevated depression and potentially warrant clinical monitoring.
Ethnicity also moderated the association between overvaluation and BMI, such that there was no association between overvaluation and BMI in Latinx/Hispanic participants while there was a negative association between overvaluation and BMI in White participants. Ethnicity also moderated the positive association between overvaluation and depression, with a stronger association among White participants than Latinx participants. Previous work has shown some associations between BMI and body dissatisfaction (Grilo, Ivezaj, et al., 2019), but other work has failed to find associations between BMI and body image variables (Lydecker et al., 2017). Our results contribute to the complexity of understanding weight status and body image by suggesting that ethnicity changes the extent of the relationship between these variables. Given pervasive pressure in society to attain a certain body size (Harper & Tiggemann, 2008; Stice, Maxfield, & Wells, 2003), and some degree of body dissatisfaction being considered normative (Britton, Martz, Bazzini, Curtin, & LeaShomb, 2006; Rodin, Silberstein, & Striegel-Moore, 1984), it is possible that cultural differences buffer Latinx/Hispanic individuals. Cultural norms differ between White and Latinx individuals, including views that outcomes may not be under one’s own control (Anez, Paris, Bedregal, Davidson, & Grilo, 2005; Foreyt, 2003; Moreira et al., 2018), which might limit the degree to which body shape and weight influence self-evaluation. Cultural variables such as acculturation have been identified as potential buffers for the effects of body image concerns on psychological distress in ethnic minorities (Xie et al., 2010), aligning with the “immigrant paradox,” which posits that less acculturated individuals experience better mental health outcomes compared to those who are more acculturated (Vega, Sribney, Aguilar-Gaxiola, & Kolody, 2004), perhaps due to a protective effect from the country of origin. Latinx individuals who are less acculturated to European-American culture might experience less sociocultural pressure toward thinness and put less emphasis on body image. This could partly account for the weakened association between dissatisfaction and BMI in Latinx compared to White individuals, and lack of association between overvaluation and BMI in Latinx individuals (whereas White individuals displayed an inverse association). This aligns with previous cross-sectional research indicating that Mexican American women who are less acculturated to European-American culture are at lower risk for eating disorders (Cachelin, Phinney, Schug, & Striegel-Moore, 2006). Alternatively, acculturation has been suggested as a stressor that leads to developing disordered eating behaviors as a means of coping with negative affect (Claudat, White, & Warren, 2016; Higgins Neyland & Bardone-Cone, 2017; Rodgers, Berry, & Franko, 2018). Thus, future research should include measurement of relevant cultural constructs and assess degree of acculturation to clarify the nature of these differences. As cultural constructs likely intersect with other identities and roles, qualitative research may allow for more nuanced understanding of body image experiences among Hispanic/Latinx individuals. Likewise, because some of the quantitative tests revealed small significant differences, research with diverse treatment-seeking populations, epidemiological work, and more nuanced assessment of culture and body image, could add to the clinical relevance of our findings.
Strengths of our research include the large sample size that allowed for fine-grained analyses of body image constructs and the use of established self-report measures that have previously been psychometrically supported for use with Latinx/Hispanic individuals. Nevertheless, limitations of our research exist, including the reliance on self-report measures that may be less accurate for certain behaviors (e.g., restraint, overeating) than objective or observational measurements. Conversely, it is possible that self-reported data may be more accurate in some respects because it does not elicit the same demand characteristics as observational measurement (Fairburn & Beglin, 1994) and self-report might facilitate disclosing sensitive subjective phenomena such as body image concerns. Notably, research suggests self-reported height and weight are fairly accurate for adults (Kuczmarski, Kuczmarski, & Najjar, 2001) and discrepancies between self-reported and measured anthropometric data are not associated with eating disorder psychopathology (White, Masheb, & Grilo, 2010). Additionally, we used the Spanish-language EDE-Q, which has some psychometric support, but further research is needed to determine measurement invariance between Hispanic/Latinx individuals and White non-Hispanic individuals. Our data were cross-sectional, thereby not allowing for speculation about causality or the direction of relationships. Prior research using longitudinal designs with community (Sharpe et al., 2018) and clinical (Askew et al., 2020; Masheb & Grilo, 2003) samples indicates that dissatisfaction and overvaluation have differential associations with depressive symptoms, binge eating, and unhealthy weight-control behaviors. Longitudinal research is needed to extend our findings, as well as those from prior work, to understand how body image relates to eating disorder psychopathology in diverse patient groups. In particular, future research should include preoccupation in addition to overvaluation and dissatisfaction as key constructs related to body image. Our study focused on Latinx/Hispanic and White adults and the findings might not generalize to individuals of other races and ethnicities. Relatedly, we did not assess cultural variables that might account for differences observed in the association of the body image constructs with eating/weight-related psychopathology. Future research should consider including measures of ethnic identity, acculturation, assimilation, or Latinx/Hispanic cultural constructs (e.g., machismo, fatalismo) that may provide further information about the relations between body image constructs and eating disorder features. Finally, our data were gathered from community members online, which, while more diverse than college samples, still tend to be younger and more educated than nationally-representative samples (Walters, Christakis, & Wright, 2018), and findings may not translate to treatment-seeking clinical samples.
