Abstract
Introduction
The SINGER pilot randomized controlled trial aims to examine the feasibility and acceptability of the Finnish Geriatric Intervention Study (FINGER) multi‐domain lifestyle interventions compared to Singaporean adaptations.
Methods
Seventy elderly participants were recruited and randomized into FINGER (n = 36) or SINGER (n = 34) interventions; involving physical exercise, cognitive training, diet, and vascular risk factors management, for 6 months.
Results
Both intervention groups were equally feasible and acceptable with participants completing at least 80% of the interventions. Body strength improved in both groups (Pupper body = .04, P lower body = .06, P core = .05). More participants in the SINGER group attained good blood pressure control at month‐6 compared to FINGER (41% vs 19%; P = .06).
Discussion
This study is the first to compare the feasibility of multi‐domain interventions adapted to local culture with the FINGER interventions. The findings will be utilized for a larger study to provide evidence for the efficacy of multi‐domain lifestyle interventions in preventing cognitive decline.
Keywords: cognitive impairment, dementia, feasibility, intervention, lifestyle, randomized controlled trial
1. INTRODUCTION
The prevalence of cognitive impairment and dementia is rising globally, 1 with Asia having the most rapidly ageing societies worldwide. Consequently, there will be a marked increase in the prevalence of cognitive impairment which is associated with poor long‐term health outcomes, such as hospitalization and dependency in daily activities. 2 In Singapore, a multicultural Asian country, dementia prevalence is projected to increase exponentially due to a rapidly ageing population from 12.4% above the age of 65 in 2019 to 33.3% in 2050. 3 , 4 Such an increase will put an enormous strain on societies. Therefore, the challenge lies in the development of safe and effective interventions that can prevent and reduce cognitive impairment.
In recent years, there has been a shift from pharmacological treatment after symptom onset to non‐pharmacological interventions that may help prevent and delay the emergence of symptoms. Compared to pharmacological interventions, non‐pharmacological interventions are less expensive and invasive with fewer side effects. 5 Several promising non‐pharmacological multi‐domain interventions have been studied, 6 , 7 , 8 yet not all have yielded positive efficacy outcomes. Hence, illustrating the importance of the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER) trial, which has produced promising results. 8 The FINGER study, a population‐based 2‐year randomized controlled trial (RCT), showed that a multi‐domain lifestyle intervention of physical activity, nutritional advice, cognitive training, social activities and vascular risk factors management slowed cognitive decline in older adults at increased risk of dementia, suggesting a promising role of such interventions in reducing dementia risk which could halt the worldwide increase of affected people. As a result, World‐Wide FINGERS (WW‐FINGERS) was established in 2017 as the first global network of multi‐domain lifestyle intervention trials for dementia prevention. WW‐FINGERS aims to adapt, test, and optimize the FINGER model in different geographical, cultural, and economic settings. 9
As part of the WW‐FINGERS initiative, the SINgapore GERiatric intervention study to reduce physical frailty and cognitive decline (SINGER) was designed as a proof‐of‐concept pilot study testing a series of multi‐domain interventions adapted from the original FINGER study. This trial will help determine the cultural feasibility and practicality of the adaptations in a multi‐ethnic Asian community, as a precursor to expand into a large‐scale community‐based RCT to determine the efficacy of such interventions in delaying cognitive decline and preventing dementia. Therefore, the present study sought to primarily evaluate the feasibility of the SINGER interventions compared to the original FINGER interventions. Additionally, as a secondary aim, the study evaluated the efficacy of the SINGER interventions compared to the FINGER interventions. We hypothesized that the individual arms in the locally modified SINGER interventions will be more feasible than, and equally effective to the FINGER multi‐domain lifestyle interventions in Singaporean older adults.
RESEARCH IN CONTEXT
Systematic review: We reviewed the literature using PubMed, PsychInfo, Google Scholar, and references of relevant articles on the effect of multi‐domain lifestyle interventions for prevention of dementia. Mixed results from non‐pharmacological multi‐domain interventions on efficacy outcomes have been reported. Nonetheless, the Finnish Geriatric Intervention Study (FINGER) multi‐domain lifestyle interventions study demonstrated the promising role of such interventions in improving cognition and reducing dementia risk. Results on cultural adaptation have not been established.
Interpretation: The SINGER intervention demonstrated good feasibility compared to FINGER. More subjects in SINGER completed >50% of cognitive training sessions compared to FINGER (81% vs 58%). We also found a trend towards good BP outcome in more subjects in SINGER, suggesting the effectiveness of close monitoring of vascular risk factors.
Future directions: The findings warrant a large‐scale study to provide robust evidence for long‐term efficacy and practicality of multi‐domain lifestyle interventions in preventing cognitive decline among community‐dwelling elderly.
