Abstract
Background: Psychological well-being (PWB) is predictive of future health and mortality. Midlife is a pivotal time in women's lives and may impact future PWB. This study, based on a longitudinal cohort of women, sought to identify how personal and social resources and modifiable behaviors at midlife relate to women's PWB in later life, and to determine if psychological resilience in later life moderates the impact of health problems on PWB.
Materials and Methods: We assessed the association of midlife factors with PWB ∼9 years later in 1693 women from the multiracial/ethnic Study of Women's Health Across the Nation (SWAN) cohort. PWB was a composite score with cognitive and affective components. Midlife factors included sociodemographics, health, menopause-related, and psychosocial factors collected over the course of midlife.
Results: In a multivariable model, greater PWB at an older age was associated with the following at midlife: less financial strain, greater physical activity, not smoking, better physical functioning, and fewer sleep problems. More positive attitudes toward menopause and aging, less cynicism, greater optimism, less trait anxiety, greater spirituality, and greater resilience were also independently associated with better PWB. Chinese women reported lower PWB compared with whites. Later life resilience moderated the impact of sleep problems on PWB.
Conclusions: Several modifiable factors at midlife are associated with better PWB in older women and highlight the importance of healthy behaviors such as physical activity and good sleep hygiene at midlife. Interventions to increase optimism, spirituality, and resilience are also worth exploring.
Keywords: psychological well-being, aging, women, midlife
Introduction
Psychological or subjective well-being (PWB or SWB) has long been a major focus of studies of aging. Well-being has been conceptualized and defined in multiple ways, including SWB, PWB, positive affect, and life satisfaction. Two broad conceptualizations of well-being are hedonic and eudaimonic. Hedonic well-being refers to the pursuit of happiness and is generally characterized by high positive affect and the evaluation of one's life as satisfying.1 Eudaimonic well-being typically refers to a more evaluative component and includes meaningful pursuits and personal growth as seen in the scales developed by Ryff.2 PWB is considered the broadest and most all-inclusive term that covers SWB, cognitive reflections, and affect.3 To assess this broad construct of PWB, studies often use multiple measures4,5 or a composite score6 that encompasses these various aspects of well-being.
Despite being defined and measured in multiple ways, PWB importantly has been shown to predict future health and mortality.7–10 For example, the longitudinal survey of Midlife Development in the United States (MIDUS) found that participants who were persistently high in PWB over 9–10 years had better subjective health, fewer symptoms, chronic conditions, and functional impairments compared with those who had persistently low PWB.8 A study of men and women aged 60 years and older found that higher levels of life enjoyment predicted less impaired functioning 8 years later.9 Positive well-being was also strongly related to less cardiovascular disease after 12 years of follow-up in an initially healthy group of men and women.10
Given the importance of PWB or SWB for subsequent health and mortality, studies have examined determinants of well-being, although most of these are cross-sectional.11 Education and income are strong predictors of well-being later in life,12 with income being a bit stronger. Self-rated health, social integration, social support, a sense of control, and mastery have also been related to well-being.11,13 In a cross-sectional study of women aged 65 years and older, Lukaschek et al. found that low income, physical inactivity, multimorbidity, depression, anxiety, and sleeping problems were associated with low SWB.14 However, given the cross-sectional nature of the majority of this research, we know little about how earlier life characteristics impact well-being at older ages.
Dispositional factors such as psychological resilience and optimism may be related to PWB and may moderate decreases in physical function or increases in comorbidities associated with aging. Psychological resilience, a personal characteristic that enables one to thrive in the face of adversity and adapt to change,15 has been shown to be protective in the face of worsening health or living circumstances in later life.16,17 Longitudinal studies have also found that greater optimism18,19 predicts better life satisfaction in later life.
Midlife can be a pivotal time in women's lives, with the menopausal transition representing a key physiological and psychosocial event. This transition, encompassing hormonal and biological changes, can provide a marker in the aging process, and may occur at a time of changes in family structure and social roles. All of these factors may influence women's health or lifestyle behaviors, which may have important implications for later PWB. In conceptualizing well-being during the menopausal transition, Brown et al. considered both hedonic well-being and eudaimonic well-being important.20 Their systematic review of studies of positive well-being during the menopausal transition identified a range of factors related to well-being, including stress, life events, loneliness, exercise, smoking, work satisfaction, attitudes toward aging and menopause, and mastery.
Only one study, however, went beyond the transition.21 The Melbourne Women's Midlife Health Project (MWMHP) reports longitudinal data on life satisfaction and well-being among 267 mostly white women who were followed for 9 years over the menopausal transition. They found that more positive attitudes toward aging and menopause, positive feelings for partner, fewer daily hassles, and not smoking were related to better later life satisfaction.21 They also found that becoming married or partnered and increased work satisfaction were related to more positive well-being (defined as the difference between positive and negative affect), while experiencing a major life event and increased daily hassles were related to decreased well-being 9 years later.22
The present analyses take advantage of data from the 20-year longitudinal multiethnic/racial Study of Women's Health Across the Nation (SWAN) to evaluate how factors collected over the course of midlife contribute to PWB measured ∼9 years later. Specifically, the objectives of the present study are as follows: (1) to examine the extent to which personal and social resources and modifiable behaviors at midlife contribute to women's PWB at later life, and the extent to which race or ethnicity is associated with PWB; and (2) to determine if concurrent psychological resilience moderates the impact of health problems (e.g., poor health, sleep problems) or negative events on PWB in older age.
