Abstract
Background:
The association between drug use and condomless anal sex (CAS) is well documented among sexual minority men (SMM). Less is known about whether this association generalizes to marijuana and across relationship status and sexual agreements groups (single, partnered monogamous, partnered open –outside partners permitted, and partnered monogamish –outside partners permitted when main partners are together).
Methods:
A nationwide sample of SMM (N = 65,707) were recruited through a geosocial networking app between November, 2017 and November, 2019. Participants reported on drug use and instances of CAS with casual partners in the previous 30 days.
Results:
Both marijuana and club drug use were associated with the occurrence of CAS with casual partners among single men. Only club drug use was associated with CAS frequency in this group. The association between marijuana and the occurrence of CAS was equivalent among monogamous men, while the associations between club drug use and the occurrence as well as frequency of CAS were significantly weaker. Meanwhile, the associations between club drug use and the occurrence as well as frequency of CAS did not differ significantly between single and non-monogamous (open and monogamish) subgroups; however, the association between marijuana and the occurrence of CAS was significantly weaker.
Conclusions:
Findings largely replicated the robust association between club drug use and CAS with casual partners. They support the assertion that marijuana use predicts sexual risk for some SMM subgroups. Finally, they illustrate the potential for relationship status – and sexual agreements – to contextualize associations between drug use and CAS.
Keywords: same-sex male couples, sexual minority men, HIV, drug use
1.0. INTRODUCTION
Sexual minority men (SMM) accounted for over two-thirds of all new HIV diagnoses in the United States in 2018, despite only accounting for 2% of the population (Centers for Disease Control and Prevention, 2018). While a substantial body of research on HIV risk has focused predominantly on sexual transmission risk behaviors such as condomless anal sex (CAS) with casual partners among single SMM, the past decade has seen increasing attention directed towards HIV transmission risk in the context of relationships. This shift is grounded in epidemiological research indicating that main partner transmissions account one to two-thirds of all new HIV infections (Goodreau et al., 2012; Sullivan et al., 2009).
Extensive research has shown that SMM who use drugs are more likely to engage in CAS with casual partners, which increases their risk of HIV acquisition or transmission (Rendina et al., 2015; Theodore et al., 2014). The purpose of the current study is to address two contextual issues in this area of research. First, despite being consistently reported among the drugs most commonly used during sex (Centers for Disease Control and Prevention, 2016), links between marijuana use and CAS with casual partners are less well studied than other substances. Second, the agreements male couples form about sex with outside partners predict both drug use and sexual behavior (Mitchell, 2016; Mitchell et al., 2014; Parsons, Starks, et al., 2013; Starks, Robles, et al., 2019); however, no study has directly tested whether relationship status and sexual agreements moderate the association between drug use and CAS.
Available evidence suggests that partnered SMM use drugs during sex at rates potentially approaching those observed among single SMM. Thirty-one percent of SMM report using drugs (e.g., marijuana, cocaine and crack, and amphetamines) during sex (Centers for Disease Control and Prevention, 2016). Among partnered SMM, rates of drug use during sex between main partners varied between 12.5% (for club drugs) and 33% (for marijuana) (Mitchell, 2016). Meanwhile, the use of drugs specifically during sex with outside partners varied between 10.6% (for club drugs) and 31% (for marijuana) (Mitchell et al., 2016; Parsons & Starks, 2014).
While both partnered and single SMM consistently identify marijuana among the drugs most commonly combined with sex, there is little data evaluating the relationship between marijuana and CAS with casual partners. Much of the research on drug use and CAS with casual partners has been primarily concerned with “club drugs” (e.g., cocaine, methamphetamine, GHB, ketamine, LSD and ecstasy) (Theodore et al., 2014; Vosburgh et al., 2012). There is at least some evidence that marijuana may be associated with increased sexual risk taking as well. While some findings are equivocal (Carey et al., 2008; Hendershot et al., 2010), others have found that partnered SMM who use drugs – inclusive of marijuana – during sex are more likely to engage in CAS with casual partners (Mitchell et al., 2016; Parsons & Starks, 2014). Furthermore, poly-substance use – inclusive of marijuana – contributes to the prediction of lapses in HIV prevention communication between main partners (Starks et al., 2016).
Despite the abundance of research linking drug use and CAS with casual partners, no studies have tested whether this association is moderated by relationship status. This gap in the literature is important because research from the past decade has indicated that sexual agreements – the rules or boundaries couples establish related to sex with partners outside their relationship – are a consistent predictor of sexual behavior with casual partners and drug use. Men in relationships in which explicit agreements around monogamy have been formed – where sex with casual partners is prohibited – are less likely to have sex with casual partners compared to those in non-monogamous relationships (Parsons, Starks, et al., 2013; Spicer et al., 2019; Starks, Robles, et al., 2019). They are also less likely to use club drugs and marijuana compared to those in non-monogamous relationships (Mitchell et al., 2013; Parsons & Starks, 2014). There is some evidence that monogamish agreements – a specific subtype of non-monogamy in which sex with casual partners is limited to instances where both main partners are present – predict higher rates of marijuana use compared to both monogamous and non-monogamous agreements that permit main partners to have sex with casual partners independently (Starks, Robles, et al., 2019).
To date, no studies have specifically evaluated the association between marijuana use and CAS above and beyond club drug use. In addition, no studies have tested whether associations between drug use and CAS are equivalent across single and partnered men – accounting for sexual agreements among those men in relationships. The purpose of the current study was to address these gaps. This study has two specific objectives. First we evaluated the contributions of marijuana and club drug use to models predicting CAS with casual partners. Second, we tested whether relationship status moderated the associations between drug use and CAS with casual partners. We utilized hurdle models in order to simultaneously predict the occurrence of CAS with casual partners as well as the frequency of CAS with casual partners among SMM reporting at least one instance.
2.0. METHODS
2.1. Participants
Eligible participants were aged 18 or older and identified as cis-male. In addition, SMM who indicated that they had a main partner were included if they indicated that their partner was also cis-male and aged 18 or older. All participants reported a residence within the United States and were able to communicate in English.
2.2. Procedures
Data were drawn from a large screening survey intended to determine eligibility for a portfolio of U.S. based studies focused on sexual health and substance use among SMM. Participants were recruited through a popular geosocial networking app for gay, bi, trans, and queer people seeking out sexual partners. Interested participants who clicked on the ad advanced to the survey landing page that included consent information. Participants who wished to complete the survey indicated their consent electronically and advanced into the survey. The survey took approximately 10 minutes to complete. No compensation was provided. All procedures were approved by the Institutional Review Board of Hunter College of the City University of New York.
2.3. Measures
2.3.1. Demographic covariates.
age, race, ethnicity, zip code, sexual identity/orientation, HIV status, and current PrEP use. Zip codes were used to determine region. SMM with main partners also provided data about relationship length and main partner demographics (i.e., gender, age and HIV status).
2.3.2. Relationship status and sexual agreement.
Participants were asked, “As of today, do you have a main partner?” Those who responded “no” were categorized as single. Those who reported a main partner were asked to indicate their sexual agreement. A categorical relationship status variable was created to distinguish between single men and partnered men who were monogamous versus non-monogamous (open or “monogamish”).
