Abstract
This study aims to assess rehabilitation needs and provision of rehabilitation services for individuals with moderate-to-severe disability and investigate factors influencing the probability of receiving rehabilitation within six months after traumatic brain injury (TBI). Overall, the analyses included 1206 individuals enrolled in the CENTER-TBI study with severe-to-moderate disability. Impairments in five outcome domains (daily life activities, physical, cognition, speech/language, and psychological) and the use of respective rehabilitation services (occupational therapy, physiotherapy, cognitive and speech therapies, and psychological counselling) were recorded. Sociodemographic and injury-related factors were used to investigate the probability of receiving rehabilitation. Physiotherapy was the most frequently provided rehabilitation service, followed by speech and occupational therapy. Psychological counselling was the least frequently accessed service. The probability of receiving a rehabilitative intervention increased for individuals with greater brain injury severity (odds ratio (OR) 1.75, CI 95%: 1.27–2.42), physical (OR 1.92, CI 95%: 1.21–3.05) and cognitive problems (OR 4.00, CI 95%: 2.34–6.83) but decreased for individuals reporting psychological problems (OR 0.57, CI 95%: 1.21–3.05). The study results emphasize the need for more extensive prescription of rehabilitation services for individuals with disability. Moreover, targeted rehabilitation programs, which aim to improve outcomes, should specifically involve psychological services to meet the needs of individuals recovering from TBI.
Keywords: rehabilitation needs, traumatic brain injury, disability, outcome
1. Introduction
Physical, cognitive and emotional problems after traumatic brain injury (TBI) may cause physical, behavioral and psychosocial impairments, work disability [1], and an overall reduction in health-related quality of life [2]. These problems require a wide range of rehabilitation services delivered to both inpatients and outpatients after TBI by medical, allied health and social care professionals. Such services include nursing services, physical therapy, occupational therapy, psychological and neuropsychological services, speech therapy, social worker aid, vocational services, and more [3].
TBI rehabilitation is beneficial in that it improves patients’ functional outcomes beyond those expected from spontaneous recovery [4,5]. The key criteria for successful health and rehabilitation services are the inclusion of, and access to, well-coordinated multidisciplinary processes, which address the varying needs of patients with TBI [5,6]. Despite this, existing studies of rehabilitation needs and the use of rehabilitation services following TBI indicate a lack of multidisciplinary rehabilitation services during acute care [7,8]. Furthermore, traditional rehabilitation services, such as physical, occupational, and speech and language therapies are far more likely to be used than psychological counselling during the first three months post-TBI [3] or during the post-acute care after severe TBI [9]. As a result, more than one-third of patients may present unmet rehabilitation needs in the long-run following TBI [10]. These unmet needs may be attributable to the prevailing community-level approach where rehabilitation consists of interventions focusing on physical functioning, rather than a systematic multidisciplinary approach based on individual needs [11]. A lack of resources allocated for rehabilitation of variable post-injury needs likely also contributes.
Service utilization may vary based on demand and specific needs across different demographics and injury severity characteristics, and service provision and access may further vary across regions and countries. Studies determining the predictive value of socio-demographics on the use of rehabilitation services after TBI show contradictory results. Some report sex differences in service utilization, such as higher healthcare use among females [7,10]. In other studies, however, males received more services [12], or no correlation between sex and service utilization was observed [3,9]. Furthermore, some studies report that younger individuals more often received rehabilitation after TBI [10,12,13], while others report that older individuals more often received such services [14,15]. More frequent service utilization has been reported to be more frequent among patients after severe TBI [7,16,17], among those with more severe overall trauma [7] and in those with more severe disabilities [16]. Other studies report that unmet rehabilitation needs were significantly higher in individuals with a less severe disability outcome [10].
Johnstone et al., report that geographical regions might influence access to TBI rehabilitation services [18], which may explain the presence of contradictory study results. Supporting this, a survey study by Cnossen et al. found substantial variation in the general policies governing the structure and process of acute in-hospital rehabilitation and referrals to post-acute rehabilitation among the European neurotrauma centers [13]. However, most studies on rehabilitation needs and the use of rehabilitation services are conducted within the United States (USA) [19], and few occur outside the USA [7,9,20]. Therefore, to improve the service provision, a better understanding of rehabilitation needs and culture- and country-related differences is required. To gain this understanding, additional studies must be conducted in a diverse range of countries.
To this end, the Collaborative European NeuroTrauma Effectiveness Research in TBI (CENTER-TBI) [21] observational study was conducted from 2014 to 2017 in Europe and Israel. A recently published paper from this large multicenter study including all injury severity levels reported the prevalence of rehabilitation use to be 32.4% in the first year after TBI across the European countries and identified predictors of access to rehabilitation following TBI [7]. However, an assessment of the specific rehabilitation needs and service provision among sub-group of individuals with functional impairments and moderate-to-severe disability outcomes according to the Glasgow Outcome Scale—Extended (GOSE) [22] has not yet been performed. This subgroup was chosen as this impairment level is considered to generate needs for rehabilitation. Such a study is essential for further development of best practices for TBI rehabilitation service provision and delivery in Europe.
The aims of this study were as follows:
To assess the rehabilitation needs and provision of rehabilitation services for individuals exhibiting TBI-related impairments and disability across Europe during the first six months post-injury.
To investigate whether sociodemographic, premorbid, and injury-related factors predict the probability of receiving rehabilitation services at three and six months after injury.
Based on previous studies, we hypothesized that:
There will be a high percentage of rehabilitation needs among individuals with TBI-related impairments and disabilities in the first six months following TBI.
There will be an association between the probability of receiving rehabilitation and age, sex, injury severity, comorbidities, and geographical regions.
2. Methods
2.1. Study Design
Participants were recruited from the CENTER-TBI project, a multicenter, prospective observational longitudinal cohort study that aims to better characterize TBI and to identify the most effective interventions for managing TBI [21]. The core study enrolled patients with all TBI severities from 18 countries (Austria, Belgium, Denmark, France, Finland, Germany, Hungary, Israel, Italy, Romania, Serbia, Spain, Sweden, Latvia, Lithuania, Norway, the Netherlands, and the United Kingdom) and 65 participating centers between 19 December 2014 and 17 December 2017. Inclusion criteria were a clinical diagnosis of TBI, an indication for a computed tomography (CT) scan and presentation to a medical center within 24 h of injury. Individuals were excluded if they had a severe pre-existing neurological disorder that could bias outcome assessments. Three strata were used to prospectively differentiate patients by clinical care pathway: emergency room (ER; patients evaluated in the ER and discharged afterwards), admission (patients admitted to a hospital ward), and intensive care unit (ICU; patients who were initially admitted to the ICU). The main descriptive findings of CENTER-TBI have been published elsewhere [23].
This study is a part of Work Package 14 (WP-14), aimed at describing optimal ways to provide different levels of care to individuals after TBI. The complex issue of rehabilitation is a major focus of this WP. Thus, the assessments included in the current study were from the original CENTER-TBI study.
