Abstract
Background
One of the main concerns using low-dose (LD) CT for evaluation of patients with suspected intestinal obstruction or pneumoperitoneum is the potential need to make an additional standard-dose (SD) CT scan (retake) due to insufficient diagnostic accuracy of the LD CT.
Purpose
To determine the frequency of retakes and evaluate the diagnostic accuracy of LD CT for the assessment of intestinal obstruction and pneumoperitoneum.
Material and Methods
This retrospective study registered all LD CT scans over a one-year period at Aarhus University Hospital, Denmark in patients with suspected intestinal obstruction or perforation, comprising a total of 643 LD CT scans. A retake was defined as a SD CT scan of the abdomen and pelvis performed with or without intravenous contrast within 72 h after the initial LD CT due to either continued suspicion of intestinal obstruction or perforation or due to unclarified secondary findings. The sensitivity and specificity of LD CT for diagnosing intestinal obstruction and pneumoperitoneum compared to the discharge diagnoses of the scanned patients were determined.
Results
The frequency of retakes was 3%. The overall LD CT sensitivity and specificity for assessment of patients with suspected intestinal obstruction and pneumoperitoneum was 83% and 99%, respectively, but higher in certain subgroups.
Conclusions
LD CT led to few retakes and had a high diagnostic accuracy for diagnosing intestinal obstruction and pneumoperitoneum. Thus, LD CT can be recommended as the examination of choice in patients with suspected intestinal obstruction or perforation in order to reduce radiation dose.
Keywords: Abdomen/GI; CT; Adults; Radiation safety, Intestinal obstruction, Low dose CT
Introduction
In Denmark, acute abdomen is the fifth most common cause of hospital admission.1 In the United States, abdominal pain accounts for 1.5% of all office-based patient visits and 8% of all Departments of Emergency contacts.2 CT imaging is often the preferred modality to evaluate patients with acute abdominal pain. It is widely accessible, fast, low cost and, in most cases, superior to ultrasound and conventional radiography due to the limited sensitivity of these modalities.3–6
Over the last decades, the use of CT has increased rapidly worldwide. In Denmark, the annual number of CT scans of the abdomen increased from 30,889 in 2003 to 119,373 in 2014 (386%).7 However, CT also has a considerable drawback, as it has been estimated that 1–2% of patients scanned with a SD trauma CT will develop radiation-induced cancer during their lifespan.8 Thus, development of LD CT with sufficient diagnostic quality is warranted.
LD CT has already proven beneficial for diagnosing nephrolithiasis,5,9,10 acute colon diverticulitis,11 acute appendicitis,12 acute non-traumatic abdominal pain in general,13 and intestinal obstruction and pneumoperitoneum.5 Intestinal obstruction and pneumoperitoneum are both conditions that can be assessed by non-contrast-enhanced LD CT.5 Additional intravenous contrast administration constitutes a potential risk in terms of allergy and renal adverse reactions and costs hospital resources.
One of the major concerns using LD CT to diagnose intestinal obstruction and pneumoperitoneum is the potential need for additional SD CT scans (retakes), due to either inability to establish a reliable diagnosis of intestinal obstruction and pneumoperitoneum or due to inconclusive incidental findings – both problems inherent to the decreased image quality of LD CT imaging. Retakes entails increased radiation dose, healthcare resources, financial costs as well as diagnostic and treatment delays.
Non-contrast-enhanced LD CT has proven superior to abdominal radiography for assessing intestinal obstruction and pneumoperitoneum.4,6 Since 2007, non-contrast-enhanced LD CT has been the primary method to assess patients with suspected intestinal obstruction or pneumoperitoneum at Department of Radiology at Aarhus University Hospital. To our knowledge, substantial evidence to support the use of LD CT rather than SD CT is lacking.
The objectives of this study were to:
Determine the frequency of retakes and
Evaluate the diagnostic accuracy of LD CT for diagnosing intestinal obstruction and pneumoperitoneum by comparing LD CT findings to discharge diagnoses and subsequently performed retakes.
