Abstract
Purpose
We aimed to develop a simple scoring system based on baseline inflammatory and nutritional parameters to predict the efficacy of first-line chemotherapy and survival outcomes for de novo metastatic nasopharyngeal carcinoma (mNPC).
Patients and Methods
We retrospectively collected ten candidate inflammatory and nutritional parameters from de novo mNPC patients who received platinum-based first-line chemotherapy treatment. We examined the effects of these ten candidate variables on progression-free survival (PFS) using the Cox regression model. We built a risk-scoring system based on the regression coefficients associated with the identified independent prognostic factors. The predictive accuracy of the scoring system was evaluated and independently validated.
Results
A total of 460 patients were analyzed. Four independent prognostic factors were identified in a training cohort and were used to construct the scoring system, including nutritional risk index, C-reactive protein level, alkaline phosphatase level, and lactate dehydrogenase level. Based on the score obtained from the scoring system, we stratified patients into three prognostic subgroups (low: 0–1 point, intermediate: 2–3 points, and high: 4 points) associated with significantly different disease control rates (94.7% vs. 92.5% vs. 66.0%, respectively) and survival outcomes (3-year PFS: 55.8% vs. 29.1% vs. 11.9%, respectively). The scoring system had a good performance for the prediction of short-term disease control (area under the receiver operating characteristic curve [AUC]: 0.701) and long-term survival outcomes (time-dependent AUC for 5-year PFS: 0.713). The results were internally validated using an independent cohort (AUC for predicting disease control: 0.697; time-dependent AUC for 5-year PFS: 0.713).
Conclusion
We developed and validated a clinically useful risk-scoring system that could predict the efficacy of first-line chemotherapy and survival outcomes in de novo mNPC patients. This system may help clinicians to design personalized treatment strategies.
Keywords: metastatic nasopharyngeal carcinoma, nutritional status, cancer-related inflammation, chemotherapy efficacy, survival outcomes
Introduction
Epstein-Barr virus (EBV) infection is the predominant etiologic factor for the development of nasopharyngeal carcinoma (NPC). This virus-related cancer represents a typical “inflamed tumor”, which often exhibits the massive infiltration of lymphocytes and inflammatory stroma.1 Cancer-related inflammation is frequently considered to be a cardinal feature of malignancy, contributing to cancer initiation, development, and progression.2–4 Many lines of evidence have demonstrated that cancer patients with systemic inflammation are characterized by inadequate antitumor responses and unfavorable outcomes compared with those patients without systemic inflammation.4–13
In addition to systemic inflammation, the nutritional status of cancer patients is another aspect that can affect antitumor treatment efficacy. Several nutritional indexes, such as the prognostic nutritional index (PNI), nutritional risk index (NRI), and controlling nutritional status (CONUT) score, have been closely correlated with treatment-related complications, therapeutic responses, and clinical outcomes in various cancer types, including NPC.13–19 Malnourished patients suffer more from treatment-related side effects, resulting in worse quality of life, insufficient treatment intensity, and poor prognoses.
Currently, platinum-based systemic chemotherapy is a mainstay, first-line treatment for de novo mNPC, as recommended by the National Comprehensive Cancer Network (NCCN) guidelines.20 Our previous work and an updated clinical trial have confirmed that additional locoregional radiotherapy can significantly improve survival among those who show satisfactory first-line chemotherapy responses.21,22 However, roughly 35% of all de novo mNPC patients do not exhibit satisfactory responses to first-line chemotherapy. These patients represent an under-appreciated subgroup that might require more intense therapy. The identification of these patients is crucial for the timely modification of treatment regimens and individualized recommendations. However, no validated biomarkers or clinically appliable tools exist that are capable of predicting the efficacy of first-line chemotherapy among patients with de novo mNPC. Thus, this study aimed to develop and validate a simple scoring system based on a panel of baseline inflammatory and nutritional parameters to allow clinicians to predict the efficacy of first-line chemotherapy and enable patients with de novo mNPC to be stratified prior to therapy initiation.
Methods
Patients and Study Design
A flowchart showing the patient enrollment strategy and inclusion criteria is illustrated in Figure S1. A total of 1067 consecutive patients with mNPC who received platinum-based chemotherapy as the first-line treatment at Sun Yat-Sen University Cancer Center (SYSUCC) between January 2008 and December 2015 were initially evaluated for study inclusion. We excluded those patients with (i) asynchronous metastasis after curative treatment (n = 546); (ii) uncertain TNM (tumor, node, metastasis) classifications (n = 3); (iii) previous history of anticancer treatment (n = 18); (iv) unconfirmed histology (n = 3); (v) fewer than two cycles of first-line chemotherapy (n = 7); (vi) previous or synchronous malignant tumors (n = 9); and (vi) missing or unmeasurable radiological evaluation data (n = 21). Finally, 460 eligible patients were enrolled in this study. This study was performed following all institutional guidelines. The Chinese Ethics Committee of Registering Clinical Trials approved this study (registration number: ChiCTR2100042432). Informed consent was waived due to the retrospective nature of the study and the anonymization of patient data.
Variables of Interest
Candidate inflammatory and nutritional parameters were selected for the development of the scoring system after a review of the literature. This study focused on ten indexes, including lactate dehydrogenase (LDH) levels, C-reactive protein (CRP) levels, alkaline phosphatase (ALP) levels, the neutrophil to lymphocyte ratio (NLR), the platelet-lymphocyte ratio (PLR), Glasgow prognostic score (GPS), systemic immune-inflammation index (SII), PNI, NRI, and CONUT scores. The LDH, CRP, and ALP levels, NLR, and PLR were obtained from routine laboratory findings. The SII was calculated as platelets × NLR. The PNI was calculated as albumin (g/L) + 5 × lymphocyte counts (109/L). The NRI was calculated as 1.489 × albumin (g/L) + 41.7 × (weight/usual body weight).23 The GPS and CONUT scores were determined using the scoring systems described in Tables S1 and S2 (available in Supplementary Materials). Besides, other conventional variables, including demographic (age and sex), clinical (comorbidity and body mass index), tumor (histology, TNM classifications, number of metastatic sites, number of metastatic lesions, and metastases sites), and laboratory (pretreatment EBV DNA titer) variables were also included in the analysis.
