Abstract
Total knee replacement (TKR) is a growing attractive treatment for a degenerative knee disease. However, there remain some certain devastating complications to be discussed with patients preoperatively, including limb amputation. This systematic review aimed to determine the rate of amputation following TKR. In this study, the literature was searched up to 2019. The papers were included in which knee amputation was reported following TKR. The primary search concluded the articles from EMBASE, SCOPUS, PubMed, Web of Science, MEDLINE, OvidSP, CINAHL, EBSCO, Web of Science™, and CENTRAL. After screening and excluding case reports, 40 papers were included in the present study. The present review showed that amputation is a real end result of knee replacements either in primary or revision knee arthroplasties, which needs to be discussed with patients for their decision-making. Prevalence of amputation in terms of failure or complications after TKR procedures was estimated between 0.1-10% in different studies , with 5.1% amputation rate in infected TKR and 0.025% amputation rate in primary TKR as a result of infection in our review. Deep infection was the main cause of amputation. Vascular complications and fractures associated with bone loss and compartment syndrome were other reasons for amputation.
Key Words: Amputation, Arthroplasty, Compartment syndrome, Infection, Total knee replacement
Introduction
Osteoarthritis (OA) is the common final result of different kinds of severe knee injuries that can be progressive and carry high rate of morbidity. Since the first report in 1968, knee replacement surgery has gradually become the most efficient predictable and popular procedure addressing end-stage arthritis (1). Today, total knee replacement (TKR) is identified as a highly successful surgery for the treatment of advanced destruction in patients with joint problems, especially primary or secondary osteoarthrosis (2). This procedure can help remarkable pain relief, modification of deformities, as well as enhancement of limb function and quality of life (3, 4).
A 90% improvement is reported in the condition of patients who received knee prostheses in long-term clinical evaluations (5-8). Persistent implants with the maintenance of joint proper function are observed in more than 90% after the initial arthroplasty (8, 9). Number of TKR procedures is increasing due to its satisfactory outcome leading to increased life expectancy and quality of life. Due to recent advantages in these procedures, the number of TKRs increased 5% related to previous years in order to grow more rapidly in the next years (10).
However, arthroplasty may lead to durability and adequate functioning after several years. Revision surgery becomes necessary in patients with failed arthroplasty (11, 12). There are certain minor or major complications regarding this surgery that any knee surgeon discusses with the patient before the operation. Yet, there is a lack of data about the risk of amputation as one of the most devastating end results of knee replacement surgery (13-15). It is possible that the vascular lesions that occur during the operation or infection by severe resistant microorganisms could impose the greatest risk on knee amputation in patients who underwent arthroplasty (16, 17). The present study aimed to determine the rate of amputation as an end result after TKR if it needs to be discussed with the patient.
Materials and Methods
This systematic review was conducted on the papers focused on the presence of amputation after TKR published up to October 2019. Cochrane Handbook guideline stages were used for designing the structure of this study. These seven stages include asking a question, determining the inclusion and exclusion criteria, searching articles, deleting inappropriate studies based on eligibility, evaluating the quality assessment, obtaining the required data, and discussing the topic (18).
Inclusion and exclusion criteria
The Participants-Intervention-Comparison-Outcome-Study design was employed for the determination of eligibility criteria. Publication in English language, selection of human samples, and clear description of the amputation after TKR were considered the inclusion criteria. The articles with insufficient data, review articles, meta-analyses, expert opinions, editorial letters, case reports, case series, consensus statements, and qualitative studies were removed from this study. Due to the observational nature of the study, which was the assessment of the prevalence of amputation in infected TKR, all case-control observational studies, as well as prospective and retrospective articles, were entered in this study. Case series performed on lower than 10 cases were excluded from the present study. All studies were also conducted on human samples. The main inclusion criteria were any outcome study that reported knee disarticulation or above-the-knee amputation as an endpoint in a previous knee replacement.
Literature Search, Study Selection, and Data Extraction
The present study was a systematic review of the relevant peer-reviewed original papers, including case series, case-control studies, and retrospective studies in large national registries. For the purpose of the present study, the data were gathered by two researchers through searching the three electronic databases, including EMBASE, SCOPUS, PubMed Publisher, MEDLINE, Ovid SP, CINAHL, EBSCO, Web of Science™, and CENTRAL, up to October 2019. The papers were selected with a focus on the presence of amputation in patients with infected TKR. The search terms were “Knee Arthroplasty” or “Knee Replacement” in combination with “Amputation”.
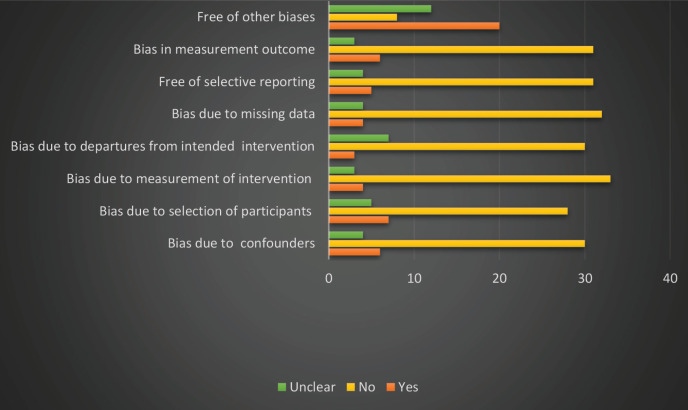
Risk of bias in individual trials
Cochrane risk of bias guideline was used to assess the risk of bias in the present study (19). The bias due to the selection of participants, bias due to the measurement of intervention, bias due to missing data, free of selective reporting bias, and other sources of bias were the eight main domains, which were assessed in this study. For the calculation of the risk of bias, these eight domains were categorized into low, high, and unknown risks of bias marked as “Yes”, “No”, and “Unclear”, respectively.
Study design
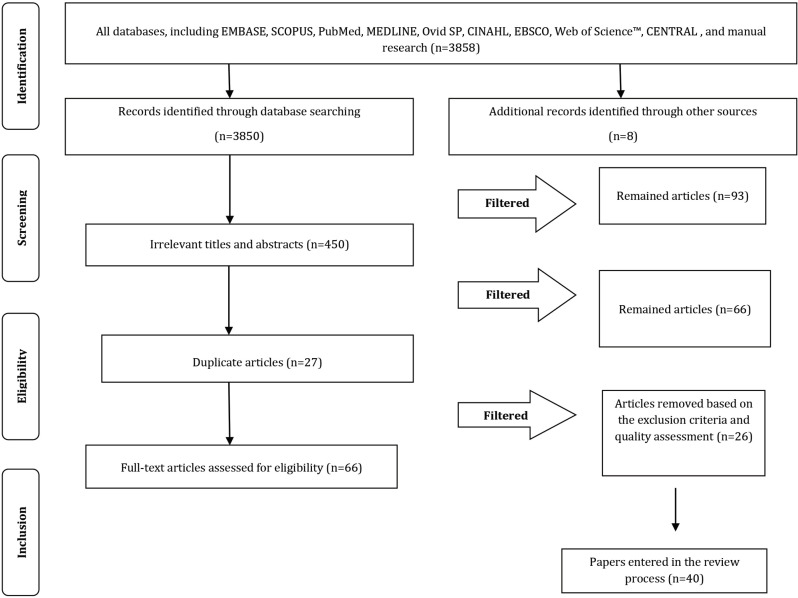
In the first step, the articles reviewing the titles and abstracts were assessed by considering the eligibility criteria. All the articles incompatible with the objectives of this study were excluded from the review. Selection process of the articles is presented in PRISMA flow diagram [Figure 1]. Two investigators (SG, ARM) screened the studies independently for eligibility. They reviewed the titles and abstracts of all the articles separately and were in contact with each other for data extraction. Finally, the remaining full texts were evaluated, and the inclusion/exclusion criteria were determined for the study. References of the included studies, as well as previous reviews, were checked for additional studies. Emails were sent to the corresponding authors of the included studies to seek and confirm any other published or unpublished data. Finally, the required results were recorded in predesigned forms.
