Abstract
Objective: The Coronavirus Disease 2019 (COVID-19) pandemic is a public health emergency of international concern and poses a challenge to people’s psychological resilience. Students are reported to have greater psychological impacts from COVID-19. This study aimed to survey international students to better understand their traumatic effects and psychological reactions from COVID-19, to develop evidence-driven strategies to reduce adverse psychological impact during the pandemic.
Method: We conducted an online survey that collected information on the demographics, economic conditions, academic conditions, and health statuses of native Chinese students attending university in the U.S. Psychological impact was assessed by the Post-traumatic Stress Disorder (PTSD) Checklist Civilian Version (PCL-C) and mental health status was assessed by the Depression, Anxiety, and Stress Scale.
Results: This study included 261 Chinese international students. In total, 37.5% of respondents’ PTSD PCL-C scores measured as moderate or severe. International students who were currently in China facing job-hunting or planning to continue studying abroad, severe economic pressure, and poor self-rated health status were significantly associated with greater PTSD PCL-C scores and higher levels of stress, anxiety, and depression.
Conclusion: During the COVID-19 pandemic, more than one-third of the respondents rated their PTSD PCL-C score as moderate-to-severe and nearly half of them reported moderate-to-severe anxiety. Our findings identify factors such as future academic plan, economic pressure, and health status are associated with higher levels of psychological impact and worse mental health status. These should receive attention and psychological interventions should be implemented to improve the mental health of international students during the COVID-19 pandemic.
Keywords: COVID-19, international students, psychological impact, DASS-21, PCL-C
1. INTRODUCTION
The rapidly spreading, ongoing, and worldwide Coronavirus Disease 2019 (COVID-19) pandemic has become a global public health emergency since it broke out in December 2019 [1–3]. Previous research has revealed that the COVID-19 pandemic has caused many overwhelming stressors, such as loss of employment; death of family members, friends, or colleagues; financial insecurity; and isolation from others [4]. It is well known that stressful events such as COVID-19 and other traumas may have a significant impact on mental health and may result in conditions such as Post-traumatic Stress Disorder (PTSD) and other psychological symptoms [5–7]. Mamun et al. [8] reported that these psychiatric sufferings also account for about 90% of the global suicide occurrences in extreme cases. As compared to the general population [6,7], Wang et al.’s study of 1738 respondents from 190 Chinese cities found that respondents aged 12–21.4 years and were students demonstrated a higher psychological impact from COVID-19 than those who were employed, which may be due to prolonged school closure, requiring online education support, and uncertainty about examinations and matriculation arrangements. Further, students were also likely to experience fear of becoming ill or dying themselves, feelings of helplessness, and stigma [9,10]. Compared to local students, international students are facing more impediments in maintaining their mental health under the COVID-19 pandemic and beyond. For example, the pandemic may have put them in a more isolated position abroad, with less access to public resources due to monetary, informational, language, or cultural barriers. Besides, some campuses were closed without considering that many international students do not have a residence outside those campuses, nor do they have access to a safe return to their home countries due to closed borders, reduced numbers of international flights, and potential exposure to COVID-19 during travel [11]. Based on these considerations, our study evaluates and identifies traumatic factors related to COVID-19 that contribute to psychological stress. These factors should become central concerns for government agencies and healthcare professionals to help international students get through this period of difficulty.
2. MATERIALS AND METHODS
The survey was completed on the Chinese Star Survey website. A snowball sampling strategy, focused on recruiting native Chinese students who are studying at U.S. universities during the epidemic of COVID-19, was utilized. The relevant smartphone link was sent by an instructor via WeChat to an international student group consisting of native Chinese students who are studying at U.S. universities. According to our preliminary survey and based on the primary outcome of Depression, Anxiety, and Stress Scale (DASS) scores, we calculated the size of the sample, and 253 respondents were required, assuming a two-sided Type I error (α) of 0.05 and a power of 80%. Potential loss during follow-up or because of drop out was expected, therefore a total of 291 respondents were enrolled in this study. Of the 291 Chinese international students, 274 completed the questionnaire. However, 13 of these were eliminated from the study owing to illogical answers, such as submitting the same answers to all questions or reporting zero at each instance. Therefore, 261 were considered effective. All questionnaires were anonymous and could be completed in 5 min. Questions gathered information about students’ demographics, economic conditions, academic conditions, and health status. We used the DASS-21 and the PTSD Check List-Civilian Version (PCL-C). Ethical approval for this study was granted by the Human Research Ethical Committee. Before the start of the investigation, the instructor provided the participants with the details about the research, and participants gave their electronic informed consent by signing the first page of the survey.
