Abstract
Objective
To describe a new method which involves anatomical distal clavicle plate fixation and titanium alloy cable system‐augmented coracoclavicular ligament reconstruction to manage Neer type IIb distal clavicle fracture.
Methods
Between January 2013 and June 2018, 28 patients with acute Neer type IIb lateral clavicle fracture were treated by a new method – precontoured locking compressive distal clavicular plate fixation of the fracture combined with titanium alloy cable system‐augmented reconstruction of the coracoclavicular ligament. There were 11 females and 17 males treated in this way. There were 15 cases of the right side and 13 of the left. The mean age of the patients was 48.5 years (range, 18–78 years). The mean time from injury to surgery was 3.9 days (range, 1–7 days). After completing the preoperative examinations and evaluations, surgeries were performed for all these patients, anatomical distal clavicle plates were used for fractures, and titanium alloy cables were implanted for the augmented reconstruction of coracoclavicular ligaments. Postoperative protocols, including arm sling management and rehabilitative activities, were unified and recommended to all the patients. These patients were followed up for at least 1 year. The mean duration of postoperative follow‐up was 23.3 months (range, 12–52 months). At the last follow‐up, the coracoclavicular distances were recorded and shoulder functional outcomes were assessed by the Constant scores and the Fudan University Shoulder Scores (FUSSs) questionnaires.
Results
Radiographic bony unions were achieved in all patients within 20 weeks. Functional and radiographic outcomes were retrospectively evaluated. The mean coracoclavicular distance was 9.61 ± 0.61 mm on the injured side vs 9.62 ± 0.57 mm on the contralateral uninjured side. The mean Constant score and mean FUSS were 90.1 ± 6.6 (range, 68–98) and 86.1 ± 7.2 (range, 64–95) respectively, which indicating good restoration of function and high level of satisfaction for both the patients and their physical therapists. There were a few major complications, including one delayed healing of the skin, one severe shoulder stiffness, three incidences of moderate shoulder stiffness, and five incidences of symptomatic hardware. There is no deep infections, neurovascular injuried, delayed union or nonunion, peri‐implant fracture, loss of reduction, implant malposition or failure, or other severe complications.
Conclusion
This combined method for the treatment of Neer type IIb distal clavicle fracture could yield high bony union rate, good functional outcome, and low complication rate. Further prospective randomized controlled studies are needed to confirm the benefits of this method of treatment.
Keywords: clavicle, ligament, fracture, rupture, orthopeadic procedure
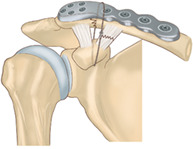
A drawing of surgical fixation of Neer type IIb distal clavicle fractures using anatomical locking plate fixation combined with titanium alloy cable for augmented reconstruction of coracoclavicular ligament.
Introduction
Fractures of the distal end of clavicle are very common in clinical practices, and account for 21%–28% of all clavicle fractures 1 . According to Banerjee et al., nonunion rates following nonsurgical management of type II distal clavicle fractures range from 28% to 44% 2 , 3 . Moreover many of these patients, especially those with Neer type IIb fractures, are symptomatic and will eventually require surgical fixation 2 , 3 . However, the surgical management of Neer type IIb distal clavicle fracture remains controversial, there is no consensus on the optimal surgical procedure for treating this problem.
Various internal fixation materials have been used for the treatment of these factures. However, there are many complications and concerns related to some previously reported and currently used methods. For K‐wires, K‐wire breakage and inward migration of the broken wire can cause serious complications in addition to treatment failure 3 . For hook plate, which used to be widely accepted as a proper implant hardware for dislocation of acromioclavicular joint and distal clavicle fracture, may bring some annoying complications, such as rotator cuff injury, acromioclavicular joint osteoarthritis, acromial fracture and hook cutout, and clavicle fracture at the medial end of the plate, which usually required a secondary surgery to remove the implanted hardware within a short period or even a secondary revision operation 4 , 5 , 6 , 7 , 8 , 9 . While titanium alloy cable or orthocord suture might cure most of the fractures, they could leave some deformities and complications due to not anatomically reducing the fracture and the long‐term cutting effect of the materials 10 , 11 . For distal clavicular plate alone, patients might face the potential risks of the screw detachment and plate back‐out, which can lead to loss of reduction, malunion or non‐union, etc., which can eventually result in the failure of the treatment. Brouwer et al. reported a series of patients who suffered this complication and other groups of authors also reported relative cases with this method; however, there were no exact statistical figures about the percentage of failures, and the failure rates ranged from 2.2% (1/46) to 6.3% (1/16) according to some studies 12 , 13 , 14 , 15 . Thus, not any of the methods mentioned above could be appreciated as a standard protocol for this type of injury and many scholars are still trying to figure out some better methods.