Figure 1.
PRISMA flowchart representing the study selection process
Results
A total of 3850 papers were explored in the first search of the databases out of which 450 were potentially eligible based on the titles and abstracts. The articles investigating other complications of knee arthroplasty, except for amputation were removed from the present review. A total of 93 articles were obtained reporting the rate of amputation in patients who underwent TKR out of which 27 papers were removed due to duplicates, and 66 papers remained. The studies with inaccessible full-text versions (n=1) and those published in other languages (n=0) were removed from the study. Moreover, experimental or in vitro articles (n=2), editorial letters (n=1), case reports (n=5), case series with sample sizes lower than 10 (n=5), qualitative and narrative articles (n=9), as well as systematic reviews (n=3), were excluded from this study. Finally, 40 related papers were selected and entered in this review [Figure 1].
The present systematic review was conducted on all papers investigating the rate of amputation due to infection in patients who underwent TKR. Due to the objective of this study, all case-control articles, prospective and retrospective observational studies, and case series with sample sizes higher than 10 were entered in this study. Majority of the articles were retrospective observational reviews. The selected papers in this study were performed in four different regions. In this regard, 18 studies were performed in different regions of Europe (United Kingdom=4, Germany=5, France=2, Switzerland=1, Netherlands=1, Finland=1, Sweden=2, Norway=1, and Ireland=1), and 18 articles were carried out in North America (USA=14 and Canada=3). In addition, two studies were conducted in South America (Brazil), and two papers were performed in the Far East (Hong Kong=1 and Korea=1). No articles were observed in Africa and other regions of Asia, except for the Far East.
The above-mentioned studies were carried out on a total of 428,314 patients who underwent TKR with postoperative infection. The age range was reported within 8-94 years. In the majority of studies, the frequency of males was higher than that of females. Most subjects suffered from OA (i.e., primary or secondary). Rheumatoid arthritis, inflammatory arthritis, juvenile idiopathic arthritis, posttraumatic OA, and other arthrosis were other common diseases leading to TKR. Diabetes mellitus was another most common disease resulting in TKR. Tuberculosis, psoriatic arthritis, morbid obesity, splenectomy, giant cell tumor, compound fracture, periprosthetic fracture TKR, liver cirrhosis, apoplexy, arterial hypertonus, hypertension, ischaemic or coronary artery disease, posttraumatic congenital dislocation, chronic obstructive pulmonary disease, history of stroke or transient ischemic attack, osteonecrosis, congenital dislocation of the knee, and haemophilic arthropathy were other diseases leading to TKR. Some studies reported being unable to identify the reasons for primary diagnosis.
Moreover, the rates of the compartment, fracture and bone loss, and vascular complications were evaluated among patients who underwent TKR. No fracture and bone loss were reported in the majority of the included articles. Two studies were performed on the subjects who had infection involving the knee and associated with mild to severe bone loss or osteomyelitis (20, 21). Bone loss was not reported in other studies. One case with bone loss was reported only in one study, which was performed on 32 patients with postoperative infection (22). There were different reports on the rate of fracture in the selected studies within the range of 1-6% due to the number of patients with infected TKR in each study (23-29). Vascular complications were reported in some studies within the range of 0.1-3.4% due to the number of subjects with infected TKR (11, 16, 25, 27, 29-32). In addition, the compartment was observed only in one study (32).
Rate of amputation was reported within 0.1-10% in different studies (24, 33). Persisting infection and uncontrollable infection were the main factors of amputation. In addition, multi resistant staphylococcus aureus infection, massive tissue destruction at the time of admission, end-stage arterial occlusion, vascular reasons, developed sepsis uncontrollable infection, periprosthetic fracture, pain, severe bone loss, and vascular complication were the main reasons for amputation (11, 27, 31, 33-36). The data extracted from each included study were associated with the time and place of the study, research objective, sample size, age of the study population, male to female ratio, and other parameters [Table 1].
Table 1.
