Abstract
Introduction:
Anterior openbite (AOB) continues to be a challenging malocclusion for orthodontists to treat and retain long-term. There is no consensus on which treatment modality is most successful. This study reports on the overall success rate of AOB orthodontic treatment in the adult population across the United States, as well as four major treatment modalities and other factors that may influence treatment success.
Methods:
Practitioners and their adult AOB patients were recruited through the National Dental Practice-Based Research Network (PBRN). Patient dentofacial and demographic characteristics, practitioner demographic and practice characteristics, and factors relating to orthodontic treatment were reported. Treatment success was determined from post-treatment lateral cephalometric films and intraoral frontal photos. Treatment was categorized into four main groups: aligners, fixed appliances, temporary anchorage devices (TADs) and orthognathic surgery. Extractions were also evaluated. Bivariate and multivariable models were used to investigate the association between treatment success and treatment modality, pre-treatment dentofacial characteristics, patient and practitioner demographics, and practice characteristics, adjusting for clustering of patients within practice.
Results:
A total of 254 patients, enrolled by 84 practitioners, contributed end of active treatment data for this study. There were 29 patients in the aligner group, 152 in fixed appliances, 20 in TADs, and 53 in surgery. A total of 49 patients underwent extractions of teeth other than third molars. Ninety-three percent finished treatment with positive overbite on the post-treatment lateral cephalogram, and 84% finished with positive vertical overlap of all incisors. The small number of aligner and TAD patients limited the ability to compare success rates in these groups. Patients treated with orthognathic surgery had a higher rate of success compared to those treated with fixed appliances only. Treatment success was also associated with academic practice setting, pre-treatment MPSN≤30°, no to mild pre-treatment crowding, and treatment duration < 30 months.
Conclusions:
The overall success of orthodontic treatment in adult AOB patients who participated in this study was very high. Orthognathic surgery was the only treatment modality that exhibited a statistically higher odds of successful outcomes. Some pre-treatment dentofacial characteristics and treatment factors were associated with successful closure of AOB.
INTRODUCTION
Anterior open bite (AOB) is defined by a lack of vertical overlap between the incisal edges of the maxillary and mandibular teeth. The prevalence of AOB has been reported to range between 0.6% and 16.5%, varying by ethnic group, age, and stage of dentition.1 This malocclusion can have significant functional and psychological effects on patients. Patients with AOB may have difficulty incising food and enunciating certain phonemes, due to the altered tongue position on the incisors and the anterior hard palate.2 Furthermore, AOB development is often associated with unfavorable growth patterns, oral habits (i.e., digit sucking and tongue posture), and nasopharyngeal airway obstructions.3 Due to its complex and multifactorial etiology, AOB continues to be one of the most challenging malocclusions for orthodontists to successfully treat and retain.
Patients with AOB can be treated using a variety of orthodontic treatment modalities. Standard edge-wise fixed appliances (FA) are commonly recommended for patients with AOB.4 Fixed appliances with extrusive mechanics for the anterior teeth can create overlap between maxillary and mandibular incisors, however, this may lead to increased gingival display and is associated with a high potential for relapse. In some cases, practitioners may elect to treat AOB patients with orthognathic surgery (SX), especially when a non-growing, adult patient presents with an AOB that is of skeletal origin. Surgery may involve the maxilla, mandible, or both to skeletally correct the AOB.5
In recent decades, the use of temporary anchorage devices (TADs) has become a popular non-surgical technique for correcting AOB.6 Mini-screws or mini-plates are used to provide anchorage for molar and premolar intrusion. Several case reports have shown TAD molar intrusion to be as successful as orthognathic surgery, suggesting a less invasive and less costly alternative to surgery.7
Clear aligner therapy (ALN) is another recently-developed alternative to traditional fixed appliances for AOB. The thickness of the plastic on the occlusal surfaces, in combination with the forces of mastication, are believed to produce an intrusive force on the posterior dentition which may aid with AOB closure.8,9 Although several case studies have demonstrated successful AOB correction, molar intrusion has not been confirmed.10,11
Extractions of premolars, and in some cases molars, may be recommended for AOB correction, especially in the presence of crowding. Premolar extractions are used to create space for greater incisor retraction and uprighting to close the AOB through what is often referred to as the “drawbridge” effect.12,13 Molar extractions allow molars to move anteriorly (“wedge effect”), resulting in a closing rotation of the mandible.6,14
Although there are a variety of orthodontic treatment modalities used to correct AOB in adults, there is still no consensus on what method(s) are most successful.15,16 A better understanding of the success rates for these treatments, as well as other factors that may influence treatment outcome, would greatly aid clinicians in the management of these patients. The purpose of this large observational prospective cohort study, conducted under the auspices of the National Dental Practice-Based Research Network (PBRN), was to explore treatment recommendations, outcomes, and stability of adult AOB patients. This publication reports on the overall success rate of AOB treatment, and explores how treatment success varies with treatment modality, pre-treatment dentofacial characteristics, and patient and practitioner demographic and practice characteristics.
MATERIALS AND METHODS
Dental providers and their adult AOB patients were recruited from six regions of the National Dental PBRN (West, Midwest, Southwest, South Central, South Atlantic and Northeast). Institutional Review Board (IRB) approval was obtained from the University of Alabama at Birmingham IRB (acting as the Central IRB), the Kaiser Permanente IRB (for the Western region), and the University of Rochester Research Subjects Review Board (for the Northeastern region). Additionally, institutional IRB approval was obtained at individual academic settings when required. Practitioners and patients were compensated for their participation in this study. As members of the National Dental PBRN, the practitioners completed an enrollment questionnaire that elicited information on their training and practices.
Inclusion criteria for practitioners:
Orthodontist or dentist who routinely performs orthodontic treatment.
Estimates to recruit three to eight adult patients in active treatment for AOB, and expects to have treatment completed within 24 months of enrollment into the study.
Routinely takes cephalometric radiographs (cephalogram) before and after treatment.
Able to upload de-identified cephalogram and digital intraoral frontal photographs to a central data repository.
Affirms that the practice can devote sufficient time in patient scheduling to allow recording of all data required for the study.
Does not anticipate retiring, selling the practice, or moving during the study.
Inclusion Criteria for Patients:
At least 18 years of age at time or enrollment.
Must have an AOB, which is defined as one or more incisors that do not have vertical overlap with teeth in the opposing arch. The remaining incisors may have minimal incisor overlap, but none can contact teeth in the opposing arch.
Must be in active treatment for AOB, and expect to have treatment completed within 24 months of enrollment into the study.
Must have an initial cephalogram (taken prior to the beginning of treatment). A cephalogram created from a cone-beam CT scan is acceptable.
Exclusion Criteria for Patients:
Clefts, craniofacial conditions or syndromes.
Significant physical, mental, or medical conditions that would affect treatment compliance, cooperation, or outcome.
Expects to move before the completion of the study.
Initial treatment plans estimated to be more than 36 months.
Pre-treatment (T1) questionnaires were completed by practitioners and patients at the enrollment visit to obtain information about patient characteristics, pre-treatment diagnosis, and recommended/ accepted treatment. Once active treatment was complete, end-of active treatment (T2) questionnaires were completed by practitioners and their patients to obtain information about treatment methods used. All study forms can be accessed at https://www.nationaldentalpbrn.org/study-results/#1589299528044-b9cab599-914e
Pre-treatment (T1) and post-treatment (T2) lateral cephalometric images were collected. These images were traced using Dolphin imaging software (version 11.0; Dolphin Imaging and Management Solutions, Chatsworth, Calif) and measurements were generated using an automated, custom analysis. Cephalometric landmarks, summarized in Figure 1, were first identified by one examiner and reviewed by the second examiner. Disagreements in landmark identification were resolved by means of consensus between the two examiners, with a third examiner consulting if the two could not reach a consensus.
