Abstract
Basilar artery perforator aneurysms are rare with a prevalence of less than 1%. These are particularly challenging to detect given their small size and tendency to intermittently thrombose. We describe a case of a ruptured basilar artery sidewall perforator aneurysm that was angiographically occult on computed tomographic angiogram and cerebral catheter angiogram. One day after the initial diagnostic work-up, intracranial vessel wall MR imaging (VWI) was performed which revealed a small outpouching along the right posterolateral basilar arterial wall with a punctate enhancing focus suggestive of a thrombosed basilar perforator artery aneurysm. Thrombus within the small aneurysm sac likely contributed to the poor opacification of the aneurysm sac on conventional lumen-based imaging techniques. Ruptured aneurysms have high morbidity and mortality due to their tendency to rebleed, making their expedient detection and treatment imperative. This case highlights the role VWI can play in detecting small ruptured aneurysms that intermittently thrombose and are otherwise challenging to diagnose with conventional vessel imaging.
Keywords: magnetic resonance imaging, vessel wall MR imaging, black blood MR imaging, aneurysm
Introduction
Basilar artery perforator aneurysms (BAPA) are rare, with less than 55 cases described in the literature.1 The vast majority of these aneurysms come to clinical attention after rupture and subarachnoid hemorrhage (SAH), and up to 50% of these aneurysms are missed on initial conventional imaging.1–4 Reasons for the high miss rate on conventional imaging include the very small size of the aneurysms (often 1 to 2 mm), the tendency of the aneurysm to thrombose after rupture, and the complicating factor of adjacent SAH and/or vasospasm, both of which can obscure the aneurysm sac on lumen-based imaging modalities such as computed tomography angiogram (CTA), magnetic resonance angiogram (MRA), and digital subtraction angiogram (DSA). Unfortunately, the tendency of these aneurysms to evolve or change over a short period of time and a reported re-rupture rate of 15% mandates considering some form of treatment.1 In this report, we detail our experience with intracranial vessel wall MR imaging (VWI) for the detection of a BAPA that was not visualized on CTA and catheter cerebral angiography.
Case Report
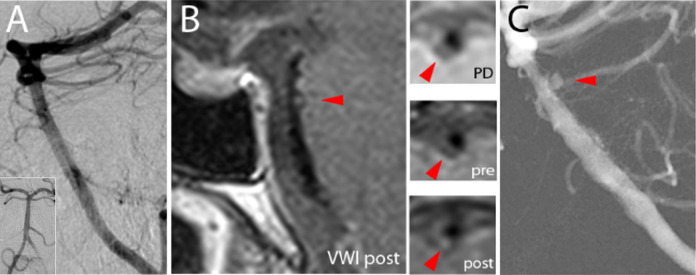
A 53-year-old man presented with acute onset worst headache of life and nausea (Hunt-Hess grade 2). A head CT revealed diffuse thick basilar and prepontine SAH tracking inferiorly into the foramen magnum with intraventricular extension, modified Fisher scale 4 (Figure 1A). An initial CTA of the head and neck did not show an aneurysm, vascular malformation, or vascular etiology of his SAH (Figure 1B). He underwent an urgent six-vessel cerebral angiogram including rotational angiography with 3D imaging, which showed no aneurysm or arteriovenous shunting. Figure 2A shows AP and lateral projections of a digital subtraction angiogram of the basilar artery, which revealed mild luminal irregularity favored to be related to underlying atherosclerosis. Otherwise no culprit lesion was identified to explain the extensive SAH. Intracranial VWI was performed 1 day later to evaluate vessel wall abnormalities of the posterior intracranial circulation. On initial review, no appreciable intimal flap, intramural hematoma or aneurysmal dilatation of the posterior circulation was identified. A repeat conventional cerebral angiogram 9 days later revealed a small 2 mm basilar artery saccular outpouching on the late arterial phase. Endovascular treatment was pursued with 2 overlapping Low-profile Visualized Intraluminal Support (LVIS) Blue braided stents (Microvention, Tustin, CA, USA), 3.5 x 17 mm and 3.5 x 22 mm, placed from the proximal posterior cerebral artery to the mid basilar artery across the inflow zone of the aneurysm. Immediately following stent placement, there was substantially decreased filling of the aneurysm. Upon re-review of the VWI, co-localizing to this site of the treated aneurysm at the distal basilar artery was a small outpouching with a crescentic rim of signal extending from the right posterolateral arterial wall. Within the sac was a punctate eccentric enhancing focus, possibly reflecting a thrombus (Figure 2B). The location and configuration suggested a thrombosed basilar perforator artery aneurysm that recanalized at the time of the repeat cerebral catheter angiogram (Figure 2C).