Treatments and Outcomes
The treatment information for the study population has previously been described in detail elsewhere.21 This study’s primary outcome was progression-free survival (PFS), which was defined as the time interval between first-line chemotherapy initiation and tumor progression or death for any cause, whichever occurred first. The secondary outcome measures were overall survival (OS) and the disease control rate (DCR). OS was defined as the time interval between chemotherapy commencement and all-cause mortality. We censored patients who were lost to follow-up at the date of the last contact. Tumor responses were assessed using the revised Response Evaluation Criteria in Solid Tumors (RECIST v1.1).24 Tumor assessments were performed every two chemotherapy cycles, starting with the initiation of first-line chemotherapy until progression or the start of another anticancer treatment. The DCR referred to the proportion of patients whose investigator-assessed, best overall response during first-line chemotherapy was complete response (CR), partial response (PR), or stable disease (SD).
Statistical Analysis
The current study was performed in two stages. During the first stage, a risk scoring system was developed to predict the response to first-line chemotherapy and therapeutic outcomes. During the second stage, the scoring system was validated. We designed the scoring system using a training cohort (n = 296) comprising patients who underwent first-line chemotherapy between January 2008 and December 2013. The scoring system was independently validated in a validation cohort (n = 164), which included consecutive patients who received treatment between 2014 and 2015.
During the first stage, we examined the impacts of ten candidate inflammatory and nutritional variables on PFS to build a risk-scoring system. We categorized candidate continuous variables using the optimal cutoff determined by Maximally Selected Rank Statistics. Cox proportional hazards models were conducted to evaluate each candidate index’s prognostic value and to calculate the corresponding hazard ratio (HR). All variables with a P-value < 0.05 were entered into the following step-wise multivariable analysis. Model selection was based on the Akaike Information Criterion (AIC).25 The AIC was first introduced in 1971 by Hirotugu Akaike. The AIC is an estimator that can be used to evaluate how well a model fits the data. In statistics, the AIC is used to compare the relative quality of various statistical models for a given dataset to determine the model with the best fit. Multicollinearity diagnostics for statistical modeling were conducted by evaluating the correlations, variance inflation factors, and eigenvalues. We assigned weighted scores proportional to β regression coefficients for each independent risk factor that was identified in the step-wise multivariate analysis to develop the risk-score system. For added convenience, each score was rounded to the nearest integer. We calculated the risk score for each patient based on the developed scoring system. We then stratified the patients into three categories according to the total score: low-, intermediate-, and high-risk. During the second stage, we applied the developed risk-scoring system to an independent validation dataset. A risk score for each patient was calculated based on the developed scoring system, and risk stratification was performed for each patient in the validation cohort.
For both the training and validation datasets, the distribution of tumor response rates and the DCR trends between the three risk groups were evaluated using the χ2 test and the Cochran Armitage trend test, respectively. The scoring system’s performance for predicting the DCR was assessed using the area under the receiver operating characteristic (ROC) curve (AUC) and was compared against other variables. As an internal analysis, PFS and OS were estimated using the Kaplan-Meier approach, and survival differences among the three risk groups were compared using the Log rank test. The HRs for each risk stratification group were calculated either alone or adjusted for confounding factors. The adjusted HRs were calculated using the multivariable Cox regression analysis with the enter method. Missing pretreatment EBV DNA values were imputed using a multivariable imputation by chained equations algorithm before the performance of multivariable modeling.26 Time-dependent ROC curve analysis was used to assess the scoring system’s performance for the prediction of PFS and OS. The Gronnesby and Borgan goodness-of-fit test for the Cox proportional hazards model was applied to evaluate the goodness-of-fit of the risk scoring system, similar to the Hosmer–Lemeshow test for logistic regression.
All statistical analyses were performed using R software, version 4.0.3 (The R Foundation, Vienna, Austria). A P-value of less than 0.05 was considered significant.
Results
Patient Characteristics of Training and Validation Cohorts
A total of 460 eligible patients with de novo mNPC who received platinum-based chemotherapy as a first-line treatment between January 2008 and December 2015 were analyzed in this study (Figure S1). The baseline characteristics for both the training and validation datasets are summarized in Table 1. The patient characteristics were comparable between the two groups. As of the last follow-up date of June 30, 2019, the median follow-up time was 64.1 months (range: 3.1–127.6 months). The median OS was 33.6 months (95% CI, 27.9–40.0 months). After first-line chemotherapy, 46 (10%) patients achieved a complete response (CR), and 58 (12.6%) patients had experienced progression disease (PD). The DCR rate for first-line chemotherapy was 87.3%. We did not’ observe any significant difference in survival between the patients in the training and validation cohorts (median OS: 34.3 vs. 29.4 months, respectively; P = 0.120).
Table 1.