2. METHODS
2.1. Study design and participants
The SINGER pilot study is a 6‐month RCT conducted at the National University Hospital in Singapore. Participants were recruited from memory clinic and the community. Inclusion criteria were: ≥65 of age, literate in either English or Mandarin Chinese, and mild‐to‐moderate frailty as defined by a Physical Performance Test (PPT) score of 17 to 32. 10 Those with severe medical conditions (eg, cardiopulmonary disease, cancer) which precluded them from performing exercise sessions, or dementia, were excluded from the study. Research staff evaluating cognitive outcome measures were blinded to intervention grouping. Ethics approval was obtained from the National Healthcare Group Domain‐Specific Review Board.
2.2. Randomization
After obtaining informed consent, participants were randomized into the FINGER intervention or the SINGER intervention in a 1:1 ratio. Randomization was computer‐generated by random allocation sequence.
2.3. Procedures
All participants completed screening and outcome measures at baseline, month‐3 and month‐6 (Figure 1). The study team attended to all participants at all 3 time points for a detailed medical history and examination. Figure 2 illustrates the COVID‐19 pandemic's impact on the study timeline.
FIGURE 1.

Recruitment flowchart
FIGURE 2.
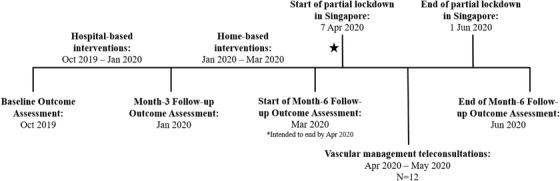
Timeline of study period affected by the COVID‐19 pandemic
2.3.1. Vascular profile
Vascular risk profile was obtained for all subjects through clinical interview, physical examination, and review of laboratory and medical records. This included hypertension, hyperlipidemia, diabetes mellitus, defined as previous history of the condition or the use of antihypertensive, lipid‐lowering, anti‐diabetic medication respectively; heart disease, defined as a previous diagnosis of myocardial infarction, congestive heart failure, atrial fibrillation, or intervention procedures such as angioplasty, or stenting; and history of smoking (ever/never).
2.3.2. Lifestyle indicators
Participants also provided self‐reported information on lifestyle factors at baseline. Level of independence was measured on a five‐point Likert scale, and subjective memory complaints was measured on a yes/no scale. Previous diagnosis of major depression and/or other major psychiatric disorders were also recorded and reported.
Lifestyle interventions were conducted in two blocks – the first 3 months comprised of hospital‐based interventions, and the next 3 months comprised of home‐based interventions where participants continued their training sessions at home. The SINGER group received a Singaporean adaptation of the lifestyle interventions (Table 1). More details of the individual interventions can be found in Appendix A. Interventions and outcome measures were conducted in the participant's primary language.
TABLE 1.
Main differences between FINGER and SINGER interventions
| FINGER | SINGER | |
|---|---|---|
| Cognitive training | Computerized cognitive training | Pen‐and‐paper cognitive training |
| Diet | Healthy Nordic diet, adapted from the Mediterranean diet | Locally modified diet consisting of Asian fruit and vegetables |
| Physical exercise | Unsupervised aerobic sessions, recommended 5 times a week for 45‐60 minutes during hospital‐based training. | Supervised aerobic sessions twice weekly for 30 minutes during hospital‐based training. |
| Supervised strength sessions, recommended twice weekly for 30‐45 minutes during hospital‐based training. | Supervised strength sessions, recommended twice weekly for 30‐45 minutes during hospital‐based training. | |
| Minimum of 55% Heart Rate Reserve (HRR) and aim for maximum 85% HRR | Minimum exercise intensity of 55% HRR at the start of the study | |
| Personalized home‐based aerobic and strength exercise programme at least twice weekly | Target of 75% HRR within 2 months | |
| Personalized home‐based aerobic and strength exercise programme at least twice weekly | ||
| Vascular risk factor management | Clinical management and initiation of medications remained under the primary healthcare physician | Clinical management and initiation of medications transferred to the study physician during the study period |
| Subjects were advised to contact their primary physician if further management was required | Blood pressure management by study team followed SPRINT protocol guidelines. 12 , 13 | |
| Blood pressure management by primary healthcare followed national healthcare guidelines. 11 |
2.4. Outcome measures
2.4.1. Feasibility
The following measures were used to assess the compliance to the study interventions:
Diet: Participants were required to attend four dietary intervention sessions (two group, two individual) across 6 months (ie, baseline, month‐3, month‐6) regardless of intervention group. The maximum number of visits was four across 6 months. Research dieticians conducted the interventions based on the Finnish Nutrition Recommendations and Singapore, My Healthy Plate. A diet compliance score with a maximum score of 8 was also generated from the 3‐day food diaries (inclusive of at least 2 weekdays and 1 weekend) to determine compliance to recommended diets by the research dieticians. Scoring criterion and dietary recommendations can be found in Appendix A.