2.2. Participants
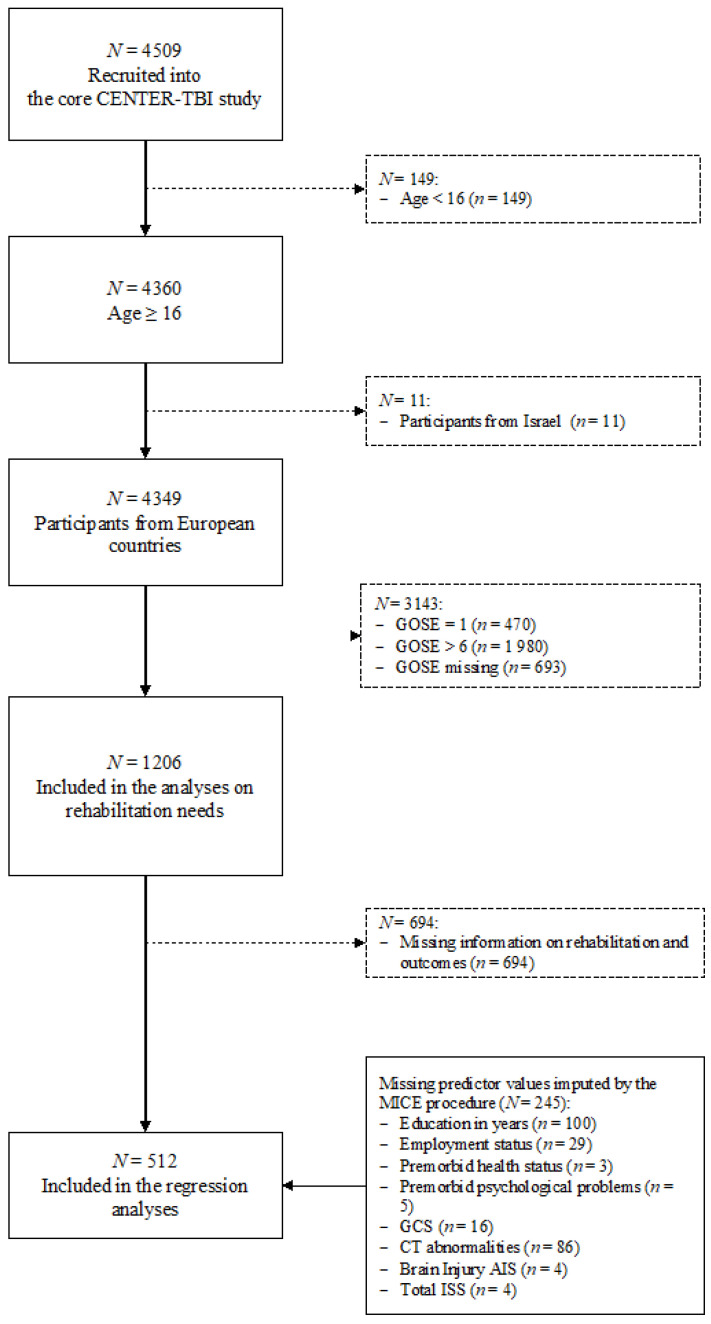
To assess rehabilitation needs, 1206 individuals over 16 years of age were selected from the 17 European countries involved in the CENTER-TBI project. Participants from Israel (n = 11) were excluded as this study assesses the rehabilitation needs across the Europe. All selected individuals showed TBI-related moderate-to-severe disability outcome—as measured by the GOSE score—at their six-month follow-up appointment. The GOSE score consists of an eight-point scale (1: dead, 2: vegetative state, 3/4: lower/upper severe disability, 5/6: lower/upper moderate disability and 7/8: lower/upper good recovery) and is based on structured clinical interviews or self- or proxy- ratings. Besides the GOSE, the patient- or proxy-reported version of the GOSE questionnaire (GOSE-Q) [24] administered by postal mail was used to collect information on disability outcomes. The GOSE-Q score was centrally computed, combined with the GOSE interview score and integrated into the CENTER-TBI database. As the questionnaire version does not distinguish between vegetative state and lower severe disability categories, the two were collapsed into one group. The present study includes individuals exhibiting lower-severe to upper- moderate disability outcomes six-months post-injury. For the regression analyses, only those individuals who provided information on received rehabilitation services and impaired outcomes were selected resulting in an effective sample size of 512 individuals. For more details on samples attrition, see Figure 1.
Figure 1.
Sample attrition flowchart.
2.3. Instruments
2.3.1. Sociodemographic, Premorbid, and Injury-Related Data
Sociodemographic and injury-related data were collected at the study’s inception. Data included sex (female or male), age in years, years of education, living situation (alone or not alone) and work participation (employed, unemployed, and other—i.e., retired, studying, or homemaker).
The geographical region was determined by the country of the participating sites. Based on the EU Vocabularies (EuroVoc) classification [25], countries were stratified into Western (Austria, Belgium, France, Germany, The Netherlands and the United Kingdom); Southern (Italy and Spain); Northern (Denmark, Finland, Latvia, Lithuania, Norway and Sweden); and Central and Eastern Europe (Hungary, Romania, and Serbia). Due to the small number of participants, Southern and Eastern European regions were collapsed into one group.
Premorbid somatic health status was assessed according to the classification of the American Society of Anesthesiologists Physical Status Classification System [26]. This classification originally comprised four groups: healthy, mild systemic disease, severe systemic disease and severe systemic disease with constant threat to life. The latter two were collapsed into one category (termed severe systematic disease) due to a low number of cases.
Injury-related information covered: (i) the injury mechanism (e.g., road traffic accident, falls, other); (ii) clinical care pathways (ER, ward, and ICU); (iii) TBI severity as measured by the Glasgow Coma Scale (GCS [27] within the first 24 h after injury as both a continuous variable and classified into mild (13–15), moderate (9–12), and severe (3–8); (iv) the presence of intracranial injuries on the first CT scan (absent/present); (v) the Abbreviated Injury Scale [28] (AIS; Brain injury AIS, score ≥ 3 considered as severe intracranial injury), and (vi) overall injury severity as measured by the Injury Severity Score (ISS) [29]. The ISS ranges from 0 (no trauma) to 75 (not survivable) and a score > 15 is considered major overall trauma [30].
2.3.2. Assessment of Rehabilitation Needs
For the assessment of rehabilitations needs, the following five outcome domains were identified: problems with activities of daily life, physical, cognitive, speech and psychological problems.
Problems with activities of daily life were measured using the scale Daily Life and Autonomy of the Quality of Life after Brain Injury Scale (QOLIBRI) [31,32] with a cut-off score of 60 and lower scores indicating impairment.
Physical problems covering mobility (e.g., problems with mobility or walking) and movement ability (e.g., problems with movement of the hands or arms) were self-reported and assessed by two questions from the Participant Questionnaire of the CENTER-TBI project. Individuals who responded affirmatively to at least one yes/no question were considered impaired.
Problems with cognition were measured using three questions from the Rivermead Post-Concussion Symptoms Questionnaire (RPQ) [33]. ‘Forgetfulness, poor memory’, ‘poor concentration’ or ‘taking longer to think’ were rated at least as mild ≥2 [34]. Individuals who reported at least one of these symptoms were considered impaired.
Problems with speech and language were measured using the yes/no question ‘problems with speaking or understanding others’ in the Participant Questionnaire mentioned above.
Psychological problems were considered to be present if at least one of the following outcomes was rated as impaired:
-
(i)
Post-traumatic stress disorder (PTSD) was captured by the Posttraumatic Stress Disorder Checklist-5 (PCL-5) [35]. The PCL-5 measures 20 symptoms of PTSD based on the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) [36] using a five-point Likert scale (from 0, ‘not at all’, to 4, ‘extreme’). The total score ranges from 0 to 80, with higher values indicating greater impairment. A cut-off value of 33 was applied to determine clinically relevant PTSD [37].
-
(ii)
Depression was assessed with the Patient Health Questionnaire (PHQ-9) [38]. The PHQ-9 assesses symptoms of depression using nine items and a four-point Likert scale (from 0 ‘not at all’ to 3 ‘nearly every day’). The PHQ-9 total score ranges from 0 to 27, with higher values indicating greater impairment. A cut-off value of 10 was applied to determine clinically relevant depression [38,39].
-
(iii)
Anxiety was assessed with the self-reported Generalized Anxiety Disorder seven-item scale (GAD-7) [40]. The GAD-7 uses seven items and a four-point Likert scale (from 0 ‘not at all’ to 3 ‘nearly every day’). The total score ranges from 0 to 21. Higher values indicate greater impairment, with a cut-off value of 10 indicating impairment [40].
2.3.3. Professional Help and Rehabilitation Services
Information concerning professional help and rehabilitation services provided after TBI was based on self-report. Participants were asked to report any specialized professional help they received because of the TBI, including help for problems with speaking (e.g., speech therapy), memory or attention (e.g., cognitive rehabilitation), problems with movements (e.g., physiotherapy), help for problems with looking after themselves (e.g., occupational therapy), emotional difficulties, behavioral regulation and fatigue (e.g., psychological services). Multiple answers were allowed. Participants were then asked to utilize the following response categories to describe the rehabilitation they received because of the TBI with the following response categories: inpatient/residential rehabilitation, out-patient/community rehabilitation, or no rehabilitation. This information contained no reference to the impaired outcome domains.
2.4. Statistical Analyses
2.4.1. Unmet Rehabilitation Needs
First, we identified rehabilitation needs at three and six months after TBI using the methods and instruments described above. The amount of professional help and rehabilitation services provided was measured using the ratio of total impaired individuals versus individuals who had received professional or rehabilitation services. Individuals with impairments who did not receive inpatient/residential or outpatient/community rehabilitation services were considered to have unmet rehabilitation needs.
To provide an overview of these unmet rehabilitation needs, we classified the ratio into three groups based on the following the cut-off values: covered needs (75% or more of the impaired individuals receiving respective services), semi-covered needs (less than 75% but more than 25% of impaired individuals receiving respective services), and uncovered needs (less than 25% receiving respective services). Coverage of rehabilitation needs is provided per outcome category. For example, if a person reported problems with activities of daily living and psychological problems but received only occupational rehabilitation and no psychological treatment, his or her needs were covered to 100% in the “activities of daily life” outcome category and not covered in the “psychological problems” category. If each person who reported an impairment in a category received appropriate rehabilitation, the total coverage was 100%. Based on the results of this classification, the coverage of rehabilitation needs was subsequently ranked according to the five outcome domains at three and six months after TBI, respectively.
Differences between timepoints were examined using chi-square tests with Bonferroni-corrected p-values for multiple outcome comparisons (e.g., = 0.05/5 = 0.01 for the five outcome domains or = 0.05/4 = 0.0125 for the four recovery status groups).
