Abstract
Obesity continues be among the top health concerns across the globe. Despite our failure to contain the high prevalence of obesity, we now have a better understanding of its pathophysiology, and how excess adiposity leads to type 2 diabetes, hypertension, and cardiovascular disease. Lifestyle modification is recommended as the cornerstone of obesity management, but many patients do not achieve long-lasting benefits due to difficulty with adherence as well as physiological and neurohormonal adaptation of the body in response to weight loss. Fortunately, five drug therapies – orlistat, lorcaserin, liraglutide, phentermine/topiramate, and naltrexone/bupropion are available for long-term weight management. Additionally, several medical devices are available for short-term and long-term use. Bariatric surgery yields substantial and sustained weight loss with resolution of type 2 diabetes, although due to high cost and a small risk of serious complications, it is recommended for patients with severe obesity. Benefit-to-risk balance should guide treatment decisions.
Keywords: Obesity, overweight, adipose tissue, weight loss, antiobesity drugs, bariatric surgery
Obesity, which is broadly defined as excess bodyweight for a given height, remains a continuing global health concern, as it is associated with increased risk of numerous chronic diseases including type 2 diabetes (T2D), hypertension, and cardiovascular disease (CVD). Body-mass index (BMI; weight in kg/height in m2), the most widely used formula to define overweight (BMI 25–29.9 kg/m2) and obesity (BMI ≥30 kg/m2), while not being a true measure of adiposity, is simple to use in health screenings and epidemiological surveys. A recent analysis of data from 195 countries revealed that the prevalence of obesity has doubled in more than 70 countries since 1980 and over 600 million adults were obese in 2015 with high BMI accounting for 4 million deaths globally (1). The pathogenesis of obesity is complex with environmental, sociocultural, physiological, medical, behavioral, genetic, epigenetic factors, and numerous other factors contributing to causation as well as persistence (2).
PATHOPHYSIOLOGY
Controlling energy intake and energy expenditure are the main mechanisms by which energy balance is achieved. For this basic energetic equation, it is true that a calorie really is a calorie and all calories are equal. However, we realize that not all calories are equal when we look beyond this purely energetic consideration and consider the pathogenesis of obesity-related comorbidities. Therefore, a proper explanation of the pathophysiology of obesity includes two parallel discussions - one from an energetic and one from a nutritional standpoint. Here, we focus mainly on the former, due in large part because there is considerable consensus for the mechanisms of energy balance regulation, whereas there is confusion and controversy regarding optimal nutrient composition (3,4). The distinction between the causes and consequences of obesity must be given due consideration, as also the importance of understanding obesity-independent and obesity-dependent pathophysiology of comorbidities including CVD.
On the basis of observations that individual adult body weight is remarkably stable and refractory to short-term experimental up or down perturbations under constant environmental conditions, most scientists agree that body weight or adiposity is actively regulated or defended (5). New insights suggest that the elevated body weight/adiposity in many obese subjects is defended just as it is in normal weight subjects (6), supporting the notion that obesity is a disease, thus shifting the blame from the person to the physiology.
Genome-wide association study-based data suggest a genetic predisposition for obesity with identification of more than 140 genetic chromosomal regions related to obesity (7). Gene expression related to BMI and general adiposity is highly enriched in the central nervous system (8). However, only a few genes with a large effect size on BMI have yet been identified. These are the genes encoding components of leptin and melanocortin signaling, as well as paternally expressed genes along a specific region of chromosome 15 responsible for Prader-Willi syndrome (9). In contrast to such monogenetic cases, common obesity is thought to be associated with a large number of genes with small effect sizes.
A widely held view is that obesity results from an interaction between environment/lifestyle and genetic susceptibility. Several hypotheses have been put forward to explain the existence of obesity susceptibility genes. The ‘thrifty’ gene hypothesis posits that genes promoting energy intake and high fuel efficiency were selected over genes promoting energy-guzzling during human evolution (10). The ‘drifty’ gene hypothesis argues that the evolutionary selection pressure for genes keeping body weight/adiposity to a minimum relaxed when humans invented weapons and fire about 2 million years ago, and thus were no longer threatened by predators, with the consequence of a random drift of genes allowing increased adiposity (11).
The early origins of adult disease hypothesis suggests that obesity can develop in offspring from mothers exposed to metabolic hardship such as undernutrition, obesity and diabetes (12). One of the molecular mechanisms responsible for early life metabolic programming is epigenetic modification of genes through methylation, histone modifications, chromatin remodeling, and noncoding RNA alterations (13). Importantly, such epigenetically-determined increased risk for adult obesity can be transmitted to future generations, further accelerating the obesity epidemic. Thus, finding the tools and therapies to break the vicious circle of epigenetic programming is an important target of obesity research.
Given the disproportionally high expression of obesity-associated genes and epigenetic modifications in the central nervous system, it is highly likely that obesity genes act not only within the hypothalamic homeostatic regulator of energy balance, but also within neural circuits that are involved in interactions with an obesogenic environment, including circuits underlying reward-based decision making, learning and memory, delayed discounting, and spatial orientation.
CONTROLLING FOOD INTAKE IN AN ENVIRONMENT OF PLENTY.
While the brain primary regulates food intake, as a behavior, it relies on information from the rest of the body and from the environment to make the decision to eat or not to eat. Well over 50 years ago, seminal studies established the hypothalamus as a key hub for the detection of hunger and organization of eating behavior (14). Since then, the importance of the hypothalamus has been confirmed with much detail added to its functional and chemical anatomy (15). In addition, the importance of crosstalk (Figure 1) between the hypothalamus and other brain regions as well as with the periphery, has been recognized (16).
Figure 1. Neural Pathways and Systems Controlling Ingestive Behavior and Energy Balance.
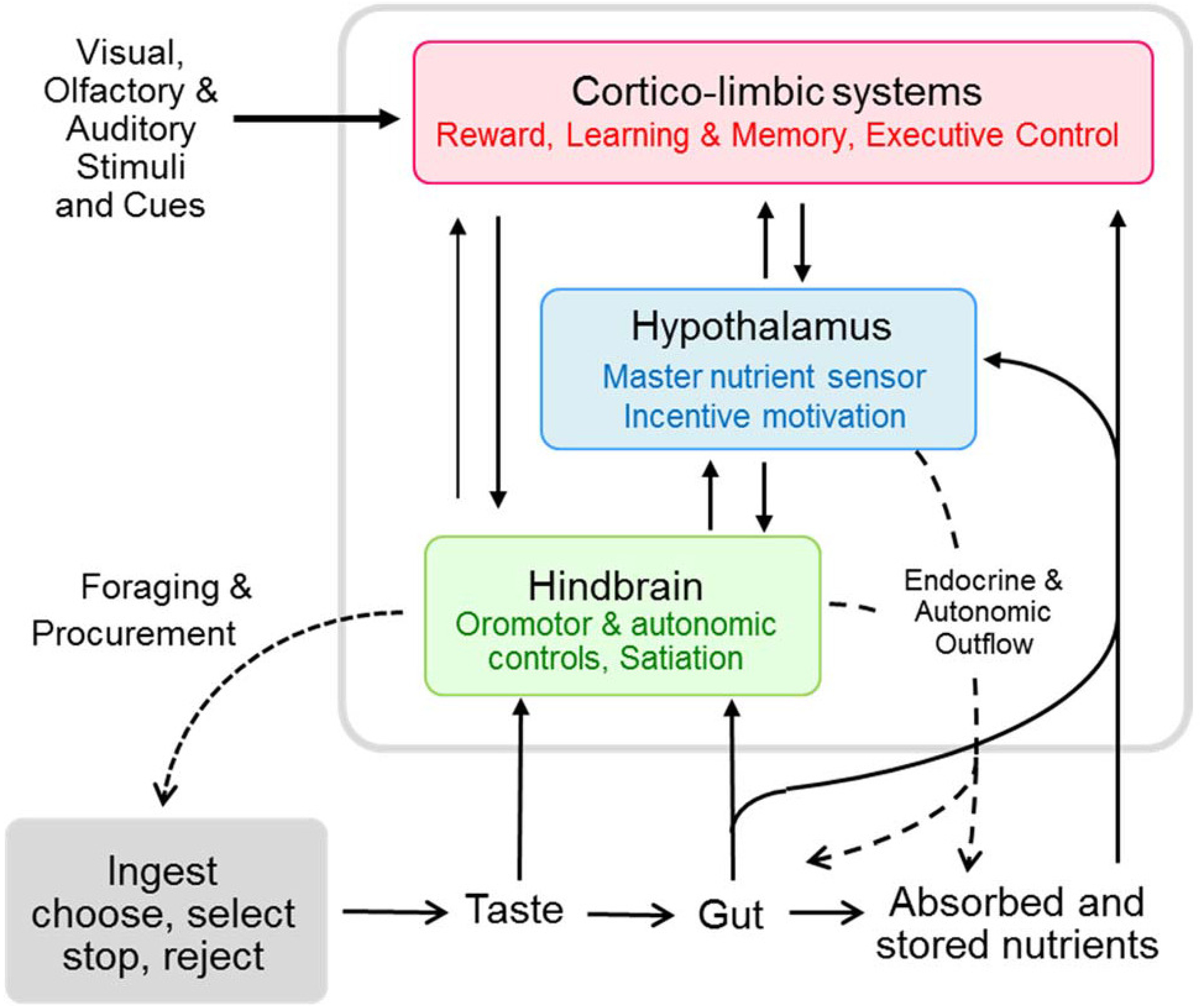
Schematic diagram shows the three heavily interconnected major brain areas constituting the core processor for the control of ingestive behavior and its relation to the gastrointestinal tract and other peripheral organs involved in energy storage and utilization. The hindbrain is mainly concerned with meal size control, as it possesses all the elements to detect sensory information mediated by vagal afferents and circulating factors, and generate motor output associated with the ingestion, digestion, and absorption of food. The cortico-limbic system, consisting of large cortical areas, basal ganglia, hippocampus, and amygdala, is intimately connected to the hypothalamus and brainstem and provides the emotional, cognitive, and executive support for ingestive behavior. The hypothalamus via its connections with the other areas is central for the drive to eat and can potently modulate peripheral organs by autonomic and endocrine outflow. Reproduced with permission from Berthoud HR et al 2017 (17).
