Abstract
The tremendous and rapid technological advances that humans have achieved in the last decade have definitely impacted how surgical tasks are performed in the operating room (OR). As a high-tech work environment, the contemporary OR has incorporated novel computational systems into the clinical workflow, aiming to optimize processes and support the surgical team. Artificial intelligence (AI) is increasingly important for surgical decision making to help address diverse sources of information, such as patient risk factors, anatomy, disease natural history, patient values and cost, and assist surgeons and patients to make better predictions regarding the consequences of surgical decisions. In this review, we discuss the current initiatives that are using AI in cardiothoracic surgery and surgical care in general. We also address the future of AI and how high-tech ORs will leverage human-machine teaming to optimize performance and enhance patient safety.
Keywords: Artificial intelligence, Machine learning, Cardiac surgical procedures
Artificial intelligence in surgery
The term artificial intelligence (AI) has a range of meanings, from specific forms of AI, such as machine learning, to the more far-fetched idea of AI that meets criteria for consciousness and sentience. AI systems range from those that seek to model human reasoning to solve a problem, to those that exclusively use large datasets to generate a framework to answer the problem of interest, to those that attempt to incorporate elements of human reasoning but do not require accurate modeling of human processes. Machine learning (ML) is a family of statistical and mathematical modeling techniques that uses a variety of approaches to automatically learn and improve the prediction of a target state, without explicit programming (e.g. Boolean rules). Different methods, such as Bayesian networks, random forests, deep learning, and artificial neural networks, each use different assumptions and mathematical frameworks for data input, and learning occurs within the algorithm.1
AI is increasingly important for surgical decision making to help address diverse sources of information, such as patient risk factors, anatomy, disease natural history, patient values and cost, and assist surgeons and patients to make better predictions regarding the consequences of surgical decisions.2 For instance, a deep learning model was used to predict which individuals with treatment-resistant epilepsy would most likely benefit from surgery.1, 3 AI platforms can provide roadmaps to aid the surgical team in the operating room, reducing risk and making surgery safer.4, 5 In cardiothoracic surgery, previous studies have developed machine learning algorithms that can outperform standard operative risk scores in predicting intrahospital mortality after cardiac procedures.6
In addition to planning and decision making, AI may be applied to change surgical techniques. Remote-controlled robotic surgery has been shown to improve the safety of interventions where clinicians are exposed to high doses of ionizing radiation and make surgery possible in anatomic locations not otherwise reachable by human hands.7, 8 As autonomous robotic surgery improves, it is likely that surgeons will in some cases oversee the movements of robots.9
Surgical data science
With the emergence of novel technologies and their incorporation into the operating room (OR), alongside the enormous amount of data generated through patient surgical care, a new scientific discipline called surgical data science (SDS) was created. The main goal of SDS is to improve the quality of interventional healthcare and its value by capturing, organizing, processing and modeling data.10 Within SDS, complex data can emerge from different sources, such as patients; operators involved in delivering care; sensors for measuring patient and procedure-related data; and domain knowledge. Built upon SDS, promising applications of AI and ML have been developed with the ultimate goal of supporting surgical decision-making and improving patient safety.11 Differently from more traditional data modeling approaches which are mostly based on regression techniques, SDS leverages machine learning techniques that can learn relationships between data features without much input from the human modeler. In unsupervised machine learning, for example, there are no pre-existing labels/annotations, requiring minimum human supervision. Previous supervised and unsupervised machine learning techniques have been used to assess physician competence in a variety of settings.12
A good example of how SDS can be used for quality improvement initiatives is the OR black box system.13 This analytic platform allows the capture and integration of a wide variety of intraoperative data (e.g. audio, video, physiological parameters), enabling both human- and AI-based metrics. Recent studies have been using this platform to investigate technical and non-technical surgical performance and their relationship with patient outcomes.14, 15 More recently, few studies have been able to demonstrate the feasibility and validity of machine learning algorithms to early predict intraoperative complications, such as hypotension and hypoxemia in both noncardiac5, 16 and cardiothoracic surgery.6, 17
Another data-driven application of AI in surgery concerns the assessment of intraoperative performance at both individual and team levels. Current gold standard assessments of intraoperative technical and non-technical skills are based on observation and rating by experts. Although these methods are widely used, there are many limitations related to the inherent subjectivity of these tools, suboptimal inter-rater reliability and limited reproducibility and scalability. The use of AI, especially computer vision, offers a promising opportunity to automate, standardize and scale performance assessment in surgery, including cardiothoracic surgery. Prior investigations have documented the reliability of video-based surgical motion analyses for assessing laparoscopic performance in the operating room as compared to the traditional time-intensive, human rater approach.18 Azari et al. compared expert surgeon’s rating assessments to computer-based assessments of technical skills (e.g. suturing, knot tying) including fluidity of motion, tissue handling and motion economy.19
Augmented cognition in the OR
The tremendous and rapid technological advances that humans have achieved in the last decade have definitely impacted how surgical tasks are performed in the OR. As a high-tech work environment, the contemporary OR has incorporated novel computational systems to the clinical workflow, aiming to optimize processes and support the surgical team.20 In addition to generating an enormous amount and variety of data, which can be used for developing predictive machine learning models, this complex computational-based environment has also enabled the augmentation of human cognition at both individual and team levels.21 In this high-tech OR, cognition is extended outside individuals’ minds throughout the entire surgical team, incorporating not only human agents but also non-human systems that are involved during the course of surgery.
