Abstract
Background and Objectives:
Medical consultation by a specialist physician consists of an evaluation to review diagnosis and management of patients with some neurological conditions referred from other specialty wards. This mode of care delivery has gained relevance in the field of neurology and adequate training on it is valuable, allowing neurologists to provide state-of-the-art management to patients with neurological manifestations. The present study aimed to characterize neurology consults and to discuss the roles of the neurologist within a hospital setting.
Methods:
A prospective analysis of neurological consultations provided to inpatients of a university hospital in São Paulo, Brazil, was performed from September 2016 to September 2017. These patients were followed by the principal investigator, who was not involved in their care.
Results:
We evaluated data from 117 female and 106 male inpatients with a mean age of 53.8 ± 2.4. The medical specialties that most frequently requested neurological consultations were Internal Medicine (17%), Cardiology (11.2%) and Pulmonology (9.4%). The main reasons for a neurology consultation request were seizures (15.6%); decreased level of consciousness (8.9%) and confusion (7.1%). The most frequent diagnosis in patients receiving a neurology consult were stroke (10.2%); hypoxic-ischemic encephalopathy (5.3%) and sepsis (2.2%).
Conclusion:
Our findings show the growing importance of the role of neurologists within hospital settings as many medical conditions present with neurological manifestations and the significance of the neurohospitalist model of care.
Keywords: consultation, internal medicine, neurology
Introduction
Medical consultation by a specialist physician consists of an evaluation to review diagnosis and management of patients receiving care in other specialty wards. This mode of care delivery has gained attention in care centers and hospitals due to its importance for education and patient care. Consultation-liaison is a term that was introduced in Brazil in the 1980s with the Psychiatric Care Reform and is understood as a care action originated in the field of mental health. At that time, the first psychiatric care units were implemented within general hospitals, and consultations focused on mental health interventions.1,2
Charlson et al. examined the role of general practitioners involved in the preoperative or postoperative evaluation of surgical patients. The most common reason (around 50%) for requesting consultations was management of chronic conditions including hypertension, diabetes and heart failure preoperatively.3
In a 2015 study, R. Monte-Secades et al. draw attention to consultations provided by internal medicine specialists to hospitalized patients, especially surgical inpatients. They argued this mode of care delivery has grown in recent years due to increased medical knowledge fragmentation into subspecialties and loss of a generalist view as well as more complex cases and comorbidities as a result of an increase in people’s life expectancy.4
The present study aimed to characterize the requests of neurology consultation services in a tertiary university hospital and to understand the roles of the neurologist within a hospital setting based on a neurohospitalist model of care.
Methods
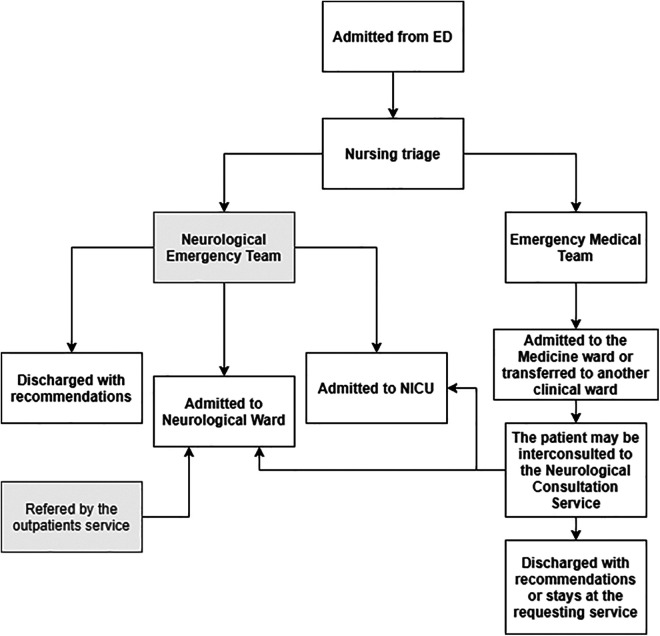
This is an observational retrospective study of data collected from records of consultations provided by resident doctors from September 2016 to September 2017. The study was based on information from 223 patients admitted to specialty wards of the Universidade Federal de São Paulo University Hospital during the study period for whom were requested neurological consultations through the hospital paging system. There were excluded patients receiving care at the emergency department (ED), general intensive care unit (ICU) and in the neurology department (ED, ward and ICU). Patients were evaluated by Neurology Consultation Service (NCS) via a standard form available at our institutional medical records application. A workflow with rule of admission and consults request is portrayed in the Figure 1.
Figure 1.
Workflow of admission of patient to the neurological ward and the neurological consultation service. ED = Emergency Department; NICU = Neurological Intensive Care Unit.
Our center is a tertiary university hospital with 753 active beds, including 74 beds in the ICU and 9 beds dedicated to the Neurological ICU (NICU); also, there are 8 beds in the Neurological wards. Our Emergency Neurology Service has admitted around 2,500 patients/month, including consults and urgent care appointments. The Emergency Neurological Service is comprised by a staff, residents and fellows, with full time working (24 hours in a day). The Neurology Consultation team is comprised by 5 staffs and residents, that evaluate inpatient from Monday to Friday, while weekend and holidays are covered by Emergency Neurology Service. The criteria to request a neurological consultation team is decided by other medical specialties, and there is no restriction.
