Abstract
Background:
There is a lack of understanding of what contributes to attitudes toward individuals with an opioid addiction and preferences for policies that support them.
Methods:
This study aimed to investigate stigmatization of an opioid addiction and support for publicly funded drug treatment. A randomized, between-subjects case vignette study (N = 1,998) was conducted with a nation-wide online survey. To assess public perceptions of stigma and support for publicly funded drug treatment, participants rated a hypothetical individual who became addicted to prescription opioids across three conditions: 1) male or female, 2) an individual who was prescribed prescription painkillers or took prescription painkillers from a friend and 3) an individual who transitioned to using heroin or who continued using prescription painkillers.
Results:
Our results showed that there were stronger negative attitudes towards a male (p < .01) and toward an individual who took prescription painkillers from a friend (all p’s < .05), and both stronger positive and negative attitudes toward an individual who transitioned to heroin from prescription painkillers (all p’s < .05). Next, we demonstrated that the probability that someone supports publicly funded drug treatment increases by 3.6 percentage points for each unit increase along a 12-point scale of positive attitudes (p < .0005), 1.3 percentage points for each unit decrease along a 12-point scale of negative attitudes (p < .005), 7.3 percentage points for each unit increase along a 6-point scale of perceived treatment efficacy (p < .0001), 0.1 percentage points for each unit decrease along a 100-point scale that measures the strength of one’s belief that addiction is controllable (p < .005) and 0.2 percentage points for each unit decrease along a 100-point scale that measures the strength of one’s belief that income is controllable (p < .005) . Lastly, when controlling for the effects of stigma, the probability of supporting publicly funded drug treatment decreases by 6.3 percentage points (p < 0.001) when an individual was prescribed prescription painkillers from a doctor. However, path analysis identified a channel through which a doctor’s prescription increased support for publicly funded drug treatment by influencing positive attitudes, negative attitudes, and responsibility.
Conclusion:
Our findings provide further evidence that information about individuals who become addicted to opioids can influence stigma perceptions and support for publicly funded drug treatment.
Keywords: opioids, stigma, heroin, nonmedical prescriptions, drug treatment, redistribution
1. Introduction
In 2017, over eleven million individuals in the United States misused opioids (heroin and prescription painkillers) (SAMHSA, 2018a). Since 1999, the sales of prescription opioids has steadily increased (Frenk, Porter, & Paulozzi, 2015) and people report obtaining painkillers from a doctor or receiving them from a friend (SAMHSA, 2018b). As the opioid epidemic persists in the United States, and as the availability of prescription opioids has curtailed due to policy measures set in place to battle prescription misuse, there is increasing evidence that people may transition from prescription opioids to heroin (Martins et al., 2019). For example, previous research has shown that prescription opioid misuse may be a risk factor for heroin use (Becker, Sullivan, Tetrault, Desai, & Fiellin, 2008; Jones, 2013).
Despite the efforts of restrictive policy measures to reduce opioid prescription misuse, there are still many individuals who misuse opioids and need treatment for their addiction. However, an individual can be deterred from seeking treatment due to stigma. Stigma can be in the form of an attitude (e.g., blame) or a shared belief about a behavior or personal attribute (Crocker, Major, & Steele, 1998; Goffman, 1963). Individuals can have self-stigma (i.e., internalized stigma) based on their behavior or a personal attribute, or they may fear the negative perceptions of others (i.e., public stigma), which can cause them to feel isolated and/or rejected. Stigma can also alter the ways in which health care professionals interact with individuals with an addiction (Botticelli & Koh, 2016), which can ultimately impact the quality of treatment they receive and further deter them from seeking medical treatment. Further, negative perceptions of individuals may be largely determined by pre-existing perceptions of individuals or groups, beliefs about the degree to which addiction is controllable (Hegarty & Golden, 2008), the type of substances that are being used and the information provided about the individual(s) who are using substances. For instance, previous research has shown that males are more stigmatized than females with a drug addiction (Sattler, Escande, Racine, & Göritz, 2017) or an opioid addiction (Goodyear, Haass-Koffler, & Chavanne, 2018; Weeks & Stenstrom, 2020). However, other studies have demonstrated that women who use cannabis and methamphetamine are rated with higher negative attributions compared to men (Sorsdahl, Stein, & Myers, 2012), while no differences between genders for persons who inject drugs are found (Kulesza et al., 2016). Therefore, stigma perceptions of males and females may vary as a function of the type of drug. Other studies investigating type of drug and its impact on stigma have indicated that there is greater internalized stigma towards individuals who use heroin compared to marijuana (Brown, 2015) and participants rate individuals in vignettes who use cannabis as less dangerous than those who use alcohol (Sorsdahl et al., 2012). In addition, background information about an individual may also influence stigma perceptions. For example, we previously reported that information provided about the precipitating events (e.g., how opioids were initially obtained) to an addiction contributes to stigma (Goodyear et al., 2018) and others have found similar effects by examining the type of drug and legality of the drug use (e.g., prescribed Vicodin versus non-prescribed Vicodin and heroin) (Weeks & Stenstrom, 2020). Yet, to our knowledge, no study has examined whether information about people transitioning from prescription painkillers to heroin affects public perceptions of stigma.
In addition to shaping how the public views people with an opioid use disorder, and how people with an opioid use disorder view themselves internally, it is also important to understand how stigmatization and other factors shape preferences for policies to respond to the opioid epidemic. Kennedy-Hendricks et al. (2017) have found that people show stronger support for punitive policies, and weaker support for public health-oriented policies, as their attitudes toward opioid users become more stigmatized. Moreover, McGinty, Pescosolido, Kennedy-Hendricks, and Barry (2017) have shown that addiction-related policy preferences can be influenced by communication strategies that destigmatize people with addictions. Chavanne and Goodyear (2020), however, have found that, despite having destigmatizing effects, knowledge that an addiction starts with a legally acquired prescription reduces support for using income redistribution to publicly fund the individual’s drug treatment. Considering the current opioid epidemic in the U.S., policymakers, medical professionals, and concerned voters would benefit from a greater understanding of how both stigma and information about the personal characteristics of those with addictions shape preferences for policies that provide support for people with opioid use disorders.
Motivated by the surge in prescription opioid use and how that influx may have contributed to the current U.S. opioid epidemic, the present study aimed to examine public stigma of individuals who transitioned from prescription opioids to heroin and the drivers of support for their publicly funded drug treatment. Therefore, we investigated precipitating events (initiation of opioid use by obtaining prescription opioids from a friend or a doctor), gender (male or female) and end point (transitioning to heroin from painkillers or continuing only with painkillers) and how this information affects attitudes towards an individual who uses opioids and the willingness to use public funding, through income redistribution, to provide this person with drug treatment. Focusing on the story of one person allowed us to cleanly manipulate precipitance, target gender and end point, and examine whether support for publicly funded drug treatment for this “type” of person is affected by the context itself and by the stigma that is influenced by the context. In addition, although beliefs about controllability may impact stigmatization of individuals with addictions (Hegarty & Golden, 2008), there are limited studies investigating the role of controllability. Therefore, we aimed to investigate how participants’ perceptions of controllability affect both stigma and levels of support for publicly funded drug treatment. Moreover, given our earlier finding that prescription precipitance reduces support for publicly funded drug treatment, we explicitly tested whether this result can be explained by differences in the perceived efficacy of treatment, which may be affected by knowledge that the healthcare system (rather than an individual’s choices) was responsible for the initiation of an addiction. We also conducted a path analysis to examine whether the effects that our manipulated variables (target gender, end point and precipitation) have on support for publicly funded drug treatment are mediated by stigma.
2. Methods
2.1. Participants
To be eligible to participate, participants had to be eighteen years old or older and had to live in the United States. Participants were recruited and paid through Amazon’s Mechanical Turk (MTurk; http://www.mturk.com). MTurk is a crowdsourcing platform that connects “Requesters,” who have tasks to be completed over the internet, and “Workers.” MTurk has become more popular among researchers as a way to conduct survey-based research and as a means to investigate clinically relevant variables (Chandler & Shapiro, 2016). Studies conducted on MTurk have been shown to replicate published experimental findings (Berinsky, Huber, & Lenz, 2012) and may provide samples that are more representative than convenience samples (Buhrmester, Kwang, & Gosling, 2011; Mason & Suri, 2012).