Figure 1.
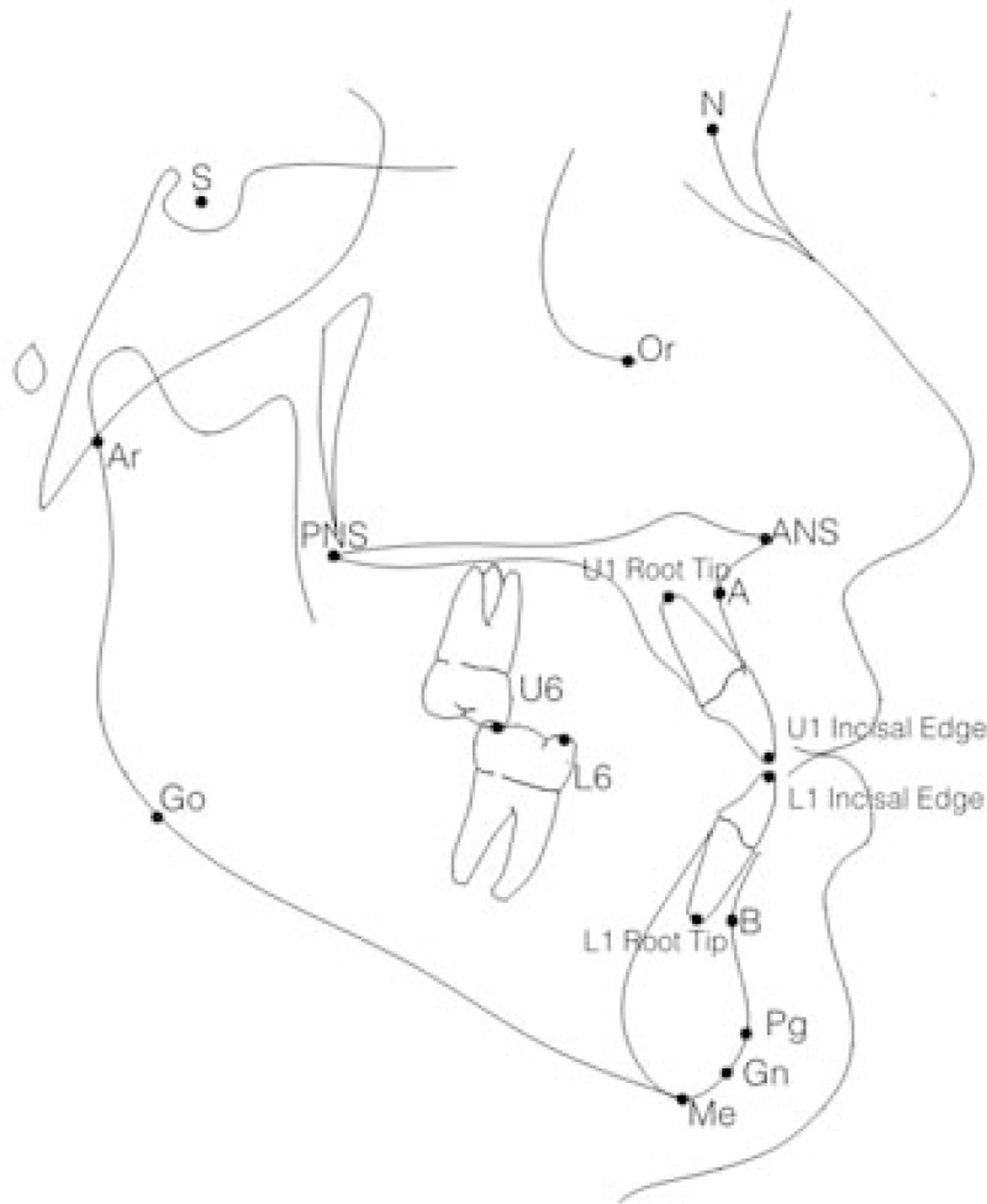
Cephalometric landmarks identified on pre- and post-treatment lateral cephalograms: sella (S), nasion (N), anterior nasal spine (ANS), posterior nasal spine (PNS), pogonion (Pg), gnathion (Gn), menton (Me), anatomic gonion (Go), articulare (Ar), A-point (A), B-point (B), incisal edge of the maxillary incisor (U1 incisal edge), root tip of the maxillary incisor (U1 root tip), incisal edge of the mandibular incisor (L1 incisal edge), root tip of the mandibular incisor (L1 root tip), mesiobuccal cusp tip of the maxillary first molar (U6), mesiobuccal cusp tip of the mandibular first molar (L6).
A standard millimetric ruler in the cephalostat was used to calibrate millimetric measurements. When a ruler was present in only one of a patient’s cephalograms (either pre- or post-treatment), the sella-nasion distance of the lateral cephalogram with the ruler present was used to calibrate the cephalogram without the ruler (13 patients). When a ruler was not present on both a patient’s pre- and post-treatment cephalograms (14 patients), a standard distance for nasion-menton, based on published norms, was used to calibrate the pre-treatment cephalogram.17,18 The post-treatment lateral cephalogram was then calibrated using the sella-nasion distance of the pre-treatment lateral cephalogram, as described above.
Pre- and post-treatment intraoral frontal photos were de-identified and forwarded to the research team at the University of Washington. The Photographic Openbite Severity Index (POSI) was developed to score the severity of the patient’s pre-treatment AOB and final result using the pre-and post-treatment intraoral frontal photographs. Seven categories were developed based on the number and type of teeth with vertical overlap (Figure 2).
Figure 2.
