Abstract
Objectives:
Support from one’s spouse has long been documented as a significant determinant of health for married individuals. However, non-spousal family support may play an important role in health particularly for unmarried individuals. Therefore, this study examined whether the association between non-spousal family support and diagnosis of heart problems differed by marital status and whether gender and education moderated these associations.
Design:
Data came from the first two waves of the Midlife in the United States (MIDUS) study. This study selected respondents who participated in both waves of MIDUS and were not diagnosed with a heart problem at Wave 1 (N = 3,119).
Main Outcome Measures:
Participants reported whether they had any heart trouble. Discrete-time event history analysis was used to examine the risk of heart problems between MIDUS Waves 1 and 2.
Results:
A higher level of non-spousal family support was associated with a lower risk of developing a heart problem only among unmarried women and unmarried individuals with high school education or less, and not for married individuals.
Conclusion:
Findings highlight the importance of considering specific sources of family support when studying heart health, and the health-protective role of non-spousal family support for those who are not married.
Keywords: health outcomes, social support, event history methods, family relationships
Introduction
Heart diseases such as coronary artery disease and heart failure are the leading cause of death in the U.S. More than 630,000 deaths in the U.S. are caused by heart disease each year, representing one-fourth of all deaths in 2015 (Murphy, Xu, Kochanek, Curtin, & Arias, 2017). As a result, much effort has been directed towards identifying the risk and protective factors related to heart disease, in the hopes of finding ways to prevent or decrease its prevalence.
Among the numerous biological, social, environmental, and behavioural correlates of heart disease, family support has shown a strong association with cardiovascular health outcomes including the onset of the disease (Uchino & Way, 2017). Among the different types of family support including material and emotional resources (Brummett, Barefoot, Vitaliano, & Siegler, 2003), perceived emotional support from family in particular (hereinafter referred to as family support) has found to be more consistently beneficial for health compared to receiving tangible support (Reinhardt, Boerner, & Horowitz, 2006; Uchino, 2009). Those who have dependable and emotionally supportive family members develop a sense of belonging and companionship, which contribute to better physical health including cardiovascular outcomes (House, Landis, & Umberson, 1988). Emotional support from family members can also encourage individuals to engage in health-promoting behaviours (e.g., exercise, healthy diet) and avoid risky behaviours (e.g., excessive drinking, smoking), thereby lowering the risk of having a heart problem (Gruenewald & Seeman, 2010).
Although prior research generally suggests that family support is a significant correlate of heart problems, many studies fail to differentiate the various sources of family support. This is an important factor to consider, as family support is found to have stronger associations with health when they come from the most primary tie (Walen and Lachman, 2000). According to the convoy model of social relations (Antonucci, Ajrouch, & Birditt, 2013; Antonucci, Birditt, & Akiyama, 2009), an individual’s family network is composed of multiple relationships (i.e., convoys) that vary in their closeness and function. Spouses are mostly placed in the closest inner circle of the support network, while other family members are spread in closer inner or middle circles (Antonucci & Akiyama, 1987).
Due to the saliency of spouses as a primary source of support, numerous studies have found significant associations between marital interaction and relationship functioning and various indicators of heart health including heart rate variability, blood pressure, and coronary-artery calcification (Birditt, Newton, & Hope, 2012; Donoho, Seeman, Sloan, & Crimmins, 2015; Uchino, Smith, & Berg, 2014). On the other hand, the role of support from family members other than spouses in heart health has received much less attention as it was considered to be a secondary source of support. However, the convoy model posits that the importance of supportive functions is determined by the individual’s personal or situational factors such as sociodemographic characteristics (Antonucci et al., 2013).
Marital status can be one of the determinants that influence how much non-spousal family support would matter to an individual. For married individuals, receiving support from family members other than the spouse may not be so central to health because their spouses function as a core source of support. However, for unmarried individuals without a spouse (e.g., divorced, separated, widowed, or never married), other family members may take on the role as the closest source of support. This is also in line with the hierarchical-compensatory model of social care (Cantor, 1979; 1991), which suggests that the support system of an individual follows a hierarchy based on the primacy of the relationship. When ties in the upper hierarchy (i.e., spouses) are missing, their supportive role is substituted by the ties in the lower hierarchy (i.e., other family members). Therefore, family members other than the spouse may serve a primary supportive function for the unmarried individuals, and non-spousal family support may have stronger associations with heart health among the unmarried individuals compared to married individuals.
The implications of non-spousal family support on heart health may also differ by sociodemographic characteristics such as gender and level of education. Studies generally find that women have stronger family relationships than men (Thompson & Walker, 1989; West & Zimmerman, 1987). Women actively engage in creating and maintaining kin networks and have more intimate ties than men (Marks & McLanahan, 1993). Because women have more supportive and closer ties, they seek and use more support from their family members and benefit more from the support they receive compared to men (Perrewé & Carlson, 2002). Furthermore, since the meaning and importance of support tends to be greater for women, the benefits of receiving family support on decreasing the risk of heart disease may be stronger for women (Shumaker & Hill, 1991).
Having strong family support may also be particularly important for individuals with lower levels of education (Schöllgen, Huxhold, Schüz, & Tesch-Römer, 2011). Numerous studies consistently find that those with less education are at higher risk of experiencing cardiovascular disease (Havranek et al., 2015; Mensah, Mokdad, Ford, Greenlund, & Croft, 2005), due to the prolonged exposure to chronic stressors such as financial constraints or unemployment that trigger risky health habits (Havranek et al., 2015) and physiological dysregulation (Steptoe, 2011). Because of limited access to resources that can protect them against the detrimental effects of disadvantaged SES backgrounds, family members often function as the most reliable source of support for less educated adults. Family members can provide necessary knowledge about health care, encourage and monitor healthy behaviours, and help with positive reframing and reappraisal of the given situation (Pietromonaco & Collins, 2017). Therefore, receiving such support from family can be particularly beneficial for the less educated who otherwise lack protective resources for health.
This study assessed whether the prospective links between non-spousal family support and heart disease differed by marital status. We examined the effects of non-spousal family support on the subsequent risk of being diagnosed with a heart problem separately for married and unmarried individuals. Furthermore, this study also tested whether these associations differed by gender and level of education. Based on previous studies of support, gender, and education (Perrewé & Carlson, 2002; Ross & Mirowsky, 2010; Shumaker & Hill, 1991), we hypothesized that higher levels of non-spousal family support would be associated with a lower risk of being diagnosed with a heart problem among the unmarried compared to the married, particularly for women and those with lower levels of education.