Comparison of Baseline Characteristics Between the Training and Validation Datasets
| Variable | Total (N=460) | Training Set (N=296) | Validation Set (N=164) | P-value |
|---|---|---|---|---|
| Age (year), median [IQR] | 46 [39–54] | 46 [39–55] | 46 [40–53] | 0.859 |
| Sex | 1.000 | |||
| Female | 69 (15.0) | 44 (14.9) | 25 (15.2) | |
| Male | 391 (85.0) | 252 (85.1) | 139 (84.8) | |
| Comorbidity | 0.566 | |||
| Absent | 322 (70.0) | 204 (68.9) | 118 (72.0) | |
| Present | 138 (30.0) | 92 (31.1) | 46 (28.0) | |
| BMI (kg/m2), median [IQR] | 20.8 [18.7–23.4] | 20.8 [18.7–23.2] | 21.1 [19.0–23.9] | 0.370 |
| Histology | 0.645 | |||
| Type II | 18 (3.91) | 13 (4.39) | 5 (3.05) | |
| Type III | 442 (96.1) | 283 (95.6) | 159 (97.0) | |
| T category | 0.262 | |||
| T1–2 | 84 (18.3) | 59 (19.9) | 25 (15.2) | |
| T3–4 | 376 (81.7) | 237 (80.1) | 139 (84.8) | |
| N category | 0.170 | |||
| N0–1 | 87 (18.9) | 62 (20.9) | 25 (15.2) | |
| N2–3 | 373 (81.1) | 234 (79.1) | 139 (84.8) | |
| No. of metastatic sites | 0.180 | |||
| Single | 303 (65.9) | 202 (68.2) | 101 (61.6) | |
| Multiple | 157 (34.1) | 94 (31.8) | 63 (38.4) | |
| No. of metastatic lesions | 0.827 | |||
| Single | 97 (21.1) | 61 (20.6) | 36 (22.0) | |
| Multiple | 363 (78.9) | 235 (79.4) | 128 (78.0) | |
| Liver metastasis | 0.403 | |||
| Absent | 307 (66.7) | 193 (65.2) | 114 (69.5) | |
| Present | 153 (33.3) | 103 (34.8) | 50 (30.5) | |
| Bone metastasis | 0.799 | |||
| Absent | 155 (33.7) | 98 (33.1) | 57 (34.8) | |
| Present | 305 (66.3) | 198 (66.9) | 107 (65.2) | |
| Lung metastasis | 0.655 | |||
| Absent | 327 (71.1) | 213 (72.0) | 114 (69.5) | |
| Present | 133 (28.9) | 83 (28.0) | 50 (30.5) | |
| Pretreatment EBV DNA | 0.001 | |||
| Negative | 67 (14.6) | 44 (14.9) | 23 (14.0) | |
| Positive | 356 (77.4) | 217 (73.3) | 139 (84.8) | |
| Missing | 37 (8.0) | 35 (11.8) | 2 (1.2) | |
| LDH (U/L), median [IQR] | 209 [173–298] | 207 [173–293] | 211 [174–304] | 0.417 |
| CRP (mg/L), median [IQR] | 3.93 [1.30–13.7] | 3.78 [1.16–14.9] | 4.17 [1.52–12.2] | 0.649 |
| ALP (U/L), median [IQR) | 82.0 [68.2–101] | 80.1 [67.9–99.2] | 85.4 [69.7–105] | 0.054 |
| GPS | 0.559 | |||
| 0 | 319 (69.3) | 202 (68.2) | 117 (71.3) | |
| 1–2 | 141 (30.7) | 94 (31.8) | 47 (28.7) | |
| NLR, median [IQR] | 2.70 [1.92–3.79] | 2.68 [1.88–3.75] | 2.78 [1.96–3.80] | 0.763 |
| PLR, median [IQR] | 142 [107–194] | 141 [104–193] | 143 [111–200] | 0.917 |
| SII, median [IQR] | 648 [426–1056] | 642 [416–1054] | 665 [471–1059] | 0.479 |
| PNI, median [IQR] | 52.2 [48.5–55.3] | 52.2 [48.5–55.5] | 52.3 [48.5–54.6] | 0.487 |
| NRI, median [IQR] | 107 [102–112] | 107 [101–112] | 107 [102–112] | 0.661 |
| CONUT score | 0.117 | |||
| 3–4 | 389 (84.6) | 244 (82.4) | 145 (88.4) | |
| 5–6 | 71 (15.4) | 52 (17.6) | 19 (11.6) |
Note: Statistical comparisons of patient characteristics between groups were analyzed using the Mann–Whitney U-tests (for continuous variables) or χ2 tests (for categorical variables).
Abbreviations: BMI, body mass index; EBV, Epstein-Barr virus; LDH, lactate dehydrogenase; CRP, C reactive protein; ALP, alkaline phosphatase; GPS, Glasgow prognostic score; NLR, neutrophil-lymphocyte ratio; PLR, platelet-to-lymphocyte ratio; SII, systemic immune-inflammation index; PNI, prognostic nutritional index; NRI, nutrition risk index; CONUT score, controlling nutritional status score.
Development of Risk-Scoring System
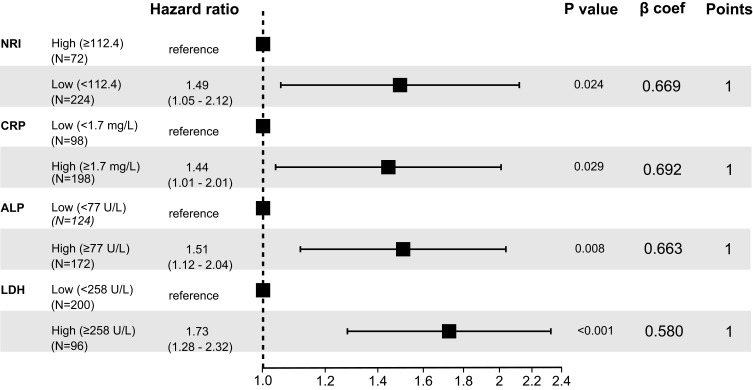
First, we categorized the candidate continuous variables based on the optimal cutoff values, as determined by the Maximally Selected Rank Statistics in the training dataset. We evaluated the prognostic impacts of each candidate on PFS using the Kaplan-Meier method (Figures S2–S11). Those variables with a log-rank P-value of less than 0.05, including CRP, LDH, and ALP levels, GPS, SII, PNI, and NRI, were entered into the step-wise multivariable analysis. The independent risk factors (with P-values < 0.05) identified by the final model (with the lowest AIC of 1987.9) were selected for the scoring system, including NRI, CRP, ALP, and LDH levels. Multicollinearity diagnostic tests, including pair-wise correlations, variance inflation factor plots, and Eigenvalue plots, showed no evidence of severe multicollinearity issues (Figures S12 and S13). We then assigned points proportional to the regression coefficients for each of the four prognostic factors to design a risk score (Figure 1). Here, 1 point was allocated to each of the four prognostic risk factors was allocated. Subsequently, the points corresponding to the risk factors associated with each patient were summed to obtain a total risk score, which was named the prognostic nutrition and inflammation index (PNII) score. Finally, patients were categorized into low (0–1 point), intermediate (2–3 points), and high (4 points) PNII groups based on their total risk scores.
Figure 1.
The four independent risk factors in the final model were illustrated in a forest plot and selected for developing the scoring system, including nutritional risk index, C-reactive protein, alkaline phosphatase, and lactate dehydrogenase. The assignment of points to each variable was based on the corresponding β regression coefficient. Each variable’s coefficient was divided by 0.580 (the lowest β value, corresponding to lactate dehydrogenase) and rounded to the nearest integer.