Extracted data from each included study
|
Authors
(year) References |
Country | Type of study | Age | Female/male ratio | Primary TKR 1 |
Infected TK
R (sample size) prosthetic joint infection |
Combination diseases | Compartment | Fracture and bone loss |
Vascular
complications |
Amputation |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hsieh et al. (2013) (36) |
Hong Kong | Retrospective cohort analysis |
RA2: 51 (35-75) NonRA3: 63 (32-85) |
RA: 34 (74) NonRA: 82 (27) |
-- | 346 | RA: 46 (13.3%) | -- | -- | -- | One patient with amputation to control sepsis |
| Gardner et al. (2010) (37) |
USA | Retrospective cohort study | 70 (48-94) | 9/35 (79.5%) |
12549 | 44 (44 knees) with culture-positive periprosthetic infection |
-- | -- | -- | -- | One above-the-knee amputation |
| Laffer (2006) (38) |
Switzerland | Retrospective cohort study | 70 (44-90) median |
18/17 (51.4-48.6%) | 534 primary knee arthroplasties | 35 patients undergoing surgery for TKR associated infection 13 subjects (2.4%) among whom developed TKR-associated infection |
Diabetes mellitus, RA |
-- | -- | -- | Death of one patient due to sepsis despite upper-leg amputation |
| Van Rensch et al. (2012) (33) |
Netherlands | Retrospective observational study |
66 | 50/50% | 22 | 20: (12 Primary TKR 7: Revision TKR 1: Following unicompartmental knee arthroplasty |
Tuberculosis, advanced primary arthrosis, and RA | -- | -- | -- | Upper-leg amputation in two patients due to persisting infection |
| S Joshy et al. (2007) (39) |
United Kingdom | Retrospective | 70 (46-92) | 16/15 | 31 | 31 | Osteoarthritis, psoriatic arthritis, RA, diabetes, morbid obesity, and splenectomy | -- | -- | -- | Death of one case due to myocardial infarction One case with septicemia Death of eight cases with arthrodesis |
| Helito et al. (2015) (35) |
Brazil | Retrospective | 66.3 (42-84) | 50/50% | 1596 | 63 (3.9%) | Primary osteoarthrosis RA, Juvenile RA |
-- | -- | -- | In 10 cases, control of the infection was not achieved. Five cases (50%) underwent amputation. One of the patients who refused amputation developed sepsis and underwent an emergency surgical amputation procedure but died. |
| Macmull et al. (2010) All patients (20) |
United Kingdom | Retrospective review | 56 (18-74) | 8/11 | 19 | 19 | Osteoarthritis compound fracture giant cell tumor, RA, periprosthetic fracture TKR |
-- | All patients with deep infection involving the knee and associated with extensive bone loss or osteomyelitis | -- | Of the three patients in whom the SMILES spacer did not eliminate infection. Two cases proceeded to an above-the-knee amputation |
| Pelt et al. (2014) (23) |
USA | Retrospective review | 63 (35-85) | 34/24 (59/41%) |
58 | 58 | Osteoarthritis, RA, posttraumatic arthritis and unable to identify the reason for primary diagnosis |
-- | Two cement mold fractures and 2 intraoperative tibia fractures | -- | One case with above-the-knee amputation. Three unknown mortalities and one death on postoperative day Three mortalities due to a myocardial infarction associated with ventricular tachycardia |
| Rohner et al. (2015) (40) |
Germany | Retrospective observational | 68 | -- | 26 | 26 | Osteoarthritis | -- | -- | -- | An above-the-knee amputation in three of the patients |
| Sierra RJ et al. (2003) (11) |
USA | Retrospective observational | 8.6 (8-23.6) | -- | 18443 | 18443 | -- | -- | -- | 24 knees with amputation related to peripheral vascular disease | Amputation in 67 (0.36%) cases out of which 22 cases related to TKR, 19 cases for uncontrollable infection, two cases for periprosthetic fracture, two cases for pain, one case for severe bone loss, and one case for vascular complication |
| Briffa et al. (2012) (24) |
UK | Retrospective observational | 71.3 | 20/18 | 38 | 38 | RA | -- | One fracture of the modular implant | -- | Three patients with an above-the-knee amputation for extensor mechanism failure and failure of suppression treatment Arthrodesis required in 10% and amputation in 6% of the cases |
| Herold et al. (2011) (31) |
Germany | Retrospective chart review | 66±14 | 5/7 | 25 | 12 | Diabetes, liver cirrhosis, and apoplexy, and arterial hypertonus | -- | -- | Eight cases out of twelve patients (67%) with pathological vascular status | Amputation performed on one patient due to a multiresistant staphylococcus aureus infection and massive tissue destruction at the time of admission |
| Klinger et al. (2005) (21) |
Germany | Retrospective observational | 67 (47-81) | 8/12 | 20 | 20 | Osteoarthritis, RA, and posttraumatic | -- | Mild bone loss in 3 patients, moderate in 12 patients, and severe in 5 patients | -- | An above-the-knee amputation due to infection with methicillin-resistant staphylococcus aureus |
| Stammers et al. (2014) (25) |
United Kingdom | Retrospective observational | 72 (23-89) | 24/27 | 430 | 51 | Hypertension, ischemic heart disease, RA, obesity | -- | One case with a periprosthetic fracture around the cement spacer with nonhealing wounds due to lymphedema | One case | Seven cases |
| Parvizi et al. (2008) (32) |
USA | Retrospective observational | 66 (44-86) | 13/3 | 13517 | 16 | Hypertension, diabetes mellitus, and coronary artery disease | Four compartment fasciotomies performed on 8 of the 16 patients | -- | All cases (n=16) | Above-the-knee amputation performed on one patient with popliteal artery thrombosis with failed bypass |
| Mahmud et al. (2012) (30) |
Canada | Retrospective review | 70±10 | 135/104 | 239 | 239 | -- | -- | -- | One patient with peripheral vascular disease |
One patient with peripheral vascular disease and a chronically discharging sinus over the knee with an above knee amputation |
| Larson et al. (2008) (29) |
USA | Retrospective matched case-control | Case: 58 (28-75) Control: 58 (29-75) |
-- | 26077 | 19 | -- | -- | Open fracture in three patients | One peripheral vascular disease |
Two cases |
| Jenny et al. (2012) (34) |
France | Retrospective review | 72 (45-93) | 27/20 | 47 | 47 | -- | -- | -- | -- | Amputation in one patient for endstage arterial occlusion |
| Kim et al. (2015) (41) |
Korea | Retrospective review | 66.3 (40-90) | 147/44 | 191 | 191 | Osteoarthritis | -- | -- | -- | Two patients who underwent above-the-knee amputation |
| Choi et al. (2012) (42) |
USA | Retrospective review | 64 (38-85) | 24/23 | 65 | 65 | Osteoarthritis, posttraumatic arthritis, RA, congenital dislocation | -- | -- | -- | Two cases Four deaths |
| Holmberg et al. (2015) (28) |
Sweden | Retrospective review | 70 (45-91) | 62/83 | 145 | 145 | Osteoarthritis and inflammatory arthritis |
-- | Four cases with osteoarthritis secondary to the fracture | -- | Two above-the-knee amputation Four deaths |
| Jämsen et al. (2010) (26) |
Finland | 70 (35-97) | 70/30% | 2647 | 24 | Primary or secondary osteoarthritis, RA, and other arthritis |
-- | 1.2% osteosynthesis for fracture | -- | No lower limb amputations or deaths due to infection | |
| Kuchinad et al. (2014) (43) |
Canada | Retrospective cohort analysis |
66.9 | 11/10 | 21 | 21 | -- | -- | -- | -- | Two cases |
| Jämsen et al. (2006) (22) |
Finland | Retrospective cohort analysis |
68 (39-85) | 21/11 | 34 | 32 | Osteoarthritis and inflammatory arthritis | -- | bone loss in one case | -- | One case |
| Abularrage et al. (2008) (16) |
USA | Prospectively collected | 64.9 | 4/96% 1605/ 40028 |
24029 | 24029 | Diabetes mellitus, chronic obstructive pulmonary disease, history of stroke or transient ischemic attack |
-- | -- | 2% cerebrovascular accident | Two patients undergoing lower extremity amputation |
| Heyse et al. (2014) (27) |
Germany | Retrospective review | 28.9 (11-58) | -- | 219 | 31: Four revisions for infection (1.2% of all cases) | Juvenile idiopathic arthritis | -- | Two periprosthetic fractures | Two vascular reasons | Two bilateral amputation for vascular reasons |