Materials and Methods
Sample and procedures
SWAN is a multiracial/ethnic cohort study characterizing biological and psychosocial changes occurring during the menopausal transition.23 From 1995 to 1997, each of seven clinical sites recruited non-Hispanic white women and women belonging to a predetermined racial/ethnic minority (African American women in Pittsburgh, Boston, Michigan, Chicago; Japanese women in Los Angeles; Hispanic women in Newark; Chinese women in Oakland, California). The protocol was approved by the institutional review boards at each site. All participants provided written informed consent.
Baseline eligibility included age 42–52 years; an intact uterus and at least one ovary; not pregnant, lactating, using oral contraceptives, or hormone therapy (HT); and having a menstrual cycle in the 3 months before screening. Among cohort-eligible women, 50.7% (n = 3303) entered the longitudinal study.23 The SWAN cohort sample size was determined to have adequate power to detect menopause transition-related within-women changes in outcomes. Participants were assessed in-person at baseline and through follow-up visit 15 from 1996 to 2017 using a standardized protocol of detailed questions about medical, reproductive, and menstrual history; lifestyle and psychosocial factors; physical and psychological symptoms; and anthropometric measurements. Visits occurred approximately annually until after visit 10 when they were spaced further apart. All instruments were translated into Spanish, Japanese, and Cantonese.
PWB was measured for the first, and only, time at follow-up visit 15 and was obtained from 1911 women still participating in SWAN at that follow-up visit. Reasons for nonparticipation at visit 15 were as follows: withdrew from SWAN before visit 15 (n = 788), missed the visit (n = 275), and deceased (n = 149). Of the 2091 women still participating in SWAN, 180 did not complete the measures of well-being because they either had an abbreviated telephone interview or did not complete the full SWAN protocol (n = 106), or had missing data on one or more of the well-being scales (n = 37).
Researchers have generally considered midlife to encompass the ages of 40–60, but also consider other factors, making it a relative approximation.24 For the purpose of these analyses, we consider the ages of 40–60 as midlife, but also take the menopause transition into account. In considering midlife predictors of PWB, we include SWAN data from baseline to visit 10 encompassing ages 42–60. Our primary outcome, PWB, which was measured at visit 15, occurred ∼9 years after visit 10 when women were ages 61–69. We exclude women from analyses who were older than 60 at or before visit 10 (n = 211), had not yet entered the menopause transition by visit 10 (n = 5), or were not yet postmenopausal by visit 15 (n = 2), for a final sample size of 1693. Supplementary Fig. S1 shows when SWAN visits occurred and the age of the sample at these visits.
Measures
Primary outcome
To include both the hedonic and eudaimonic aspects of PWB, we developed a composite measure of PWB consisting of four measures: the Satisfaction with Life scale,25 the Positive and Negative Affect Scale (PANAS) positive affect scale26 and the Ryff Purpose in Life and Personal Growth scales.2 The Life Satisfaction scale contains 5 items (e.g., “I am satisfied with my life,” “So far, I have gotten the important things I want in life”) that are rated on a 7-point scale from strongly disagree to strongly agree. Items are summed to create a total score where high scores reflect greater life satisfaction. The PANAS positive affect scale,26 which contains 10 adjectives (e.g., interested, excited, alert) asking how a person felt in the past 7 days, served as the affective measure. Responses are on a 6-point scale that range from very slightly or not at all to extremely. The Purpose in Life and Personal Growth scales each contain 7 items asking respondents to rate their agreement on a 6-point scale from strongly disagree to strongly agree with statements such as: “I have a sense of direction and purpose in life” and “For me, life has been a continuous process of learning, changing, and growth.”
Principal component analysis (PCA) was used to examine the factor structure of the four well-being measures. The PCA was run on standardized values of the total scores of each of the four well-being measures to account for differences in scales and variances. Examination of PCA results, including scree plots and eigenvalues, indicated one factor, with all items loading strongly on the factor (Cronbach's alpha = 0.77). The composite score was created by using factor loading results as weights for each of the scales and then summing the weighted values. The PWB score is thus also a standardized score, with a mean of zero and a standard deviation equal to one.
Predictors
Midlife predictors of later life PWB were selected to include sociodemographic, health-related, menopause-related, and psychosocial factors considered to influence SWB13 and previously found to be associated with PWB during the menopause transition.20 Predictors included (1) those that were obtained once during the midlife period and were not considered to be time-varying (race/ethnicity, educational attainment, duration of perimenopause, cynicism, optimism, trait anxiety, spirituality); (2) those that were obtained annually during midlife and were considered to be time-varying (difficulty paying for basics, marital status, self-assessed health, comorbidities, sleep problems, quality of life, use of HT, vasomotor symptoms (VMS), smoking, physical activity, body mass index (BMI), anxiety, depressive symptoms, stress, and social support); and (3) those that were concurrent with PWB at visit 15 (age at visit 15, resilience).
Because we only have one measure of PWB in later life, time-varying midlife predictors were summarized for modeling. To do this, we considered baseline through visit 10 to be the midlife period and obtained cumulative values of predictors from all available visits during this time. Area under the curve (AUC) analysis was used for continuous predictors. We calculated AUC for each time-varying continuous predictor using Reimann sums.27 The proportion of visits from baseline through visit 10 with reporting of a specific characteristic (e.g., the proportion of visits the participant reported being married/partnered vs. not) was used to summarize dichotomous time-varying predictors. For predictors that were unlikely to change over time (e.g., education), we used values from SWAN baseline or the visit at which the predictor was assessed since these were not assessed at every visit. Predictors were organized into five domains: sociodemographic, health-related, menopause-related, health behaviors, and psychosocial factors. Details of the measures used are provided below.