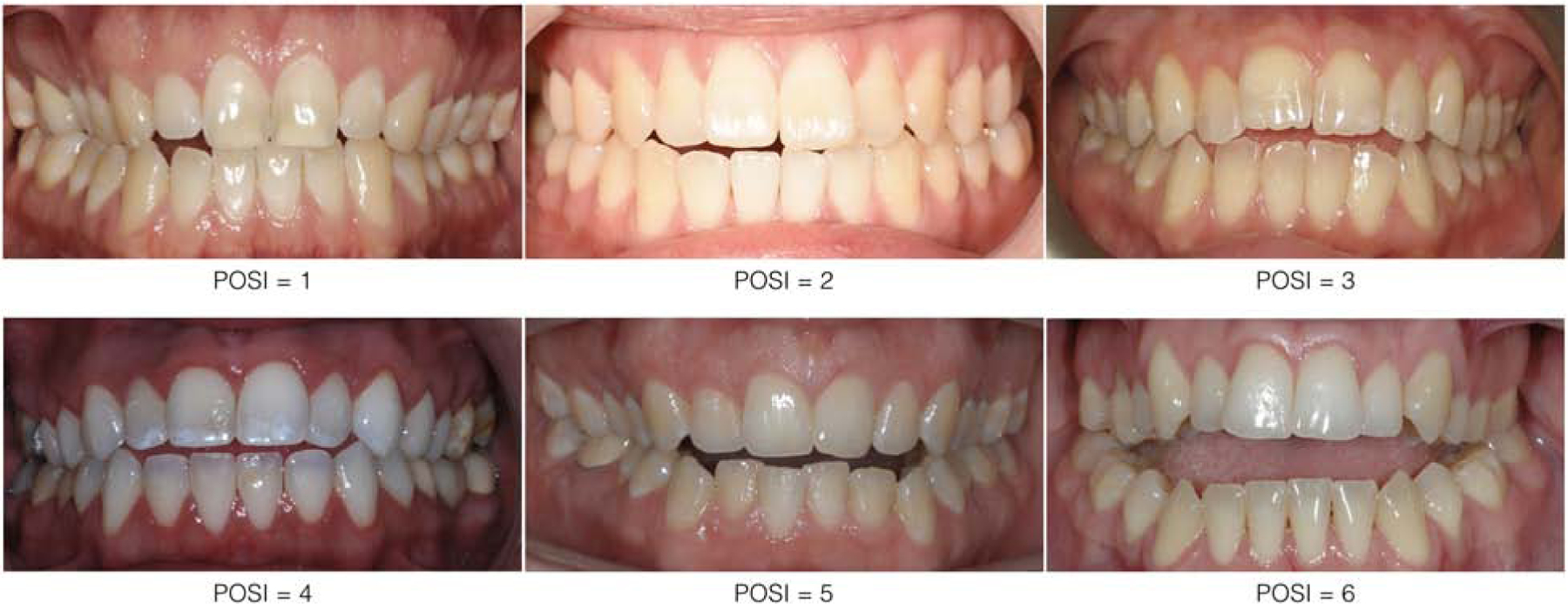
Photographic Openbite Severity Index (POSI)
0 = All four incisor with positive overlap
1 = One or two maxillary lateral incisors without vertical overlap (but both maxillary central incisors have vertical overlap)
2 = One maxillary central incisor without vertical overlap (the other maxillary central has vertical overlap)
3 = Two maxillary central incisors without vertical overlap (at least one maxillary lateral has vertical overlap)
4 = All four maxillary incisors without vertical overlap
5 = All anterior teeth, including canines, without overlap
6 = All anterior teeth, including canines, plus at least one premolar without vertical overlap
Each image was rated independently by the same two examiners, and the scores were compared. Disagreements in ratings were resolved by means of consensus between the examiners, with a third examiner consulting if the two could not reach a consensus.
To calculate intra- and inter-rater reliability, ten cephalometric images and twenty intraoral frontal images were randomly selected. Cephalometric images were traced and frontal photographic images were rated by each evaluator and repeated one month later. Both inter- and intra-rater reliability were excellent as determined using intraclass correlations. For the cephalometric analysis, the mean inter-rater reliability was 97% and the mean intra-rater reliability was 98%. For the POSI, the inter-rater mean percent agreement was 92.5% and the mean kappa was 95.5%. The intra-rater mean percent agreement was 97% and the mean kappa was 98.5%.
DATA ANALYSIS
Treatment success was defined using the following outcomes measures:
Cephalometric analysis - Lateral cephalometric radiographs were used to evaluate treatment success, defined by positive overbite at the end of active treatment (T2). The most anterior central incisors were measured.
Photographic Openbite Severity Index (POSI) - Intraoral frontal photographs were used to evaluate treatment success, defined by a score of 0 (all four incisors with positive overlap) at the end of active treatment (T2).
Success rates were calculated for the following variables to identify potential factors related to successful AOB treatment:
Treatment modality (ALN, FA, TAD, SX, and extractions)
Patient pre-treatment dentofacial characteristics
Treatment duration
Patient demographic characteristics
Practitioner demographic and practice characteristics
Treatment was ascertained based on the enrollment and post-treatment questionnaires, with the latter enquiring about any changes in the treatment plan that were implemented after the enrollment time. In cases where there were inconsistencies in reported treatment, clinical records were reviewed to confirm treatment.
Four mutually exclusive treatment categories were identified for investigation:
Aligners (ALN) (with no fixed appliances, TADs, or orthognathic surgery)
Fixed appliances (FA) (with no TADs, or orthognathic surgery)
Temporary anchorage devices (TAD) (with no orthognathic surgery)
Orthognathic surgery (SX)
The treatment groups represent an increasing ability to manage complex malocclusions and an increasing level of invasiveness. Patients with treatment from multiple categories were categorized into the more invasive treatment category. For example, a patient treated with both aligners and fixed appliances was placed in the fixed appliances group. Almost all patients in the TADs or orthognathic surgery groups also underwent fixed appliances. Extractions of premolar or anterior teeth were also identified, which could be performed in combination with any of the treatment groups listed above.
Patient pre-treatment dentofacial characteristics were reported at enrollment and cephalometric values were obtained from pre-treatment cephalograms. Dentofacial characteristics identified for examination included, profile, molar classification, maxillary and mandibular crowding, posterior cross-bite, facial pattern, habits, and missing teeth. Pre-treatment cephalometric values evaluated included: ANB (°), MP-SN (°), IMPA (°), and overbite (mm).
Duration of active orthodontic treatment was calculated as the time from appliance placement to appliance removal, based on information from the enrollment and end of active treatment questionnaires, respectively. Patient characteristics included age, gender, race, insurance coverage, education level, and previous orthodontic treatment. Practitioner characteristics included, specialization, country of dental school, age when enrolled in dental network, gender, race and ethnicity, years since graduated dental school, geographic region of practice, and practice type.
Descriptive statistics were performed on the patient and practitioner sample.
Overall success rates were calculated based on the following outcome measures:
Positive overbite (mm) on post-treatment lateral cephalogram.
Post-treatment POSI equal to zero, indicating positive overlap of all anterior teeth.
Because the cephalometric overbite measurements were only based on the most anterior central incisors, the POSI, which assesses the vertical position of all incisors, was used in most analyses.
Success rates for treatment modality, patient pre-treatment dentofacial characteristics and cephalometric measures, treatment duration, patient demographic characteristics, and practitioner demographic and practice characteristics were obtained. Bivariate analyses were performed to preliminarily identify factors with statistically significant differences in treatment success. Clustering of patients within practitioners were adjusted for by using a generalized estimating equation (GEE). This was implemented using PROC GENMOD in SAS with the CORR=EXCH option.
Multivariable predictive models were developed to identify predictors for treatment success, defined as POSI=0. Specifically, the differences between success rates for different treatment categories (i.e., SX vs. no SX, SX vs. FA, TADs vs FA, ALN vs. FA) were explored. The predictive models were developed by entering all variables with p <0.10 after adjusting for clustering of patients within practices. Backwards elimination was performed until all characteristics had a p<0.10. Treatment category, extractions, and initial overbite (mm) were retained in the final reduced models regardless of significance level because of clinical importance. SAS software was used to perform all statistical analyses (SAS v9.4, SAS Institute Inc., Cary NC).
RESULTS
A total of 91 practitioners and 347 patients and were recruited for this study from October 2015 to June 2016. End-of-active treatment data were collected from 84 practitioners and 260 patients through December 2018. Six patients had insufficient data for analyses, leaving a total of 254. The remainder of the practitioners and patients either withdrew from the study (24) or did not complete treatment within the study period (63). Additionally, 24 patients were missing T2 cephalometric data, leaving a total of 230 patients for cephalometric analysis. Patients missing T2 intraoral images (22) were excluded from the POSI analysis, resulting in a total of 232 patients for POSI analysis.
The mean age of the practitioner sample was 48.8 years (SD = 9.8 years; range = 31–66 years), and 73% were male. The mean age of the patient sample was 32.1 years (SD = 11.9 years; range: 18–71 years), 75% were female, and 42% of the patients had prior orthodontic treatment. Details of practitioner and patient demographic characteristics are summarized in Tables 1 and 2.
Table 1.