| Choi MD et al. (2011) (44) |
USA | Retrospective review | 66.6 (38-87) | 31/29 | 75 (79 knees) | 75 | Osteoarthritis, RA, posttraumatic osteoarthritis, osteonecrosis, and congenital dislocation of the knee | -- | -- | -- | Five cases with amputation |
| Westberg et al. (2014) (45) |
Norway | Retrospective review | 41 (20-82) | 4/70 | 74 (107 knees) | 74 | Hemophilic arthropathy | -- | Four patients with an osteosynthesis due to a periprosthetic fracture without removing TKR | -- | One patient with an above-knee amputation |
| Son et al. (2017) (46) |
USA | Retrospective review | 74±7 | 48/52% | 44466 | 44466 | -- | -- | -- | -- | 1864 amputations (4.1%) |
| George J et al. (2016) (47) |
USA | Retrospective review | 50-80 | -- | 341954 | 341954 | -- | -- | -- | -- | 9733 amputations (2.8%) |
| Amouyel et al. (2015) (48) |
France | Retrospective review | 68 | 27/39 | 109 | 72 | -- | -- | -- | -- | Six cases (8%) undergoing amputation |
| Bengston and Knutson (1991) (49) |
Sweden | Retrospective review | 69 (17-91) | 87/34% | 12118 | 357 | -- | -- | -- | -- | 23 cases |
| Isiklar et al. (1994) (50) |
USA | Retrospective review | 72 | 50/50% | 5045 | -- | -- | -- | -- | -- | 9 cases |
| de Paula Mozellaa et al. (2012) (2) |
Brazil | Retrospective | 67.1 53-80 |
50/50% | 2409 | 8 | Primary gonarthrosis, RA, posttraumatic arthrosis | -- | One case | One case | 10 0.41% Recurrent deep infection as the cause of amputation in 81% of cases |
| Pala et al. (2010) (51) |
United Kingdom | Retrospective review | 69.4 (54-79 ) | 55/45% | 3913 | 9 | Osteoarthritis | Two cases | One case | One case | Two cases |
| Houdek et al. (2019) (52) |
USA | Retrospective review | 65 | 58/42% | 5783 | -- | -- | -- | Previous periarticular fracture in 16 patients | -- | Transfemoral amputation performed on 14 patients |
| Friedrich et al. (2017) (53) |
Germany | Retrospective review | 70.2 (43-89) | -- | 37 | 32 | -- | -- | -- | -- | One of patients treated with knee amputation and died due to reasons unrelated to the surgery 12 months after index surgery |
| Goldman et al. (2019) (54) |
USA | Retrospective review | 65 | -- | 23 (25 knees) | 23 | -- | -- | -- | -- | one patient |
| McQuail et al. (2018) (55) |
Ireland | Retrospective case series | 65.8 (36-86) | 7/16 | 23 | 19 | Osteoarthritis | -- | One case | -- | Three above-the-knee amputations |
| Perry et al. (2018) (56) |
USA | Retrospective case series review | 64 | 7/9 | 16 | 16 | RA | -- | -- | -- | One case |
Table 1 listed all the original papers that reported amputation as a consequence or end result of knee replacement in nontumoral knee replacements. Moreover, the categorization of the original papers was conducted according to the reason for amputation. There have been few original studies that reported amputation in the infected group and total primary replacements at the same time. Table 2 tabulates the summary of the obtained results in the present study. Quality assessment of the entered articles is depicted in Figure 2.
Table 2.
Studies reported amputation rate in infected and total knee replacements
|
Year of
publication |
Primary total knee
replacement |
Infected total knee
replacement |
Amputation |
|---|---|---|---|
| Jeremy et al. (2012) (37) |
12549 | 44 | 1 |
| Laffer1 et al. (2006) (38) |
534 | 13 | 1 |
| Helito et al. (2015) (35) |
1596 | 63 | 5 |
| Jämsen et al. (2010) (57) |
3137 | 24 | 0 |
| Abularrage et al. (2008)4 (16) |
24029 | 20 | 2 |
| Westberg et al. (2014) (45) |
107 | 6 | 1 |
Figure 2.
Quality assessment of the articles included in the review process
Discussion
Prevalence of amputation as an irreparable complication of infected total knee replacement
Due to the irreparable complications of TKR, the discussion on this issue is very important. However, there is not enough data on the incidence of amputation due to the failure of knee arthroplasty (2). The TKR, in particular is a growing procedure in orthopedic settings. New versions of products, advancement in technique, and especially less time of recovery, compared to other reconstructive procedures make the replacement as an attractive procedure. However, after more than 40 years, there remain some hidden facts regarding the durability and prognosis of TKR. According to the literature, there have been few reports of amputation after replacement. No single study or expert opinion reported amputation as a real consequence or end result of this procedure. The present review showed that this risk is not negligible and may need to be discussed with the patient as other important complications.
Regarding all new advancements, the infection has remained the worst complication after the surgery with psycho-social and economic costs for the patients. Majority (>90%) of these infections are killed by accurate staged reconstruction. If the infection cannot be removed or multiple revision leads to severe unreconstructable bone or soft tissue loss, knee arthrodesis, spacer arthroplasty, and amputation will be three main viable salvage interventions with knee amputation as the final option for the failure of these salvage procedures (58-69). Based on the present review, the rate of amputation was estimated between 0.1-10% in different studies (24, 33).
Deep infection after TKR was assessed in a study by Bengston and Knutson. In the aforementioned study, an evaluation was performed on transfemoral amputation reported in 23 cases patients (out of 357 cases) with infected TKR. Rates of amputation were calculated at 0.18% and 6% in all cases and patients with infected arthroplasty, respectively (49). The aforementioned study was conducted in 1991; therefore, the high rate of amputation may be due to the failure to develop surgical procedures. Rate of amputation was reported as 0.18% in another study by Isiklar et al. (50). In addition, the rate of amputation was estimated at 0.14% in another study by Sierra et al. (11). In a study performed by Van Rensch et al., the prevalence of amputation in infected arthroplasties was reported as 0.41% (33). Identification of amputation as a complication of TKR or due to unrelated causes is a fundamental problem. Some included studies were multicenter, and the data did not contain the cause of amputation. Exact cause of amputation is unclear in several studies due to uncompleted medical records. It is recommended to perform future studies focused on the main causes of amputation.
Main cause and complication leading to amputation after total knee replacement
Generally, infection is identified as the main cause of amputation, which was observed in the majority of the patients who underwent TKR. In a study carried out by Paula Mozella et al., infection was identified as the main cause of amputation in 81% of cases (2). In the aforementioned study, the rates of primary knee replacement and arterial injury were reported about 0.49% and 0.08%, respectively (16). According to the evidence, the rate of infection is about 0.5% to 1.9% in primary TKRs and increases to 8-10% in revision TKRs (70-72). T. Amouyel et al. in a retrospective cohort study conducted on 72 chronic infected knee prostheses removal and considered fusion and spacer as salvage procedures. According to this study on chronic knee infections, the removal of implant leads to 38-46% failure rate either with fusion or spacer. At the end of 5 years of follow-up, they were reported with an amputation rate of 8% (48). Min-Sun Son et al. in a national registry database study followed the results of revision surgeries on 44,466 failed total knee arthroplasties retrospectively. Rate of above-the-knee amputations was reported as 4.1% according to the obtained results of the aforementioned study (46).our review showed 5.1% amputation rate in infected TKR and 0.025% amputation rate in primary TKR as a result of infection [Table 2].