2.4.2. Prediction of Probability of Receiving Rehabilitation
Logistic regression was applied separately to predict the probability of receiving rehabilitation at three and six months post-injury adjusting for factors suggested by previous research. The dependent variable represents provided rehabilitation services (0 = no rehabilitation vs. 1 = inpatient or outpatient rehabilitation). Nineteen independent variables include sociodemographic information at baseline (sex, age, living situation, years of education, employment status, and geographical region); premorbid health status (overall health and mental health); injury-related factors such as injury cause, clinical care pathways, TBI severity (GCS, abnormalities on the first CT scan, brain injury) and overall injury severity. In addition, impairments in the five outcome domains were included.
The following steps were performed to run the regression analyses. First, the missing values in the predictor variables (varying from 1% for the premorbid health status to 19% for the number of education years) were imputed using multivariate imputation by the chained equations (MICE) procedure [41]. The MICE procedure is a multi-step approach that is able to account for the influence of multiple factors simultaneously and impute missing values based on variable type (e.g., continuous, dichotomous, or polytomous) [42]. Missing values are imputed by applying a series of corresponding regression models multiple times and using pooled data for target analyses to avoid bias [41]. Second, the initially defined model was estimated. Factors contributing to the probability of receiving rehabilitation were chosen according to the backward stepwise Akaike’s information criterion (AIC) procedure with a liberal p-value of 0.157 corresponding to a predictor with 1 degree of freedom. While the regression model was defined based on previous research, a liberal p-value was used to justify variable selection for the final model reported [43]. A bootstrapping validation procedure assessed the goodness of fit on the imputed data providing optimism-corrected fit indices. Nagelkerke’s R2 [44] was used to assess whether the estimated model differed from a hypothetical null-model without any predictors. The Nagelkerke’s R2 ranges from 0 to 1 with higher values indicating the relative improvement of the estimated model compared to a null model. The area under the receiver operating (ROC) curve (AUC), which corresponds to the c-statistic [45,46], was used to assess model’s ability to distinguish between individuals who received rehabilitation services and those who did not. AUC values from 0.70 to 0.80 were considered acceptable, while values over 0.80 were considered excellent and over 0.90 were considered outstanding [47].
All analyses were performed with the R version 4.0.2 [48] using the packages ‘mice’ [49] for the missing values imputation and ‘psfmi’ [50] for the model estimation, selection of potential predictors, and bootstrapping validation. The alpha level was set at 0.05 except for multiple comparisons between three and six month assessments and the stepwise AIC procedure.
3. Results
3.1. Sample Characteristics
The study sample (N = 1206) consisted of majority males (67.7%) and had a mean age of 49.3 (SD = 18.9 years, Mdn = 50, IQR = 77). Half of the participants had at least 13 years of education and were employed (52.5%) at the time of the injury, and half were residents of Western European countries (49.2%). Most individuals (52.4%) reported no somatic health problems and no psychological problems (80.3%) prior to TBI. Road traffic accidents (45.6%) were the most common cause of TBI, and most of patients with TBI were admitted to the ICU (71.2%). Of the sample group, 49.1% sustained a mild TBI, 11.7% sustained a moderate and 35.2% a severe TBI. Finally, 62.2% showed abnormalities on the first CT-scan (Table 1).
Table 1.
Sample characteristics.
| Variable | Group/Values |
N (%) or M (SD) or Md [Min, Max] |
|---|---|---|
| Sex | Female | 390 (32.3%) |
| Male | 816 (67.7%) | |
| Age in years | M (SD) | 49.3 (18.9) |
| Md [Min, Max] | 50.0 [16.00, 93.00] | |
| Missing | 0 (0%) | |
| Education in years | M (SD) | 13.1 (3.84) |
| Md [Min, Max] | 13.0 [1.00, 30.00] | |
| Missing | 321 (26.6%) | |
| Employment status | Employed | 633 (52.5%) |
| Unemployed | 104 (8.6%) | |
| Other | 341 (28.3%) | |
| Missing | 128 (10.6%) | |
| Living status | Alone | 948 (78.6%) |
| Not alone | 255 (21.1%) | |
| Missing | 3 (0.2%) | |
| Geographical regions | Western Europe | 593 (49.2%) |
| Northern Europe | 306 (25.4%) | |
| Southern/Eastern Europe | 307 (25.5%) | |
| Premorbid somatic health status | Healthy | 632 (52.4%) |
| Mild disease | 417 (34.6%) | |
| Severe disease | 130 (10.8%) | |
| Missing | 27 (2.2%) | |
| Premorbid psychological problems | No | 968 (80.3%) |
| Yes | 198 (16.4%) | |
| Missing | 40 (3.3%) | |
| Injury cause | Road traffic accident | 550 (45.6%) |
| Fall | 455 (37.7%) | |
| Violent/other | 196 (16.3%) | |
| Missing | 5 (0.4%) | |
| Clinical care pathways | ER | 76 (6.3%) |
| ward | 271 (22.5%) | |
| ICU | 859 (71.2%) | |
| GOSE (6 months) | M (SD) | 4.66 (1.17) |
| Md [Min, Max] | 5.00 [3.00, 6.00] | |
| Missing | 0 (0%) | |
| TBI severity | Mild | 592 (49.1%) |
| Moderate | 141 (11.7%) | |
| Severe | 425 (35.2%) | |
| Missing | 48 (4.0%) | |
| Abnormalities on the first CT scan | Absent | 223 (18.5%) |
| Present | 750 (62.2%) | |
| Missing | 233 (19.3%) | |
| Brain Injury AIS | M (SD) | 3.82 (1.25) |
| Md [Min, Max] | 4.00 [1.00, 6.00] | |
| Missing | 19 (1.6%) | |
| Total ISS | M (SD) | 27.7 (16.2) |
| Md [Min, Max] | 25.0 [1.00, 75.0] | |
| Missing | 19 (1.6%) | |
| Total | 1206 (100%) |
Note. Percentages may contain rounding errors in the second decimal place. M = mean; SD = Standard deviation; Md = median; Min = minimum; Max = maximum; Employment status = employed (full-time employed, part-time employed, on sick leave, special/sheltered employment), unemployed (looking for work, unemployed, unable to work), other (retired, student/school-going, homemaker); Geographical regions = Western Europe (Austria, Belgium, France, Germany, the Netherlands, United Kingdom); Northern Europe (Denmark, Finland, Latvia, Lithuania, Norway, Sweden); Southern/Eastern Europe (Italy, Spain, Hungary, Romania, Serbia); Premorbid somatic health status is based on the ASA-PS classification; ER = emergency room; ward = admission to hospital ward; ICU = intensive care unit; CT = computed tomography; AIS = Abbreviated Injury Scale; ISS = Injury Severity Score.
3.2. Rehabilitation Needs
Almost all participants had at least one impaired outcome at both three and six months post-TBI (91% and 89%, respectively). Over 40% reported suffering from at least two or three impairments, and nearly 9% were impaired in all five areas (problems with activities of daily life and physical, cognition, speech, and language and psychological problems) at three and six months after TBI.
Table 2 summarizes the distribution of N = 1206 individuals with GOSE scores from 2/3 to 6 and outcome domains at three and six months after TBI, respectively. At three months after TBI, participants mostly exhibited difficulties with physical problems closely followed by cognitive problems. At six months, cognitive problems were more frequently reported than physical problems (with approximately half of the participants reporting cognitive problems). Other outcome areas were nearly equally distributed at three and six months after TBI with speech and language problems showing the lowest frequency of impairments. Across all time points and all outcome domains, individuals admitted to the ICU exhibited the highest degree of impairment.
Table 2.
Impairment in the different outcome areas at three and six months after TBI.
| Outcome Type | Impairment | Three Months | Six Months | p |
|---|---|---|---|---|
| N (%) | N (%) | |||
| Problems with activities of daily life | Not impaired | 283 (23.5%) | 361 (29.9%) | 0.01 |
| Impaired | 411 (34.1%) | 400 (33.2%) | ||
| Missing | 512 (42.5%) | 445 (36.9%) | ||
| Physical problems | Not impaired | 289 (24.0%) | 333 (27.6%) | 0.06 |
| Impaired | 506 (42.0%) | 480 (39.8%) | ||
| Missing | 411 (34.1%) | 393 (32.6%) | ||
| Cognition problems | Not impaired | 209 (17.3%) | 215 (17.8%) | 0.41 |
| Impaired | 498 (41.3%) | 567 (47.0%) | ||
| Missing | 499 (41.4%) | 424 (35.2%) | ||
| Speech and language problems | Not impaired | 579 (48.0%) | 607 (50.3%) | 0.49 |
| Impaired | 215 (17.8%) | 207 (17.2%) | ||
| Missing | 412 (34.2%) | 392 (32.5%) | ||
| Psychological problems | Not impaired | 411 (34.1%) | 454 (37.6%) | 0.70 |
| Impaired | 277 (23.0%) | 292 (24.2%) | ||
| Missing | 518 (43.0%) | 460 (38.1%) |
Note. Percentages may contain rounding errors in the second decimal place. N = number of observations; % = percentage; Problems with activities of daily life (QOLIBRI scale Daily Life and Autonomy, score > 60); Physical problems (problems with mobility/walking, problems with moving arms and hands); Cognition problems (RPQ: ‘Forgetfulness, poor memory’ or ‘Poor concentration’, or ‘Taking longer to think’; score ≥ 2); Speech/language problems (problems with speaking or understanding others); Psychological problems (one of the following outcomes considered impaired according to the respective cut-off scores: PTSD: PCL-5 score ≥ 33; Depression: PHQ-9 score ≥ 10; Anxiety: GAD-7 score ≥ 10); p = p-values are obtained from the chi-square tests and are significant at <1% (Bonferroni-adjusted alpha level for multiple comparisons: 0.05/5).