Practitioner demographics
| N | % | |
|---|---|---|
| Status | ||
| Orthodontist | 82 | 98% |
| General practitioner | 2 | 2% |
| Gender | ||
| Male | 61 | 73% |
| Female | 23 | 27% |
| Age, years | ||
| < 45 | 32 | 38% |
| 45 – 54 | 24 | 29% |
| 55 – 64 | 23 | 27% |
| ≥ 65 | 5 | 6% |
| Race and ethnicity (N = 83) | ||
| White/Caucasian | 52 | 63% |
| Asian | 19 | 23% |
| Multirace | 2 | 2% |
| Hispanic | 10 | 12% |
| Geographic region of practice | ||
| West | 34 | 41% |
| Midwest | 8 | 10% |
| Southwest | 16 | 19% |
| South Central | 6 | 7% |
| South Atlantic | 9 | 11% |
| Northeast | 11 | 13% |
N = 84, unless indicated otherwise
Table 2.
Patient demographics
| N | % | |
|---|---|---|
| Gender (N = 253) | ||
| Male | 64 | 25% |
| Female | 189 | 75% |
| Age, years (N = 253) | ||
| 18 – 20 | 43 | 17% |
| 21 – 30 | 106 | 42% |
| 31 – 40 | 58 | 23% |
| ≥ 41 | 46 | 18% |
| Race and ethnicity (N = 253) | ||
| White/Caucasian | 146 | 58% |
| Black/African-American | 23 | 9% |
| Asian | 24 | 9% |
| Multirace | 8 | 3% |
| Hispanic | 52 | 21% |
| Previous orthodontic treatment (N = 253) | ||
| Yes | 106 | 42% |
| No | 147 | 58% |
| Insurance coverage (N=254) | ||
| No dental or medical insurance | 54 | 21% |
| Dental insurance does not cover orthodontics | 64 | 25% |
| Dental insurance covers orthodontics | 74 | 29% |
| Insurance covers orthognathic surgery | 62 | 24% |
| Highest level of education (N = 253) | ||
| High school graduate or less | 45 | 18% |
| Some college or associate degree | 79 | 31% |
| Bachelor degree | 84 | 33% |
| Graduate degree | 45 | 18% |
The mean pre-treatment (T1) overbite measured from the lateral cephalograms was −2.3mm (SD = 2.1; range = −12.9 to 1.1mm). All patients did not have vertical overlap of at least one incisor (POSI >0), and no incisors had contact with opposing teeth. Sixty-five percent (N=151) exhibited no vertical overlap of all four incisors (POSI ≥ 4).
The mean post-treatment (T2) overbite measured from the lateral cephalograms was 1.3mm (SD = 1.1mm; range = −5.6 to 3.7mm). Ninety-three percent of patients (N=215) had a positive overbite measured on the post-treatment lateral cephalogram. Eighty-four percent (N=194) of the patients exhibited positive vertical overlap of all anterior teeth at the end of treatment (POSI=0). A summary of pre- and post-treatment POSI scores are presented in Table 3. Two-thirds of our sample was classified as having a long-face skeletal pattern based on the vertical morphological classification system.19
Table 3.
Pre-treatment (T1) and post-treatment (T2) POSI scores
| POSI at T1 | # of patients | POSI at T2 | ||||||
|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | ||
| 1 | 35 | 33 | 2 | 0 | 0 | 0 | 0 | 0 |
| 2 | 34 | 27 | 7 | 0 | 0 | 0 | 0 | 0 |
| 3 | 12 | 9 | 1 | 0 | 1 | 1 | 0 | 0 |
| 4 | 85 | 70 | 11 | 2 | 1 | 1 | 0 | 0 |
| 5 | 13 | 9 | 4 | 0 | 0 | 0 | 0 | 0 |
| 6 | 53 | 46 | 2 | 1 | 0 | 0 | 2 | 2 |
| total | 232 | 194 | 27 | 3 | 2 | 2 | 2 | 2 |
Frequency Missing = 22
Eleven percent of patients were treated with aligners only, 60% with fixed appliances only (no TADS or SX), 8% with TADs (no SX), and 21% with surgery. Most of the TAD and SX patients also underwent fixed appliance therapy. Despite a recommendation rate of 37% for orthognathic surgery, only 21% of patients who completed treatment had surgery.20 Treatment is summarized in Table 4.
Table 4.
Treatment summary
| Final Treatment Category | Extractions | |||
|---|---|---|---|---|
| N | % | No | Yes | |
| Aligners only | 29 | 11% | 29 | 0 |
| Fixed (no TADs or surgery) | 152 | 60% | 111 | 41 |
| TADs (no surgery) | 20 | 8% | 17 | 3 |
| Surgery | 53 | 21% | 48 | 5 |
| Treatment duration | POSI at T2 = 0 |
|||
| N=190 | % | |||
| <17 months | 52 | 23% | 45 | 86% |
| 17 – 22 months | 52 | 23% | 44 | 85% |
| 23 – 29 months | 70 | 31% | 63 | 90% |
| 30+ months | 54 | 24% | 38 | 70% |
Patients in the TADs and surgery treatment groups exhibited slightly higher success rates compared to those treated with aligners or with fixed appliances only, but these differences were not statistically significant when comparing all four groups in a single model (Table 5).
Table 5.
Treatment modality and extractions vs. treatment success
| ALL | POSI = 0 |
P | Extractions | POSI = 0 |
P | No Extractions | POSI = 0 |
P | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N=232 | N=194 | % | N=45 | N=34 | % | N=187 | N=160 | % | ||||
| Final Treatment Category | 0.3 | NE | 0.4 | |||||||||
| Aligners only | 26 | 21 | 81% | 0 | 0 | Undefined | 26 | 21 | 81% | |||
| Fixed (no TADs or surgery) | 141 | 114 | 81% | 37 | 27 | 73% | 104 | 87 | 84% | |||
| TADs (no surgery) | 19 | 17 | 89% | 3 | 2 | 67% | 16 | 15 | 94% | |||
| Surgery | 46 | 42 | 91% | 5 | 5 | 100% | 41 | 37 | 90% | |||
| missing n=22 | ||||||||||||
| Extractions | 0.2 | |||||||||||
| No | 187 | 160 | 86% | |||||||||
| Yes | 45 | 34 | 76% | |||||||||
| OR=0.5 | ||||||||||||
Percents are “row” %s, namely, the proportion of the “outcome” treatment (column heading) for that treatment comparison.
P-values are adjusted for clustering of patients within practitioners using generalized estimating equations
NE: Not estimable
Nineteen percent of patients had extractions of anterior or premolar teeth for orthodontic treatment. Extractions were most common in the fixed appliances treatment group. No patients treated with aligners had extractions. Only three patients treated with TADs and five patients treated with surgery had extractions. Although non-extraction patients had a 10% greater success than those treated with extractions (86% vs. 76%), this difference did not reach statistical significance (Table 5).
Pre-treatment dentofacial characteristics were evaluated for differences in treatment success. The results are summarized in Table 6. Initial crowding was the only characteristic with significance in the bivariate analysis. Success rates were about 17% higher in patients with less crowding.
Table 6.