Cardiothoracic surgery is a perfect example of how AI can be used to support surgical care through cognitive augmentation. The cardiothoracic OR is a high-risk high-stakes environment, where multiple specialized professionals interact with each other, coordinate tasks as a team, and use a variety of equipment, technological devices and interfaces to effectively care for complex patients in need of surgical treatment.22 By functioning as a complex socio-technical system, the cardiothoracic team performs tasks in a coordinated way, requiring cognitive abilities that are beyond each individual team member’s performance. Since each team member in isolation does not have control of the team performance as a whole, cognitive activities are emergent processes of teamwork rather than individual tasks.23
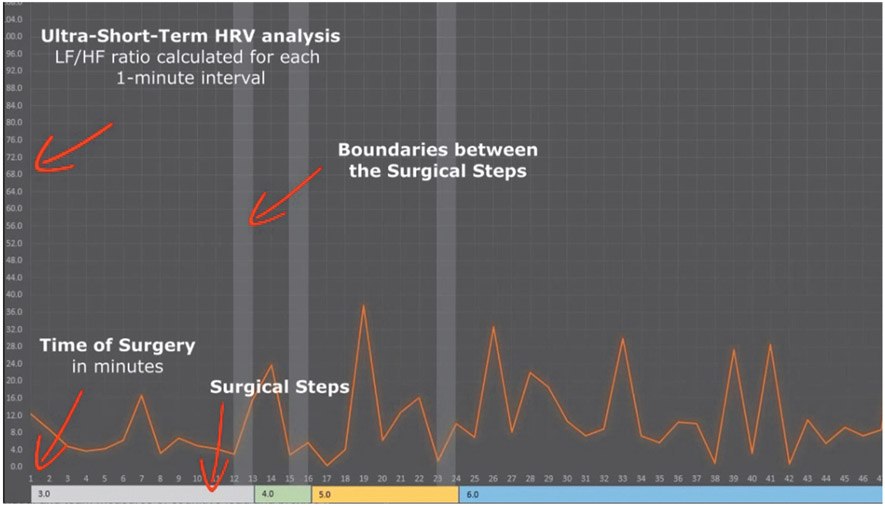
Existing AI systems are able to collect, process and make sense of information gathered in the OR.24 However, an important requirement for these systems is the ability to understand and adapt their algorithms based on real-time contextual information, enabling them to provide context-aware assistance.25, 26 Predictive accuracy is also important. In order to be able to support and guide team cognitive tasks, an AI system should anticipate future states by using past and current information from the OR’s human and non-human systems.27 In terms of cognitive augmentation in the OR, cognitive state monitoring and human activity recognition are essential features of an AI system. To monitor cognitive states at both individual and team levels, physiological metrics such as heart rate variability (HRV), electroencephalography (EEG) and near-infrared spectroscopy (NIRS) are the most used, since they allow real-time objective measures of cognitive load.28 Figure 1 displays the cardiac surgeon’s cognitive load, indexed by HRV (LF/HF ratio) during different steps of a cardiac procedure.
Figure 1.—
Surgeon’s cognitive load as measured by the HRV parameter: low frequency (LF)/high frequency (HF) ratio captured by a wearable physiological sensor.