Overall, our findings add to a growing literature that suggests overvaluation and dissatisfaction are distinct body image constructs and offer important information about individuals’ eating disorder psychopathology in addition to depression and weight. In particular, our data suggest that overvaluation is indicative of eating disorder behavior, whereas dissatisfaction is associated with body size. The moderating effect of ethnicity on the associations between overvaluation and depression, overvaluation and BMI, and dissatisfaction and BMI, suggest that further research assessing cultural variables and eating disorder psychopathology will offer insights into individuals’ risk for developing biopsychosocial comorbidities, help clinicians and researchers refine intervention targets, and ensure diverse populations are receiving appropriate treatments.
Acknowledgments
This research was supported, in part, by National Institutes of Health grants K24 DK070052, K23 DK115893, K23 AT011049, and UL1 TR001863. Drs. Grilo and Lydecker were supported, in part, by National Institutes of Health grants R01 DK112771, R01 DK49587 and R01 DK114075. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH. The authors report no conflicts of interest.
Data availability:
Data will be made available upon reasonable request.
References
- Abraido-Lanza AF, Chao MT, & Flórez KR (2005). Do healthy behaviors decline with greater acculturation?: Implications for the Latino mortality paradox. Social Science & Medicine, 61, 1243–1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Woo M, Cao Z, Torres M, Meng XL, & Striegel-Moore R (2007). Prevalence and correlates of eating disorders in Latinos in the United States. International Journal of Eating Disorders, 40 Suppl, S15–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anez LM, Paris M Jr., Bedregal LE, Davidson L, & Grilo CM (2005). Application of cultural constructs in the care of first generation Latino clients in a community mental health setting. Journal of Psychiatric Practice, 11, 221–230. [DOI] [PubMed] [Google Scholar]
- Askew AJ, Peterson CB, Crow SJ, Mitchell JE, Halmi KA, Agras WS, & Haynos AF (2020). Not all body image constructs are created equal: Predicting eating disorder outcomes from preoccupation, dissatisfaction, and overvaluation. International Journal of Eating Disorders. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behrend TS, Sharek DJ, Meade AW, & Wiebe EN (2011). The viability of crowdsourcing for survey research. Behavior Research Methods, 43, 800–813. [DOI] [PubMed] [Google Scholar]
- Britton LE, Martz DM, Bazzini DG, Curtin LA, & LeaShomb A (2006). Fat talk and self-presentation of body image: Is there a social norm for women to self-degrade? Body Image, 3, 247–254. [DOI] [PubMed] [Google Scholar]
- Buhrmester M, Kwang T, & Gosling SD (2011). Amazon's Mechanical Turk: A new source of inexpensive, yet high-quality, data? Perspectives on Psychological Science, 6, 3–5. [DOI] [PubMed] [Google Scholar]
- Cachelin FM, Phinney JS, Schug RA, & Striegel-Moore RH (2006). Acculturation and eating disorders in a Mexican American community sample. 30, 340–347. [Google Scholar]
- Calugi S, & Dalle Grave R (2019). Body image concern and treatment outcomes in adolescents with anorexia nervosa. International Journal of Eating Disorders, 52, 582–585. [DOI] [PubMed] [Google Scholar]
- Cash TF (2004). Body image: past, present, and future. Body Image, 1, 1–5. [DOI] [PubMed] [Google Scholar]
- Cash TF, & Smolak L (2011). Body image: A handbook of science, practice, and prevention: Guilford Press. [Google Scholar]
- Claudat K, White EK, & Warren CS (2016). Acculturative stress, self-esteem, and eating pathology in Latina and Asian American female college students. Journal of Clinical Psychology, 72, 88–100. [DOI] [PubMed] [Google Scholar]
- Cummings JR, & Tomiyama AJ (2019). Food loves company: Risky eating with friends increases interpersonal closeness. Journal of Experimental Social Psychology, 81, 61–69. [Google Scholar]
- Dalle Grave R, Misconel A, Fasoli D, & Calugi S (2020). Overvaluation of Shape and Weight and Associated Features in Patients Without Eating Disorders Seeking Treatment for Obesity. Obesity, 28, 733–739. [DOI] [PubMed] [Google Scholar]
