Abstract
Objective
To describe the clinical use of patient-reported outcome measures (PROMs) and screening tools (STs) for low back pain (LBP) in clinics of chiropractic teaching institutions in the United States.
Methods
A descriptive analysis was completed with data collection achieved between June 2018 and March 2019. PROMs/STs were classified as disability/functional measures, pain measures, psychosocial measures, and other measures. Frequencies of use of PROM/ST instruments were calculated.
Results
Representatives from 18 of 19 chiropractic institutions (94.75%) provided a description of PROM/ST use for LBP in their teaching clinics. Seventeen institutions (94.4%) reported the routine clinical use of PROMs/STs for LBP. Disability/functional measures were the most common type of instruments used, followed by pain measures, psychosocial measures, and others. The 4 most common individual PROMs/STs reported were (1) Oswestry Disability Index, (2) a variation of a pain rating scale, (3) Keele STarT Back Tool, and (4) Patient Specific Functional Scale. Six out of 18 (33%) institutions reported the use of a PROM/ST specifically designed to focus on psychosocial influences.
Conclusion
Most chiropractic institution teaching clinics in the United States reported the clinical use of PROMs/STs for patients presenting with LBP. This mirrors trends in chiropractic literature of increasing use of PROMs/STs. A minority of institutions described the clinical use of a PROM/ST specifically designed to detect psychosocial influences.
Keywords: Chiropractic, Education, Patient-Reported Outcome Measures, Low Back Pain
INTRODUCTION
Low back pain (LBP) is an increasingly common and challenging global issue.1,2 The point prevalence of physically altering LBP has been estimated at approximately 540 million, or 7.3% of individuals worldwide.2 Spine-related disorders, primarily LBP, are the leading causes of disability.3 The influence of LBP is widespread, affecting high-income, middle-income, and low-income countries.2,3 The presence and impact of disabling LBP in the United States is pervasive. Chronic LBP in the United States has been estimated at 10% of the population, with a total cost association topping $200 billion annually.4 Several nonpharmacologic approaches are supported by evidence-based guidelines as treatment options for acute and chronic LBP.5 Many of these approaches are provided by doctors of chiropractic (DCs).6
A multitude of factors have been implicated as potential contributors to the development of persistent, disabling LBP, including biophysical, psychological, social, genetic, and comorbid factors.2 As scientific research strengthens the argument for a paradigm shift from the biomedical model toward the biopsychosocial (BPS) model, particularly in the management of pain, it is now generally accepted that illness and health are the result of an interaction between biological, psychological, and social factors.7 To aid in shared clinical decision making, quality assurance in health care, and potential stratification for best clinical care pathways, it is reasonable for clinicians to incorporate validated patient-reported outcome measures (PROMs) and/or screening tools (STs).8,9 Administering these tools may help facilitate communication regarding issues that are important to the patient and reflect all domains of health encompassed in the BPS model.10
LBP-related PROMs may be particularly beneficial in identifying patients' self-reported pain levels, physical capacity, and disability, and for monitoring clinical progress during a course of treatment.8,11 LBP-related STs provide useful information in identifying subpopulations of patients susceptible to the development of chronic, disabling back pain and/or to stratify patients into evidence-based treatment plans.12 For the purpose of this study, STs help identify risk and prognosis and are generally given once in the acute phase of care, while PROMs assess for disability and may be recorded periodically throughout a patient's clinical course.
Chiropractic education has been shown to have a clear impact on the practice characteristics of licensed DCs.13 It is reasonable to assume that chiropractic teaching institutions' clinical use of PROMs and STs may affect the behavior of prospective chiropractic graduates' clinical practice patterns in this area of patient management. The purpose of this descriptive analysis was to obtain the current clinical use of PROMs and STs for LBP within US chiropractic teaching institution clinics.
METHODS
Study Design
We conducted a descriptive analysis of the use of PROMs/STs for LBP in chiropractic institutions' teaching clinics in the United States (n = 19). The Parker University institutional review board (IRB) for the protection of human subjects in research approved this study (Protocol no.: A-00178). Eligibility criteria included United States–based chiropractic institutions with accreditation from the Council on Chiropractic Education.14 We included chiropractic institutions with multiple geographic campuses, and for purposes of this study accounted for each campus as a separate institution. Specifically, we sought the use of PROMs/STs at chiropractic teaching institution clinics and not at ancillary clinics, which may have an affiliation but are not owned by the chiropractic institution or available to all students (ie, Veterans Affairs clinics, private practitioner clinics with chiropractic student interns, volunteer clinics, specialty clinics). For data collection purposes, PROMs and STs were defined as instruments administered to LBP patients that were implemented and evaluated by faculty and/or chiropractic students. PROMs/STs excluded third-party mandated measures that were conducted on behalf of health insurance organizations.