Sociodemographic variables were race/ethnicity, age at visit 15, educational attainment (<high school, high school or some college, college/more than college), the proportion of visits with difficulty paying for basics (somewhat/very hard to pay for basics vs. not at all hard), and the proportion of visits married or partnered. Ethnicity was self-defined at baseline by participants in response to the open-ended question: “How would you describe your primary racial or ethnic group?” Responses were categorized as white, black, Chinese, Hispanic, or Japanese.
Health-related factors included the proportion of visits with self-assessed health rated fair or poor; number of medical conditions ever reported during midlife (none, 1, or 2 or more of the following: diabetes, hypertension, high cholesterol, arthritis/osteoarthritis, under/overactive thyroid, heart attack, angina, or stroke); and the proportion of visits with sleep problems (any of the following: difficulty falling asleep, staying asleep, and/or early morning awakening reported ≥3 times/week in past 2 weeks). We also examined three domains from the SF-36,28 which assesses the impact of health in various life areas: physical functioning, role limitations due to physical health, and role limitations due to emotional health. For all three domains, we used the previously used cut-point of scoring in the lowest 25% to indicate poor functioning29 and computed the proportion of visits with poor functioning in each domain. We also controlled for psychiatric medication use at visit 15. Participants completed a detailed medication review, and those reporting having taken antidepressant, anxiolytic, or antipsychotic medications were classified as psychiatric medication users.
Menopause-related variables included duration of perimenopause (calculated as the estimated time a woman began early perimenopause, defined as bleeding in the previous 3 months and changes in menstrual regularity in the past year, to one year after the final menstrual period), ever use of HT, attitudes toward menopause and aging from Visit 9,30 and the proportion of visits with frequent VMS, defined as experiencing hot flashes or night sweats, at least 6 days in the previous 2 weeks. Duration of perimenopause was used instead of menopause status because 97% of women were postmenopausal by visit 15 and longer duration of perimenopause has been shown to be an important variable related to depression.31
Health behaviors included physical activity (AUC)32 and BMI (weight [kg]/height [m2] [AUC]), and the proportion of visits reporting cigarette smoking. The physical activity measure in SWAN, referred to as the Kaiser Physical Activity Survey (KPA) is adapted from the short physical activity survey developed by Baecke.33 We used the total score that includes the sports, active living, and household/childcare domains.
Psychosocial factors included a one-time measure at baseline of cynicism from the Cook-Medley Cynicism scale34; optimism as measured by the short version Life Orientation Test35 at visit 1; trait anxiety by the Spielberger State-Trait Anxiety Inventory at visit 4,36 and spirituality by the Daily Spiritual Experience Scale37 at visit 4. Other psychosocial measures were the cumulative measures of the proportion of visits with high anxiety (sum of 4 items with score ≥4), the proportion of visits with depressive symptoms (Center for Epidemiologic Studies Depression [CES-D] ≥16 CES-D scale),38 proportion of visits with 2+ stressful life events, and perceived stress (AUC of summed score of 4 items),39 and emotional and instrumental social support (AUC).40 Psychological resilience was measured at visit 15 with the 10-item Connor-Davidson Resilience Scale.15
Statistical analyses
Preliminary analyses included descriptive plots and statistics (means, standard deviations, ranges, frequencies), as well as an examination of the correlation among predictors. Continuous variables were assessed for normality and transformations applied as necessary.
Multiple linear regression was used to assess the relationship of the PWB composite score with midlife health status, health behaviors, psychological and social function, and menopause-related and socioeconomic characteristics. Nontime-varying variables were ethnicity, education, daily spiritual experiences, trait anxiety, optimism, hostility, and attitudes toward menopause, as these variables were either measured at one visit or are thought not to change over time. All other variables were summarized from visits baseline to 10 as described in the methods.
All linear regression models included age, ethnicity, and clinical site. Remaining variables were then assessed separately within their domains (sociodemographic, health-related, menopause-related, health behaviors, and psychosocial) for collinearity and significance of relationship with the PWB score. Variables that were significant at p < 0.05 within each domain were included in the final multivariable model and manual backward elimination was performed until all variables in the model (except forced—site, age, ethnicity, psychiatric medications at visit 15) were significant at p < 0.05. In addition, we tested the interactions between psychological resilience and stressful life events, perceived stress, self-reported health, number of comorbidities, and sleep problems.
SAS system version 9.3 (SAS Institute, Inc., Cary, NC) was used for all analyses.
Results
Sample characteristics
Characteristics of the analytic sample at the SWAN baseline are shown in Table 1. The mean age of the sample at the beginning of SWAN was 45.8 years, about 69% of women were partnered, almost half (47.9%) had completed college, and 58.6% were premenopausal and 41.4% early perimenopausal.
Table 1.
Baseline Characteristics of the Analytic Sample Expressed as Percentage of Sample Unless Otherwise Noted (n = 1693)
| Characteristic | n | % |
|---|---|---|
| Race/ethnicity | ||
| Non-Hispanic white | 822 | 48.5 |
| Black | 442 | 26.1 |
| Hispanic | 94 | 5.6 |
| Chinese | 167 | 9.9 |
| Japanese | 168 | 9.9 |
| Age (years) at baseline, mean, SD | 45.8 | 2.2 |
| Education | ||
| Less than high school | 345 | 20.6 |
| High School/some college | 529 | 31.5 |
| College/more than college | 803 | 47.9 |
| Somewhat/very hard pay basics | 582 | 34.6 |
| Partnered | 1143 | 68.6 |
| Self-reported fair/poor health | 239 | 14.2 |
| No. of chronic medical conditions | ||
| 0 | 928 | 56.3 |
| 1 | 476 | 28.9 |
| ≥2 | 245 | 14.8 |
| Menopausal status | ||
| Premenopause | 986 | 58.6 |
| Early perimenopause | 698 | 41.4 |
| Frequent VMS | 156 | 9.3 |
| Physical activity score, mean, SD | 7.7 | 1.8 |
| Current smoking | 233 | 13.8 |
| BMI, mean, SD | 27.5 | 7.0 |
| High anxiety | 346 | 20.7 |
| CES-D ≥ 16 | 391 | 23.1 |
BMI, body mass index; CES-D, Center for Epidemiologic Studies Depression; VMS, vasomotor symptoms.