Methods
Data and Sample
This study used Waves 1 and 2 of the Midlife in the United States (MIDUS) data (Brim, Ryff, & Kessler, 2004), collected in 1995–1996 for Wave 1, and 2004–2006 for Wave 2. MIDUS interviewed and surveyed a national probability sample of non-institutionalized, English-speaking adults aged between 20 and 75 when it began in 1995, and then carried out a longitudinal follow-up survey 9 to 10 years later. The baseline sample was composed of individuals recruited nationally via random digit dialing (RDD) of phone numbers selected from working telephone banks and with oversampling from five metropolitan areas in the US, siblings of individuals from the RDD sample, and a national RDD sample of twin pairs (Brim et al., 2004).
The sample included in this study were the respondents who participated in both waves of the survey, provided full information about all of the variables used in this study, did not report being diagnosed with a heart problem prior to Wave 1, and marital status remained the same in Waves 1 and 2. Specifically, this study started with 4,953 respondents who provided information about their heart problem diagnosis in both MIDUS Waves 1 and 2. We excluded 722 respondents who reported having been diagnosed with a heart problem prior to Wave 1 (including congenital disease). Among the remaining 4,231 respondents, 513 cases with missing values for one or more key study variables were dropped from the sample. Those who were excluded from analysis due to missing data were younger, less educated, and less likely to be married at Wave 1. There were no significant differences between included and excluded subjects in the levels of spousal and non-spousal family support. Then, 599 individuals whose marital status changed between Waves 1 and 2 (i.e., married to unmarried or unmarried to married) or did not report marital status in Wave 2 were excluded from the study sample. The final analytic sample of this study included 3,119 individuals (2,349 married and 770 unmarried). This study examined the patterns of diagnosis with a heart problem over a period from 1995 to 2006, including 286 individuals (9.17%) who were diagnosed with a heart problem between the two intervals.
Measures
Diagnosis with heart problem.
In both MIDUS Waves 1 and 2, this outcome was measured with the question, “Have you ever had heart trouble suspected or confirmed by a doctor?” For those who reported as having been suspected or diagnosed with a heart problem, MIDUS asked a follow-up question about the age in which they first heard about the heart trouble from a doctor. Based on these two variables, this study excluded the respondents whose age of diagnosis was younger than their age at Wave 1 of MIDUS or those who reported having a congenital heart problem.
To check the validity of the self-reported measurement of heart problems, the cardiovascular health indicators of the subsample of our study who participated in the Biomarker Project of MIDUS Wave 2 (n = 710) were assessed. Independent sample t-test results showed that respondents who reported being diagnosed with a heart problem between MIDUS Waves 1 and 2 had higher systolic blood pressure (p < .05; MWithout a heart problem = 130.83, MWith a heart problem = 136.62) and higher triglyceride levels (p < .05; MWithout a heart problem = 133.72, MWith a heart problem = 169.97), compared to those who were not diagnosed with a heart problem. There was no significant difference in diastolic blood pressure between the two groups. Previous studies have also found self-reporting as a valid measure of cardiovascular conditions such as hypertension and stroke (Okura, Urban, Mahoney, Jacobsen, & Rodeheffer, 2004).
Non-spousal family support and spousal support.
Using data from MIDUS Wave 1, non-spousal family support was measured by taking the mean of four items on non-spousal family support. The items for support in MIDUS were adapted from the scale used by Schuster, Kessler, and Aseltine (1990), and a more detailed description of the scales are available in Walen and Lachman (2000). The four items on non-spousal family support were “Not including your spouse or partner, how much do members of your family really care about you?”, “How much do they understand the way you feel about things?”, “How much can you rely on them for help if you have a serious problem?”, and “How much can you open up to them if you need to talk about your worries?”
For spousal support, the mean of six items was used, including the four questions used for measuring non-spousal support (wordings were changed from members of your family to your spouse or partner). Two additional items used for measuring spouse or partner support were “How much does your spouse or partner appreciate you?” and “How much can you relax and be yourself around your spouse or partner?” The responses to all these items were on a scale of 1 to 4, with 1 = Not at all and 4 = A lot. Cronbach’s alpha for non-spousal and spousal support were α = .83 and α = .90, respectively.
Non-spousal family strain and spousal strain.
Studies on family relationships consider family strain, which refers to unpleasant and aversive interactions and conflicts involving family members, as a distinct dimension of relationship quality independent of support (Rook, 1990; Silverstein, Gans, Lowenstein, Giarrusso, & Bengtson, 2010). Thus, we included measures of spousal and non-spousal family strain as covariates in our models. Non-spousal family strain was measured using the mean of four items on strain from family members other than a spouse or partner. The four items were: “Not including your spouse or partner, how often do members of your family make too many demands on you?”, “How often do they criticise you?”, “How often do they let you down when you are counting on them?”, and “How often do they get on your nerves?” For spousal strain, the wordings for these four items were changed from members of your family to your spouse or partner.
Two additional items used for measuring spouse or partner strain included: “How often does your spouse or partner argue with you?” and “How often does your spouse or partner make you feel tense?” For all six items, the responses ranged from 1 = Never to 4 = Often. Cronbach’s alpha was α = .79 for non-spousal family strain, and α = .87 for spousal strain. Spousal support and strain were included in the analysis as covariates for the married group only, as spouses are considered to be another significant source of support and strain among the married individuals (Uchino et al., 2014). Also, a large proportion of non-married individuals (85.1%) did not respond to spousal or partner support and strain questionnaires.
Sociodemographic variables.
Sociodemographic characteristics included as covariates in this study were gender, race, level of education, logged household income, and age at Wave 1. Race was coded as a binary variable indicating 0 = Non-white and 1 = White. Non-white included black and/or African American, native American or Aleutian Islander/Eskimo, Asian or Pacific Islander, multiracial, and other. Total annual household income was calculated by summing annual income from various sources in the past 12 months for all of the individuals living with the respondent, including earnings from employment, Social Security benefits, government assistance programs, pensions, child support, and alimony. Information about sociodemographic characteristics came from Wave 1.
Risk factors for heart disease.