A cadaveric biomechanical study by Rieser et al. showed that stability of the fractured clavicle was greater with a combination of distal clavicle fixation and coracoclavicular ligament reconstruction than with either measure alone, implying that fracture‐healing rates would be better with the combined treatment 16 . Madsen et al. also concluded that coracoclavicular fixation adds stability to type IIB distal clavicle fractures fixed with plate and screws when the laters used alone might be overloaded to failure 17 . This has also been confirmed in many clinical studies. Tiefenboeck et al. considered that vertical stability cannot be sufficiently achieved with plate fixation alone 18 . Seyhan et al. concluded that anatomic locking plate and coracoclavicular stabilization with suture endo‐button technique provided more stable and biomechanically superior fixation among other techniques with low complication rates in the treatment of Neer Type IIb fractures 19 .
Several scholars have used the combination of anatomical locking plate fixation of the bone and suture anchor or suture endo‐button augmented reconstruction of the coracoclavicular ligament for treatment of Neer type IIb distal clavicle fractures and reported satisfactory clinical outcomes 17 , 19 , 20 . During this period, we developed an analogic technique in which we perform augmented reconstruction of the coracoclavicular ligament, using a titanium alloy cable system instead of suture anchors or suture endo‐buttons, and fixation of the distal clavicle using a precontoured locking compressive distal clavicular plate.
In this study, we retrospectively analyzed the clinical outcomes of patients who were treated with this method in our department. The purpose of this study was to investigate the following concerns. First, evaluate the efficacy of the method to treat this injury. Second, record the complications and analyze the underlying reasons why these patients should be treated using this method. Third, assess the short‐term and long‐term safety for patients living with the implanted materials after surgery by this method.
Materials and Methods
Inclusion and Exclusion Criteria
Study Design
This retrospective clinical trial was conducted at the Department of Orthopedic Surgery in Shanghai Changzheng Hospital from January 2013 to June 2018. It was approved by the ethics committee of our hospital and informed consent was obtained from all the patients.
Inclusion Criteria
The inclusion criteria were: (i) patients aged older than 18 years, diagnosed with Neer type IIb distal clavicle fracture according to Neer classification; (ii) precontoured locking compressive distal clavicular plate fixation and augmented reconstruction of the coracoclavicular ligament with a titanium alloy cable system; (iii) the patients were willing to participate after giving written informed consent; and (vi) complete clinical data of the patient was obtained.
Exclusion Criteria
Patients with the following circumstances were excluded: (i) time from injury to surgery more than 2 weeks; (ii) open or pathologic distal clavicle fractures; (iii) fracture with neurovascular damage; (iv) patient who suffers multiple trauma, including distal clavicle fracture, which might affect the postoperative rehabilitation program;and (v) followed for less than12 months.
Patients
According to the inclusion and exclusion criteria, the study population comprised 28 consecutive patients with Neer type IIb distal clavicle fracture who were treated in our department with precontoured locking compressive distal clavicular plate fixation and augmented reconstruction of the coracoclavicular ligament with a titanium alloy cable system between January 2013 and June 2018. All patients had closed fractures without neurovascular damage.
Operative Technique
Anesthesia and Position
Regional block combined with general anesthesia was applied. The patient was placed in the beach‐chair position on a radiolucent table.
Approach and Exposure
A curved incision was made over the fracture site, along the superior aspect of the lateral half of the clavicle and the acromion. The platysma, deltoid, and trapezius were elevated with an electric scalpel, and the fracture pattern and the ruptured coracoclavicular ligament were explored.