2.3.3. Drug use.
Participants indicated whether or not they used each of 11 drugs in the past 90 days. Data on crack, cocaine, ecstasy/MDMA, GHB/GBL, ketamine, and methamphetamine/”tina” were aggregated to create a single dichotomous indicator of club drug use. Marijuana use was summarized separately with a dichotomous indicator. These variables were then used to create a 4 category variable distinguishing among participants who reported neither marijuana or club drug use, marijuana use only, club drug use only, and both marijuana and club drug use.
2.3.4. Condomless anal sex.
Participants also indicated the number of times (in the previous 90) days they engaged in CAS with a casual partner (not their main partner). A small proportion of the sample (0.8%) provided responses greater than 100. To limit the influence of extreme values, these were reassigned values equal to 100.
2.4. Analytic Plan
Hurdle models were calculated using the hurdle function included in the pscl package in R. Hurdle models contain a binary logit component that models the likelihood of reporting at least one instance of CAS with casual partners and a negative binomial component modeling the frequency of CAS with casual partners among those who report at least one instance (Hu et al., 2011). In the binary component of the hurdle model, regression coefficients are presented as Odds Ratios (OR) and represent the association between the predictor and the odds of any CAS with casual partners. In the count portion of the model, regression coefficients are presented as Rate Ratios (RR) and represent the association between the predictor and the amount (or frequency) of CAS with casual partners among those who reported at least on instance.
Covariates included for both components of the model were race and ethnicity (African-American, Asian, Latino, Other, White), region (Northeast, Midwest, South, West), a variable describing HIV and PrEP uptake (HIV-positive, HIV-negative/unknown without PrEP, HIV-negative on PrEP), sexual orientation/identity (gay, bisexual, other), relationship agreement (single, monogamous, monogamish, open), and a variable describing marijuana and club drug use (neither, marijuana only, club drug only, both). Models included interaction terms between the relationship agreements and drug use.
Models were initially calculated in the full sample including both single and partnered SMM. Models were subsequently calculated restricting the sample only to partnered men. This permitted an evaluation of the sensitivity of findings to the inclusion of main partner characteristics (i.e., age, HIV status, relationship duration) as covariates.
3.0. RESULTS
Between November 2017 and November 2019, 65,707 cis-gender SMM over the age of 18 responded to the survey. Table 1 contains sample demographic data. Participants’ average age was 36.3 years (SD = 12.0). The majority were White (54.9%), in a relationship (82.1%), identified as gay (85.2%), and indicated an HIV negative (79.4%) serostatus. HIV negative men on PrEP comprised 18.2% of the sample.
Table 1.
Demographic characteristics
| Total | Single | Monogamous | Monogamish | Open | ||
|---|---|---|---|---|---|---|
| Single, Partnered | n (%) | n (%) | n (%) | n (%) | n (%) | X2 |
| n | 65707 | 11773 (17.9) | 13298 (20.2) | 5493 (8.4) | 35143 (53.5) | |
| Race/Ethnicity | 1727.0** | |||||
| African-Am | 7602 (11.6) | 1884 (16.0) | 2332 (17.5) | 457 (8.3) | 2929 (8.3) | 1105.1** |
| Asian | 3050 (4.6) | 577 (4.9) | 594 (4.5) | 144 (2.6) | 1735 (4.9) | 60.3** |
| Latino | 11652 (17.7) | 2317 (19.7) | 2700 (20.3) | 886 (16.1) | 5749 (16.4) | 146.0** |
| White | 36087 (54.9) | 5520 (46.9) | 6123 (46.0) | 3410 (62.1) | 21034 (59.9) | 1189.0** |
| Other | 7316 (11.1) | 1475 (12.5) | 1549 (11.6) | 596 (10.9) | 3696 (10.5) | 40.7** |
| Region | 418.7** | |||||
| Northeast | 13949 (21.2) | 2285 (19.4) | 2579 (19.4) | 1023 (18.6) | 8062 (22.9) | 134.0** |
| Midwest | 11348 (17.3) | 1989 (16.9) | 2499 (18.8) | 1002 (18.2) | 5858 (16.7) | 35.2** |
| South | 22789 (34.7) | 4145 (35.2) | 5204 (39.1) | 2102 (38.3) | 11338 (32.3) | 239.7** |
| West | 17621 (26.8) | 3354 (28.5) | 3016 (22.7) | 1366 (24.9) | 9885 (28.1) | 174.1** |
| Sexual Orientation | 858.8** | |||||
| Gay | 55995 (85.2) | 9117 (77.4) | 11378 (85.6) | 4877 (88.8) | 30623 (87.1) | 725.1** |
| Bisexual | 8199 (12.5) | 2351 (20.0) | 1699 (12.8) | 531 (9.7) | 3618 (10.3) | 799.2** |
| Other | 1513 (2.3) | 305 (2.6) | 221 (1.7) | 85 (1.5) | 902 (2.6) | 53.4** |
| PrEP, HIV | 1772.2** | |||||
| Positive | 13531 (20.6) | 2536 (21.5) | 2627 (19.8) | 1086 (19.8) | 7282 (20.7) | 14.8* |
| Neg/Unk, no Rx | 40225 (61.2) | 7245 (61.5) | 9694 (72.9) | 3498 (63.7) | 19788 (56.3) | 1135.7** |
| Neg, PrEP Rx | 11951 (18.2) | 1992 (16.9) | 977 (7.3) | 909 (16.5) | 8073 (23.0) | 1613.4** |
| SU, past 90 days | 545.6** | |||||
| no MJ no CD | 32614 (49.6) | 4904 (41.7) | 7841 (59.0) | 2484 (45.2) | 17385 (49.5) | 806.1** |
| MJ no CD | 19079 (29.0) | 3681 (31.3) | 3796 (28.5) | 1701 (31.0) | 9901 (28.2) | 52.6** |
| CD no MJ | 4209 (6.4) | 855 (7.3) | 485 (3.6) | 439 (8.0) | 2430 (6.9) | 221.4** |
| MJ & CD | 9805 (14.9) | 2333 (19.8) | 1176 (8.8) | 869 (15.8) | 5427 (15.4) | 620.2** |
| M(SD) | M(SD) | M(SD) | M(SD) | M(SD) | ||
| Age | 36.3 (12.0) | 33.3 (11.5) | 33.1 (11.3) | 36.4 (11.3) | 38.4 (12.1) | 951.0* |
| CAS with CP | 7.5 (15.5) | 8.3 (15.5) | 4.8 (15.2) | 5.5 (12.9) | 8.5 (15.7) | 227.0* |
| Partnered Only | n (%) | n (%) | n (%) | n (%) | ||
| n | 53934 | NA | 13298 (24.7) | 5493 (10.2) | 35143 (65.2) | |
| MP HIV Status | 84.6** | |||||
| Negative | 41685 (77.3) | NA | 10317 (77.6) | 4270 (77.7) | 27098 (77.1) | 1.9 |
| Positive | 9968 (18.5) | NA | 2288 (17.2) | 1081 (19.7) | 6599 (18.8) | 21.6** |
| Unknown | 2281 (4.2) | NA | 693 (5.2) | 142 (2.6) | 1446 (4.1) | 69.5** |
| Relationship Duration | 3362.4** | |||||
| ≤ 2YR | 21054 (39.0) | NA | 8020 (60.3) | 1679 (30.6) | 11355 (32.3) | |
| > 2YR | 32880 (61.0) | NA | 5278 (39.7) | 3814 (69.4) | 23788 (67.7) | |
| M(SD) | M(SD) | M(SD) | M(SD) | |||
| MP Age | 36.9 (12.0) | NA | 33.0 (11.1) | 36.2 (11.3) | 38.6 (12.5) | 1047.5* |
p < 0.05
p < 0.01
CD – club drugs
Mish – monogamish; those that endorsed “both of us have sex w/others, but only together”
Mono – monogamous
MJ – marijuana
MP – main partner
Open – those not having monogamous or monogamish relationship agreements
Ref – referent
Rel Len – relationship length
The available sample size yielded considerable power. Mean power across predictive variables was calculated through simulations using R. Average power across parameters indicated that the sample of this size has power exceeding .95 to reject a null hypothesis.