Bivariate associations between predictors and PWB score
Table 2 shows the bivariate associations between the predictors and PWB. As can be seen in this table, most predictors were significantly associated with PWB in the expected direction. Better PWB was associated with being partnered; more positive attitudes toward menopause and aging; and greater physical activity, optimism, resilience, spirituality, and social support. Lower PWB was associated with less education; difficulty paying for basics; sleep problems; self-reported fair/poor health; poor role physical, role emotional, and physical function; frequent VMS; current smoking; higher BMI; greater cynicism; both trait and state anxiety; depressive symptom; 2+ stressful events; and greater perceived stress. Compared with women with no comorbidities, having only one comorbidity was not significantly related to PWB, but having two or more comorbidities was. Blacks did not differ significantly from whites, although Hispanic, Chinese, and Japanese women had significantly lower PWB compared with whites. The only variables not associated with PWB were age, duration of perimenopause, and ever use of HT.
Table 2.
Bivariate Associations Between Predictors and Psychological Well-Being
| Predictor | β (95% CI) | p-Value |
|---|---|---|
| Sociodemographics | ||
| Race/ethnicity | ||
| White (reference) | — | — |
| Black | −0.06 (−0.18 to 0.05) | 0.26 |
| Hispanic | −0.77 (−0.97 to −0.56) | <0.0001 |
| Chinese | −0.52 (−0.68 to −0.36) | <0.0001 |
| Japanese | −0.32 (−0.48 to −0.16) | <0.001 |
| Age at visit 15 | −0.01 (−0.03 to 0.01) | 0.32 |
| Education | ||
| Less than high school | −0.59 (−0.72 to −0.47) | <0.0001 |
| High school/some college | −0.24 (−0.35 to −0.13) | <0.0001 |
| College/more than college (reference) | — | — |
| Proportion of visits somewhat/very hard pay basics | −0.65 (−0.78 to −0.53) | <0.0001 |
| Proportion of visits partnered | 0.19 (0.08 to 0.30) | 0.001 |
| Health-related | ||
| No. of chronic medical conditions | ||
| 0 (reference) | — | — |
| 1 | −0.09 (−0.023 to 0.06) | 0.25 |
| 2+ | −0.28 (−0.41 to −0.16) | <0.0001 |
| Proportion of visits with sleep problems | −0.50 (−0.65 to −0.35) | <0.0001 |
| Proportion of visits with self-reported fair/poor health | −1.38 (−1.57 to −1.19) | <0.0001 |
| Proportion of visits with poor role physical | −0.93 (−1.10 to −0.76) | <0.0001 |
| Proportion of visits with poor role emotional | −0.96 (−1.12 to −0.80) | <0.0001 |
| Proportion of visits with poor physical function | −0.79 (−0.91 to −0.65) | <0.0001 |
| Menopause-related | ||
| Attitudes toward menopause and aging | 0.70 (0.58 to 0.83) | <0.0001 |
| Proportion of visits with frequent vasomotor symptoms | −0.28 (−0.49 to −0.07) | 0.01 |
| Duration of perimenopause | 0.002 (−0.02 to 0.02) | 0.82 |
| Ever use of hormone therapy | 0.02 (−0.07 to 0.12) | 0.62 |
| Health behaviors | ||
| Physical activity (area under curve) | 0.17 (0.15 to 0.21) | <0.0001 |
| Proportion of visits with current smoking | −0.46 (−0.63 to −0.29) | <0.0001 |
| Body mass index (area under curve) | −0.01 (−0.01 to −0.002) | 0.04 |
| Psychosocial | ||
| Cynicism | −0.08 (−0.10 to −0.06) | <0.0001 |
| Optimism | 0.10 (0.09 to 0.12) | <0.0001 |
| Trait anxiety | −0.10 (−0.11 to −0.09) | <0.0001 |
| Resilience visit 15 | 0.098 (0.09 to 0.10) | <0.0001 |
| Proportion of visits with high anxiety | −1.26 (−1.44 to −1.08) | <0.0001 |
| Proportion of visits with CES-D ≥ 16 | −1.59 (−1.77 to −1.42) | <0.0001 |
| Spirituality | 0.17 (0.12 to 0.21) | <0.0001 |
| Proportion of visits with 2+ stressful life events | −0.40 (−0.58 to −0.22) | <0.0001 |
| Perceived stress (area under curve) | −0.22 (−0.23 to −0.19) | <0.0001 |
| Social support (area under curve) | 0.12 (0.10 to 0.14) | <0.0001 |
Adjusted model of PWB
Before analyzing an adjusted model, we analyzed together the predictors listed above within each domain to check for collinearity and to identify which predictors within the domain were significantly associated with PWB. The following variables were significant within the domain models and were included in the multivariable modeling process: sociodemographic factors: education and difficulty paying for basics (financial strain); health-related: self-assessed health, sleep problems, role emotional, and poor physical function; menopause-related: attitudes toward menopause; health behaviors: physical activity, smoking; psychosocial: trait anxiety, optimism, cynicism, depressive symptoms, stressful life events, perceived stress, spirituality, and resilience.