Reduce and Fix the Fracture
Blood clots and any soft tissue interposed between the fracture ends were removed, and the fractured clavicle was meticulously reduced and temporarily fixed with one or two (or more if necessary) K‐wires passed through the acromion into the proximal fragment. A precontoured locking compressive distal clavicular plate of suitable size was placed over the lateral clavicle, bridging the fractured fragments. Under direct visualization and fluoroscopic control, the plate was fixed with three to four cortical locking screws on the medial end and four to eight smaller cancellous locking screws on the lateral end. Care was taken to ensure that the screws did not penetrate into the acromioclavicular joint.
Augmented Reconstruction of the Ligament
The coracoid process was approached by blunt dissection through the overlying muscles. A strand of titanium alloy cable (or cables) was conducted beneath the base of coracoid process and over the plate using right‐angle forceps and then fastened with tools provided with the system so that the distance between the clavicle and the coracoid process was the same as that on the unaffected side in anteroposterior fluoroscopic view (Fig. 1). The ruptured coracoclavicular ligament was then explored and repaired without tension. The integrity of the coracoclavicular ligament was restored by regular repair after it was augmentedly protected with a titanium alloy cable system (with single or double head).
Fig. 1.
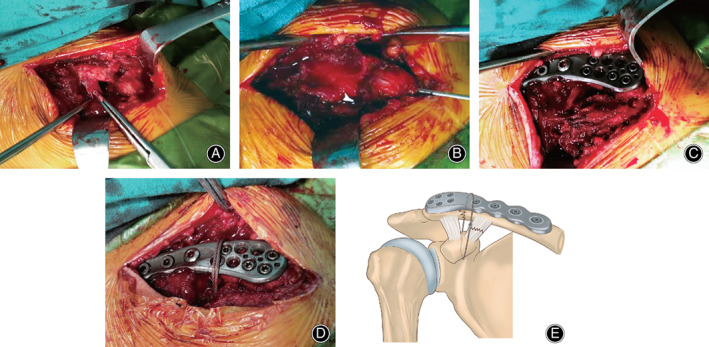
Intraoperative photographs and drawing of anatomical distal clavicle plate fixation and augmented coracoclavicular ligament reconstruction to manage Neer type IIb distal clavicle fracture. (A) Intraoperative exploration shows the fractured lateral clavicle and the ruptured coracoclavicular ligament. (B) The fractured lateral clavicle was temporarily fixed with one K‐wire passed through acromion into the proximal fragment. (C) A suitable precontoured locking compressive distal clavicular plate was placed over the lateral clavicle bridging the fractured fragments. (D) The distal clavicle fracture was fixed with the combination of the anatomical distal clavicle plate and the cable system. (E) A drawing of surgical fixation of Neer type IIb distal clavicle fractures using anatomical locking plate fixation combined with titanium alloy cable for augmented reconstruction of coracoclavicular ligament.
The wound was irrigated and closed in layers.
Postoperative Management
Postoperatively, an arm sling was routinely used for 2 weeks until the wound had healed completely. Active exercise of hands and forearms was encouraged immediately after surgery. Passive exercise of the shoulder was started after pain had subsided. Active shoulder movement was begun 2 weeks after surgery (after the arm sling was removed) and continued till normal range of motion was achieved.
Follow‐Up Methods
Patients were followed up in the outpatient clinic at 2 weeks, 6 weeks, and 12 weeks after the surgery. Radiographs were obtained to examine the bony union and to compare the coracoclavicular distance on both two sides. Physical and mental rehabilitative status was evaluated, and any complications were recorded. After this initial period, patients were followed up every 3 months (or every 1 month till bony union) for at least 1 year after operation. At the last follow‐up, the coracoclavicular distances were recorded and shoulder functional outcomes were assessed by the Constant scores 21 and the Fudan University Shoulder Scores (FUSSs) questionnaires 22 (Fig. 2). Informed consent was obtained from all individual participants included in the study.
Fig. 2.