- Elder KA, & Grilo CM (2007). The Spanish language version of the Eating Disorder Examination Questionnaire: comparison with the Spanish language version of the eating disorder examination and test-retest reliability. Behaviour Research and Therapy, 45, 1369–1377. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, & Beglin SJ (1994). Assessment of eating disorders: Interview or self-report questionnaire? International Journal of Eating Disorders, 16, 363–371. [PubMed] [Google Scholar]
- Fairburn CG, & Cooper Z (1993). The Eating Disorder Examination. In Fairburn CG & Wilson GT (Eds.), Binge Eating: Nature, Assessment, and Treatment (pp. 317–360). New York: Guilford Press. [Google Scholar]
- Fairburn CG, Cooper Z, & Shafran R (2003). Cognitive behaviour therapy for eating disorders: A "transdiagnostic" theory and treatment. Behaviour Research and Therapy, 41, 509–528. [DOI] [PubMed] [Google Scholar]
- Favaro A, & Santonastaso P (1996). Purging behaviors, suicide attempts, and psychiatric symptoms in 398 eating disordered subjects. International Journal of Eating Disorders, 20, 99–103. [DOI] [PubMed] [Google Scholar]
- Feingold A, & Mazzella R (1998). Gender differences in body image are increasing. Psychological Science, 9, 190–195. [Google Scholar]
- Foreyt JP (2003). Cultural competence in the prevention and treatment of obesity: Latino Americans. The Permanente Journal, 7, 42–45. [Google Scholar]
- Franko DL, & Keel PK (2006). Suicidality in eating disorders: occurrence, correlates, and clinical implications. Clinical Psychology Review, 26, 769–782. [DOI] [PubMed] [Google Scholar]
- Friederich HC, Brooks S, Uher R, Campbell IC, Giampietro V, Brammer M, … Treasure J (2010). Neural correlates of body dissatisfaction in anorexia nervosa. Neuropsychologia, 48, 2878–2885. [DOI] [PubMed] [Google Scholar]
- Grabe S, & Hyde JS (2006). Ethnicity and body dissatisfaction among women in the United States: a meta-analysis. Psychological Bulletin, 132, 622–640. [DOI] [PubMed] [Google Scholar]
- Grilo CM (2013). Why no cognitive body image feature such as overvaluation of shape/weight in the binge eating disorder diagnosis? International Journal of Eating Disorders, 46, 208–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Crosby RD, & Machado PPP (2019). Examining the distinctiveness of body image concerns in patients with anorexia nervosa and bulimia nervosa. International Journal of Eating Disorders, 52, 1229–1236. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Crosby RD, Masheb RM, White MA, Peterson CB, Wonderlich SA, … Mitchell JE (2009). Overvaluation of shape and weight in binge eating disorder, bulimia nervosa, and sub-threshold bulimia nervosa. Behaviour Research and Therapy, 47, 692–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Crosby RD, & White MA (2012). Spanish-language Eating Disorder Examination interview: Factor structure in Latino/as. Eating Behaviors, 13, 410–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Hrabosky JI, White MA, Allison KC, Stunkard AJ, & Masheb RM (2008). Overvaluation of shape and weight in binge eating disorder and overweight controls: Refinement of a diagnostic construct. Journal of Abnormal Psychology, 117, 414–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Ivezaj V, Lydecker JA, & White MA (2019). Toward an understanding of the distinctiveness of body-image constructs in persons categorized with overweight/obesity, bulimia nervosa, and binge-eating disorder. Journal of Psychosomatic Research, 126, 109757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, & White MA (2010). Significance of overvaluation of shape/weight in binge-eating disorder: Comparative study with overweight and bulimia nervosa. Obesity, 18, 499–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Reas DL, Hopwood CJ, & Crosby RD (2015). Factor structure and construct validity of the Eating Disorder Examination-Questionnaire in college students: Further support for a modified brief version. International Journal of Eating Disorders, 48, 284–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, White MA, & Masheb RM (2012). Significance of overvaluation of shape and weight in an ethnically diverse sample of obese patients with binge-eating disorder in primary care settings. Behaviour Research and Therapy, 50, 298–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper B, & Tiggemann M (2008). The effect of thin ideal media images on women’s self-objectification, mood, and body image. Sex Roles, 58, 649–657. [Google Scholar]