A key function of the basomedial hypothalamus is to detect shortages in nutrient supply, both short-term and long-term, and translate them into behavior. To this end, separate groups of chemically distinct neurons (AGRP/NPY and POMC/CART) are sensitive to circulating metabolites and hormones signaling availability of energy, such as leptin, ghrelin, insulin, and glucose, in addition to neural signals reflecting the nutritional status of the gut conveyed through the vagus nerve and brainstem (5). Even though every tissue and cell has its own evolutionarily conserved energy sensor, and much of energy needs can be covered by cell and tissue-autonomous and peripheral reflexes without the brain, the hypothalamus should thus be considered a master energy sensor that integrates past, current, and future needs of the entire body with prevailing or expected environmental conditions (17). Thus, any interference with the normal functions of this hypothalamic circuitry leads to impairments in energy balance regulation, and much research effort is directed to this circuitry.
It is increasingly clear that the integrative capacity of the hypothalamus is also enriched by extensive crosstalk with other brain areas such as the cortex and limbic system, which are concerned with processing external sensory information, cognitive and emotional control, and reward-based decision making. Even before it is tasted and absorbed, food can have powerful effects on the brain through visual and olfactory stimuli. This is particularly important for humans in an environment with high food availability and constant reminders of appetizing food by conditioned stimuli and the media. Neuroimaging studies have identified several key brain nodes and networks that are differentially affected by visual food stimuli under conditions of fasting, weight loss (induced by both calorie restriction and bariatric surgery), refeeding, overfeeding, exercise, hormone infusion, leanness and obesity, as well as voluntary cognitive control (18). Besides areas obviously involved in processing of visual stimuli, a salience network, associated with the motivation, desire, and craving for food, particularly palatable and high-energy food (also referred to as ‘wanting’), consisting of areas in the frontal cortex, ventral and dorsal striatum, and amygdala was found to be more activated in obese vs. lean subjects (19). An inhibitory network centered around the dorsolateral prefrontal cortex is activated in subjects instructed to resist craving (20), and this ability of cognitive self-control is greater in patients with the highest weight loss after gastric bypass surgery (21). Furthermore, connectivity between the salience and inhibitory network and other cortical areas (referred to as hedonic controls), as well as the hypothalamus (homeostatic controls) is different in lean vs. obese subjects (22). Therefore, the classical dichotomy between homeostatic and hedonic controls has given way to a more unified and integrative or allostatic control system and an effective strategy to prevent or treat obesity based on targeting multiple pathways (17).
Regulation of intake of specific nutrients is still poorly understood, even though it has direct and powerful implications on metabolic and cardiovascular diseases. Whether the same neural system responsible for controlling total calories is also responsible for controlling intake of carbohydrates, fats, and proteins, and what conveys specificity remains to be demonstrated. The neural control of salt intake may serve as a blueprint for deciphering such specificity in the circuitry (23).
MAXIMIZING ENERGY EXPENDITURE IN THE MODERN WORLD.
Besides energy intake, energy expenditure is the other important determinant of energy balance and body weight. Much of the control of energy expenditure is tightly coupled to the controls of food intake and embedded in the powerful integrative hypothalamic energy sensor and regulator of body weight and adiposity. If we accept the notion that adult body weight is actively defended, any increase in energy expenditure will be compensated by increased energy intake. This outcome is supported by many but not all human studies using exercise to increase energy expenditure and reduce body weight (24). Thus, selective increase of energy expenditure as a strategy to reduce body weight/adiposity would only work if it can be at least partially uncoupled from this compensatory increase in food intake, and deciphering the molecular mechanisms involved in coupling energy expenditure to energy intake would go a long way in finding novel obesity therapies. Interestingly, complete uncoupling appears to occur in the activity-based rodent model of anorexia nervosa, where rodents paradoxically reduce food intake in the face of increased expenditure in a running wheel (25). Identification of this powerful uncoupling process could provide useful molecular targets for a new class of antiobesity drugs that would prevent the compensatory increase in food intake typically observed after a bout of physical activity (24). Alternatively, strategies to cognitively influence this uncoupling process would also be valuable. By not replacing, but enhancing, the effects of physical activity, such an approach would take advantage of the many other beneficial effects of exercise on cardiovascular (26) and mental health (27).
BMI, BODY SHAPE AND COMPOSITION, AND DISEASE RISK.
The patient’s size and shape can be used to estimate their risk of developing cardiovascular and other non-communicable chronic diseases. The two most available measures of body size are height and weight. As first reported in 1842 by Adolphe Quetelet, weight varies across adults as height squared (28). Several carefully analyzed large samples of men and women of variable ethnicity have largely confirmed Quetelet’s seminal observation (29). By dividing weight by height squared (kg/m2), a shape index is created that is independent of height.
The emerging area of nutritional epidemiology five decades ago prompted Ancel Keys and his colleagues to seek a simple shape index highly correlated with weight but independent of height (30). The investigators examined several shape indices relative to adiposity as assessed with underwater weighing and skinfold anthropometry methods. The highest correlation between the evaluated adiposity measures and a shape index was for weight/height2, renamed from Quetelet’s Index to BMI. Numerous studies that have since examined the relations between BMI and clinical outcomes have suggested that disease risk and mortality rates are higher in people with BMI at the low and high ends of population BMI distributions. Some debate continues on the “optimum” BMI for maintaining health and longevity (31), but there is near universal acceptance of ranges consistent with good health (32).
BMI ranges for Americans and Europeans for underweight, normal weight, overweight, and obese are <18.5, 18.5–24.9, 25–29.9, and ≥30 kg/m2, respectively (32). Various health panels (32,33) have further stratified obesity by BMI cutpoints: 30–34.9 kg/m2 (class-I), 35–39.9 kg/m2 (class-II), ≧40 kg/m2 (class-III), ≧50 kg/m2 (class-IV), and ≧60 kg/m2 (class-V). Recommended cut points for overweight and obesity lower in some Asian nations (34).
Adiposity, defined as percent fat, increases as a curvilinear function of BMI. Fat-free mass, including the mass of skeletal muscles and visceral organs, also increases in relation to BMI (29). Left ventricular (LV) mass, including LV wall thickness and internal dimensions, is larger with greater adiposity, particularly at BMI ≥30 kg/m2 (35). The risks of LV hypertrophy, hypertension, CVD, atrial fibrillation, and heart failure (HF), all increase in relation to BMI (2, 36–39). HF relative risk for every 5-unit increment in BMI was recently reported as 1.41 with a 95% confidence interval (CI) of 1.34–1.47 for HF incidence and 1.26 with a 95% CI of 0.85–1.87 for HF mortality (39). Ten- and thirty-year risk scores in simplified Framingham models include BMI as a CVD predictor variable (40).
BMI as a measure of adiposity and health outcomes at the individual level is often challenged because percent fat and risk for any given BMI can be highly variable secondary to patient sex, age, race/ethnicity, cardiovascular fitness levels, and many other factors (41,42). BMI should be evaluated as part of the initial patient assessment but interpreted with the knowledge that additional history, physical examination, and laboratory studies are important at arriving at an accurate risk assessment and treatment plan (32). Although both cross-sectional and longitudinal observations link BMI with a range of cardiovascular effects and outcomes, some controversy surrounds the “obesity paradox” (43). A number of studies report associations with obesity as defined by BMI and “protective” effects in patients in whom HF has been diagnosed (43). While the mechanisms underlying the obesity paradox are unknown, attention is now being directed at measures of body composition beyond BMI as an adiposity phenotype (43,44).
Not all adipose tissue depots appear to commute the same magnitude of chronic disease risk, an observation that launched a search for body size and shape measures with predictive value beyond BMI. Waist circumference is a body size measure that encircles subcutaneous and visceral adipose tissues, some visceral organs, skeletal muscle, and bone. Although highly correlated with BMI (Figure 2), waist circumference measurements in some studies add to or exceed the disease risk predictive value of BMI alone (45). As an example, Yusuf et al. (46) found that the odds ratio for acute myocardial infarction in a case-control study was significant for waist circumference (1.77, 95% CI 1.59–1.97) even after adjustment for BMI (p<0.0001, top versus bottom quintiles). In contrast, Aune et al. (39) found in a meta-analysis of 23 prospective studies that a 10-cm waist circumference increment (relative risk: 1.41 [95% CI, 1.34–1.47]) and a 5-unit BMI increment (1.29 [1.21–1.37]) were both associated with increased risk of HF.
Figure 2. Interrelations Among Adiposity Biomarkers.