Predictive Performance of PNII Score
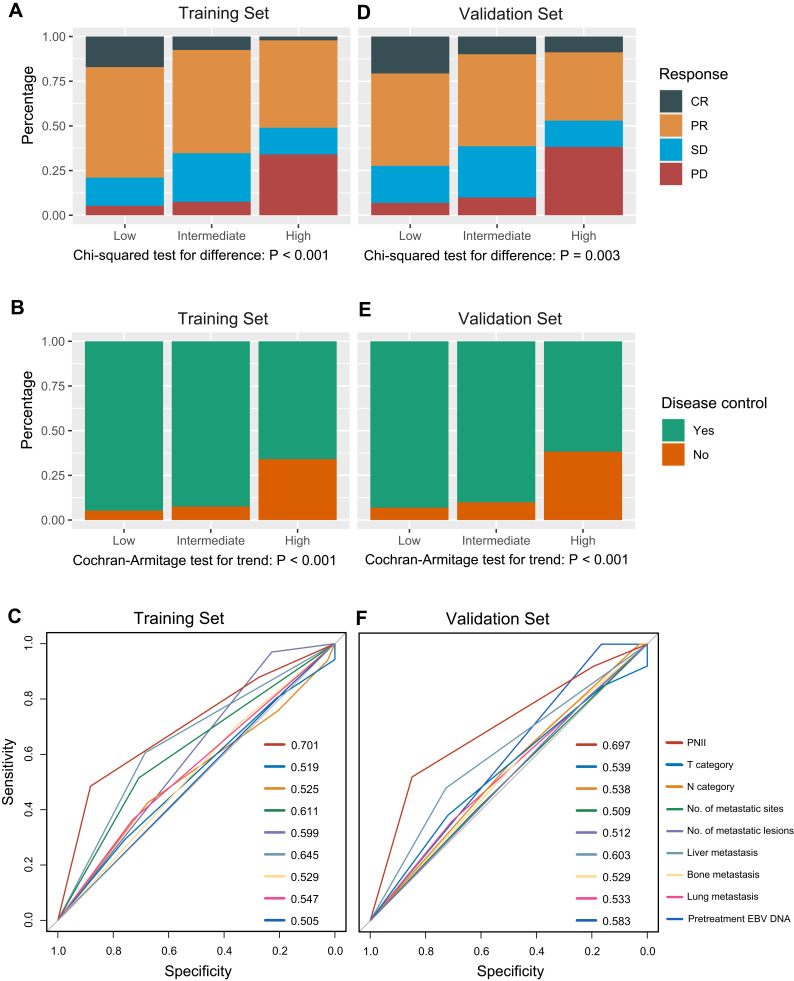
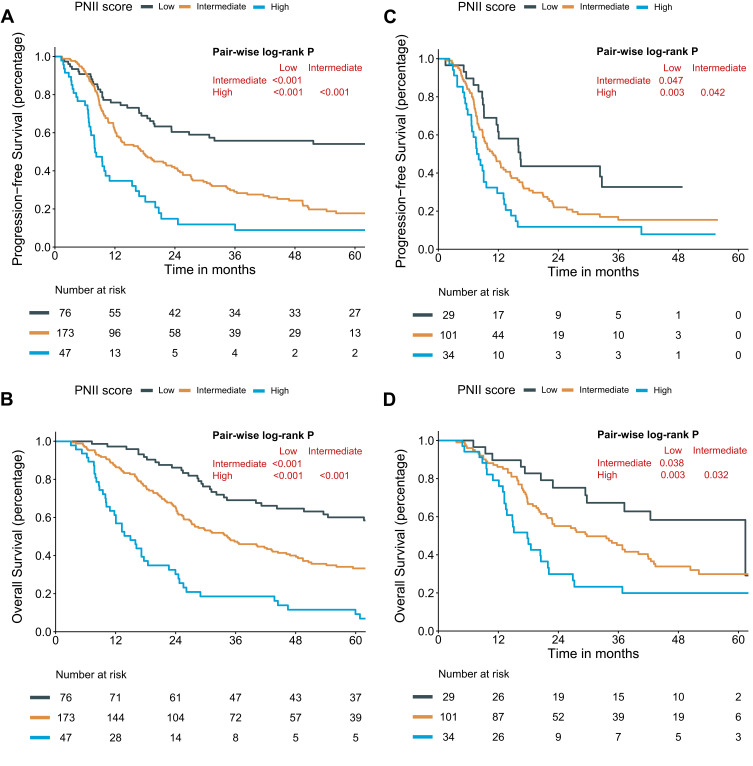
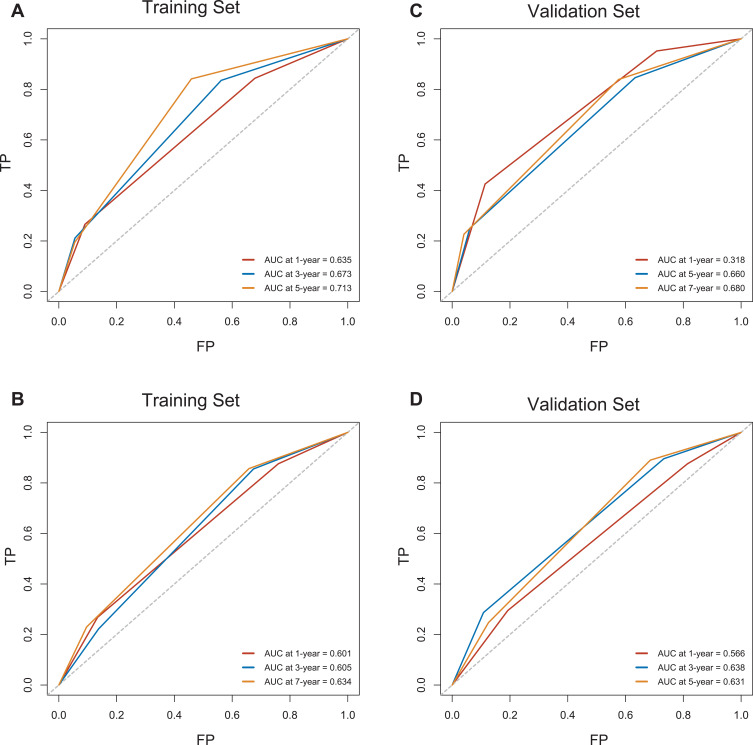
The distribution of chemotherapeutic responses for each PNII category within the training cohort is illustrated in Figure 2A. A significant difference in response was observed across the three groups (χ2 test, P < 0.001). The rates of CR and PD among the low-, intermediate- and high-PNII score groups were 17.1% and 5.3%, 7.5% and 7.5%, and 2.1% and 34.0%, respectively. The DCR showed a significantly decreasing trend from the low- to high-PNII score groups (Cochran-Armitage trend test, P < 0.001, Figure 2B). The discriminative ability of the PNII score to predict short-term disease control, as measured by the AUC, was 0.701 (95% CI: 0.604–0.797, Figure 2C), which was significantly higher than the predictive abilities of any traditional baseline factors. Survival analyses based on PFS and OS, either crude or with adjustments, indicated that patients with higher PNII scores were significantly associated with unfavorable outcomes (Table S3). The 3-year PFS and OS probabilities for the low-, medium-, and high-PNII score subgroups were 55.8% and 69.1%, 29.1% and 47.4%, and 11.9% and 18.6%, respectively (Figure 3A and B, all log-rank P < 0.001). As measured by the time-independent AUC, the predictive accuracies of the PNII score were 0.713 and 0.634 for 5-year PFS and OS, respectively (Figure 4A and B). In addition, the PNII scores were well-calibrated, based on the Gronnesby and Borgan goodness-of-fit test (for PFS: χ2=5.8, P = 0.214; for OS: χ2=7.5, P = 0.110).