Some of the major well-known risk factors for heart disease measured at MIDUS Wave 1 were also included as covariates in this study, including smoking, diagnosis with diabetes or high blood sugar level, and body mass index (BMI). For smoking, MIDUS first asked if the respondent ever smoked cigarettes regularly (i.e. at least a few cigarettes every day). For those who have smoked regularly, a follow-up question asked if the respondent was still smoking cigarettes regularly at time of the interview. Based on these questions, this study created two dummy variables indicating whether the respondent was a former or current smoker. For the diagnosis of diabetes, this was measured with a question asking “In the past twelve months, have you experienced or been treated for diabetes or high blood sugar?” Lastly, BMI was calculated from respondents’ reported height and weight. To limit extreme values, any height greater than 84 inches was set to 84 inches (Brim et al., 2009).
Analysis
Discrete-time event history analysis was used to examine the likelihood of diagnosis with a heart problem occurring between MIDUS Waves 1 and 2. This approach was used because unit of time available in MIDUS for measuring the timing of the event (i.e., diagnosis with a heart problem) was age in years. This is less precise than having the measurements of time in age in months or days. When time intervals are more discrete than continuous, use of discrete-time approach is suggested (Singer & Willett, 2003). We divided the sample into married and unmarried groups based on their marital status reported at Wave 1 and ran the analysis separately for these two groups. There were 2,349 married individuals and 770 non-married individuals. The non-married group consisted of divorced (n = 319), separated (n = 36), widowed (n = 123), and never married (n =292) respondents.
Estimation of the hazard model used a person-year file, in which every respondent contributes a certain number of person-year observations that he or she was at the risk of being diagnosed with a heart problem. Each person-year record provides information about whether the person was diagnosed with a heart problem in that year and the value of covariates. For the married group, the person-year data contained 22,324 person-year observations from 2,349 individuals. For the unmarried group, 7,356 person-year observations came from 770 individuals.
After creating person-year files, we first performed a preliminary analysis with a combined sample of married and unmarried individuals. In this analysis, this study tested for the interaction effects between marital status and non-spousal family support to examine whether the associations between non-spousal family support and the risk of diagnosis with a heart problem differed by marital status. Spousal support and strain were not included as covariates in the preliminary analysis because a majority of the unmarried individuals (85.1%) were missing on these variables.
For the main analyses, three logistic regression models were run separately for each marital status group to test the effects of non-spousal family support on being diagnosed with a heart problem (Model 1) and its interactions with education and gender (Models 2 and 3). In these models, spousal support and strain were included as covariates for the married group. To interpret the interaction effects, two separate models were analysed for the interactions of support with gender and education respectively, and all continuous variables were centered at their mean. The analysis was done in two steps, in which the main effects of education, gender, and support were tested first and then the interaction terms were added in the subsequent models. If there were any significant interaction terms, the interaction effects were plotted to visualise the results.
Results
Sample Description
Descriptive statistics for the sample from the baseline individual-level data and tests of group differences between the married and unmarried group are presented in Table 1. Results showed that compared to the unmarried individuals, those who were married were younger (t(3117) = 3.81, p < .05), had higher levels of household income (t(3117) = −15.09, p < .05), and consisted of more men (χ2(1) = 59.95, p < .05). Married individuals also had higher levels of non-spousal family support (t(3117) = −5.62, p < .05) and lower levels of non-spousal family strain (t(3117) = 4.52, p < .05) compared to unmarried individuals. There were no significant differences in level of education and the prevalence of heart problems between the two groups.
Table 1.
Descriptive Characteristics from Baseline Sample and Tests of Group Differences between the Married and Unmarried Groups (2,349 Married and 770 Unmarriede)
| Married | Unmarried | Tests of Differences | |
|---|---|---|---|
| Variablea | Mean (SD) or % | Mean (SD) or % | χc or td |
| Age at Wave 1 | 45.90 (11.62) | 47.79 (13.00) | 3.81*** |
| Educationb | 2.79 (0.78) | 2.76 (0.80) | −0.63 |
| Logged Annual Income | 11.03 (1.55) | 9.94 (2.22) | −15.09*** |
| BMI | 26.59 (5.03) | 26.87 (5.72) | 1.30 |
| Non-spousal Family Support | 3.49 (0.56) | 3.35 (0.66) | −5.62*** |
| Non-spousal Family Strain | 2.07 (0.58) | 2.18 (0.61) | 4.52*** |
| Spousal Support | 3.63 (0.50) | - | |
| Spousal Strain | 2.18 (0.58) | - | |
| Diagnosis with Heart Problem | 9.11 % | 9.35 % | 0.04 |
| Male | 51.51 % | 35.45 % | 59.95*** |
| White | 95.62 % | 88.83 % | 46.88*** |
| Former Smoker | 30.91 % | 23.77 % | 14.32*** |
| Current Smoker | 15.54 % | 28.18 % | 61.08*** |
| Diabetes or High Blood Sugar | 3.58 % | 3.51 % | 0.01 |
Note. SD = standard deviation.
Except for diagnosis with heart problem, all variables were measured at MIDUS Wave 1. Diagnosis with heart problem was measured at MIDUS Wave 2.
1 = less than high school; 2 = GED or high school diploma; 3 = some college or Bachelor’s degree; 4 = higher than Bachelor’s degree.
Independent sample t-test of difference between the married and unmarried.
Chi-square test of difference between the married and unmarried.
N derived after list-wise deletion of observations with missing data across the study variables.
p < .001.
Non-spousal Family Support, Education, Gender, and Diagnosis with Heart Problem
Results from preliminary analysis on the interaction between non-spousal family support and marital status for the combined sample is presented in Supplementary Table 1. Results showed a significant interaction effect (OR = 1.57, p < .05), indicating that the association between non-spousal support and diagnosis of a heart problem differed by marital status. Further probing of the interaction effects showed that the association was significant only for the unmarried individuals and not for the married individuals. Specifically, a one unit increase in non-spousal family support (e.g., from 3 = Some to 4 = A lot) was associated with a 7% lower probability of being diagnosed with a heart problem (B = −0.07, p < .05) among the unmarried (Supplementary Figure 1).
For the main analyses, Table 2 presents the results from logistic regression models that separately tested the married and unmarried group for the main effects of non-spousal family support, education, and gender, and interactions among the three variables on the risk of being diagnosed with a heart problem. Model 1 tested for the main effects of non-spousal family support, education, and gender, Model 2 added an interaction term between education and non-spousal family support, and Model 3 added an interaction term between gender and non-spousal family support.
Table 2.