In the adjusted model (Table 3), greater PWB at an older age was associated with the following characteristics at midlife: greater physical activity, more positive attitudes toward menopause and aging, greater optimism, and greater spirituality, and greater resilience at visit 15. Difficulty paying for basics, poor physical function, sleep problems, smoking, cynicism, and trait anxiety at midlife were all associated with lower PWB. We also found racial/ethnic differences with Chinese women reporting lower PWB compared with whites.
Table 3.
Adjusted Model of Psychological Well-Being
| Variable | β (95% CI) | p-Value |
|---|---|---|
| Race/ethnicity | ||
| Non-Hispanic white (reference) | — | — |
| Black | 0.07 (−0.05 to 0.19) | 0.22 |
| Hispanic | −0.23 (−0.50 to 0.03) | 0.09 |
| Chinese | −0.25 (−0.45 to −0.05) | 0.01 |
| Japanese | −0.14 (−0.33 to 0.05) | 0.15 |
| Age (years) at visit 15 | −0.005 (−0.02 to 0.01) | 0.59 |
| Proportion of visits somewhat/very hard pay basics | −0.16 (−0.29 to −0.04) | 0.01 |
| Proportion of visits with poor physical function | −0.22 (−0.35 to −0.09) | <0.001 |
| Proportion of visits with sleep problems | −0.87 (−1.44 to −0.29) | 0.003 |
| Attitudes toward menopause/aging | 0.13 (0.02 to 0.24) | 0.02 |
| Physical activity (AUC) | 0.05 (0.02 to 0.08) | <0.001 |
| Proportion of visits with current smoking | −0.17 (−0.32 to −0.02) | 0.02 |
| Cynicism/hostility | −0.02 (−0.04 to −0.01) | <0.001 |
| Optimism | 0.01 (0.002 to 0.03) | 0.02 |
| Trait anxiety | −0.02 (−0.03 to −0.01) | <0.0001 |
| Spirituality | 0.05 (0.01 to 0.09) | 0.02 |
| Resilience visit 15 | 0.07 (0.06 to 0.08) | <0.0001 |
| Sleep × resilience | 0.02 (0.005 to 0.04) | 0.01 |
| Psychiatric medication use visit 15 | −0.02 (−0.12 to 0.08) | 0.70 |
Bold indicates significance.
Also adjusted for study site.
AUC, area under the curve.
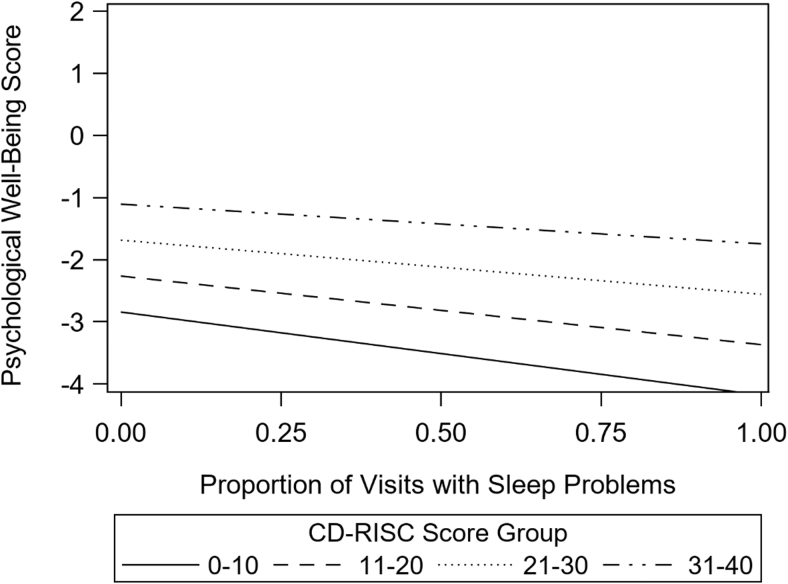
Of those variables tested for an interaction with resilience (self-reported health, number of comorbidities, stressful life events, sleep, and physical function), the only variable that had a significant interaction with resilience was sleep (β = 0.02, p = 0.01). Reporting sleep problems was negatively related to PWB when resilience was low, but was unrelated to PWB when resilience was high. This interaction is depicted in Figure 1where the Connor-Davidson score is broken into four levels for illustrative purposes.
FIG. 1.
Relationship between psychological well-being and sleep problems across levels of psychological resilience. CD-RISC, Connor-Davidson Resilience Scale.
Discussion
Our study identified a range of factors assessed over the course of midlife that were related to better PWB at later life. Most notably, modifiable factors such as higher levels of physical activity, not smoking, and fewer sleep problems were each independently related to better PWB at an older age. The health benefits of physical activity have been well documented41 and studies have shown a positive association between physical activity and SWB in older adults.14 However, studies have also reported declines in physical activity with age.42 MIDUS has shown that over an 18- to 20-year period of middle and later life, 50% of respondents showed a steady decline in physical activity.43 Nevertheless, in general, these declines in physical activity are not inevitable and physical activity can be increased during middle and later life.44 A regimen to increase physical activity at midlife and beyond is feasible and important for later well-being.
Sleep health is also increasingly recognized as critically important for health and well-being,45–47 yet numerous studies have shown that sleep problems increase with age with 40%–60% of postmenopausal women reporting poor sleep.48 Our results highlight the importance of sleep during midlife for long-term well-being and suggest that mitigation of sleep problems in midlife may have benefits for PWB in later life. An increasing body of evidence points to effective behavioral modifications that help improve sleep.49,50 Taken together, these results provide further evidence that middle age may represent an important time point for improving health behaviors for future PWB.