3.1. Drug use and CAS: Models comparing single and partnered SMM
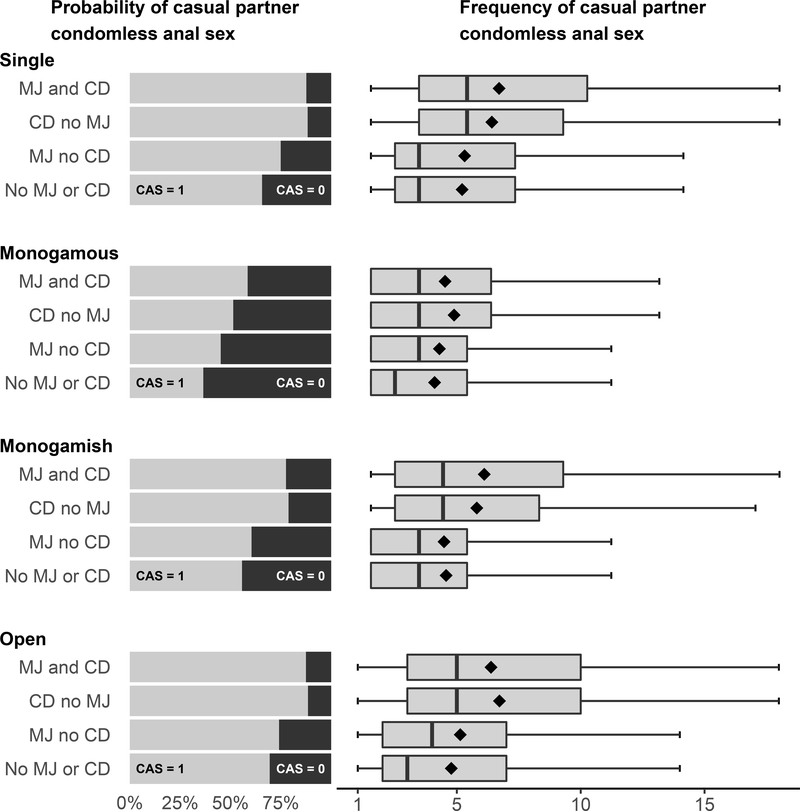
Table 2 contains the results of hurdle models calculated in the full sample (including single and partnered SMM). Figure 1 contains visualizations of both the binary and count portions of the hurdle model. Bar charts in the left column depict the probability of CAS for each drug use category across all relationship status and sexual agreement groups. Likewise, corresponding box plots in the right column depict the frequency of CAS with casual partners (among those who indicated at least 1 instance) for each drug use category across all relationship status and sexual agreement groups.
Table 2.
Hurdle model predicting CAS with Casual Partners Full Sample (n = 65,707)
| Any CAS with Casual Partners (Binomial) | Frequency of CAS with Casual Partners (Count) | |||
|---|---|---|---|---|
| Odds Ratio | 95% CI | Rate Ratio | 95% CI | |
| Age | 0.986** | (0.985, 0.988) | 1.001 | (0.999, 1.003) |
| Race/Ethnicity (ref = White) | ||||
| African-American | 0.90** | (0.85, 0.96) | 0.72** | (0.67, 0.77) |
| Asian | 0.64** | (0.60, 0.70) | 0.64** | (0.58, 0.72) |
| Latino | 0.91** | (0.87, 0.96) | 0.81** | (0.77, 0.86) |
| Other | 0.98 | (0.92, 1.04) | 1.03 | (0.97, 1.10) |
| Region (ref = Northeast) | ||||
| Midwest | 1.19** | (1.12, 1.25) | 1.00 | (0.94, 1.06) |
| South | 1.19** | (1.13, 1.24) | 1.01 | (0.95, 1.06) |
| West | 1.19** | (1.13, 1.25) | 1.07* | (1.01, 1.13) |
| PrEP, HIV (ref = Negative/Unknown, without PrEP) | ||||
| HIV positive | 1.90** | (1.81, 1.99) | 1.75** | (1.68, 1.84) |
| Current PrEP prescription | 2.86** | (2.72, 3.03) | 1.84** | (1.76, 1.93) |
| Sexual Orientation (ref = Gay) | ||||
| Bisexual | 1.06* | (1.01, 1.13) | 1.09** | (1.02, 1.16) |
| Other | 0.79** | (0.70, 0.89) | 1.12 | (0.98, 1.27) |
| Relationship Status (ref = Single) | ||||
| Monogamous | 0.31** | (0.29, 0.34) | 1.63** | (1.46, 1.83) |
| Monogamish | 0.67** | (0.61, 0.74) | 0.77** | (0.67, 0.89) |
| Open | 1.22** | (1.14, 1.31) | 0.99 | (0.91, 1.07) |
| Substance Use (ref no MJ, no CD) | ||||
| MJ no CD | 1.48** | (1.34, 1.63) | 1.07 | (0.96, 1.19) |
| CD no MJ | 3.63** | (2.91, 4.51) | 2.32** | (2.02, 2.64) |
| MJ and CD | 3.35** | (2.92, 3.85) | 2.05** | (1.86, 2.28) |
| Interactions | ||||
| Monogamous*MJ no CD | 0.91 | (0.81, 1.04) | 1.03 | (0.86, 1.23) |
| Monogamous*CD no MJ | 0.48** | (0.36, 0.65) | 0.51** | (0.37, 0.70) |
| Monogamous*MJ & CD | 0.66** | (0.55, 0.80) | 0.55** | (0.45, 0.68) |
| Monogamish*MJ no CD | 0.77** | (0.66, 0.91) | 1.06 | (0.84, 1.33) |
| Monogamish*CD no MJ | 0.73 | (0.52, 1.00) | 0.77 | (0.59, 1.00) |
| Monogamish*MJ & CD | 0.73** | (0.58, 0.91) | 0.94 | (0.76, 1.17) |
| Open*MJ no CD | 0.79** | (0.70, 0.88) | 1.04 | (0.92, 1.18) |
| Open*CD no MJ | 0.83 | (0.64, 1.07) | 0.94 | (0.81, 1.09) |
| Open*MJ & CD | 0.79** | (0.67, 0.92) | 0.99 | (0.88, 1.11) |
p ≤ .05
p ≤ .01
NOTE: MJ = Marijuana; CD = Club Drug; CAS = Condomless anal sex
Figure 1.