Logits and Odds Ratios for Diagnosis with Heart Problem, with Main and Interaction Effects of Gender, Education, and Non-spousal Family Support for Married and Unmarried Individuals
| Married Individuals (n = 22,324 person years) | Unmarried Individuals (n = 7,356 person years) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |||||||
| B (SE) | OR (SE) | B (SE) | OR (SE) | B (SE) | OR (SE) | B (SE) | OR (SE) | B (SE) | OR (SE) | B (SE) | OR (SE) | |
| Constant | −5.73*** (0.38) | 0.003*** (0.001) | −5.73*** (0.38) | 0.003*** (0.001) | −5.76*** (0.39) | 0.003*** (0.001) | −5.76*** (0.47) | 0.003*** (0.001) | −5.72*** (0.47) | 0.003*** (0.002) | −5.93*** (0.48) | 0.003*** (0.001) |
| Male | 0.61*** (0.16) | 1.84*** (0.29) | 0.61*** (0.16) | 1.84*** (0.29) | 0.64*** (0.16) | 1.90*** (0.31) | 0.51* (0.25) | 1.67* (0.42) | 0.56* (0.26) | 1.75* (0.45) | 0.77** (0.26) | 2.16** (0.56) |
| Education | −0.04 (0.09) | 0.96 (0.09) | −0.05 (0.09) | 0.95 (0.09) | −0.04 (0.09) | 0.96 (0.09) | −0.23 (0.15) | 0.80 (0.12) | −0.12 (0.15) | 0.89 (0.14) | −0.18 (0.15) | 0.84 (0.12) |
| Non-spousal Family Support | −0.003 (0.15) | 1.00 (0.14) | 0.02 (0.15) | 1.02 (0.15) | 0.20 (0.28) | 1.22 (0.34) | −0.38* (0.18) | 0.68* (0.12) | −0.25 (0.20) | 0.78 (0.15) | −0.79*** (0.21) | 0.45*** (0.10) |
| Non-spousal Family Support × Education | - | - | 0.16 (0.15) | 1.17 (0.17) | - | - | - | - | 0.36* (0.17) | 1.44* (0.25) | - | - |
| Non-spousal Family Support × Gender | - | - | - | - | −0.26 (0.30) | 0.77 (0.23) | - | - | - | - | 0.96** (0.34) | 2.61** (0.88) |
| −2 Log Likelihood | 2,246.00 | 2,244.91 | 2,245.24 | 752.33 | 747.93 | 743.90 | ||||||
Notes. All predictors and covariates were measured in MIDUS Wave 1; All continuous variables centered at their mean; Time was centered at age 50; The model controlled for time, age at Wave 1, race, logged household income, smoking status, diabetes, BMI, spousal support and strain (for married individuals), and non-spousal family strain.
B = Unstandardized beta coefficient; SE = Standard error; OR = Odds ratio.
p < .001
p < .01
p < .05.
Results from Table 2 show that for those who were married, the hazard of being diagnosed with a heart problem was higher for men (OR = 1.84, p < .05). Expressed in odds ratios, this indicates that the odds of diagnosis with a heart problem increased by 84% for men compared to women. There were no significant main effects of education and non-spousal family support. In Models 2 and 3, none of the interaction terms were significant.
For unmarried individuals, the main effects model (Model 1) suggested that the hazard of being diagnosed with a heart problem was higher for men (OR = 1.67, p < .05). Expressed in odds ratios, this indicates that the odds of diagnosis with a heart problem increased by 67% for men compared to women. There was no significant main effect of education. Results showed a significant main effect of non-spousal family support on the risk of being diagnosed with a heart problem, such that higher levels of family support were related to having a lower risk of being diagnosed with a heart problem. Specifically, for a unit increase in the level of non-spousal family support (e.g., from 3 = Some to 4 = A lot), the odds of diagnosis decreased by 32% (OR = 0.68, p < .05).
In Models 2 and 3 which tested for the interaction terms, both interactions between non-spousal family support and education (OR = 1.44, p < .05) and non-spousal family support and gender were significant (OR = 2.61, p < .05). To better interpret the interaction terms, we estimated marginal effects to examine how the effect of non-spousal family support differed by gender and level of education among unmarried individuals. For both Models 2 and 3, marginal effects were estimated at the age of 80 because the hazard rate estimated from the sample on the risk of being diagnosed with a heart problem showed that the risk peaked around that age (results not shown).
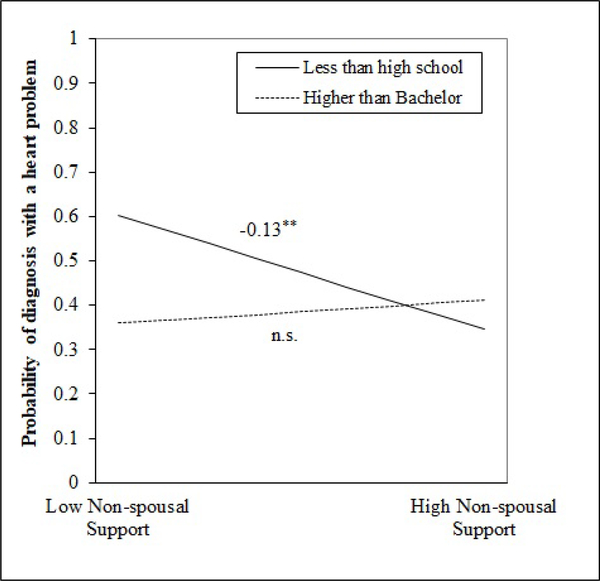
Estimation of marginal effects showed that the effect of non-spousal family support differed by the level of education. A higher level of non-spousal family support was significantly associated with a lower probability of being diagnosed with a heart problem for those with general equivalency degree (GED) or high school diploma (B = −0.08, p < .05) or with less than high school education (B = −0.13, p < .01). For example, for an unmarried 80-year-old person with less than a high school education, a one unit increase in non-spousal family support (e.g., from 3 = Some to 4 = A lot) was associated with a 13% lower probability of being diagnosed with a heart problem. Figure 1 is the graphical representation of the interaction effect (Dawson, 2014), using one standard deviation (SD) above and below average levels of non-spousal family support as anchor points. The interaction lines were drawn for those with less than a high school education and those with education beyond a Bachelor’s degree. The graph shows that for an unmarried 80-year-old with less than a high school education and one SD higher level of non-spousal family support, the probability of being diagnosed with a heart problem was 0.35. For a less-educated individual with one SD lower level of non-spousal family support, the probability was 0.60. This shows that among unmarried individuals with less than a high school education, those with a higher level of non-spousal family support had a lower probability of being diagnosed with a heart problem compared to those who had a lower level of non-spousal family support.