We also found several dispositional characteristics related to better PWB. Greater optimism, spirituality, lower trait anxiety, and cynicism at midlife were all independently related to better PWB at an older age. Although other studies have also shown that these characteristics are related to better well-being,18,19 it is worth pointing out that these characteristics were all independently associated with better PWB at an older age. Although these characteristics are generally viewed as stable over time, there have been some attempts to increase optimism19 and spirituality51 and such interventions are worth pursuing. It is also possible that PWB earlier in life led to greater optimism. Although longitudinal studies have also found that greater optimism18,19 predicts better life satisfaction in later life, one cannot rule out the possibility that PWB is a precursor to optimism.
Consistent with other studies,4 poor physical function over midlife was negatively related to PWB. Although social support was significantly related to PWB in the bivariate analyses, it was not significant in the final multivariable model building, possibly due to its correlation with resilience (positive) and cynicism (negative). The presence of depressive symptoms was also significant in the bivariate analysis and the multivariable model building, but dropped out of the final model due to its correlations with poor physical function and sleep problems. These results suggest that resilience, physical function, and sleep problems may be especially important and modifiable factors related to PWB.
In terms of racial/ethnic disparities, blacks did not report significantly lower PWB compared with whites in either bivariate or multivariable analyses. A deeper look at our composite measure of PWB revealed that blacks scored significantly lower than whites on the Life Satisfaction measure, but not the Ryff or PANAS measures. We note that studies finding racial differences in SWB tend to focus on life satisfaction,52,53 thus suggesting that racial differences may vary by specific measure. Consistent with our findings, a study from the Women's Health Initiative did not find significant differences between whites and non-whites older than the age of 80 on the Ryff Personal Growth or Purpose in Life measures.54 We also found that Chinese women reported significantly lower PWB compared with white women, even after controlling for a range of variables. Although we are unable to find other studies that specifically compare Chinese women with white women on PWB. Cross-cultural research suggests that well-being is likely to have different meanings across cultures,55,56 but it is beyond the scope of this article to determine if the ethnic differences in SWAN are reflections of “real” differences in PWB or if they reflect cultural differences in response to these items.
We hypothesized that psychological resilience would moderate the relationship between health problems (poor self-assessed health, comorbidities, and sleep problems) and stressful life events and PWB. Results showed that resilience only moderated the relationship between sleep problems and PWB such that sleep problems at midlife had a greater negative impact on PWB among those women with low resilience. It is possible that resilience did not reduce the effect of stressful life events as this measure takes into account a person's perceptions of stressfulness and perhaps the same event is less likely to be rated as stressful among women with higher levels of resiliency. It is also possible that resilience did not moderate the relationships between comorbidities or physical function and PWB as the Connor-Davidson scale measures psychological resilience and may have less influence on physical measures. Nevertheless, results suggest that resilience may help reduce the negative impact of sleep problems on PWB.
We should also point out that resilience was measured only at visit 15, concurrently with PWB, and not at midlife, although there is some evidence that resilience as measured by the Connor- Davidson Resilience Scale is relatively stable.57 Taken together, our findings suggest that resilience may play an important role in PWB as women age. Although the research on interventions to increase resilience is sparse, there is some evidence that resilience can be increased among older adults58,59 and such interventions are worth investigating for middle-aged and older women.
The study has several limitations. Although results are based on a multiracial/ethnic cohort, some of these groups were too small to stratify results by race/ethnicity. Second, the analyses only include women who were still active in SWAN at visit 15. SWAN, like other cohort studies, has loss to follow-up and those women who dropped out before V15 were likely worse off in terms of physical and/or emotional health than those still participating. However, this bias is unlikely to impact the identification of factors related to better PWB. One should also interpret the results related to dispositional characteristics with caution, as there is some overlap between these concepts and PWB. Finally, we did not have a baseline measure of PWB and were thus unable to examine change in PWB from midlife to older age.
Important strengths of this study include the following: (1) the availability of multiple repeated standard measures of diverse psychosocial and health-related correlates of PWB and menopausal status; (2) the long follow-up period that allows for the evaluation of modifiable risk factors across the menopausal transition and midlife; and (3) a diverse sample with respect to race, ethnicity, and geography. This study adds to previous literature by highlighting the importance of healthy behaviors during midlife for better PWB at older ages. In addition, we found that Chinese women report significantly lower PWB compared with white women, even after controlling for a range of variables. However, it is unclear whether this is due to cultural biases in reporting well-being or actual well-being.
This study provides information for clinicians and women about midlife factors that are important for PWB in older age and are modifiable, including sleep behaviors and physical activity. Such factors can be addressed both in midlife and beyond to help women achieve successful aging. Results further suggest that interventions to increase optimism, spirituality, and resilience are worth exploring.
Supplementary Material
Acknowledgments
We thank the study staff at each site and all the women who participated in SWAN.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
The Study of Women's Health Across the Nation (SWAN) has grant support from the National Institutes of Health (NIH), DHHS, through the National Institute on Aging (NIA), the National Institute of Nursing Research (NINR), and the NIH Office of Research on Women's Health (ORWH) (Grants U01NR004061; U01AG012505, U01AG012535, U01AG012531, U01AG012539, U01AG012546, U01AG012553, U01AG012554, and U01AG012495). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NIA, NINR, ORWH, or the NIH.