After accepting the assignment on MTurk, participants were taken to Qualtrics (https://www.qualtrics.com), where they provided informed consent. This study was approved by Connecticut College’s Institutional Review Board (IRB). All participants were randomly assigned to one of eight possible scenarios in a self-completed survey. The survey lasted about 7-12 minutes and they were compensated for their time. Participants were informed that they would be asked comprehension questions throughout the survey to ensure they were paying attention. Participants who missed any comprehension question were eliminated with analysis (final sample was 1,998 participants).
2.2. Case Vignettes
Similar to our previous work on opioid use and stigma (Goodyear et al., 2018), each vignette described a hypothetical individual who became addicted to opioids. There were three conditions: Target Gender (male or female), Precipitance (doctor or individual) and End Point (heroin or pills). The hypothetical individual was either male or female, prescribed prescription painkillers or took prescription painkillers from a friend and transitioned to using heroin or continued using prescription painkillers. (See Table S1 for descriptions of the vignettes.)
2.3. Outcomes
Participants rated the individual on interval scales for the four stigma variables (responsibility, dangerousness, positive affect [concern, sympathy] and negative affect [anger, disappointment]) (1 is low and 6 is extremely), support for a policy that uses income redistribution to fund a program that provides the individual with drug treatment (1 is dislike extremely and 6 is like extremely) and perceived efficacy of drug treatment (1 is very unlikely and 6 is very likely). The stigma variables were selected based on our previous work (Goodyear et al., 2018) and others (Sattler et al., 2017; Skinner, Feather, Freeman, & Roche, 2007) who have investigated the relationship between substance use and stigma. The prompt eliciting support for using income redistribution to publicly fund drug treatment was selected based on our earlier work (Chavanne & Goodyear, 2020) as well as other studies of redistributive preferences (Chavanne, 2016, 2018, 2020). As described by Chavanne and Goodyear (2020), the solicitation of preferences for using income redistribution to fund drug treatment is explicitly motivated by the prevalence of treatment-driven legislative proposals, as well as the inevitability that support for present and future addiction-related legislation will depend, to some degree, on how the public feels about tax revenues being used to fund drug treatment.
2.4. Measures
After the vignette, participants completed demographic measures, substance use history, the Perceived Stigma of Addiction Scale (PSAS) – a eight-item single-score scale that assesses perceptions of public stigma towards substance users (Luoma, O’Hair, Kohlenberg, Hayes, & Fletcher, 2010), familiarity with addiction (i.e., knowing someone with an opioid addiction), addiction controllability (a 100-point scale ranging from a belief that someone has no control over an addiction to a belief that someone has full control) and income controllability (a 100-point scale ranging from a belief that someone has no control over their income to a belief that someone has full control) (Table 1).
Table 1.
Descriptive statistics on demographic measures
| Measure | N (%) | M ± SD |
|---|---|---|
| Age | 38.6 ± 12.15 | |
| Gender | ||
| Male | 1067 (53.40) | |
| Female | 921 (46.10) | |
| Other | 10 (0.50) | |
| Race | ||
| American Indian/Native American | 10 (0.50) | |
| Asian | 114 (5.71) | |
| Black/African American | 160 (8.01) | |
| Hispanic/Latino | 74 (3.70) | |
| White/Caucasian | 1534 (76.78) | |
| Pacific Islander | 2 (0.10) | |
| Other | 17 (0.85) | |
| Mixed race | 87 (4.35) | |
| Income ($) | ||
| Less than 12,000 | 271 (13.56) | |
| 12,000-29,000 | 486 (24.32) | |
| 30,000-47,999 | 512 (25.63) | |
| 48,000-66,000 | 343 (17.17) | |
| More than 66,000 | 386 (19.32) | |
| Education | ||
| Eighth grade or lower | 1 (0.050) | |
| Some high school | 14 (0.70) | |
| High school graduate | 181 (9.06) | |
| Some college | 581 (29.08) | |
| Professional training/license | 72 (3.60) | |
| College graduate | 850 (42.54) | |
| Graduate degree | 299 (14.97) | |
| Political Party | ||
| Extremely liberal | 264 (13.21) | |
| Liberal | 534 (26.73) | |
| Slightly liberal | 262 (13.11) | |
| Middle of the road | 358 (17.92) | |
| Slightly conservative | 219 (10.96) | |
| Conservative | 220 (11.01) | |
| Extremely conservative | 96 (4.80) | |
| N.A. | 45 (2.25) | |
| Familiarity | ||
| Yes | 702 (35.14) | |
| No | 1296 (64.86) | |
| Current/past opioid use | ||
| Yes | 254 (12.71) | |
| No | 1744 (87.29) | |
| Control | 51.1 ± 25.71 | |
| Total PSAS Score | 27.8 ± 5.50 |
PSAS = Perceived Stigma of Addiction Scale
2.5. Statistical Analysis
To assess any differences across scenarios, one-way analyses of variance (ANOVAs) and chi-square (χ2) analyses were conducted for continuous and binary measures (Table S2). First, to investigate stigma perceptions (responsibility, dangerousness, positive affect and negative affect), a 2 (Target Gender) x 2 (Precipitance) x 2 (End Point) multivariate analysis of covariance (MANCOVA) was implemented. A principal component factor analysis with varimax rotation was conducted on the four affect scales (concern, sympathy, anger and disappointment). Two components with an eigenvalue greater than 1 were found and scores for anger and disappointment were combined for a measure of negative affect and concern and sympathy were combined for a measure of positive affect. Participant’s past and current nonmedical prescription opioid use (yes, no), familiarity (yes, no) with addiction and addiction controllability (1-100) were included as covariates. Mann-Whitney U tests were conducted as a robustness check for our results. Second, to examine support for publicly funded drug treatment, logistical regression analysis was used to measure how manipulated variables, stigma variables and personal characteristics affect the probability that a participant supports publicly funded drug treatment for the individual in the vignette. Although results from binary logistic regression are presented to simplify the analysis ease interpretation of effect sizes, results remain substantively similar when ordered logistic regression is used with a categorical (1-6) expression of support for publicly funded drug treatment is used. Third, a path analysis was conducted to test whether stigma variables and perceived efficacy mediated the effects that the manipulated variables had on support for publicly funded drug treatment. Data analysis was conducted with the Statistical Package for Social Sciences 24.0 (SPSS 24.0, IBM Corp.) and Stata with alpha set to p < .05.
3. Results
3.1. Stigma Results
3.1.1. Responsibility
The MANCOVA indicated that there was a significant main effect of Precipitance (F(1, 1987) = 55.99, p < .0001) indicating that individual was rated with higher responsibility compared to doctor (Figure 1). There were no significant main effects of Target Gender (F(1, 1987) = 0.06, p = .815) or End Point (F(1, 1987) = 0.22, p = .639). There was also a significant covariate effect of addiction controllability (F(1, 1987) = 168.17, p < .0001). A bivariate Spearman’s rho correlation was conducted for addiction controllability and the results showed that individuals who rated with higher controllability also rated with higher responsibility r(1996) = .31, p < .0001). No other covariate effects or interaction effects were found for responsibility (all p’s > .05).
Figure 1. Responsibility Ratings.