Figure 1.
Interaction between non-spousal family support and education level on the diagnosis of a heart problem among unmarried individuals at age 80. Solid line indicates those with less than high school education and dotted line indicates individuals with Bachelor’s degree or higher.
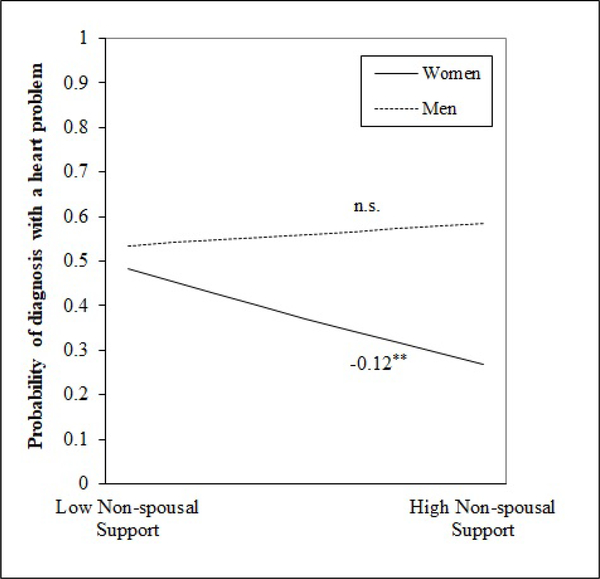
Estimation of marginal effects for gender showed that the effect of non-spousal family support was significant only for unmarried women (B = −0.12, p < .01) and not for men. Specifically, among unmarried women aged 80, a one unit increase in non-spousal family support (e.g., from 3 = Some to 4 = A lot) was associated with an 12% decrease in the risk of being diagnosed with a heart problem. Figure 2 is a graphic visualization of the interaction term, using one SD above and below average levels of non-spousal family support as anchor points. The graph shows that the probability of being diagnosed with a heart problem for an unmarried woman aged 80 with one SD higher level of non-spousal family support was 0.27, whereas the probability for an unmarried woman with one SD lower level of non-spousal family support was 0.48. For both level of education and gender, additional analyses were performed to test if the marginal effects of the interaction terms were consistent at younger ages. The results showed that the patterns of interaction effects for education and gender remained robust from ages 40 to 79 (results not shown).
Figure 2.
Interaction between non-spousal family support and gender on the diagnosis of a heart problem among unmarried individuals at age 80. Solid line indicates women and dotted line is for men.
As supplementary analyses for the interaction effects by education and gender, this study examined three-way interactions among non-spousal family support, marital status, and education and gender using the combined sample of married and unmarried groups. Spousal support and strain were not included as covariates in these analyses because the vast majority of the unmarried individuals had missing data on these variables. Results showed significant three-way interaction among marital status, non-spousal family support, and gender that echoed the results from the main analyses. Specifically, the associations between non-spousal family support and diagnosis of a heart problem differed by gender (i.e., association significant for women and not for men) only among the unmarried individuals and not for the married individuals (results not shown).
Discussion
This study examined the association between non-spousal family support and the risk of being suspected of or diagnosed with a heart problem among married and unmarried individuals. We also tested whether these associations differed by gender and the level of education. This analysis is one of the few prospective studies to specifically examine the role of non-spousal family relationships in heart health, using data from a national sample of US adults across 10 years.
The results showed that higher levels of non-spousal family support were associated with a lower risk of diagnosis with a heart problem among the unmarried individuals. As for the interaction effects, this study found significant interactions by gender and level of education only among the unmarried. Specifically, higher levels of non-spousal family support were associated with a lower risk of diagnosis of a heart problem only for unmarried women and unmarried individuals who were less educated. Because studies on social support identify friends as another significant source of support (Montpetit, Nelson, & Tiberio, 2017; Walen & Lachman, 2000), we conducted sensitivity analyses that included support and strain from friends as additional covariates. Inclusion of these variables did not change the results.
Our findings on the main effect of non-spousal family support showed that the salubrious role of non-spousal family support may vary by the marital status of the individual. The role of non-spousal family support in decreasing the risk of heart problems among unmarried adults is important to note, as it highlights the benefits of support from family members for those without a spouse. Also, the findings on interaction effects were consistent with previous studies on social support that found significantly stronger health benefits for women and less educated adults (Elliot, Heffner, Mooney, Moynihan, & Chapman, 2018; Schöllgen et al., 2011; Shumaker & Hill, 1991).
In this study, non-spousal family support was not associated with the risk of having heart problems among married adults. Being married often provides better economic resources, social control, and psychological support from spouses (Carr & Springer, 2010), which could mitigate the effects of non-spousal family support on health. For example, Table 1 shows that those who were married had higher incomes and were less likely to be current smokers compared to unmarried individuals. Although this study did not find significant associations between spousal support and heart problems (Supplementary Table 2), Donoho and colleagues (2015) found that higher marital relationship satisfaction was related to better heart rate variability. It is also possible that non-spousal support might matter for those in low-quality marriages, considering that both marital status and relationship quality are important for heart health (Holt-Lunstad, Birmingham, & Jones, 2008).
For unmarried individuals, on the other hand, receiving support from other family members was found to be particularly important for heart health. Specifically, a higher level of non-spousal family support was associated with a lower risk of being diagnosed with a heart problem among unmarried individuals. Such finding is in part consistent with a previous study by Pinquart (2003) which found that relationships with adult children and siblings were more strongly associated with well-being for unmarried adults compared to the married individuals. This is also in accordance with the hierarchical compensatory model of support (Cantor, 1979; 1991) which postulates that when the most primary source of support (e.g., spouse) is missing, its role is taken over by the next primary tie. For unmarried individuals without a spouse, close family members other than the spouse may function as a main source of support that bears significant health implications.
Further examination of the interaction effects showed that among the unmarried individuals, the association between non-spousal family support and heart problems was significant only for women and those with less education. For gender differences, social integration models posit that having a support network allows individuals to receive information about health-related behaviours or medical services (Cohen, Kaplan, & Manuck, 1994), and women may benefit more than men from family support in this regard. Women generally have more intimate relationships with family members than men, and more frequently receive advice and support from their kin (Marks & McLanahan, 1993). Thus, for women, family support may be more likely to function as a source of advice which provides encouragement to have a healthier lifestyle that may lower susceptibility to a heart problem (Umberson, Crosnoe, & Reczek, 2010). Also, women may benefit more than men from positive support from family members as they are more sensitive to interpersonal relationships (Lett et al., 2005).