2.1. Measurements
2.1.1. Depression, anxiety, and stress scale-21
This 21-item scale allows for the simultaneous assessment of the three emotional states of DAS. It is easy to apply in both clinical and non-clinical settings, and suitable for use in different age groups, as well as for medical students [12]. Each item has a 4-point Likert scale. The rating choices are “never applied to oneself” (0 points), “some degree/some of the time” (1 point), “considerable degree/a good part of the time” (2 points), and “very much/most of the time” (3 points). For depression, the measures were normal (0–9 points), mild (10–13 points), moderate (14–20 points), severe (21–27 points), and extremely severe (28+ points). For anxiety, the measures were normal (0–7 points), mild (8–9 points), moderate (10–14 points), severe (15–19 points), and extremely severe (20+ points). For stress, the measures were normal (0–14 points), mild (15–18 points), moderate (19–25 points), severe (26–33 points), and extremely severe (34+ points). Each subscale’s score is the doubled sum of the seven items. A depression score >9, anxiety score >7, and stress score >14 were considered to be symptomatic [13]. Cronbach’s alpha value is 0.76.
2.1.2. PTSD check list-civilian version
Students’ PTSD was assessed using the PCL-C. The PCL-C is a 17-item self-report that can be used for PTSD screening, diagnosis, or symptom monitoring. Developed by Weathers et al. [14], the civilian version can be applied generally to any traumatic event and is easily modifiable to fit specific time frames or events. It is self-administered and requires respondents to rate how often they have been bothered by PTSD symptoms using a 5-point scale (from 1 = not at all to 5 = extremely). The total scores range from 17 to 85. Scores of 38 or higher indicate the presence of PTSD [15,16]. This scale is valid and reliable, and the instrument has been translated into Mandarin [17]. Cronbach’s alpha value is 0.88.
2.2. Statistical Analysis
Statistical Package for the Social Sciences (SPSS) 20.0 statistical software (SPSS Inc., Chicago, IL, USA) was used for data analysis. A Chi-square test was used to analyze the categorical data of Chinese international students. The scores for the PTSD and DASS subscales were expressed as means and standard deviations. Percentages of responses were calculated according to the number of responses per question concerning the total number of respondents. One-way analysis of variance followed by Bonferroni correction was used for multiple comparisons. We used linear regressions to calculate the univariate associations between sociodemographic characteristics, health status, academic condition, and the PTSD score, as well as the subscales of the DASS. All tests were two-tailed, with a significance level of p < 0.05.
3. RESULTS
3.1. Demographic Characteristics and their Association with Psychological Impact
The psychological impact of the COVID-19 pandemic, measured using the PTSD PCL-C scale, revealed a sample mean score of 33.50 (SD = 10.90). Of all respondents, 98 (37.5%) reported a moderate or severe psychological impact (score > 38). Respondents’ DAS levels were measured using the DASS 21-item scale. For the depression subscale, 157 (60.2%) were considered to have a normal score (score: 0–9); 54 (20.7%) were considered to suffer from mild depression (score: 10–12); 50 (19.2%) were considered to suffer from moderate depression (score: 13–20); none of them were considered to suffer from severe or extremely severe depression (score: 21–42). For the anxiety subscale, 132 (50.6%) were considered to have a normal score (score: 0–6); 30 (11.5%) were considered to suffer from mild anxiety (score: 7–9); 69 (26.4%) were considered to suffer from moderate anxiety (score: 10–14); and 30 (11.5%) were considered to suffer from severe or extremely severe anxiety (score: 15–42). For the stress subscale, 164 (62.8%) were considered to have a normal score (score: 0–10); 79 (30.3%) were considered to suffer from mild stress (score: 11–18); 18 (6.9%) were considered to suffer from moderate stress (score: 19–26); and none of them were considered to suffer from severe or extremely severe stress (score: 27–42). Demographic characteristics are presented in Table 1. Aged 20–23 years was significantly associated with higher scores in the PTSD PCL-C [B = 0.20, 95% Confidence Interval (CI): 1.20–5.11], DASS depression subscale (B = 0.32, 95% CI: 1.41–2.89), DASS anxiety subscale (B = 0.19, 95% CI: 0.55–2.43), and DASS stress subscale (B = 0.14, 95% CI: 0.15–2.41). The female gender was significantly associated with lower scores on the DASS anxiety subscale (B = −4.18, 95% CI: −3.87 to −1.39) and DASS stress subscale (B = −0.34, 95% CI: −5.72 to −2.85). Four (1.5%) of the international students self-diagnosed or their relatives confirmed infections with COVID-19, which was not associated with the PTSD PCL-C and DASS subscale scores.