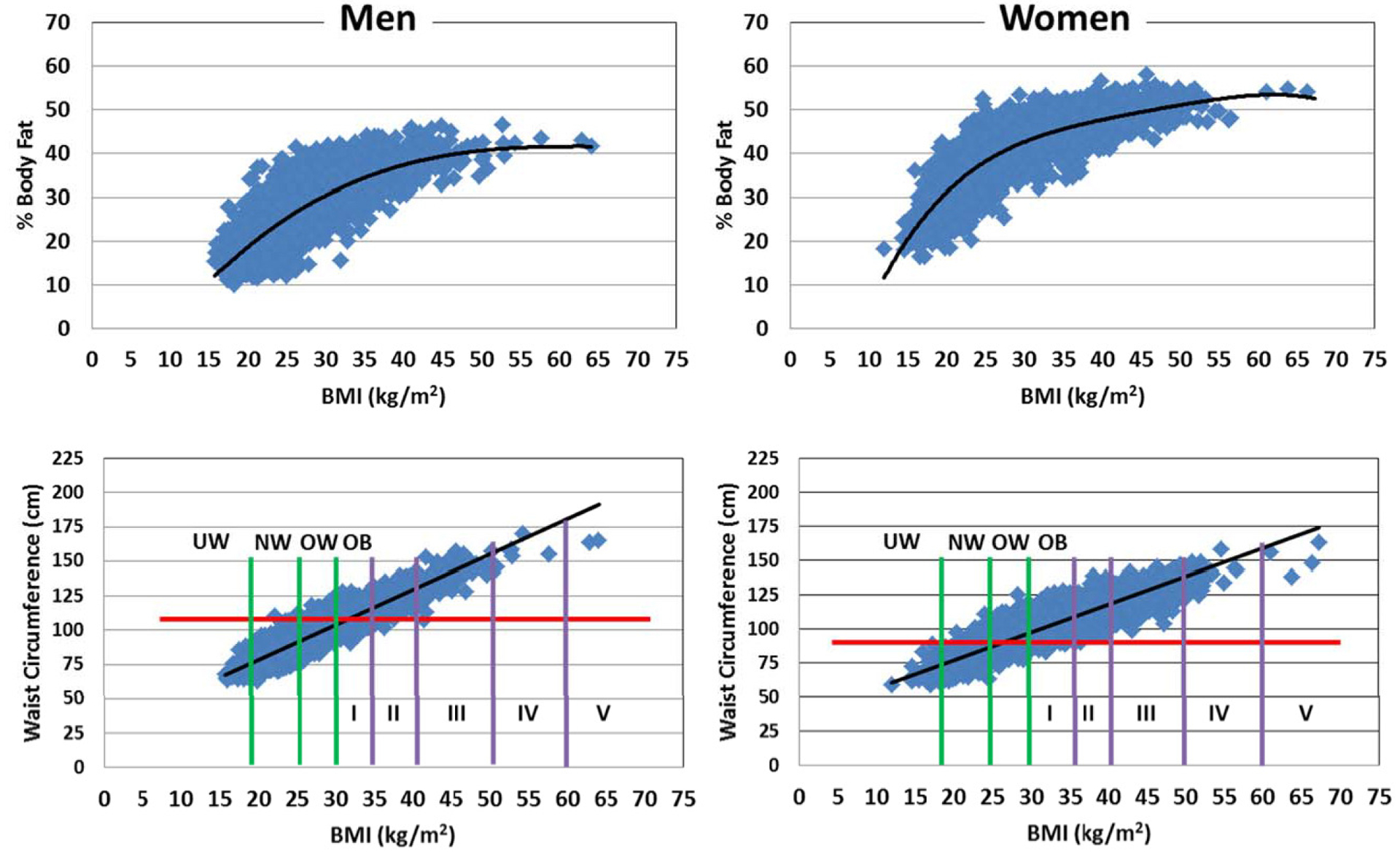
Upper Panels. Percent (%) body fat measured by dual-energy x-ray absorptiometry (DXA) versus BMI in participants of the National Health and Nutrition Survey (1999–2006). The data were fit with polynomial regression lines (R2 men, 0.61; women, 0.68; both p<0.001). Note the curvilinear relation between BMI and % fat and the wide range of % body fat at any given level of BMI. Lower Panels. Waist circumference versus BMI in the same group of subjects as in the upper panels (R2 men, 0.84; women, 0.80; both p<0.001). Horizontal lines are shown at waist circumference cut points (>102 cm men, >88 cm women) above which health risks increase within the BMI range 24.9–34.9. No additional waist circumference predictive value is present with BMI levels ≥35. Vertical lines identify BMI ranges for underweight (UW), normal weight (NW), overweight (OW), and obesity (OB) classes I to V. Definitions of severe obesity are variable in the medical literature.
The mechanistic basis (Central Illustration) attributed to the associations between waist circumference and risk is capture of patient variance in mesenteric and omental adiposity, hepatic steatosis, and other known anatomic changes linked with obesity-related pathophysiological derangements (2). At present the mixed results of studies positioning BMI against waist circumference lead us to continue support of the current obesity guidelines suggesting that waist circumference be measured in people with a BMI between 25 and 34.9 kg/m2 to refine risk prediction with levels of >88 cm and >102 cm considered high in women and men, respectively (32). Waist circumference measurements at BMI ≥35 kg/m2 add little predictive value beyond that of BMI alone as most patients already have waist circumference levels above the cutpoints (32).
CENTRAL ILLUSTRATION: Adiposity-Associated Major Risk Factors for Developing HF and Other Weight-Related Comorbidities.
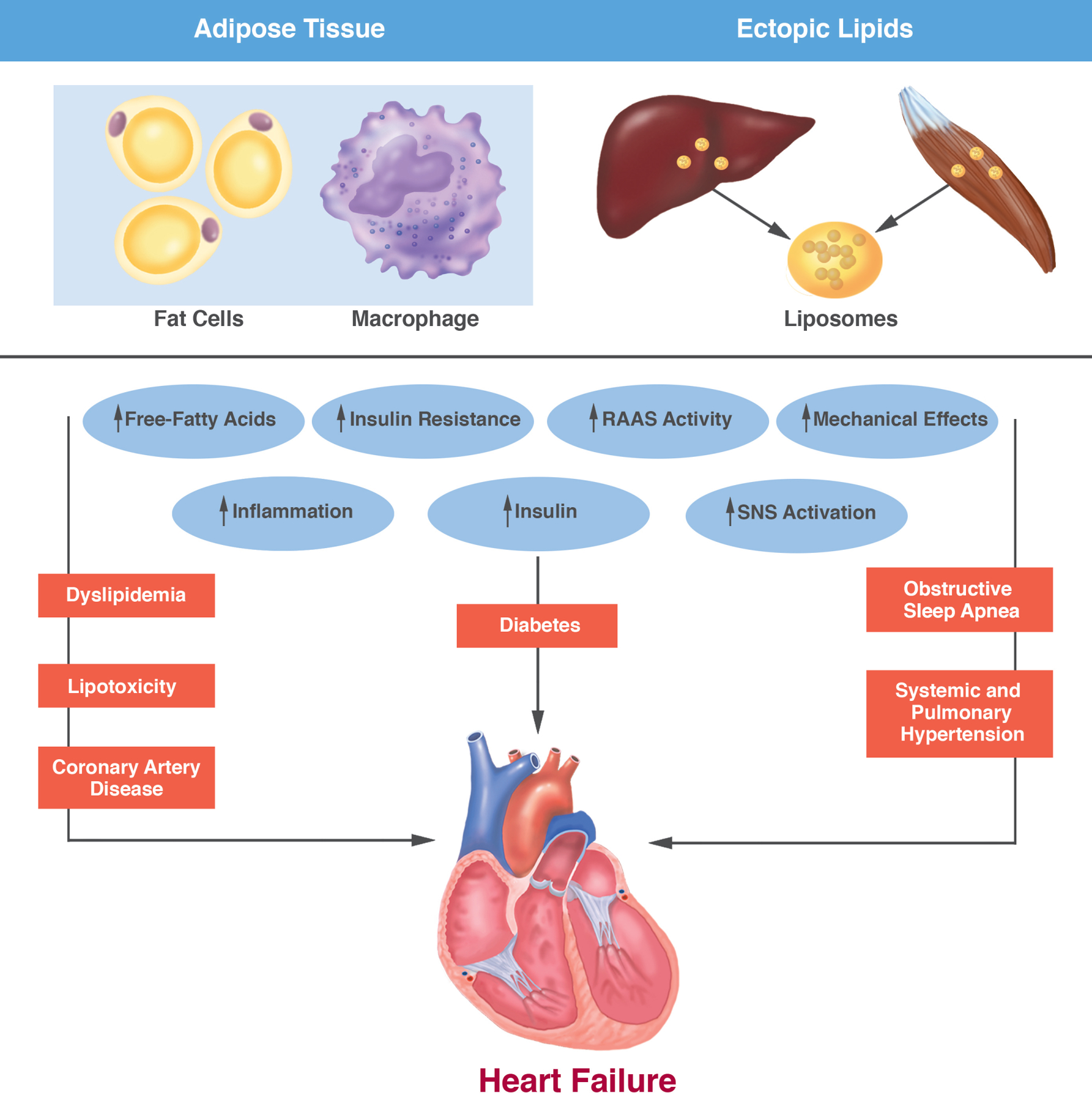
Increased plasma levels of free-fatty acids and cytokines, intracellular non-adipose tissue lipids (e.g., liposomes), and ectopic adipose tissue depots (e.g., within the visceral compartment) can contribute to systemic inflammation, insulin resistance, and over-activity of the sympathetic nervous system. The metabolic and anatomic effects of excess adiposity can lead to the development of type 2 diabetes, non-alcoholic fatty liver disease, obesity-related dyslipidemias, high blood pressure, and osteoarthritis. The cascade of these pathophysiologic mechanisms and associated diseases are the main contributors to obesity-related heart failure. RAAS, renin-angiotensin aldosterone system; SNS, sympathetic nervous system.
Several additional shape indices that include waist circumference measurements are available that purportedly show improved associations with percent body fat, visceral adiposity, health risks, and mortality rates than BMI or waist circumference alone. These include “a body shape index” (47) and the “body roundness index” (48). Other measures such as waist-to-hip circumference ratio, waist-to-height ratio, and body adiposity index have also reported to be associated with cardiovascular risk factors in some studies but not in others (46,49,50).
Although body weight, height, and circumferences are the main somatic measures that can be applied in the clinical setting, more advanced technologies can probe other lipid depots associated with CVD risk. In addition to within the visceral compartment, adipose tissue is found embedded in discrete locations around the myocardium and kidney, within skeletal muscles, and in several other anatomic sites (2, 51). Associations between the size of these adipose tissue deposits and clinical outcomes have been reported with quantification by magnetic resonance imaging (MRI), computed tomography, and echocardiography (52). Small lipid droplets, the size of which can be quantified using MRI, also reside within the cytoplasm of cardiomyocytes, skeletal muscle cells, hepatocytes, and pancreatic β-cells (52). These ectopic lipid deposits have also been linked with pathological states that include cardiomyopathies, liver diseases, and adult-onset diabetes (53).