3.3. Coverage of Rehabilitation Needs
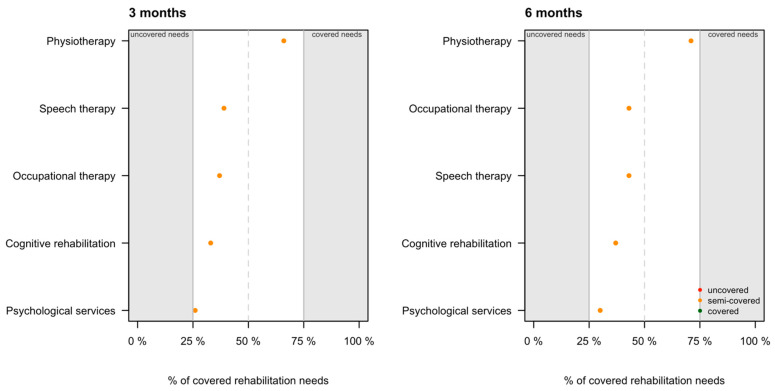
Table 3 presents information on the type of rehabilitation services provided in the defined outcome domains. At three and six months, physiotherapy was the most frequently prescribed service (66% and 71%, respectively) followed by speech (39% and 43%, respectively) and occupational therapy (37% and 43%, respectively). Approximately 33% of patients with cognitive problems at three months and 37% at six months self-reported that they received cognitive rehabilitation. Psychological services, including professional help with anxiety, depression, stress, behavioral problems and fatigue, were provided to approximately 26% and 30% of the individuals who reported psychological problems at three- and six-months assessments, respectively.
Table 3.
Professional help provided for patients with impaired outcomes at three and six months.
| Outcome Type | Type of Professional Help | Three Months | Six Months | p | ||||
|---|---|---|---|---|---|---|---|---|
| Impaired | Help Provided | % | Impaired | Help Provided | % | |||
| Problems with activities of daily life | Occupational therapy | 411 | 153 | 37% | 400 | 170 | 43% | 0.34 |
| Physical problems | Physiotherapy | 506 | 334 | 66% | 480 | 340 | 71% | 0.82 |
| Cognition problems | Cognitive rehabilitation | 498 | 166 | 33% | 567 | 212 | 37% | 0.02 |
| Speech and language problems | Speech therapy | 215 | 84 | 39% | 207 | 89 | 43% | 0.70 |
| Psychological problems | Psychological services | 277 | 73 | 26% | 292 | 89 | 30% | 0.21 |
Note. Impaired = number of individuals considered impaired according to the respective cut-offs; Help provided = number of individuals received respective rehabilitation services based on self-report; % = relative frequency of individuals received respective rehabilitation services; p = p-values are obtained from the chi-square tests comparing distributions of provided professional help between three and six months and are significant at <1% (Bonferroni-adjusted alpha level for multiple comparisons: 0.05/5).
Irrespective of the outcome area impaired, individuals admitted to the ICU participated more frequently in in-patient rehabilitation programs at both time points. In contrast, out-patient treatments were used by those admitted to the ER and then discharged, followed by individuals treated in the hospital ward (see Table A1 in Appendix A).
Overall, at both time points rehabilitation needs were semi-covered across all outcome domains (i.e., between 25% and 75% of those impaired received the necessary support)—the only ranking difference between the time points involved occupational and speech therapies. While occupational therapy was a more frequent part of the rehabilitation program component at three months post-TBI, speech therapy was more highly ranked at six months. At each time point, psychological services were the least frequent service provided relative to documented impairment. For details, see Figure 2.
Figure 2.
Rehabilitation services provided to individuals with the respective impaired outcomes. Services were ranked based the relative frequency (e.g., physiotherapy was provided more frequently than speech therapy at three months and more frequently than occupational therapy at six months after TBI).
Of the 1206 participants, approximately 30% received inpatient rehabilitation at three and six months after TBI, irrespective of the impaired outcome domains. Individuals admitted to the ICU displayed the highest rate of involvement in rehabilitation programs (35% and 39% at three and six months, respectively). At three months post-TBI, 13% of individuals admitted to a hospital ward participated in inpatient rehabilitation programs, whereas at six months after TBI, only 8% received inpatient treatment. Among all groups, individuals admitted to the ER and subsequently discharged showed the lowest percentage of participation in rehabilitation programs with 2% and 5% at three and six months, respectively. Overall, about 15% of participants received outpatient rehabilitation regardless of the impaired outcome domains. Individuals admitted to the ER and then discharged (17% and 20% at three and six months, respectively) were closely followed by those admitted to a hospital ward (14% and 18%) in terms of the frequency with which they received outpatient rehabilitation services. Approximately 12% and 14% of those admitted to the ICU took part in outpatient rehabilitation programs at three and six months, respectively. Around one-fourth did not take part in any rehabilitation programs. Nearly one-third provided no information on rehabilitation treatments at each time point with individuals admitted to the ICU showing the highest number of missing values (37% and at 34% at three and six months, respectively). For details, see Table A1 in Appendix A.
The group of individuals with low recovery status (GOSE scores of 2/3) had the highest number of missing values (i.e., no information regarding rehabilitation was available). Still, the lower the GOSE score, the lower was the likelihood of outpatient rehabilitation. For further details, see Table 4.
Table 4.
Rehabilitation services received at there and six months (total and split by recovery status at six months).
| Recovery Status | Rehabilitation | Three Months | Six Months | p |
|---|---|---|---|---|
| N (%) | N (%) | |||
| Total | No | 306 (25.4%) | 276 (22.9%) | 0.07 ‡ |
| In-patient | 341 (28.3%) | 356 (29.5%) | ||
| Out-patient | 150 (12.4%) | 183 (15.2%) | ||
| Missing | 409 (33.9%) | 391 (32.4%) | ||
| Total | 1206 (100.0%) | 1206 (100.0%) | ||
| GOSE 2/3 (vegetative state/lower severe disability) | No | 30 (9.7%) | 18 (5.8%) | 0.05 † |
| In-patient | 103 (33.3%) | 93 (30.1%) | ||
| Out-patient | 9 (2.9%) | 18 (5.8%) | ||
| Missing | 167 (54.0%) | 180 (58.3%) | ||
| Total | 309 (100.0%) | 309 (100.0%) | ||
| GOSE 4 (upper severe disability) | No | 35 (20.1%) | 33 (19.0%) | 0.34 † |
| In-patient | 51 (29.3%) | 68 (39.1%) | ||
| Out-patient | 14 (8.0%) | 23 (13.2%) | ||
| Missing | 74 (42.5%) | 50 (28.7%) | ||
| Total | 174 (100.0%) | 174 (100.0%) | ||
| GOSE 5 (lower moderate disability) | No | 95 (28.0%) | 75 (22.1%) | 0.12 † |
| In-patient | 100 (29.5%) | 98 (28.9%) | ||
| Out-patient | 52 (15.3%) | 67 (19.8%) | ||
| Missing | 92 (27.1%) | 99 (29.2%) | ||
| Total | 339 (100.0%) | 339 (100.0%) | ||
| GOSE 6 (upper moderate disability) | No | 146 (38.0%) | 150 (39.1%) | 0.89 † |
| In-patient | 87 (22.7%) | 97 (25.3%) | ||
| Out-patient | 75 (19.5%) | 75 (19.5%) | ||
| Missing | 76 (19.8%) | 62 (16.1%) | ||
| Total | 384 (100.0%) | 384 (100.0%) |
Note. Percentages may contain rounding errors in the second decimal place. N = number of cases, % = percentage p = p-values are obtained from the chi-square tests comparing distributions of provided rehabilitation services at three and six months and are significant at ‡ <5% and at † <1.25% (Bonferroni-adjusted alpha level for multiple comparisons: 0.05/4).