Table 1.
Association between different variables and the PTSD PCL-C of the 2019 coronavirus disease (COVID-19) outbreak as well as adverse mental health status during the epidemic
| Variables | N (%) | PTSD PCL-C | Depression | Anxiety | Stress | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| R-Squared (R2) | Adjusted R-squared (AR2) | Beta (95% confidence interval) B (95% CI) | R2 | AR2 | B (95% CI) | R2 | AR2 | B (95% CI) | R2 | AR2 | B (95% CI) | ||
| Age | |||||||||||||
| ≤19 | 132 (50.6) | 0.043 | 0.036 | Reference | 0.231 | 0.225 | Reference | 0.042 | 0.035 | Reference | 0.015 | 0.018 | Reference |
| 20–23 | 88 (33.7) | 0.20* (1.20–5.11) | 0.32* (1.41–2.89) | 0.19* (0.55–2.43) | 0.14* (0.15–2.41) | ||||||||
| >23 | 41 (15.7) | 0.11 (−0.16 to 3.45) | 0.43* (1.99–3.36) | 0.11 (−0.07 to 1.67) | 0.11 (−0.13 to 1.96) | ||||||||
| Gender | |||||||||||||
| Male | 122 (46.7) | 0.001 | −0.003 | Reference | 0.000 | −0.004 | Reference | 0.063 | 0.060 | Reference | 0.118 | 0.114 | Reference |
| Female | 139 (53.3) | −0.46 (−3.29 to 2.05) | 0.00 (−1.13 to 1.13) | −4.18 * (−3.87 to −1.39) | −0.34* (−5.72 to −2.85) | ||||||||
| Self-diagnosed or relatives confirmed infection with COVID-19 | |||||||||||||
| No | 257 (98.5) | 0.004 | 0.000 | Reference | 0.011 | 0.007 | Reference | 0.007 | 0.003 | Reference | 0.014 | 0.010 | Reference |
| Yes | 4 (1.5) | 0.06 (−2.90 to 9.30) | −0.11 (−4.81 to 0.36) | 0.08 (−0.95 to 4.90) | 0.12 (−0.10 to 6.86) | ||||||||
| Place of residence | |||||||||||||
| China | 125 (47.8) | 0.023 | 0.019 | Reference | 0.049 | 0.045 | Reference | 0.017 | 0.013 | Reference | 0.001 | −0.003 | Reference |
| The United States | 136 (52.1) | −0.15* (−5.95 to −0.68) | −0.22* (−3.15 to −0.95) | −0.13* (−2.62 to −0.08) | −0.04 (−1.98 to 1.07) | ||||||||
| Health condition | |||||||||||||
| Health | 121 (46.3) | 0.139 | 0.132 | Reference | 0.15 | 0.143 | Reference | 0.125 | 0.119 | Reference | 0.067 | 0.060 | Reference |
| Average | 103 (39.4) | 0.24* (1.95–5.47) | 0.29* (1.16–2.64) | 0.12* (0.05–1.75) | 0.14* (0.18–2.28) | ||||||||
| Poor/very poor | 37 (14.1) | 0.32* (3.17–6.79) | 0.29* (1.21–2.74) | 0.35* (1.77–3.52) | 0.24* (1.06–3.22) | ||||||||
| Economic pressure | |||||||||||||
| None/little | 119 (45.5) | 0.347 | 0.342 | Reference | 0.101 | 0.094 | Reference | 0.141 | 0.135 | Reference | 0.059 | 0.051 | Reference |
| Moderate | 94 (36) | 0.44* (5.07–8.18) | 0.15* (0.18–1.73) | 0.18* (0.42–2.14) | 0.09 (−0.33 to 1.81) | ||||||||
| Severe | 48 (18.3) | 0.52* (6.06–9.02) | 0.32* (1.23–2.71) | 0.38* (1.82–3.45) | 0.25* (1.05–3.08) | ||||||||
| Academic plan | |||||||||||||
| Not sure | 132 (50.5) | 0.045 | 0.037 | Reference | 0.272 | 0.266 | Reference | 0.101 | 0.094 | Reference | 0.055 | 0.047 | Reference |
| Continue studying abroad | 95 (36.3) | 0.20* (1.29–5.24) | 0.42* (2.17–3.63) | 0.32* (1.59–3.43) | 0.23* (1.06–3.31) | ||||||||
| Go back to China | 34 (13) | 0.09 (−0.45 to 3.27) | 0.35* (1.63–3.01) | 0.04 (−0.54 to 1.19) | 0.06 (−0.56 to 1.57) | ||||||||
p < 0.05.