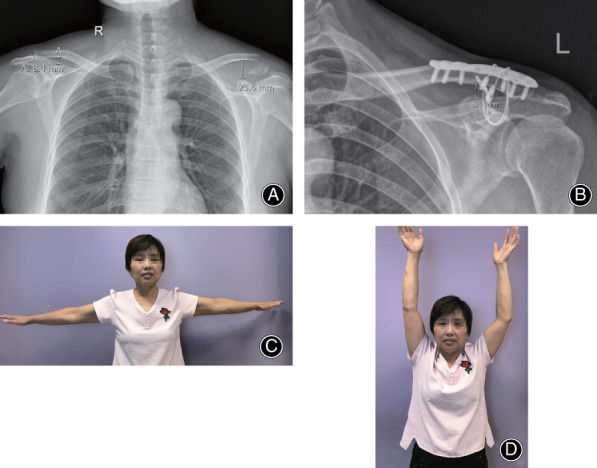
Postoperative radiographs of a 46‐year‐old woman 28 months after surgical repair of Neer type IIb distal clavicle fracture; the injury was on the left side. (A) Anteroposterior radiograph of the chest showing the coracoclavicular distance on both sides. (B) The patient has achieved radiographic bony union; the coracoclavicular distance on the injured side is 8.4 mm. (C) The involved shoulder joint had the same range of motion as the contralateral in abduction function. (D) The involved shoulder joint had a nearly normal range of motion as the contralateral in lift function.
Outcome Evaluation
Bony Union Rates
A parameter used to reveal the fracture healing status of all the patients in a group is a very important indicator for the success of the treatment and premise for the implementation of individual rehabilitative protocol. Bony union status is mainly evaluated by the radiograph.
Coracoclavicular Distances
Coracoclavicular distance is the shortest distance between clavicle and coracoid process in an anteroposterior X‐ray photograph. The distances are measured for both the injured side and the contralateral side of the same patient in one radiograph. A normal coracoclavicular distance means well‐reduced fracture and well‐repaired ligament.
Constant Score
A method of functional assessment of the shoulder, which includes individual parameters like pain, activities of daily living, range of motion, and power, could provide an overall clinical functional assessment. It is accurately reproducible by different observers and is sufficiently sensitive to reveal even small changes in function.
Fudan University Shoulder Scores (FUSSs)
A shoulder scoring system based on patients' and physicians' points of view, which includes a two‐dimensional visual analog scale, night pain subscale, and patient–physician satisfaction scale, combined with several functional parameters, could reveal the patients’ condition both physically and emotionally.
Statistical Methods
Statistical analysis was performed with IBM SPSS 21.0 statistical software (IBM SPSS, Inc., Chicago, IL, US). Coracoclavicular distances, total scores of both Constant scores and Fudan University Shoulder Scores (FUSSs) were presented as mean standard deviations. Student t‐test and ANOVA were used to compare numeral data. Statistical significance was defined as 0.05, and a P‐value <0.05 was taken to indicate a statistically significant difference.
Results
Epidemiological Results
A total of 28 consecutive patients (11 females, 17 males) were included in this study. There were 15 cases of the right side and 13 of the left. The mean age of the patients was 48.5 years (range, 18–78 years). The mean time from injury to surgery was 3.9 days (range, 1–7 days).The mean duration of postoperative follow‐up was 23.3 months (range, 12–52 months).
Operation Condition
The average operation time was 66.1 ± 10.2 min (range, 50–90 min), blood loss was 50.4 ± 20.8 mL (range, 25–100 mL), and there was no blood transfusion for any patient in this group. There was no injury of great vessels or nerves occurring during the operation, and also no death.
Bony Union Rates
All these 28 patients treated by this method achieved bony reunion within 20 weeks. This allowed all the patients to participate in their own rehabilitative protocols at early stage and also prevented the patients receiving a secondary or multiple revision surgery for the fracture.
Coracoclavicular Distances
The mean preoperational coracoclavicular distance of the injured side was 20.58 ± 1.58 mm while the last follow‐up coracoclavicular distance on the same side was 9.61 ± 0.61 mm, P < 0.01(P = 0.000), indicating there is significant difference between these two time points of the injured side. The mean coracoclavicular distance was 9.61 ± 0.61 mm on the injured side vs 9.62 ± 0.57 mm on the contralateral uninjured side at last follow‐up. The P = 0.525, indicating there is no statistical difference between the two sides.