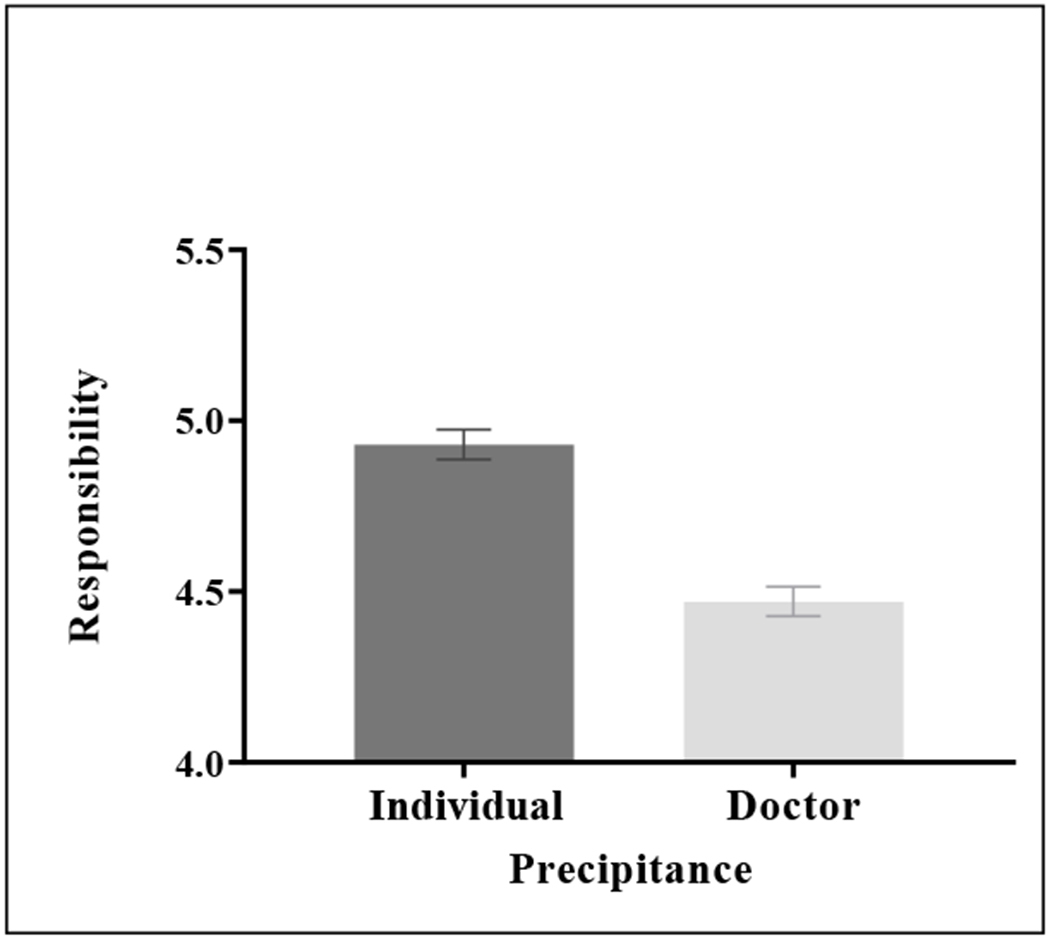
Participants in the individual condition rated with higher responsibility compared to the doctor condition (p < .0001).
Planned follow-up Mann-Whitney U tests showed a significant difference for Precipitance between individual and doctor (U = 376576.00, p < .0001), which is consistent with the MANCOVA findings. Target Gender (U = 494190.50, p = .713) and End Point (U = 495650.50, p = .792) were not significant.
3.1.2. Dangerousness
There were significant main effects of Target Gender (F(1, 1987) = 7.13, p = .008), Precipitance (F(1, 1987) = 4.95, p = .026) and End Point (F(1, 1987) = 29.50, p < .0001). For Target Gender, male was rated with higher dangerousness compared to female (Figure 2A). For Precipitance, individual was rated with higher dangerousness compared to doctor (Figure 2B). Lastly, for End Point, heroin was rated with higher dangerousness compared to pills (Figure 2C). There was also a significant covariate effect of addiction controllability (F(1, 1987) = 46.77, p < .0001). The bivariate Spearman’s rho correlation for addiction controllability showed that individuals who rated with higher controllability also rated with higher dangerousness r(1996) = .16, p < .0001). No other covariate effects or interaction effects were found for dangerousness (all p’s > .05).
Figure 2. Dangerousness Ratings.
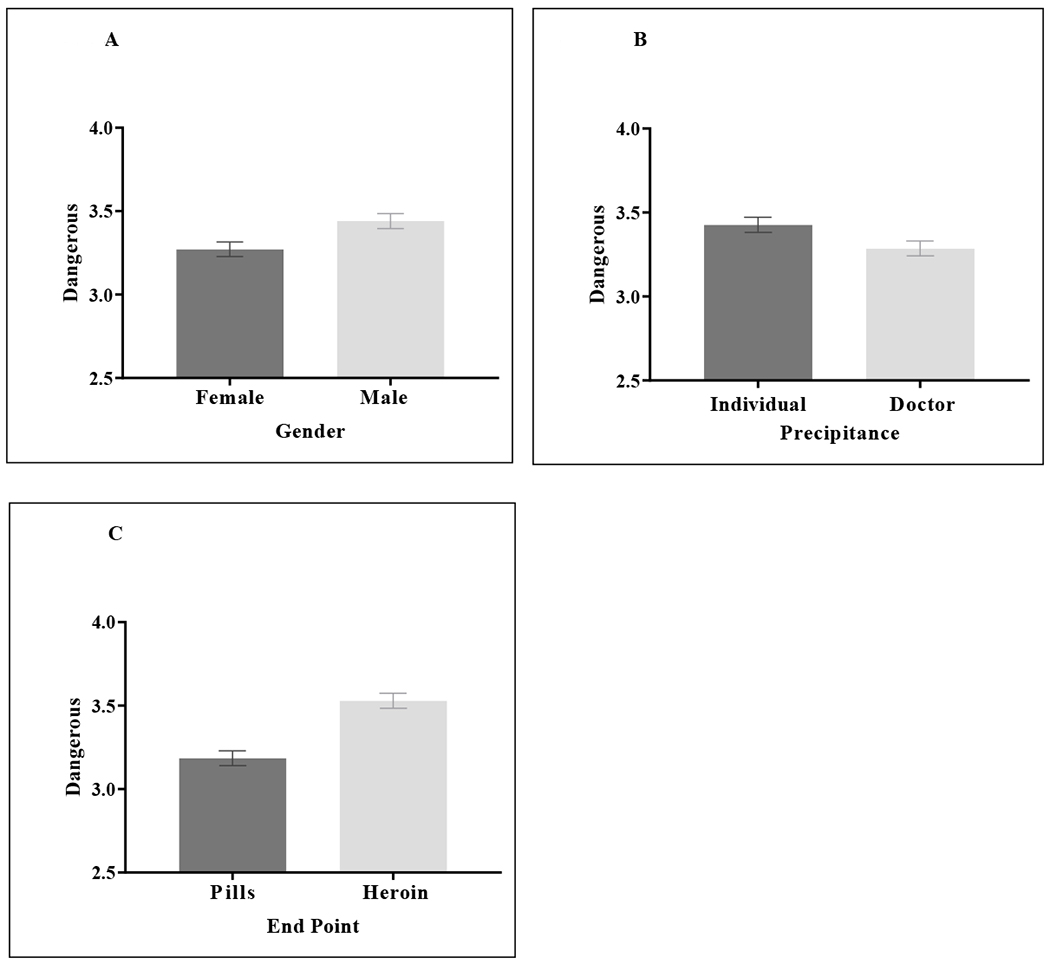
A) Participants in the male condition rated with higher dangerousness compared to the female condition (p = .008). B) Participants in the individual condition rated with higher dangerousness ratings compared to the doctor condition (p = .026). C) Participants in the heroin condition rated with higher dangerousness compared to the pills condition (p < .0001)
Planned follow-up Mann-Whitney U tests showed a significant difference for Target Gender between male and female (U = 462102.00, p = .004), Precipitance between individual and doctor (U = 472984.00, p = .043) and End Point between pills and heroin (U = 429231.00, p < .0001), which are consistent with the MANCOVA findings.