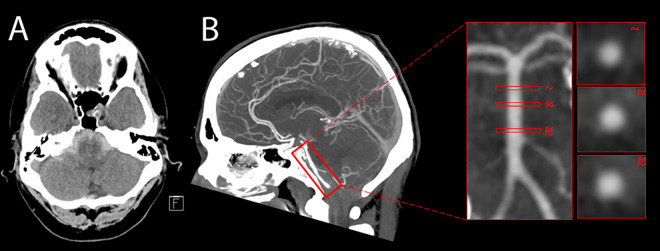
Figure 1.
A-B: (A) Axial noncontrast CT of the head showed diffuse subarachnoid hemorrhage in the posterior fossa suggesting a posterior circulation culprit lesion. (B) Sagittal maximum intensity projection of a CTA head revealed no appreciable aneurysm along the course of the basilar artery. Representative orthogonal planes of the basilar artery lumen are depicted in the insets.
Figure 2.
A-C: (A) Initial lateral projection digital subtraction angiogram of the basilar artery was unrevealing, presumably due to thrombosis of the aneurysm at the time of imaging. Inset shows an anteroposterior projection. (B) Vessel wall MR imaging showed a focal outpouching with punctate enhancement along the basilar artery posterolateral wall (arrowhead) on postcontrast imaging. Insets show axial proton density, axial T1-weighted precontrast, and axial T1-weighted postcontrast images through the basilar artery outpouching with punctate enhancement. (C) Repeat lateral projection digital subtraction angiogram of the basilar artery showed a 2 mm perforator aneurysm.
The patient was placed on dual anti-platelet therapy with a daily aspirin 325 mg and Prasugrel 10 mg. Short term CTA performed during the hospital stay confirmed patency of the overlapping stent construct. There was gradual resolution of the SAH without evidence of rebleeding. Post-intervention angiogram on day 7 showed complete obliteration of the aneurysm, Raymond-Roy class I. Post-intervention MRI brain showed small punctate infarcts in the cerebellar hemispheres, presumably embolic, which were clinically asymptomatic and managed conservatively. Conventional cerebral angiography was performed on post-SAH day 14 before discharge, confirming complete occlusion of the basilar artery perforator aneurysm and patency of the stent construction (Figure 3A and B). No new intracranial hemorrhage was present. The patient was discharged to an acute rehabilitation facility on dual antiplatelet therapy. Surveillance catheter angiogram 6 months after stent treatment continued to show occlusion of the aneurysm sac and patency of the basilar artery, and the patient was neurologically intact with a modified Rankin scale score of 0.
Figure 3.
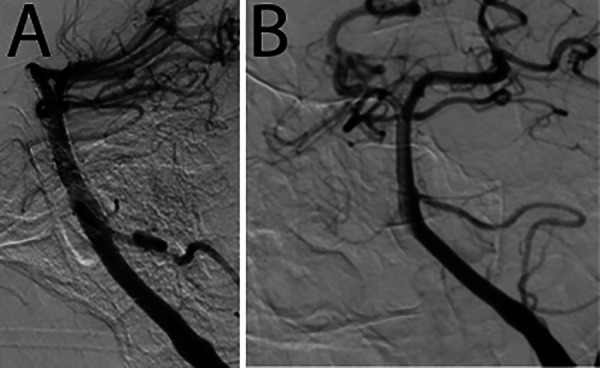
A-B: Follow-up digital subtraction angiogram of the basilar artery confirms complete occlusion of the basilar artery perforator aneurysm and patency of the stent construct seen in (A) lateral oblique and (B) anteroposterior projections.
Discussion
Perforating artery aneurysms are rare. Most have been reported in the anterior circulation, specifically in the M1 segment of the middle cerebral artery or lateral lenticulostriate arteries. Basilar artery perforator aneurysms are exceptionally rare with less than 55 cases reported in the literature since their initial description in 1996.1 These aneurysms may initially be angiographically occult both on CTA and DSA due to their small size and predilection to intermittently thrombose. Thus, confidently identifying these ruptured aneurysms is challenging and the diagnosis is often delayed. The risk of rebleeding in BAPAs poses a high degree of morbidity for these patients. As such, conclusive identification and definitive treatment of these aneurysms are imperative and prognostic. VWI may help identify angiographically occult acutely ruptured BAPAs facilitating an expedient diagnosis and treatment plan.
Intracranial VWI is a black blood MR imaging technique optimized to suppress intraluminal blood and cerebrospinal fluid to increase conspicuity of the vessel wall.5 For small aneurysms, such as perforator or blister aneurysms, imaging techniques to visualize the vessel wall can provide additional diagnostic information to conventional lumen-based techniques. The diagnostic advantage is illustrated in this basilar artery perforator aneurysm case. Increased awareness of the utility of VWI for angiogram negative SAH may improve diagnostic review by the radiologist and ultimately decrease the related morbidity and mortality of these challenging cases.