Table 5 presents information regarding rehabilitation type (no rehabilitation, in- or outpatient services) provided for patients with impaired outcomes. The data includes no information about the primary reason for the rehabilitation (e.g., mobility issues, cognitive and communication problems, or both).
Table 5.
Rehabilitation provided to patients with impaired outcomes.
| Imapired Outcome | Rehabilitation ‡ | Three Months | Six Months | p |
|---|---|---|---|---|
| Problems with activities of daily life | No | 153 (37.2%) | 116 (29.0%) | 0.03 |
| In-patient | 164 (39.9%) | 178 (44.5%) | ||
| Outpatient | 82 (20.0%) | 98 (24.5%) | ||
| Missing | 12 (2.9%) | 8 (2.0%) | ||
| Physical problems | No | 175 (34.6%) | 145 (30.2%) | 0.06 |
| In-patient | 240 (47.4%) | 223 (46.5%) | ||
| Outpatient | 87 (17.2%) | 110 (22.9%) | ||
| Missing | 4 (0.8%) | 2 (0.4%) | ||
| Cognition problems | No | 182 (36.5%) | 170 (30.0%) | 0.05 |
| In-patient | 200 (40.2%) | 236 (41.6%) | ||
| Outpatient | 105 (21.1%) | 146 (25.7%) | ||
| Missing | 11 (2.2%) | 15 (2.6%) | ||
| Speech and language problems | No | 62 (28.8%) | 51 (24.6%) | 0.06 |
| In-patient | 118 (54.9%) | 104 (50.2%) | ||
| Outpatient | 34 (15.8%) | 52 (25.1%) | ||
| Missing | 1 (0.5%) | 0 (0.0%) | ||
| Psychological problems | No | 123 (44.4%) | 108 (37.0%) | 0.19 |
| In-patient | 96 (34.7%) | 109 (37.3%) | ||
| Outpatient | 53 (19.1%) | 68 (23.3%) | ||
| Missing | 5 (1.8%) | 7 (2.4%) |
‡ Note that the type of rehabilitation is independent of the impaired outcome. Note. Percentages may contain rounding errors in the second decimal place. p = p-values are obtained from the chi-square tests comparing distributions of provided rehabilitation services at 3 and 6 months and are significant at <1% (Bonferroni-adjusted alpha level for multiple comparisons: 0.05/5).
3.4. Prediction of the Probability of Receiving Rehabilitation
Since there was almost no difference in the three- and six-months prediction results, only the six months results are reported here.
At six months post-TBI, a more severe TBI (i.e., lower GCS and higher Brain Injury AIS), the presence of physical and cognitive problems, and the absence of psychological problems contributed significantly to a higher probability of receiving rehabilitation services. The total ISS and clinical pathways (ER, ward, and ICU) were included in the model according to the stepwise AIC procedure, but they generated no significant results. The corrected AUC/c-statistic produced the value of 0.84 (optimism correction of −0.01), indicating a strong model with excellent discriminating ability [47]. According to the model, individuals who had received rehabilitation had a higher predicted probability (i.e., 84%) to be identified as such than individuals who had not received rehabilitation. The corrected pseudo R2 = 0.42 (optimism correction of −0.01) indicated prediction improvement from the null model to the final model. For more details, see Table 6.
Table 6.
Results of the logistic regression (final model).
| Variable/Category | Reference Group | Estimate | S.E. | p | OR | CI 2.5% | CI 97.5% |
|---|---|---|---|---|---|---|---|
| Intercept | - | 1.38 | 0.80 | 0.086 | 3.99 | 0.82 | 19.29 |
| GCS | - | −0.24 | 0.04 | <0.001 | 0.79 ‡ | 0.72 | 0.86 |
| Brain Injury AIS | - | 0.56 | 0.16 | 0.001 | 1.75 ☥ | 1.27 | 2.42 |
| ISS | - | −0.02 | 0.01 | 0.063 | 0.98 | 0.96 | 1.00 |
| Physical problems | - | 0.65 | 0.24 | 0.006 | 1.92 ☥ | 1.21 | 3.05 |
| Cognition | - | 1.39 | 0.27 | <0.001 | 4.00 ☥ | 2.34 | 6.83 |
| Psychological problems | - | −0.56 | 0.25 | 0.026 | 0.57 ‡ | 0.35 | 0.93 |
| Ward | ER | −0.86 | 0.44 | 0.052 | 0.42 | 0.18 | 1.00 |
| ICU | ER | −0.38 | 0.55 | 0.499 | 0.69 | 0.23 | 2.04 |
‡ Lower probability of receiving rehabilitation services; ☥ higher probability of receiving rehabilitation services; Note. Estimate = regression coefficient; S.E. = standard error; p = p-value; OR = odds ratio; CI 2.5% = lower bound of the 95% confidence interval; CI 97.5% = upper bound of the 95% confidence interval; bold p-values are significant at 5% α-level; GCS = Glasgow Coma Scale; Brain Injury AIS = Abbreviated Injury Scale, Brain Injury severity; ISS = total Injury Severity Score; ER = emergency room; ward = admission at hospital ward; ICU = intensive care unit.
4. Discussion
The present study is, to our knowledge, the first study to assess rehabilitation needs and the use of rehabilitation services in individuals with moderate-to-severe disability after TBI from the European perspective.
We chose to focus on the more severe spectrum of the TBI population as their rehabilitation needs are unequivocal [51]. The male predominance is in accordance with the epidemiologic characteristics of this population [52], and the median age of 50 years is representative for the CENTER-TBI population [23]. Close to half of the present population had pre-existing somatic conditions and 10% of these had more severe somatic problems. In the CENTER-TBI context, the GOSE score assesses the overall functional problems in contrast to the original use of GOSE which evaluated only TBI-related disability outcomes [53]. Distinguishing the TBI-related disability from the overall disability may be a challenge, and the present analyses stress the different impairments in functioning.
Consistent with our first hypothesis, rehabilitation needs were reported by 90% of individuals, and these often presented within several outcome domains. However, the needs were only semi-covered across all outcome areas. Cognitive impairments were most common in the present study, followed by physical problems, problems with daily life activities, and psychological problems and speech problems. The burden of cognitive problems in the TBI population is well known [2], yet provision of physiotherapy continues to dominate. In the present study, physiotherapy was delivered to nearly half of the patients who did not report physical problems, which raises concerns regarding the appropriate allocation of rehabilitation resources. Our finding might be related to the fact that physiotherapy services are the ones most available across countries. In addition, the health payer system (a health care system, insurance companies and similar), may offers easy-access and full reimbursement for this service [9]. However, a detailed description of physical functioning and impairments beyond coarser mobility impairments was not included in this study, and these impairments could require physiotherapy.
In contrast, psychological services were provided to less than one-third of the individuals reporting psychological problems, representing the service with the lowest coverage of existing needs. Psychological problems may develop for various reasons, including as a result of the brain injury, secondary to other problems in functioning or because of unmet health care and rehabilitation needs related to the TBI, such as a lack of meaningful activities at an appropriate level or problems coping with injury consequences [10]. According to Jennekens et al.’s systematic review [19], a ‘prerequisite for offering adequate help is that health care providers understand the needs of these patients.’ The present results clearly underscore an urgent need for a stronger focus on monitoring psychological domains during TBI rehabilitation and the adjustment of rehabilitation service delivery to meet the needs of the TBI population.
Inpatient rehabilitation services were provided to 30% of the present population, and unsurprisingly, the highest coverage was extended to individuals admitted to the ICU, who are assumed to have the most severe injuries. Rehabilitation is considered highly beneficial for individuals after TBI; however, only 15% of patients received outpatient rehabilitation, which is considerably low given the long-term rehabilitation needs in the TBI population evidenced in earlier studies [10,54].
The applied model showed a good predictive ability and indicated that the probability of receiving rehabilitation depends primarily on injury-related factors, such as brain injury severity and impaired outcome domains. Consistent with our second hypothesis, injury severity, as well as physical and cognitive problems did increase the probability of receiving rehabilitation services, yet psychological problems decreased this probability. It is particularly worrisome that patients with psychological problems—assumed to be a vulnerable population—receive insufficient health care services [20].
Contrary to our second hypothesis, age, sex, and geographical regions (North, West and Southern/Eastern Europe) did not predict the probability of receiving rehabilitation. One possible explanation for this finding is an increased focus on the equality of health care during the last decade. In particular, the provision of rehabilitation services for those with severe injuries is supported by the current literature, which demonstrates improved outcomes for patients with severe TBI who complete specialized in-patient rehabilitation [5,55]. However, the above-mentioned findings are not entirely consistent with previous research [7,10,12] and should be interpreted with caution. It is worth mentioning that we used self-reports to assess the rehabilitation provision, which may have introduced a bias, as discussed in the limitation section.