Patient pre-treatment dentofacial characteristics and cephalometric values vs. treatment success.
| Patient dentofacial characteristics | ALL | POSI = 0 |
P | |
|---|---|---|---|---|
| N=232 | N=194 | % | ||
| Profile | 0.4 | |||
| Convex | 120 | 96 | 80% | |
| Straight | 92 | 80 | 87% | |
| Concave | 20 | 18 | 90% | |
| Molar class | 0.4 | |||
| I: Half or full cusp | 102 | 89 | 87% | |
| II: Half or full cusp | 71 | 55 | 77% | |
| III: Half or full cusp | 58 | 49 | 84% | |
| Arch length | 0.038 | |||
| No crowding | 44 | 40 | 91% | |
| Mild crowding (1–3mm) | 94 | 85 | 90% | |
| Moderate crowding (4–6mm) | 71 | 52 | 73% | |
| Severe crowding (>6mm) | 23 | 17 | 74% | |
| Posterior crossbite | 0.8 | |||
| None | 137 | 116 | 85% | |
| Unilateral | 46 | 37 | 80% | |
| Bilateral | 49 | 41 | 84% | |
| AOB Severity index (POSI) | 0.6 | |||
| 1–3 | 81 | 69 | 85% | |
| 4–6 | 151 | 125 | 83% | |
| Cephalometric values | ||||
| ANB (deg) | 0.3 | |||
| <0 | 31 | 28 | 90% | |
| 0 – 4 | 111 | 95 | 86% | |
| >4 | 84 | 65 | 77% | |
| missing n=6 | ||||
| Mandibular plane angle (MPSN, deg) | 0.07 | |||
| ≤30 deg | 24 | 23 | 96% | |
| >30 – 34 deg | 37 | 32 | 86% | |
| >34 – 38 deg | 50 | 41 | 82% | |
| >38 deg | 114 | 91 | 80% | |
| missing n=7 | ||||
| Overbite (mm) | 0.9 | |||
| ≤ −4 | 32 | 27 | 84% | |
| > −4 to −2 | 84 | 68 | 81% | |
| > −2 to 0 | 92 | 78 | 85% | |
| >0 | 19 | 16 | 84% | |
| continuous | OR = 1.10 | 0.3 | ||
| missing n=5 | ||||
| Mandibular incisor angulation (IMPA, deg) | 0.2 | |||
| ≤86 | 37 | 29 | 78% | |
| >86 – 90 | 25 | 21 | 84% | |
| >90 – 94 | 44 | 38 | 86% | |
| >94 – 98 | 42 | 39 | 93% | |
| >98 | 78 | 61 | 78% | |
| missing n=6 | 186 | |||
Percents are “row” %s, namely, the proportion of the “outcome” treatment (column heading) for that treatment comparison.
P-values are adjusted for clustering of patients within practitioners using generalized estimating equations
Patient pre-treatment cephalometric values were evaluated for differences in rates of treatment success. Steeper mandibular planes displayed a trend to be associated with less treatment success (P=0.07). There was no difference in success rates based on the magnitude of pre-treatment overbite when evaluated as either a categorical or continuous variable. Success rates ranged from 81% to 85%, based on the initial overbite measurements.
The mean treatment duration was 24.8 months (SD = 11.3 months; range = 1–72 months). There was no significant difference in treatment times between treatment groups. However, success rates were higher in patients with shorter treatment duration. Patients with treatment durations <30 months were 17% more successful than those with treatment >30 months (70% vs. 87%, P=0.02) (Table 4).
Patient demographic characteristics, including gender, age, race, type of insurance coverage, education level, and history of prior orthodontic treatment, did not have a significant effect on treatment success (Table 7).
Table 7.
Patient demographic characteristics vs. treatment success
| Patient demographics | ALL | POSI = 0 |
P | |
|---|---|---|---|---|
| N=232 | N=194 | Row % | ||
| Gender | 0.9 | |||
| Male | 57 | 48 | 84% | |
| Female | 174 | 145 | 83% | |
| Age, years | 0.12 | |||
| 18 – 20 | 38 | 29 | 76% | |
| 21 – 30 | 94 | 85 | 90% | |
| 31 – 40 | 57 | 48 | 84% | |
| ≥ 41 | 42 | 31 | 74% | |
| Race and ethnicity | 0.9 | |||
| White/Caucasian | 137 | 114 | 83% | |
| Black/African-American | 18 | 16 | 89% | |
| Asian | 22 | 19 | 86% | |
| Multirace, other | 8 | 6 | 75% | |
| Hispanic | 46 | 38 | 83% | |
| Insurance coverage | 0.7 | |||
| No dental or medical insurance | 50 | 43 | 86% | |
| Dental insurance does not cover orthodontics | 58 | 49 | 84% | |
| Dental insurance covers orthodontics | 68 | 53 | 78% | |
| Insurance covers orthognathic surgery | 56 | 49 | 87% | |
| Education level | 0.9 | |||
| High school graduate or less | 40 | 33 | 82% | |
| Some college or associate degree | 74 | 60 | 81% | |
| Bachelor degree | 77 | 66 | 86% | |
| Graduate degree | 40 | 34 | 85% | |
| Previous orthodontic treatment | 0.15 | |||
| No | 136 | 118 | 87% | |
| Yes | 95 | 75 | 79% | |
Percents are “row” %s, namely, the proportion of the “outcome” treatment (column heading) for that treatment comparison.
P-values are adjusted for clustering of patients within practitioners using generalized estimating equations
Practitioner characteristics were examined for differences in treatment success. Practice type was the only variable with significant differences in treatment success (Table 8). Patients treated by practitioners in an academic setting had the highest success rate (98%), while those treated in preferred provider practice settings had the lowest success rate (69%). The success rate for an academic practice setting was 18% greater than for non-academic settings (OR=10.5; P=0.005). Forty-two of the 43 patients treated in an academic setting had successful closures of their openbite (Table 9). It is important to note the greater percentage of patients treated with surgery and TADs in academic settings compared to other practice settings.
Table 8.
Practitioner demographic and practice characteristics vs. treatment success
| Practitioner characteristics | ALL | POSI = 0 |
P | |
|---|---|---|---|---|
| N=232 | N=194 | Row % | ||
| Country trained in | 0.6 | |||
| United States | 189 | 157 | 83% | |
| Other | 43 | 37 | 86% | |
| Gender | 0.5 | |||
| Male | 172 | 145 | 84% | |
| Female | 60 | 49 | 82% | |
| Race and ethniciity | 0.6 | |||
| White/Caucasian | 141 | 120 | 85% | |
| Asian | 64 | 53 | 83% | |
| Hispanic | 22 | 19 | 86% | |
| Other/unknown | 5 | 2 | 40% | |
| Age, years | 0.6 | |||
| < 45 | 92 | 74 | 80% | |
| 45 – 54 | 55 | 49 | 89% | |
| 55 – 64 | 71 | 60 | 84% | |
| ≥ 65 | 14 | 11 | 79% | |
| Years since dental degree, years | 0.5 | |||
| < 10 | 20 | 18 | 90% | |
| 10 – 19 | 91 | 73 | 80% | |
| 20 – 29 | 61 | 54 | 88% | |
| ≥ 30 | 59 | 49 | 83% | |
| Type of practice | 0.05 | |||
| Solo, private practice | 104 | 86 | 83% | |
| Owner, non-solo private practice | 48 | 39 | 81% | |
| Associate/employee private practice | 23 | 17 | 74% | |
| Preferred provider practice | 13 | 9 | 69% | |
| Academic | 43 | 42 | 98% | |
| Geographic Region of Practice | NE | |||
| West | 116 | 94 | 81% | |
| Midwest | 24 | 22 | 92% | |
| Southwest | 26 | 22 | 85% | |
| South Central | 5 | 5 | 100% | |
| South Atlantic | 29 | 27 | 93% | |
| Northeast | 32 | 24 | 75% | |
Percents are “row” %s, namely, the proportion of the “outcome” treatment (column heading) for that treatment comparison.