Treatment of BAPAs faces similar challenges to aneurysms elsewhere due to their very small size, which causes difficulty with aneurysm sac catheterization and microcatheter stability during endovascular procedures.6,7 The deep posterior fossa location of these aneurysms makes them much less favorable for microsurgical repair.8,9 There is also the additional consideration of perforator artery occlusion/injury during treatment, which can cause devastating brainstem ischemia when these small arteries are manipulated or occluded during surgery. Tailored flow diversion remains the cornerstone for treating these basilar side wall aneurysms. Ideal flow diversion should allow patency of perforators while promoting thrombosis of a side wall aneurysm. This is achieved with appropriate metal coverage at the site of the ruptured aneurysm origin with overlapping braided stents. A single layer of LVIS blue stent provides approximately 28% of metal coverage which can increase substantially with a double layer.10 In this case, it was sufficient to cause gradual thrombosis of the aneurysm, without compromising flow in the basilar artery perforators. With the addition of VWI for earlier diagnosis of BAPAs and overlapping stents for treatment, we may be one step closer to reducing the morbidity and mortality of an otherwise devastating neurovascular illness.
Conclusion
Basilar artery perforator aneurysms are rare with a less than 1% prevalence. These aneurysms are challenging to detect on conventional luminal imaging during the acute phase of care due to a tendency to intermittently thrombose. This case demonstrates the potential diagnostic utility of vessel wall MR imaging to help diagnose angiogram-negative ruptured aneurysms. Because perforator aneurysms may contain thrombus within the small aneurysm sac, there is often poor opacification of the aneurysm, which may not be readily apparent on conventional lumen-based imaging techniques.
Footnotes
Authors’ Note: As a single case report, IRB is waived for this manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the RSNA Research & Education Foundation, through grant number RSCH1929. The content is solely the responsibility of the authors and does not necessarily represent the official views of the RSNA R&E Foundation. This study was also funded by the Institute for Translational Medicine and Therapeutics/Thomas B. McCabe and Jeannette E. Laws McCabe Fund (JWS).
ORCID iD: Jae W. Song, MD, MS  https://orcid.org/0000-0002-3127-6427
https://orcid.org/0000-0002-3127-6427
References
- 1. Chau Y, Sachet M, Sedat J. Should we treat aneurysms in perforator arteries from the basilar trunk? Review of 49 cases published in the literature and presentation of three personal cases. Interv Neuroradiol. 2018;24(1):22–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Satti SR, Vance AZ, Fowler D, Farmah AV, Sivapatham T. Basilar artery perforator aneurysms (BAPAs): review of the literature and classification. J Neurointerv Surg. 2017;9(7):669–673. [DOI] [PubMed] [Google Scholar]
- 3. Forbrig R, Eckert B, Ertl L, et al. Ruptured basilar artery perforator aneurysms—treatment regimen and long-term follow-up in eight cases. Neuroradiol. 2016;58(3):285–291. [DOI] [PubMed] [Google Scholar]
- 4. Bhogal P, AlMatter M, Hellstern V, et al. Basilar artery perforator aneurysms: report of 9 cases and review of the literature. J Clin Neuroscie. 2019;63:122–129. [DOI] [PubMed] [Google Scholar]
- 5. Lindenholz A, van der Kolk A G, Zwanenburg JJM, Hendrikse J. The use and pitfalls of intracranial vessel wall imaging: how we do it. Radiol 2018;286(1):12–28. [DOI] [PubMed] [Google Scholar]
- 6. Lu J, Liu JC, Wang LJ, Qi P, Wang DM. Tiny intracranial aneurysms: endovascular treatment by coil embolisation or sole stent deployment. Eur J Radiol. 2012;81(6):1276–1281. [DOI] [PubMed] [Google Scholar]
- 7. Tsutsumi M, Aikawa H, Onizuka M, et al. Endovascular treatment of tiny ruptured anterior communicating artery aneurysms. Neuroradiol. 2008;50(6):509–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Maeda K, Fujimaki T, Morimoto T, Toyoda T. Cerebral aneurysms in the perforating artery manifesting intracerebral and subarachnoid haemorrhage—report of two cases. Acta Neurochir. 2001;143(11):1153–1156. [DOI] [PubMed] [Google Scholar]
- 9. Hamel W, Grzyska U, Westphal M, Kehler U. Surgical treatment of a basilar perforator aneurysm not accessible to endovascular treatment. Acta neurochir. 2005;147(12):1283–1286. [DOI] [PubMed] [Google Scholar]
- 10. Lim YC, Shin YS, Chung J. Flow diversion via LVIS blue stent within enterprise stent in patients with vertebral artery dissecting aneurysm. World Neurosurg. 2018;117:203–207. [DOI] [PubMed] [Google Scholar]