Relatively small thermogenic brown adipose tissue deposits and beige adipocytes are present to a varying extent in adults and can be quantified with imaging methods such as positron-emission tomography and MRI (51). Thermogenic brown adipocytes are found within supraclavicular, mediastinal, and other deposits, and are characterized by mitochondria that have uncoupling protein-1 that can be stimulated through cold exposure and sympathetic nervous system mechanisms (2). Beige adipocytes, found embedded within white adipose tissue, are also thermogenic and can be activated by exercise, cold exposure, and hormonal actions (2).
MEDICAL EVALUATION OF PATIENTS WITH OBESITY
Recent practice guidelines for the management of obesity (32) recommend assessment of BMI at least annually for all adult patients seen in clinical practices. Waist circumference measurement provides additional information to determine the risk of comorbidities, especially CVD risk. For patients with overweight and obesity, standard assessment includes medical history including medical conditions and medications which could be contributing to weight gain, sleep apnea, history of weight gain, family history of obesity, dietary and physical activity habits, environmental and cultural factors impacting weight, pattern of weight changes over the years, and history of weight loss attempts; and, physical examination, blood pressure assessment, and fasting glucose and lipid measures. For patients receiving medications that are known to induce weight gain, alternative treatment choices should be considered, when possible.
MANAGEMENT OF PATIENTS WITH OBESITY
Weight loss should be recommended for all patients with obesity and also for overweight patients in the presence of comorbid conditions such as prediabetes, diabetes, hypertension and dyslipidemia. For most patients who need to lose weight for medical reasons, the initial goal should be 5%-10% weight loss over the first 6 months (32). A common theme of various professional guidelines developed in the US, Europe and elsewhere for management of patients with obesity is the emphasis on a multimodal lifestyle intervention that includes dietary changes, increase in physical activity, and behavior modification. Pharmacotherapy, medical devices and bariatric surgery are other treatment options for patients needing additional interventions. It is important to recognize that currently the diagnosis of obesity is made with a formula that uses height and weight, not on the basis of a specific biomarker. Hence, the contributing causes of obesity and its pathophysiology might not be the same all patients. Therefore, there is considerable heterogeneity of response (54) to approved and established treatments, whether these are lifestyle modifications, drug therapies or surgical interventions. In numerous analyses of the moderators and mediators of response to therapeutic interventions for obesity, the most consistent factor that appears to predict long-term weight loss success is the rate of initial weight loss (55). Hence, when employing non-surgical interventions for obesity, it would be prudent to choose an alternative or augmentation approach when the current modality has yielded less than optimal results after 3–4 months.
LIFESTYLE INTERVENTIONS
To successfully achieve clinically meaningful weight loss of 5–10%, a comprehensive intense lifestyle intervention is needed that includes at least 14 in-person sessions within 6 months (32). Effective weight loss interventions, which include dietary modification via the prescription of a calorie-reduced diet, increased exercise or physical activity, and behavioral strategies to foster adherence to dietary and physical activity recommendations, can be delivered via individual or group sessions, with both approaches being effective at promoting weight loss. Common behavioral strategies include self-monitoring of diet and physical activity, regular or daily weighing, behavioral contracts, goal setting, and stimulus control (e.g., limiting the locations where one eats). Comprehensive lifestyle interventions that incorporate portion-controlled foods and daily weighing are effective at promoting weight loss over the short and long-term (56). Face-to-face counseling is considered most effective, with electronic treatments receiving moderate strength of evidence and telephone-based treatments having low evidence (32).
After achieving initial weight loss, long-term weight loss maintenance remains challenging and continued participation in comprehensive weight loss treatment for one or more years is necessary (32). The focus of treatment during follow-up is maintaining adherence to dietary and physical activity recommendations. Weight loss maintenance is facilitated by continued and regular personal contact with professionals rather than more passive approaches, such as newsletters (56). Continued use of portion-controlled foods as part of a healthy meal plan also facilitates long-term weight loss maintenance (57). A higher level of physical activity is generally needed for weight maintenance (58), and it is important to recognize that exercise, independent of weight loss, confers significant health effects (59).
Internet-based weight loss treatments are available, though many are passive and low in treatment intensity, which likely limits their efficacy. For example, randomized participation a weight loss program delivered via a commercial website resulted in weight loss of only 1% after 4 and 12 months (60). Maintaining utilization of Internet-based interventions has proven to be challenging (61). Nonetheless, Internet-based interventions that promote more intensive treatment have been found to be more efficacious (62,63).
Weight loss applications or “apps” for smartphones and other portable devices are a logical extension of Internet-based interventions. Weight loss apps are very popular, yet only a small percentage (~15%) included 5 or more evidence-based practices for weight management (64). Despite their popularity, weight loss apps have limited evidence of efficacy (65), though smartphone-based approaches and apps that rely on evidence-based weight loss principles have been found to promote clinically meaningful weight loss that is commensurate with the amount of weight loss observed in face-to-face interventions (66).
EFFECTS OF WEIGHT LOSS ACHIEVED WITH LIFESTYLE INTERVENTIONS ON CVD.
Weight loss of 5–10% results in improvements in cardiometabolic risk factors (32). The Diabetes Prevention Program (DPP) study is the largest and longest RCT to date that examined the effect of weight loss achieved with diet and exercise on the onset of diabetes among participants who were at risk (67). The study randomized 3234 patients with prediabetes to an intensive lifestyle intervention (ILI) to promote weight loss, metformin, or placebo. Over a mean follow-up of 2.8 years, the ILI, metformin, and placebo groups lost 5.6, 2.1, and 0.1 kg, respectively. The ILI and metformin reduced the incidence of diabetes by 58% and 31% compared to placebo. At the 10-year follow-up from randomization, the metformin group maintained their modest weight loss while the ILI group regained much of their initial weight loss (68). Importantly, the ILI and metformin groups reduced diabetes incidence by 34% and 18%, respectively, compared to placebo, cumulatively over the 10-year period although the incidence rates were similar among the three groups in the 5.7-year follow-up when the ILI group experienced weight regain. These results emphasized the importance of weight loss as well as weight loss maintenance on diabetes risk.
The Look AHEAD (Action for Health in Diabetes) trial examined the effect of weight loss with lifestyle intervention among patients with established T2D. A total of 5,145 overweight/obese adults, aged 45–74 years, with T2D were randomized to an Intensive Lifestyle Intervention (ILI) or a control group consisting of diabetes support and education (DSE). At 1-year, patients assigned to ILI had greater weight loss (8.6% vs. 0.7%), greater reduction in HbA1c (7.3 to 6.6% vs. 7.3 to 7.2%), improved fitness level, and greater improvements on a host of disease risk factors, such as blood pressure and lipid profile (69). After a median 10-year follow-up when the study was stopped on the basis of a futility analysis (70), the ILI group had greater weight loss (6.0% vs 3.5%) and greater reductions in HbA1c, but there was no difference between groups (1.83 vs 1.92 events per 100 person-years; hazard ratio 0.95; 95% CI 0.83 to 1.09; P=0.51) in major adverse cardiovascular events (MACE) (death from cardiovascular causes, nonfatal myocardial infarction, nonfatal stroke, or hospitalization for angina). These results suggested that a modest weight loss (2.5% greater weight loss relative control) via diet and exercise alone might not be sufficient to reduce adverse cardiovascular events at the group level though the use of statins and improved medical management of cardiovascular disease risk factors might have diminished the differences between the groups. A recent analysis found that baseline HbA1c and general health distinguished participants who did and did not benefit from the intervention (71). This analysis revealed that 85% of participants in the intervention group averted cardiac events, but 15% had increased rate of events, which might have negatively affected the main study results.
EFFECT OF DIETS ON CVD RISK FACTORS.
Some studies find that diet type affects disease risk factors even in the context of similar weight loss. For example, a low-carbohydrate diet resulted in larger improvements in high-density lipoprotein cholesterol (HDL-C) and triglycerides after one year compared to a low-fat conventional diet, even though both diets yielded similar weight loss (72). A large subsequent study found similar results over 2 years (73). Specifically, both a low-carbohydrate and a low-fat diet promoted weight loss of ~7% over 2 years, but the low-carbohydrate diet was associated with greater increases in HDL-C levels, and had more adverse effects. Nevertheless, a meta-analysis of low-carbohydrate high-protein diets found that long-term benefits of such diets are marginal (74) and some authors have argued to end the debate over the ‘best diet’ and to focus on adherence to dietary and exercise recommendations, which is the most consistent predictor of weight loss (75). It is unlikely that any single diet works best for all people and it is conceivable that diet type interacts with personal factors to affect responses to different diets, as indicated by interest in personalized or precision medicine. At least one study has demonstrated meaningful differences in weight loss in response to diets based on baseline levels of fasting plasma glucose (FPG); specifically, people with elevated FPG levels lose more weight and better maintain weight loss with low glycemic load diets that include more whole grains and fiber (76).
The DASH (Dietary Approaches to Stop Hypertension) study compared the effects of three diets for 8 weeks on blood pressure (77). The three diets were: a control diet, a diet rich in fruits and vegetables, and a “combination diet” rich in fruits, vegetables, and low-fat dairy products with reduced saturated and total fat. Relative to control diet, the combination diet (−5.5 and −3.0 mm Hg for systolic and diastolic, respectively) and the fruit and vegetable diet (−2.7 and −1.9 mm Hg) reduced blood pressure. Similar results were obtained after adjusting for weight change. For the combination diet, the effect was larger among subjects with hypertension at baseline (−11.4 and −5.5 mm Hg vs control diet for systolic and diastolic blood pressure, respectively).
Mediterranean diets have been found to protect against cardiovascular disease in epidemiological studies. A large RCT tested the effect of two Mediterranean diets (one that was supplemented with extra-virgin olive oil and another that was supplemented with mixed nuts) compared to a control diet on the primary prevention of cardiovascular events (78) among 7447 subjects aged 55 to 80 years with a mean BMI of 30 and high CVD risk. After a median follow-up of 4.8 years, relative to the control diet, both Mediterranean diets reduced the incidence of MACE (hazard ratios 0.70 and 0.72).