- Hauser DJ, & Schwarz N (2016). Attentive Turkers: MTurk participants perform better on online attention checks than do subject pool participants. Behavior Research Methods, 48, 400–407. [DOI] [PubMed] [Google Scholar]
- Higgins Neyland M, & Bardone-Cone AM (2017). Tests of escape theory of binge eating among Latinas. Cultural Diversity & Ethnic Minority Psychology, 23, 373. [DOI] [PubMed] [Google Scholar]
- Kroenke K, MD, Spitzer RL, MD, & Williams JBW, DSW. (2003). The Patient Health Questionnaire-2: Validity of a Two-Item Depression Screener. Medical Care, 41, 1284–1293. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JBW (2001). The PHQ-9. Journal of General Internal Medicine, 16, 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczmarski MF, Kuczmarski RJ, & Najjar M (2001). Effects of age on validity of self-reported height, weight, and body mass index: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. Journal of the American Dietetic Association, 101, 28–34. [DOI] [PubMed] [Google Scholar]
- Lydecker JA, White MA, & Grilo CM (2017). Form and formulation: Examining the distinctiveness of body image constructs in treatment-seeking patients with binge-eating disorder. Journal of Consulting & Clinical Psychology, 85, 1095–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machado PPP, Grilo CM, & Crosby RD (2018). Replication of a modified factor structure for the Eating Disorder Examination-Questionnaire: Extension to clinical eating disorder and non-clinical samples in Portugal. European Eating Disorders Review, 26, 75–80. [DOI] [PubMed] [Google Scholar]
- Machado PPP, Grilo CM, Rodrigues TF, Vaz AR, & Crosby RD (2020). Eating Disorder Examination - Questionnaire short forms: A comparison. International Journal of Eating Disorders. [DOI] [PubMed] [Google Scholar]
- Masheb RM, & Grilo CM (2003). The nature of body image disturbance in patients with binge eating disorder. International Journal of Eating Disorders, 33, 333–341. [DOI] [PubMed] [Google Scholar]
- Masheb RM, Grilo CM, Burke-Martindale CH, & Rothschild BS (2006). Evaluating oneself by shape and weight is not the same as being dissatisfied about shape and weight: A longitudinal examination in severely obese gastric bypass patients. International Journal of Eating Disorders, 39, 716–720. [DOI] [PubMed] [Google Scholar]
- Menon CV, & Harter SL (2012). Examining the impact of acculturative stress on body image disturbance among Hispanic college students. Cultural Diversity & Ethnic Minority Psychology, 18, 239–246. [DOI] [PubMed] [Google Scholar]
- Mitchison D, Hay P, Griffiths S, Murray SB, Bentley C, Gratwick-Sarll K, … Mond J (2017). Disentangling body image: The relative associations of overvaluation, dissatisfaction, and preoccupation with psychological distress and eating disorder behaviors in male and female adolescents. International Journal of Eating Disorders, 50, 118–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mond JM, & Hay PJ (2011). Dissatisfaction versus over-evaluation in a general population sample of women. International Journal of Eating Disorders, 44, 721–726. [DOI] [PubMed] [Google Scholar]
- Moreira T, Hernandez DC, Scott CW, Murillo R, Vaughan EM, & Johnston CA (2018). Susto, coraje, y fatalismo: cultural-bound beliefs and the treatment of diabetes among socioeconomically disadvantaged Hispanics. American journal of lifestyle medicine, 12, 30–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohring R, Graber JA, & Brooks-Gunn J (2002). Girls' recurrent and concurrent body dissatisfaction: correlates and consequences over 8 years. International Journal of Eating Disorders, 31, 404–415. [DOI] [PubMed] [Google Scholar]
- Rodgers RF, Berry R, & Franko DL (2018). Eating disorders in ethnic minorities: An update. Curr Psychiatry Rep, 20, 90. [DOI] [PubMed] [Google Scholar]
- Rodin J, Silberstein L, & Striegel-Moore R (1984). Women and weight: A normative discontent. Nebraska Symposium on Motivation, 32, 267–307. [PubMed] [Google Scholar]
- Schwartz MB, & Brownell KD (2004). Obesity and body image. Body Image, 1, 43–56. [DOI] [PubMed] [Google Scholar]