P-values are adjusted for clustering of patients within practitioners using generalized estimating equations
NE: Not estimable
Table 9.
Academic and non-academic practice settings vs. treatment success
| Academic practice | ALL | POSI = 0 |
P | OR = 10.4 | |
|---|---|---|---|---|---|
| N=231 | N=193 | % | |||
| Yes | 43 | 42 | 98% | 0.005 | |
| No | 188 | 151 | 80% | ||
| Primary treatment rendered |
|||||
| Academic practices | N=43 | N=42 | % | P | |
| Aligners only | 4 | 4 | 100% | NE | |
| Fixed, no TADs or surgery | 17 | 17 | 100% | ||
| TADs, no surgery | 9 | 8 | 89% | ||
| Surgery | 13 | 13 | 100% | ||
| Non-academic practices | N=188 | N=151 | % | P | |
| Aligners only | 22 | 17 | 77% | 0.4 | |
| Fixed, no TADs or surgery | 123 | 96 | 78% | ||
| TADs, no surgery | 10 | 9 | 90% | ||
| Surgery | 33 | 29 | 87% | ||
Percents are “row” %s, namely, the proportion of the “outcome” treatment (column heading) for that treatment comparison.
P-values are adjusted for clustering of patients within practitioners using generalized estimating equations
NE: Not estimable
Multivariable models were used to predict treatment success. Four separate models were developed to compare treatment groups (FA vs. ALN, TAD vs. FA, SX vs. FA, and SX vs. no-SX). The results from these predictive models are summarized in Table 10. The full models include all variables that had P<0.1, as well as three variables that were included in all models due to their clinical importance (treatment category, extractions, and initial overbite in mm). The reduced models only included the three variables mentioned above, as well as any variables that retained statistical significance. Academic practice setting was not included in the final model as only one patient had unsuccessful treatment. However, it should be stressed that treatment at academic centers was associated with the highest success rates.
Table 10.
Multivariable predictive models* for treatment success (pairwise comparisons) defined as POSI = 0 at end of active treatment.
| Fixed vs Aligners (N=167 [141 vs 26]**) |
TADs vs Fixed (N=160 [19 vs 141]**) |
||||
|---|---|---|---|---|---|
| OR | P | OR | P | ||
|
FULL |
FULL |
||||
| Fixed vs aligners | 1.3 | 0.6 | TADs vs fixed | 1.6 | 0.5 |
| Extract | 0.8 | 0.7 | Extract | 0.6 | 0.4 |
| No/mild crowding | 2.7 | 0.04 | No/mild crowding | 2.1 | 0.13 |
| Tx duration <30 months | 2.9 | 0.038 | Tx duration <30 months | 2.1 | 0.15 |
| MPSN (Base: <30 deg) | 3.4 | 0.14 | MPSN (Base: <30 deg) | 3.3 | 0.13 |
| OB(mm) (Base: continuous) | 1.14 | 0.2 | OB(mm) (Base: continuous) | 1.10 | 0.4 |
|
REDUCED |
REDUCED |
||||
| Fixed vs aligners | 1.3 | 0.6 | TADs vs fixed | 1.6 | 0.5 |
| Extract | 0.8 | 0.7 | Extract | 0.5 | 0.2 |
| No/mild crowding | 2.9 | 0.027 | MPSN (Base: <30 deg) | 4.1 | 0.046 |
| Tx duration <30 months | 3.0 | 0.036 | OB(mm) (Base: continuous) | 1.14 | 0.3 |
| OB(mm) (Base: continuous) | 1.12 | 0.3 | |||
| Surgery vs Fixed (N=187 [46 vs 141]**) |
Surgery vs No surgery (N=232 [46 vs 186]**) |
||||
| OR | P | OR | P | ||
|
FULL |
FULL |
||||
| Surgery vs fixed | 2.4 | 0.07 | Surgery vs no surgery | 2.2 | 0.10 |
| Extract | 0.9 | 0.8 | Extract | 0.8 | 0.7 |
| No/mild crowding | 2.3 | 0.06 | No/mild crowding | 2.6 | 0.02 |
| Tx duration <30 months | 2.1 | 0.2 | Tx duration <30 months | 2.6 | 0.035 |
| MPSN (Base: <30 deg) | 3.1 | 0.16 | MPSN (Base: <30 deg) | 4.1 | 0.039 |
| OB(mm) (Base: continuous) | 1.12 | 0.2 | OB(mm) (Base: continuous) | 1.10 | 0.3 |
|
REDUCED |
REDUCED |
||||
| Surgery vs fixed | 2.6 | 0.04 | No change - all retained | ||
| Extract | 0.8 | 0.7 | |||
| No/mild crowding | 2.5 | 0.04 | |||
| OB(mm) (Base: continuous) | 1.15 | 0.2 | |||
Treatment comparison of interest, whether extraction of tooth other than 3rd molar was performed, and baseline openbite measurement (OBmm) are included in models regardless of statistical significance. All characteristics with p<0.1 when adjusted only for clustering of patients within practice are entered in the full model. Characteristicsare removed until all remaining have P<0.1, with exceptions noted.
Numbers used in each model; numbers in brackets are for treatment comparison of interest.
The predictive model of treatment success comparing fixed appliances to aligners had two significant variables. Patients having no to mild pre-treatment crowding (OR=2.9; P=0.03) and patients with shorter treatment durations (<30 months) (OR=3.0; P=0.04) were more likely to have a successful treatment result.
In a model comparing TADs to fixed appliances only, treatment modality did not have a significant effect on success. The only variable that had a significantly higher level of success was pre-treatment MPSN <30° (OR=4.1; P=0.046).
The predictive model comparing surgery to fixed appliances had two significant factors. Surgical treatment was associated with higher success (OR=2.6; P=0.04), and those with no to mild pre-treatment crowding (OR=2.5; P=0.04) also had higher levels of success.
In a model comparing surgical patients to all other patients, three factors were significant. Patients with no to mild pre-treatment crowding (OR=2.6; P=0.02), those whose treatment duration was less than 30 months (OR=2.6; P=0.04), and those with a pre-treatment MPSN <30° (OR=4.1; P=0.04) had higher levels of success. Surgical treatment was associated with a trend toward more successful treatment (OR=2.2; P=0.10)
DISCUSSION
This study shows very high success rates for orthodontically treated adult AOB patients in the United States. At the end of treatment, 84% of the patient sample had positive vertical overlap of all four incisors, and 93% had positive overbite as measured using the central incisors on the post-treatment lateral cephalogram. Given the complexity and challenges commonly associated with treatment of AOB patients, these success rates are encouraging. However, experienced practitioners know the challenge will be the successful retention of these treatment results in the coming years.
While the small number of patients in the TAD and aligner groups hampered statistical analyses, there were some interesting findings about treatment modality. The success rates for patients treated with aligners and fixed appliances were the same (81%). This is consistent with findings from a retrospective study by Garnett, et al., reporting no differences in the magnitude of openbite and associated cephalometric changes between patients treated with fixed appliances versus clear aligners.11 The success rates in patients treated with TADs (89%) and orthognathic surgery (91%) were also similar. Kuroda, et al. found similar magnitudes of overbite correction when comparing patients treated with TADs and orthognathic surgery.7 The greater success in TADs and surgery might be related to the ability of these treatments to predictably change the vertical position of the molars, along with closure of the mandibular plane.21 With TADs, intrusion of both upper and lower molars is possible, and with surgery, impaction of the posterior maxilla effectively raises the vertical position of the molars.22,23
In the final models, which adjust for pre-treatment characteristics and other influencing factors, orthognathic surgery was the only treatment modality found to have a statistically significant higher rate of treatment success, compared to fixed appliances only. These findings are consistent with a systematic review published in 2011, reporting slightly higher treatment success and stability for surgical treatment of AOB malocclusions.16
In some cases, extractions are recommended for AOB treatment. Our results, showed no significant difference in treatment success between patients treated with and without extractions. In fact, the absolute success rates were lower in extraction patients. Janson, et al. showed no difference, but a similar trend, in final overbite measures for patients treated with and without extractions (1.09mm vs. 1.43 mm, respectively).12 In our sample, extractions were typically reserved for AOB patients with severe crowding and increased mandibular incisor proclination.20 In these cases, it is possible that the extraction spaces were primarily used to resolve crowding and reduce incisor proclination, and the “drawbridge” effect may not have been fully realized.