3.1.3. Positive Affect
For positive affect, there were significant main effects of Precipitance (F(1, 1987) = 23.91, p < .0001) and End Point (F(1, 1987) = 4.41, p = .036). Target Gender was not found to be significant (F(1, 1987) = 2.61, p = .106). For Precipitance, doctor was rated with higher positive affect compared to individual (Figure 3A) and for End Point, heroin was rated with higher positive affect compared to pills (Figure 3B). There was also significant covariate effects found for familiarity (F(1, 1987) = 5.08, p = .024) and addiction controllability (F(1, 1987) = 234.91, p < .0001). Familiarity was associated with higher positive affect ratings (Figure 3C). The bivariate Spearman’s rho correlation for addiction controllability indicated that individuals who rated with higher controllability also rated with lower positive affect r(1996) = −.32, p < .0001). No other covariate effects or interaction effects were found (all p’s > .05).
Figure 3. Positive Affect Ratings.
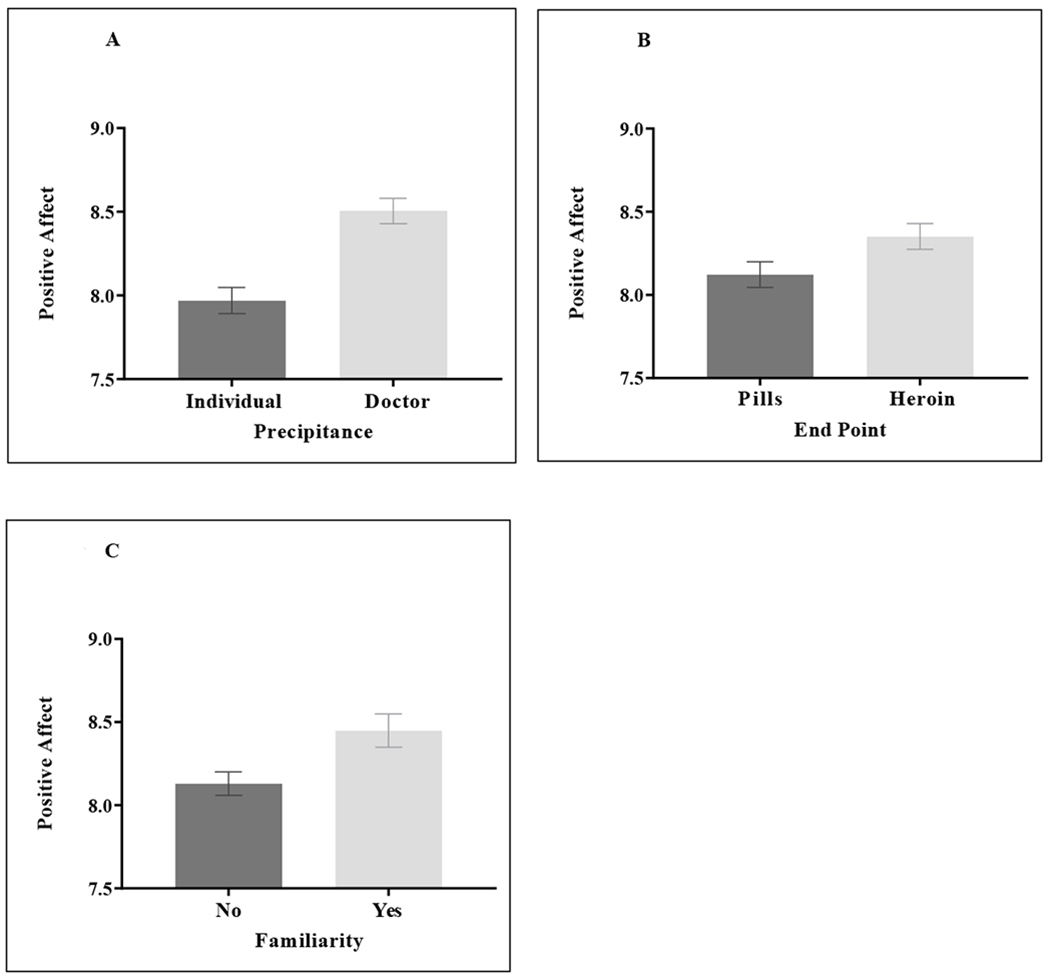
A) Participants in the doctor condition rated with higher positive affect compared to the individual condition (p < .0001). B) Participants in the heroin condition rated with higher positive affect compared to the pills condition (p = .036). C) Participants who knew someone with an opioid addiction had higher overall positive affect ratings compared to participants who did not know someone with an opioid addiction (p = .024).
Planned follow-up Mann-Whitney U tests showed a significant difference for Target Gender between male and female (U = 473118.50, p = .045) and Precipitance between individual and doctor (U = 437603.50, p < .0001) and End Point between pills and heroin (U = 473709.00, p = .049). We did not find a significant main effect of Target Gender in the MANCOVA, however, the Mann-Whitney U tests don’t account for covariates. We did confirm robustness of our main effects.
3.1.4. Negative Affect
There were significant main effects of Precipitance (F(1, 1987) = 39.32, p < .0001) and End Point (F(1, 1987) = 5.34, p = .021). No main effect of Target Gender was found (F(1, 1987) = 0.61, p = .435). For Precipitance, individual was rated with higher negative affect than doctor and for End Point (Figure 4A), heroin was rated with higher negative affect than pills (Figure 4B). Significant covariate effects for opioid use (F(1, 1987) = 29.80, p < .0001) and addiction controllability (F(1, 1987) = 122.35, p < .0001) were found. Opioid use was associated with lower negative affect ratings (Figure 4C). The bivariate Spearman’s rho correlation for addiction controllability indicated that individuals who rated with higher controllability also rated with higher negative affect r(1996) = .24, p < .0001. No other covariate effects or interaction effects were found (all p’s > .05).
Figure 4. Negative Affect Ratings.
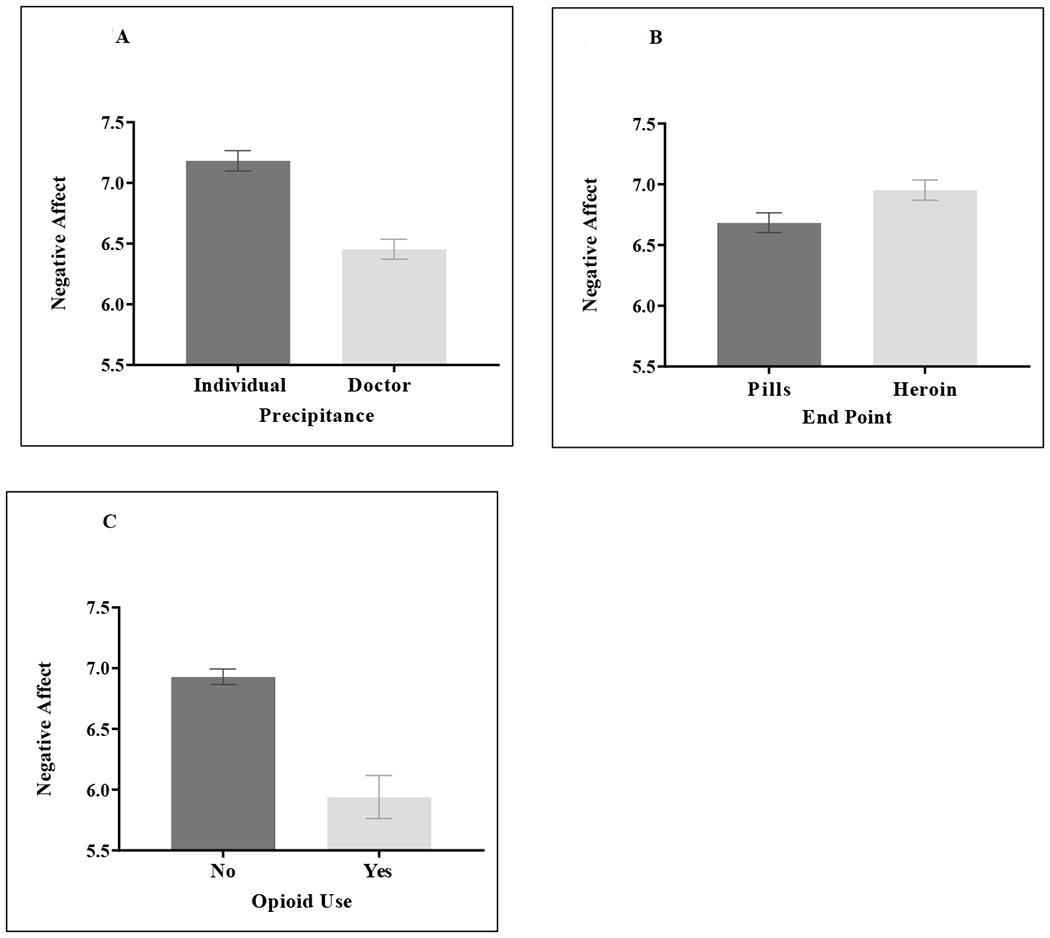
A) Participants in the individual condition rated with higher negative affect compare to the doctor condition (p < .0001). B) Participants in the heroin condition rated with higher negative affect compared to the pills condition (p = .021). C) Participants who had used nonmedical prescription opioids had lower negative affect compared to participants who had not used nonmedical prescription opioids (p < .0001).