Supplementary Material
References
- 1. Disabato DJ, Goodman FR, Kashdan TB, Short JL, Jarden A. Different types of well-being? A cross-cultural examination of hedonic and eudaimonic well-being. Psychol Assess 2016;28:471–482 [DOI] [PubMed] [Google Scholar]
- 2. Ryff CD, Keyes CL. The structure of psychological well-being revisited. J Pers Soc Psychol 1995;69:719–727 [DOI] [PubMed] [Google Scholar]
- 3. Diener E, Pressman SD, Hunter J, Delgadillo-Chase D. If, why, and when subjective well-being influences health, and future needed research. Appl Psychol Health Well Being 2017;9:133–167 [DOI] [PubMed] [Google Scholar]
- 4. Freedman VA, Carr D, Cornman JC, Lucas RE. Aging, mobility impairments and subjective wellbeing. Disabil Health J 2017;10:525–531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jivraj S, Nazroo J, Vanhoutte B, Chandola T. Aging and subjective well-being in later life. J Gerontol B Psychol Sci Soc Sci 2014;69:930–941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Woods NF, Cochrane BB, LaCroix AZ, et al. . Toward a positive aging phenotype for older women: Observations from the women's health initiative. J Gerontol A Biol Sci Med Sci 2012;67:1191–1196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Diener E. New findings and future directions for subjective well-being research. Am Psychol 2012;67:590–597 [DOI] [PubMed] [Google Scholar]
- 8. Ryff CD, Radler BT, Friedman EM. Persistent psychological well-being predicts improved self-rated health over 9–10 years: Longitudinal evidence from MIDUS. Health Psychol Open 2015;2:2055102915601582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Steptoe A, de Oliveira C, Demakakos P, Zaninotto P. Enjoyment of life and declining physical function at older ages: A longitudinal cohort study. CMAJ 2014;186:E150–E156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yanek LR, Kral BG, Moy TF, et al. . Effect of positive well-being on incidence of symptomatic coronary artery disease. Am J Cardiol 2013;112:1120–1125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. George LK. Still happy after all these years: Research frontiers on subjective well-being in later life. J Gerontol B Pychol Sci Soc Sci 2010;65b:331–339 [DOI] [PubMed] [Google Scholar]
- 12. Yang Y. Social inequalities in happiness in the United States, 1972 to 2004: An age-period-cohort analysis. Am Sociol Rev 2008;73:204–226 [Google Scholar]
- 13. Diener E. Subjective well-being. Psychol Bull 1984;95:542–575 [PubMed] [Google Scholar]
- 14. Lukaschek K, Vanajan A, Johar H, Weiland N, Ladwig KH. “In the mood for ageing”: Determinants of subjective well-being in older men and women of the population-based KORA-Age study. BMC Geriatr 2017;17:126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Connor KM, Davidson JR. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety 2003;18:76–82 [DOI] [PubMed] [Google Scholar]
- 16. Hildon Z, Montgomery SM, Blane D, Wiggins RD, Netuveli G. Examining resilience of quality of life in the face of health-related and psychosocial adversity at older ages: What is “right” about the way we age? Gerontologist 2010;50:36–47 [DOI] [PubMed] [Google Scholar]
- 17. Jeste DV, Savla GN, Thompson WK, et al. . Association between older age and more successful aging: Critical role of resilience and depression. Am J Psychiatry 2013;170:188–196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Olson EA, Fanning JT, Awick EA, Chung HD, McAuley E. Differential trajectories of well-being in older adult women: The role of optimism. Appl Psychol Health Well Being 2014;6:362–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Carver CS, Scheier MF, Segerstrom SC. Optimism. Clin Psychol Rev 2010;30:879–889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Brown L, Bryant C, Judd FK. Positive well-being during the menopausal transition: A systematic review. Climacteric 2015;18:456–469 [DOI] [PubMed] [Google Scholar]
- 21. Dennerstein L, Dudley E, Guthrie J, Barrett-Connor E. Life satisfaction, symptoms, and the menopausal transition. Medscape Womens Health 2000;5:E4. [PubMed] [Google Scholar]
- 22. Dennerstein L, Lehert P, Guthrie J. The effects of the menopausal transition and biopsychosocial factors on well-being. Arch Womens Ment Health 2002;5:15–22 [DOI] [PubMed] [Google Scholar]
- 23. Sowers M, Crawford S, Sternfeld B, et al. . Design, survey sampling and recruitment methods of SWAN: A multi-center, multi-ethnic, community-based cohort study of women and the menopausal transition. In: Lobo RA, Kelsay J, Marcus R, eds. Menopause: Biology and pathobiology. San Diego, CA: Academic Press, 2000:175–188 [Google Scholar]
- 24. Infurna FJ, Gerstorf D, Lachman ME. Midlife in the 2020s: Opportunities and challenges. Am Psychol 2020;75:470–485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess 1985;49:71–75 [DOI] [PubMed] [Google Scholar]
- 26. Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J Pers Soc Psychol 1988;54:1063–1070 [DOI] [PubMed] [Google Scholar]
- 27. Herbers PM, Elder DA, Woo JG. Area under a curve: Calculation and visualization. 2011. Report No: DG12-2011. 2011
- 28. Ware J. The SF-36 health survey manual and interpretation guide. New England Medical Center, Boston: The Health Institute, 1993 [Google Scholar]
- 29. Avis NE, Colvin A, Bromberger JT, et al. . Change in health-related quality of life over the menopausal transition in a multiethnic cohort of middle-aged women: Study of Women's Health Across the Nation. Menopause 2009;16:860–869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sommer B, Avis N, Meyer P, et al. . Attitudes toward menopause and aging across ethnic/racial groups. Psychosom Med 1999;61:868–875 [DOI] [PubMed] [Google Scholar]