Although patient and practitioner demographic characteristics were not significant predictors of treatment success in our sample, practitioner practice type was found to have a significant influence on treatment success. Patients treated in an academic setting (N=42) had an 18% higher rate of treatment success that those treated in other practice settings (98% vs. 80%). TADs and surgery were used more often in academic settings, which might be associated with this finding. This may also be explained by the high clinical standards that accompany teaching institutions.
The predictive models for treatment success identified three additional variables that exhibited statistically significant relationships to treatment success: pre-treatment mandibular plane angle, pre-treatment crowding and treatment duration.
Patients with pre-treatment mandibular plane angles (MPSN) less than 30 degrees had a greater chance for treatment success than those with steeper mandibular plane angles. It is possible that the patients with lower mandibular plane angles had openbites that were more dental in nature. Conversely, the patients with steeper mandibular plane angles may have had openbites that were more skeletal in nature. It is interesting to note that the mean mandibular plane angle was highest in the patients who were recommended orthognathic surgery. However, even though surgery was recommended to 37% of our subjects, only 21% of the patients who provided end-of-treatment data had undergone surgery.
Pre-treatment crowding was a significant variable in three predictive models for treatment success. Ninety-four patients were categorized as having moderate to severe crowding, but only 45 subjects underwent extractions other than third molars. Thus, almost half of the patients with moderate to severe crowding were treated non-extraction. Typically, resolution of moderate to severe crowding when no extractions are performed will result in forward tipping of the incisors, which is associated with further worsening of the openbite. Patients with no crowding or mild crowding would be less affected by this issue.
Treatment duration was also found to be a significant predictor of success in patients treated with fixed appliances and patients treated with aligners. Patients with treatment less than 30 months had a 15–20% higher rate of treatment success. This is consistent with the relationship between treatment complexity and duration frequently observed. More complex treatments often require more time and yield less predictable results, which may explain this finding. It may also reflect changes to treatment plans or patients expectations when treatment is not progressing as expected. It is important to consider that shorter treatment duration may also be associated with other factors, such as patient compliance, oral habits, and practitioner proficiency. None of these were controlled for in this study. Interestingly, this relationship was not observed in the models comparing TADs or surgery to fixed appliances. This may be explained by greater predictability and success rates of TAD and surgery treatments observed in our study. These treatment modalities also do not rely on compliance as much as aligner therapy does, which is a large contributing factor to length of treatment.
AOBs of greater magnitude are considered more challenging malocclusions to treat, and are often thought of being associated with lower success rates. Interestingly, initial AOB severity, classified by pre-treatment cephalometric overbite, was not a significant predictor of treatment success in any of the final models. Several factors might have influenced this finding. First, it is possible that practitioners particularly interested and skilled in openbite treatment enrolled in the study, and their clinical expertise resulted in high success rates, regardless of the initial severity. Related to this, practitioners were not limited to one specific treatment modality, and could recommend the treatment they thought was most appropriate. In fact, surgery was recommended to 37% of the subjects. Thus, it is possible that more robust techniques were appropriately recommended to patients with more severe openbites. Another factor may have been the effect of participating in a study, which may have influenced the practitioner’s attention to the case, as well as the patient’s cooperation with treatment. Finally, practitioners were allowed to change treatment plans, and if treatment was not progressing well with one treatment, additional treatments could be recommended. We plan to evaluate whether severity of the initial overbite may be a factor if we only look at one treatment modality, for example fixed appliances only. Also, it will be interesting to assess the relationship between initial severity and stability in the follow-up stage of the study.
LIMITATIONS
There were several limitations of our study. The patient and practitioner sample was not randomly selected. The practitioners were recruited from the National Dental PBRN and their participation was voluntary. However, other than a greater number of practitioners in an academic setting, the sample was demographically similar to the AAO membership. Practitioners were asked to enroll all patients who met the study’s inclusion criteria to minimize patient selection bias. Another limitation was treatment was not randomized. Practitioners selected the method of treatment for each patient. This resulted in an uneven distribution of patients in treatment groups as well as a clustering effect with treatment and proficiency biases. The treatment group sample sizes varied significantly. The small numbers of patients in the ALN and TAD groups reduced the power of our statistical analyses. The treatment timeline constraints may have resulted in a biased patient sample consisting of fewer unsuccessfully treated patients. End of active treatment data was not received from 93 subjects who either submitted incomplete data (6), withdrew from the study (24), or did not complete treatment in the study period (63). The patients who did not complete treatment may have been more difficult cases with a lower chance for success. However, baseline characteristics of patients with end-of-active treatment data (N= 254) and patients missing end of active treatment data (N=93) were compared. There was no difference in mean pre-treatment overbite or recommended treatment modality. Although not statistically significant, there was a trend of higher POSI scores for patients missing end-of-active-treatment data. There was a significant difference in the estimated treatment time, with patients completing treatment having shorter estimated treatment times (Appendix, Table 1). An additional source of bias could arise from preferential levels of treatment being provided to patients that practitioners judged to be more likely to have favorable outcomes. While we do not have any evidence that practitioners displayed this type of bias, we have no way to assess this.
CONCLUSIONS
Overall success rates were very high for adult patients receiving orthodontic treatment for anterior openbite malocclusions. While there was a range of success for the major treatment modalities, orthognathic surgery was the only treatment group exhibiting a statistically significant influence on success rates. There were no statistically significant associations between patient or practitioner demographics and treatment success. Several pre-treatment dentofacial characteristics, including pre-treatment mandibular plane angle and amount of crowding, academic practice setting, and treatment duration were significant predictors of treatment success in adult anterior openbite patients.
Supplementary Material
ACKNOWLEDGEMENTS
This study was funded by NIDCR grant U19-DE-28717 and U19-DE-22516. Opinions and assertions contained herein are those of the authors and are not to be construed as necessarily representing the views of the respective organizations or the National Institutes of Health. The informed consent of all human subjects who participated in this investigation was obtained after the nature of the procedures had been explained fully. An Internet site devoted to details about the nation’s network is located at http://NationalDentalPBRN.org and is conducted under the auspices of the National Dental Practice-Based Research Network. We gratefully acknowledge all the practitioners and patients who made this study possible. We are also grateful to the network’s regional coordinators, Sarah Basile, RDH, MPH, Chris Enstad, BS, and Hannah Van Lith, BA (Midwest); Stephanie Hodge, MA, and Kim Stewart (Western); Pat Ragusa (Northeast); Deborah McEdward, RDH, BS, CCRP, and Danny Johnson (South Atlantic); Claudia Carcelèn, MPH, Shermetria Massingale, MPH, CHES, and Ellen Sowell, BA (South Central); Stephanie Reyes, BA, Meredith Buchberg, MPH, and Monica Castillo, BA (Southwest). We also thank Kavya Vellala and the Westat Coordinating Center staff, the American Association of Orthodontists (AAO), Jackie Hittner (AAO Librarian), Gregg Gilbert, DDS, MBA (National Network Director), and Dena Fischer, DDS, MSD, MS (NIDCR Program Director).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Lauren S. Todoki, Private Practice, Seattle, Washington.