Computer vision in surgery
In the realm of human activity recognition, computer vision is a promising AI method that can be used for surgical task segmentation and team dynamics monitoring. To encompass all the advances and future potentials of the use of AI to enhance cognition in the OR, a new interdisciplinary field called “cognitive surgery” or “cognition-guided surgery” has recently been created.25 Computer vision is a branch of AI that extracts and processes data from images and videos and provides the machine understanding of this data.29 In several fields, computer vision technologies are able to achieve human-level performance, and in certain cases even exceed human abilities.29-31
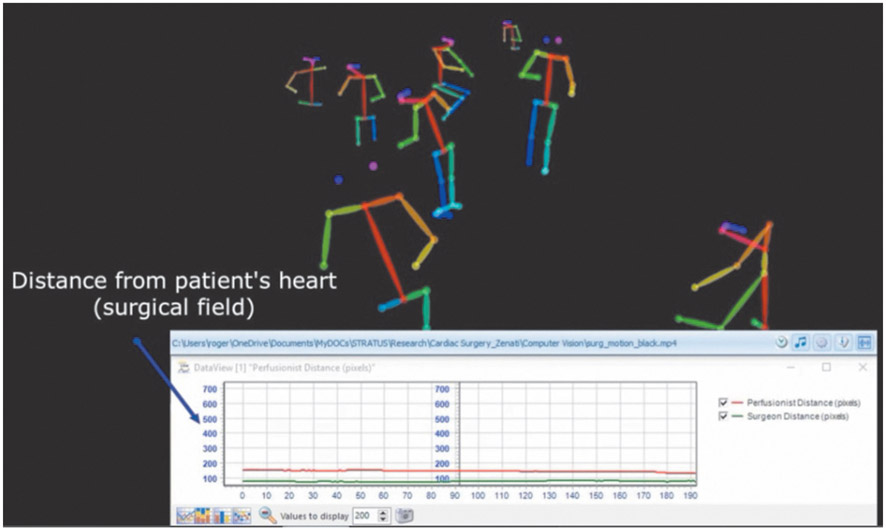
In surgery, the main applications of computer vision are related to surgical workflow segmentation,32, 33 instrument recognition and detection,34 and image-guided surgical interventions.35 However, a new area for applying computer vision in the OR, especially in team-based complex procedures, such as cardiothoracic surgery, is in the understanding of individual and team behaviors. Other fields of medicine and psychology already are using automated body position and movement tracking to investigate human non-verbal behaviors.36 In surgery, most of the applications of this technology involve tracking surgeon’s gestures and hands motion to extract objective metrics of technical psychomotor skills.37 However, recent studies have explored the use of position and motion data generated by computer vision applications to measure team dynamics and coordination in the OR. Team centrality and team proximity are examples of behavioral metrics investigated in these studies (Figure 2).37-39
Figure 2.—
Computer vision system extracting human body position and motion in the cardiac operating room.
Autonomous robotic surgery
Robotic technology is going to change the face of surgery in the near future. Robots are expected to become the standard modality for many common procedures, including coronary bypass and abdominal surgery. Autonomous and semi-autonomous modes are increasingly being investigated and implemented in surgical procedures, automating various phases of the operation. The complexity of these tasks is also shifting from the low-level automation early medical robots to high-level autonomous features, such as complex endoscopic surgical manoeuvres and shared-control approaches in stabilized image-guided beating-heart surgery. Future progress will require a continuous interdisciplinary work, with breakthroughs such as nanorobots entering the field. Autonomous robotic surgery is a fascinating field of research involving progress in artificial intelligence technology.9, 40
Machine-learning-empowered instrumentation for robotic-assisted surgery is the object of intense investigation. For ML surgical skill learning, expert knowledge is typically supplied by experienced surgeons. Implicit imitation learning is a form of supervised learning, which is usually concerned with accelerating reinforced learning through the observation of an expert mentor. The agent observes the state transitions of the experts’ actions and uses the information extracted from these observations to update its own states and actions. The mentor (surgeon) and the agent may have identical or different action capabilities, or identical or different reward structures. Several methods that have been developed for modeling human movement could be used to learn the state and actions of the expert. Human skill has been modeled from sets of recorded data using hidden Markov models, neural networks, and fuzzy nets.41
Human-machine teaming in the OR
As computational systems become ubiquitous, and our workplace is full of computer-based devices and networks, new forms of interaction, communication, and coordination have surged.42 The way computer-based systems are designed and operated in the cardiothoracic OR plays a critical role in workflow efficiency, clinicians’ cognitive load and, ultimately, surgical performance.22
When AI systems are integrated within a complex OR environment, the opportunity for human-machine teaming emerges, creating novel cognitive engineering opportunities that have the potential to enhance patient safety and improve clinical outcomes in complex team-based surgery.