Material and Methods
In this retrospective study, CT scans were identified using the radiological management software RIS (Carestream RIS, Version 10.1.10 Build 60) and IMPAX (AGFA Healthcare, Version 6.5.5.1608). Included were all LD CT scans of the abdomen and pelvis performed from 1 April 2015 to 31 March 2016 at Department of Radiology, Aarhus University Hospital on patients referred from Department of Emergency or Department of Surgery with suspected intestinal obstruction and/or pneumoperitoneum (including retroperitoneal free air). In total, 643 LD CT scans were included. No scans fulfilling the inclusion criteria were excluded. Written informed consent was waived by the Institutional Review Board.
Retakes were defined as SD CT scans of the abdomen and pelvis performed meeting the following criteria: (a) with or without intravenous contrast (b) within 72 h after the initial LD CT and (c) with the same indication as the initial LD CT or due to inconclusive secondary findings on the initial LD CT. Excluded were SD CT scans performed due to a medical condition arisen after the LD CT (e.g. fever and suspicion of abscess), SD CT scans performed after a major clinical intervention such as surgery, which would change the occurrence of intestinal obstruction or pneumoperitoneum between the LD CT and SD CT, or dedicated SD CT scans requiring contrast phases other than the portal venous phase such as for example CT angiography or CT urography. The retakes were identified using the RIS software to find all patients with a LD CT and a subsequent SD CT scan who met the inclusion and exclusion criteria.
In addition to the retakes, other radiological examinations with relevance to the abdominal condition performed within the first 72 h were registered.
The LD CT scans were performed on either a Philips Brilliance 64, a Philips Brilliance 40 or a Philips iCT 256 (Philips Healthcare) with the following parameters: Tube voltage = 120 kV, 1 mAs/kg/slice, pitch = 0.923–1.175, gantry rotation time = 0.5 s, collimation = 64 × 0.625 mm; slice thickness = 2.0 mm, increment = 1.0 mm, performed with filtered backprojection but without iterative reconstruction. All scans were performed without intravenous contrast.
The retakes comprised several CT protocols. The most frequently used protocol had the following parameters: Tube voltage = 120–140 kV, 200–250 mAs/slice, pitch = 1.172, gantry rotation time = 0.75 s, collimation = 64 × 0.625, slice thickness = 2.0 mm, increment = 1.0 mm, performed with D-DOM and filtered backprojection but without iterative reconstruction.
For all LD CT scans and retakes, the CT diagnosis was recorded; the images were not evaluated. All scans were evaluated by medical doctors with at least 3.5 years of experience in radiology (radiologists and residents in radiology). A diagnosis of intestinal obstruction or pneumoperitoneum was only recorded if stated specifically in the conclusion of the CT description. If the CT conclusion stated possible intestinal obstruction, incomplete intestinal obstruction or similar, the CT diagnosis was registered as possible intestinal obstruction. If the CT conclusion did not mention whether the nature of the intestinal obstruction was paralytic or mechanical, the CT description was reviewed for additional information. Also, additional CT diagnoses other than pneumoperitoneum or intestinal obstruction potentially causing abdominal pain were registered.
In Denmark, all patients are given a diagnosis at discharge. The discharge diagnoses of all patients scanned with LD CT were identified in the electronic patient record system (Columna, Systematic A/S, version 25.2.2.2-25).
To establish the diagnostic accuracy, the LD CT diagnosis was compared to the corresponding discharge diagnosis, which considers both clinical assessment, biochemistry, diagnostic imaging, and potential surgical procedures; thus, it can be regarded as the most accurate evidence of a patients’ true diagnosis (the gold standard). To identify patients diagnosed with either intestinal obstruction or pneumoperitoneum, all discharge diagnoses were reviewed for conditions associated with intestinal obstruction or pneumoperitoneum according to the International Classification of Disease – 10th edition14 (see Table 1 in Supplementary Material).
Table 1.