In summary, weight loss achieved with diet and exercise improves cardiometabolic risk factors, reduces the incidence of diabetes, and improves glycemic control (67–69) in patients with prediabetes and diabetes, although failing to reduce MACE at the group level among patients with type 2 diabetes after 10 years in the Look AHEAD trial (70); a recent post-hoc analysis, however, found that 15% of participants in the intervention group who were characterized by mild or well treated diabetes and a negative perception of their health had increased rate of events, which might have contributed to the failure to find a mean group effect (71). Blood pressure can be improved, even without large weight loss, by eating a diet that is high in fruits, vegetables, and low-fat dairy and low in saturated fat and fat (77); however, the long-term effects of such a diet on morbidity and mortality have not been examined. For prevention of MACE in patients at high risk, the evidence to date supports Mediterranean diets supplemented with olive oil or nuts (78). Finally, the 2013 Guidelines for the Management of Overweight and Obesity in Adults specify that clinicians should consider the effects of weight loss diets on all of a patient’s risk factors and should work with nutrition professionals to prescribe a weight loss diet that addresses the needs of the individual patient (32).
PHARMACOTHERAPY
Pharmacotherapy should be a consideration for patients with a BMI of ≥30 kg/m2 and BMI of ≥27 kg/m2 with weight-related comorbidities such as T2D (32), and is the next logical therapeutic approach for patients who have historically failed to benefit from lifestyle modification approaches and for those with difficulty maintaining weight loss over the long-term. Patients should be counseled about what to expect from medications including the beneficial and adverse effects. With the exception of orlistat, all currently approved antiobesity medications help patients limit their caloric intake and achieve better compliance with their diet plan. Reduction in energy intake is achieved primarily via enhancement of satiety and reduction in hunger and food cravings (79). Since medications do not modify the choices patients make with regard to food selection, it is still important to counsel the patients about lifestyle changes, such as avoiding energy-dense foods. As is the case with all non-surgical weight loss interventions, there is some weight regain when currently approved antiobesity medications are continued beyond a year, and more weight is regained when the medication is stopped (80). Because obesity is a chronic condition, when a patient is continuing to benefit from an antiobesity medication and tolerating well, and if there are no safety issues that limit chronic use, consideration should be given to continue the medication as long as benefit outweighs risk. Clinical trials data provide very little guidance to the clinician with regard to making the right selection for a specific patient. Weight loss in the first 3–4 months is the only consistent predictor of further success with all currently available antiobesity medications. In most cases, if 5% weight loss is not achieved after 3–4 months, discontinue drug therapy, barring a few cases when there is significant improvement in comorbidities despite marginal weight loss (80).
Four medications – phentermine, diethylpropion, phendimetrazine, and benzphetamine – all structurally related to amphetamine, and approved for short-term use only, have been available for well over fifty years in the US. Phentermine is by far the most prescribed antiobesity medication in the US, perhaps due to its low-cost and ease of use. In two recent 12-week RCTs, both conducted in Korea, phentermine 30 mg/day was associated with >6% weight loss relative to placebo (81,82). In a 28-week RCT conducted in the US, phentermine 15 mg/day led to 4.4% placebo-subtracted weight loss (83). Common adverse effects of phentermine and other drugs in this class are dry mouth, constipation and insomnia. There is some abuse potential with these drugs, more so with phendimetrazine and benzphetamine.
Of the 5 medications (Table 1) currently approved in the US for long-term weight management, orlistat is the only one with a purely peripheral mechanism of action. Available since 1999 in many countries, it is a gastric and pancreatic lipase inhibitor that reduces absorption of fat in the gut, thereby decreasing caloric intake. In RCTs of 1–2 years duration, orlistat treatment leads to ~3% weight loss relative to placebo (84,85). In a 4-year RCT, orlistat treatment led to ~2.4% placebo-subtracted weight loss and decreased incidence (6.2% vs 9.0%) of diabetes among patients with obesity and prediabetes (86). Currently, orlistat is the only weight loss drug approved for use in adolescents. Despite its good safety profile, orlistat’s use is limited by its gastrointestinal adverse effects including oily stools/spotting, flatus, and fecal urgency. Patients should be advised to take daily multivitamin supplement to make up for reduced absorption of fat-soluble vitamins.
TABLE 1:
Drugs for Long-Term Weight Management
| Drug | 1-Year Weight Loss, Placebo- Subtracted | Adverse Events | Precautions | Contraindications & Limitations |
|---|---|---|---|---|
| Orlistat | ~3% | Fecal urgency, fecal incontinence, flatus with discharge, oily spotting | Daily multivitamin to make up for malabsorption of fat-soluble vitamins. | Chronic malabsorption syndrome; cholestasis. |
| Lorcaserin | 3.0–3.6% | Headache, dizziness, fatigue, nausea, dry mouth, constipation, cough, hypoglycemia in patients with diabetes | Monitor of symptoms of serotonin toxicity. Monitor for signs and symptoms of valvular heart disease. | Safety of use in patients taking antidepressants in unknown. |
| Liraglutide | 4.0–5.4% | Nausea, vomiting, diarrhea, constipation, dyspepsia, abdominal pain, headache, fatigue, hypoglycemia, increased lipase. | Causes thyroid C-cell tumors in rats and mice. Discontinue if pancreatitis is suspected. | Personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. Do not use with insulin or other GLP-1 agonists. |
| Phentermine/Topiramate | 8.6–9.3% | Paresthesia, dizziness, insomnia, dysguesia, constipation, dry mouth | Small increase in heart rate. Monitor electrolytes to detect metabolic acidosis and elevated creatinine. Monitor closely for depression, anxiety, and memory problems. | Glaucoma; hyperthyroidism; within 2 weeks of taking MAOIs. REMS requires negative pregnancy test before treatment and monthly thereafter to reduce the risk of teratogenicity. |
| Naltrexone/Bupropion | 3.3–4.8% | Nausea, vomiting, headache, dizziness, insomnia, dry mouth, diarrhea | Monitor for suicidal ideation and behavior. Monitor for increases in heart rate and blood pressure. Rare cases of hepatotoxicity. | Uncontrolled hypertension; seizure disorders; chronic opioid use; anorexia nervosa or bulimia; during withdrawal from alcohol, barbiturates, benzodiazepines, and antiepileptic drugs; within 2 weeks of taking MAOIs; co-administration with other bupropion-containing products. |
MAOIs = monoamine oxidase inhibitors; REMS = risk evaluation and mitigation strategy; Pregnancy is a contraindication for all. Lorcaserin and phentermine/topiramate are Schedule IV controlled substances. For orlistat, weight loss is based on various meta-analyses. For all others, weight losses shown are from phase 3 trials. When multiple doses were tested, weight loss shown above is for the most effective dose.
Lorcaserin is a serotonergic drug with selective agonism for 5-HT2C receptors. In three RCTs, lorcaserin treatment achieved 3.0% to 3.6% placebo-subtracted weight loss at 1-year (87–89). When lorcaserin was continued for the second year, nearly half of the weight lost was regained (87). Prescribing information for lorcaserin recommends discontinuation of the drug if weight loss is <5% after 12 weeks. Yet, in a recently published trial, only 28% of patients on lorcaserin achieved 5% weight loss at 12 weeks (90). Overall, lorcaserin is tolerated well, but its efficacy is marginal. In light of the observations of valvular heart disease in patients treated with the withdrawn serotonergic drugs fenfluramine and dexfenfluramine, echocardiographic assessments were performed in RCTs of lorcaserin revealing a relative risk of 1.16 (95% CI: 0.81 to 1.67) for the drug. FDA required a cardiovascular outcomes trial (CVOT), which is underway.
Liraglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist, approved at 1.8 mg for T2D and at a higher dose of 3.0 mg for obesity. It is administered as daily subcutaneous injection. Liraglutide results in 4.0% to 5.4% placebo-subtracted weight loss at 1-year (91,92). In one of the trials in which double-blind treatment was extended for an additional 2 years, 1.8% patients on liraglutide developed diabetes compared with 6.2% on placebo (93). In a weight maintenance trial, obese patients who lost an average 6.0% with a low-calorie diet, lost an additional 6.2% weight with liraglutide (vs. 0.2% for placebo) over a year (94). A CVOT with a median follow-up of 3.8 years demonstrated lower MACE incidence with liraglutide 1.8 mg among patients with T2D (95). Nausea and diarrhea are very common with liraglutide, especially in the first month.
Phentermine/Topiramate (PHEN/TPM) is the first combination therapy approved in the US for the treatment of obesity in 2012. Of all the currently approved antiobesity drugs, PHEN/TPM has the most robust efficacy with a placebo-subtracted 1-year weight loss of 8.6% to 9.3% at the 15/92 mg dose in two large RCTs (96,97). Topiramate, an antiepileptic drug, is reported to carry teratogenic risk of oral clefts; therefore, a negative pregnancy test is required for women of childbearing potential before starting PHEN/TPM and monthly thereafter. Paresthesia is the most common adverse effect of PHEN/TPM, especially at the start of therapy. Adverse effects related to mood and memory needs close attention of the clinician. The complex dose titration of PHEN/TPM and its potential for inducing cognitive and mood-related adverse effects requires a skilled clinician.
Naltrexone/Bupropion (NB) is the second combination therapy for obesity, approved in late 2014. In 1-year RCTs, at the recommended dose of 32/360 mg/day, NB is associated with 3.3% to 4.8% placebo-subtracted weight loss (98–100). Weight loss with NB is not associated with improvement in blood pressure or lipids. Nausea is a very frequent and bothersome adverse effect of NB therapy, leading to high dropout rates in RCTs. NB is also associated with heart rate and blood pressure increases that concerned the FDA to require a CVOT, which unfortunately was stopped due to inappropriate disclosure of data by the sponsor while the trial was ongoing (101). NB requires complex dose titration.
In summary, five medications are currently approved in the US for long-term management of obesity with placebo-subtracted weight loss ranging from ~9% for phentermine/topiramate to ~3% for lorcaserin and orlistat (102).
MEDICAL DEVICES
Seven FDA-approved medical devices (Table 2) are available for obesity management. These include two slightly different laparoscopic adjustable gastric band (LAGB) devices. We will discuss the LAGB procedures in the bariatric surgery section.