Based on the obtained results of the entered studies, staphylococcus aureus has been the germ most frequently isolated in postoperative TKR infections (2, 50, 73). The germ was isolated in 54% of the cultures from patients amputated due to infection (2). Staphylococcus epidermidis is reported as another common germ isolated in infected TKR (50). Vascular complications in patients who underwent TKR are catastrophic; however, they are very rare. Accordingly, the prevalence of vascular complications is estimated within the range of 0.03-0.17% as reported in the literature (74). Based on a previous study, only 0.02% of infrapatellar amputations were related to vascular insufficiency (2). Commonly, vascular complications after TKR are observed in patients with previously undiagnosed atherosclerotic disease. Amputation due to the ischemia of the limb after arthroplasty was reported in two cases in a study by Paula Mozella et al. (2).
Another complication of infected TKR was the periprosthetic fracture associated with bone loss, which was reported in some studies, leading to amputation in 6.5% of the cases (2). Infection of the surgical site may be developed after the fracture. Risk of amputation in infected cases is much lower than that in patients with vascular injuries or compartment syndrome; however, infection in TKR is about 46 times higher than vascular complications. According to the present review, the risk of amputation in acute arterial injury is about 27%. There have been various rates of arterial complications after TKR (0.03-0.17) (16, 32, 74-76). These complications are mostly ischemia, thrombosis, and pseudoaneurysm, and few of them are the results of direct popliteal artery lesions. Most surgeons are not anxious about ischemic complications due to their rarity; however, if they occur, there will be a significant increase in the risk of amputation or mortality (77, 78). Moreover, this risk of amputation is about 15% in compartment syndrome and 2.6% in infected cases. Nevertheless, considering the prevalence of these complications, about 97% of the related amputations are the result of infection. Risk of amputation as the outcome of infection is about 81% in a study by Van Rensch (33). In our study amputation rate is 28% in direct vascular injury and 13% in compartment syndrome although these complications are very rare. amputation in infected cases is about 5.1% yet considering its prevalence, infection is the most common reason for amputation (0.025%) [Table 3].
Table 3.
amputation rate based on complication
| complication | Rate in primary TKR% | Rate of Amputation | Amputation rate in complicated TKR |
|---|---|---|---|
| infection | 0.5 | 0.025% | 5.1% |
| Vascular injury | rare | rare | 28% |
| compartment | rare | rare | 13% |
May ethnicity and race affect the outcome of knee arthroplasty?
Ethnicity and race may affect the results of knee replacement. Dunlop et al. reported the role of ethnicity in the rate of joint replacement. They showed fewer rates of arthroplasty in African-Americans, compared to those in Caucasians of the same age (79). This disparity is mainly considered a matter of socio-economic differences; however, an American national database study revealed that this difference exists in the rate of above-the-knee amputation between these two groups (80, 81). The included studies in the present review were not able to prove any specific race as a risk factor for increasing the rate of above-the-knee amputation after knee replacement surgery.
Is arthroplasty identified as a safe procedure?
According to Sierra et al. (2003), only 0.36% of amputations occurred with reasons directly related to TKR, and about 64% of amputations resulted from unrelated reasons to TKR. According to the literature, there is not enough reports related to the real rate of amputations. There is no agreement on specific indications for amputation versus limb salvage procedures, and it is another source of different reported rates in various centers. Almost all mentioned related reasons are infection, severe bone loss, vascular injury, and compartment syndrome. Sierra suggested peripheral vascular disease as the most common reason for amputations (82). The present review demonstrated that infection is the leading cause of related amputations following TKR.
In failed arthroplasties, trying for multiple reconstructions or exact indication of arthrodesis and resection arthroplasty or amputation is not well understood and is different among studies. Even the trend toward both of these two salvage procedures has declined in recent years (83). Amputation may be preferred under certain conditions, such as for tall patients with long lower limbs or cases with extensive and persistent involvement of soft tissues, massive bone loss, or after failure of fusion (84). Most of knee replacements are conducted in older people with lower demand and retired; therefore, there is a need for performing cost-benefit studies to achieve the best outcomes. Psychosocial and economic burdens of TKR are the main concerns for the application of this procedure. Legal issues are among other growing concerns when the patients are not told about the catastrophes (78).
According to the present review, it was shown that amputation is a real end result for knee replacements either in primary or revision knee arthroplasties that needs to be discussed with patients for decision-making. Prevalence of amputation to failure or complications after TKR procedures was estimated between 0.1-10% in different studies. Deep infection was the major cause of amputation. Vascular complications and fractures associated with bone loss and compartment syndrome were other reasons for amputation.
References
- 1.Girzadas DV, Geens S, Clayton ML, Leidholt JD. Performance of a Hinged Metal Knee Prosthesis: A Case Report With A Follow-up Of Three And One-half Years And Histological And Metallurgical Data. JBJS. 1968;50(2):355–64. [PubMed] [Google Scholar]
- 2.de Paula Mozella A, da Palma IM, de Souza AF, Gouget GO, Cobra HAdAB. Amputation after failure or complication of total knee arthroplasty: prevalence, etiology and functional outcomes. Revista Brasileira de Ortopedia (English Edition). 2013;48(5):406–11. doi: 10.1016/j.rboe.2012.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coyte PC, Hawker G, Croxford R, Wright JG. Rates of revision knee replacement in Ontario, Canada. JBJS. 1999;81(6):773–82. doi: 10.2106/00004623-199906000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Why are total knee arthroplasties failing today? Clinical Orthopaedics and Related Research®. 2002;404:7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Font-Rodriguez DE, Scuderi GR, Insall JN. Survivorship of cemented total knee arthroplasty. Clinical orthopaedics and related research. 1997;(345):79–86. [PubMed] [Google Scholar]