Findings in the 643 low-dose CT scans.
| Bowel obstruction | 143 (22%) | ||
| Mechanical obstruction | 132 (92%) | ||
| Small bowel | 113 (86%) | ||
| Large bowel | 19 (14%) | ||
| Paralytic ileus | 11 (8%) | ||
| Possible intestinal obstruction | 101 (16%) | ||
| Pneumoperitoneum | 45 (7%) | ||
| Other findings possibly causing abdominal pain | 191 (30%) | ||
| No findings | 164 (25%) |
Note: One scan showed both bowel obstruction and pneumoperitoneum, and thus the total number of findings is 644.
If intestinal obstruction or pneumoperitoneum was diagnosed using LD CT and listed as the patient’s discharge diagnosis, this was accepted as a true positive finding. If no intestinal obstruction or pneumoperitoneum was described on LD CT and the discharge diagnosis was different from the diagnoses listed in Supplementary Table 1, this was accepted as a true negative finding. In all other cases, patient records were reviewed for final diagnosis.
After identifying all retakes, the frequency of retakes was calculated. The diagnostic accuracy of LD CT was established by determining the sensitivity and specificity for diagnosing intestinal obstruction and pneumoperitoneum by comparing the LD CT diagnoses to the discharge diagnoses/clinical records and to the retake diagnoses, respectively. Some patients had more than one LD CT performed during the study period. To ensure that all 643 LD CT scans were in fact independent, diagnostic accuracy was also calculated for the single first LD CT scan of each patient, omitting all following LD CT scans.
Statistics
Sensitivity, specificity, and 95% confidence intervals were calculated using the online statistical tool MEDCALC.15 The confidence intervals were calculated using the Clopper-Pearson method.
All other statistical analyses were performed using Microsoft Excel (Microsoft Corporation, Version 16.23).
Results
LD CT
The LD CT scans had a mean effective dose of 4.3 mSv dependent on patient size.
A total of 643 LD CT scans was performed in 568 patients (264 males, 304 females, mean age 61 years, range 11 to 99). Of the 568 included patients, 61 patients had more than one LD CT performed during the study period. The maximum was 5 LD CT scans performed in one patient, comprising 75 repeated LD CT scans. The median interval between the repeated LD CT scans was 22 days, range 0 to 230). In the 643 LD CT scans, intestinal obstruction was identified in 143 scans (22%), possible intestinal obstruction in 101 scans (16%), and pneumoperitoneum in 45 scans (7%) (Table 1).
Possible causes of abdominal pain other than intestinal obstruction and pneumoperitoneum were identified in 191 scans and are listed in Table 2.
Table 2.
Low-dose CT findings of possible causes of abdominal pain in patients without intestinal obstruction or pneumoperitoneum.
| Findings | N |
|---|---|
| Gallstones and/or cholecystitis | 42 |
| Constipation | 35 |
| Urinary tract findingsa | 28 |
| Chest findingsb | 23 |
| Ascites | 21 |
| Pancreatitis | 13 |
| Tumour/metastasesc | 13 |
| Bowel wall thickening | 12 |
| Gastric retention | 10 |
| Diverticulitis | 8 |
| Herniad | 8 |
| Peritoneal fat inflammation | 6 |
| Meteorism | 6 |
| Fluid collection or abscesses | 5 |
| Postoperative findingse | 4 |
| Abdominal aortic aneurysms | 3 |
| Appendicitis acuta | 3 |
| Carcinosis | 3 |
| Othersf | 11 |
| Total | 254 |
aIncludes renal stones, pyelonephritis, hydroureter, hydronephrosis, and bladder retention.
bIncludes pneumonia and pleural fluid.
cIncludes known malignant tumours and metastases and tumours of unknown pathology.
dIncludes hiatus, internal, and inguinal hernia.
eIncludes haematomas and radiofrequency liver ablation changes.
fIncludes enlarged lymph nodes, splenomegaly, collapsed vertebrae, pancreas cysts, ovary cysts, and ingested foreign bodies.