- Sharpe H, Griffiths S, Choo TH, Eisenberg ME, Mitchison D, Wall M, & Neumark-Sztainer D (2018). The relative importance of dissatisfaction, overvaluation and preoccupation with weight and shape for predicting onset of disordered eating behaviors and depressive symptoms over 15 years. International Journal of Eating Disorders, 51, 1168–1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sladek MR, Salk RH, & Engeln R (2018). Negative body talk measures for Asian, Latina(o), and White women and men: Measurement equivalence and associations with ethnic-racial identity. Body Image, 25, 66–77. [DOI] [PubMed] [Google Scholar]
- Smith TB, & Silva L (2011). Ethnic identity and personal well-being of people of color: a meta-analysis. Journal of Counseling Psychology, 58, 42–60. [DOI] [PubMed] [Google Scholar]
- Stice E, Maxfield J, & Wells T (2003). Adverse effects of social pressure to be thin on young women: an experimental investigation of the effects of "fat talk". International Journal of Eating Disorders, 34, 108–117. [DOI] [PubMed] [Google Scholar]
- Tabri N, Murray HB, Thomas JJ, Franko DL, Herzog DB, & Eddy KT (2015). Overvaluation of body shape/weight and engagement in non-compensatory weight-control behaviors in eating disorders: Is there a reciprocal relationship? Psychological Medicine, 45, 2951–2958. [DOI] [PubMed] [Google Scholar]
- Thompson JK, Heinberg LJ, Altabe M, & Tantleff-Dunn S (1999). Exacting beauty: Theory, assessment, and treatment of body image disturbance. Washington, DC: American Psychological Association. [Google Scholar]
- Thompson JK, & Stice E (2001). Thin-ideal internalization: Mounting evidence for a new risk factor for body-image disturbance and eating pathology. Current Directions in Psychological Science, 10, 181–183. [Google Scholar]
- Thorstad R, & Wolff P (2018). A big data analysis of the relationship between future thinking and decision-making. PNAS, 115, E1740–E1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiggemann M (2004). Body image across the adult life span: stability and change. Body Image, 1, 29–41. [DOI] [PubMed] [Google Scholar]
- Van den Berg P, Paxton SJ, Keery H, Wall M, Guo J, & Neumark-Sztainer D (2007). Body dissatisfaction and body comparison with media images in males and females. Body Image, 4, 257–268. [DOI] [PubMed] [Google Scholar]
- Vega WA, Sribney WM, Aguilar-Gaxiola S, & Kolody B (2004). 12-month prevalence of DSM-III-R psychiatric disorders among Mexican Americans: nativity, social assimilation, and age determinants. Journal of Nervous and Mental Disease, 192, 532–541. [DOI] [PubMed] [Google Scholar]
- Villicana AJ, Delucio K, & Biernat M (2016). “Coming out” among gay Latino and gay White men: implications of verbal disclosure for well-being. Self and Identity, 15, 468–487. [Google Scholar]
- Walters K, Christakis DA, & Wright DR (2018). Are Mechanical Turk worker samples representative of health status and health behaviors in the US? PLoS One, 13, e0198835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White MA, Masheb RM, & Grilo CM (2010). Accuracy of self-reported weight and height in binge eating disorder: Misreport is not related to psychological factors. Obesity, 18, 1266–1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildes JE, Emery RE, & Simons AD (2001). The roles of ethnicity and culture in the development of eating disturbance and body dissatisfaction: a meta-analytic review. Clinical Psychology Review, 21, 521–551. [DOI] [PubMed] [Google Scholar]
- Williamson G, Guidinger C, & Kelly NR (2020). Low body mass and ethnic identity exploration exacerbate the association between body image concerns and loss of control eating in Hispanic/Latino men. International Journal of Eating Disorders, 53, 180–190. [DOI] [PubMed] [Google Scholar]
- Wulsin L, Somoza E, & Heck J (2002). The Feasibility of Using the Spanish PHQ-9 to Screen for Depression in Primary Care in Honduras. Prim Care Companion J Clin Psychiatry, 4, 191–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie B, Unger JB, Gallaher P, Johnson CA, Wu Q, & Chou C-P (2010). Overweight, body image, and depression in Asian and Hispanic adolescents. Am J Health Behav, 34, 476–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yank V, Agarwal S, Loftus P, Asch S, & Rehkopf D (2017). Crowdsourced Health Data: Comparability to a US National Survey, 2013–2015. American Journal of Public Health, 107, 1283–1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available upon reasonable request.