Vascular monitoring: All participants were required to attend study team visits thrice across 6 months (ie, baseline, month‐3, month‐6) regardless of intervention group. SINGER participants may have attended more than three study team visits due to the intensive vascular management. However, only results collected at the three specified visits were used for analysis.
Cognitive training: Similar to the FINGER study, participants were recommended to complete cognitive training sessions thrice weekly. The maximum number of sessions completed was capped at 72 across 6 months. Participants also attended two memory group talks.
Exercise: Home‐based aerobic and strength exercises were recommended twice weekly by the physiotherapist. The overall home‐based exercise completion was determined by the number of strength or aerobic exercise completed, whichever is higher. The maximum number of sessions completed was capped at 48 across 6 months.
2.4.2. Efficacy
The following measures were used to evaluate the efficacy of the study interventions:
Diet and vascular management: Diet and vascular risk factor management outcomes were measured by a series of assessments. Body weight, Body Mass Index (BMI), Hip‐Waist Ratio (HWR), fasting blood glucose and lipid assessed the effectiveness of the diet intervention. Differences in blood pressure (BP), fasting blood glucose and lipid outcomes were the endpoints of vascular risk factor measurement. Good BP control was defined as ≤120 mmHg, shown to be effective and safe by the SPRINT trial. 12 , 13 Good hyperlipidemia (HLD) control was defined as cholesterol level ≤6.1 mmol/L and LDL ≤4mmol/L. Good diabetes control was defined as fasting blood glucose levels between 3 and 6 mmol/L. We categorized participants into two groups according to the respective clinical outcome measures: (1) good outcome – persistently good control at all 3 time points or poor at baseline to good at month‐6, (2) poor outcome – persistently poor control at all 3 time points or good at baseline to poor at month‐6.
Cognitive intervention: The Neuropsychological Test Battery (NTB) and Color Trails Test (CTT) A & B were used to assess cognition at baseline and month‐6. The NTB has been validated in Asia, including Singapore. 14 Raw scores for all individual tests were transformed into individual z‐scores using the mean and standard deviation (SD) of the reference group. Tests assessing the same domain were added to obtain an overall unstandardized score, which was further transformed into standardized individual domain z‐scores using the composite mean and SD of the reference group. Global cognition was calculated by averaging the z‐scores of the individual domains and standardized using the mean and SD of the reference group. Higher scores represent better cognitive performance.
Physical intervention: Activity and fitness were measured at all 3 time points. The 6‐minutes walk test measured endurance, 10 minutes walk test measured walking speed, and one Repetition Measurement (RM) of eight major muscle groups assessed upper body, lower body and core strength. The self‐reported Late‐Life Function Disability Instrument (LLFDI) was also used to assess function. 15 To unify the RM tests into specific strength domains for analysis, raw scores were transformed for all individual tests into individual z‐scores using the mean and SD of the reference group. Upper body domain encompassed the following individual tests: shoulder raise, biceps, triceps, chest expansion. Lower body domain included hip flexion, hip extension and knee extension tests. Core domain included abdominal and back muscle tests. All tests were measured using kilograms. Individual domain scores were created using the composite mean and SD of the reference group. Higher scores represent better physical performance.
2.5. Statistical analysis
Descriptive statistics were performed to determine participants’ demographics such as age, sex and education (Table 2). Both groups were compared using repeated‐measures analysis of variance for continuous variables and chi‐square tests for categorical variables. Age, sex and years of education were taken as covariates. Feasibility was determined by the attendance to hospital‐based and home‐based interventions, and the diet compliance score – these were the dependent variables, with group being the independent variable. NTB global z‐scores were computed at baseline and month‐6 to examine efficacy and change in cognition. Efficacy of exercise intervention was assessed by endurance (6‐minutes walk test raw score) and upper body, lower body, and core strength z‐scores. Efficacy of diet and vascular risk factor management were measured using raw scores of clinical outcomes (eg, BMI, HWR, BP, blood biomarkers). BP was analyzed categorically, and participants were divided into good and poor BP outcome using the predefined target BP of ≤120 mmHg. Sensitivity analyses were also conducted using other BP targets of ≤130 mmHg and ≤140 mmHg to examine if our study cut‐off provided a more robust indication of the effectiveness of the SINGER BP management (data not shown). Hyperlipidemia and diabetes were also assessed categorically according to good/poor BP outcome.
TABLE 2.