Overall, the present study highlights an inadequate provision of services, which leads to a high prevalence of unmet rehabilitation needs and emphasizes the necessity of more extensive and standardized assessment of functional impairments and corresponding rehabilitation needs. This finding may provide a starting point for further development of personalized and targeted interventions following TBI.
Strengths and Limitations of the Study
The present study’s strengths are its large sample size and the number of participating European countries, which together render a robust overview. Nevertheless, the study also exhibits some limitations.
Firstly, patients with the two lowest functional recovery statuses were combined into one category, as the questionnaire version of the GOSE applied in the study cannot distinguish between vegetative status and severe disability. Further, functional impairments and the use of rehabilitation services were based on self-reports from the participants. By including the subjective experience of patients in a patient-centered rehabilitation, greater satisfaction, better adherence to treatment, and improved outcomes can be achieved; nevertheless, self-reported information can be biased [56], especially in those with impaired memory and self-awareness deficits [57]. To overcome this limitation, future studies, should combine self-reports with objective administrative data and clinical evaluations.
Secondly, overall, more than half of the initial group of patients did not provide information on different aspects of functioning and rehabilitation services. Among those were mostly male; they also had fewer years of education on average and resided predominantly in Western and Northern European countries. They were mostly admitted to the ICU, had significantly more severe injuries and suffered from more severe disabilities post-TBI. These findings suggest that non-participation could be related to an inability to complete self-report questionnaires due to cognitive impairments. Utilizing the perspective of the families or caregivers could allow for the inclusion of more severely injured patients. At the same time, however, it would likely introduce other biases such as the overestimation of problems—this may be related to a proxy’s inability to accurately assess a patient’s problems or the proxy’s own perceptions of what is important.
Thirdly, to avoid losing statistical power, the study imputed missing predictor values using the MICE procedure. Nevertheless, the influence of the imputed values was negligible, since in the final model only injury severity (GCS) and brain injury severity (brain AIS) were retained. Both variables initially showed 3% and 1% missing values, respectively. Furthermore, even if a stepwise selection procedure for model building is sometimes criticized, backward selection appears to be the best of all stepwise approaches [43,58], and the bootstrapping validation prevented the drawing of premature conclusions.
Finally, distinguishing between in- and out-patient rehabilitation was not possible in the regression model due to the relatively low number of observations. Therefore, future studies should provide a broader overview of various rehabilitation types by differentiating between in- and outpatient rehabilitation programs.
5. Conclusions
This study indicates numerous unmet rehabilitation needs across different outcome domains for individuals with moderate-to-severe disabilities after TBI. The study results emphasize the necessity of more extensive multidimensional and standardized assessments of functional and psychological impairments and the provision of corresponding rehabilitation services. Moreover, targeted rehabilitation programs aimed at improving outcomes should involve psychological services to meet the needs of individuals after TBI. Future research studies, which take into account objective administrative data, clinical evaluations, reports of caregivers and, as well as patients reports, will further improve knowledge about rehabilitation needs and services for TBI patients.
Acknowledgments
The authors would like to thank all study participants and the CENTER-TBI participants and investigators. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. In the Affiliations section ‘Oxford Health NHS Foundation Trust’.
Supplementary Materials
The following are available online at https://www.mdpi.com/2077-0383/10/5/1035/s1: list of CENTER-TBI participants and investigators.
Appendix A
The Appendix A contains additional tables.
Table A1.
In- and out-patient rehabilitation provided at 3 and 6 months after TBI by clinical pathways.
| Rehabilitation | 3 Months | 6 Months | p | ||||||
|---|---|---|---|---|---|---|---|---|---|
| ER | Ward | ICU | Total | ER | Ward | ICU | Total | ||
| No | 43 (56.6%) | 126 (46.5%) | 137 (15.9%) | 306 (25.4%) | 36 (47.4%) | 125 (46.1%) | 115 (13.4%) | 276 (22.9%) | 0.61 |
| In-patient | 2 (2.6%) | 36 (13.3%) | 303 (35.3%) | 341 (28.3%) | 4 (5.3%) | 21 (7.7%) | 331 (38.5%) | 356 (29.5%) | 0.06 |
| Out-patient | 13 (17.1%) | 38 (14.0%) | 99 (11.5%) | 150 (12.4%) | 15 (19.7%) | 48 (17.7%) | 120 (14.0%) | 183 (15.2%) | 0.98 |
| Missing | 18 (23.7%) | 71 (26.2%) | 320 (37.3%) | 409 (33.9%) | 21 (27.6%) | 77 (28.4%) | 293 (34.1%) | 391 (32.4%) | |
| Total | 76 (6.3%) | 271 (22.5%) | 859 (71.2%) | 1206 (100%) | 76 (6.3%) | 271 (22.5%) | 859 (71.2%) | 1206 (100%) | |
Note. Percentages may contain rounding errors in the second decimal place. ER = emergency room; ward = hospital ward; ICU = intensive care unit; p = p-values are obtained from a two-dimensional chi-square test comparing distributions of the clinical care pathways in rehabilitation groups at three and six months and are significant at <1.7% (Bonferroni-adjusted alpha level for multiple comparisons: 0.05/3).
Author Contributions
Conceptualization: N.A., C.R., N.v.S., and M.Z.; methodology: N.A., C.R., N.v.S., and M.Z.; software: M.Z.; validation: N.v.S., M.Z., N.A., and C.R.; formal analysis: M.Z.; investigation: N.A., C.R., O.T., P.A., H.D., M.M., N.v.S., and M.Z.; resources: Oslo University Hospital and University Medical Center Göttingen; data curation: M.Z.; writing—original draft preparation: N.A., C.R., N.v.S., and M.Z.; writing—review and editing: N.A., C.R., N.v.S., M.Z., O.T., P.A., H.D., M.M., J.R., E.J.A.W., E.I.H., C.T., I.B., M.V.F., I.K., H.M.D., L.J., M.C., and J.L.; visualization: M.Z.; supervision: N.A., C.R., and N.v.S.; project administration: C.R. and N.v.S.; funding acquisition: C.R. and N.v.S. All authors have read and agreed to the published version of the manuscript.
Funding
The data used in preparation of this manuscript were obtained in the context of CENTER-TBI, a large collaborative project with the support of the European Union 7th Framework program (EC grant 247 602150). Additional funding was obtained from the Hannelore Kohl Stiftung (Germany), from OneMind (USA) and from Integra LifeSciences Corporation (USA). Helen Dawes is supported by the Elizabeth Casson Trust and the NIHR Oxford Health Biomedical Research Centre.