As for differences by level of education, the stress-buffering model posits that social support reduces the risk of heart problems by protecting individuals from the detrimental influences of stressful events (Cohen et al., 1994), and that individuals who experience more stressors are more likely to benefit from the protective effects of support (Lett et al., 2005). Considering that those with less education are exposed to higher levels of negative life events and stressors (Grzywacz, Almeida, Neupert, & Ettner, 2004), support from family may give a greater boost to cardiovascular health outcomes of unmarried less educated adults compared to those who are highly educated. For example, when faced with a stressor, family members can either provide tangible resources to resolve a stressful situation or offer emotional comfort that allows less educated individuals to better cope with stressors (Thomas, Liu, & Umberson, 2017). In addition, by helping to perceive situations as less stressful, support from family may decrease the risk of heart problems by dampening the physiological response to stress that harms cardiovascular health or by helping individuals avoid engaging in unhealthy stress-coping behaviours such as heavy drinking or binge eating (Cohen et al., 1994). Therefore, having family members as a support network would be particularly crucial for the health of unmarried adults who are less educated, as those with fewer socioeconomic resources face a higher risk of cardiovascular disease due to their disadvantaged life circumstances (Hawkins, Jhund, McMurray, & Capewell, 2012). Furthermore, family may be the only source of support that unmarried less educated individuals can rely on in times of distress, compared to the more varied resources that highly educated persons have available (Ajrouch, Blandon, & Antonucci, 2005).
Some limitations to this study are useful to note. First, due to having data available from only two survey waves with a 9- to 10-year interval on average, this study only used time-invariant variables. For example, while the respondents’ level of non-spousal family support may change between the two waves, this study was not able to account for such change in the analysis. For a more accurate estimation of the model, incorporating time-varying changes of the study variables would be needed. Also, in measuring the diagnosis of a heart problem, MIDUS asked whether respondents had ever been “suspected or confirmed” with a heart problem by a doctor. This indicates that people who heard concerns about their heart condition may not have necessarily been confirmed as having a heart problem. If so, this group might be different from people whose diagnosis with a heart problem has been confirmed. Furthermore, in our analysis, a younger age at baseline was associated with a higher risk of a heart problem (Supplementary Tables 2 and 3), which differs from the typical increased risk of heart disease at older ages. This finding may be due to selection effects, in which healthy older adults who were not diagnosed with a heart problem before the baseline interview were selected into the sample (Masters, Powers, & Link, 2013). Also, the adjustment for time to an event (i.e. diagnosis with a heart problem) in our statistical models may have influenced the estimation of the coefficient for baseline age. When time to event was omitted from the models, the typical rising risk of heart disease with older age at baseline was observed.
In addition, the unmarried group in this study was composed of a heterogeneous set of divorced, separated, widowed, or never married persons. To examine whether the results would differ across the four unmarried groups, we conducted a set of supplementary analyses that tested models separately for each unmarried group. Results showed significant interaction effects in the same direction for gender among the divorced and the never married. This may be due to the small sample size of the separated (n = 36) and widowed (n = 123) individuals to detect significant effects. Because each of these marital status categories involves distinct experiences and processes (Carr & Springer, 2010), detailed examination of each type of unmarried status may better capture the nuanced health effects of non-spousal family support for unmarried individuals.
Also, measurement of non-spousal family support in this study was limited to perceived emotional support. Support is consisted of multiple dimensions, including both qualitative and quantitative properties (Gottlieb & Bergen, 2010). While emotional support reflects a qualitative attribute of support, support can also be measured using more objective, quantifiable measures such as frequency of contact, exchanges of instrumental support, or number of dependable ties. Studies that compare different aspects of support suggest that links to health outcomes differ across distinct types of support (Uchino, 2009). Therefore, exploring the implications of quantifiable aspects of non-spousal family support would be needed in order to have a more comprehensive understanding of the role of family support in heart problems.
Lastly, the study sample was racially homogeneous, primarily composed of white adults. Considering that race and ethnicity are critical determinants of cardiovascular disease and social support (Balfour, Ruiz, Talavera, Allison, & Rodriguez, 2016; Bell, Thorpe, & LaVeist, 2010; Graham, 2015), results may differ with a more racially and ethnically diverse sample. The role of non-spousal family support on the risk of a heart disease diagnosis may also differ by race or ethnicity, which requires further exploration with such a sample.
Despite the above limitations, this study contributes to previous studies on family support and health by distinguishing spousal and non-spousal family support and showing how the association between non-spousal family support and cardiovascular health may differ by marital status, gender, and level of education. While non-spousal family support did not have significant associations with the risk of having heart problems among married individuals, further examination is needed to identify their potential family-related correlates of heart health such as family composition and family roles. In addition, future research can use time-varying covariates and confirmed diagnoses of heart problems, and also explore the ways in which family relationships may influence the risk, treatment, and outcomes of heart disease.
Supplementary Material
Funding Information and Acknowledgments
The original Midlife in the United States (MIDUS) study was supported by the John D. and Catherine T. MacArthur Foundation Research Network on Successful Midlife Development. Support also came from the National Institute on Aging under Grant P01-AG020166 and U19-AG051426 to conduct a longitudinal follow-up of the original MIDUS study. Biomarker data collection was further supported by the National Institutes of Health National Center for Advancing Translational Sciences (NCATS) Clinical and Translational Science Award (CTSA) program under Grants UL1TR001409 for Georgetown, UL1TR001881 for UCLA, and 1UL1RR025011 for UW-Madison. The authors would also like to acknowledge assistance provided by the Population Research Institute at Pennsylvania State University, which is supported by an infrastructure grant by the Eunice Kennedy Shriver National Institute of Child Health and Human Development under Grant P2CHD041025. The authors thank Dr. Jennifer Van Hook for her helpful advice regarding the analysis of this study. The authors declare no conflicts of interest.