Samuel A. Finkleman, Private Practice, Seattle, Washington.
Ellen Funkhouser, Division of Preventive Medicine School of Medicine, University of Alabama, Birmingham.
Geoffrey M. Greenlee, Department of Orthodontics, University of Washington, Seattle.
Kelly W. Choi, Private Practice, Santa Rosa, California.
Hsiu-Ching Ko, Department of Orthodontics University of Washington, Seattle.
Hsuan-Fang Wang, Department of Orthodontics, University of Washington, Seattle; Attending Physician, Division of Orthodontics, Department of Dentistry, Far Eastern Memorial Hospital, Taipei, Taiwan.
Peter A. Shapiro, Department of Orthodontics, University of Washington, Seattle.
Rooz Khosravi, Department of Orthodontics, University of Washington, Seattle.
Camille Baltuck, Western Region, National Dental Practice-Based Research Network.
Veerasathpurush Allareddy, Department of Orthodontics, UIC, Director of the Specialty Node of National Dental Practice-Based Research Network.
Calogero Dolce, Department of Orthodontics, UF.
Chung How Kau, Department of Orthodontics, UAB.
Kyungsup Shin, Department of Orthodontics, University of Iowa.
Jaime de Jesus-Vinas, Private practice, San Juan, Puerto Rico.
Michael Vermette, Private Practice, Concord, New Hampshire.
Cameron Jolley, Private practice, Trophy Club, TX.
National Dental Practice-Based Research Network Collaborative Group, The National Dental PBRN Collaborative Group comprises practitioners, faculty, and staff investigators who contributed to this network activity. A list of these persons are at http://www.nationaldentalpbrn.org/collaborative-group.php.
Greg J. Huang, Department of Orthodontics, University of Washington, Seattle.
REFERENCES
- 1.Kelly JE, Sanchez M, Van Kirk LE. An Assessment of the Occlusion of the Teeth of Children 6–11Years, United States. Vital Health Stat 11 1973:1–60. [PubMed] [Google Scholar]
- 2.Leavy KM, Cisneros GJ, LeBlanc EM. Malocclusion and its relationship to speech sound production: Redefining the effect of malocclusal traits on sound production. Am J Orthod Dentofacial Orthop 2016;150:116–123. [DOI] [PubMed] [Google Scholar]
- 3.Subtelny JD, Sakuda M. Open-bite: Diagnosis and treatment. Am J Orthod 1964;50:337–358. [Google Scholar]
- 4.Choi KW, Ko HC, Todoki LS, Finkleman SA, Khosravi R, Wang HF et al. The National Dental Practice-Based Research Network adult anterior open bite study: A description of the practitioners and patients. Angle Orthod 2018;88:675–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fontes AM, Joondeph DR, Bloomquist DS, Greenlee GM, Wallen TR, Huang GJ. Long-term stability of anterior open-bite closure with bilateral sagittal split osteotomy. Am J Orthod Dentofacial Orthop 2012;142:792–800. [DOI] [PubMed] [Google Scholar]
- 6.Nanda R. Biomechanics and esthetic strategies in clinical orthodontics. St. Louis, Mo.: Elsevier Saunders; 2005. [Google Scholar]
- 7.Kuroda S, Sakai Y, Tamamura N, Deguchi T, Takano-Yamamoto T. Treatment of severe anterior open bite with skeletal anchorage in adults: comparison with orthognathic surgery outcomes. Am J Orthod Dentofacial Orthop 2007;132:599–605. [DOI] [PubMed] [Google Scholar]
- 8.Schupp W, Haubrich J, Neumann I. Treatment of anterior open bite with the Invisalign system. J Clin Orthod 2010;44:501–507. [PubMed] [Google Scholar]
- 9.Guarneri MP, Oliverio T, Silvestre I, Lombardo L, Siciliani G. Open bite treatment using clear aligners. Angle Orthod 2013;83:913–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khosravi R, Cohanim B, Hujoel P, Daher S, Neal M, Liu W et al. Management of overbite with the Invisalign appliance. Am J Orthod Dentofacial Orthop 2017;151:691–699.e692. [DOI] [PubMed] [Google Scholar]
- 11.Garnett BS, Mahood K, Nguyen M, Al-Khateeb A, Liu S, Boyd R et al. Cephalometric comparison of adult anterior open bite treatment using clear aligners and fixed appliances. Angle Orthod 2019;89:3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Janson G, Valarelli FP, Beltrao RT, de Freitas MR, Henriques JF. Stability of anterior open-bite extraction and nonextraction treatment in the permanent dentition. Am J Orthod Dentofacial Orthop 2006;129:768–774. [DOI] [PubMed] [Google Scholar]
- 13.Beane RA Jr. Nonsurgical management of the anterior open bite: a review of the options. Semin Orthod 1999;5:275–283. [DOI] [PubMed] [Google Scholar]
- 14.Aras A Vertical changes following orthodontic extraction treatment in skeletal open bite subjects. Eur J Orthod 2002;24:407–416. [DOI] [PubMed] [Google Scholar]
- 15.Huang GJ. Long-term stability of anterior open-bitetherapy: A review. Seminars in Orthodontics 2002;8:162–172. [Google Scholar]
- 16.Greenlee GM, Huang GJ, Chen SS, Chen J, Koepsell T, Hujoel P. Stability of treatment for anterior open-bite malocclusion: a meta-analysis. Am J Orthod Dentofacial Orthop 2011;139:154–169. [DOI] [PubMed] [Google Scholar]
- 17.Scheideman GB, Bell WH, Legan HL, Finn RA, Reisch JS. Cephalometric analysis of dentofacial normals. Am. J Orthod 1980;78:404–420. [DOI] [PubMed] [Google Scholar]
- 18.Riolo MW, Moyers RE, McNamara JA, Hunter WS. An atlas of craniofacial growth, monograph No. 2, Craniofacial Growth Series. University of Michigan: Ann Arbor Press; 1974 [Google Scholar]
- 19.Fields HW, Proffit WR, Nixon WL, Phillips C, Stanek E. Facial pattern and differences in long faced children and adults. Am J Orthod 1984; 85(3): 217–223. [DOI] [PubMed] [Google Scholar]
- 20.Huang GJ, Baltuck C, Funkhouser E, Wang H-F, Todoki LS, Finkleman SA et al. The National Dental PBRN Adult Anterior Openbite Study: Treatment Recommendations and Their Association with Patient and Practitioner Characteristics; Am J Orthod Dentofacial Orthop 2019;156:312–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alsafadi AS, Alabdullah MM, Saltaji H, Abdo A, Youssef M. Effect of molar intrusion with temporary anchorage devices in patients with anterior open bite: a systematic review. Prog Orthod 2016;17:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cousley RRJ. Molar intrusion in the management of anterior openbite and ‘high angle’ Class II malocclusions. Journal of orthodontics. 2014;41 Suppl 1:S39–S46. [DOI] [PubMed] [Google Scholar]
- 23.Bailey LJ, Phillips C, Proffit WR, Turvey TA. Stability following superior repositioning of the maxilla by Le Fort I osteotomy: five-year follow-up. Int J Adult Orthodon Orthognath Surg 1994;9:163–173. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