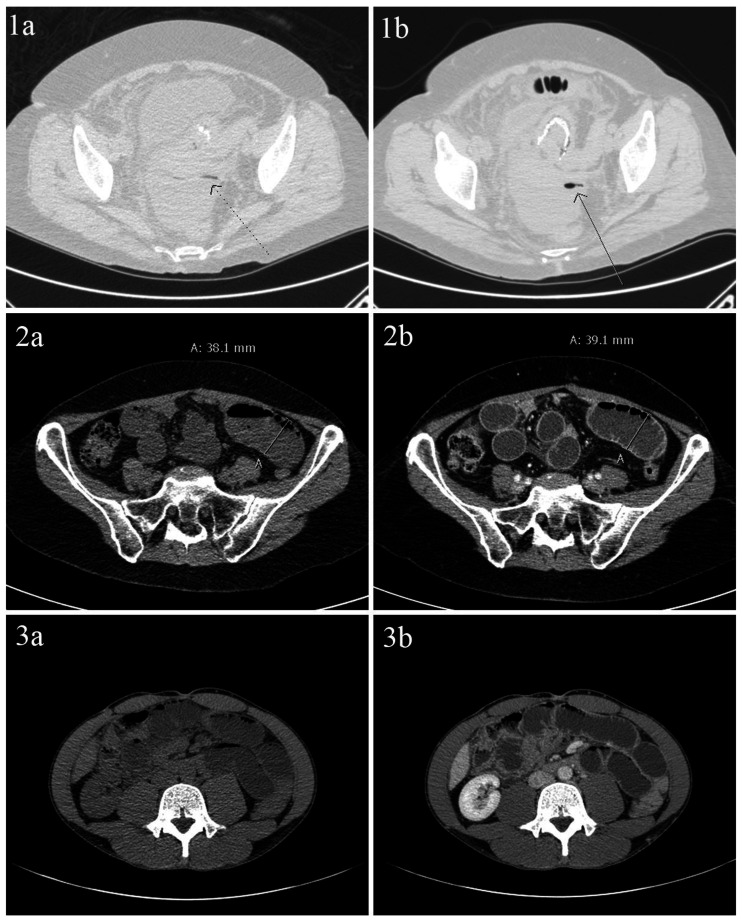
Examples of LD CT images from patients with intestinal obstruction and pneumoperitoneum are presented in Fig. 1.
Fig. 1.
(a) low-dose CT images, (b) retake standard-dose CT images. 1. 61-yr-old woman with pneumoperitoneum due to colon perforation after insertion of a colonic stent. Time interval between scans: 12 h. The shown retake is before contrast enema and without i.v. contrast. Arrows: Intraabdominal free gas. 2. 57-yr-old woman with small bowel obstruction. Time interval between scans: 12,5 h. The retake is contrast enhanced. 3. 32-yr-old man with small bowel obstruction. Time interval between scans: 0,5 h. The retake is contrast enhanced.
Retakes
The most frequently used retake protocol had a mean effective dose of 14.2 mSv dependent on patient size.
The frequency of retakes was 3% (22/643). Of the 22 retakes, five showed mechanical obstruction (four small bowel obstruction and one large bowel obstruction), one scan showed possible intestinal obstruction, and one scan showed pneumoperitoneum.
The four diagnoses of bowel obstruction and the one diagnosis of pneumoperitoneum remained unchanged between the LD CT scans and the retakes. The one case of possible bowel obstruction on LD CT was confirmed as mechanical obstruction of the large bowel on the following retake.