Data Collection
We contacted a designated representative at each institution who oversaw the institution's teaching clinics or who was knowledgeable regarding PROM/ST use at the institution. Through a semistructured qualitative interview format, we described the study design, the voluntary nature of this study, and after obtaining consent via e-mail, asked the designated representative to share the LBP instrument(s) being used for patients with LBP and the frequency/timing of these instruments. The script is available from the authors. The IRB protocol and approval were also voluntarily shared with representatives at each institution if requested. Data were provided to the investigators via e-mail and/or phone. Data collection was completed between June 2018 and March 2019.
Data Analysis
Data were collected and transcribed to a Microsoft Excel ver. 1808 (Microsoft Corp, Redmond, WA) file. Descriptive statistics for PROMs/STs specific instruments and use at each chiropractic institution were computed. Frequencies of use of individual PROM/ST instruments were also calculated.
RESULTS
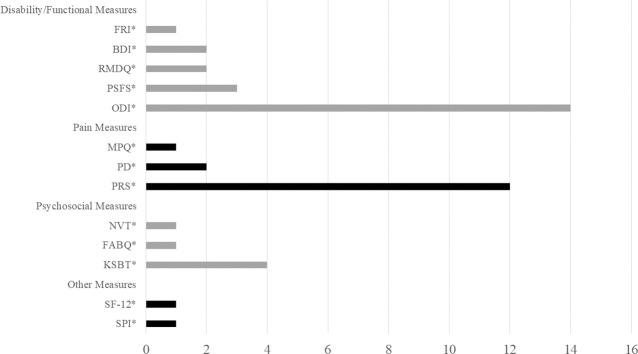
Representatives from a total of 18 eligible chiropractic institutions (94.7%) provided a description of PROMs/STs use in their teaching clinics. A total of 17 of the 18 (94.4%) participating institutions reported routine clinical use of PROMs/STs. We categorized the reported PROMs/STs into 4 measurement groups: disability/functional, pain, psychosocial, and others. As illustrated in Figure 1, a total of 13 different PROM/ST instruments were reported. Based on our categorization, disability/functional measures were the most common type of measure used (n = 22), as some institutions used more than 1 disability measure. These included Bournemouth Disability Index (BDI),15 Functional Rating Index (FRI),16 Roland Morris Disability Questionnaire (RMDQ),17 Patient Specific Functional Scale (PSFS),18 and Oswestry Low Back Pain Disability Index or Revised Oswestry (ODI).19 Pain measures were the second most commonly used measures reported (n = 15). These included McGill Pain Questionnaire (MPQ),20 Pain Diagram (PD),21 and Pain Rating Scale (PRS).22 Psychosocial measures (n = 6), and other measures (n = 2) were the least reported types of used measures. These included a nonvalidated tool for confidence, depression, passive coping, self-efficacy (NVT), Fear-Avoidance Beliefs Questionnaire (FABQ),23 and Keele STarT Back Tool (KSBT).24 Other measures (n = 2) included the Short Form-12 Item Questionnaire (SF-12)25 and Self-Perceived Improvement (SPI).
Figure 1-.
The number of chiropractic teaching institution clinics reporting use of PROMs/STs: BDI,15 FABQ,23 FRI,16 KSBT,24 MPQ,20 NVT, ODI,19 PD,21 PRS,22 PSFS,18 RMDQ,17 SF-12,25 SPI.
The KSBT was the only validated ST described to be used by 4 US chiropractic teaching institutions.24 Although the KSBT has been validated for use only at initial presentation for acute LBP,26 all 4 institutions claiming its use did so appropriately, but 3 also used it at reexamination or at end of care.
All institutions administered PROMs (n = 12 instruments) during a new patient examination or at visit 1. Follow-up occurred at all reporting institutions at evaluations on either week 2, week 4, every 30–120 days, or at a reexamination visit.
DISCUSSION
The use of PROMs/STs in chiropractic literature is increasing.8 Clohesy et al8 conducted a systematic review and found that along with self-created PROMs tailored to the desired outcome, the 4 most common standardized PROMs appearing in chiropractic literature are (1) ODI, (2) RMDQ, (3) Numerical Rating Scales, and (4) Visual Analogue Scales.7 Our study revealed some similarities, including that the 4 most commonly reported PROMs/STs were (1) ODI, (2) a variation of PRS, (3) KSBT, and (4) PSFS. Our study also identified 1 institution using a nonvalidated tool to assess for confidence, depression, passive coping, and self-efficacy.