The planned follow-up Mann-Whitney U tests showed a significant difference for Precipitance between individual and doctor (U = 424638.50, p < .0001) and for End Point (U = 469494.00, p = .022) and no significant difference for Target Gender (U = 482921.50, p = .217). These results are consistent with the MANCOVA findings.
3.2. Drug Treatment Results
In addition to quantifying relationships between our manipulated variables and stigma, the design also allowed us to examine the set of factors that were associated with support for publicly funded drug treatment for the person in the vignette. Table 2 presents results from a set of logistic regressions that, across a variety of specifications, examined the factors that are associated with support for publicly funded drug treatment. Across all specifications, the dependent variable was set equal to one if the respondent stated that they would like the individual in the vignette to receive publicly funded drug treatment (like slightly, like very much, like extremely) and zero otherwise (dislike slightly, dislike very much, dislike extremely); manipulated variables were included across all specifications, while personal characteristics (sociodemographic variables and variables that relate to familiarity with opioid use), stigma variables, perceptions of treatment efficacy and perceptions of the controllability of income and addiction were included or omitted depending on the specification. Although logistic regressions were used to facilitate presentation of effect sizes, all results described below met the stated significance thresholds under ordered logistic regression. All variables met the assumption of proportional odds under ordered logistic models (Brant test, p > .05) across all specifications except age (Brant test, p < .05 in specifications 2-6), efficacy (Brant test, p < .05 in specifications 5 and 6) and negative affect (Brant test, p < .05 in specification 2). Specification five included the entire set of personal characteristics, perceptions of efficacy and perceptions of income- and addiction-controllability, while omitting the stigma variables; the included variables in this specification, therefore, may be absorbing some of the effects of stigma. Specification 6, with the stigma variables included, showed us the effects that the manipulated variables, personal characteristics and beliefs about efficacy and controllability had above and beyond the effects of stigma.
Table 2.
Logistic regressions examining support for publicly funded drug treatment
| Dependent variable equals 1 if respondent supports publicly funded drug treatment | ||||||
|---|---|---|---|---|---|---|
|
VARIABLES |
(1) Treatment Only |
(2) Treatment and Personal |
(3) Treatment, Personal and Stigma |
(4) Treatment, Personal, Stigma and Efficacy |
(5) Treatment, Personal, Efficacy and Controllability |
(6) Treatment, Personal, Stigma, Efficacy and Controllability |
| John | −0.106 (0.0898) | −0.113 (0.0991) | −0.0596 (0.106) | −0.0695 (0.108) | −0.0668 (0.105) | −0.0507 (0.109) |
| Heroin ending | −0.0411 (0.0898) | 0.00495 (0.0992) | −0.0282 (0.106) | 0.0185 (0.108) | 0.0957 (0.106) | 0.0382 (0.110) |
| Doctor | −0.119 (0.0898) | −0.137 (0.0989) | −0.416*** (0.108) | −0.412*** (0.110) | −0.134 (0.105) | −0.363*** (0.112) |
| Male | 0.120 (0.101) | 0.113 (0.107) | 0.181* (0.109) | 0.237** (0.107) | 0.215* (0.111) | |
| White | −0.116 (0.122) | −0.139 (0.129) | −0.128 (0.131) | −0.111 (0.128) | −0.117 (0.133) | |
| College graduate | 0.0643 (0.105) | 0.0304 (0.113) | 0.0238 (0.115) | 0.0488 (0.113) | 0.0285 (0.117) | |
| Income < $30,000 | 0.417*** (0.106) | 0.451*** (0.113) | 0.452*** (0.116) | 0.360*** (0.114) | 0.385*** (0.118) | |
| Liberal | 1.643*** (0.101) | 1.448*** (0.108) | 1.400*** (0.109) | 1.338*** (0.108) | 1.281*** (0.112) | |
| Age | −0.0186*** (0.00417) | −0.0178*** (0.00449) | −0.0200*** (0.00459) | −0.0204*** (0.00458) | −0.0184*** (0.00473) | |
| Current use | −0.237 (0.321) | −0.384 (0.355) | −0.299 (0.340) | −0.0661 (0.315) | −0.247 (0.344) | |
| Past use | 0.00874 (0.163) | −0.212 (0.175) | −0.159 (0.179) | 0.0104 (0.177) | −0.157 (0.184) | |
| Know opioid user | 0.218** (0.108) | 0.169 (0.115) | 0.211* (0.117) | 0.235** (0.117) | 0.188 (0.119) | |
| Positive affect | 0.267*** (0.0226) | 0.219*** (0.0237) | 0.209*** (0.0243) | |||
| Negative affect | −0.0883*** (0.0227) | −0.0878*** (0.0232) | −0.0739*** (0.0234) | |||
| Responsibility | −0.115*** (0.0384) | −0.142*** (0.0395) | −0.0936** (0.0410) | |||
| Dangerous | −0.0273 (0.0411) | −0.00194 (0.0419) | 0.00767 (0.0423) | |||
| Treatment efficacy | 0.422*** (0.0563) | 0.553*** (0.0578) | 0.424*** (0.0591) | |||
| Addiction control | −0.0135*** (0.00217) | −0.00674*** (0.00235) | ||||
| Income control | −0.0143*** (0.00252) | −0.0142*** (0.00261) | ||||
| Constant | 0.000453 (0.0901) | −0.429* (0.241) | −1.153*** (0.396) | −2.556*** (0.453) | −1.242*** (0.382) | −1.708*** (0.479) |
| Observations | 1,998 | 1,998 | 1,998 | 1,998 | 1,998 | 1,998 |
| Pseudo R2 | 0.001 | 0.131 | 0.213 | 0.233 | 0.211 | 0.250 |
Robust standard errors in parentheses
p < .01
p < .05
p < .10
The results found that our treatment effects did not show consistent significant connections with support for drug treatment. For end point and target gender, no significant effect was found in any specification (across specifications 1-6, for end point and for target gender, all p’s > .05). For precipitance, however, the results showed that, in each of the three specifications that included the stigma variables (2, 3, 4 and 6), the effect of doctor, relative to individual, was negative and significant (p < .001). This result indicated that, when controlling for the effects of stigma, being told that an opioid prescription from a doctor precipitated an addiction made respondents significantly less likely to support drug treatment. The fact that the coefficient on doctor remained significant in specification 6, which controlled for beliefs about treatment efficacy, suggests that the relationship between prescription precipitance and weaker support for publicly funded drug treatment was not driven by a decreased faith in treatment efficacy stemming from an addiction starting at the hands of a medical professional.