Figure 2.
The distribution of chemotherapy responses (A) and disease control (B) for each prognostic nutrition and inflammation index (PNII) category in the training cohort. The PNII score’s performance for predicting short-term disease control against other traditional baseline factors in the training cohort (C). The distribution of chemotherapy responses (D) and disease control (E) for each prognostic nutrition and inflammation index (PNII) category in the validation cohort. The PNII score’s performance for predicting short-term disease control against other traditional baseline factors in the validation cohort (F).
Figure 3.
Survival curves for progression-free survival and overall survival stratified by prognostic nutrition and inflammation index (PNII) category in the training (A, B) and validation (C, D) cohorts.
Figure 4.
The predictive accuracy of the prognostic nutrition and inflammation index (PNII) score for progression-free survival and overall survival in the training (A, B) and validation (C, D) cohorts.
Validation of PNII Score
The distribution of chemotherapy responses for each risk subgroup in the validation cohort is shown in Figure 2D. A significant difference was observed across the three risk groups (χ2 test, P = 0.003). The rates of CR and PD for the low-, intermediate-, and high-PNII score groups were 20.7% and 6.9%, 9.9% and 9.9%, and 8.8% and 33.2%, respectively. The DCR showed a significantly reducing trend from the low- to high-risk groups (Cochran-Armitage trend test, P < 0.001, Figure 2E). The discriminative ability of the PNII score for the prediction of short-term disease control, as measured by the AUC, was 0.697 (95% CI: 0.587–0.807, Figure 2F), which outperformed the discriminative abilities of other baseline factors. Survival analyses according to PFS and OS, either alone or adjusted, revealed that patients with higher PNII scores were significantly associated with poor prognosis (Table S3). The 3-year PFS and OS probabilities for the low-, medium-, and high-PNII subgroups were 32.4% and 67.3%, 15.4% and 45.1%, and 11.8% and 23.2%, respectively (Figure 3C and D, all log-rank P < 0.05). As measured by the time-dependent AUC, the predictive performances of the PNII score were 0.680 and 0.631 for 5-year PFS and OS, respectively (Figure 4C and D). The PNII score was also well-calibrated in the validation cohort according to the Gronnesby and Borgan goodness-of-fit test (for PFS: χ2=1.6, P=0.448; for OS: χ2=4.6, P = 0.102).
Discussion
Over the past few decades, the optimal treatment strategy for mNPC has remained controversial but has recently shifted towards personalized medicine.27–29 Platinum-based chemotherapy is the current standard of care for de novo mNPC, as recommended by current NCCN guidelines.20 The combination of immune checkpoint inhibitors and chemotherapy has demonstrated promising antitumor activity with manageable adverse effects for both treatment-naïve and previously treated recurrent or metastatic disease.29–31 In addition to systemic therapy, locoregional radiotherapy combined with chemotherapy was associated with significantly prolonged OS in chemotherapy-sensitive de novo mNPC patients.21,22 Therefore, we believe that the pretherapy prediction of first-line chemotherapy efficacy is crucial for the timely identification of patients who might have an inadequate response to chemotherapy, allowing personalized treatment recommendations to be designed from the start.
To our knowledge, this is the first study that has developed a clinically applicable tool for the prediction of first-line chemotherapy efficacy among patients with de novo mNPC. Using a relatively large cohort, we designed and validated a risk-scoring system (PNII score) based on four readily ascertainable baseline factors. The PNII score accurately predicted both short-term disease control and long-term survival outcomes among patients who received platinum-based chemotherapy as first-line treatments. The PNII score could serve as a simple-to-use tool for the guidance of treatment strategies prior to initiating first-line chemotherapy. Based on the PNII scoring system, patients were stratified into three prognostic subgroups with varying DCRs and survival outcomes. The low- and intermediate-PNII score groups showed high DCR values, exceeding 90%, indicating a better chance of benefiting from locoregional radiotherapy. In contrast, the high-PNII score groups had lower DCRs and higher HRs for OS and PFS than those in the low- and intermediate-PNII score groups. Therefore, for those patients in the high-PNII score groups, chemotherapy combined with immune checkpoint inhibitors or other targeted therapies should be recommended to achieve better disease control and increase the likelihood of receiving subsequent curative treatments.