The occurrence and frequency of CAS with casual partners: associations with drug use across relationship status groups
NOTE: MJ = Marijuana; CD = Club Drugs
Results of the binary component of the hurdle model indicated that, among men who did not use marijuana or club drugs, those in monogamous (OR = 0.31; 95%CI: 0.29, 0.34) and monogamish (OR = 0.67; 95%CI = 0.61, 0.74) relationships were significantly less likely to report any CAS with casual partners compared to single men, while those in open relationships were significantly more likely (OR = 1.22; 95% CI: 1.14, 1.31). Those who reported marijuana use alone (OR = 1.48; 95% CI: 1.34, 1.63), club drug use alone (OR = 3.63; 95% CI: 2.91, 4.51), and both marijuana and club drug use (OR = 3.35; 95% CI: 2.92, 3.85) were all more likely to report at least one instance of CAS than those who reported no use. In addition, rotation of the referent category revealed that men who reported club drug use, alone and combined with marijuana, were significantly more likely to report at least one instance of CAS than those who reported marijuana use only (OR =2.46, 95% CI:1.95, 3.06; p < 0.01 and OR = 2.27; 95% CI: 1.95, 2.61; p < 0.01, respectively).
These latter coefficients serve to illustrate how much larger the effect size associated with club drug use is compared to marijuana use. The odds of CAS with a casual partner was more than twice as large among subgroups reporting club drug use compared to those who reported marijuana alone. While OR’s are an unstandardized measure of effect size, the relative magnitude of marijuana and club drug use associations with the logistic outcome can be directly compared in these analyses because dummy codes place both variables on a 0 (no use) versus 1 (use) scale (Martin, 2020). It is therefore noteworthy to observe that the OR associated with club drug use (alone and in conjunction with marijuana) among single men is more than twice as large as the OR associated with marijuana use alone. While the use of marijuana alone was associated with a 48% increase in the odds of CAS with a casual partner among single men, the use of club drugs (alone and in conjunction with marijuana) was associated with increases in the odds of CAS with a casual partner that exceeded 300%.
Examination of interaction terms indicated that the association between marijuana use and the occurrence of CAS with casual partners among monogamous men did not differ significantly from that observed among single men. Meanwhile, the association between club drug use and CAS with casual partners, alone (OR = 0.48, 95%CI = 0.36, 0.65) and combined with marijuana (OR = 0.66, 95%CI: 0.55, 0.80), was significantly weaker among monogamous men compared to those who were single. The reverse pattern was observed in both non-monogamous subgroups. Among monogamish and open men, the association between club drug use and the occurrence of CAS with casual partners did not differ significant from that observed among single men; however, the associations between marijuana use, alone and combined with club drug use, and CAS were significantly weaker (OR = 0.77, 95%CI: 0.66, 0.91 and OR = 0.73, 95%CI: 0.58, 0.91 for monogamish men respectively and OR = 0.79, 95%CI: 0.70, 0.88 and OR = 0.79, 95%CI: 0.67, 0.92 for open men respectively).
With respect to demographic covariates, odds of engaging in at least one instance of CAS with a casual partner decreased with age (OR = 0.986; 95%CI: 0.985, 0.988). African-American (OR = 0.90; 95%CI: 0.85, 0.96), Latino (OR = 0.91; 95%CI: 0.87, 0.96) and Asian men (OR = 0.64; 95%CI: 0.60, 0.70) were less likely to report CAS with a casual partner than White respondents, while those living in the Midwest (OR = 1.19; 95%CI: 1.12, 1.25), South (OR = 1.19; 95%CI: 1.13, 1.24), and West (OR = 1.19; 95%CI: 1.13, 1.25) were more likely than from the Northeast to report at least one instance of CAS with a casual partner. HIV-positive respondents (OR = 1.90; 95%CI: 1.81, 1.99) and HIV-negative respondents with a PrEP prescription (OR = 2.86; 95%CI: 2.72, 3.03) were more likely to report CAS with casual partners than HIV-negative/unknown respondents without PrEP prescriptions to report CAS with a casual partner than those without. Bisexual respondents were more likely than gay respondents to report any CAS with casual partners (OR = 1.06; 95%CI: 1.01, 1.13) while other sexual identities (i.e. queer) were less likely (OR = 0.79; 95%CI: 0.70, 0.89).
Results of the negative binomial component of the hurdle model indicated that, among those who did not report marijuana or club drug use, monogamous men reported significantly more frequent CAS with casual partners compared to single men (RR = 1.63, 95%CI: 1.46, 1.83); meanwhile, monogamish men reported significantly fewer instances of CAS with casual partners compared to single men (RR = 0.77; 95%CI: 0.67, 0.89). Those in open relationships did not differ significantly from single men. Among single men, the use of club drugs, alone and combined with marijuana, was associated with significantly more instances of CAS with casual partners (RR = 2.32; 95%CI: 2.02, 2.64 and RR = 2.05; 95%CI: 1.86 2.28 respectively); however, those who used only marijuana did not differ significantly from those who did not report any drug use.
Examination of interaction terms indicated that the association between club drug use and CAS with casual partners —alone and combined with marijuana—was significantly weaker among monogamous men compared to single men (RR = 0.51; 95%CI: 0.37, 0.70 and RR = 0.55; 95%CI: 0.45, 0.68). The associations between drug use variables and frequency of CAS did not differ significantly between monogamish and single men or between open and single men.
With respect to demographic covariates, African-American (RR = 0.72; 95%CI: 0.67, 0.77), Latino (RR = 0.81; 95%CI: 0.77, 0.86), and Asian men (RR = 0.64; 95%CI: 0.58, 0.72) reported fewer instances of CAS with casual partners compared to White participants. Only those living in the Western U.S. reported mores instances of CAS with casual partners than those in the Northeast (RR = 1.07; 95%CI: 1.01, 1.13). HIV-positive respondents (RR = 1.75 95%CI: 1.68, 1.84) and those HIV negative respondents on PrEP (RR = 1.84, 95%CI: 1.76, 1.93) reported more frequent CAS with casual partners compared to HIV-negative/unknown respondents without PrEP prescriptions. Bisexual respondents reported more frequent CAS with casual partners than gay respondents (RR = 1.09; 95%CI: 1.02, 1.16), while other sexual identities did not differ significantly from either gay or bisexual men. Age was not significantly associated with multiple instances of CAS.