In contrast to the lack of consistent results associated with the manipulated variables, stigma, beliefs about efficacy, beliefs about controllability and personal characteristics show significant associations with support for drug treatment. Higher levels of positive affect (p < .0005 across specifications 2, 3, 4 and 6), lower levels of negative affect (p < .005 across specifications 2, 3, 4 and 6) and weaker ratings of responsibility (p = .023 across specifications 2, 3, 4 and 6) all made someone significantly more likely to support drug treatment. No significant relationship between dangerousness and support for drug treatment was found in any specification. A greater perceived likelihood of treatment efficacy was significantly associated with support for drug treatment (p < .0001 across specifications 4-6), as were beliefs that income (p < .0001 across specifications 5 and 6) and addiction (p < .005 across specifications 5 and 6) are less controllable. Regarding sociodemographic characteristics, having an annual income below $30,000 (p < .005 across specifications 3-6), identifying politically as a liberal (extremely liberal, liberal or slightly liberal) (p < .0001 across specifications 3-6) and being younger (p < .0001 across specifications 3-6) all made someone significantly more likely to support publicly funded drug treatment for the individual in the vignette.
To show effect sizes associated with the variables, marginal effects for specification 6 of Table 2 are presented in Table S3. When controlling for the effects of stigma, a participant who read about a doctor’s prescription precipitating the addiction was 6.3 percentage points less likely to support drug treatment than a participant who read about an addiction precipitated by the decision to take pills from a friend. A unit increase in positive affect rating increased the probability that someone supports drug treatment by 3.6 percentage points, while a unit increase in negative stigma rating (responsibility) decreased the probability by 1.3 percentage points (1.6 percentage points). For perceived treatment efficacy, each stepwise increase in perceived efficacy was associated with a 7.3 percentage point increase in the probability that someone supported drug treatment. For the controllability scales, a unit increase along the 100-point scale decreased the probability that someone supported drug treatment by 0.1 percentage points for addiction controllability and 0.2 percentage points for income controllability. Having an annual income below $30,000 increased the probability that someone supports drug treatment by 6.6 percentage points, while identifying as a liberal increased the probability that someone supports drug treatment by 22 percentage points, and an additional year of age decreased the probability of supporting drug treatment by 0.3 percentage points.
Finally, given both the effects of the manipulated variables on stigma and the effects of stigma and perceived efficacy on support for drug treatment, a path analysis formally examined how stigma and perceived efficacy mediate the effects that our manipulated variables had on support for drug treatment. Figure 5 provides a simplified presentation of the model which, for ease of presentation, captures the path among the categories of variables without listing each variable. Regression coefficients are denoted in the figure as either bx (direct effects on support for drug treatment) or ax (mediation effects of manipulated variables on stigma variables or perceived efficacy). Support for drug treatment on the 1-6 ordinal scale was used as the outcome variable in the model, though all results are substantively unchanged when support for drug treatment is treated as binary. With the stigma variables and efficacy also being measured ordinally, the paths of interest are all estimated using ordinal logistic regression.
Figure 5:
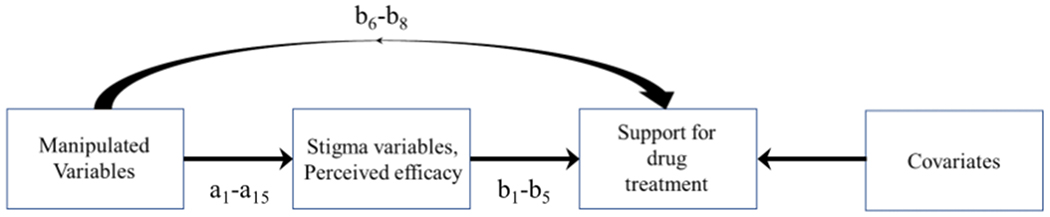
Path Analysis Model
Stata’s generalized structural equation modeling function (GSEM) was used to conduct the analysis. Table 3 presents the results of the analysis, including the direct effects of the independent variables on support for drug treatment (coefficients b1-b8) and mediation effects found when the manipulated variables are regressed on each separate stigma variable and the efficacy variable (coefficients a1-a15). Direct effects of all covariates from specification 6 of Table S3 were included in the model, but coefficients were omitted from the table. For direct effects, positive affect (p < .001) and perceived treatment efficacy (p < .001) were associated with a greater likelihood of supporting drug treatment; negative affect (p < .001), responsibility (p < .001) and an addiction precipitated by a doctor’s prescription (p < .001) were associated with a reduced likelihood of supporting drug treatment.
Table 3.
Path analysis of the effects of treatment and stigma variables on support for drug treatment
| VARIABLES | Coefficient (standard error) |
|
|---|---|---|
| Dependent variable: Binary support for redistributive drug treatment | ||
| Positive affect | b1 | 0.207*** (0.0197) |
| Negative affect | b2 | −0.0818*** (0.0190) |
| Responsibility | b3 | −0.128*** (0.0335) |
| Dangerous | b4 | 0.0224 (0.0345) |
| Treatment efficacy | b5 | 0.350*** (0.0475) |
| Target male | b6 | −0.0780 (0.0831) |
| Heroin ending | b7 | 0.0313 (0.0843) |
| Doctor | b8 | −0.312*** (0.0859) |
| Dependent variable: Positive affect | ||
| Target male | a1 | −0.147* (0.0781) |
| Heroin ending | a2 | 0.152* (0.0781) |
| Doctor | a3 | 0.371*** (0.0786) |
| Dependent variable: Negative affect | ||
| Target male | a4 | 0.0874 (0.0784) |
| Heroin ending | a5 | 0.180** (0.0783) |
| Doctor | a6 | −0.450*** (0.0786) |
| Dependent variable: Responsibility | ||
| Target male | a7 | 0.00987 (0.0805) |
| Heroin ending | a8 | −0.0203 (0.0805) |
| Doctor | a9 | −0.825*** (0.0857) |
| Dependent variable: Dangerousness | ||
| Target male | a10 | 0.238*** (0.0794) |
| Heroin ending | a11 | 0.445*** (0.0797) |
| Doctor | a12 | −0.163** (0.0791) |
| Dependent variable: Efficacy | ||
| Target male | a13 | −0.104 (0.0815) |
| Heroin ending | a14 | −0.205** (0.0816) |
| Doctor | a15 | 0.0880 (0.0817) |
| Observations | 1,998 |
Standard errors in parentheses
p < .01
p < .05
p < .10
Indirect and total effects of the manipulated variables on support for drug treatment were calculated using Stata’s nlcom function, which also provides standard errors, z-statistics, and probability levels. Table 4 presents the separate indirect effect for each manipulated variable mediated by positive affect, negative affect, responsibility, dangerousness, and efficacy; the multiplied coefficients are also presented using the notation for coefficients from Table 3. Table 4 also provides, for each manipulated variable, (1) the sum of the five indirect effects and (2) the total effect, which is found by adding the direct effect for each manipulated variable identified in Table 3 and the sum of indirect effects. The results showed that none of the manipulated variables have a statistically significant total effect, but the significant indirect effects of doctor precipitance (positive affect, p < .001; negative affect, p < 0.005; responsibility, p < .001) show that there is a channel through which support for drug treatment is increased via the destigmatizing effects of doctor precipitance. Additionally, the analysis found that a heroin end point has significantly negative indirect effects on support for drug treatment via its effect on negative affect (p = .046) and perceived efficacy (p = .018).
Table 4.