Although the outcomes of PROM/ST use in clinical practice in the treatment of pain is not fully known, it appears they may impact clinical practice in multiple domains.11 The use of PROMs/STs in health profession education is likely an important component in developing skills for understanding the importance of objectively measuring clinical change for healthcare students, as well as supporting communication between patient and clinician.27 Furthermore, we suggest that an increased aptitude in the diverse range of PROMs/STs used in clinical practice could potentially bolster a student's awareness of social determinants of health and empower them to initiate more patient-centered conversations within the student-faculty clinic environement.28
Though multiple PROM/ST instruments contain some questions that may touch on psychosocial determinants, our study revealed only 6 out of 18 (33%) institutions reported the use of a PROM/ST specifically designed to focus on psychosocial influences related to LBP (eg, KSBT, FABQ, NVT). The BPS model, which emphasizes the assessment of psychosocial determinants of health, is increasingly recognized as the leading approach to explaining and managing pain.29 With only 1 institution identifying the correct application of the KSBT ST, the chiropractic profession may not be appreciating the BPS model to its full extent.30 Reflection of use within chiropractic institution teaching clinics may forecast the future practice habits in this area of clinical practice.13 However, it is important to note this is speculative as there remains a lack of clear understanding of the impact of PROMs/STs in clinical care,11 and chiropractic teaching institutions may be addressing psychosocial elements of patient presentation in other forms.
Limitations
Our study was limited by several factors. Information provided by a representative at each individual chiropractic institution may not have been a full description of the usage of PROMs/STs, and data collection was limited by self-report from 1 representative, leaving the potential for recall/response error. Though our study found a low use rate of PROM/ST instruments purposely aimed at capturing psychosocial factors for patients presenting with LBP, we did not collect data on other forms of potential avenues of addressing psychosocial determinants, thus limiting the ability to view the full landscape of instruction at chiropractic institutions' teaching clinics in this domain. Finally, PROM/ST use in clinical practice is not fully known. We acknowledge that we are unable to make conclusions regarding the implications of use, or lack of use, of PROMs/STs and are merely providing a descriptive overview of PROMs/STs use in US chiropractic teaching institutions.
CONCLUSION
Teaching clinics in chiropractic educational institutions in the United States are regularly implementing PROMs/STs in clinical care for patients presenting with LBP. This is reflective of the current state of literature, which shows increasing use of PROMs/STs in chiropractic studies. Few institutions described the clinical use of a PROM/ST specifically designed to detect psychosocial influences, which could reflect the chiropractic profession's failure to fully recognize the BPS model in the assessment and management of LBP.
ACKNOWLEDGMENTS
The authors thank the representatives who provided data from each participating chiropractic institution in this study.
FUNDING SOURCES AND CONFLICTS OF INTEREST
There was no funding associated with this study. The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Clark S, Horton R. Low back pain: a major global challenge. Lancet. 2018;391(10137):2302. doi: 10.1016/S0140-6736(18)30725-6. [DOI] [PubMed] [Google Scholar]
- 2.Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356–2367. doi: 10.1016/S0140-6736(18)30480-X. [DOI] [PubMed] [Google Scholar]
- 3.Global Burden of Disease, Injury, Incidence, Prevalence Collaborators. Global regional and national incidence prevalence and years lived with disability for 310 diseases and injuries 1990–2015 a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Freburger JK, Holmes GM, Agans RP, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169(3):251–258. doi: 10.1001/archinternmed.2008.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Qaseem A, Wilt TJ, McLean RM, Forciea MA; Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–530. doi: 10.7326/M16-2367. [DOI] [PubMed] [Google Scholar]
- 6.Meeker WC, Haldeman S. Chiropractic: a profession at the crossroads of mainstream and alternative medicine. Ann Intern Med. 2002;136(3):216–227. doi: 10.7326/0003-4819-136-3-200202050-00010. [DOI] [PubMed] [Google Scholar]
- 7.Wade DT, Halligan PW. The biopsychosocial model of illness: a model whose time has come. Clin Rehabil. 2017;31(8):995–1004. doi: 10.1177/0269215517709890. [DOI] [PubMed] [Google Scholar]
- 8.Clohesy NC, Schneiders AG, Eaton S. Utilization of low back pain patient reported outcome measures within chiropractic literature: a descriptive review. J Manipulative Physiol Ther. 2018;41(7):628–639. doi: 10.1016/j.jmpt.2017.11.007. [DOI] [PubMed] [Google Scholar]
- 9.Khan Y. The STarT back tool in chiropractic practice: a narrative review. Chiropr Man Therap. 2017;25:11. doi: 10.1186/s12998-017-0142-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Dulmen SA, Lukersmith S, Muxlow J, et al. Supporting a person-centred approach in clinical guidelines. A position paper of the Allied Health Community–Guidelines International Network (G-I-N) Health Expect. 2015;18(5):1543–1558. doi: 10.1111/hex.12144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holmes MM, Lewith G, Newell D, Field J, Bishop FL. The impact of patient-reported outcome measures in clinical practice for pain: a systematic review. Qual Life Res. 2017;26(2):245–257. doi: 10.1007/s11136-016-1449-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hill JC, Dunn KM, Lewis M, et al. A primary care back pain screening tool: identifying patient subgroups for initial treatment. Arthritis Rheum. 2008;59(5):632–641. doi: 10.1002/art.23563. [DOI] [PubMed] [Google Scholar]
- 13.Puhl AA, Reinhart CJ, Doan JB, McGregor M, Injeyan HS. Relationship between chiropractic teaching institutions and practice characteristics among Canadian doctors of chiropractic: a random sample survey. J Manipulative Physiol Ther. 2014;37(9):709–718. doi: 10.1016/j.jmpt.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 14.Council on Chiropractic Education. The Council on Chiropractic Education. Members. http://www.cce-usa.org/members.html Published 2019. Accessed May 7, 2019.