Baseline participant demographics
| FINGER | SINGER | Whole sample | |
|---|---|---|---|
| n = 36 | n = 34 a | n = 70 | |
| Demographics | |||
| Age | 73.9 ± 4.9 | 74.2 ± 4.9 | 74.0 ± 4.9 |
| Education (years) | 11.2 ± 3.5 † | 9.0 ± 3.6 | 10.1 ± 3.7 |
| Sex (female, %) | 20 (55.6%) | 20 (58.8%) | 40 (57.1%) |
| Ethnicity (Chinese, %) | 35 (97.2%) | 31 (91.2%) | 66 (94.3%) |
| Language (English, %) | 20 (55.6%) | 12 (35.3%) | 32 (45.7%) |
| Vascular risk factors | |||
| History of stroke/TIA (yes, %) | 5 (13.9%) | 3 (8.8%) | 8 (11.4%) |
| Hypertension (yes, %) | 31 (86.1%)‡ | 22 (64.7%) | 53 (75.7%) |
| Hyperlipidemia (yes, %) | 27 (75.0%) | 28 (82.4%) | 55 (78.6%) |
| Diabetes (yes, %) | 10 (27.8%) | 9 (26.5%) | 19 (27.1%) |
| Lifestyle | |||
| Depression (yes, %) | 0 | 2 (5.9%) | 2 (2.9%) |
| Alcohol (yes, %) | 13 (36.1%) | 15 (44.1%) | 28 (40.0%) |
| Smoking (yes, %) | 0 | 0 | 0 |
| Level of independence (independent, %) | 35 (97.2%) | 33 (97.1%) | 68 (97.1%) |
| Subjective memory complaint (yes, %) | 26 (72.2%) | 24 (70.6%) | 50 (71.4%) |
| Baseline outcome assessment | |||
| Body Mass Index, BMI (kg/m2) | 25.2 ± 4.6 | 23.8 ± 3.7 | 24.5 ± 4.2 |
| Hip‐Waist‐Ratio | 1.1 ± 0.1 | 1.2 ± 0.1 | 1.1 ± 0.1 |
| Good Blood Pressure control b (yes, %) | 4 (11.1%) | 10 (29.4%) | 14 (20.0%) |
| Good Cholesterol control c (yes, %) | 32 (88.9%) | 30 (88.2%) | 62 (88.6%) |
| Good Diabetes control d (yes, %) | 20 (55.6%) | 26 (76.5%) | 46 (65.7%) |
| NTB global cognition z‐score | 0.0 ± 1.0 | ‐0.3 ± 1.3 | ‐0.1 ± 1.2 |
| Dietary compliance score (/8) | 6.5 ± 0.7 | 6.4 ± 1.0 | 6.5 ± 0.8 |
| 6‐minutes walk test (m) | 361.2 ± 70.2 | 351.1 ± 63.7 | 356.3 ± 66.9 |
| Upper body strength z‐score | 0.0 ± 1.0 | 0.2 ± 1.3 | 0.1 ± 1.1 |
| Lower body strength z‐score | 0.0 ± 1.0 | ‐0.05 ± 1.3 | ‐0.02 ± 1.1 |
| Core strength z‐score | 0.0 ± 1.0 | ‐0.02 ± 1.0 | ‐0.01 ± 1.0 |
Two subjects dropped out after baseline outcome measures were completed and before interventions began.
Good BP control defined as ≤120 mmHg.
Good cholesterol control defined as cholesterol ≤6.1 mmol/L and LDLC ≤4 mmol/L.
Good diabetes control defined as fasting blood glucose between 3 to 6 mmol/L.
P = .02, FINGER versus SINGER, ‡ P = .04, FINGER versus SINGER
3. RESULTS
Seventy‐one participants were recruited between October 2018 and April 2020. Of which, one did not meet inclusion criteria hence 70 participants were randomized – 36 into FINGER and 34 into the SINGER intervention, with a mean age of 74 years in the whole sample (Table 2). Two participants withdrew consent before interventions began, resulting in a total of 68 participants who completed the study (Figure 1). FINGER group participants were more educated than the SINGER group, and were more hypertensive (P < .05). Notably, while all participants completed month‐6 BP measurement, 12 of them recorded their BP at home via teleconsultation (due to COVID‐19 pandemic) with the study doctor ensuring that the BP measurement followed the SPRINT protocol (n FINGER = 7, n SINGER = 5). There was no difference in BP measurements between subjects who measured their BP in clinic versus at home (P > .05).
3.1. Feasibility
Overall, there was no difference between groups in terms of the feasibility of the exercise, diet and vascular risk factor interventions in a Singaporean population (Table 3). There was no difference between groups in terms of the compliance to the completion of food diaries throughout the study period, and the change in dietary compliance scores. Significantly more participants in SINGER completed cognitive training intervention than in FINGER across the 6 months (P = .04). Overall, health education sessions (two diet and cognitive group sessions each, and two individual diet sessions) were well‐attended by all participants (Median = 6, SD = 1.1).