Institutional Review Board Statement
The CENTER-TBI study (EC grant 602150) has been conducted in accordance with all relevant laws of the European Union (EU) if directly applicable or of direct effect and all relevant laws of the country where the recruiting sites were located. Informed consent by the patients and/or the legal representative/next of kin was obtained, accordingly to the local legislations, for all patients recruited in the Core Dataset of CENTER-TBI and documented in the electronic case report form (e-CRF). For the full list of sites, ethical committees, and ethical approval details, see the official CENTER-TBI website (https://www.center-tbi.eu/project/ethical-approval).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All relevant data are available upon request from CENTER-TBI, and the authors are not legally allowed to share it publicly. The authors confirm that they received no special access privileges to the data. CENTER-TBI is committed to data sharing and in particular to responsible further use of the data. Hereto, we have a data sharing statement in place: https://www.center-tbi.eu/data/sharing. The CENTER-TBI Management Committee, in collaboration with the General Assembly, established the Data Sharing policy, and Publication and Authorship Guidelines to assure correct and appropriate use of the data as the dataset is hugely complex and requires help of experts from the Data Curation Team or Bio- Statistical Team for correct use. This means that we encourage researchers to contact the CENTER-TBI team for any research plans and the Data Curation Team for any help in appropriate use of the data, including sharing of scripts. Requests for data access can be submitted online: https://www.center-tbi.eu/data. The complete Manual for data access is also available online: https://www.center-tbi.eu/files/SOP-Manual-DAPR-20181101.pdf.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Andelic N., Sigurdardottir S., Schanke A.-K., Sandvik L., Sveen U., Roe C. Disability, Physical Health and Mental Health 1 Year after Traumatic Brain Injury. Disabil. Rehabil. 2010;32:1122–1131. doi: 10.3109/09638280903410722. [DOI] [PubMed] [Google Scholar]
- 2.Sigurdardottir S., Andelic N., Roe C., Schanke A.-K. Cognitive Recovery and Predictors of Functional Outcome 1 Year after Traumatic Brain Injury. J. Int. Neuropsychol. Soc. 2009;15:740–750. doi: 10.1017/S1355617709990452. [DOI] [PubMed] [Google Scholar]
- 3.Phillips V.L., Greenspan A.I., Stringer A.Y., Stroble A.K., Lehtonen S. Severity of Injury and Service Utilization Following Traumatic Brain Injury: The First 3 Months. J. Head Trauma Rehabil. 2004;19:217–225. doi: 10.1097/00001199-200405000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Turner-Stokes L., Pick A., Nair A., Disler P.B., Wade D.T. Multi-Disciplinary Rehabilitation for Acquired Brain Injury in Adults of Working Age. Cochrane Database Syst. Rev. 2015 doi: 10.1002/14651858.CD004170.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andelic N., Ye J., Tornas S., Roe C., Lu J., Bautz-Holter E., Moger T., Sigurdardottir S., Schanke A.-K., Aas E. Cost-Effectiveness Analysis of an Early-Initiated, Continuous Chain of Rehabilitation after Severe Traumatic Brain Injury. J. Neurotrauma. 2014;31:1313–1320. doi: 10.1089/neu.2013.3292. [DOI] [PubMed] [Google Scholar]
- 6.Andelic N., Bautz-Holter E., Ronning P., Olafsen K., Sigurdardottir S., Schanke A.-K., Sveen U., Tornas S., Sandhaug M., Roe C. Does an Early Onset and Continuous Chain of Rehabilitation Improve the Long-Term Functional Outcome of Patients with Severe Traumatic Brain Injury? J. Neurotrauma. 2012;29:66–74. doi: 10.1089/neu.2011.1811. [DOI] [PubMed] [Google Scholar]
- 7.Jacob L., Cogné M., Tenovuo O., Røe C., Andelic N., Majdan M., Ranta J., Ylen P., Dawes H., Azouvi P., et al. Predictors of Access to Rehabilitation in the Year Following Traumatic Brain Injury: A European Prospective and Multicenter Study. Neurorehabil. Neural Repair. 2020;34:814–830. doi: 10.1177/1545968320946038. [DOI] [PubMed] [Google Scholar]
- 8.Ponsford J., Carrier S., Hicks A., McKay A. Assessment and Management of Patients in the Acute Stages of Recovery after Traumatic Brain Injury in Adults—A World-Wide Survey. J. Neurotrauma. 2020 doi: 10.1089/neu.2020.7299. [DOI] [PubMed] [Google Scholar]
- 9.Jourdan C., Bayen E., Darnoux E., Ghout I., Azerad S., Ruet A., Vallat-Azouvi C., Pradat-Diehl P., Aegerter P., Weiss J.-J., et al. Patterns of Post-Acute Health Care Utilization after a Severe Traumatic Brain Injury: Results from the PariS-TBI Cohort. Brain Inj. 2015;29:701–708. doi: 10.3109/02699052.2015.1004646. [DOI] [PubMed] [Google Scholar]
- 10.Andelic N., Soberg H.L., Berntsen S., Sigurdardottir S., Roe C. Self-Perceived Health Care Needs and Delivery of Health Care Services 5 Years after Moderate-to-Severe Traumatic Brain Injury. PM&R. 2014;6:1013–1021. doi: 10.1016/j.pmrj.2014.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Soberg H., Finset A., Roise O., Bautz-Holter E. Identification and Comparison of Rehabilitation Goals after Multiple Injuries: An ICF Analysis of the Patients’, Physiotherapists’ and other Allied Professionals’ Reported Goals. J. Rehabil. Med. 2008;40:340–346. doi: 10.2340/16501977-0174. [DOI] [PubMed] [Google Scholar]
- 12.Schumacher R., Walder B., Delhumeau C., Müri R.M. Predictors of Inpatient (Neuro)Rehabilitation after Acute Care of Severe Traumatic Brain Injury: An Epidemiological Study. Brain Inj. 2016;30:1186–1193. doi: 10.1080/02699052.2016.1183821. [DOI] [PubMed] [Google Scholar]
- 13.Cnossen M.C., Lingsma H.F., Tenovuo O., Maas A.I.R., Menon D., Steyerberg E.W., Ribbers G.M., Polinder S. Rehabilitation after Traumatic Brain Injury: A Survey in 70 European Neurotrauma Centres Participating in the CENTER-TBI Study. J. Rehabil. Med. 2017;49:395–401. doi: 10.2340/16501977-2216. [DOI] [PubMed] [Google Scholar]
- 14.Corrigan J.D., Whiteneck G., Mellick D. Perceived Needs Following Traumatic Brain Injury. J. Head Trauma Rehabil. 2004;19:205–216. doi: 10.1097/00001199-200405000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Ta’eed G., Skilbeck C., Slatyer M. Service Utilisation in a Public Post-Acute Rehabilitation Unit Following Traumatic Brain Injury. Neuropsychol. Rehabil. 2015;25:841–863. doi: 10.1080/09602011.2014.990043. [DOI] [PubMed] [Google Scholar]
- 16.Andelic N., Forslund M.V., Perrin P.B., Sigurdardottir S., Lu J., Howe E., Sveen U., Rasmussen M.S., Søberg H.L., Røe C. Long-Term Follow-Up of Use of Therapy Services for Patients with Moderate-to-Severe Traumatic Brain Injury. J. Rehabil. Med. 2020 doi: 10.2340/16501977-2662. [DOI] [PubMed] [Google Scholar]
- 17.Prang K.-H., Ruseckaite R., Collie A. Healthcare and Disability Service Utilization in the 5-Year Period Following Transport-Related Traumatic Brain Injury. Brain Inj. 2012;26:1611–1620. doi: 10.3109/02699052.2012.698790. [DOI] [PubMed] [Google Scholar]
- 18.Johnstone B., Nossaman L.D., Schopp L.H., Holmquist L., Rupright S.J. Distribution of Services and Supports for People with Traumatic Brain Injury in Ruraland Urban Missouri. J. Rural Health. 2002;18:109–117. doi: 10.1111/j.1748-0361.2002.tb00882.x. [DOI] [PubMed] [Google Scholar]
- 19.Jennekens N., de Casterlé B.D., Dobbels F. A Systematic Review of Care Needs of People with Traumatic Brain Injury (TBI) on a Cognitive, Emotional and Behavioural Level. J. Clin. Nurs. 2010;19:1198–1206. doi: 10.1111/j.1365-2702.2009.03114.x. [DOI] [PubMed] [Google Scholar]
- 20.Rathmann K., Nellen C., Wetzel L.D. Behinderungsspezifischer Gradient in der Psychischen Gesundheit und dem Gesundheitsbewusstsein: Ergebnisse der Repräsentativen GEDA-Studie für Deutschland. Rehabilitation. 2020;59:223–230. doi: 10.1055/a-1119-2905. [DOI] [PubMed] [Google Scholar]
- 21.Maas A.I.R., Menon D.K., Steyerberg E.W., Citerio G., Lecky F., Manley G.T., Hill S., Legrand V., Sorgner A. Collaborative European Neurotrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI): A Prospective Longitudinal Observational Study. Neurosurgery. 2015;76:67–80. doi: 10.1227/NEU.0000000000000575. [DOI] [PubMed] [Google Scholar]
- 22.Wilson J.T.L., Pettigrew L.E.L., Teasdale G.M. Structured Interviews for the Glasgow Outcome Scale and the Extended Glasgow Outcome Scale: Guidelines for Their Use. J. Neurotrauma. 1998;15:573–585. doi: 10.1089/neu.1998.15.573. [DOI] [PubMed] [Google Scholar]
- 23.Steyerberg E.W., Wiegers E., Sewalt C., Buki A., Citerio G., De Keyser V., Ercole A., Kunzmann K., Lanyon L., Lecky F., et al. Case-Mix, Care Pathways, and Outcomes in Patients with Traumatic Brain Injury in CENTER-TBI: A European Prospective, Multicentre, Longitudinal, Cohort Study. Lancet Neurol. 2019;18:923–934. doi: 10.1016/S1474-4422(19)30232-7. [DOI] [PubMed] [Google Scholar]
- 24.Wilson J.T.L., Edwards P., Fiddes H., Stewart E., Teasdale G.M. Reliability of Postal Questionnaires for the Glasgow Outcome Scale. J. Neurotrauma. 2002;19:999–1005. doi: 10.1089/089771502760341910. [DOI] [PubMed] [Google Scholar]
- 25.Publications Office of the European Union EuroVoc Thesaurus [(accessed on 9 January 2020)]; Available online: http://publications.europa.eu/resource/dataset/eurovoc.
