Across the US, elective surgical operations were canceled or delayed by the SARS-CoV-2 (COVID-19) pandemic on March 18, 2020, through an official Centers for Medicaid and Medicare press release.1 The American College of Surgeons (ACS) and other organizations quickly mobilized to try to provide guidance as to prioritization of surgical cases recognizing that many nonurgent cases still require timely intervention to prevent escalation of disease or disability. Within days of the nationwide announcement tools such as the Elective Surgery Acuity Scale as well the “Elective Case Triage Guidelines for Surgical Care” appeared on the ACS web site.2,3 The Department of Veterans Affairs (VA), which performs over 600,000 operations annually and is the largest single health system in the US, followed the national guidelines with a mandate to stop all elective surgery effective March 15, 2020. There was no VA directive defining urgent or elective cases, thus these decisions were made at the local facility level. The VA, like many nonfederal hospitals, rapidly moved consultations to telemedicine for nonurgent cases, thus prioritizing face-to-face visits for emergent and urgent patient presentations only. The VA has a capitated care payment model minimally influenced by market forces and thus may be useful in surgical planning to approximate the minimum volume of adult operations necessary in a national health crisis, absent trauma, or obstetrics.
METHODS
Using the VA Corporate Data Warehouse, a national repository of electronic health records at VA facilities, we analyzed all operations from January 1, 2019, to July 1, 2020. Time comparisons surrounded 2020 VA mandates to stop and then to restart elective surgery on March 15 and April 30. We compared weekly surgical procedure counts by specialty and 17 specific procedures across specialties for three seven-week periods defined as Pre-Mandate (Jan 27–March 15), Mandate (March 16–May 3), and Restart (May 4–June 28). We estimated incidence rate ratios (IRRs) by comparing daily surgical procedure counts during epidemiological calendar (Sunday-Saturday) weeks 12 to 18 in 2019 and 2020 with Poisson regressions adjusted for seasonal variation and secular trends with week-of-year and year fixed effects. To examine the proportion of patients either admitted postoperatively or with an American Society of Anesthesiologists (ASA) score of 3 or 4 during the Mandate time period, we analyzed the cohort of procedures that had an inpatient admission rate between 5% and 95% in 2019. This study was approved by the IRB at the Palo Alto VA.
RESULTS
In 2020, surgical operations in the VA system decreased from 57,525 (Pre-Mandate) to 12,377 (Mandate), a case reduction greater than 75% (IRR, .22; 95% CI, 0.12–0.32) (Fig. 1 and Supplemental Table 1). Specialties most affected were ophthalmology (IRR 0.06; 95% CI, −0.01 to 0.12), plastic surgery (IRR 0.16; 95% CI, 0.07–0.25), and orthopedic surgery (IRR 0.16; 95% CI, 0.08–0.24). Procedures that almost completely stopped included cataract procedures (99% reduction), carpal tunnel release (99%), and knee and hip arthroplasty (99% and 97%). Specialties least affected were cardiac surgery (IRR, 0.39; 95% CI 0.21–0.57), vascular surgery (IRR, 0.46; 95% CI 0.29–0.63), and thoracic surgery (IRR, 0.57; 95% CI 0.39–0.75), although all case counts decreased greater than 45%.
FIGURE 1.
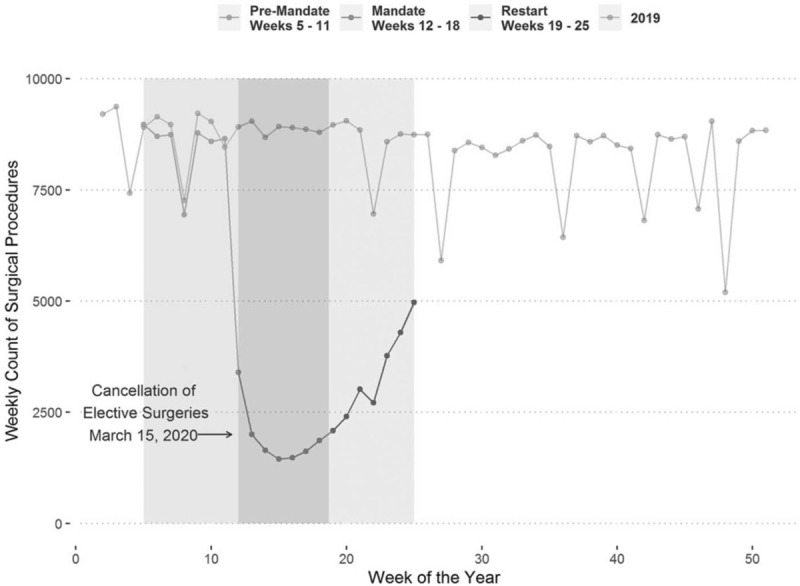
Time profile of VA surgical procedures: Jan 1 to July 1 2019 and Jan 1 to July 1, 2020.