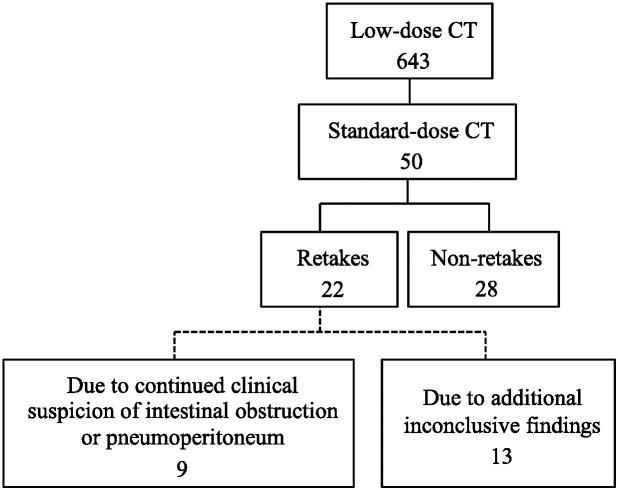
Nine retakes were performed with the same indication as the initial LD CT, i.e. continued clinical suspicion of intestinal obstruction/pneumoperitoneum, while the remaining 13 were rescanned due to inconclusive secondary findings in the initial LD CT (Fig. 2).
Fig. 2.
Distribution of the included low-dose CT and standard-dose CT scans (retakes and non-retakes) and retake indication.
Examples of SD CT images from patients with intestinal obstruction and pneumoperitoneum are presented in Fig. 1.
Additional examinations
In addition to the 22 retakes, a total of 79 other radiological examinations relevant to the abdominal condition were performed within 72 h following the LD CT – including 28 non-retake CT scans (Table 3). Of these 79 radiologic examinations, 58 were performed due to secondary findings in the initial LD CT (e.g. ultrasound guided drainage of pleural fluid).
Table 3.
Radiological examinations other than retakes performed within 72 h after initial low-dose CT.
| Modality | N |
|---|---|
| Ultrasound examinations | 33a |
| Standard-dose CT (non-retakes) | 28 |
| Small-bowel follow-throughs | 13 |
| Lower gastrointestinal tract radiography | 2 |
| Cystography | 1 |
| PET-CT | 1 |
| MRI | 1 |
| Total | 79 |
aComprising 17 interventions including 10 ascites and pleural fluid drainages.
Diagnostic accuracy of LD CT
Compared to the discharge diagnoses, LD CT had an overall sensitivity (95% CI) of 83% (77–88%) and a specificity of 99% (97–100%) for diagnosing intestinal obstruction and pneumoperitoneum combined (see Table 4). For diagnosing intestinal obstruction, the sensitivity was 80% (73–85%) and the specificity was 100% (98–100%); for diagnosing intestinal obstruction and possible intestinal obstruction combined, the sensitivity was 99% (97–100%) and the specificity was 85% (82–89%). Finally, for diagnosing pneumoperitoneum, the sensitivity was 95% (85–99%) and the specificity was 100% (99–100%).
Omitting all repeated LD CT scans using only the initial 568 LD CT scans did not change the overall sensitivity and specificity (Table 4).
Table 4.
Diagnostic accuracy of low-dose CT assessing intestinal obstruction, possible intestinal obstruction, pneumomediastinum, and combinations of these.
| TP | FP | FN | TN | Sensitivity (95% CI) | Specificity (95% CI) | |
|---|---|---|---|---|---|---|
| Discharge diagnoses | ||||||
| For all low-dose CT scans (n=643) | ||||||
| Intestinal obstruction | 141 | 2 | 36 | 464 | 80% (73–85%) | 100% (98–100%) |
| Intestinal obstruction and possible intestinal obstruction | 176 | 68 | 1 | 398 | 99% (97–100%) | 85% (82–89%) |
| Pneumoperitoneum | 42 | 3 | 2 | 596 | 95% (85–99%) | 100% (99–100%) |
| Intestinal obstruction and pneumoperitoneum | 183 | 5 | 38 | 417 | 83% (77–88%) | 99% (97–100%) |
| For the first low-dose CT scan in each patient (n=568) | ||||||
| Intestinal obstruction | 122 | 2 | 29 | 415 | 81% (74–87%) | 100% (98–100%) |
| Intestinal obstruction and possible intestinal obstruction | 145 | 60 | 1 | 362 | 99% (96–100%) | 86% (82–89%) |
| Pneumoperitoneum | 40 | 3 | 2 | 523 | 95% (84–99%) | 99% (98–100%) |
| Intestinal obstruction and pneumoperitoneum | 162 | 5 | 31 | 370 | 84% (78–89%) | 99% (97–100%) |
| Retakes | ||||||
| Intestinal obstruction and pneumoperitoneum | 4 | 0 | 1 | 17 | 80% (28–99%) | 100% (80–100) |
Note: The low-dose CT sensitivity and specificity was calculated by comparison of low-dose CT findings to the scanned patients discharge diagnoses and to standard-dose CT findings.