3.2. Current Location of International Students and its Association with Psychological Impact
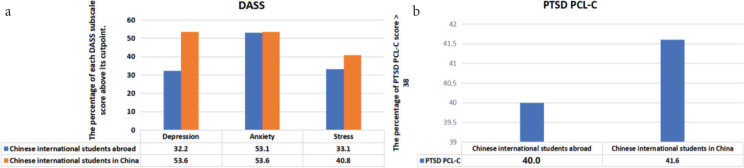
Of all respondents, 125 international students (47.9%) who study in abroad were currently in China due to the pandemic and 136 international students (52.1%) were still in the U.S. Being in the U.S. was significantly associated with lowers scores on the PTSD PCL-C (31.91 ± 12.0, p = 1.013, B = −0.15, 95% CI: −5.95 to −0.68), DASS depression subscale (B = −0.22, 95% CI: −3.15 to −0.95), and DASS anxiety subscale (7.48 ± 5.3, p = 0.038, B = −0.13, 95% CI: −2.62 to −0.08). Though international students in the U.S. also showed lower scores on the DASS stress subscale (8.72 ± 5.9, p = 0.559, B = −0.04, 95% CI: −1.98 to −0.07), there was no statistically significant difference when compared to the international students in China (Tables 1 and 2). We found that the percentage of DASS depression, DASS anxiety, and DASS stress subscale scores above their cutoff point among international students in China were higher than those among international students in the U.S. (53.6% vs. 32.2%, 53.6% vs. 53.1%, and 40.8% vs. 33.1%, respectively; Figure 1a), and the percentage of PTSD PCL-C scores above 38 among international students in China was larger than that among international students in the U.S. (41.6% vs. 40.0%; Figure 1b).
Table 2.
The basic information between Chinese international students in China and Chinese international students abroad
| Chinese International students in China | Chinese International students abroad | t | p | |||
|---|---|---|---|---|---|---|
| Age | 20.14 ± 2.9 | 20.26 ± 2.8 | −0.125 | 0.715 | ||
| Gender | N | % | N | % | – | 0.103 |
| Female | 60 | 48 | 79 | 58.1 | – | – |
| Male | 65 | 52 | 57 | 41.9 | – | – |
| DASS-21 | – | – | ||||
| Depression | 8.95 ± 4.5 | 6.90 ± 4.6 | 3.657 | <0.001 | ||
| Anxiety | 8.82 ± 5.1 | 7.48 ± 5.3 | 2.089 | 0.038 | ||
| Stress | 9.18 ± 6.6 | 8.72 ± 5.9 | 0.585 | 0.559 | ||
| PTSD PCL-C | 35.22 ± 9.3 | 31.91 ± 12.0 | 2.504 | 0.013 | ||
Figure 1.
(a) The percentage of each DASS subscale score above its cutpoint. Depression > 9; Anxiety > 7; Stress > 14. (b) The percentage of PTSD PCL-C score > 38.
3.3. Health Status and Psychological Impact
Of all the respondents, 46.3% reported good health status. Poor or very poor self-rated health status was significantly associated with a higher PTSD score (B = 0.32, 95% CI: 3.17–6.79), and higher DASS stress subscale (B = 0.24, 95% CI: 1.06–3.22), DASS anxiety subscale (B = 0.35, 95% CI: 1.77–3.52), and DASS depression subscale (B = 0.29, 95% CI: 1.21–2.74) scores as compared to those with good self-rated health status (Table 1).