TABLE 3.
Adherence to exercise, diet, vascular and cognitive training interventions between subjects in the FINGER and SINGER groups from baseline to month‐6
| FINGER | SINGER | |
|---|---|---|
| No. of sessions completed | n = 36 | n = 32 |
| Home‐based exercise | ||
| None | 5 (14%) | 4 (13%) |
| ≤50% | 12 (33%) | 11 (34%) |
| >50% | 19 (53%) | 17 (53%) |
| Food diary completion a | ||
| None | 0 | 1 (3%) |
| ≤50% | ‐ | ‐ |
| >50% | 36 (100%) | 31 (97%) |
| Cognitive training † | ||
| None | ‐ | ‐ |
| ≤50% | 15 (42%) | 6 (19%) |
| >50% | 21 (58%) | 26 (81%) |
| Vascular risk factors management | ||
| 100% | 36 (100%) | 32 (100%) |
Completion of food diary based on whether participants filled in their meals for all three required days (2 weekdays, 1 weekend) at each time‐point.
P = .04; significantly more subjects in the SINGER group completed >50% of home‐based cognitive training sessions (M3‐M6) while significantly more subjects in the FINGER group did not complete any sessions.
3.2. Efficacy
Though there was no significant difference between groups in intervention effectiveness (P > .05), average performance improved across the 6 months regardless of grouping. Specifically, upper body strength improved (P upper body = .04) while lower body and core strength trended to significance respectively (P lower body = .06; P core = .05). Notably, we found a positive trend where more in SINGER attained overall good BP outcome at month‐6 compared to the FINGER group (41% vs 19%; P = .06; Figure 3). Further analysis showed that subjects in SINGER with poor BP at baseline were driving this trend towards good BP outcome at month‐6. Hyperlipidemia (HLD) and diabetes mellitus (DM) were well‐controlled in both FINGER and SINGER groups, with good outcomes at month‐6 (89% vs 97%, 64% vs 75% respectively; P > .05).
FIGURE 3.

Overall BP outcome between groups
4. DISCUSSION
This is one of the first studies within WW‐FINGERS to develop and assess the feasibility and efficacy of culturally modified lifestyle interventions based on the original FINGER interventions. Examples of locally modified interventions include the transference from primary care to the study physicians for vascular risk factors management, and the use of pen‐and‐paper cognitive training tools. These modifications represented the cultural and healthcare structural uniqueness of Singapore.
Our findings showed that the original FINGER interventions were equally as feasible as the adapted SINGER lifestyle interventions. Both groups fared well in vascular risk factor monitoring, and home‐based exercise over the 6 months. Both groups completed a large proportion of home‐based exercise sessions across the 6 months, with over 85% from both groups completing at least one home‐based session. Our findings are comparable to the adherence to home‐based exercise reported in previous literature, including the FINGER study where about 76% completed at least one home‐based exercise session. 8 , 16
Notably, the SINGER cognitive training intervention demonstrated greater feasibility than FINGER. Our finding is consistent with the 79% adherence rate based on the mean sessions completed previously reported in an RCT that used home‐based pen‐and‐paper training mode. 16 Moreover, 44% of our subjects in the FINGER group completed more than half home‐based sessions – a comparable percentage to previous RCTs using computerized training, including FINGER where about 30% completed more than half of the cognitive sessions. 8 Further analysis showed no difference between groups when subjects with no access to computers were excluded (data not shown). Consistent with previous literature, the main reason behind the lower adherence rate in the FINGER group was the lack of access to computers, resulting in more SINGER participants completing home‐based training. In this study, participants were provided with the training programme on a thumb‐drive, allowing them the option of using public computers. For the SINGER group, pen‐and‐paper materials for all 3 months were provided at the beginning of the home‐based intervention, hence participants had full access to all training materials. Our study demonstrates that though compliance rate for home‐based interventions decreased compared to hospital‐based interventions, the majority of subjects still participated actively in other intervention components. These findings strongly demonstrate the feasibility of the interventions particularly in times of public health emergencies such as the COVID‐19 pandemic where most research studies and interventions have to be conducted remotely.
Both groups achieved 100% attendance for study team visits even during COVID‐19, suggesting the feasibility of a combination of regular face‐to‐face and teleconsultation health monitoring. The SPRINT protocol did not recommend taking BP home readings due to potential bias and error. Nevertheless, due to the circumstances experienced during the partial lockdown in Singapore, 12 participants measured their BP at home according to SPRINT procedures with the guidance of the study physician during their teleconsultation. Of the 12, 10 used their personal BP machines while two used portable BP machines that were delivered to their homes. There was no difference between BP readings taken in clinic versus at home. The effectiveness of teleconsultation, home‐based lifestyle interventions and ease of obtaining intervention logs and materials through delivery illustrate the adaptability of the SINGER pilot study in continuing through a time where most clinical research were halted.