Conclusions
Recent research has aimed to develop intelligent machine teammates, developing innovative computational algorithms and expanding the use of human cognitive models for AI.43 This research has produced novel forms of human-machine teaming in healthcare applications, transportation, manufacturing assembly lines and defense.44, 45
In cardiac surgery, novel systems have been developed aiming to integrate clinicians’ physiological data, as a proxy for cognitive performance, with patient data and OR medical devices.46, 47 Some studies have attempted to optimize surgical coordination and team communication by using a data-driven approach that integrates human and non-human agents to enhance safety and mitigate errors in the cardiothoracic OR.48, 49
Acknowledgments
Funding.—This study was funded by the National Insitutes of Health (NIH) (grant number R01HL126896-01A1). The NIH had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data, or preparation, review or approval of the manuscript.
Footnotes
Conflicts of interest.—The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
References
- 1.Joshi AV. Essential concepts in artificial intelligence and machine learning. Machine Learning and Artificial Intelligence. Redmond, WA: Springer; 2020. p.9–20 [Google Scholar]
- 2.Kilic A Artificial Intelligence and Machine Learning in Cardiovascular Health Care. Ann Thorac Surg 2020;109:1323–9. [DOI] [PubMed] [Google Scholar]
- 3.Gleichgerrcht E, Munsell B, Bhatia S, Vandergrift WA 3rd, Rorden C, McDonald C, et al. Deep learning applied to whole-brain connectome to determine seizure control after epilepsy surgery. Epilepsia 2018;59:1643–54. [DOI] [PubMed] [Google Scholar]
- 4.Newmarker C Digital Surgery touts artificial intelligence for the operating room ∣ Medical Design and Outsourcing. Medical Design and Outsourcing; 2018. [Internet]. Available from: https://www.medicaldesignandoutsourcing.com/digital-surgery-touts-artificial-intelligence-for-the-operating-room/ [cited 2020, Jul 16]. [Google Scholar]
- 5.Wijnberge M, Geerts BF, Hol L, Lemmers N, Mulder MP, Berge P, et al. Effect of a Machine Learning-Derived Early Warning System for Intraoperative Hypotension vs Standard Care on Depth and Duration of Intraoperative Hypotension During Elective Noncardiac Surgery: The HYPE Randomized Clinical Trial. JAMA 2020;323:l052–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Allyn J, Allou N, Augustin P, Philip I, Martinet O, Belghiti M, et al. A Comparison of a Machine Learning Model with EuroSCORE II in Predicting Mortality after Elective Cardiac Surgery: A Decision Curve Analysis. PLoS One 2017;12:e0169772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shen H, Wang C, Xie L, Zhou S, Gu L, Xie H. A novel remote-controlled robotic system for cerebrovascular intervention. Int J Med Robot 2018;14:e1943. [DOI] [PubMed] [Google Scholar]
- 8.Zhao J, Wang G, Jiang Z, Jiang C, Liu J, Zhou J, et al. Robotic Gastrotomy With Intracorporeal Suture for Patients With Gastric Gastrointestinal Stromal Tumors Located at Cardia and Subcardiac Region. Surg Laparosc Endosc Percutan Tech 2018;28:e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shademan A, Decker RS, Opfermann JD, Leonard S, Krieger A, Kim PC. Supervised autonomous robotic soft tissue surgery. Sci Transl Med 2016;8:337ra64. [DOI] [PubMed] [Google Scholar]
- 10.Maier-Hein L, Vedula SS, Speidel S, Navab N, Kikinis R, Park A, et al. Surgical data science for next-generation interventions. Nat Biomed Eng 2017;1:691–6. [DOI] [PubMed] [Google Scholar]
- 11.Loftus TJ, et al. Artificial Intelligence and Surgical Decision-Making. JAMA Surg 2019. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dias RD, Gupta A, Yule SJ. Using Machine Learning to Assess Physician Competence: A Systematic Review. Acad Med 2019;94:427–39. [DOI] [PubMed] [Google Scholar]
- 13.Goldenberg MG, Jung J, Grantcharov TP. Using Data to Enhance Performance and Improve Quality and Safety in Surgery. JAMA Surg 2017;152:972–3. [DOI] [PubMed] [Google Scholar]
- 14.Jung JJ, Jüni P, Lebovic G, Grantcharov T. First-year Analysis of the Operating Room Black Box Study. Ann Surg 2020;271:122–7. [DOI] [PubMed] [Google Scholar]