- 26.Mayhew D., Mendonca V., Murthy B.V.S. A Review of ASA Physical Status—Historical Perspectives and Modern Developments. Anaesthesia. 2019;74:373–379. doi: 10.1111/anae.14569. [DOI] [PubMed] [Google Scholar]
- 27.Teasdale G., Jennett B. Assessment of Coma and Impaired Consciousness: A Practical Scale. Lancet. 1974;304:81–84. doi: 10.1016/S0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 28.Gennarelli T.A., Wodzin E. AIS 2005: A Contemporary Injury Scale. Injury. 2006;37:1083–1091. doi: 10.1016/j.injury.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 29.Gennarelli T.A., Wodzin E., Association for the Advancement of Automotive Medicine . Abbreviated Injury Scale 2005: Update 2008. Association for the Advancement of Automative Medicine; Barrington, IL, USA: 2008. [Google Scholar]
- 30.Baker S.P., O’Neill B., Haddon W., Long W.B. The Injury Severity Score: A Method for Describing Patients with Multiple Injuries and Evaluating Emergency Care. J. Trauma. 1974;14:187–196. doi: 10.1097/00005373-197403000-00001. [DOI] [PubMed] [Google Scholar]
- 31.Von Steinbuechel N., Wilson L., Gibbons H., Hawthorne G., Höfer S., Schmidt S., Bullinger M., Maas A., Neugebauer E., Powell J., et al. Quality of Life after Brain Injury (QOLIBRI): Scale Validity and Correlates of Quality of Life. J. Neurotrauma. 2010;27:1157–1165. doi: 10.1089/neu.2009.1077. [DOI] [PubMed] [Google Scholar]
- 32.Wilson J.T.L., Marsden-Loftus I., Koskinen S., Bakx W., Bullinger M., Formisano R., Maas A., Neugebauer E., Powell J., Sarajuuri J., et al. Interpreting Quality of Life after Brain Injury Scores: Cross-Walk with the Short Form-36. J. Neurotrauma. 2017;34:59–65. doi: 10.1089/neu.2015.4287. [DOI] [PubMed] [Google Scholar]
- 33.King N.S., Crawford S., Wenden F.J., Moss N.E., Wade D.T. The Rivermead Post Concussion Symptoms Questionnaire: A Measure of Symptoms Commonly Experienced after Head Injury and Its Reliability. J. Neurol. 1995;242:587–592. doi: 10.1007/BF00868811. [DOI] [PubMed] [Google Scholar]
- 34.Voormolen D.C., Cnossen M.C., Polinder S., von Steinbuechel N., Vos P.E., Haagsma J.A. Divergent Classification Methods of Post-Concussion Syndrome after Mild Traumatic Brain Injury: Prevalence Rates, Risk Factors, and Functional Outcome. J. Neurotrauma. 2018;35:1233–1241. doi: 10.1089/neu.2017.5257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Blevins C.A., Weathers F.W., Davis M.T., Witte T.K., Domino J.L. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. J. Trauma. Stress. 2015;28:489–498. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- 36.American Psychiatric Association, editor. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Publishing; Washington, DC, USA: 2013. [Google Scholar]
- 37.Stein M.B., Jain S., Giacino J.T., Levin H., Dikmen S., Nelson L.D., Vassar M.J., Okonkwo D.O., Diaz-Arrastia R., Robertson C.S., et al. Risk of Posttraumatic Stress Disorder and Major Depression in Civilian Patients after Mild Traumatic Brain Injury: A TRACK-TBI Study. JAMA Psychiatry. 2019;76:249–258. doi: 10.1001/jamapsychiatry.2018.4288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kroenke K., Spitzer R.L. The PHQ-9: A New Depression Diagnostic and Severity Measure. Psychiatr. Ann. 2002;32:509–515. doi: 10.3928/0048-5713-20020901-06. [DOI] [Google Scholar]
- 40.Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 41.Rubin D.B., editor. Multiple Imputation for Nonresponse in Surveys. John Wiley & Sons, Inc.; Hoboken, NJ, USA: 1987. (Wiley Series in Probability and Statistics). [Google Scholar]
- 42.Azur M.J., Stuart E.A., Frangakis C., Leaf P.J. Multiple Imputation by Chained Equations: What Is It and How Does It Work? Int. J. Methods Psychiatr. Res. 2011;20:40–49. doi: 10.1002/mpr.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Heinze G., Dunkler D. Five Myths about Variable Selection. Transpl. Int. 2017;30:6–10. doi: 10.1111/tri.12895. [DOI] [PubMed] [Google Scholar]
- 44.Nagelkerke N.J.D. A Note on a General Definition of the Coefficient of Determination. Biometrika. 1991;78:691–692. doi: 10.1093/biomet/78.3.691. [DOI] [Google Scholar]
- 45.Bamber D. The Area above the Ordinal Dominance Graph and the Area below the Receiver Operating Characteristic Graph. J. Math. Psychol. 1975;12:387–415. doi: 10.1016/0022-2496(75)90001-2. [DOI] [Google Scholar]
- 46.Hanley J.A., McNeil B.J. The Meaning and Use of the Area under a Receiver Operating Characteristic (ROC) Curve. Radiology. 1982;143:29–36. doi: 10.1148/radiology.143.1.7063747. [DOI] [PubMed] [Google Scholar]
- 47.Mandrekar J.N. Receiver Operating Characteristic Curve in Diagnostic Test Assessment. J. Thorac. Oncol. 2010;5:1315–1316. doi: 10.1097/JTO.0b013e3181ec173d. [DOI] [PubMed] [Google Scholar]
- 48.R Core Team . R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; Vienna, Austria: 2020. [Google Scholar]
- 49.Van Buuren S., Groothuis-Oudshoorn K. Mice: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2011;45:1–67. doi: 10.18637/jss.v045.i03. [DOI] [Google Scholar]
- 50.Heymans M. Psfmi: Prediction Model Selection and Performance Evaluation in Multiple Imputed Datasets. [(accessed on 12 January 2020)]. R Package Version 0.5.0. Available online: https://CRAN.R-project.org/package=psfmi. [Google Scholar]
- 51.Pradat-Diehl P., Joseph P.-A., Beuret-Blanquart F., Luauté J., Tasseau F., Remy-Neris O., Azouvi P., Sengler J., Bayen É., Yelnik A., et al. Physical and Rehabilitation Medicine (PRM) Care Pathways: Adults with Severe Traumatic Brain Injury. Ann. Phys. Rehabil. Med. 2012;55:546–556. doi: 10.1016/j.rehab.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 52.Majdan M., Plancikova D., Brazinova A., Rusnak M., Nieboer D., Feigin V., Maas A. Epidemiology of Traumatic Brain Injuries in Europe: A Cross-Sectional Analysis. Lancet Public Health. 2016;1:e76–e83. doi: 10.1016/S2468-2667(16)30017-2. [DOI] [PubMed] [Google Scholar]
- 53.Jennett B., Snoek J., Bond M.R., Brooks N. Disability after Severe Head Injury: Observations on the Use of the Glasgow Outcome Scale. J. Neurol. Neurosurg. Psychiatry. 1981;44:285–293. doi: 10.1136/jnnp.44.4.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wilson J.T.L., Stewart W., Dams-O’Connor K., Diaz-Arrastia R., Horton L., Menon D.K., Polinder S. The Chronic and Evolving Neurological Consequences of Traumatic Brain Injury. Lancet Neurol. 2017;16:813–825. doi: 10.1016/S1474-4422(17)30279-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sveen U., Røe C., Sigurdardottir S., Skandsen T., Andelic N., Manskow U., Berntsen S.A., Soberg H.L., Anke A. Rehabilitation Pathways and Functional Independence One Year after Severe Traumatic Brain Injury. Eur. J. Phys. Rehabil. Med. 2016;52:650–661. [PubMed] [Google Scholar]
- 56.Althubaiti A. Information Bias in Health Research: Definition, Pitfalls, and Adjustment Methods. J. Multidiscip. Healthc. 2016;9:211–217. doi: 10.2147/JMDH.S104807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Arnould A., Dromer E., Rochat L., Van der Linden M., Azouvi P. Neurobehavioral and Self-Awareness Changes after Traumatic Brain Injury: Towards New Multidimensional Approaches. Ann. Phys. Rehabil. Med. 2016;59:18–22. doi: 10.1016/j.rehab.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 58.Sauerbrei W., Royston P., Binder H. Selection of Important Variables and Determination of Functional Form for Continuous Predictors in Multivariable Model Building: Selection of Variables and Functional Forms. Stat. Med. 2007;26:5512–5528. doi: 10.1002/sim.3148. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All relevant data are available upon request from CENTER-TBI, and the authors are not legally allowed to share it publicly. The authors confirm that they received no special access privileges to the data. CENTER-TBI is committed to data sharing and in particular to responsible further use of the data. Hereto, we have a data sharing statement in place: https://www.center-tbi.eu/data/sharing. The CENTER-TBI Management Committee, in collaboration with the General Assembly, established the Data Sharing policy, and Publication and Authorship Guidelines to assure correct and appropriate use of the data as the dataset is hugely complex and requires help of experts from the Data Curation Team or Bio- Statistical Team for correct use. This means that we encourage researchers to contact the CENTER-TBI team for any research plans and the Data Curation Team for any help in appropriate use of the data, including sharing of scripts. Requests for data access can be submitted online: https://www.center-tbi.eu/data. The complete Manual for data access is also available online: https://www.center-tbi.eu/files/SOP-Manual-DAPR-20181101.pdf.