Path analysis indirect and total effects of treatment variables
| Treatment variable | Source of mediation | Indirect effect | Coefficient (Standard error) |
|---|---|---|---|
| Doctor | Positive affect | b1*a3 | 0.077*** (0.018) |
| Negative affect | b2*a6 | 0.037*** (0.011) | |
| Responsibility | b3*a9 | 0.105*** (0.030) | |
| Dangerousness | b4*a12 | −0.004 (0.006) | |
| Efficacy | b5*a15 | 0.031 (0.029) | |
| Sum of indirect effects | 0.246*** (0.050) | ||
| Total effect | −0.066 (0.093) | ||
| Heroin end | Positive affect | b1*a2 | 0.031* (0.016) |
| Negative affect | b2*a5 | −0.015** (0.007) | |
| Responsibility | b3*a8 | 0.003 (0.010) | |
| Dangerousness | b4*a11 | 0.010 (0.015) | |
| Efficacy | b5*a14 | −0.072** (0.030) | |
| Sum of indirect effects | −0.043 (0.046) | ||
| Total effect | −0.011 (0.093) | ||
| Target male | Positive affect | b1*a1 | −0.030* (0.016) |
| Negative affect | b2*a4 | −0.007 (0.007) | |
| Responsibility | b3*a7 | −0.001 (0.010) | |
| Dangerousness | b4*a10 | 0.005 (0.008) | |
| Efficacy | b5*a13 | −0.036 (0.029) | |
| Sum of indirect effects | −0.070* (0.043) | ||
| Total effect | −0.148 (0.093) | ||
Standard errors in parentheses
p < .01
p < .05
p < .10
4. Discussion
This study aimed to further understand the stigmatization of an opioid addiction and support for publicly funded drug treatment by assessing the contributions of precipitance, gender and end point on public attitudes. When investigating the role of precipitance (initiation of opioid use by obtaining prescription opioids from a friend or a doctor) on stigma attitudes, participants in the individual condition rated with higher stigma (higher responsibility, dangerousness and negative affect and lower positive affect) compared to the doctor condition. These results confirm our hypothesis that there would be higher stigma towards an individual who took opioids from a friend compared to receiving a prescription from a doctor and also replicates our previous findings on precipitance (Goodyear et al., 2018). These findings further substantiate that information provided about how an individual develops an opioid addiction contributes to public perceptions of stigma. In addition, we again found that gender plays a role in stigma perceptions. Our results indicated that participants in the male condition rated with higher dangerousness compared to participants in the female condition. In our previous work, we did not find an overall effect of dangerousness for gender; however, we did see lower positive affect ratings in the male condition compared to the female condition.
In addition to our findings on precipitance and gender, we also investigated the end point of an addiction – the transition from prescription painkillers to heroin. We showed that participants in the heroin condition rated with higher dangerousness, positive affect (sympathy and concern) and negative affect (anger and disappointment) compared to the pill condition (continuing with prescription painkillers). Although the finding that both positive and negative attitudes are enhanced in the heroin condition may seem surprising, it suggests that an individual who transitions to heroin compared to prescription painkillers conjures a wider range of emotional perceptions since heroin is illegal and considered more of a street drug than prescription opioids. In general, this finding highlights that information about the type substance used can have noteworthy effects on perceptions of stigma. Since, to our knowledge, no studies have compared public perceptions of stigma when comparing heroin to prescription opioids, future studies are needed to confirm and validate our results.
In addition to our main condition findings on stigma, we also demonstrated several covariate effects. First, we showed that participants who were familiar with addiction (i.e., knowing someone with an opioid addiction) rated with higher positive affect and participants that had current or past opioid use rated with lower negative affect. Past research of ours (Goodyear et al., 2018) and others (Corrigan, Kuwabara, & O’Shaughnessy, 2009; Sattler et al., 2017) have shown that familiarity with addictions may influence stigma perceptions and these results confirm past findings. In light of the role that perceptions of controllability (the belief that someone has control over an addiction) may have on stigma towards someone with an opioid addiction, we investigated the relationship between addiction controllability and stigma. We found that higher controllability ratings were associated with lower positive affect and higher negative affect, dangerousness and responsibility. These results indicate that the more that participants believed that addiction is within someone’s control, the higher the stigma ratings.
Lastly, we showed that greater levels of positive attitudes, lower levels of negative attitudes, greater perceived likelihood of treatment efficacy, the belief that addiction is less controllable and the belief that income is less controllable were all also associated with stronger support for publicly funded drug treatment. The effect of perceptions of income controllability on preferences for drug treatment is consistent with earlier studies identifying beliefs about the role of luck in shaping life situations as a robust driver of preferences for income redistribution (see Chavanne (2016, 2018) for recent reviews). Likewise, the effect of perceptions of addiction controllability on preferences for drug treatment is consistent with earlier studies that find information about the controllability of health outcomes to be robust drivers of preferences for using income redistribution to fund healthcare (Dolan & Tsuchiya, 2009; Edlin, Tsuchiya, & Dolan, 2012; Gu, Lancsar, Ghijben, Butler, & Donaldson, 2015; Le Clainche & Wittwer, 2015; Van der Star & Van den Berg, 2011). Finally, although we found through our path analysis that an addiction precipitated by a doctor’s prescription had no significant total effect on support for drug treatment, we identified a channel through which doctor precipitance increased support for drug treatment by destigmatizing addiction. Further studies are needed to identify the mechanisms that counteract these destigmatizing indirect effects of doctor precipitance and drive the offsetting reduction in support for drug treatment that is attached to it. Doctor precipitance, despite its destigmatizing effects, may be shifting attitudes toward the appropriate role of government and/or taxation. Knowledge that an addiction started at the hands of a medical professional may, for instance, be making people less willing to use tax dollars to fund treatment for those with addictions.
Our study has a few limitations. Since our sample was mostly white, the public perceptions of stigma may not be generalizable. Second, independent variables (e.g., addiction controllability) were taken at the end of the study to avoid any influence on participants’ perceptions about the experimental task. As noted earlier, further studies are needed to confirm our findings on stigma perceptions when comparing prescription painkillers to heroin and for support on drug treatment. Third, we measured addiction controllability and income controllability as one-item continuous scales. Future studies should consider creating a validified multi-item scale with the inclusion of additional items. Fourth, the generalizability of individual descriptions depicted in vignettes should be considered. Our study investigated an individual depicted in a vignette and future studies should consider examining potential differences when groups of individuals are described and how that relates to policy preferences, for example. Fifth, as noted earlier, there is evidence that MTurk may provide samples that are more representative than convenience samples. Nonetheless, the cross-sectional nature of the study should be noted as a limitation.
It is also important to consider both the strengths and limitations of our method for soliciting support for using income redistribution to fund drug treatment. The design choice assumes that the person in the vignette can serve as an archetype; support for treatment for someone who, for example, first acquired pills from a doctor and eventually transitioned to heroin is intended to represent support for generic treatment under the belief, or after receiving information that indicates, that typical people with addictions share this history. For our design choice to have external validity, changes in support for providing drug treatment for the person in the vignette must be aligned with changes in support for providing generic drug treatment. Additional work is needed to explore whether our results extend to conditions when support for generic treatment is solicited.
In conclusion, this study aimed to examine the stigmatization of an opioid addiction and support for publicly funded drug treatment. Our findings substantiate the claim that information provided about how an individual develops an addiction (i.e., initiation of opioid use and the transition from prescriptions opioids to heroin) influences stigma perceptions and support for publicly funded drug treatment. These findings have two-fold implications. First, the study findings provide knowledge of what creates opioid stigma and the perpetuation of negative attitudes. This information can help to combat stigma by breaking down internal barriers for treatment providers and how they can provide effective delivery of care to individuals with an opioid addiction. Second, greater information about stigma can facilitate treatment modalities that change the way individuals view themselves. With the high rates of individuals who are negatively impacted by their opioid addiction, understanding the variables that may affect public perceptions can provide a deeper knowledge of how to reshape negative perspectives. The ultimate goal would be to better inform people about the impact that stigma can have on individuals with an opioid addiction, which can potentially impact positive behaviors such as treatment seeking.
Supplementary Material
Acknowledgments
Funding
This study was funded by Connecticut College, faculty support account 152-10000-202380 (PI: Dr. Chavanne). Dr. Goodyear is supported by the National Institute on Alcohol Abuse and Alcoholism (K01 AA026874) and previously by the 5T32AA007459 training grant.
Footnotes
Conflict of interest
The author reports no conflict of interest.