In the current study, one nutritional index (NRI) and three inflammation-related biomarkers (CRP, ALP, and LDH levels) were identified as being significantly correlated with chemotherapy efficacy and survival outcomes in patients with de novo mNPC. Patients diagnosed with malnutrition risk factors and elevated systemic inflammation were more likely to suffer from an insufficient response to chemotherapy and poor prognosis than those without malnutrition or inflammation indicators. Our results agreed with the results reported by previous studies investigating single nutritional or inflammatory parameters in NPC.13–16,32–34 Severe nutritional risks and elevated levels of CRP, ALP, and LDH have been associated with worse survival outcomes. Our results indicated that measurements of nutritional and inflammatory status might reflect the true tumor status o and predict chemotherapeutic efficacy in patients with de novo mNPC. Patients who present with systemic inflammation and malnutrition represent an under-appreciated sub-population that might require personalized therapy.
However, the underlying biological mechanisms responsible for the correlation observed among these biomarkers, treatment effectiveness, and prognosis remain far from being fully understood. Cancer-related inflammation involves complex interactions between the tumor and host immune and inflammatory responses, which could represent potential targets of cancer treatments.3,35 Cancer-related inflammation is a well-recognized cancer hallmark that substantially regulates all phases of malignancies, including susceptibility, initiation, development, dissemination, and mortality. Mediators of systemic inflammation comprise circulating immune cells, circulating cytokines, small inflammatory proteins, and acute-phase proteins.3 Both CRP and LDH are acute-phase proteins. CRP is primarily synthesized in hepatocytes in response to proinflammatory cytokines before being secreted into the blood. Our previous studies have demonstrated that elevated CRP levels were correlated with more advanced disease stages, including increased metastatic risk in patients with nonmetastatic NPC and decreased survival in metastatic NPC patients treated with palliative chemotherapy.34,36 Unlike CRP, LDH plays an essential role in the promotion of glycolysis. LDH is abundant in many different cell types, although the blood levels are generally low. The increased levels of circulating LDH in cancer patients have primarily been attributed to LDH release from malignant cells.37,38 The selective inhibition of LDH may, therefore, represent a potential therapeutic target for cancer treatments designed to target cancer metabolism.37,38
Similar to CRP and LDH, ALP is another accepted biomarker of systemic inflammation. ALP is a ubiquitous enzyme that is primarily secreted from the liver, bone, and a wide variety of tumors.39–41 ALP levels often increase together with CRP or LDH levels, such as in metabolic syndrome and some types of cancers. ALP has been identified to serve as a reliable indicator for the prediction of prognosis associated with several malignancies, including NPC.21,32,41 Currently, the exact mechanisms and functions through which ALP is associated with tumor progression remain undefined; however, elevated tumor-derived ALP has been demonstrated to regulate cancer cell proliferation, death, and epithelial plasticity.42,43 These findings suggested that ALP could be a potential therapeutic target, and recent studies have shown that bone-targeted ALP can act as a form of enzyme replacement therapy for hypophosphatasia, highlighting the promising role of ALP as a therapeutic target.44
In addition to the vital roles played by the mediators mentioned above, systemic inflammation has also been correlated with malnutrition, muscle loss, and cachexia development.45 Many lines of evidence have revealed that the activation of a sustaining, chronic, systemic inflammatory response represents one of the earliest and most essential contributing factors for the development of cachexia.46 High levels of circulating cytokines and chemokines play crucial roles in driving the interplay between systemic inflammation, tumor progression, and cachexia.3 Therefore, patients who present with severe systemic inflammation are more likely to suffer from malnutrition. In our study, patients associated with a high risk of malnutrition were also associated with worse survival, in agreement with the findings of several previous studies of nonmetastatic NPC.13–16 Because nutritional status has significant impacts on prognosis, the identification of patients who are at high risk of malnutrition and providing nutritional intervention as early as possible is essential to improving disease outcomes.
The present cohort study has some inevitable limitations. First, this study was performed as a retrospective study, which is associated with the inherent potential for selection bias. Second, the study population was based on patients who had the appropriate measurements of the selected markers; thus, the patient cohorts used in this study are not necessarily representative of all cancer patients who are diagnosed and treated at our institution. Finally, patients who have cancer might also have been diagnosed with some accompanying diseases that can cause changes in the investigated markers, such as metabolic syndrome, hepatic diseases, and skeletal disease. In the current study, 138 (30%) patients were presented with comorbidities, including 43 (9.4%) hepatitis, 22 (4.8%) hypertension, 15 (3.3%) diabetes. Notably, our exploratory sensitivity analysis (Figures S14 and S15) revealed that our findings were quite robust, regardless of comorbidity status. Therefore, the effectiveness of the PNII score would not be hampered by the non-cancer related inflammation in this study.
Conclusion
In conclusion, we developed a clinically useful risk-scoring system based on four readily ascertainable factors that were able to predict the efficacy of first-line chemotherapeutic and survival outcomes for patients with de novo mNPC. This system may help clinicians determine the necessity of personalized treatment strategies before the initiation of first-line treatment. Further external verification of this scoring system remains necessary.
Acknowledgments
The first three authors contributed equally to this manuscript. Dr. Shu-Hui Lv has recently taken up a new post in the Medical Affairs Office of the Fifth Affiliated Hospital of Sun Yat-sen University (Zhuhai, 519000, China).
Funding Statement
This study is supported by the National Natural Science Foundation of China (No. 81672680 and 81802712), the Guangdong Medical Research Foundation (No. A2017492), and the Young Teacher Training Project of Sun Yat-Sen University (No. 19ykpy188).
Data Sharing Statement
This article’s authenticity has been validated by uploading the critical raw data onto the Research Data Deposit public platform (www.researchdata.org.cn), with the approval RDD number as RDDA2020001582.