Constant Score
The mean Constant scores were 72.3 ± 8.3 (range, 54–90), 85.8 ± 7.5 (range, 65–98), and 90.1 ± 6.6 (range, 68–98) at 6 weeks, 12 weeks, and final follow‐up time points after surgeries, respectively. P < 0.01 (P = 0.000), indicating there is significant difference of shoulder function of the injured sides between these three different postoperative time points. Due to both mental and physical disabilities of the post traumatic state of patients, there is no preoperative data available for the comparison.
Fudan University Shoulder Scores
The mean Fudan University Shoulder Scores were 69.4 ± 9.2 (range, 50–88), 82.2 ± 7.9 (range, 60–94). and 86.1 ± 7.2 (range, 64–95) at 6 weeks, 12 weeks, and final follow‐up time points after surgeries, respectively. P<0.01 (P = 0.000), indicating there is significant difference of shoulder function of the injured sides between these three different postoperative time points. Paresthesia around the incision and decreased strength of the injured shoulder are universally presented in various extents in this group of patients, which could be the main reason for decreased functional scores of injured shoulders.
Postoperative Complications
One patient had delayed healing of the skin wound, but it healed eventually with regular dressing changes for 1 month. Three patients suffered moderate shoulder stiffness and one patient had severe stiffness at the last follow‐up point, which might have been due to corresponding degrees of pain resulted from irregular follow‐ups and lack of timely physical treatments and appropriate intervention. Five patients reported symptomatic hardware, added with 11 patients' concern about the implanted hardware in the future (even though there were no clinical symptoms or imaging abnormalities). All these 16 patients experienced a second surgery to remove the hardware, and they were all greatly relieved in both physical and mental aspects after the second surgery and exhibited elevated functional scores in various degrees. Paresthesia and decreased strength have been mentioned above. There is no deep infection, neurovascular injury, delayed union or nonunion, peri‐implant fracture, loss of reduction, implant malposition or failure, or other major complication.
Discussion
Neer type IIb distal clavicle fracture refers to injury in which there is a clavicle fracture between the trapezoid ligament and the conoid ligament, with rupture of the latter but sparing of the former 2 . Due to the high rate of nonunion of this fracture type, primary surgical management is generally recommended 2 , 3 , 23 , 24 . Neer recommended K‐wire fixation. However, K‐wire breakage and inward migration of the broken wire can cause serious complications 3 . Not long ago we had a female patient with a broken transacromial K‐wire that had migrated close to the cervical spine; serious damage might have resulted if she had not sought treatment in time. Webber and Haines used Dacron arterial graft, with or without a lag screw, to treat a group of patients with displaced Neer type II fractures of the lateral clavicle. Erosion around the graft loop and difficulty in screw fixation in the narrow area beneath the coracoid were reported to be the main problems with this technique 23 .
In the past decade, open reduction and fixation with the hook plate was widely considered an acceptable treatment 4 , 5 , 6 , 7 , 8 , 9 . However, the hook plate was later found to be associated with several complications, including rotator cuff injury, shoulder stiffness, acromioclavicular joint osteoarthritis, acromial fracture and hook cutout, and clavicle fracture at the medial end of the plate. These problems often necessitated a second operation for removal of the hook plate 25 .
Kalamaras et al. treated a group of unstable distal clavicle fractures with open reduction and internal fixation using titanium distal radial locking plates and reported promising results 26 . Martetschlager et al. experimented with the use of distal radial locking plates; they found that the use of locking T‐plate and cerclage can provide good and reliable outcomes in unstable distal clavicle fractures 27 . However, as the name implies, the distal radial locking plate is designed for the distal radius, and its configuration does not match the anatomy of the distal clavicle. Specifically, the distal end of the broken clavicle does not provide sufficient space for locking screw fixation, while the proximal end does not fit well with the plate. This results in problems such as insufficient fixation, failure of internal fixation, subcutaneous prominence of the metal implantation, and so on.