References
- Antonucci TC, & Akiyama H (1987). Social networks in adult life and a preliminary examination of the convoy model. Journal of Gerontology, 42(5), 519–527. doi: 10.1093/geronj/42.5.519 [DOI] [PubMed] [Google Scholar]
- Antonucci TC, Ajrouch KJ, & Birditt KS (2013). The convoy model: Explaining social relations from a multidisciplinary perspective. The Gerontologist, 54(1), 82–92. doi: 10.1093/geront/gnt118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antonucci TC, Birditt KS, & Akiyama H (2009). Convoys of social relations: An interdisciplinary approach. In Bengtson VL, Gans D, Putney NM, & Silverstein M (Eds.), Handbook of theories of aging (2nd ed., pp. 247–260). New York, NY: Springer Publishing Company. [Google Scholar]
- Ajrouch KJ, Blandon AY, & Antonucci TC (2005). Social networks among men and women: The effects of age and socioeconomic status. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 60(6), S311–S317. doi: 10.1093/geronb/60.6.s311 [DOI] [PubMed] [Google Scholar]
- Balfour PC Jr, Ruiz JM, Talavera GA, Allison MA, & Rodriguez CJ (2016). Cardiovascular disease in Hispanics/Latinos in the United States. Journal of Latina/o Psychology, 4(2), 98–113. doi: 10.1037/lat0000056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell CN, Thorpe RJ, & LaVeist TA (2010). Race/ethnicity and hypertension: The role of social support. American Journal of Hypertension, 23(5), 534–540. doi: 10.1038/ajh.2010.28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birditt KS, Newton N, & Hope S (2012). Implications of marital/partner relationship quality and perceived stress for blood pressure among older adults. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 69(2), 188–198. doi: 10.1093/geronb/gbs123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brim OG, Baltes PB, Bumpass LL, Cleary PD, Featherman DL, Hazzard WR, … Shweder RA (2009). Documentation of scales and constructed variables in MIDUS 1. Retrieved from: http://midus.colectica.org/Item/midus.wisc.edu/2bdf9141-eab4-4784-919e-efe9b408f9c8.
- Brim OG, Ryff CD, & Kessler RC (2004). How healthy are we? A national study of well-being at midlife. Chicago, IL: University of Chicago Press. [Google Scholar]
- Brummett BH, Barefoot JC, Vitaliano PP, & Siegler IC (2003). Associations among social support, income, and symptoms of depression in an educated sample: The UNC Alumni Heart Study. International Journal of Behavioral Medicine, 10(3), 239–250. doi: 10.1207/s15327558ijbm1003_04 [DOI] [PubMed] [Google Scholar]
- Cantor MH (1979). Neighbors and friends: An overlooked resource in the informal support system. Research on Aging, 1(4), 434–463. doi: 10.1177/016402757914002 [DOI] [Google Scholar]
- Cantor MH (1991). Family and community: Changing roles in an aging society. The Gerontologist, 31(3), 337–346. doi: 10.1093/geront/31.3.337 [DOI] [PubMed] [Google Scholar]
- Carr D, & Springer KW (2010). Advances in families and health research in the 21st century. Journal of Marriage and Family, 72(3), 743–761. doi: 10.1111/j.1741-3737.2010.00728.x [DOI] [Google Scholar]
- Cohen S, Kaplan JR, Manuck SB (1994). Social support and coronary heart disease: Underlying psychological and biological mechanisms. In Shumaker SA & Czajkowski SM (Eds.), Social support and cardiovascular disease (pp.195–221). New York, NY: Springer Science & Business Media. doi: 10.1007/978-1-4899-2572-5_9 [DOI] [Google Scholar]
- Dawson JF (2014). Moderation in management research: What, why, when, and how. Journal of Business and Psychology, 29(1), 1–19. doi: 10.1007/s10869-013-9308-7 [DOI] [Google Scholar]
- Donoho CJ, Seeman TE, Sloan RP, & Crimmins EM (2015). Marital status, marital quality, and heart rate variability in the MIDUS cohort. Journal of Family Psychology, 29(2), 290–295. doi: 10.1037/fam0000068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliot AJ, Heffner KL, Mooney CJ, Moynihan JA, & Chapman BP (2018). Social relationships and inflammatory markers in the MIDUS Cohort: The role of age and gender differences. Journal of Aging and Health, 30(6), 904–923. doi: 10.1177/0898264317698551 [DOI] [PubMed] [Google Scholar]
- Gottlieb BH, & Bergen AE (2010). Social support concepts and measures. Journal of Psychosomatic Research, 69(5), 511–520. doi: 10.1016/j.jpsychores.2009.10.001 [DOI] [PubMed] [Google Scholar]
- Graham G (2015). Disparities in cardiovascular disease risk in the United States. Current Cardiology Reviews, 11(3), 238–245. doi: 10.2174/1573403X11666141122220003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruenewald TL & Seeman SE (2010). Social support and physical health: Links and mechanisms. In Steptoe A (Ed.). Handbook of behavioral medicine: Methods and applications (pp.225–236). New York, NY: Springer. doi: 10.1007/978-0-387-09488-5 [DOI] [Google Scholar]
- Grzywacz JG, Almeida DM, Neupert SD, & Ettner SL (2004). Socioeconomic status and health: A micro-level analysis o exposure and vulnerability to daily stressors. Journal of Health and Social Behavior, 45(1), 1–16. doi: 10.1177/002214650404500101 [DOI] [PubMed] [Google Scholar]
- Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, … & Rosal M (2015). Social determinants of risk and outcomes for cardiovascular disease. Circulation, 132(9), 873–898. doi: 10.1161/cir.0000000000000228 [DOI] [PubMed] [Google Scholar]
- Hawkins NM, Jhund PS, McMurray JJ, & Capewell S (2012). Heart failure and socioeconomic status: Accumulating evidence of inequality. European Journal of Heart Failure, 14(2), 138–146. doi: 10.1093/eurjhf/hfr168 [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Birmingham W, & Jones BQ (2008). Is there something unique about marriage? The relative impact of marital status, relationship quality, and network social support on ambulatory blood pressure and mental health. Annals of Behavioral Medicine, 35(2), 239–244. doi: 10.1007/s12160-008-9018-y [DOI] [PubMed] [Google Scholar]
- House JS, Landis KR, & Umberson D (1988). Social relationships and health. Science, 241(4865), 540–545. doi: 10.1126/science.3399889 [DOI] [PubMed] [Google Scholar]
- Lett HS, Blumenthal JA, Babyak MA, Strauman TJ, Robins C, & Sherwood A (2005). Social support and coronary heart disease: Epidemiologic evidence and implications for treatment. Psychosomatic Medicine, 67(6), 869–878. doi: 10.1097/01.psy.0000188393.73571.0a [DOI] [PubMed] [Google Scholar]