The effects of the lifestyle interventions on clinical outcomes suggest that participants are trending to improvement regardless of whether they were assigned to the FINGER or SINGER lifestyle interventions. Our findings thus suggest that a multi‐domain lifestyle intervention has positive effects on mild‐to‐moderately frail older adults. Supporting this is an RCT consisting 246 pre‐frail and frail older adults in Singapore that delivered cognitive training, nutritional intervention and a combination of both alongside physical training over 6 months, and were found to improve cognition over time. 16 Though Ng et al. 16 utilized a series of lifestyle interventions similar to the SINGER study, a vascular management component was not included. While the vascular management clinical outcomes (eg, BP, cholesterol) did not show any significant improvement, this was due to the short study duration. Although there was no difference between groups in good HLD and DM outcomes at month‐6, these vascular risk factors were generally well‐controlled in both groups. Our sample has a higher prevalence of hypertensive elderly compared to the Singaporean general population (76% vs 49% to 66%). 17 We found a trend towards better BP outcome at month‐6 in the SINGER group, suggesting that close monitoring of BP is vital in attaining improved outcomes compared to general management in the primary healthcare system. Interestingly, further analysis demonstrated that subjects with poor baseline BP in SINGER were driving this trend as they had better BP outcomes compared to those in the FINGER group (35% vs 12%, P = .048). These findings therefore illustrate the effectiveness of intensive management in managing good BP outcome. Notably the Singaporean national standards for target BP control is 130‐140 mmHg, however recent studies have demonstrated the effectiveness of a lower target (ie, 120 mmHg) in reducing rates of both fatal and nonfatal major cardiovascular outcomes and possibly cognition. 18 Therefore, our results demonstrating an improvement in BP by reaching the 120 mmHg target using the SINGER vascular intervention over 6 months are promising.
The SINGER pilot facilitates the design of a larger SINGER study in a community setting for older adults at higher risk of dementia. While previous studies have demonstrated the positive long‐term effects of lifestyle interventions, such as those in SINGER, on cognition, 8 , 19 it remains possible that the benefits of these lifestyle interventions are wider. The vascular risk factors actively managed in SINGER, physical exercise, cognitive training and a healthy and balanced diet may also contribute to the prevention of other chronic diseases, including stroke, diabetes and hypertension. 20 , 21 Active participation in SINGER may also help improve public health literacy, promoting the concept and content of “healthy ageing” and “confident ageing in place” in a wider range of community‐dwellers. Importantly, the unprecedented novel COVID‐19 pandemic has severely limited social interaction. Hence it is essential to equip such active and regular lifestyle interventions and management programmes with a remote yet convenient access and execution. This should also be further developed in a larger scale study.
4.1. Limitations and implications
Our study has strengths and weaknesses. This is the first to evaluate the feasibility of the FINGER interventions in a multi‐ethnic population. By implementing an RCT design, we were able to compare the established FINGER interventions with locally modified SINGER interventions and illustrate the cultural acceptance and feasibility of both sets of interventions. Moreover, our study followed a rigorous protocol, with blinded raters assessing comprehensive outcome measurement. Extensive considerations for intervention materials such as thumb‐drives for the FINGER home‐based cognitive training, and light weights for the home‐based exercise training were also taken into account. Conversely, one limitation is the short period of time for intervention. We only provided interventions for 6 months, which may be too short to obtain a more robust secondary measurement of intervention efficacy. Nonetheless, as our primary outcome is feasibility, the intervention period was deemed sufficient. Nevertheless, even with a shorter intervention period, we were able to establish superiority in BP management for the SINGER intervention, highlighting the importance of having a dedicated study physician to monitor BP compared to leaving it to the general healthcare system. Other limitations include the small sample size and the lack of a control (general health management) group to evaluate the efficacy of the SINGER intervention. This will be addressed in a larger‐scale trial that will be developed.
Future studies should include more biomarkers of ageing, such as blood and imaging biomarkers, as well as quality of life assessments for both participants and caregivers, to determine a more comprehensive presentation of the intervention outcomes. Our study has found that the SINGER vascular management and both types of cognitive training, physical exercise and diet interventions are feasible in Singapore. It is therefore essential to develop a larger RCT with at least 2 years of interventions such as the original FINGER study to further evaluate the efficacy of these interventions on cognition in older adults in Singapore.