- 31. Avis NE, Brambilla D, McKinlay SM, Vass K. A longitudinal analysis of the association between menopause and depression. Results from the Massachusetts Women's Health Study. Ann Epidemiol 1994;4:214–220 [DOI] [PubMed] [Google Scholar]
- 32. Sternfeld B, Ainsworth BE, Quesenberry CP. Physical activity patterns in a diverse population of women. Prev Med 1999;28:313–323 [DOI] [PubMed] [Google Scholar]
- 33. Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr 1982;36:936–942 [DOI] [PubMed] [Google Scholar]
- 34. Barefoot J, Dodge K, Peterson B, et al. . The Cooke-Medley Hostility Scale: Item content and ability to predict survival. Psychosom Med 1989;51:46–57 [DOI] [PubMed] [Google Scholar]
- 35. Scheier MF, Carver CS. Optimism, coping, and health: Assessment and implications of generalized outcome expectancies. Health Psychol 1985;4:219–247 [DOI] [PubMed] [Google Scholar]
- 36. Spielberger CD, Gorsuch RL, Lushene RE. STAI manual for the Stait-Trait Anxiety Inventory (“self-evaluation questionnaire”). Palo Alto, CA: Consulting Psychologists Press, 1970 [Google Scholar]
- 37. Underwood LG, Teresi JA. The daily spiritual experience scale: Development, theoretical description, reliability, exploratory factor analysis, and preliminary construct validity using health-related data. Ann Behav Med 2002;24:22–33 [DOI] [PubMed] [Google Scholar]
- 38. Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas 1977;1:385–401 [Google Scholar]
- 39. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983;24:385–396 [PubMed] [Google Scholar]
- 40. Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med 1991;32:705–714 [DOI] [PubMed] [Google Scholar]
- 41. Giroir BP, Wright D. Physical activity guidelines for health and prosperity in the United States. JAMA 2018;320:1971–1972 [DOI] [PubMed] [Google Scholar]
- 42. Kim ES, Kubzansky LD, Soo J, Boehm JK. Maintaining healthy behavior: A prospective study of psychological well-being and physical activity. Ann Behav Med 2017;51:337–347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Rector JL, Christ SL, Friedman EM. Well-being and long-term physical activity participation in midlife adults: A latent class analysis. Ann Behav Med 2019;53:53–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Adams MA, Hurley JC, Todd M, et al. . Erratum to: Adaptive goal setting and financial incentives: A 2 × 2 factorial randomized controlled trial to increase adults' physical activity. BMC Public Health 2017;17:303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Institute of Medicine. Leading health indicators for healthy people 2020: letter report. Washington, DC: The National Academies Press, 2011 [PubMed] [Google Scholar]
- 46. Ong AD, Kim S, Young S, Steptoe A. Positive affect and sleep: A systematic review. Sleep Med Rev 2017;35:21–32 [DOI] [PubMed] [Google Scholar]
- 47. Stone KL, Xiao Q. Impact of poor sleep on physical and mental health in older women. Sleep Med Clin 2018;13:457–465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Moline ML, Broch L, Zak R, Gross V. Sleep in women across the life cycle from adulthood through menopause. Sleep Med Rev 2003;7:155–177 [DOI] [PubMed] [Google Scholar]
- 49. Germain A, Richardson R, Moul DE, et al. . Placebo-controlled comparison of prazosin and cognitive-behavioral treatments for sleep disturbances in US Military Veterans. J Psychosom Res 2012;72:89–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Guthrie KA, Larson JC, Ensrud KE, et al. . Effects of pharmacologic and nonpharmacologic interventions on insomnia symptoms and self-reported sleep quality in women with hot flashes: A pooled analysis of individual participant data from four MsFLASH Trials. Sleep 2018;41:zsx190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Bauereiβ N, Obermaier S, Ozunal SE, Baumeister H. Effects of existential interventions on spiritual, psychological, and physical well-being in adult patients with cancer: Systematic review and meta-analysis of randomized controlled trials. Psychooncology 2018;27:2531–2545 [DOI] [PubMed] [Google Scholar]
- 52. Barger SD, Donoho CJ, Wayment HA. The relative contributions of race/ethnicity, socioeconomic status, health, and social relationships to life satisfaction in the United States. Qual Life Res 2009;18:179–189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Thomas M, Hughes M. The continuing significance of race: A study of race, class, and quality of life in America, 1972–1985. Am Sociol Rev 1986;51:830–841 [PubMed] [Google Scholar]
- 54. Woods NF, Rillamas-Sun E, Cochrane BB, et al. . Aging well: Observations from the women's health initiative study. J Gerontol A Biol Sci Med Sci 2016;71 Suppl 1(Suppl 1):S3–S12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Diener E, Lucas RE, Oishi S. Advances and open questions in the science of subjective well-being. Collabra Psychol 2018;4:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Karasawa M, Curhan KB, Markus HR, et al. . Cultural perspectives on aging and well-being: A comparison of Japan and the United States. Int J Aging Hum Dev 2011;73:73–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Edwards KA, Alschuler KA, Ehde DM, Battalio SL, Jensen MP. Changes in resilience predict function in adults with physical disabilities: A longitudinal study. Arch Phys Med Rehabil 2017;98:329–336 [DOI] [PubMed] [Google Scholar]
- 58. Perez-Blasco J, Sales A, Meléndez JC, Mayordomo T. The effects of mindfulness and self-compassion on improving the capacity to adapt to stress situations in elderly people living in the community. Clin Gerontol 2016;39:90–103 [Google Scholar]
- 59. Cheavens JS, Cukrowicz KC, Hansen R, Mitchell SM. Incorporating resilience factors into the interpersonal theory of suicide: The role of hope and self-forgiveness in an older adult sample. J Clin Psychol 2016;72:58–69 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.