The precontoured locking compressive distal clavicular plate was developed recently for the treatment of distal clavicular fractures and has been widely used in clinical practice. Lee et al. and Kapil‐Mani et al. have demonstrated the feasibility and efficacy of precontoured locking compressive distal clavicular plate fixation for treatment of displaced fractures of the distal end of the clavicle 12 , 28 . This newly developed plate has some obvious favorable characteristics. First, the broad distal end has multiple locking screw holes that offer multidirectional – and therefore stronger – fixation. Second, the plate can be used for bridging two or more parts of the fracture as it is precontoured to match the shape of the distal clavicle.
Some scholars attempted another approach for the treatment of these fractures. Instead of reducing and fixing the fracture, they focused on restoring the function of the coracoclavicular ligaments using different techniques. They believed that restoration of the normal coracoclavicular distance would be sufficient for promoting fracture healing. Li et al. used titanium cable in a minimally invasive technique 10 . Kenyon et al. used an orthocord suture and two flip tacks to reconstruct the coracoclavicular ligaments via a minimally invasive approach 11 . Both groups reported favorable outcomes.
None of the methods mentioned above gained wide acceptance, and researchers have been continuing to try and find better ways to treat this injury. Rieser et al. and Madsen et al. compared the different treatments and concluded that greater fracture stability was achieved with the combination of the two methods – reconstruction of the coracoclavicular ligament plus fixation of the distal clavicle – than with either method alone 16 , 17 . This has been confirmed in other studies 17 , 19 , 20 , and also in our own clinical practice. In our department we often encounter patients with Neer type IIb distal clavicle fracture who have undergone unsuccessful surgical treatment, some with anatomical distal clavicle compressive plate alone and some with only reconstruction of the coracoclavicular ligament function.
Brouwer et al. reported a group of patients treated with locking clavicle plate, all of whom had failure due to axial pullout of the locking screws from the lateral clavicular fragment 15 . Their study demonstrated that the strong pull exerted by the trapezius muscle could hinder bony reunion. We therefore decided to combine anatomical reduction and fixation of the fractured fragments with some measure to counter the pull of the trapezius muscle. For the former we decided to use the precontoured locking compressive distal clavicular plate and for the latter we chose the titanium alloy cable system, which is widely used in the treatment of injuries such as acromioclavicular joint dislocation, patella or olecranon fracture, distal clavicle fracture, and so on 10 , 29 , 30 . The cable system consists of a strand of titanium alloy cable and its matched fixation system. The diameter of cable is 1.0 mm. Due to the physical properties of titanium alloy, the cable possesses both good strength and elasticity. However, since it is rigid and serves as a foreign body to human beings, there are some potential specific complications of using this cable. Irritation, or even penetration can be seen if not well situated and/or covered the suap‐close of the cable. Breakage resulting from long‐term and/or intensive activities of the shoulder could also be observed. Allergy, infection, and other complications of other implant materials might be concerns as well. The titanium alloy cable system would help restrict the coracoclavicular distance within the normal range, while its elasticity would allow the subtle motion of the acromioclavicular joint. We believe that this combined approach was responsible for the success achieved in all patients. An additional advantage with this method is that there is no need to remove the plates and cable(s) by a secondary surgery except for those patients with persistent concern about the hardware in the long term.
In this study, we are not intending to introduce this method as superior or the best option for this group of injured patients; however, we would like to consider it as a practical solution in our current healthcare environment. As mentioned in the context above, many other papers reported several tools and methods for this injury, which brought good outcomes as well as some complications; however, some complications such as bone ununion and reoperation may not be well accepted in our country. As the conflicts between healthcare providers and patients escalate in China, surgeons need to give priority to some key points like bone union rates, reoperation rates, etc. Hence, we choose this safer, assured method as our preferred option.
According to the results stated above, the almost identical pre‐ and postoperative mean coracoclavicular distances mean we can both well reduce the distal clavicle fracture and restore the function of coracoclavicular ligament at the same time, with the Constant scores and Fudan University Shoulder Scores (FUSSs) indicating good restoration of function and high level of satisfaction for the treatment. There were a few complications mainly related to functional recovery, which might be ascribed to the imperfect medical system of our nation, in which the surgeons and physical therapists are mostly working independently due to heavy workload and imperfect treatment system at some large medical centers, as well as the heavy healthcare burdens for some patients or some people responsible for the patients. In the near future, we believe this could be promoted as the nation's health care reform advanced.