3.4. Economic Pressure and Future Academic Plan and their Association with Psychological Impact
For all the international students, those who reported severe economic pressure reported significantly higher scores on the PTSD PCL-C score (B = 0.52, 95% CI: 6.06–9.02), DASS stress (B = 0.25, 95% CI: 1.05–3.08), DASS anxiety (B = 0.38, 95% CI: 1.82–3.45) and DASS depression (B = 0.32, 95% CI: 1.23–2.71) subscales. Planning to continue studying abroad was also significantly associated with higher scores on the PTSD PCL-C score (B = 0.20, 95% CI: 1.29–5.24), DASS stress (B = 0.23, 95% CI: 1.06–3.31), DASS anxiety (B = 0.32, 95% CI: 1.59–3.43) and DASS depression (B = 0.42, 95% CI: 2.17–3.63) subscales (Table 1).
4. DISCUSSION
This may be one of the first studies to examine the psychological impact on international students during the COVID-19 pandemic. Our results found that 37.5% of respondents rated the psychological impact of the outbreak as moderate or severe. Among them, 52.1% were students who currently stay abroad; 39.8% of respondents reported depressive symptoms >9; 49.4% of respondents reported anxiety symptoms >7; and 34.1% reported stress levels >14. The percentage of each psychological symptom score which was above its cut-off point among the students currently in China was higher than those among the students still in the U.S.
The difference between PTSD and DASS-21 scores may be because the PTSD Scale assesses the psychological impact after an event. The COVID-19 pandemic has disrupted the lives of students in different ways, depending not only on their level and course of study but also on the point they have reached in their programs, such as those transitioning from secondary to tertiary education, or from tertiary education to employment. However, respondents from different nationalities or ethnicities may manifest psychological symptoms differently or may be less likely to accept a negative mood [18]. In our study, we investigated an international student group of Chinese natives who are studying in the U.S. The percentage of students that chose to go back to China during the outbreak of COVID-19 was 47.8%, while 52.1% chose to stay abroad. Those who returned home to China reported more serious psychological symptoms, and their symptoms of DAS were more obvious than those of students who were still in the U.S. One possible reason for this may be that besides COVID-19 leading to anxiety, COVID-19-related stressors may also cause anxiety, such as the disintegration of future plans, decreased communication with teachers, economic pressure, academic delays, and restrictions that are aimed toward students from China returning to U.S. universities. These stressors were positively associated with the level of negative psychological symptoms experienced during the pandemic [19]. Currently, according to press reports, international students’ chances of getting jobs in the U.S. after graduation are limited. This comes on the heels of the COVID-19 pandemic, which was already projected to reduce international student enrollment by up to 25% [20]. Moreover, during the pandemic, many international students have been worrying about long-term disadvantages when they move to another level of study or enter the labor market. These concerns may be why international students who are aged 20–23 years and facing the pressure of job-hunting or planning to continue studying abroad were significantly associated with higher scores on the DASS depression, DASS anxiety, and DASS stress subscales. Apart from academic pressures, the traumatic economic effects brought on by COVID-19 may also harm students’ mental wellbeing. For the Chinese international students who come from middle-class families, extracurricular work may relieve their financial pressure to a certain extent. However, many shops and restaurants closed due to COVID-19; limited financial resources might become one of the things that produce the most anxiety. Based on a systematic review, 31 global studies exhibit a positive association between economic recession and increased suicide rates [21]. In our study, those who reported severe economic pressure were significantly associated with higher scores on the DASS stress, DASS anxiety, and DASS depression subscales. The results of our study might provide vital guidance for the government to apply supplementary policies to help international students who are experiencing elevated stress, anxiety, and depression. Institutions and parents should step in to aid these students and form a stable emotional support system during such a difficult time [22]. Although negative emotions will have adverse effects on international students’ psychology, the majority of mental disorders following COVID-19 such as sadness, anxiety, fear, anger, paranoia, and short-term adjustment issues and long-term adaptation to the uncertain future may be “reactive” in nature, which is transient rather than persistent. It is necessary to take effective measures in time to improve international students’ mental health [23]. First, our data suggest that education authorities need to develop online portals and web-based applications to deliver lectures or other teaching activities [24]. As young people are receptive to smartphone applications [25], health authorities could consider providing online or smartphone-based psychoeducation and psychological interventions that will also reduce the risk of virus transmission by forgoing face-to-face therapy. Moreover, due to the limitations of online teachings, such as time difference and lack of interactive communication in the classroom, special policies that provide more choices for international students are extremely valuable during this period, such as Cornell University’s Study Away option. In this policy, international students at Cornell could choose educational institutions in their home country; such alternatives provided students with a different approach than online meetings. In this way, Chinese students can not only continue their studies in their home country, but also, to a large extent, avoid the risk of infection during travel and contact with people. Second, health authorities need to identify the immediate psychological needs of international students presenting with psychological symptoms during the pandemic. Our results reveal that international students presenting with poor self-rated health statuses reported higher PTSD levels and higher levels of stress, anxiety, and depression. Health professionals should take the opportunity to provide resources for psychological support and interventions for those who present with poor health status. Further, health authorities need to provide accurate health information during the pandemic to reduce the spread of misinformation [26,27]. Third, Chinese international students who are abroad may face unfair treatment and be discriminated against in some countries, being viewed as possible COVID-19 carriers. This misconception causes public fear, alienation, and discrimination, which may also lead to mental health problems such as denial, stress, anxiety, and fear [28]. As a result, it may be better for the World Health Organization and governments worldwide to minimize the possibility of discrimination against certain groups of people regarding the origin of COVID-19 by providing cognitive behavior therapy and mindfulness-based therapy [22]. Fourth, colleges and universities should help college students establish proper career ideals and re-plan their career goals. Colleges and universities at home and abroad should establish a new type of cooperative employment work model, implement more flexible employment measures for graduate students, and provide them with diversified job opportunities to minimize the pandemic’s negative impact on international students’ economic concerns.
This study has several limitations. First, as the study focused on Chinese international students, the results may not apply to other adults or the general population. Second, personality and coping styles of different participants, which may influence the results, were not measured in this study. Third, due to the constant changes that occur in both the crisis and in international relations, our research only represents the mental status of students in this particular period. Fourth, we did not adjust for baseline depression as a covariate. The present sample is also small and was limited to a convenience sample. And the snowball sampling method is susceptible to sampling bias. Since participants are chosen by individuals who have already been selected, it is possible that all of the participants will share certain characteristics or traits. Finally, socioeconomic status varies over time in this age range, and could not be assessed in the present study.
5. CONCLUSION
During the COVID-19 pandemic in China, more than one-third of the respondents rated their psychological impact as moderate-to-severe, and nearly half of them reported moderate-to-severe anxiety. Students currently stayed in China who were at the age of graduation with facing job-hunting or planning to continue studying abroad, with severe economic pressure, and poor self-rated health status were associated with a greater psychological impact from the outbreak and higher levels of stress, anxiety, and depression. In the future, the COVID-19 epidemic may continue to affect people’s work and life, and the results of this study may assist in identifying Chinese international students with mental health problems so that they can be targeted for appropriate mental health interventions.
ACKNOWLEDGMENTS
The authors would like to thank Gang Zhu, MD, Ph.D., from the Department of Psychology, the first affiliated hospital of China Medical University, Shenyang, China for his discussion and advice on this study. Also the authors would like to thank the Northeast Yucai Oxford International Senior High School (NYO) and STF International English Training School for their help with the study.
Footnotes
Data availability statement: The data that supported the findings of this study are available from the corresponding author (Junchao Zhu), upon reasonable request.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
BJS and YLZ designed the current study. BJS, YLZ and JCZ collected data. BJS and JCZ analyzed the data. BJS and YLZ wrote the manuscript. All the authors read and approved the final manuscript.