3.2. Drug use and CAS: Models comparing variability among partnered SMM
Table 3 contains the results of hurdle models predicting CAS with casual partners among only partnered men. This model was calculated to examine the impact of including main partner characteristics as model covariates. Similar to the previous model results, among men who did not report drug use, monogamish (OR = 2.53; 95%CI: 2.30, 2.79) and open men (OR = 4.48; 95%CI: 4.22, 4.76) were more likely to engage in CAS than men in monogamous relationships. Among monogamous men, marijuana use (OR =1.34; 95%CI: 1.23, 1.44), club drug use alone (OR = 1.70; 95%CI: 1.40, 2.05), and combined marijuana and club drug use (OR = 2.08; 95%CI: 1.83, 2.36) were all associated with increased odds of CAS with casual partners.
Table 3.
Hurdle model predicting CAS with Casual Partners Partnered men (n = 53,934)
| Any CAS with Casual Partners (Binomial) | Frequency of CAS with Casual Partners (Count) | |||
|---|---|---|---|---|
| Odds Ratio | 95% CI | Rate Ratio | 95% CI | |
| Age | 0.989** | (0.987, 0.991) | 0.996** | (0.994, 0.998) |
| Race/Ethnicity (ref = White) | ||||
| African-American | 0.84** | (0.78, 0.90) | 0.73** | (0.67, 0.79) |
| Asian | 0.64** | (0.59, 0.71) | 0.58** | (0.52, 0.65) |
| Latino | 0.90** | (0.85, 0.95) | 0.81** | (0.77, 0.87) |
| Other | 0.97 | (0.91, 1.04) | 1.07 | (0.99, 1.15) |
| Region (ref = Northeast) | ||||
| Midwest | 1.20** | (1.12, 1.27) | 0.97 | (0.90, 1.04) |
| South | 1.16** | (1.10, 1.22) | 0.99 | (0.93, 1.05) |
| West | 1.15** | (1.09, 1.22) | 1.07* | (1.01, 1.14) |
| PrEP, HIV (ref = Negative/Unknown, no PrEP) | ||||
| HIV positive | 1.92** | (1.81, 2.02) | 1.73** | (1.64, 1.83) |
| Current PrEP prescription | 2.89** | (2.73, 3.07) | 1.95** | (1.85, 2.05) |
| Sexual Orientation (ref Gay) | ||||
| Bisexual | 1.06 | (0.99, 1.13) | 1.15** | (1.06, 1.23) |
| Other | 0.78** | (0.68, 0.89) | 1.20* | (1.04, 1.39) |
| Relationship Agreement (ref = Monogamous) | ||||
| Monogamish | 2.53** | (2.30, 2.79) | 0.47** | (0.40, 0.55) |
| Open | 4.48** | (4.22, 4.76) | 0.59** | (0.54, 0.66) |
| Main Partner Age | 1.003* | (1.000, 1.005) | 1.005** | (1.003, 1.007) |
| Relationship Length > 2 years | 0.61** | (0.58, 0.64) | 0.99 | (0.95, 1.04) |
| Main Partner HIV Status (ref = Negative) | ||||
| Positive | 1.07* | (1.01, 1.13) | 1.17** | (1.11, 1.24) |
| Unknown | 1.75** | (1.58, 1.95) | 1.20** | (1.08, 1.33) |
| Substance Use (ref = no MJ, no CD) | ||||
| MJ no CD | 1.34** | (1.23, 1.44) | 1.08 | (0.94, 1.25) |
| CD no MJ | 1.70** | (1.40, 2.05) | 1.17 | (0.87, 1.59) |
| MJ and CD | 2.08** | (1.83, 2.36) | 1.09 | (0.91, 1.32) |
| Interactions | ||||
| Monogamish*MJ no CD | 0.85* | (0.73, 0.99) | 1.03 | (0.80, 1.32) |
| Monogamish*CD no MJ | 1.43* | (1.04, 1.95) | 1.48* | (1.01, 2.14) |
| Monogamish*MJ & CD | 1.08 | (0.87, 1.36) | 1.72** | (1.31, 2.24) |
| Open*MJ no CD | 0.86** | (0.78, 0.96) | 1.01 | (0.87, 1.18) |
| Open*CD no MJ | 1.68** | (1.34, 2.12) | 1.82** | (1.34, 2.48) |
| Open*MJ & CD | 1.20* | (1.03, 1.40) | 1.80** | (1.49, 2.20) |
p ≤ .05
p ≤ .01
NOTE: MJ = Marijuana; CD = Club Drug; CAS = Condomless anal sex
As with the previous model that included single SMM, this model illustrates the difference in magnitude of association for marijuana relative to club drug use. While the use of marijuana alone was associated with a 34% increase in the odds of CAS with casual partners among monogamous men, the odds of CAS increased by 70% among those monogamous men who reported club drug use alone versus those who reported no use. Meanwhile, the use of both marijuana and club drugs was associated with a 208% increase in the odds of CAS compared to those who reported no use.
Examination of interaction terms indicated that the association between marijuana use alone and the odds of CAS with casual partners was significantly weaker among monogamish and open men (OR = 0.85; 95%CI: 0.73, 0.99 and OR = 0.86; 95%CI: 0.78, 0.96 respectively). In contrast, the association between club drug use alone and CAS with casual partners was significantly stronger among monogamish (OR = 1.43; 95%CI: 1.04, 1.95) and open (OR = 1.68; 95%CI: 1.34, 2.12) compared to monogamous men. While the association between combined marijuana and club drug use and CAS with casual partners did not differ significantly between monogamish and monogamous men, it was significantly stronger among open (OR = 1.20; 95%CI: 1.03, 1.40) compared to monogamous men.
With respect to demographic covariates, odds of reporting any CAS with a casual partner decreased with age (OR = 0.989; 95%CI: 0.987, 0.991). Similar to the previous model, African-American (OR = 0.84; 95%CI: 0.78, 0.90), Latino (OR = 0.90; 95%CI: 0.85, 0.95), and Asian (OR = 0.64; 95%CI: 0.59, 0.71) respondents were less likely to report any CAS with casual partners compared to White participants. Those living in the Midwest (OR = 1.20; 95%CI: 1.12, 1.27), South (OR = 1.16; 95%CI: 1.10, 1.22), and West (OR = 1.15; 95%CI: 1.09, 1.22) were again more likely than Northeasterners to report any CAS with casual partners. Further aligning, HIV-positive respondents (OR = 1.92; 95%CI: 1.81, 2.02) and HIV negative respondents with PrEP prescriptions (OR = 2.89; 95%CI: 2.73, 3.07) were significantly more likely to engage in CAS with casual partners compared to HIV negative men without PrEP prescriptions. Men who identified as something other than gay or bisexual were significantly less likely to report at least one instance of CAS compared to gay men (OR = 0.78; 95%CI: 0.68, 0.89). Bisexual men did not differ significantly from gay identified men. Men in relationships longer than 2 years were significantly less likely to report CAS with casual partners (OR = 0.61; 95%CI: 0.58, 0.64). Those in relationships with main partners of positive (OR = 1.07; 95%CI: 1.01, 1.13) or unknown HIV status (OR = 1.75; 95%CI: 1.58, 1.95) were more likely to report CAS with a casual partner than those with HIV-negative partners.