Limitation
Obviously there are some limitations of our study. First of all, this is not a control study which includes control group or other method groups. Second, this method is more complicated and more expensive than any other methods using only one kind of implant material, which may not well‐appreciated in many circumstances. In the future, we will keep exploring superior implant materials and more delicate procedures, and we could compare and share our data with other treatment teams or centers of this injury type to justify a better procedure that can benefit more patients.
Conclusion
The patients with acute Neer type IIb lateral clavicle fracture treated by precontoured locking compressive distal clavicular plate fixation of the fracture combined with titanium alloy cable system augmented reconstruction of the coracoclavicular ligament can achieve bony reunion and restoration of shoulder functions. There were few complications mainly related with functional recovery. We believe that this technique will find wide acceptance as a reliable method for the treatment of Neer type IIb distal clavicle fracture.
References
- 1. Khan LA, Bradnock TJ, Scott C, Robinson CM. Fractures of the clavicle. J Bone Joint Surg Am, 2009, 91: 447–460. [DOI] [PubMed] [Google Scholar]
- 2. Banerjee R, Waterman B, Padalecki J, Robertson W. Management of distal clavicle fractures. J Am Acad Orthop Surg, 2011, 19: 392–401. [DOI] [PubMed] [Google Scholar]
- 3. Neer CS 2nd. Fractures of the distal third of the clavicle. Clin Orthop Relat Res, 1968, 58: 43–50. [PubMed] [Google Scholar]
- 4. Kirsch JM, Blum L, Hake ME. Distal clavicle fractures: open reduction and internal fixation with a hook plate. J Orthop Trauma, 2018, 32: S2–S3. [DOI] [PubMed] [Google Scholar]
- 5. Sukur E, Ozturkmen Y, Akman YE, Gungor M. Clinical and radiological results on the fixation of Neer type 2 distal clavicle fractures with a hook plate. Acta Orthop Traumatol Turc, 2016, 50: 489–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Good DW, Lui DF, Leonard M, Morris S, McElwain JP. Clavicle hook plate fixation for displaced lateral‐third clavicle fractures (Neer type II): a functional outcome study. J Shoulder Elbow Surg, 2012, 21: 1045–1048. [DOI] [PubMed] [Google Scholar]
- 7. Tiren D, van Bemmel AJ, Swank DJ, van der Linden FM. Hook plate fixation of acute displaced lateral clavicle fractures: mid‐term results and a brief literature overview. J Orthop Surg Res, 2012, 7: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Haidar SG, Krishnan KM, Deshmukh SC. Hook plate fixation for type II fractures of the lateral end of the clavicle. J Shoulder Elbow Surg, 2006, 15: 419–423. [DOI] [PubMed] [Google Scholar]
- 9. Flinkkila T, Ristiniemi J, Lakovaara M, Hyvonen P, Leppilahti J. Hook‐plate fixation of unstable lateral clavicle fractures: a report on 63 patients. Acta Orthop, 2006, 77: 644–649. [DOI] [PubMed] [Google Scholar]
- 10. Li Y, Shi S, Ou‐Yang YP, Liu TL. Minimally invasive treatment for Neer IIb distal clavicle fractures with titanium cable. J Trauma, 2011, 71: E37–E40. [DOI] [PubMed] [Google Scholar]
- 11. Kenyon P, Morgan BW, Webb M, Ebreo D, Wheelton A, Ravenscroft MJ. Open reduction and fixation of displaced lateral clavicle fractures using the minimally invasive acromioclavicular joint reconstruction (MINAR(R)) technique: a case series review. Shoulder Elbow, 2015, 7: 13–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. KC K‐M, P A, S A. Precontoured clavicular locking plate with broad lateral end: a newly designed plate for lateral third clavicle fractures. Malays Orthop J, 2018, 12: 15–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Xu H, Chen WJ, Zhi XC, Chen SC. Comparison of the efficacy of a distal clavicular locking plate with and without a suture anchor in the treatment of Neer IIb distal clavicle fractures. BMC Musculoskelet Disord, 2019, 20: 503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Vaishya R, Vijay V, Khanna V. Outcome of distal end clavicle fractures treated with locking plates. Chin J Traumatol, 2017, 20: 45–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Brouwer KM, Wright TC, Ring DC. Failure of superior locking clavicle plate by axial pull‐out of the lateral screws: a report of four cases. J Shoulder Elbow Surg, 2009, 18: e22–e25. [DOI] [PubMed] [Google Scholar]