- 6.Weir D, Moran C, Pinder I. Kinematic condylar total knee arthroplasty: 14-year survivorship analysis of 208 consecutive cases. The Journal of bone and joint surgery British volume. 1996;78(6):907–11. doi: 10.1302/0301-620x78b6.6678. [DOI] [PubMed] [Google Scholar]
- 7.Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M. Early failures in total knee arthroplasty. Clinical Orthopaedics and Related Research®. 2001;392:315–8. doi: 10.1097/00003086-200111000-00041. [DOI] [PubMed] [Google Scholar]
- 8.Mulhall KJ, Ghomrawi HM, Scully S, Callaghan JJ, Saleh KJ. Current etiologies and modes of failure in total knee arthroplasty revision. Clinical Orthopaedics and Related Research®. 2006;446:45–50. doi: 10.1097/01.blo.0000214421.21712.62. [DOI] [PubMed] [Google Scholar]
- 9.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. JBJS. 2007;89(4):780–5. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 10.Gonzalez MH, Mekhail AO. The failed total knee arthroplasty: evaluation and etiology. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2004;12(6):436–46. doi: 10.5435/00124635-200411000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Sierra RJ, Trousdale RT, Pagnano MW. Above-the-knee amputation after a total knee replacement: prevalence, etiology, and functional outcome. JBJS. 2003;85(6):1000–4. doi: 10.2106/00004623-200306000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Rand JA, Peterson L, Bryan R, Ilstrup D. Revision total knee arthroplasty. Instructional course lectures. 1986;35:305–18. [PubMed] [Google Scholar]
- 13.Bottner F, Gotze C, Koller A, Steinbeck J, Winkelmann W, Gosheger G. Creation of an above-the-knee amputation stump after hip disarticulation for severe periprosthetic infection and fracture A report of two cases. J Bone Joint Surg Am. 2005;87(2):410–3. doi: 10.2106/JBJS.D.01948. [DOI] [PubMed] [Google Scholar]
- 14.Cavadas PC, Thione A, Perez-Garcia A, Lorca-Garcia C, Aranda-Romero F. Salvage of infected intramedullary knee arthrodesis with vascularized free fibula and staged fixation. Injury. 2014;45(11):1772–5. doi: 10.1016/j.injury.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 15.De Paula Mozella A, Da Palma IM, De Souza AF, Gouget GO, De Araújo Barros Cobra HA. Amputation after failure or complication of total knee arthroplasty: Prevalence, etiology and funcional outcomes. Revista Brasileira de Ortopedia. 2013;48(5):406–11. doi: 10.1016/j.rboe.2012.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abularrage CJ, Weiswasser JM, DeZee KJ, Slidell MB, Henderson WG, Sidawy AN. Predictors of lower extremity arterial injury after total knee or total hip arthroplasty. Journal of Vascular Surgery. 2008;47(4):803–7. doi: 10.1016/j.jvs.2007.11.067. [DOI] [PubMed] [Google Scholar]
- 17.Aleto T, Ritter MA, Berend ME. Case report: superficial femoral artery injury resulting from cerclage wiring during revision THA. Clin Orthop Relat Res. 2008;466(3):749–53. doi: 10.1007/s11999-007-0109-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Green S, Higgins J. Cochrane handbook for systematic reviews of interventions. Version. 2005 [Google Scholar]
- 19.Higgins J. Cochrane handbook for systematic reviews of interventions. Version 5.1. 0 [updated March 2011]. The Cochrane Collaboration. www cochrane. handbook org. [Google Scholar]
- 20.Macmull S, Bartlett W, Miles J, Blunn GW, Pollock RC, Carrington RW, et al. Custom-made hinged spacers in revision knee surgery for patients with infection, bone loss and instability. Knee. 2010;17(6):403–6. doi: 10.1016/j.knee.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 21.Klinger H-M, Spahn G, Schultz W, Baums MH. Arthrodesis of the knee after failed infected total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy. 2006;14(5):447–53. doi: 10.1007/s00167-005-0664-3. [DOI] [PubMed] [Google Scholar]
- 22.Jamsen E, Sheng P, Halonen P, Lehto MU, Moilanen T, Pajamaki J, et al. Spacer prostheses in two-stage revision of infected knee arthroplasty. Int Orthop. 2006;30(4):257–61. doi: 10.1007/s00264-006-0102-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pelt CE, Grijalva R, Anderson L, Anderson MB, Erickson J, Peters CL. Two-Stage Revision TKA Is Associated with High Complication and Failure Rates. Adv Orthop. 2014;2014:659047. doi: 10.1155/2014/659047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Briffa N, Ringrose A, Mitchell P, Bridle S. Salvage revision TKR for infection: a 10-year experience of a two-stage re-implantation technique. European Orthopaedics and Traumatology. 2013;4(1):3–8. [Google Scholar]
- 25.Stammers J, Kahane S, Ranawat V, Miles J, Pollock R, Carrington RW, et al. Outcomes of infected revision knee arthroplasty managed by two-stage revision in a tertiary referral centre. The Knee. 2015;22(1):56–62. doi: 10.1016/j.knee.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 26.Jamsen E, Varonen M, Huhtala H, Lehto MU, Lumio J, Konttinen YT, et al. Incidence of prosthetic joint infections after primary knee arthroplasty. J Arthroplasty. 2010;25(1):87–92. doi: 10.1016/j.arth.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 27.Heyse TJ, Ries MD, Bellemans J, Goodman SB, Scott RD, Wright TM, et al. Total knee arthroplasty in patients with juvenile idiopathic arthritis. Clinical Orthopaedics and Related Research®. 2014;472(1):147–54. doi: 10.1007/s11999-013-3095-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holmberg A, Thorhallsdottir VG, Robertsson O, A WD, Stefansdottir A. 75% success rate after open debridement, exchange of tibial insert, and antibiotics in knee prosthetic joint infections. Acta Orthop. 2015;86(4):457–62. doi: 10.3109/17453674.2015.1026756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Larson AN, Hanssen AD, Cass JR. Does prior infection alter the outcome of TKA after tibial plateau fracture? Clinical Orthopaedics and Related Research®. 2009;467(7):1793–9. doi: 10.1007/s11999-008-0615-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mahmud T, Lyons MC, Naudie DD, MacDonald SJ, McCalden RW. Assessing the gold standard: a review of 253 two-stage revisions for infected TKA. Clinical Orthopaedics and Related Research®. 2012;470(10):2730–6. doi: 10.1007/s11999-012-2358-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Herold C, Steiert A, Knobloch K, Busche MN, Altintas MA, Vogt PM. Angiographic findings in patients with postoperative soft tissue defects following total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy. 2011;19(12):2045–9. doi: 10.1007/s00167-011-1532-y. [DOI] [PubMed] [Google Scholar]