Results of the negative binomial component predicting the frequency of CAS with casual partners indicated that, among men who did not report drug use, monogamish and open men reported significantly fewer instances of CAS with casual partners compared to monogamous men (RR = 0.47; 95%CI; 0.40, 0.55 and RR = 0.59; 95%CI: 0.54, 0.66). Among monogamous men, neither marijuana, or club drug use, or combined marijuana and club drug use was significantly associated with amount of CAS. Examination of interaction terms revealed that the association between marijuana and the frequency of CAS with casual partners did not differ significantly between monogamous men and either of the non-monogamous subgroups; however, the association between club drug use and frequency of CAS with casual partners, alone and combined with marijuana, was significantly greater among both monogamish (RR = 1.48; 95%CI: 1.01, 2.14 and RR = 1.72, 95%CI: 1.31, 2.24 respectively) and open (RR = 1.82; 95%CI: 1.34, 2.48 and RR = 1.80; 95%CI: 1.49, 2.20 respectively) groups compared to monogamous men.
Results for demographic covariates in the count portion of the model aligned with those from the model that included single men. African-American (RR = 0.73, 95%CI: 0.67, 0.79), Latino (RR = 0.81; 95%CI: 0.77, 0.87), and Asian men (RR = 0.58; 95%CI: 0.52, 0.65) reported fewer instances of CAS with casual partners compared to White participants. Partnered participants living in the Western U.S. reported more frequent CAS with casual partners than those in the Northeast (RR = 1.07, 95%CI: 1.01, 1.14). Partnered HIV-positive men (RR = 1.73, 95%CI: 1.64, 1.84) and those HIV negative men on PrEP (RR = 1.95; 95%CI: 1.85, 2.05) reported significantly more frequent CAS with casual partners than HIV-negative respondents without PrEP prescriptions. Both bisexual (RR = 1.15; 95%CI: 1.06, 1.23) and other identified participants (RR = 1.20; 95%CI: 1.04, 1.39) reported significantly more frequent CAS with casual partners than gay identified men. While respondent age was negatively associated with the frequency of CAS with casual partners (RR = 0.996; 95%CI: 0.994, 0.998), main partner age was positively associated with the frequency of CAS with casual partners (RR = 1.005; 95%CI: 1.003, 1.007). Relationship length was not associated with the frequency of CAS with casual partners. The frequency of CAS was greater for men with partners of positive (RR = 1.17; 95%CI: 1.11, 1.24) and unknown HIV status (RR = 1.20; 1.08, 1.33) than men with HIV-negative partners.
4.0. DISCUSSION
Both marijuana and club drug use contributed in some ways to the prediction of CAS with casual partners; however, associations were moderated by relationship status. Marijuana use was associated with increased odds of the occurrence of CAS with casual partners – but not the frequency – for single men and those in monogamous relationships. In contrast, club drug use consistently predicted both the occurrence and frequency of CAS among single men and those in non-monogamous relationships. While the use of club drugs was also significantly associated with increased odds CAS with casual partners among monogamous men, the association was significantly weaker than that observed among single and non-monogamous men.
While some have indicated a significant association between marijuana use and CAS with casual partners (e.g., Feinstein et al., 2019; Halkitis et al., 2018; Hendershot et al., 2010) other studies have not (e.g., Janulis et al., 2018; Rendina et al., 2015). These findings point to several factors that may contribute to such variability in previous research. First, associations between marijuana use and CAS with casual partners were appreciably smaller in magnitude compared to club drug use. This may make it more challenging to detect effects of marijuana in smaller samples or those with greater variance. Second, marijuana was only associated with significant increases in the odds of CAS among single men and those in monogamous agreements. Studies that do not incorporate relationship status as a covariate and differentiate among sexual agreements implicitly assume that associations between drug use sexual behavior are uniform across these groups. Finally, in those subgroups where it was significant (i.e., single and monogamous men), marijuana use increased the odds of CAS with casual partners – but not the frequency. It predicted “who was risky,” but not “amount of risk among the risky.” Disaggregating those components may have contributed to differences between the current results and previous research, where CAS with casual partners was measured only as a count variable (Melendez-Torres et al., 2016; Millar et al., 2016; Perry et al., 2016).
Substantial evidence has supported the conclusion that SMM who use club drugs are more likely to engage in CAS with casual partners (e.g., Parsons, Lelutiu-Weinberger, et al., 2013; Rendina et al., 2015). Results in this study indicated that this association is highly robust. Club drug use predicted both the occurrence and the frequency of CAS with casual partners uniformly across single and non-monogamous subgroups. The association was significantly diminished only among monogamous men. Even in this subgroup were the association was weakest, club drug use significantly predicted the odds (though not the frequency) of CAS with casual partners.
One limitation of these cross-sectional data is the inability to examine event-level associations between drug use and sex. As such, a number of potential explanations may exist for the results observed. One potential explanation arises from the observed rates of drug use and CAS with casual partners. Consistent with the results of previous research in smaller samples (e.g., Mitchell & Petroll, 2013; Parsons & Starks, 2014), non-monogamous men and single men were more likely to use club drugs and to have CAS with casual partners. The diminished likelihood of both of these behaviors among men in monogamous relationships may limit the potential for their correspondence.
It is noteworthy that in the current sample, monogamous men were less likely to have CAS with casual partners; however, among men who had CAS with casual partners, monogamous men actually reported more frequent CAS compared to single and non-monogamous men. In other words, while monogamous men were “least likely to be risky,” those that were risky, “had the most risk.” Hurdle models are uniquely suited to detecting this kind of process because they separate out the prediction of the mere occurrence of risk (the binary component of the model) and the prediction of amount or frequency of risky among those who are risky (Hu et al., 2011). Previous research has found that monogamous men report fewer instances of CAS with casual partners compared to single and non-monogamous men (Mitchell et al., 2012; Spicer et al., 2019; Starks, Robles, et al., 2019); however, these studies examined overall frequencies. These results reveal that while monogamous men may be at lower risk of HIV transmission overall, those who do experience risk are in urgent need of prevention. Central to risk reduction for high-risk partnered men is a focus on prevention efforts that teach relationship and communication skills. Several recent HIV prevention efforts have attempted to approach risk reduction for partnered men through dyadic interventions, in which both members of the dyad receive intervention and work together on risk reduction plans. These interventions include couples HIV testing and counseling (CHTC) (Sullivan et al., 2014); the telehealth delivered version (Project Nexus) (Stephenson et al., 2017); We Test (Starks, Dellucci, et al., 2019); the Couples Health Project (Starks et al., 2020); and 2Gether (Newcomb et al., 2017). All facilitate discussions between partners about their sexual agreement and shared HIV prevention goals. Such dyadic interventions, may be particularly useful for monogamous couples generally in order to insure that those who do need to discuss risk with casual partners have the opportunity.
Several demographic covariates are noteworthy. While SMM of color – particularly Latino and Black SMM – face disproportionate rates of HIV infection, these analysis are consistent with previous findings indicating that SMM of color are actually less likely to engage in CAS compared to White SMM (Harawa et al., 2004). Furthermore, frequency of CAS was lower among SMM of color. These results also support previous research highlighting the vulnerability of bisexually identified SMM, who were more likely to report CAS and reported higher frequencies of CAS compared to gay identified men (Goodenow et al., 2002; Smalley et al., 2016). Finally, PrEP uptake was associated with increased likelihood and frequency of CAS. While PrEP is highly effective at reducing the risk of HIV transmission during sex, this finding highlights the potential need for other STI prevention in conjunction with PrEP uptake.