TP: true positive, FP: false positive, FN: false negative, TN: true negative.
Compared to the corresponding retakes, LD CT had a sensitivity of 80% (28–99%) and a specificity of 100% (80–100%) for diagnosing intestinal obstruction and pneumoperitoneum combined.
Discussion
The present study demonstrated a frequency of retakes of only 3% for LD CT in the diagnosis of intestinal obstruction and pneumoperitoneum. We found that the indications for retakes were either continued suspicion of intestinal obstruction or pneumoperitoneum (nine scans) or inconclusive findings on the initial LD CT (13 scans). Evaluating the diagnostic accuracy of LD CT compared to the patients' discharge diagnoses, the sensitivity and specificity were 83% and 99%, respectively, for diagnosing intestinal obstruction and pneumoperitoneum combined. Compared to the corresponding retakes, the sensitivity and specificity were 80% and 100%, respectively.
The low frequency of retakes found in this study indicates that LD CT is highly reliable for diagnosing intestinal obstruction or pneumoperitoneum, which is emphasized by the high diagnostic accuracy.
The LD CT scans elicited additional examinations other than retakes, mainly due to inconclusive secondary findings. We, however, do not consider this a disadvantage, as these included a significant number of arterial phase contrast-enhanced CT scans as well as e.g. ultrasound-guided ascites and pleural fluid drainage. Thus, indicating that the optimal radiological examination to manage secondary findings might be based on LD CT instead of SD CT, resulting in a lower radiation dose.
We also determined the diagnostic accuracy of LD CT for diagnosing intestinal obstruction and possible intestinal obstruction combined and found a very high sensitivity (99%). We have reported this as well, as the subdivisions into intestinal obstruction and possible intestinal obstruction reflect the daily clinical practice in radiology, where a definitive diagnosis cannot always be established, and where clinicians will intervene in case of possible intestinal obstruction – if symptoms adequately correlate.
Comparison with other studies
To our knowledge, we are the first to determine the frequency of retakes for LD CT assessing intestinal obstruction and pneumoperitoneum. Udayasankar et al. found that 12% of the initial 163 patients undergoing ultra-LD CT had a contrast-enhanced CT performed during the same admission.5 However, they did not specify the scan-phase or the interval length between scans. In a non-contrast-enhanced SD CT study, 4% out of the initial 72 patients had an additional contrast-enhanced SD CT performed within seven days after the initial CT due to continued clinical doubt about the diagnosis.16 These results are in fairly good agreement with our findings of 7.8% SD CT (retake + non-retake CT) and 3% retakes performed within 72 h after the initial LD CT. Assessing the diagnostic accuracy of LD CT, Alshamari et al. found an overall sensitivity and specificity of 75% and 87%, when assessing non-traumatic abdominal pain in general and comparing CT findings with clinical diagnoses.6 Udayasankar et al. found that the sensitivity, specificity, and positive predictive value for 163 ultra-LD CT for the detection of pneumoperitoneum, urinary tract stone, and intestinal obstruction was 100%, 99%, and 92%, respectively, compared to the patients’ clinical records.5 However, in this study, they had two different radiologists reviewing the scans separately, which might have led to a higher sensitivity and specificity due to less missed diagnoses. We do, however, believe our approach to assess only the CT diagnoses established by different radiologists with varying levels of experience more accurately reflects the everyday clinical practices, which makes it possible to extrapolate our results.