TABLE 2:
Medical Devices for Weight Management
| Device | Indications | Weight loss vs control | Adverse events | Contraindications |
|---|---|---|---|---|
| Intragastric Balloons | ||||
| Orbera | BMI 30–40 Up to 6 months |
10.2% vs 3.3% | Abdominal pain, bloating, nausea Rare cases of gastrointestinal obstruction or perforation. |
Prior GI surgery, inflammatory GI disease, gastroduodenal ulcers, large hiatal hernia, esophageal structural abnormalities, esophageal motility disorders, gastric mass, severe coagulopathy, hepatic insufficiency or cirrhosis, serious mental disorders, alcoholism or drug addiction, unable to use proton pump inhibitors during device use, or receiving aspirin, NSAIDs, or blood thinners. |
| ReShape Duo | 6.8% vs 3.3% | |||
| Obalon | 6.6% vs 3.4% (at 6 months) |
|||
| Electrical Stimulation Systems | ||||
| Maestro | BMI 35–45 Long-term use |
9.2% vs 6.0%* (at 1-year) |
Pain at neuroregulator disc site, heart burn, abdominal pain, nausea, belching | Cirrhosis, portal hypertension, esophageal varices, large hiatal hernia. |
| Gastric Emptying Systems | ||||
| AspireAssist | Aged >22 years BMI 35–55 Long-term use |
12.1% vs 3.5% (at 1-year) |
Pain, abdominal discomfort, nausea, change in bowel habits, electrolyte abnormalities, irritation or infection at site. | Prior GI surgery, esophageal stricture, severe gastroparesis, inflammatory GI disease, severe ulcers or bleeding conditions, or gastric masses, chronic abdominal pain, coagulation disorders, moderate-to-severe anemia, hepatic insufficiency or cirrhosis, serious pulmonary or cardiovascular disease, eating disorders, physical or mental disability that could affect compliance, poor general health. |
Control was sham stimulation. BMI = body mass index; GI = gastrointestinal; NSAID = nonsteroidal anti-inflammatory drug
Three intragastric balloons are approved for use up to 6 months to assist weight loss among patients with BMI 30–40 kg/m2. Orbera is a single balloon that is introduced in the stomach via an endoscopic procedure. Once in place, the balloon is filled with 400 to 700 cc of saline to expand. Reshape is similar except it uses two balloons. Obalon is a swallowable capsule that opens once inside the stomach and the balloon is filled with air via an inflation catheter. All three gastric balloons are for use up to 6 months only. Some weight is regained in the months following removal of the devices.
The Maestro Rechargeable System is a form of vagal nerve blockage (vBLOC) that is thought to work by suppressing neural communication between the stomach and the brain, leading to increased satiety and decreased caloric intake (103). Electrodes placed on the trunks of the vagus nerve at the gastroesophageal junction are connected to a rechargeable pulse generator called neuroregulator, which is secured subcutaneously. Obviously, it is more invasive than the gastric balloons and requires surgeons skilled in laparoscopic procedures.
AspireAssist is a device that consists of a gastrostomy tube that connects to a skin-port outside of the abdomen. The patient attaches an external connector and tubing to the skin-port, opens the port valve, and flushes out food 20–30 minutes after each meal. To prevent obstruction in the tube, food needs to be thoroughly chewed. Serum electrolytes should be monitored. Some patients may need potassium supplementation. For a detailed discussion of medical devices for weight management, refer to a recent comprehensive review by Lee & Dixon (104).
BARIATRIC SURGERY
Bariatric surgery has gained considerable popularity in the past decade with about half a million procedures performed annually worldwide (105). Surgery is indicated for patients with BMI ≥40 and ≥35 in the presence of weight-related comorbidities such as T2D, with lower BMI cut-offs for LAGB. Common surgical procedures are sleeve gastrectomy (SG, 58%), Roux-en-Y gastric bypass (RYGB, 38%) laparoscopic adjustable gastric banding (LAGB, 3%) and biliopancreatic diversion with duodenal switch (BPD-DS, 1%), for which minimal outcomes data exist (106). RYBG is associated with the most weight loss in long-term follow-up studies (Table 3). In one study of 2410 patients, weight losses at 4-year follow-up for RYGB, SB and LAGB were 27%, 18%, and 11%, respectively (107).
TABLE 3:
Bariatric Surgery
| Procedure | Weight Loss* | Pros and Cons† | ||
|---|---|---|---|---|
| 1-Year | ≥ 6 years | Pros | Cons | |
| LAGB | 14–30% | 13–14% |
|
|
| RYGB | 23–43% | 25–28% |
|
|
| Sleeve Gastrectomy | 20–28% | 22% |
|
|
GERD = gastroesophageal reflux disease; LAGB = laparoscopic adjustable gastric banding; RYGB = Roux-en-Y gastric bypass; SG = sleeve gastrectomy; T2D = type 2 diabetes
Source of data: Ref 108;
Adapted from Ref 113.
Biliopancreatic diversion with duodenal switch (BPD-DS) is not listed in the table because it accounts for ~1% of bariatric surgeries.
LAGB is the least invasive of the four procedures and involves laparoscopic placement of an adjustable silicone band around the gastric fundus. Advantages of this procedure are that it can be done in an outpatient setting, has the least complications, and is reversible. Two band devices, Lap-Band and Realize, were FDA-approved. The Realize Band was discontinued in early 2017. LAGB results in 14–30% weight loss after a year (108). Although weight regain is more common with LAGB relative to other procedures, there is long-lasting benefit for some patients (104,108).
In the SG procedure, a staple line is placed along the greater curvature of the stomach followed by removal of approximately 80% of the lateral aspect of the stomach in a vertical fashion. SG has gained popularity in the past decade due to procedural ease and less frequency of serious complications (106).
In RYGB, a small stomach pouch is created in the upper stomach. The jejunum is then divided and the middle part of it, the Roux limb, is connected to the stomach pouch, thus allowing food to bypass most of the stomach. The procedure is more demanding than SG and has a slightly higher rate of complications, but is associated with the largest sustained weight loss with a very high rate of remission of T2D (109,110).
Bariatric surgery is now endorsed by leading diabetes organizations as an effective intervention for T2D with inclusion in the treatment algorithm (111) with recommendation for patients with class III obesity and for those with class II obesity whose hyperglycemia is inadequately controlled by lifestyle and medical therapy. Bariatric surgery also leads to a significant reduction in the prevalence of hypertension and dyslipidemia over a 2-year follow-up although data from RCTs of longer follow-up are inadequate (112). Serious complication rates for bariatric surgery rates have decreased over the years with recent studies showing perioperative morbidity and mortality rates of 5% and 0.3%, respectively (113,114).
CONCLUSIONS
Obesity, besides impairing quality of life, is associated with numerous chronic diseases. Fortunately, weight reduction improves management of many of these diseases, especially T2D. Although global obesity prevalence has not decreased, more therapeutic options are available today, thus improving management of patients with obesity and related comorbidities.
Acknowledgements:
The authors thank Katelyn Daigle for editorial assistance in preparing this manuscript.
Funding for this review paper: None
Disclosures: Dr. Gadde is an advisor to AstraZeneca in his role as International Coordinating Investigator for a clinical trial in diabetes with related payments made to his employer, Pennington Biomedical Research Center; he has received research support from the National Institutes of Health (NIH) and AstraZeneca, and speaking honorarium from the American Diabetes Association. Dr. Martin has served as an advisor for ACAP Health, Zafgen, Gila Therapeutics, Weight Watchers, Florida Hospital and Kitchry; he has received research funding from the NIH, Centers for Disease Control, U.S. Department of Agriculture, Ohio State University, Elizabeth Blackwell Institute for Health Research, Patient-Centered Outcomes Research Institute, Egg Board, University of Pennsylvania, Lousiana LIFT Fund, Weight Watchers, and Regents of Georgia State University, and Access Business Group International; and, royalties from his institution licensing smartphone-based technology he invented. Dr. Berthoud has received research funding from the NIH. Dr. Heymsfield received fees for serving on advisory boards from Janssen Pharmaceuticals, Tanita, Merck, and Medifast.