These results must be viewed in light of several limitations. First, while the sample size is large and diverse, it remains a sample of convenience. All participants were recruited through a social networking or dating app. This study is therefore not represented of the larger population of SMM. Second, we utilized an aggregate club-drug use variable instead of examining individual substances. This prevented the introduction of a large number of correlated predictors and their associated interaction terms. While this analytic strategy prevents conclusions about the relative risk associated with specific kinds of club drugs, the use of an aggregated variable such as this is consistent with other studies (Coyer et al., 2019; Halkitis et al., 2018; Morgan et al., 2016).
PUBLIC HEALTH IMPLICATIONS
These findings highlight the extent to which relationship status contextualizes drug use and sexual behavior with casual partners among SMM. Initial efforts to develop interventions that address the co-occurrence of drug use and sexual HIV risk among SMM were largely developed for single men (Morgenstern et al., 2009; Parsons et al., 2014). They do not address relationship factors (e.g., partner communication or behavioral agreements) that are uniquely relevant for partnered SMM. More recent intervention development work has sought to integrate intervention components that enhance relationship functioning and facilitate agreement formation between partners in order to achieve reductions in drug use and sexual risk taking (Newcomb et al., 2017; Starks, Dellucci, et al., 2019; Starks et al., 2020). This kind of work has the potential to identify specific aspects of relationship functioning that are casually linked to drug use and sexual risk taking. Such work may benefit from ongoing attention to the role sexual agreements play in contextualizing drug use and sexual risk behavior outcomes.
Finally, these findings suggest that decisions about drug policy and intervention that are based upon the behavioral risks associated with marijuana use should be made with caution. The association between marijuana use and CAS with casual partners in this sample is, overall, less robust than the association between club drug use and CAS with casual partners. Marijuana use predicts only the occurrence (not the frequency) of CAS with casual partners and this association is restricted to single men and those in monogamous agreements. It would be an overstatement to assert that marijuana use poses the same degree of behavioral risk as club drug use; however, it would also be an overstatement to assert that there is no evidence of increased sexual risk taking associated with marijuana use (Halladay et al., 2018; Ryan & Ammerman, 2017). It would seem reasonable then that drug policy and intervention development might prioritize club drug use as the behavior of greater concern; however, for at least some populations of SMM, policy makers and intervention developers would do well to retain a focus on marijuana use.
Despite its limitations, this study provides a robust test of whether associations between drug use and sexual risk taking generalize from single to partnered men. Results highlight the utility of three methodological elements in studying drug use among SMM: 1) assessing both the occurrence and frequency of sexual behavior; 2) disaggregating marijuana and club drug use; and 3) distinguishing between sexual agreement groups when studying drug use among partnered SMM. In doing so, this study demonstrated the robust nature of the association between club drug use and CAS with casual partners while also illustrating the potential for marijuana to predict the occurrence of CAS in specific subgroups.
HIGHLIGHTS.
Relationship status contextualized drug use and casual partner CAS associations.
Marijuana increased odds of CAS for single and monogamous SMM.
Club drugs increased CAS odds and frequency for single and non-monogamous SMM.
Associations between marijuana and CAS were smaller than club drugs.
ACKNOWLEDGEMENT
Data collection was supported by grants from the National Institute of Allergy and Infectious Diseases, National Institute on Mental Health, Eunice Kennedy Shriver National Institute on Child Health and Human Development, and National Institute on Drug Abuse (PI: Starks; R34DA043422, PI: Starks; R01DA045613, PI: Starks; U19HD089875, PI: Naar; UG3AI133674, PI: Rendina; R01MH114735, PI: Rendina; R01DA041262).
REFERENCES
- Carey JW, Mejia R, Bingham T, Ciesielski C, Gelaude D, Hebst JH, Sinunu M, Sei E, Pranchand N, Jenkins RA, Stall R, 2008. Drug use, high-risk sex behaviors and increased risk for recent HIV infection among men who have sex with men in Chicago and Los Angeles. AIDS Behav. 13(6), 1084–1096 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 2016. HIV infection risk, prevention, and testing behaviors among men who have sex with men—National HIV Behavioral Surveillance, 20 U.S. Cities, 2014 http://www.cdc.gov/hiv/library/reports/surveillance/#panel2
- Centers for Disease Control and Prevention. 2018. HIV in the United States by Region. https://www.cdc.gov/hiv/pdf/statistics/overview/cdc-hiv-geographic-distribution.pdf
- Coyer L, Boyd A, Davidovich U, Prins M, Matser A, 2019. Trends in recreational drug use and associations with CAS, HIV and STI among HIV-negative MSM in Amsterdam between 2008–2017. Sex Transm Infect. 95(suppl 1), A246–A246 [Google Scholar]
- Feinstein BA, Moran KO, Newcomb ME, Mustanski B, 2019. Differences in HIV risk behaviors between self-identified gay and bisexual young men who are HIV-negative. Arc Sex Behav. 48(1), 261–275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodenow C, Netherland J, Szalacha L, 2002. Aids-related risk among adolescent males who have sex with males, females, or both: Evidence from a statewide survey. Am J Public Health. 92(2), 203–210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodreau SM, Carnegie NB, Vittinghoff E, Lama JR, Sanchez J, Grinsztein B, Koblin BA, Mayer K,H, Buchbinder SP, 2012. What drives the US and Peruvian HIV epidemics in men who have sex with men (MSM). PLoS One. 7(11) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Bub K, Stults CB, Bates FC, Kapadia F, 2018. Latent growth curve modeling of non-injection drug use and condomless sexual behavior from ages 10 to 21 in gay, bisexual and other YMSM: The P18 Cohort Study. Subst Use Misuse. 53(1), 101–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halladay J, Petker T, Fein A, Munn C, Mackillop J, 2018. Brief Interventions for cannabis use in emerging adults: protocol for a systemic review, meta-analysis, and evidence map. Syst Rev. 7(1), 106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harawa NT, Greenland S, Bingham TA, Johnson DF, Cochran SD, Cunningham WE, Celentano DD, Koblin BA, LaLota M, Mackellar DA, McFarland W, Shehan D, Stoyanoff S, Thiede H, Torian L, Valleroy LA, 2004. Associations of race/ethnicity with HIV prevalence and HIV-related behaviors among young men who have sex with men in 7 urban centers in the United States. J Acquir Immune Defic Syndr. 35(5), 526–536 [DOI] [PubMed] [Google Scholar]