Patients
Data was collected from electronic clinical charts using a specific form. Variables of interest included age, sex, requesting medical specialty, mortality rates, reason for neurology consult, initial diagnosis and final diagnosis. This study was approved by the institutional review board
Statistical Analysis
Data were tabulated and data analyses involved descriptive statistics using a test for the equality of 2 proportions and confidence intervals for the mean. There was set a significance level of 0.05 (5%) with 95% confidence intervals. Statistical analysis was performed with SPSS 25 software (Chicago, Ill., USA).
Results
Demographic and Clinical Features
We reviewed information from 223 patients over a study period of 12 months. There were 117 female (52.4%) and 106 male inpatients (47.5%) with a mean age of 53.8 ± 2.4 years (ranging from 13 to 89 years). Of these patients, 16.3% died while being evaluated or after the consultation and 83.7% were followed up at our outpatient clinic or referred back to the referral services for follow-up after hospital discharge.
Characteristics and Requests of Consultation Service
Medical specialties that most frequently requested neurological consultation services for evaluation of hospitalized patients during the study period were Internal Medicine (17%), Cardiology (11.2%), Pulmonology (9.4%) and Infectious diseases (7.6%).
The main reasons for requesting neurological consultations per medical specialty were: seizures (13.1%), decreased level of consciousness (13.1%) and confusion (13.1%) listed on Table 1. The main final diagnosis after neurological consultations are listed on Table 2.
Table 1.
Main Reasons for Requesting Neurological Consultations by Medical Specialty.
| Reason for consult (%) | Internal medicine | Cardiology | Pulmonology | Infectious diseases |
|---|---|---|---|---|
| Headache | 0 | 0 | 5.9 | 10 |
| Movement disorders | 10.5 | 4 | 5.8 | 10 |
| Behavioral disturbances | 0 | 0 | 0 | 5 |
| Confusion | 13.1 | 8 | 0 | 5 |
| Muscle weakness | 5.2 | 4 | 0 | 5 |
| Decreased level of consciousness 13.1 | 24 | 17.6 | 5 | |
| Seizures | 13.1 | 16 | 17.6 | 15 |
Table 2.
Main Final Diagnosis After Neurological Consultations by Medical Specialty.
| Final diagnosis | Internal medicine | Cardiology | Pulmonology | Infectious diseases |
|---|---|---|---|---|
| Stroke | 13.1 | 16 | 5.8 | 0 |
| Hypoxic-ischemic encephalopathy | 2.6 | 28 | 17.6 | 0 |
| Sepsis | 2.6 | 0 | 5.8 | 0 |
| Delirium | 5.2 | 8 | 0 | 0 |
| Meningoencephalitis | 5.2 | 0 | 0 | 0 |
Discussion
Neurological consultation plays a relevant role in care of hospitalized patients in a large public university hospital. This model of care is central for diagnosis, treatment and post-discharge follow-up of several patients admitted by medical specialties. Our findings underline the importance of assessing patients who present with neurological manifestations with various causes.
In our study, we observed the highest prevalence of requests by medical specialties, the most requesting ones included internal medicine, cardiology, pulmonology and infectious diseases. This prevalence can be explained by the higher number of hospitalizations for these specialties in our center, with greater variability of systemic symptoms presenting neurological manifestations, higher prevalence of hospitalizations for cerebrovascular diseases and infectious diseases with neurological symptoms. Among the main reasons for consultations, we observed a higher incidence of seizures, lowering of consciousness level and mental confusion, clinical features common to cerebrovascular events, toxic-metabolic and infectious disorders. Furthermore, among the findings of the main final diagnoses made after the neurological evaluation, we found that stroke was the main diagnosis in internal medicine, nephrology and cardiac surgery, whereas hypoxic-ischemic encephalopathy remained primarily for cardiology and pulmonology, delirium being the most prevalent picture for the transplant ward.
Chang et al. defined a neurohospitalist as a medical doctor who provides care to hospitalized patients, especially for those with acute vascular conditions.5 Thrombolytic therapy is a major milestone and stroke patients can benefit substantially from therapy, which requires immediate neurological assessment in the emergency department. They also pointed out the main causes for requesting a neurohospitalist evaluation at a tertiary care setting: ischemic stroke; encephalopathies; seizures; intracranial hemorrhage; subarachnoid bleeding; meningitis; anoxic brain injury; transient ischemic attack; and status epilepticus. They are consistent with our findings.5
In our study, the highest mortality rates were found in pulmonology (41.2%) cardiac surgery (33.3%), possibly related to pre-existing comorbidities and more severe cerebrovascular events associated with stroke and hypoxic-ischemic encephalopathy.