ABBREVIATIONS:
- AGRP
agouti-related peptide
- CART
cocaine and amphetamine regulated transcript
- CNS
central nervous system
- CVD
cardiovascular disease
- GWAS
genome-wide association studies
- MACE
major adverse cardiovascular events
- NPY
neuropeptide Y
- POMC
proopiomelanocortin
- RCT
randomized controlled trial
- RNA
ribonucleic acid
References
- 1.The GBD 2015 Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 2017;377:13–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J Med 2017;376:1492. [DOI] [PubMed] [Google Scholar]
- 3.Mozaffarian D, Ludwig DS. The 2015 US Dietary Guidelines: lifting the ban on total dietary fat. JAMA 2015;313:2421–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Souza RJ, Bray GA, Carey VJ, et al. Effects of 4 weight-loss diets differing in fat, protein, and carbohydrate on fat mass, lean mass, visceral adipose tissue, and hepatic fat: results from the POUNDS LOST trial. Am J Clin Nutr 2012;95:614–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schwartz MW, Seeley RJ, Zeltser LM, et al. Obesity pathogenesis: an Endocrine Society scientific statement. Endocr Rev 2017. [E-pub ahead of print]; 10.1210/er.2017-00111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hall KD, Guo J. Obesity energetics: body weight regulation and the effects of diet composition. Gastroenterology 2017;152:1718–1727 e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fall T, Mendelson M, Speliotes EK. Recent advances in human genetics and epigenetics of adiposity: pathway to precision medicine? Gastroenterology 2017;152:1695–1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Locke AE, Kahali B, Berndt SI, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature 2015;518:197–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Angulo MA, Butler MG, Cataletto ME. Prader-Willi syndrome: a review of clinical, genetic, and endocrine findings. J Endocrinol Invest 2015;38:1249–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Speakman JR. Thrifty genes for obesity and the metabolic syndrome- time to call off the search? Diab Vasc Dis Res 2006;3:7–11. [DOI] [PubMed] [Google Scholar]
- 11.Speakman JR. Thrifty genes for obesity, an attractive but flawed idea, and an alternative perspective: the ‘drifty gene’ hypothesis. Int J Obes (Lond) 2008;32:1611–7. [DOI] [PubMed] [Google Scholar]
- 12.Barker DJ. Developmental origins of adult health and disease. J Epidemiol Community Health 2004;58:114–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cordero P, Li J, Oben JA. Epigenetics of obesity: beyond the genome sequence. Curr Opin Clin Nutr Metab Care 2015;18:361–6. [DOI] [PubMed] [Google Scholar]
- 14.Brobeck JR. Mechanism of the development of obesity in animals with hypothalamic lesions. Physiol Rev 1946;26:541–59. [DOI] [PubMed] [Google Scholar]
- 15.Sternson SM, Eiselt AK. Three pillars for the neural control of appetite. Annu Rev Physiol 2017;79:401–423. [DOI] [PubMed] [Google Scholar]
- 16.Berthoud HR, Munzberg H. The lateral hypothalamus as integrator of metabolic and environmental needs: from electrical self-stimulation to opto-genetics. Physiol Behav 2011;104:29–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berthoud HR, Munzberg H, Morrison CD. Blaming the brain for obesity: Integration of hedonic and homeostatic mechanisms. Gastroenterology 2017;152:1728–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carnell S, Gibson C, Benson L, et al. Neuroimaging and obesity: current knowledge and future directions. Obes Rev 2012;13:43–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scholtz S, Miras AD, Chhina N, et al. Obese patients after gastric bypass surgery have lower brain-hedonic responses to food than after gastric banding. Gut 2014;63:891–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hollmann M, Hellrung L, Pleger B, et al. Neural correlates of the volitional regulation of the desire for food. Int J Obes (Lond) 2012;36:648–55. [DOI] [PubMed] [Google Scholar]
- 21.Goldman RL, Canterberry M, Borckardt JJ, et al. Executive control circuitry differentiates degree of success in weight loss following gastric-bypass surgery. Obesity (Silver Spring) 2013;21:2189–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wijngaarden MA, Veer IM, Rombouts SA, et al. Obesity is marked by distinct functional connectivity in brain networks involved in food reward and salience. Behav Brain Res 2015;287:127–34. [DOI] [PubMed] [Google Scholar]
- 23.Berthoud HR, Munzberg H, Richards BK, et al. Neural and metabolic regulation of macronutrient intake and selection. Proc Nutr Soc 2012;71:390–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Franz MJ, VanWormer JJ, Crain AL, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc 2007;107:1755–67. [DOI] [PubMed] [Google Scholar]
- 25.Madra M, Zeltser LM. BDNF-Val66Met variant and adolescent stress interact to promote susceptibility to anorexic behavior in mice. Transl Psychiatry 2016;6:e776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.King NA, Horner K, Hills AP, et al. Exercise, appetite and weight management: understanding the compensatory responses in eating behaviour and how they contribute to variability in exercise-induced weight loss. Br J Sports Med 2012;46:315–22. [DOI] [PubMed] [Google Scholar]
- 27.Hillman CH, Erickson KI, Kramer AF. Be smart, exercise your heart: exercise effects on brain and cognition. Nat Rev Neurosci 2008;9:58–65. [DOI] [PubMed] [Google Scholar]
- 28.Quetelet LAJ. A treatise on man and the development of his faculties. Knox R (translator) & Smibert T (editor). Edinburgh: William and Robert Chambers, 1842. [Google Scholar]
- 29.Heymsfield SB, Peterson CM, Thomas DM, et al. Scaling of adult body weight to height across sex and race/ethnic groups: relevance to BMI. Am J Clin Nutr 2014;100:1455–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Keys A, Fidanza F, Karvonen MJ, et al. Indices of relative weight and obesity. J Chronic Dis 1972;25:329–43. [DOI] [PubMed] [Google Scholar]
- 31.Heymsfield SB, Cefalu WT. Does body mass index adequately convey a patient’s mortality risk? JAMA 2013;309:87–8. [DOI] [PubMed] [Google Scholar]
- 32.Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol 2014;63:2985–3023. [DOI] [PubMed] [Google Scholar]
- 33.Poirier P, Cornier MA, Mazzone T, et al. Bariatric surgery and cardiovascular risk factors: a scientific statement from the American Heart Association. Circulation 2011;123:1683–701. [DOI] [PubMed] [Google Scholar]
- 34.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157–63. [DOI] [PubMed] [Google Scholar]
- 35.Lauer MS, Anderson KM, Kannel WB, et al. The impact of obesity on left ventricular mass and geometry: the Framingham Heart Study. JAMA 1991;266:231–6. [PubMed] [Google Scholar]
- 36.Davy KP, Hall JE. Obesity and hypertension: two epidemics or one? Am J Physiol Regul Integr Comp Physiol 2004;286:R803–13. [DOI] [PubMed] [Google Scholar]
- 37.Staerk L, Sherer JA, Ko D, et al. Atrial Fibrillation: Epidemiology, Pathophysiology, and Clinical Outcomes. Circ Res 2017;120:1501–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kenchaiah S, Evans JC, Levy D, et al. Obesity and the risk of heart failure. N Engl J Med 2002;347:305–13. [DOI] [PubMed] [Google Scholar]
- 39.Aune D, Sen A, Norat T, et al. Body mass index, abdominal fatness, and heart failure incidence and mortality: a systematic review and dose-response meta-analysis of prospective studies. Circulation 2016;133:639–49. [DOI] [PubMed] [Google Scholar]
- 40.Pencina MJ, D’Agostino RB Sr, Larson MG, et al. Predicting the 30-year risk of cardiovascular disease: the Framingham Heart Study. Circulation 2009;119:3078–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sun Q, van Dam RM, Spiegelman D, et al. Comparison of dual-energy x-ray absorpstiometric and anthropometric measures of adiposity in relation to adiposity-related biologic factors. Am J Epidemiol 2010;172:1442–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Church TS, LaMonte MJ, Barlow CE, et al. Cardiorespiratory fitness and body mass index as predictors of cardiovascular disease mortality among men with diabetes. Arch Intern Med 2005;165:2114–20. [DOI] [PubMed] [Google Scholar]
- 43.Carbone S, Lavie CJ, Arena R. Obesity and heart failure: focus on the obesity paradox. Mayo Clin Proc 2017;92:266–79. [DOI] [PubMed] [Google Scholar]
- 44.Prado CM, Gonzalez MC, Heymsfield SB. Body composition phenotypes and obesity paradox. Curr Opin Clin Nutr Metab Care 2015;18:535–51. [DOI] [PubMed] [Google Scholar]
- 45.Shen W, Punyanitya M, Chen J, et al. Waist circumference correlates with metabolic syndrome indicators better than percentage fat. Obesity (Silver Spring) 2006;14:727–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yusuf S, Hawken S, Ounpuu S, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet 2005;366:1640–9. [DOI] [PubMed] [Google Scholar]
- 47.Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PLoS One 2012;7:e39504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thomas DM, Bredlau C, Bosy-Westphal A, et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity 2013;21:2264–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dhana K, Kavousi M, Ikram MA, et al. Body shape index in comparison with other anthropometric measures in prediction of total and cause-specific mortality. J Epidemiol Community Health 2016;70:90–6. [DOI] [PubMed] [Google Scholar]
- 50.Bergman RN, Stefanovski D, Buchanan TA, et al. A better index of body adiposity. Obesity (Silver Spring). 2011;19:1083–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shen W, Wang Z, Punyanita M, et al. Adipose tissue quantification by imaging methods: a proposed classification. Obes Res 2003;11:5–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Heymsfield SB, Hu HH, Shen W, et al. Emerging technologies and their applications in lipid compartment measurement. Trends Endocrinol Metab 2015;26:688–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wolf P, Winhofer Y, Krššák M, et al. Heart, lipids, and hormones. Endocr Connect 2017;6:R59–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gadde KM, Allison DB. Combination therapy for obesity and metabolic disease. Curr Opin Endocrinol Diabetes Obes 2009;16:353–8. [DOI] [PubMed] [Google Scholar]
- 55.Elfhag, Rossner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev 2005;6:67–85. [DOI] [PubMed] [Google Scholar]
- 56.Wing RR, Tate DF, Gorin AA, et al. A self-regulation program for maintenance of weight loss. N Engl J Med 2006;355:1563–71. [DOI] [PubMed] [Google Scholar]
- 57.Rock CL, Flatt SW, Sherwood NE, et al. Effect of a free prepared meal and incentivized weight loss program on weight loss and weight loss maintenance in obese and overweight women: a randomized controlled trial. JAMA 2010;304:1803–10. [DOI] [PubMed] [Google Scholar]
- 58.Hill JO, Wyatt HR. Role of physical activity in preventing and treating obesity. J App Physiol 2005;99:765–70. [DOI] [PubMed] [Google Scholar]
- 59.Thompson PD, Buchner D, Piña IL, et al. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease. Circulation 2003;107:3109–16. [DOI] [PubMed] [Google Scholar]