Ethics Approval and Informed Consent
Chinese Ethics Committee of Registering Clinical Trials approved this study (registration number: ChiCTR2100042432). Informed consent was waived due to this study’s retrospective nature and the anonymization of patient data.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
- 1.Tsao SW, Tsang CM, Lo KW. Epstein-barr virus infection and nasopharyngeal carcinoma. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 2017;372(1732):1732. doi: 10.1098/rstb.2016.0270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hanahan D, Weinberg R. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–674. doi: 10.1016/j.cell.2011.02.013 [DOI] [PubMed] [Google Scholar]
- 3.Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15(11):e493–e503. doi: 10.1016/S1470-2045(14)70263-3 [DOI] [PubMed] [Google Scholar]
- 4.Shinko D, Diakos CI, Clarke SJ, Charles KA. Cancer-related systemic inflammation: the challenges and therapeutic opportunities for personalized medicine. Clin Pharmacol Ther. 2017;102(4):599–610. doi: 10.1002/cpt.789 [DOI] [PubMed] [Google Scholar]
- 5.Putzu C, Cortinovis DL, Colonese F, et al. Blood cell count indexes as predictors of outcomes in advanced non-small-cell lung cancer patients treated with nivolumab. Cancer Immunol Immunother. 2018;67(9):1349–1353. doi: 10.1007/s00262-018-2182-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aziz MH, Sideras K, Aziz NA, et al. The systemic-immune-inflammation index independently predicts survival and recurrence in resectable pancreatic cancer and its prognostic value depends on bilirubin levels: a Retrospective Multicenter Cohort Study. Ann Surg. 2019;270(1):139–146. doi: 10.1097/SLA.0000000000002660 [DOI] [PubMed] [Google Scholar]
- 7.Varkaris A, Katsiampoura A, Davis JS, et al. Circulating inflammation signature predicts overall survival and relapse-free survival in metastatic colorectal cancer. Br J Cancer. 2019;120(3):340–345. doi: 10.1038/s41416-018-0360-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Galvano A, Peri M, Guarini AA, et al. Analysis of systemic inflammatory biomarkers in neuroendocrine carcinomas of the lung: prognostic and predictive significance of NLR, LDH, ALI, and LIPI score. Ther Adv Med Oncol. 2020;12:1758835920942378. doi: 10.1177/1758835920942378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Banna GL, Signorelli D, Metro G, et al. Neutrophil-to-lymphocyte ratio in combination with PD-L1 or lactate dehydrogenase as biomarkers for high PD-L1 non-small cell lung cancer treated with first-line pembrolizumab. Transl Lung Cancer Res. 2020;9(4):1533–1542. doi: 10.21037/tlcr-19-583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marinari E, Allard M, Gustave R, et al. Inflammation and lymphocyte infiltration are associated with shorter survival in patients with high-grade glioma. Oncoimmunology. 2020;9(1):1779990. doi: 10.1080/2162402X.2020.1779990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van Berckelaer C, Van Geyt M, Linders S, et al. A high neutrophil-lymphocyte ratio and platelet-lymphocyte ratio are associated with a worse outcome in inflammatory breast cancer. Breast. 2020;53:212–220. doi: 10.1016/j.breast.2020.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zengin M, Karahan İ. The role of cancer-related inflammation for prediction of poor survival in postmenopausal female patients with stage II/III colon cancer. Int Immunopharmacol. 2020;85:106624. doi: 10.1016/j.intimp.2020.106624 [DOI] [PubMed] [Google Scholar]
- 13.Tu X, Ren J, Zhao Y. Prognostic value of prognostic nutritional index in nasopharyngeal carcinoma: a meta-analysis containing 4511 patients. Oral Oncol. 2020;110:104991. doi: 10.1016/j.oraloncology.2020.104991 [DOI] [PubMed] [Google Scholar]
- 14.Miao J, Xiao W, Wang L, et al. The value of the Prognostic Nutritional Index (PNI) in predicting outcomes and guiding the treatment strategy of nasopharyngeal carcinoma (NPC) patients receiving intensity-modulated radiotherapy (IMRT) with or without chemotherapy. J Cancer Res Clin Oncol. 2017;143(7):1263–1273. doi: 10.1007/s00432-017-2360-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peng H, Chen B, Tang L, et al. Prognostic value of nutritional risk screening 2002 scale in nasopharyngeal carcinoma: a large-scale cohort study. Cancer Sci. 2018;109(6):1909–1919. doi: 10.1111/cas.13603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deng J, He Y, Sun X, et al. Construction of a comprehensive nutritional index and its correlation with quality of life and survival in patients with nasopharyngeal carcinoma undergoing IMRT: a prospective study. Oral Oncol. 2019;98:62–68. doi: 10.1016/j.oraloncology.2019.09.014 [DOI] [PubMed] [Google Scholar]
- 17.Kubo N, Sakurai K, Tamura T, et al. The impact of geriatric nutritional risk index on surgical outcomes after esophagectomy in patients with esophageal cancer. Esophagus. 2019;16(2):147–154. doi: 10.1007/s10388-018-0644-6 [DOI] [PubMed] [Google Scholar]
- 18.Mao Y, Hao S, Zou C, Xie Z, Fu D. Controlling nutritional status score is superior to prognostic nutritional index score in predicting survival and complications in pancreatic ductal adenocarcinoma: a Chinese propensity score matching study. Br J Nutr. 2020;1–8. doi: 10.1017/S0007114520004195 [DOI] [PubMed] [Google Scholar]
- 19.Lee S, Fujita K, Morishita T, et al. Prognostic utility of a geriatric nutritional risk index in combination with a comorbidity index in elderly patients with diffuse large B cell lymphoma. Br J Haematol. 2021;192(1):100–109. [DOI] [PubMed] [Google Scholar]
- 20.National comprehensive cancer network head and neck cancers, version 2.June 9, 2020. Available from: http://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf. Accessed October22, 2020.