Limitations of the study
The 72-h limit to include SD CT scans was chosen after a thorough preliminary assessment of 50 LD CT scans considering (a) the need for a certain length of the interval, enabling clinicians to reevaluate the patient and order a new CT scan in case of a false negative LD CT and (b) a limited interval length to minimise the risk of a significant change in the clinical situation that would result in different findings in the LD CT and the subsequent SD CT. We do, however, realise that the dynamic nature of intestinal obstruction may still have caused underestimation of the accuracy of LD CT, simply due to clinical changes in the patients' conditions between the LD CT and the following SD CT or discharge diagnosis.
The mean dose of 4.3 mSv for the LD CT scans reported in this study is higher than other studies using LD CT for abdominal issues (mean doses 1.1 mSv – 2.1 mSv).5,6,17 The reason for this discrepancy is probably that our LD-CT protocol did not include iterative reconstruction, which has the potential to lower radiation dose substantially.18
The low number of patients diagnosed with paralytic ileus in our study is possibly in part due to the high number of CT scans registered as possible intestinal obstruction, where a transition zone was not identified. Additionally, most patients presenting with paralytic ileus at our institution are in the post-operative period. We often use SD CT scans with intravenous contrast in these cases for assessing abscesses as well. These CT scans are therefore not included in the study.
Our restriction of the referring departments to include only the Department of Emergency and the Department of Surgery was chosen to make sure that the referred patients were evaluated by clinicians with amble experience in evaluating patients with abdominal conditions. Hereby, the quality of the referrals should be high, and thus it is possible that a larger part of the referred patients had positive findings of bowel obstruction and pneumoperitoneum compared to patients referred from a wider range of departments.
The determined sensitivity and specificity of LD CT compared to the retakes are less credible statistically, due to the low number of retakes – as illustrated by the wide confidence intervals. The result, however, is in good agreement with the diagnostic accuracy of LD CT compared to the discharge diagnosis and is provided as supplementary information to the main result.
Conclusion
LD CT can be recommended as the examination of choice for patients with suspected intestinal obstruction or perforation to reduce radiation dose.
Supplemental Material
Supplemental material, sj-pdf-1-arr-10.1177_2058460121989313 for Low-dose CT for diagnosing intestinal obstruction and pneumoperitoneum; need for retakes and diagnostic accuracy by Nis E Larsen, Eva Mikkelsen, Anders R Knudsen and Lars P Larsen in Acta Radiologica Open
Acknowledgements
Many thanks to M.Sc. Jesper Thygesen from the Dept. of Procurement & Clinical Engineering, Aarhus University Hospital, for calculating effective radiation doses. Also many thanks to Cand. ling. merc. Marianne Godt Hansen from Aarhus University Hospital for aiding with the scientific writing. The writing aid is provided by Aarhus University Hospital and is free of charge.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Research Ethics and Patient Consent: This study was approved by the Danish Data Protection Agency (2015-57-0002) and the Danish Patient Safety Authority (3-3013-2166/1).