- 60.Womble LG, Wadden TA, McGuckin BG, et al. A randomized controlled trial of a commercial internet weight loss program. Obes Res 2004;12:1011–8. [DOI] [PubMed] [Google Scholar]
- 61.Stewart T, Han H, Allen RH, et al. H.E.A.L.T.H.: Efficacy of an internet/population-based behavioral weight management program for the U. S. Army. J Diabetes Sci Technol 2011;5:178–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tate DF, Jackvony EH, Wing RR. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: a randomized trial. JAMA 2003;289:1833–6. [DOI] [PubMed] [Google Scholar]
- 63.Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an Internet weight loss program. Arch Intern Med 2006;166:1620–5. [DOI] [PubMed] [Google Scholar]
- 64.Breton ER, Fuemmeler BF, Abroms LC. Weight loss—there is an app for that! But does it adhere to evidence-informed practices? Transl Behav Med 2011;1:523–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Thomas JG, Bond DS. Review of innovations in digital health technology to promote weight control. Curr Diab Rep 2014;14:485. [DOI] [PubMed] [Google Scholar]
- 66.Martin CK, Miller AC, Thomas DM, et al. Efficacy of SmartLoss, a smartphone-based weight loss intervention: results from a randomized controlled trial. Obesity (Silver Spring) 2015;23:935–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Diabetes Prevention Program Research Group, Knowler WC, Barrett-Connor E, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Diabetes Prevention Program Research Group, Knowler WC, Fowler SE, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 2009;374:1677–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Look AHEAD Research Group, Pi-Sunyer X, Blackburn G, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the Look AHEAD trial. Diabetes Care 2007;30:1374–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.LookAHEAD Research Group, Wing RR, Bolin P, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med 2013;369:145–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Baum A, Scarpa J, Bruzelius E, et al. Targeting weight loss interventions to reduce cardiovascular complications of tpe 2 diabetes: a machine learning-based post-hoc analysis of heterogeneous treatment effects in the Look AHEAD trial. Lancet Diabetes Endocrinol 2017;5:808–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Foster GD, Wyatt HR, Hill JO, et al. A randomized trial of a low-carbohydrate diet for obesity. N Engl J Med 2003;348:2082–90. [DOI] [PubMed] [Google Scholar]
- 73.Foster GD, Wyatt HR, Hill JO, et al. Weight and metabolic outcomes after 2 years on a low-carbohydrate versus low-fat diet: a randomized trial. Ann Intern Med 2010;153:147–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Clifton PM, Condo D, Keogh JB. Long term weight maintenance after advice to consume low carbohydrate, higher protein diets- a systematic review and meta analysis. Nutr Metabo Cardiovasc Dis 2014;24:224–35. [DOI] [PubMed] [Google Scholar]
- 75.Pagoto SL, Appelhans BM. A call for an end to the diet debates. JAMA 2013;310:687–8. [DOI] [PubMed] [Google Scholar]
- 76.Hjorth MF, Ritz C, Blaak EE, et al. Pretreatment fasting plasma glucose and insulin modify dietary weight loss success: results from 3 randomized clinical trials. Am J Clin Nutr 2017;106:499–505. [DOI] [PubMed] [Google Scholar]
- 77.Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med 1997;336:1117–24. [DOI] [PubMed] [Google Scholar]
- 78.Estruch R, Ros E, Salas-Salvadó J, et al. Primary prevention of cardiovascular disease with a Mediterranean Diet. N Engl J Med 2013;368:1279–90. [DOI] [PubMed] [Google Scholar]
- 79.Gadde KM. Current pharmacotherapy for obesity: extrapolation of clinical trials data to practice. Expert Opin Pharmacother 2014;15:809–22. [DOI] [PubMed] [Google Scholar]
- 80.Gadde KM, Raj YP. Pharmacotherapy of obesity: clinical trials to clinical practice. Curr Diab Rep 2017;17:34. [DOI] [PubMed] [Google Scholar]
- 81.Kim KK, Cho HJ, Kang HC, Youn BB, et al. Effects on weight reduction and safety of short-term phentermine administration in Korean obese people. Yonsei Med J 2006;47:614–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kang JG, Park CY, Kang JH, et al. Randomized controlled trial to investigate the effects of a newly developed formulation of phentermine diffuse-controlled release for obesity. Diabetes Obes Metab 2010;12:876–82. [DOI] [PubMed] [Google Scholar]
- 83.Aronne LJ, Wadden TA, Peterson C, et al. Evaluation of phentermine and topiramate versus phentermine/topiramate extended-release in obese adults. Obesity 2013;21:2163–71. [DOI] [PubMed] [Google Scholar]
- 84.Leblanc ES, O’Connor E, Whitlock EP, et al. Effectiveness of primary care-relevant treatments for obesity in adults: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med 2011;155:434–47. [DOI] [PubMed] [Google Scholar]
- 85.Yanovski SZ, Yanovski JA. Long-term drug treatment of obesity. A systematic and clinical review. JAMA 2014;311:74–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Torgerson JS, Hauptman J, Boldrin M, et al. XENical in the prevention of diabetes in obese subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care 2004;27:155–61. [DOI] [PubMed] [Google Scholar]
- 87.Smith SR, Weissman NJ, Anderson CM, et al. Multicenter, placebo-controlled trial of lorcaserin for weight management. N Engl J Med 2010;363:245–56. [DOI] [PubMed] [Google Scholar]
- 88.Fidler MC, Sanchez M, Raether B, et al. A one-year randomized trial of lorcaserin for weight loss in obese and overweight adults: The BLOSSOM Trial. J Clin Endocrinol Metab 2011;96:3067–77. [DOI] [PubMed] [Google Scholar]
- 89.O’Neil PM, Smith SR, Weissman NJ, et al. Randomized placebo-controlled clinical trial of lorcaserin for weight loss in type 2 diabetes mellitus: The BLOOM-DM Study. Obesity 2012;20:1426–36. [DOI] [PubMed] [Google Scholar]
- 90.Smith SR, Garvey WT, Greenway FL, et al. Coadministration of lorcaserin and phentermine for weight management: a 12-week, randomized, pilot safety study. Obesity 2017;25:857–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Pi-Sunyer X, Astrup A, Fujioka K, et al. A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N Engl J Med 2015, 373:11–22. [DOI] [PubMed] [Google Scholar]
- 92.Davies MJ, Bergenstal R, Bode B, et al. Efficacy of liraglutide for weight loss among patients with type 2 diabetes: the SCALE Diabetes randomized clinical trial. JAMA 2015;314:687–99. [DOI] [PubMed] [Google Scholar]
- 93.le Roux CW, Astrup A, Fujioka K, et al. 3 years of liraglutide versus placebo for type 2 diabetes risk reduction and weight management in individuals with prediabetes: a randomised, double-blind trial. Lancet 2017;389:1399–1409. [DOI] [PubMed] [Google Scholar]
- 94.Wadden TA, Hollander P, Klein S, et al. Weight maintenance and additional weight loss with liraglutide after low-calorie-diet induced weight loss: The SCALE Maintenance randomized study. Int J Obes 2013;37:1443–51. [DOI] [PubMed] [Google Scholar]
- 95.Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2016;375:311–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Allison DB, Gadde KM, Garvey WT, et al. Controlled-release phentermine/topiramate in severely obese adults: a randomized controlled trial (EQUIP). Obesity 2012;20:330–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gadde KM, Allison DB, Ryan DH, et al. Effects of low-dose, controlled-release, phentermine plus topiramate combination on weight and associated comorbidities in overweight and obese adults (CONQUER): a randomised, placebo-controlled, phase 3 trial. Lancet 2011;377:1341–52. [DOI] [PubMed] [Google Scholar]
- 98.Greenway FL, Fujioka K, Plodkowski RA, et al. Effect of naltrexone plus bupropion on weight loss in overweight and obese adults (COR-1): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2010;376:595–605. [DOI] [PubMed] [Google Scholar]
- 99.Wadden TA, Foreyt JP, Foster GD, et al. Weight loss with naltrexone SR/bupropion SR combination therapy as an adjunct to behavior modication: the COR-BMOD trial. Obesity 2011;19:110–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hollander P, Gupta AK, Plodkowski R, et al. Effects of naltrexone sustained-release/bupropion sustained-release combination therapy on body weight and glycemic parameters in overweight and obese patients with type 2 diabetes. Diabetes Care 2013;36:4022–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Nissen SE, Wolski KE, Prcela L, et al. Effect of naltrexone-bupropion on major adverse cardiovascular events in overweight and obese patients with cardiovascular risk factors: a randomized clinical trial. JAMA 2016, 315:990–1004. [DOI] [PubMed] [Google Scholar]
- 102.Khera R, Murad MH, Chandar A, et al. Association of pharmacological treatments for obesity with weight loss and adverse effects: a systematic review and meta-analysis. JAMA 2016;315:2424–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ikramuddin S, Blackstone RP, Brancatisano A, et al. Effect of reversible intermittent intra-abdominal vagal nerve blockade on morbid obesity: the ReCharge randomized clinical trial. JAMA 2014;312:915–22. [DOI] [PubMed] [Google Scholar]
- 104.Lee PC, Dixon J. Medical devices for the treatment of obesity. Nat Rev Gastroenterol Hepatol 2017. [E-pub ahead of print]; doi: 110.1038/nrgastro.2017.80. [DOI] [PubMed] [Google Scholar]
- 105.Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg 2015;25:1822–32. [DOI] [PubMed] [Google Scholar]
- 106.Khorgami Z, Shoar S, Andalib A, et al. Trends in utilization of bariatric surgery, 2010–2014: sleeve gastrectomy dominates. Surg Obes Relat Dis 2017;13:774–8. [DOI] [PubMed] [Google Scholar]
- 107.Maciejewski ML, Arterburn DE, Van Scoyoc, et al. Bariatric surgery and long-term durability of weight loss. JAMA Surg 2016;151:1046–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Piché ME, Auclair A, Harvey J, et al. How to choose and use bariatric surgery in 2015. Can J Cardiol 2015;31:153–66. [DOI] [PubMed] [Google Scholar]
- 109.Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes - 3-year outcomes. N Engl J Med 2014;370:2002–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ikramuddin S, Korner J, Lee WJ, et al. Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA 2013;309:2240–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Rubino F, Nathan DM, Eckel RH, et al. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by international diabetes organizations. Diabetes Care 2016;39:861–77. [DOI] [PubMed] [Google Scholar]
- 112.Beamish AJ, Olbers T, Kelly AS, et al. Cardiovascular effects of bariatric surgery. Nat Rev Cardiol 2016;13:730–43. [DOI] [PubMed] [Google Scholar]
- 113.Schauer PR, Mingrone G, Ikramuddin S, et al. Clinical outcomes of metabolic surgery: efficacy of glycemic control, weight loss, and remission of diabetes. Diabetes Care 2016;39:902–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Nguyen NT, Varela JE. Bariatric surgery for obesity and metabolic disorders: state of the art. Nat Rev Gastroenterol Hepatol 2017;14:160–9. [DOI] [PubMed] [Google Scholar]