Following the mandated shutdown, surgical procedures rebounded in the Restart period (24,465 cases), but remained well below prepandemic levels. The largest increase by specialty was in ophthalmology (590%), followed by gynecology (230%) and orthopedic surgery (140%). Knee arthroplasty (5500%), carpal tunnel release (2273%), and cataract procedures (1694%) represented the largest increases among specific procedures.
The proportion of patients admitted post-operatively during the mandate period increased by +6.8 percentage points overall (P-value <0.001; 2019 mean = 69.3%). Patients who underwent laparoscopic cholecystectomy and inguinal hernia demonstrated the largest change in proportion admitted compared to 2019. The proportion of patients who were ASA 3 or 4 decreased during the mandate time period by −1.5 percentage points (P-value <0.001; 2019 mean = 67%. (Table 1)
TABLE 1.
Changes in Proportion of Admissions and ASA 3 or 4 cases: Mandate Period Compared to 2019
| Operation | Proportion Admitted in 2019 (%) | Change in Proportion Admitted (Percentage Points) | P-value | Proportion ASA III/IV in 2019 (%) | Change in Proportion ASA III/IV (Percentage Points) | P-value |
| Lap Cholecystectomy | 59.5 | 23.7 | <0.001 | 76.3 | 7.1 | 0.002 |
| Inguinal Hernia | 32.4 | 18.8 | <0.001 | 66.2 | 5.6 | <0.001 |
| Appendectomy | 77.4 | 5.9 | <0.001 | 46.1 | −7.2 | <0.001 |
| Thyroidectomy | 56.0 | 5.1 | 0.047 | 76.3 | 3.0 | 0.014 |
| Prostatectomy | 79.9 | 3.1 | 0.004 | 73.1 | −3.6 | 0.069 |
| Lower Extremity Amputation | 81.6 | 2.2 | 0.022 | 66.0 | 7.4 | <0.001 |
| AV Shunt Placement | 25.5 | 1.2 | 0.493 | 51.1 | −9.8 | <0.001 |
| Lumber Laminectomy | 76.3 | -4.7 | 0.015 | 77.2 | 2.5 | 0.022 |
Changes in proportion of patients admitted and proportion ASA III/IV for operations with >5% and <95% percent admitted in 2019. The overall change in proportion admitted was +6.8 percentage points (P-value <0.001; 2019 mean = 69.3%) and the overall change in proportion ASA III/IV was −1.5 percentage points (P-value <0.001; 2019 mean = 67%).
DISCUSSION
In the 7 weeks of mandated elective surgery cancellation from March 15 until May 4, 2020, 78% fewer surgical operations were performed in the VA than in the previous 7 weeks. This magnitude is larger than the decline in VA hospital admissions during the same period.4 Appropriately, surgical operations with the largest decline were associated with function and quality of life rather than survival. During the Restart period, these same quality of life-driven procedures rebounded most dramatically but no procedures have yet to return to prepandemic levels.
The April 30, 2020 “VA Moving Forward Plan” outlined phased low-level resumption of elective cases within each region.5 Procedure continuation will require careful management as the pandemic continues. The VA will likely take longer to resume full operative services due to different financial pressures than non-Federal hospitals.
Results of this study should be interpreted in the context of some limitations, including imperfect generalizability of the VA health system and Veteran patients to a national population.6 Our data, for example, excluded trauma and obstetrics.
As COVID-19 continues to have an impact on various communities, the continuous availability of elective surgery remains unclear. Scheduling elective cases will continue to require consideration of hospital resources and special consideration of patients who may be negatively affected to ensure that procedure deferral does not cause harm.
Supplementary Material
REFERENCES
- 1.CMS Releases Recommendations on Adult Elective Surgeries, Non-Essential Medical, Surgical, and Dental Procedures During COVID-19 Response. Available at: https://www.cms.gov/newsroom/press-releases/cms-releases-recommendations-adult-elective-surgeries-non-essential-medical-surgical-and-dental. Accessed November 14, 2020. [Google Scholar]
- 2.Available at: https://www.facs.org/covid-19/clinical-guidance/triage. Accessed November 14, 2020. [Google Scholar]
- 3.Available at: https://www.facs.org/covid-19/clinical-guidance/elective-case. Accessed November 14, 2020. [Google Scholar]
- 4.Baum A, Schwartz MD. Admissions to veterans affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA 2020; 324:96–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Available at: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwin2OjrnfTqAhXJpJ4KHb_YDPwQFjABegQIBRAB&url=https%3A%2F%2Fwww.va.gov%2Fcovidtraining%2Fdocs%2F20200519InvasiveProcedures%2F20200509_Moving_Forward_Plan.pdf&usg=AOvVaw1VQtBhe1qi7DPPsp-zWsUX. Accessed July 20, 2020. [Google Scholar]
- 6.Agha Z, Lofgren RP, VanRuiswyk JV, et al. Are patients at veterans affairs medical centers sicker?: A comparative analysis of health status and medical resource use. Arch Intern Med 2000; 160:3252–3257. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