- 15.Fecso AB, Kuzulugil SS, Babaoglu C, Bener AB, Grantcharov TP. Relationship between intraoperative non-technical performance and technical events in bariatric surgery. Br J Surg 2018;105:1044–50. [DOI] [PubMed] [Google Scholar]
- 16.Lundberg SM, Nair B, Vavilala MS, Horibe M, Eisses MJ, Adams T. et al. Explainable machine-learning predictions for the prevention of hypoxaemia during surgery. Nat Biomed Eng 2018;2:749–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee HC, Yoon HK, Nam K, Cho YJ, Kim TK, Kim WH. et al. Derivation and Validation of Machine Learning Approaches to Predict Acute Kidney Injury after Cardiac Surgery. J Clin Med 2018;7:322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dosis A, Aggarwal R, Bello F, Moorthy K, Munz Y, Gillies D. et al. Synchronized video and motion analysis for the assessment of procedures in the operating theater. Arch Surg 2005;140:293–9. [DOI] [PubMed] [Google Scholar]
- 19.Azari DP, Frasier LL, Quamme SR, Greenberg CC, Pugh CM, Greenberg JA. et al. Modeling Surgical Technical Skill Using Expert Assessment for Automated Computer Rating. Ann Surg 2019;269:574–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nagy DA, Rudas IJ, Haidegger T. Surgical data science, an emerging field of medicine. Proceedings of 30th Neumann Colloquium of the IEEE; 2017 Nov 24-25; Budapest, Hungary. Winston-Salem, NC: Institute of Electrical and Electronics Engineers Inc.; 2018. [Google Scholar]
- 21.Zenati MA, Kennedy-Metz L, Dias RD. Cognitive Engineering to Improve Patient Safety and Outcomes in Cardiothoracic Surgery. Semin Thorac Cardiovasc Surg 2020;32:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wahr JA, Prager RL, Abernathy JH 3rd, Martinez EA, Salas E, Seifert PC, et al. ; American Heart Association Council on Cardiovascular Surgery and Anesthesia, Council on Cardiovascular and Stroke Nursing, and Council on Quality of Care and Outcomes Research. Patient safety in the cardiac operating room: human factors and teamwork: a scientific statement from the American Heart Association. Circulation 2013;128:1139–69. [DOI] [PubMed] [Google Scholar]
- 23.Hazlehurst B, McMullen CK, Gorman PN. Distributed cognition in the heart room: how situation awareness arises from coordinated communications during cardiac surgery. J Biomed Inform 2007;40:539–51. [DOI] [PubMed] [Google Scholar]
- 24.Hashimoto DA, Rosman G, Rus D, Meireles OR. Artificial Intelligence in Surgery: promises and Perils. Ann Surg 2018;268:70–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kenngott HG, Apitz M, Wagner M, Preukschas AA, Speidel S, Müller-Stich BP. Paradigm shift: cognitive surgery. Innov Surg Sci 2017;2:139–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vercauteren T, Unberath M, Padoy N, Navab N. CAI4CAI: The Rise of Contextual Artificial Intelligence in Computer Assisted Interventions; 2020. [Internet]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6952279/ [cited 2020, Jul 16]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Obermeyer Z, Emanuel EJ. Predicting the Future - Big Data, Machine Learning, and Clinical Medicine. N Engl J Med 2016;375:1216–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dias RD, Ngo-Howard MC, Boskovski MT, Zenati MA, Yule SJ. Systematic review of measurement tools to assess surgeons’ intraoperative cognitive workload. Br J Surg 2018;105:491–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Szeliski R Computer Vision: Algorithms and Applications. London: Springer-Verlag; 2011. [Google Scholar]
- 30.Spinrad N Google car takes the test. Nature 2014:514:528–528. [Google Scholar]
- 31.Gomes JF, Leta FR. Applications of computer vision techniques in the agriculture and food industry: a review. Eur Food Res Technol 2012;235:989–1000. [Google Scholar]
- 32.Forestier G, Lalys F, Riffaud L, Trelhu B, Jannin P. Classification of surgical processes using dynamic time warping. J Biomed Inform 2012;45:255–64. [DOI] [PubMed] [Google Scholar]