ORCID iD: Nis E Larsen https://orcid.org/0000-0003-2874-3984
References
- 1.Schmidt M, Schmidt SAJ, Sandegaard JL, et al. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 2015; 7:449–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cartwright SL, Knudson MP. Diagnostic imaging of acute abdominal pain in adults. Am Fam Physician 2015; 91:452–459. [PubMed] [Google Scholar]
- 3.van Randen A, Lameris W, van Es HW, et al. A comparison of the accuracy of ultrasound and computed tomography in common diagnoses causing acute abdominal pain. Eur Radiol 2011; 21:1535–1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haller O, Karlsson L, Nyman R. Can low-dose abdominal CT replace abdominal plain film in evaluation of acute abdominal pain? Ups J Med Sci 2010; 115:113–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Udayasankar UK, Li J, Baumgarten DA, et al. Acute abdominal pain: value of non-contrast enhanced ultra-low-dose multi-detector row CT as a substitute for abdominal radiographs. Emerg Radiol 2009; 16:61–70. [DOI] [PubMed] [Google Scholar]
- 6.Alshamari M, Norrman E, Geijer M, et al. Diagnostic accuracy of low-dose CT compared with abdominal radiography in non-traumatic acute abdominal pain: prospective study and systematic review. Eur Radiol 2016; 26:1766–1774. [DOI] [PubMed] [Google Scholar]
- 7.Sundhedsstyrelsen. Udviklingen I Brug Af Røntgenundersøgelser I Danmark. Copenhagen: Sundhedsstyrelsen, https://www.sst.dk/-/media/Udgivelser/2015/Udviklingen-i-brug-af-r%C3%B8ntgenunders%C3%B8gelser-i-Danmark.ashx?la=da&hash=D543430343A6DC65C1E4C361E854191450C9D217 (2015, accessed 5 March 2020). [Google Scholar]
- 8.Tien HC, Tremblay LN, Rizoli SB, et al. Radiation exposure from diagnostic imaging in severely injured trauma patients. J Trauma 2007; 62:151–156. [DOI] [PubMed] [Google Scholar]
- 9.Niemann T, Van Straten M, Resinger C, et al. Detection of urolithiasis using low-dose CT – a noise simulation study. Eur J Radiol 2011; 80:213–218. [DOI] [PubMed] [Google Scholar]
- 10.Rob S, Bryant T, Wilson I, et al. Ultra-low-dose, low-dose, and standard-dose CT of the kidney, ureters, and bladder: is there a difference? Results from a systematic review of the literature. Clin Radiol 2017; 72:11–15. [DOI] [PubMed] [Google Scholar]
- 11.Tack D, Bohy P, Perlot I, et al. Suspected acute colon diverticulitis: imaging with low-dose unenhanced multi-detector row CT. Radiology 2005; 237:189–196. [DOI] [PubMed] [Google Scholar]
- 12.Yun SJ, Ryu C-W, Choi NY, et al. Comparison of low- and standard-dose CT for the diagnosis of acute appendicitis: a meta-analysis. AJR Am J Roentgenol 2017; 208:W198–W207. [DOI] [PubMed] [Google Scholar]
- 13.Othman AE, Bongers MN, Zinsser D, et al. Evaluation of reduced-dose CT for acute non-traumatic abdominal pain: evaluation of diagnostic accuracy in comparison to standard-dose CT. Acta Radiol 2018; 59:4–12. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization. International Classification of Disease-10th edition, version 2016. Geneva: WHO, www.who.int/classifications/icd/en (2016, accessed 5 March 2020). [Google Scholar]
- 15.MedCalc Software Ltd. Diagnostic test evaluation calculator. Ostend: MedCalc Software Ltd, https://www.medcalc.org/calc/diagnostic_test.php (accessed 5 March 2020). [Google Scholar]
- 16.Payor A, Jois P, Wilson J, et al. Efficacy of noncontrast computed tomography of the abdomen and pelvis for evaluating nontraumatic acute abdominal pain in the emergency department. J Emerg Med 2015; 49:886–892. [DOI] [PubMed] [Google Scholar]
- 17.Kim K, Kim YH, Kim SY, et al. Low-dose abdominal CT for evaluating suspected appendicitis. N Engl J Med 2012; 366:1596–1605. [DOI] [PubMed] [Google Scholar]
- 18.Tabari A, Ramandeep S, Khera RD, et al. Can fully iterative reconstruction technique enable routine abdominal CT at less than 1 mSv? Eur J Radiol open 2019; 6:225–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-arr-10.1177_2058460121989313 for Low-dose CT for diagnosing intestinal obstruction and pneumoperitoneum; need for retakes and diagnostic accuracy by Nis E Larsen, Eva Mikkelsen, Anders R Knudsen and Lars P Larsen in Acta Radiologica Open