- Marks NF, & McLanahan SS (1993). Gender, family structure, and social support among parents. Journal of Marriage and Family, 55(2), 481–493. doi: 10.2307/352817 [DOI] [Google Scholar]
- Masters RK, Powers DA, & Link BG (2013). Obesity and US mortality risk over the adult life course. American Journal of Epidemiology, 177(5), 431–442. doi: 10.1093/aje/kws325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, & Croft JB (2005). State of disparities in cardiovascular health in the United States. Circulation, 111(10), 1233–1241. doi: 10.1161/01.cir.0000158136.76824.04 [DOI] [PubMed] [Google Scholar]
- Montpetit MA, Nelson NA, & Tiberio SS (2017). Daily interactions and affect in older adulthood: Family, friends, and perceived support. Journal of Happiness Studies, 18(2), 373–388. doi: 10.1007/s10902-016-9730-4 [DOI] [Google Scholar]
- Murphy SL, Xu JQ, Kochanek KD, Curtin SC, & Arias E (2017). Death: Final data for 2015. National Vital Statistics Reports, 66(6), Hyattsville, MD: National Center for Health Statistics. Retrieved from: https://www.cdc.gov/nchs/data/nvsr/nvsr66/nvsr66_06.pdf [PubMed] [Google Scholar]
- Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, & Rodeheffer RJ (2004). Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. Journal of Clinical Epidemiology, 57(10), 1096–1103. doi: 10.1016/j.jclinepi.2004.04.005 [DOI] [PubMed] [Google Scholar]
- Perrewé P, & Carlson D (2002). Do men and women benefit from social support equally? Results from a field examination within the work and family context. In Nelson DL & Burke RJ (Eds.), Gender, work stress, and health: Current research issues (pp. 101–114). American Psychological Association. doi: 10.1037/10467-007 [DOI] [Google Scholar]
- Pietromonaco PR, & Collins NL (2017). Interpersonal mechanisms linking close relationships to health. American Psychologist, 72(6), 531–542. doi: 10.1037/amp0000129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M (2003). Loneliness in married, widowed, divorced, and never-married older adults. Journal of Social and Personal Relationships, 20(1), 31–53. doi: 10.1177/02654075030201002 [DOI] [Google Scholar]
- Reinhardt JP, Boerner K, & Horowitz A (2006). Good to have but not to use: Differential impact of perceived and received support on well-being. Journal of Social and Personal Relationships, 23(1), 117–129. doi: 10.1177/0265407506060182 [DOI] [Google Scholar]
- Rook KS (1990). Parallels in the study of social support and social strain. Journal of Social and Clinical Psychology, 9(1), 118–132. doi: 10.1521/jscp.1990.9.1.118 [DOI] [Google Scholar]
- Ross CE, & Mirowsky J (2010). Why education is the key to socioeconomic differentials in health. In Bird CE, Conrad P, Fremont AM, & Timmermans S (Eds.), Handbook of medical sociology (5th ed., pp. 33–51). Nashville, TN: Vanderbilt University Press. [Google Scholar]
- Schöllgen I, Huxhold O, Schüz B, & Tesch-Römer C (2011). Resources for health: Differential effects of optimistic self-beliefs and social support according to socioeconomic status. Health Psychology, 30(3), 326–335. doi: 10.1037/a0022514 [DOI] [PubMed] [Google Scholar]
- Schuster TL, Kessler RC, & Aseltine RH (1990). Supportive interactions, negative interactions, and depressed mood. American Journal of Community Psychology, 18(3), 423–438. doi: 10.1007/bf00938116 [DOI] [PubMed] [Google Scholar]
- Shumaker SA, & Hill DR (1991). Gender differences in social support and physical health. Health Psychology, 10(2), 102–111. doi: 10.1037//0278-6133.10.2.102 [DOI] [PubMed] [Google Scholar]
- Silverstein M, Gans D, Lowenstein A, Giarrusso R, & Bengtson VL (2010). Older parent–child relationships in six developed nations: Comparisons at the intersection of affection and conflict. Journal of Marriage and Family, 72(4), 1006–1021. doi: 10.1111/j.1741-3737.2010.00745.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer JD & Willet JB (2003). Applied longitudinal data analysis: Modeling change and event occurrence. Oxford University Press: New York. [Google Scholar]
- Steptoe A (2011). Stress, inflammation, and coronary heart disease. In Hjemdahl P, Steptoe E, Rosengren A (Eds.), Stress and cardiovascular disease (pp.111–128). Springer: London. doi: 10.1007/978-1-84882-419-5_7 [DOI] [Google Scholar]
- Thomas PA, Liu H, & Umberson D (2017). Family relationships and well-being. Innovation in Aging, 1(3), doi: 10.1093/geroni/igx025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson L, & Walker AJ (1989). Gender in families: Women and men in marriage, work, and parenthood. Journal of Marriage and the Family, 51(4), 845–871. doi: 10.2307/353201 [DOI] [Google Scholar]
- Uchino BN (2009). What a lifespan approach might tell us about why distinct measures of social support have differential links to physical health. Journal of Social and Personal Relationships, 26(1), 53–62. doi: 10.1177/0265407509105521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino BN, Smith TW, & Berg CA (2014). Spousal relationship quality and cardiovascular risk: Dyadic perceptions of relationship ambivalence are associated with coronary-artery calcification. Psychological Science, 25(4), 1037–1042. doi: 10.1177/0956797613520015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino BN, & Way BM (2017). Integrative pathways linking close family ties to health: A neurochemical perspective. American Psychologist, 72(6), 590–600. doi: 10.1037/amp0000049 [DOI] [PubMed] [Google Scholar]
- Umberson D, Crosnoe R, & Reczek C (2010). Social relationships and health behavior across the life course. Annual Review of Sociology, 36(1), 139–157. doi: 10.1146/annurev-soc-070308-120011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walen HR, & Lachman ME (2000). Social support and strain from partner, family, and friends: Costs and benefits for men and women in adulthood. Journal of Social and Personal Relationships, 17(1), 5–30. doi: 10.1177/0265407500171001 [DOI] [Google Scholar]
- West C, & Zimmerman D (1987). Doing gender. Gender and Society, 1(2), 125–151. doi: 10.1177/0891243287001002002 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.