In conclusion, our study evaluated the feasibility and efficacy of the SINGER lifestyle interventions, which were adapted from the FINGER lifestyle interventions. We found that the FINGER lifestyle interventions were as feasible as the SINGER interventions in a Singaporean population of older adults. Furthermore, we found that all interventions were effective over the 6 months regardless of intervention group. Of note, more subjects in SINGER achieved good BP control than those in FINGER in 6 months, illustrating the effectiveness of close monitoring by a study physician.
CONFLICTS OF INTEREST
None declared.
ACKNOWLEDGMENTS
The authors would like to thank Dr. Miia Kivipelto, Dr. Tiia Ngandu and Dr. Alina Solomon, and the FINGER team for their support and guidance during the planning of the project. The authors would also like to acknowledge the study participants for their keen interest and cooperation in the study interventions and measures. The authors would also like to thank the research coordinators and raters at the Memory, Ageing and Cognition Centre, research dieticians at A*STAR and the exercise and rehabilitation team at the National University Hospital for their hard work and dedication. This work was supported by the Functional Ageing Initiative (NUSMed).
Appendix A.
SINGER Diet Intervention Programme
Participants were recommended to consume wholegrain products instead of refine products, sufficient intake of vegetables, fruits and protein, fish consumption at least twice a week, reduce consumption of added sugar in food/drinks and choosing low fat option. The SINGER diet intervention followed the FINGER dietary component criteria. Specifically, the SINGER diet consisted of the following:
High consumption of Asian fruits and vegetables (eg, kai lan, guava, papaya)
Whole grain rice including brown rice; consumption of oats, wholemeal bread
Soy milk (substitute for milk)
Lean meat, bean products (tofu) and less saturated fat
Peanut, sunflower and canola, rice bran oils (avoid frying)
Almonds and walnuts
Consumption of two portions of fish/fish oil supplementation and tofu per week
Less added sugar and salt.
The group sessions took ≈ 60‐90 minutes and included topics on a healthy meal/plate, healthy food choices and reading food labels. The individual sessions (30‐minutes) were adapted and personalized to each participant's needs identified by the nutritionist. 3‐day food diaries (2 weekdays, 1 weekend) were completed by participants at baseline, month‐3 and month‐6. Participants attended two group‐based nutritional sessions and two individual nutritional sessions over the first 3 months. A diet compliance score was generated using the participants’ food diaries and were based on a specific criterion (Figure 1).
Figure 1: Scoring criterion for diet compliance score based on the 3‐day food diary
SINGER Exercise Intervention Programme
The SINGER exercise programme consisted of supervised strength and aerobic exercise classes. Both occurred twice weekly over 12 weeks. The supervised strength class comprised of:
Stretching (5 minutes)
Balance training (10 minutes)
-
Strengthening (30 to 45 minutes)
-
∘
10 reps of 10 Repetition Maximum (RM) of major muscle groups using free weights, TheraBands and weights machine
-
∘
The supervised 30‐minutes aerobic exercise class were recommended twice weekly and required a minimum Heart Rate Reserve (HRR) of 55% at the start of the study. The target HRR after 2 months is 75%.
Individualized home‐based programmes were also provided to all subjects for them to complete muscle strength training and aerobic exercise for a recommended twice weekly. Subjects recorded their activities in an exercise diary.
SINGER Cognitive Intervention Programme
The SINGER cognitive intervention programme comprised of individual sessions and group‐based sessions. Participants attended two group‐based sessions consisting non‐structured discussions on topics such as age‐related changes in cognition, memory strategies and everyday memory training. The pen‐and‐paper training tasks were designed to enhance multidomain skills such as memory, executive function, attention and processing speed. There were three levels in total, with 24 sessions within one level. Each session comprised of four tasks. There were two different sets of the four tasks and these sets switched every four sessions. Participants advanced to a higher level of difficulty after 24 sessions. Level advancements aimed to reduce practice effects and adjust to participants’ cognitive abilities. Participants were provided with the instructions for each task at every session.
SINGER Vascular Risk Factor Management
Participants attended a minimum of three study team visits (ie, baseline, month‐3, month‐6). Participants in the FINGER group had their vascular risk factors managed by their primary healthcare physicians. They were advised by the study team at baseline, month‐3 and month‐6 follow‐ups to contact their primary physician if further management such as high BP was required. Meanwhile, subjects in the SINGER group had their medical care transferred to the study physician for the duration of the study. Therefore, changes in medications were also handled by the study physician. BP of the SINGER group was managed by the study physician, who followed the SPRINT protocol guidelines for clinical management of BP (ie, good BP control defined as ≤120 mmHg).
Chew KA, Xu X, Siongco P, et al. SINgapore GERiatric intervention study to reduce physical frailty and cognitive decline (SINGER)–pilot: A feasibility study. Alzheimer's Dement. 2021;7:e12141. 10.1002/trc2.12141
Kimberly Ann Chew and Xin Xu Equal contribution to this study.