- 21.Li W-Z, Lv S-H, Liu G-Y, et al. Development of a prognostic model to identify the suitable definitive radiation therapy candidates in de novo metastatic nasopharyngeal carcinoma: a Real-World Study. Int J Radiat Oncol Biol Phys. 2021;109(1):120–130. doi: 10.1016/j.ijrobp.2020.08.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.You R, Liu Y-P, Huang P-Y, et al. Efficacy and safety of locoregional radiotherapy with chemotherapy vs chemotherapy alone in de novo metastatic nasopharyngeal carcinoma: a multicenter phase 3 randomized clinical trial. JAMA Oncol. 2020;6(9):1345. doi: 10.1001/jamaoncol.2020.1808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bouillanne O, Morineau G, Dupont C, et al. Geriatric nutritional risk index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr. 2005;82(4):777–783. doi: 10.1093/ajcn/82.4.777 [DOI] [PubMed] [Google Scholar]
- 24.Eisenhauer E, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–247. doi: 10.1016/j.ejca.2008.10.026 [DOI] [PubMed] [Google Scholar]
- 25.Sakamoto Y, Ishiguro M, Kitagawa G. Akaike information criterion statistics. Dordrecht Netherlands D Reidel. 1986;81(10.5555):26853. [Google Scholar]
- 26.van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):67%. [Google Scholar]
- 27.Chan O, Ngan R. Individualized treatment in stage IVC nasopharyngeal carcinoma. Oral Oncol. 2014;50(9):791–797. doi: 10.1016/j.oraloncology.2014.01.004 [DOI] [PubMed] [Google Scholar]
- 28.Prawira A, Oosting SF, Chen TW, et al. Systemic therapies for recurrent or metastatic nasopharyngeal carcinoma: a systematic review. Br J Cancer. 2017;117(12):1743–1752. doi: 10.1038/bjc.2017.357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen Y, Chan A, Le Q, Blanchard P, Sun Y, Ma J. Nasopharyngeal carcinoma. Lancet. 2019;394(10192):64–80. doi: 10.1016/S0140-6736(19)30956-0 [DOI] [PubMed] [Google Scholar]
- 30.Fang W, Yang Y, Ma Y, et al. Camrelizumab (SHR-1210) alone or in combination with gemcitabine plus cisplatin for nasopharyngeal carcinoma: results from two single-arm, Phase 1 trials. Lancet Oncol. 2018;19(10):1338–1350. doi: 10.1016/S1470-2045(18)30495-9 [DOI] [PubMed] [Google Scholar]
- 31.Wang F, Wei X, Feng J, et al. Efficacy, safety, and correlative biomarkers of toripalimab in previously treated recurrent or metastatic nasopharyngeal carcinoma: a phase II clinical trial (POLARIS-02). J Clin Oncol. 2021;39(7):704–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jin Y, Cai XY, Cai YC, et al. To build a prognostic score model containing indispensible tumour markers for metastatic nasopharyngeal carcinoma in an epidemic area. Eur J Cancer. 2012;48(6):882–888. doi: 10.1016/j.ejca.2011.09.004 [DOI] [PubMed] [Google Scholar]
- 33.Jin Y, Ye X, Shao L, et al. Serum lactic dehydrogenase strongly predicts survival in metastatic nasopharyngeal carcinoma treated with palliative chemotherapy. Eur J Cancer. 2013;49(7):1619–1626. doi: 10.1016/j.ejca.2012.11.032 [DOI] [PubMed] [Google Scholar]
- 34.Xia WX, Ye YF, Lu X, et al. The impact of baseline serum C-reactive protein and C-reactive protein kinetics on the prognosis of metastatic nasopharyngeal carcinoma patients treated with palliative chemotherapy. PLoS One. 2013;8(10):e76958. doi: 10.1371/journal.pone.0076958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Choi Y, Kim JW, Nam KH, et al. Systemic inflammation is associated with the density of immune cells in the tumor microenvironment of gastric cancer. Gastric Cancer. 2017;20(4):602–611. doi: 10.1007/s10120-016-0642-0 [DOI] [PubMed] [Google Scholar]
- 36.Xia WX, Zhang HB, Shi JL, et al. A prognostic model predicts the risk of distant metastasis and death for patients with nasopharyngeal carcinoma based on pretreatment serum C-reactive protein and N-classification. Eur J Cancer. 2013;49(9):2152–2160. doi: 10.1016/j.ejca.2013.03.003 [DOI] [PubMed] [Google Scholar]
- 37.Feng Y, Xiong Y, Qiao T, Li X, Jia L, Han Y. Lactate dehydrogenase A: a key player in carcinogenesis and potential target in cancer therapy. Cancer Med. 2018;7(12):6124–6136. doi: 10.1002/cam4.1820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang SL, He Y, Tam KY. Targeting cancer metabolism to develop human lactate dehydrogenase (hLDH)5 inhibitors. Drug Discov Today. 2018;23(7):1407–1415. doi: 10.1016/j.drudis.2018.05.014 [DOI] [PubMed] [Google Scholar]
- 39.Liu -C-C, Ahearn JM. Chapter 10 - acute-phase proteins and inflammation: immunological and clinical implications. In: Lotze MT, Thomson AW, editors. Measuring Immunity. London: Academic Press; 2005:131–143. [Google Scholar]
- 40.Cheung BM, Ong KL, Cheung RV, et al. Association between plasma alkaline phosphatase and C-reactive protein in Hong Kong Chinese. Clin Chem Lab Med. 2008;46(4):523–527. doi: 10.1515/CCLM.2008.111 [DOI] [PubMed] [Google Scholar]
- 41.Namikawa T, Ishida N, Tsuda S, et al. Prognostic significance of serum alkaline phosphatase and lactate dehydrogenase levels in patients with unresectable advanced gastric cancer. Gastric Cancer. 2019;22(4):684–691. doi: 10.1007/s10120-018-0897-8 [DOI] [PubMed] [Google Scholar]
- 42.Kojima Y, Sakurada T. Increase in alkaline phosphatase activity in the liver of mice bearing ehrlich ascites tumor. Cancer Res. 1976;36(1):23–27. [PubMed] [Google Scholar]
- 43.Rao SR, Snaith AE, Marino D, et al. Tumour-derived alkaline phosphatase regulates tumour growth, epithelial plasticity and disease-free survival in metastatic prostate cancer. Br J Cancer. 2017;116(2):227–236. doi: 10.1038/bjc.2016.402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Whyte MP, Greenberg CR, Salman NJ, et al. Enzyme-replacement therapy in life-threatening hypophosphatasia. N Engl J Med. 2012;366(10):904–913. doi: 10.1056/NEJMoa1106173 [DOI] [PubMed] [Google Scholar]
- 45.McMillan DC. The systemic inflammation-based glasgow prognostic score: a decade of experience in patients with cancer. Cancer Treat Rev. 2013;39(5):534–540. doi: 10.1016/j.ctrv.2012.08.003 [DOI] [PubMed] [Google Scholar]
- 46.McMillan DC. An inflammation-based prognostic score and its role in the nutrition-based management of patients with cancer. Proc Nutr Soc. 2008;67(3):257–262. doi: 10.1017/S0029665108007131 [DOI] [PubMed] [Google Scholar]