- 16. Rieser GR, Edwards K, Gould GC, Markert RJ, Goswami T, Rubino LJ. Distal‐third clavicle fracture fixation: a biomechanical evaluation of fixation. J Shoulder Elbow Surg, 2013, 22: 848–855. [DOI] [PubMed] [Google Scholar]
- 17. Madsen W, Yaseen Z, LaFrance R, et al. Addition of a suture anchor for coracoclavicular fixation to a superior locking plate improves stability of type IIB distal clavicle fractures. Arthroscopy, 2013, 29: 998–1004. [DOI] [PubMed] [Google Scholar]
- 18. Tiefenboeck TM, Boesmueller S, Binder H, et al. Displaced Neer Type IIB distal‐third clavicle fractures‐long‐term clinical outcome after plate fixation and additional screw augmentation for coracoclavicular instability. BMC Musculoskelet Disord, 2017, 18: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Seyhan M, Kocaoglu B, Kiyak G, Gereli A, Turkmen M. Anatomic locking plate and coracoclavicular stabilization with suture endo‐button technique is superior in the treatment of Neer Type II distal clavicle fractures. Eur J Orthop Surg Traumatol, 2015, 25: 827–832. [DOI] [PubMed] [Google Scholar]
- 20. Han L, Hu Y, Quan R, Fang W, Jin B, Huang L. Treatment of Neer IIb distal clavicle fractures using anatomical locked plate fixation with coracoclavicular ligament augmentation. J Hand Surg, 2017, 42: 1036 e1–e6. [DOI] [PubMed] [Google Scholar]
- 21. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res, 1987, 214: 160–164. [PubMed] [Google Scholar]
- 22. Ge Y, Chen S, Chen J, Hua Y, Li Y. The development and evaluation of a new shoulder scoring system based on the view of patients and physicians: the Fudan University shoulder score. Art Ther, 2013, 29: 613–622. [DOI] [PubMed] [Google Scholar]
- 23. Webber MCB, Haines JF. The treatment of lateral clavicle fractures. Injury, 2000, 31: 175–179. [DOI] [PubMed] [Google Scholar]
- 24. Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br, 1998, 80: 476–484. [DOI] [PubMed] [Google Scholar]
- 25. Lopiz Y, Checa P, Garcia‐Fernandez C, Valle J, Vega ML, Marco F. Complications with the clavicle hook plate after fixation of Neer type II clavicle fractures. Int Orthop, 2019, 43(7): 1701–1708. [DOI] [PubMed] [Google Scholar]
- 26. Kalamaras M, Cutbush K, Robinson M. A method for internal fixation of unstable distal clavicle fractures: early observations using a new technique. J Shoulder Elbow Surg, 2008, 17: 60–62. [DOI] [PubMed] [Google Scholar]
- 27. Martetschlager F, Kraus TM, Schiele CS, et al. Treatment for unstable distal clavicle fractures (Neer 2) with locking T‐plate and additional PDS cerclage. Knee Surg Sports Traumatol Arthrosc, 2013, 21: 1189–1194. [DOI] [PubMed] [Google Scholar]
- 28. Lee SK, Lee JW, Song DG, Choy WS. Precontoured locking plate fixation for displaced lateral clavicle fractures. Orthopedics, 2013, 36: 801–807. [DOI] [PubMed] [Google Scholar]
- 29. Gao YS, Zhang YL, Ai ZS, Sun YQ, Zhang CQ, Zhang W. Transarticular fixation by hook plate versus coracoclavicular stabilization by single multistrand titanium cable for acute Rockwood grade‐V acromioclavicular joint dislocation: a case‐control study. BMC Musculoskelet Disord, 2015, 16: 360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Huang SL, Xue JL, Gao ZQ, Lan BS. Management of patellar fracture with titanium cable cerclage. Medicine, 2017, 96: e8525. [DOI] [PMC free article] [PubMed] [Google Scholar]