REFERENCES
- 1. World Health Organisation . Dementia. World Health Organisation; 2019. https://www.who.int/news-room/fact-sheets/detail/dementia. Accessed August 7, 2020. [Google Scholar]
- 2. Fulop T, Larbi A, Witkowski JM, et al. Aging, frailty and age‐related diseases. Biogerontology. 2010;11(5):547‐563. [DOI] [PubMed] [Google Scholar]
- 3. Chen C, Xu X, Chew E, Henry CJ, Koo EH. Singapore intervention study to prevent cognitive impairment and disability (singer) initiative. Alzheimers Dement. 2017;13(7). [Google Scholar]
- 4. United Nations, Department of Economic and Social Affairs, Population Division. New York: United Nations: World Population Ageing; 2019. (ST/ESA/SER.A/444) [Google Scholar]
- 5. Klimova B, Valis M, Kuca K. Cognitive decline in normal aging and its prevention: a review on non‐pharmacological lifestyle strategies. Clin Interv Aging. 2017;12:903‐910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Moll van Charante E, Richard E, Eurelings LS, et al. Effectiveness of a 6‐year multidomain vascular care intervention to prevent dementia (preDIVA): a cluster‐randomized controlled trial. Lancet. 2016;388:797‐805. [DOI] [PubMed] [Google Scholar]
- 7. Andrieu S, Guyonnet, S , Coley, N , et al. Effect of long‐term omega 3 polyunsaturated fatty acid supplementation with or without multidomain intervention on cognitive function in elderly adults with memory complaints (MAPT): a randomized, placebo‐controlled trial. Neurol. 2017;16:377‐389. [DOI] [PubMed] [Google Scholar]
- 8. Ngandu T, Lehtisalo J, Solomon A, et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at‐risk elderly people (FINGER): a randomised controlled trial. Lancet. 2015;385(9984):2255‐2263. [DOI] [PubMed] [Google Scholar]
- 9. Kivipelto M, Mangialasche F, Snyder HM, et al. World‐wide FINGERS network: a global approach to risk reduction and prevention of dementia. Alzheimers Dement. 2020;16(7):1078‐1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lusardi MM, Pellecchia GL, Schulman M. Functional performance in community living older adults. J Geriatr Phy Ther. 2003;26(3):14‐22. [Google Scholar]
- 11. Ministry of Health Singapore. Hypertension: MOH Clinical Practice Guidelines 01/2017. https://www.moh.gov.sg/docs/librariesprovider4/guidelines/cpg_hypertension–booklet—nov–2017.pdf. Accessed August 7, 2020.
- 12. SPRINT . Systolic Blood Pressure Intervention Trial. SPRINT Version 4.0. 2012. [Google Scholar]
- 13. The SPRINT research group. A randomized trial of intensive versus standard blood‐pressure control. N Engl J Med. 2015;373:2103‐2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shen JHQ, Shen, Q , Yu, H , et al. Validation of an Alzheimer's disease assessment battery in Asian participants with mild to moderate Alzheimer's disease. Am J Neurodegener Dis 2014;3(3):158‐169. [PMC free article] [PubMed] [Google Scholar]
- 15. Sayers SP, Jette AM, Haley SM, et al. Validation of the late‐life function and disability instrument. J Am Geriatr Soc. 2004;52(9):1554‐1559. [DOI] [PubMed] [Google Scholar]
- 16. Ng TP, Ling LHA, Feng L, et al. Cognitive effects of multi‐domain interventions among pre‐frail and frail community‐living older persons: randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2018;73(6):806‐812. [DOI] [PubMed] [Google Scholar]
- 17. Malhotra R, Chan A, Malhotra C, Østbye T. Prevalence, awareness, treatment and control of hypertension in the elderly population of Singapore. Hypertens Res. 2010;33:1223‐1231. [DOI] [PubMed] [Google Scholar]
- 18. The SPRINT MIND investigators for the SPRINT research group. Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial. JAMA. 2019;321(6):553‐561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Blumenthal JA, Smith PJ, Mabe S, et al. Lifestyle and neurocognition in older adults with cognitive impairments: a randomized trial. Neurol. 2019;92(3):e212‐e223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yusuf S, Joseph P, Rangarajan S, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high‐income, middle‐income, and low‐income countries (PURE): a prospective cohort study. Lancet. 2020;395:795‐808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Global burden of metabolic risk factors for chronic diseases collaboration. Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010: a comparative risk assessment. Lancet Diabetes Endocrinol. 2014;2:634‐647. [DOI] [PMC free article] [PubMed] [Google Scholar]