The aging of the population and the demand for acute care services have resulted in an increase in the number of hospitalizations and therefore higher rates of neurological complications. In our study, hospitalized patients presented several complications arising from chronic degenerative conditions including hypertension, diabetes mellitus and endocrine diseases. These conditions occur with high rates of cerebrovascular events, altered level of consciousness, seizures and movement disturbances that may be associated with fluid and electrolyte disorders, and renal and hepatic dysfunction6.
In a systematic review, Peterson et al. evaluated the impact of this new model of care by comparing hospitalist and non-hospitalist care in terms of clinical outcomes, costs, length of hospital stay and patient satisfaction.7 He found better outcomes with the hospitalist model of care because it brings together medical knowledge and hospital management which allows for cost savings, lower complication rates due to shorter hospitalization stay and higher quality of care as hospitalists can provide exclusive care to hospitalized patients and are able to identify early complications and minimize harmful outcomes.
Authors such as Shah et al. and Rennke et al. also pointed out the importance of post-hospital follow-up, as important as hospital care, for short-term patient re-evaluation, identifying possible treatment failures or diagnostic investigation, thus avoiding complications due to loss of follow-up / poor adherence and hospital readmissions.8-10
Other authors also highlight that neurological emergencies including myasthenic crisis and status epilepticus have also gained more attention further reinforcing the significant role played by the neurologist within a hospital setting.11–13 This same scenario is found in our service where neurological assessment is often requested by providers across the hospital, from the emergency department for patients with acute conditions to various specialties for hospitalized patients presenting with neurological manifestations associated with systemic conditions.
This is study has some limitations. Firstly, considering the high number of patients in our hospital, it is possible that we have some missing data. Also, some clinics may judge that neurology consultation is not necessary for simple cases. And finally, our institution is a reality from an university hospital, which can bring some bias for the final results, comparing to a private or other public hospital.
In conclusion, this study allows us to better understand the frequency, epidemiology and progression of neurological symptoms in impatient care, and also improve treatment and management of these patients. This is an interesting statistical analysis to evaluate the association between internal medicine and neurological symptoms related to each specialty. A clear understanding of our service scenarios may help medical and multidisciplinary impatient care teams to develop more effective protocols, guidelines, models of care of neurological patients and guiding training strategies in Neurology.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Statement: Full consent was obtained from the patients for this publication. This study was approved by our Ethics Institution.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Karin Mitiyo Corrêa, MD  https://orcid.org/0000-0003-3068-8996
https://orcid.org/0000-0003-3068-8996
References
- 1. Interconsulta psiquiátrica e unidades de internação psiquiátrica no Brasil: uma pesquisa bibliográfica, Silva NG; Oliveira AGB; O Mundo da Saúde, São Paulo: 2010;34(2):244–251. [Google Scholar]
- 2. Fajardo AP, Farias GB. A interconsulta em serviços de atenção primária à saúde. Published 2013. Accessed November 4, 2019. http://www.convibra.com.br/artigo.asp?ev=31&id=9733
- 3. Charlson ME, Cohen RP, Sears CL. General medicine consultation. Am J Med. 1983;75(1):121–128. doi:10.1016/0002-9343(83)91175-0 [DOI] [PubMed] [Google Scholar]
- 4. Monte-Secades R, Montero-Ruiz E, Gil-Díaz A, Castiella-Herrero J. Principios generales de la interconsulta médica en enfermos hospitalizados. Revista Clínica Española. 2016;216(1):34–37. doi:10.1016/j.rce.2015.05.005 [DOI] [PubMed] [Google Scholar]
- 5. Chang I, Pratt RW. Neurohospitalists: an emerging subspecialty. Curr Neurol Neurosci Rep. 2012;12(4):481–488. doi:10.1007/s11910-012-0273-8 [DOI] [PubMed] [Google Scholar]
- 6. Shah M, Douglas V, Scott B, Josephson SA. A neurohospitalist discharge clinic shortens the transition from inpatient to outpatient care. Neurohospitalist. 2015;6(2):64–69. doi:10.1177/1941874415618707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Peterson MC. A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clin Proc. 2009;84(3):248–254. doi:10.4065/84.3.248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shah M, Douglas V, Scott B, Josephson SA. A neurohospitalist discharge clinic shortens the transition from inpatient to outpatient care. Neurohospitalist. 2015;6(2):64–69. doi:10.1177/1941874415618707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rennke S, Ranji SR. Transitional care strategies from hospital to home. Neurohospitalist. 2014;5(1):35–42. doi:10.1177/1941874414540683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ranji SR, Moriates C. Neurohospitalists and patient safety. Neurohospitalist. 2014;4(2):55–57. doi:10.1177/1941874414525171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Likosky D, Shulman S, Restrepo L, Freeman WD. Survey of neurohospitalists: subspecialty definition and practice characteristics. Front Neurol. 2010;1:9. doi:10.3389/fneur.2010.00009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Aragon J, Likosky D. Models of inpatient neurologic care. Semin Neurol. 2015;35(06):716–721. [DOI] [PubMed] [Google Scholar]
- 13. Barrett KM, Freeman WD. Emerging subspecialties in neurology: neurohospitalist. Neurology. 2010;74(2):e9–e10. [DOI] [PubMed] [Google Scholar]