REFERENCES
- [1].Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395:e37–e8. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55 doi: 10.1016/j.ijantimicag.2020.105924. 105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395:689–97. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Shader RI. COVID-19 and depression. Clin Ther. 2020;42:962–3. doi: 10.1016/j.clinthera.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Tan W, Hao F, McIntyre RS, Jiang L, Jiang X, Zhang L, et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuro immunity prevention measures of Chinese workforce. Brain Behav Immun. 2020;87:84–92. doi: 10.1016/j.bbi.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. 2020;87:100–6. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Mamun MA, Siddique AB, Sikder MT, Griffiths MD. Student suicide risk and gender: a retrospective study from Bangladeshi press reports. Int J Mental Health Addic. 2020 doi: 10.1007/s11469-020-00267-3. [DOI] [Google Scholar]
- [9].Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40–8. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Ng QX, De Deyn MLZQ, Lim DY, Chan HW, Yeo WS. The wounded healer: a narrative review of the mental health effects of the COVID-19 pandemic on healthcare workers. Asian J Psychiatr. 2020;54 doi: 10.1016/j.ajp.2020.102258. 102258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Tran BX, Ha GH, Nguyen LH, Vu GT, Hoang MT, Le HT, et al. Studies of novel coronavirus disease 19 (COVID-19) pandemic: a global analysis of literature. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17114095. 4095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Vignola RCB, Tucci AM. Adaptation and validation of the depression, anxiety and stress scale (DASS) to Brazilian Portuguese. J Affect Disord. 2014;155:104–9. doi: 10.1016/j.jad.2013.10.031. [DOI] [PubMed] [Google Scholar]
- [13].Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the beck depression and anxiety inventories. Behav Res Ther. 1995;33:335–43. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- [14].Weathers F, Huska J, Keane T. PTSD Checklist (PCL) Washington, DC: National Center for PTSD, US Department of Veterans Affairs; 1991. [Google Scholar]
- [15].Dobie DJ, Kivlahan DR, Maynard C, Bush KR, McFall M, Epler AJ, et al. Screening for post-traumatic stress disorder in female Veteran’s Affairs patients: validation of the PTSD checklist. Gen Hosp Psychiatry. 2002;24:367–74. doi: 10.1016/s0163-8343(02)00207-4. [DOI] [PubMed] [Google Scholar]
- [16].Harrington T, Newman E. The psychometric utility of two self-report measures of PTSD among women substance users. Addict Behav. 2007;32:2788–98. doi: 10.1016/j.addbeh.2007.04.016. [DOI] [PubMed] [Google Scholar]
- [17].Jin Y, Xu J, Liu H, Liu D. Posttraumatic stress disorder and posttraumatic growth among adult survivors of Wenchuan earthquake after 1 year: prevalence and correlates. Arch Psychiatr Nurs. 2014;28:67–73. doi: 10.1016/j.apnu.2013.10.010. [DOI] [PubMed] [Google Scholar]
- [18].Tan BYQ, Chew NWS, Lee GKH, Jing M, Goh Y, Yeo LLL, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020;173:317–20. doi: 10.7326/M20-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. 112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Foreign Student Enrollment At U.S. Universities May Plummet This Fall. 2020 Available from: https://www.forbes.com/sites/prestoncooper2/2020/06/01/foreign-student-enrollment-at-us-universities-may-plummet-this-fall/#e3524eaa7685.
- [21].Oyesanya M, Lopez-Morinigo J, Dutta R. Systematic review of suicide in economic recession. World J Psychiatry. 2015;5:243–54. doi: 10.5498/wjp.v5.i2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Ho CS, Chee CY, Ho RC. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann Acad Med Singapore. 2020;49:155–60. https://pubmed.ncbi.nlm.nih.gov/32200399/ [PubMed] [Google Scholar]
- [23].Ng QX, Lim DY, Chee KT. Not all trauma is the same. Proc Natl Acad Sci U S A. 2020 doi: 10.1073/pnas.2013204117. 202013204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Zhang MWB, Ho CSH, Ho RCM. Methodology of development and students’ perceptions of a psychiatry educational smartphone application. Technol Health Care. 2014;22:847–55. doi: 10.3233/THC-140861. [DOI] [PubMed] [Google Scholar]
- [25].Do TTT, Le MD, Van Nguyen T, Tran BX, Le HT, Nguyen HD, et al. Receptiveness and preferences of health-related smartphone applications among Vietnamese youth and young adults. BMC Public Health. 2018;18:764. doi: 10.1186/s12889-018-5641-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Rubin GJ, Wessely S. The psychological effects of quarantining a city. BMJ. 2020;368:m313. doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- [27].Lee JQ, Loke W, Ng QX. The role of family physicians in a pandemic: a blueprint. Healthcare (Basel) 2020;8:198. doi: 10.3390/healthcare8030198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7:e14. doi: 10.1016/S2215-0366(20)30047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]