- 15.Bolton JE, Breen AC. The Bournemouth Questionnaire: a short-form comprehensive outcome measure. I. Psychometric properties in back pain patients. J Manipulative Physiol Ther. 1999;22(8):503–510. doi: 10.1016/s0161-4754(99)70001-1. [DOI] [PubMed] [Google Scholar]
- 16.Feise R, Menke JM. Functional rating index: literature review. Med Sci Monit. 2010. 16(2):RA25–36. [PubMed]
- 17.Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine (Phila Pa 1976) 1983;8(2):141–144. doi: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Horn KK, Jennings S, Richardson G, Vliet DV, Hefford C, Abbot JH. The patient-specific functional scale: psychometrics, clinimetrics, and application as a clinical outcome measure. J Orthop Sports Phys Ther. 2012;42(1):30–42. doi: 10.2519/jospt.2012.3727. [DOI] [PubMed] [Google Scholar]
- 19.Fairbank JC, Pysent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000;25(22):2940–2952. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 20.Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain. 1975;1(3):277–299. doi: 10.1016/0304-3959(75)90044-5. [DOI] [PubMed] [Google Scholar]
- 21.Southerst D, Cote P, Stupar M, Stern P, Mior S. The reliability of body pain diagrams in the quantitative measurement pain distribution and location in patients with musculoskeletal pain: a systematic review. J Manipulative Physiol Ther. 2013;36(7):450–459. doi: 10.1016/j.jmpt.2013.05.021. [DOI] [PubMed] [Google Scholar]
- 22.Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14(7):798–804. doi: 10.1111/j.1365-2702.2005.01121.x. [DOI] [PubMed] [Google Scholar]
- 23.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A. Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance in chronic low back pain and disability. Pain. 1993;52(2):157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 24.Keele University-STarT Back Screening Tool; https://startback.hfac.keele.ac.uk/ Published 2019. Accessed May 7, 2019. [Google Scholar]
- 25.Ware J, Jr, Kosinski M, Keller SD. A. 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Kongsted A, Andersen CH, Hansen MM, Hestbaek L. Prediction of outcome in patients with low back pain–a prospective cohort study comparing clinicians' predictions with those of the Start Back Tool. Man Ther. 2016;21:120–127. doi: 10.1016/j.math.2015.06.008. [DOI] [PubMed] [Google Scholar]
- 27.Greenhalgh J, Gooding K, Gibbons E, et al. How do patient reported outcome measures (PROMs) support clinician-patient communication and patient care? A relist synthesis. J Patient Rep Outcomes. 2018;2:42. doi: 10.1186/s41687-018-0061-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Milligan M, Wang DE, Valtis YK, et al. Implementing patient reported outcome measures in a student-faculty clinic. Free Clin Rex Collect. 2017;3:i–vii. [Google Scholar]
- 29.Edwards RR, Dworkin RH, Sullivan MD, Turk DC, Wasan AD. The role of psychosocial processes in the development and maintenance of chronic pain. J Pain. 2016;17(9 suppl):T70–92. doi: 10.1016/j.jpain.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gliedt JA, Schneider MJ, Evans MW, King J, Eubanks JE., Jr The biopsychosocial model and chiropractic: a commentary with recommendations for the chiropractic profession. Chiropr Man Therap. 2017;25:16. doi: 10.1186/s12998-017-0147-x. [DOI] [PMC free article] [PubMed] [Google Scholar]