- 33.Padoy N. Machine and deep learning for workflow recognition during surgery. Minim Invasive Ther Allied Technol 2019;28:82–90. [DOI] [PubMed] [Google Scholar]
- 34.Bouget D, Allan M, Stoyanov D, Jannin P. Vision-based and marker-less surgical tool detection and tracking: a review of the literature. Med Image Anal 2017;35:633–54. [DOI] [PubMed] [Google Scholar]
- 35.Jannin P, Fitzpatrick JM, Hawkes DJ, Pennec X, Shahidi R, Vannier MW. Validation of medical image processing in image-guided therapy. IEEE Trans Med Imaging 2002;21:1445–9. [DOI] [PubMed] [Google Scholar]
- 36.Sapiro G, Hashemi J, Dawson G. Computer vision and behavioral phenotyping: an autism case study. Curr Opin Biomed Eng 2019;9:14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen J, Cheng N, Cacciamani G, Oh P, Lin-Brande M, Remulla D, et al. Objective Assessment of Robotic Surgical Technical Skill: A Systematic Review. J Urol 2019;201:461–9. [DOI] [PubMed] [Google Scholar]
- 38.Tonidandel S, King EB, Cortina JM. Big Data at Work: The Data Science Revolution and Organizational Psychology. New York, NY: Routledge; 2015. [Google Scholar]
- 39.Dias RD, Yule SJ, Kennedy-Metz L, Zenati MA. Psycho-physiological Data and Computer Vision to Assess Cognitive Load and Team Dynamics in Cardiac Surgery. Semin Thorac Cardiovasc Surg 2019;32. [Google Scholar]
- 40.Moustris GP, Hiridis SC, Deliparaschos KM, Konstantinidis KM. Evolution of autonomous and semi-autonomous robotic surgical systems: a review of the literature. Int J Med Robot 2011;7:375–92. [DOI] [PubMed] [Google Scholar]
- 41.Kassahun Y, Yu B, Tibebu AT, Stoyanov D, Giannarou S, Metzen JH, et al. Surgical robotics beyond enhanced dexterity instrumentation: a survey of machine learning techniques and their role in intelligent and autonomous surgical actions. Int J CARS 2016;11:553–68. [DOI] [PubMed] [Google Scholar]
- 42.Sharma D Toward a new foundation of human-computer interaction. Proceedings of the 3rd International Conference on Electronics Computer Technology; 2011 Apr 8-10; Kanyakumari, India. Winston-Salem, NC: Institute of Electrical and Electronics Engineers Inc; 2013. [Google Scholar]
- 43.Modares H, Ranatunga I, AlQaudi B, Lewis FL, Popa DO. Intelligent Human–Robot Interaction Systems Using Reinforcement Learning and Neural Networks. In: Wang Y, Zhang F, editors. Trends in Control and Decision-Making for Human–Robot Collaboration Systems. Cham: Springer; 2017. p.153–76. [Google Scholar]
- 44.Shah J, Wiken J, Williams B, Breazeal C. Improved human-robot team performance using chaski, a human-inspired plan execution system; 2011. [Internet]. Available from: http://motrin.media.mit.edu/robots/wp-content/uploads/sites/7/2015/01/Shah-etal-HRI-11.pdf [cited 2020, Jul 16]. [Google Scholar]
- 45.Unhelkar VV, et al. Human-Aware Robotic Assistant for Collaborative Assembly: Integrating Human Motion Prediction With Planning in Time. IEEE Robot Autom Lett 2018;3:2394–401. [Google Scholar]
- 46.Dias RD, Conboy HM, Gabany JM, Clarke LA, Osterweil LJ, Arney D, et al. Intelligent Interruption Management System to Enhance Safety and Performance in Complex Surgical and Robotic Procedures. OR 2.0 Context Aware Oper Theaters Comput Assist Robot Endosc Clin Image Based Proced Skin Image Anal (2018) 2018:11041:62–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Avrunin GS, Clarke LA, Conboy HM, Osterweil LJ, Dias RD, Yule SJ. et al. Toward Improving Surgical Outcomes by Incorporating Cognitive Load Measurement into Process-Driven Guidance. Softw Eng Healthc Syst SEHS IEEE ACM Int Workshop 2018:2018:2–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Arney D, Rance G, Rithy S, Goldman JM, Zenati MA. A Novel Interoperable Safety System for Improved Coordination and Communication in Cardiac Surgery. OR 2.0 Context Aware Oper Theaters Comput Assist Robot Endosc Clin Image Based Proced Skin Image Anal (2018) 2018;11041:39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rance G, Arney D, Srey R, Goldman JM, Zenati MA. Establishing a Ventilator-Heart Lung Machine Communication Bridge to Mitigate Errors when Weaning from Bypass. J Extra Corpor Technol 2019;51:38–40. [PMC free article] [PubMed] [Google Scholar]