- 32.Parvizi J, Pulido L, Slenker N, Macgibeny M, Purtill JJ, Rothman RH. Vascular injuries after total joint arthroplasty. The Journal of arthroplasty. 2008;23(8):1115–21. doi: 10.1016/j.arth.2008.02.016. [DOI] [PubMed] [Google Scholar]
- 33.Van Rensch P, Van de Pol G, Goosen J, Wymenga A, De Man F. Arthrodesis of the knee following failed arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy. 2014;22(8):1940–8. doi: 10.1007/s00167-013-2539-3. [DOI] [PubMed] [Google Scholar]
- 34.Jenny J-Y, Barbe B, Gaudias J, Boeri C, Argenson J-N. High infection control rate and function after routine one-stage exchange for chronically infected TKA. Clinical Orthopaedics and Related Research®. 2013;471(1):238–43. doi: 10.1007/s11999-012-2480-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Helito CP, de Brito AT, Gobbi RG, Demange MK, Tirico LE, Pecora JR, et al. Evaluation of quality of life and walking ability among amputated patients and those who refused to undergo amputation following infection of total knee arthroplasty: Small case series. Prosthet Orthot Int. 2014 doi: 10.1177/0309364614543548. [DOI] [PubMed] [Google Scholar]
- 36.Hsieh PH, Huang KC, Shih HN. Prosthetic Joint Infection in Patients with Rheumatoid Arthritis: An Outcome Analysis Compared with Controls. PLoS ONE. 2013;8:8. doi: 10.1371/journal.pone.0071666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gardner J, Gioe TJ, Tatman P. Can this prosthesis be saved?: implant salvage attempts in infected primary TKA. Clinical Orthopaedics and Related Research®. 2011;469(4):970–6. doi: 10.1007/s11999-010-1417-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Laffer R, Graber P, Ochsner P, Zimmerli W. Outcome of prosthetic knee-associated infection: evaluation of 40 consecutive episodes at a single centre. Clinical microbiology and infection. 2006;12(5):433–9. doi: 10.1111/j.1469-0691.2006.01378.x. [DOI] [PubMed] [Google Scholar]
- 39.Joshy S, Gogi N, Thomas B, Mahale A, Singh B. Delayed onset of deep infection after total knee arthroplasty: comparison based on the infecting organism. Journal of Orthopaedic Surgery. 2007;15(2):154–8. doi: 10.1177/230949900701500205. [DOI] [PubMed] [Google Scholar]
- 40.Röhner E, Windisch C, Nuetzmann K, Rau M, Arnhold M, Matziolis G. Unsatisfactory outcome of arthrodesis performed after septic failure of revision total knee arthroplasty. The Journal of bone and joint surgery American volume. 2015;97(4):298. doi: 10.2106/JBJS.N.00834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim Y-H, Park J-W, Kim J-S, Kim D-J. The outcome of infected total knee arthroplasty: culture-positive versus culture-negative. Archives of orthopaedic and trauma surgery. 2015;135(10):1459–67. doi: 10.1007/s00402-015-2286-7. [DOI] [PubMed] [Google Scholar]
- 42.Choi H-R, Malchau H, Bedair H. Are prosthetic spacers safe to use in 2-stage treatment for infected total knee arthroplasty? The Journal of arthroplasty. 2012;27(8):1474–9. doi: 10.1016/j.arth.2012.02.023. [DOI] [PubMed] [Google Scholar]
- 43.Kuchinad R, Fourman MS, Fragomen AT, Rozbruch SR. Knee arthrodesis as limb salvage for complex failures of total knee arthroplasty. J Arthroplasty. 2014;29(11):2150–5. doi: 10.1016/j.arth.2014.06.021. [DOI] [PubMed] [Google Scholar]
- 44.Choi HR, von Knoch F, Zurakowski D, Nelson SB, Malchau H. Can implant retention be recommended for treatment of infected TKA? Clin Orthop Relat Res. 2011;469(4):961–9. doi: 10.1007/s11999-010-1679-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Westberg M, Paus AC, Holme PA, Tjonnfjord GE. Haemophilic arthropathy: long-term outcomes in 107 primary total knee arthroplasties. Knee. 2014;21(1):147–50. doi: 10.1016/j.knee.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 46.Son M-S, Lau E, Parvizi J, Mont MA, Bozic KJ, Kurtz S. What Are the Frequency, Associated Factors, and Mortality of Amputation and Arthrodesis After a Failed Infected TKA? Clinical Orthopaedics and Related Research®. 2017;475(12):2905–13. doi: 10.1007/s11999-017-5285-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.George J, Navale SM, Schiltz NK, Siccha M, Klika AK, Higuera CA. Racial disparities in above-knee amputations after TKA: a national database study. Clinical Orthopaedics and Related Research®. 2017;475(7):1809–15. doi: 10.1007/s11999-016-5195-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Amouyel T, Brunschweiler B, Freychet B, Lautridou C, Rosset P, Massin P, et al. No improvement in the post-TKA infection prognosis when the implant is not reimplanted: Retrospective multicentre study of 72 cases. Orthopaedics & Traumatology: Surgery & Research. 2015;101(6):S251–S5. doi: 10.1016/j.otsr.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 49.Bengtson S, Knutson K. The infected knee arthroplasty: a 6-year follow-up of 357 cases. Acta Orthopaedica Scandinavica. 1991;62(4):301–11. doi: 10.3109/17453679108994458. [DOI] [PubMed] [Google Scholar]
- 50.Isiklar ZU, Landon GC, Tullos HS. Amputation after failed total knee arthroplasty. Clinical orthopaedics and related research. 1994(299):173–8. [PubMed] [Google Scholar]
- 51.Pal A, Clarke J, Cameron A. Case series and literature review: popliteal artery injury following total knee replacement. International Journal of Surgery. 2010;8(6):430–5. doi: 10.1016/j.ijsu.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 52.Houdek MT, Wagner ER, Wyles CC, Harmsen WS, Hanssen AD, Taunton MJ, et al. Long-term outcomes of pedicled gastrocnemius flaps in total knee arthroplasty. JBJS. 2018;100(10):850–6. doi: 10.2106/JBJS.17.00156. [DOI] [PubMed] [Google Scholar]
- 53.Friedrich MJ, Schmolders J, Wimmer MD, Strauss AC, Ploeger MM, Wirtz DC, et al. Two-stage knee arthrodesis with a modular intramedullary nail due to septic failure of revision total knee arthroplasty with extensor mechanism deficiency. The Knee. 2017;24(5):1240–6. doi: 10.1016/j.knee.2017.05.019. [DOI] [PubMed] [Google Scholar]
- 54.Goldman AH, Clark NJ, Taunton MJ, Lewallen DG, Berry DJ, Abdel MP. Definitive Resection Arthroplasty of the Knee: A Surprisingly Viable Treatment to Manage Intractable Infection in Selected Patients. The Journal of Arthroplasty. 2019 doi: 10.1016/j.arth.2019.10.025. [DOI] [PubMed] [Google Scholar]
- 55.McQuail P, McCartney B, Baker J, Green J, Keogh P, Kenny P. Radiographic and Functional Outcomes following Knee Arthrodesis Using the Wichita Fusion Nail. The journal of knee surgery. 2018;31(05):479–84. doi: 10.1055/s-0037-1604148. [DOI] [PubMed] [Google Scholar]
- 56.Perry KI, Salib CG, Larson DR, Pagnano MW, Abdel MP, Hanssen AD. Two-stage exchange and Marlex-Mesh reconstruction for infection with extensor mechanism disruption after total knee arthroplasty. JBJS. 2018;100(17):1482–9. doi: 10.2106/JBJS.17.01439. [DOI] [PubMed] [Google Scholar]