- Hendershot CS, Magnan RE, Bryan AD, 2010. Associations of marijuana use and sex-related marijuana expectancies with HIV/STD risk behavior in high-risk adolescents. Psychol Addict Behav. 24(3), 404–414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu MC, Pavlicova M, Nunes EV, 2011. Zero-inflated and hurdle models of count data with extra zeros: Examples from an HIV-risk reduction intervention trial. Am J Drug Alcohol Abuse. 37(5), 367–375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janulis P, Feinstein BA, Phillips G, Newcomb ME, Birkett M, Mustanski B, 2018. Sexual partner typologies and the association between drug use and sexual risk behavior among young men who have sex with men. Arch Sex Behav. 47(1), 259–271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin KG (2008-2020). Effect size statistics in logistic regression. The Analysis Factor. Retrieved September, 2020 from https://www.theanalysisfactor.com/effect-size-statistics-logistic-regression/ [Google Scholar]
- Melendez-Torres GJ, Hickson F, Reid D, Weatherburn P, Bonell C, 2016. Nested event-level case-control study of drug use and sexual outcomes in multipartner encounters reported by men who have sex with men. AIDS Behav. 20(3), 646–654 [DOI] [PubMed] [Google Scholar]
- Millar BM, Starks TJ, Grov C, Parsons JT, 2016. Sexual risk-taking in HIV-negative gay and bisexual men increases with depression: Results from a U.S. National Study. AIDS Behav. 21(6), 1665–1675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JW, 2016. Differences in gay male couples’ use of drugs and alcohol with sex by relationship HIV status. Am J Mens Health. 10(4), 262–269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JW, Boyd C, McCabe S, Stephenson R, 2014. A cause for concern: Male couples’ sexual agreements and their use of substances with sex. AIDS Behav. 18(7), 1401–1411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JW, Champeau D, Harvey SM, 2013. Actor-partner effects of demographic and relationship factors associated with HIV risk within gay male couples. Arch Sex Behav. 42(7), 1337–1345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JW, Harvey SM, Champeau D, Seal DW, 2012. Relationship factors associated with HIV risk among a sample of gay male couples. AIDS Behav. 16(2), 404–411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JW, Pan Y, Feaster D, 2016. Actor-Partner effects of male couples substance use with sex and engagement in condomless anal sex. AIDS Behav. 20(12), 2904–2913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JW, Petroll AE, 2013. Factors associated with men in HIV-negative gay couples who practiced UAI within and outside of their relationship. AIDS Behav. 17(4), 1329–1337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan E, Skaathun B, Michaels s., Young L, Khanna A, Friedman SR, Davis B, Pitrak D, Schneider J, 2016. Marijuana use as a sex-drug is associated with HIV risk among black MSM and their networks. AIDS Behav. 20(3), 600–607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenstern J, Bux DA, Parsons JT, Hagman BT, Wainberg M, Irwin T, 2009. Randomized trial to reduce club drug use and HIV risk behaviors among men who have sex with men. Psychol Assess. 77(4), 645–656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb ME, Macapagal KR, Feinstein BA, Bettin E, Swann G, Whitton SW, 2017. Integrating HIV prevention and relationship education for young same-sex male couples: A pilot trial for the 2GETHER intervention. AIDS Behav. 21(8), 2464–2478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Lelutiu-Weinberger C, Botsko M, Golub SA, 2013. Predictors of day-level sexual risk for young gay and bisexual men. AIDS Behav. 17(4), 1465–1477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Lelutiu-Weinberer C, Botsko M Golub SA, 2014. A randomized controlled trial utilizing motivational interviewing to reduce HIV risk and drug use in young gay and bisexual men. Psychol Assess. 82(1), 9–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Starks TJ, 2014. Drug use and sexual arrangements among gay couples: Frequency, interdependence and associations with sexual risk. Arch Sex Behav. 43(1), 89–98 [DOI] [PubMed] [Google Scholar]
- Parsons JT, Starks TJ, Dubois S, Grov C, Golub SA, 2013. Alternatives to monogamy among gay male couples in a community survey: Implications for mental health and sexual risk. Arch Sex Behav. 42(2), 303–312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry NS, Taylor SW, Elsesser S,Safren SA, O’Cleirigh C, 2016. The predominant relationship between sexual environment characteristics and HIV-serodiscordant condomless anal sex among HIV-positive men who have sex with men (MSM). AIDS Behav. 20(6), 1228–1235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rendina HJ, Moody RL, Ventuneac A, Grov C Parsons JT, 2015. Aggregate and event-level associations between substance use and sexual behavior among gay and bisexual men: Comparing retrospective and prospective data. J Alcohol Drug Depend. 154, 199–207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan SA, Ammerman SD, 2017. Counseling parents and teens about marijuana use in the era of legalization of marijuana.J Pediatr X. 139(3), e1–e6 [DOI] [PubMed] [Google Scholar]
- Smalley KB, Warren JC, Barefoot KN, 2016. Differences in health risk behaviors across understudied LGBT subgroups. Health Psychol. 35(2), 103–114 [DOI] [PubMed] [Google Scholar]
- Spicer R, Darbes L, Hoff C, Sullivan PS, Stephenson R, 2019. Sexual agreements: a scoping review of measurement, prevalence and links to health outcomes. AIDS Behav, 23(1), 259–271. [DOI] [PubMed] [Google Scholar]
- Starks TJ, Dellucci TV, Gupta S, Robles G, Stephenson R, Sullivan P, Parsons JT, 2019. A pilot randomized trial of intervention components addressing drug use in Couples HIV Testing and Counseling (CHTC) with male couples. AIDS Behav. 23, 1–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starks TJ, Parsons JT, 2018. Drug use and HIV prevention with young gay and bisexual men: Partnered status predicts intervention response. AIDS Behav. 22(9), 2788–2796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starks TJ, Robles G, Bosco SC, Dellucci TV, Grov C, Parsons JT, 2019. The prevalence and correlated of sexual arrangements in a national cohort of HIV-negative gay and bisexual men in the United States. Arch Sex Behav. 48(1), 369–382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starks TJ, Tuck AN, Millar BM, Parsons JT, 2016. Linking syndic stress and behavioral indicators of main partner HIV transmission risk in gay male couples. AIDS Behav. 20(2), 439–448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson R, Freeland R, Sullivan SP, Riley E, Johnson BA, Mitchell J, McFarland D, Sullivan PS (2017). Home-based HIV testing and counseling for male couples (Project Nexus): A protocol for a randomized controlled trial. JMIR Res Protoc, 6(5), e101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan PS, Salazar L, Buchbinder S, Sanchez TH, 2009. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 23(9), 1153–1162 [DOI] [PubMed] [Google Scholar]
- Sullivan PS, Stephenson R, Grazter B, Wingood G, DiClemente RJ, Allen S, Hoff CC, Salazar L, Scales L, Montgomery J, Schwartz A, Barnes J, Grabbe K. 2014. Adaptation of the African couples HIV testing and counseling model for men who have sex with men in the United States: An application of the ADAPT-ITT framework. Springerplus, 3(1), 249–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theodore PS, Duran RE, Antoni MH, 2014. Drug use and sexual risk among gay and bisexual men who frequent party venues. AIDS Behav. 18(11), 2178–2186 [DOI] [PubMed] [Google Scholar]
- Vosburgh HW, Mansergh G, Sullivan PS, Purcell DW, 2012. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS Behav. 16(6), 1394–1410 [DOI] [PubMed] [Google Scholar]