References
- Becker WC, Sullivan LE, Tetrault JM, Desai RA, & Fiellin DA (2008). Non-medical use, abuse and dependence on prescription opioids among U.S. adults: psychiatric, medical and substance use correlates. Drug Alcohol Depend, 94(1-3), 38–47. doi: 10.1016/j.drugalcdep.2007.09.018 [DOI] [PubMed] [Google Scholar]
- Berinsky AJ, Huber GA, & Lenz GS (2012). Evaluating online labor markets for experimental research: Amazon.com’s Mechanical Turk. Political Analysis, 20(3), 351–368. [Google Scholar]
- Botticelli MP, & Koh HK (2016). Changing the language of addiction. Jama, 316(13), 1361–1362. doi: 10.1001/jama.2016.11874 [DOI] [PubMed] [Google Scholar]
- Brown SA (2015). Stigma towards Marijuana Users and Heroin Users. J Psychoactive Drugs, 47(3), 213–220. doi: 10.1080/02791072.2015.1056891 [DOI] [PubMed] [Google Scholar]
- Buhrmester M, Kwang T, & Gosling SD (2011). Amazon’s Mechanical Turk:A New Source of Inexpensive, Yet High-Quality, Data? Perspectives on Psychological Science, 6(1), 3–5. doi: 10.1177/1745691610393980 [DOI] [PubMed] [Google Scholar]
- Chandler J, & Shapiro D (2016). Conducting Clinical Research Using Crowdsourced Convenience Samples. Annu Rev Clin Psychol, 12, 53–81. doi: 10.1146/annurev-clinpsy-021815-093623 [DOI] [PubMed] [Google Scholar]
- Chavanne D (2016). Redistributive Preferences and the Dimensionality of Self-Determination and Luck. Available at SSRN 2511328. [Google Scholar]
- Chavanne D (2018). Headwinds, Tailwinds, and Preferences for Income Redistribution. Social Science Quarterly, 99(3), 851–871. [Google Scholar]
- Chavanne D (2020). Headwinds, tailwinds and preferences for redistributive healthcare. The Social Science Journal, 1–18. [Google Scholar]
- Chavanne D, & Goodyear K (2020). Waking up from Dreamland: Opioid Addiction Precipitance and Support for Redistributive Drug Treatment. Journal of Drug Policy Analysis, 1(ahead-of-print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW, Kuwabara SA, & O’Shaughnessy J (2009). The Public Stigma of Mental Illness and Drug Addiction. Journal of Social Work, 9(2), 139–147. doi: 10.1177/1468017308101818 [DOI] [Google Scholar]
- Crocker J, Major B, & Steele C (1998). Social stigma. The handbook of social psychology., Vols. 1-2, 4th ed. [Google Scholar]
- Dolan P, & Tsuchiya A (2009). The social welfare function and individual responsibility: some theoretical issues and empirical evidence. Journal of health economics, 28(1), 210–220. [DOI] [PubMed] [Google Scholar]
- Edlin R, Tsuchiya A, & Dolan P (2012). Public preferences for responsibility versus public preferences for reducing inequalities. Health Economics, 21(12), 1416–1426. [DOI] [PubMed] [Google Scholar]
- Frenk SM, Porter KS, & Paulozzi LJ (2015). Prescription opioid analgesic use among adults: United States, 1999–2012. NCHS Data Brief(189), 1–8. [PubMed] [Google Scholar]
- Goffman E (1963). Stigma: Notes on the Management of Spoiled Identity. Englewood Cliffs. [Google Scholar]
- Goodyear K, Haass-Koffler CL, & Chavanne D (2018). Opioid use and stigma: The role of gender, language and precipitating events. Drug Alcohol Depend, 185, 339–346. doi: 10.1016/j.drugalcdep.2017.12.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu Y, Lancsar E, Ghijben P, Butler JR, & Donaldson C (2015). Attributes and weights in health care priority setting: a systematic review of what counts and to what extent. Social Science & Medicine, 146, 41–52. [DOI] [PubMed] [Google Scholar]
- Hegarty P, & Golden AM (2008). Attributional beliefs about the controllability of stigmatized traits: Antecedents or justifications of prejudice? Journal of Applied Social Psychology, 38(4), 1023–1044. [Google Scholar]
- Jones CM (2013). Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers - United States, 2002-2004 and 2008-2010. Drug Alcohol Depend, 132(1-2), 95–100. doi: 10.1016/j.drugalcdep.2013.01.007 [DOI] [PubMed] [Google Scholar]
- Kennedy-Hendricks A, Barry CL, Gollust SE, Ensminger ME, Chisolm MS, & McGinty EE (2017). Social Stigma Toward Persons With Prescription Opioid Use Disorder: Associations With Public Support for Punitive and Public Health-Oriented Policies. Psychiatr Serv, 68(5), 462–469. doi: 10.1176/appi.ps.201600056 [DOI] [PubMed] [Google Scholar]
- Kulesza M, Matsuda M, Ramirez JJ, Werntz AJ, Teachman BA, & Lindgren KP (2016). Towards greater understanding of addiction stigma: Intersectionality with race/ethnicity and gender. Drug Alcohol Depend, 169(Supplement C), 85–91. doi: 10.1016/j.drugalcdep.2016.10.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Clainche C, & Wittwer J (2015). Responsibility‐Sensitive Fairness in Health Financing: Judgments in Four European Countries. Health Economics, 24(4), 470–480. [DOI] [PubMed] [Google Scholar]
- Luoma JB, O’Hair AK, Kohlenberg BS, Hayes SC, & Fletcher L (2010). The development and psychometric properties of a new measure of perceived stigma toward substance users. Substance Use & Misuse, 45(1-2), 47–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Ponicki W, Smith N, Rivera-Aguirre A, Davis CS, Fink DS, … Cerdá M. (2019). Prescription drug monitoring programs operational characteristics and fatal heroin poisoning. International Journal of Drug Policy, 74, 174–180. doi: 10.1016/j.drugpo.2019.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason W, & Suri S (2012). Conducting behavioral research on Amazon’s Mechanical Turk. Behav Res Methods, 44(1), 1–23. doi: 10.3758/s13428-011-0124-6 [DOI] [PubMed] [Google Scholar]
- McGinty E, Pescosolido B, Kennedy-Hendricks A, & Barry CL (2017). Communication Strategies to Counter Stigma and Improve Mental Illness and Substance Use Disorder Policy. Psychiatric Services, appi. ps. 201700076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA. (2018a). Results from the 2017 National Survey on Drug Use and Health. Table 1.27A. Retrieved from https://www.samhsa.gov/data/nsduh/reports-detailed-tables-2017-NSDUH
- SAMHSA. (2018b). Results from the 2017 National Survey on Drug Use and Health. Table 6.54B. Retrieved from https://www.samhsa.gov/data/nsduh/reports-detailed-tables-2017-NSDUH
- Sattler S, Escande A, Racine E, & Göritz AS (2017). Public Stigma Toward People With Drug Addiction: A Factorial Survey. Journal of Studies on Alcohol and Drugs, 78(3), 415–425. [DOI] [PubMed] [Google Scholar]
- Skinner N, Feather NT, Freeman T, & Roche A (2007). Stigma and Discrimination in Health‐Care Provision to Drug Users: The Role of Values, Affect, and Deservingness Judgments. Journal of Applied Social Psychology, 37(1), 163–186. [Google Scholar]
- Sorsdahl K, Stein DJ, & Myers B (2012). Negative attributions towards people with substance use disorders in South Africa: variation across substances and by gender. BMC Psychiatry, 12, 101. doi: 10.1186/1471-244x-12-101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Star SM, & Van den Berg B (2011). Individual responsibility and health-risk behaviour: A contingent valuation study from the ex ante societal perspective. Health Policy, 101(3), 300–311. [DOI] [PubMed] [Google Scholar]
- Weeks C, & Stenstrom DM (2020). Stigmatization of opioid addiction based on prescription, sex and age. Addict Behav, 108, 106469. doi: 10.1016/j.addbeh.2020.106469 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