- 57.Jamsen E, Nevalainen P, Kalliovalkama J, Moilanen T. Preoperative hyperglycemia predicts infected total knee replacement. Eur J Intern Med. 2010;21(3):196–201. doi: 10.1016/j.ejim.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 58.Wang KH, Yu SW, Iorio R, Marcantonio AJ, Kain MS. Long Term Treatment Results for Deep Infections of Total Knee Arthroplasty. J Arthroplasty. 2015;30(9):1623–8. doi: 10.1016/j.arth.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 59.Vu DL, Uckay I, Gonzalez A, Rohner P, Hoffmeyer P, Lubbeke A. Factors related to outcome of early and delayed prosthetic joint infections. doi: 10.1016/j.jinf.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 60.Vrgoc G, Japjec M, Gulan G, Ravlic-Gulan J, Marinovic M, Bandalovic A. Periprosthetic infections after total hip and knee arthroplasty--a review. Coll Antropol. 2014;38(4):1259–64. [PubMed] [Google Scholar]
- 61.Tigani D, Trisolino G, Fosco M, Ben Ayad R, Costigliola P. Two-stage reimplantation for periprosthetic knee infection: Influence of host health status and infecting microorganism. Knee. 2013;20(1):9–18. doi: 10.1016/j.knee.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 62.Radoicic D, Popovic Z, Barjaktarovic R, Marinkovic J. Infected total knee arthroplasty treatment outcome analysis. Vojnosanit Pregl. 2012;69(6):504–9. [PubMed] [Google Scholar]
- 63.Jones RE, Huo MH. The infected knee: all my troubles now. J Arthroplasty. 2006;21(4 Suppl 1):50–3. doi: 10.1016/j.arth.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 64.Garvin KL, Konigsberg BS. Infection following total knee arthroplasty: prevention and management. Instr Course Lect. 2012;61:411–9. [PubMed] [Google Scholar]
- 65.Garg P, Ranjan R, Bandyopadhyay U, Chouksey S, Mitra S, Gupta SK. Antibiotic-impregnated articulating cement spacer for infected total knee arthroplasty. Indian J Orthop. 2011;45(6):535–40. doi: 10.4103/0019-5413.87126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Castelli CC, Gotti V, Ferrari R. Two-stage treatment of infected total knee arthroplasty: two to thirteen year experience using an articulating preformed spacer. Int Orthop. 2014;38(2):405–12. doi: 10.1007/s00264-013-2241-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cahill JL, Shadbolt B, Scarvell JM, Smith PN. Quality of life after infection in total joint replacement. J Orthop Surg (Hong Kong). 2008;16(1):58–65. doi: 10.1177/230949900801600115. [DOI] [PubMed] [Google Scholar]
- 68.Van Rensch PJH, Van de Pol GJ, Goosen JHM, Wymenga AB, De Man FHR. Arthrodesis of the knee following failed arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy. 2014;22(8):1940–8. doi: 10.1007/s00167-013-2539-3. [DOI] [PubMed] [Google Scholar]
- 69.Joshy S, Gogi N, Thomas B, Mahale A, Singh BK. Delayed onset of deep infection after total knee arthroplasty: comparison based on the infecting organism. Journal of Orthopaedic Surgery. 2007;15(2):154–8. doi: 10.1177/230949900701500205. [DOI] [PubMed] [Google Scholar]
- 70.Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, et al. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010;468(1):45–51. doi: 10.1007/s11999-009-0945-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kurtz SM, Lau E, Schmier J, Ong KL, Zhao K, Parvizi J. Infection burden for hip and knee arthroplasty in the United States. The Journal of arthroplasty. 2008;23(7):984–91. doi: 10.1016/j.arth.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 72.Kurtz SM, Ong KL, Lau E, Bozic KJ, Berry D, Parvizi J. Prosthetic joint infection risk after TKA in the Medicare population. Clinical Orthopaedics and Related Research®. 2010;468(1):52–6. doi: 10.1007/s11999-009-1013-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fascia D, Singanayagam A, Keating J. Methicillin-resistant Staphylococcus aureus in orthopaedic trauma: identification of risk factors as a strategy for control of infection. The Journal of bone and joint surgery British volume. 2009;91(2):249–52. doi: 10.1302/0301-620X.91B2.21339. [DOI] [PubMed] [Google Scholar]
- 74.Smith DE, McGraw RW, Taylor DC, Masri BA. Arterial complications and total knee arthroplasty. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2001;9(4):253–7. doi: 10.5435/00124635-200107000-00005. [DOI] [PubMed] [Google Scholar]
- 75.Calligaro KD, Dougherty MJ, Ryan S, Booth RE. Acute arterial complications associated with total hip and knee arthroplasty. Journal of vascular surgery. 2003;38(6):1170–5. doi: 10.1016/s0741-5214(03)00918-2. [DOI] [PubMed] [Google Scholar]
- 76.Rand JA. Vascular complications of total knee arthroplasty: report of three cases. The Journal of arthroplasty. 1987;2(2):89–93. doi: 10.1016/s0883-5403(87)80014-1. [DOI] [PubMed] [Google Scholar]
- 77.Kumar SN, Chapman J, Rawlins I. Vascular injuries in total knee arthroplasty: a review of the problem with special reference to the possible effects of the tourniquet. The Journal of arthroplasty. 1998;13(2):211–6. doi: 10.1016/s0883-5403(98)90102-4. [DOI] [PubMed] [Google Scholar]
- 78.Haggis P, Yates P, Blakeway C, Fick D, Morgan D, Holt M, et al. Compartment syndrome following total knee arthroplasty: a report of seven cases. The Journal of bone and joint surgery British volume. 2006;88(3):331–4. doi: 10.1302/0301-620X.88B3.16919. [DOI] [PubMed] [Google Scholar]
- 79.Dunlop DD, Manheim LM, Song J, Sohn MW, Feinglass JM, Chang HJ, et al. Age and racial/ethnic disparities in arthritis-related hip and knee surgeries. Medical care. 2008;46(2):200–8. doi: 10.1097/MLR.0b013e31815cecd8. [DOI] [PubMed] [Google Scholar]
- 80.Centers for Disease C, Prevention Racial disparities in total knee replacement among Medicare enrollees--United States, 2000-2006. MMWR Morbidity and mortality weekly report. 2009;58(6):133. [PubMed] [Google Scholar]
- 81.George J, Navale SM, Schiltz NK, Siccha M, Klika AK, Higuera CA. Racial Disparities in Above-knee Amputations After TKA: A National Database Study. Clinical Orthopaedics and Related Research. 2016:1–7. doi: 10.1007/s11999-016-5195-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sierra RJ, Trousdale RT, Pagnano MW. Above-the-knee amputation after a total knee replacement: prevalence, etiology, and functional outcome. The Journal of bone and joint surgery American volume. 2003;85-a(6):1000–4. doi: 10.2106/00004623-200306000-00003. [DOI] [PubMed] [Google Scholar]
- 83.Son M-S, Lau E, Parvizi J, Mont MA, Bozic KJ, Kurtz S. What Are the Frequency, Associated Factors, and Mortality of Amputation and Arthrodesis After a Failed Infected TKA? Clinical Orthopaedics and Related Research®. 2017:1–9. doi: 10.1007/s11999-017-5285-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gehrke T, Alijanipour P, Parvizi J. The management of an infected total knee arthroplasty. Bone Joint J. 2015;97-b(10 Suppl A):20–9. doi: 10.1302/0301-620X.97B10.36475. [DOI] [PubMed] [Google Scholar]