Abstract
Purpose of Review
COVID-19 is a major concern for the health and wellbeing of individuals worldwide. As COVID-19 cases and deaths continue to increase in the USA, aging Black and Hispanic populations have emerged as especially at-risk for increased exposure to COVID-19 and susceptibility to severe health outcomes. The current review discusses the weathering hypothesis and the influence of social inequality on the identified health disparities.
Recent Findings
Aging minoritized populations have endured structural and social inequality over the lifecourse. Consequently, these populations experience weathering, a process that results in physiological dysregulation due to stress associated with persistent disadvantage. Through weathering and continued inequity, aging minoritized populations have an increased risk of exposure and poor health outcomes from COVID-19.
Summary
Current literature and available data suggests that aging minoritized persons experience high rates of COVID-19 morbidity and mortality. The current review hypothesizes and supports that observed disparities are the result of inequalities that especially affect Black and Hispanic populations over the lifecourse. Future efforts to address these disparities should emphasize research that supports governments in identifying at-risk groups, providing accessible COVID-19-related information to those groups, and implementing policy that addresses the structural and social inequities that perpetuate current COVID-19 disparities.
Keywords: COVID-19, Weathering, Aging, Black, Hispanic, Health disparities, This article is part of the Topical Collection on Epidemiology of Aging
Introduction
In December 2019, the novel coronavirus disease (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was identified in Wuhan, China [1]. Since then, COVID-19 has emerged as a major global health threat, infecting nearly 107 million people and killing over 2.3 million people worldwide [2]. Currently, the USA is leading globally in the number of confirmed infections and deaths. COVID-19 has killed more than 465,000 people in the USA, with the majority (80%) of those deaths occurring in individuals aged 65 years and older [3]. Evidence suggests that age is an important factor in predicting COVID-19 symptom severity and mortality, though physiological factors such as cardiovascular and metabolic diseases are also implicated, as are behavioral and social factors, including occupation and socioeconomic status [4].
While COVID-19 is of particular concern for older populations, racial and ethnic minority populations are at additionally high risk [5, 6••]. Black individuals and individuals of Hispanic origin have COVID-19 death rates nearly three times higher than non-Hispanic White (hereafter White) individuals [4]. In contrast to White persons, Black and Hispanic persons also have a higher rate of cases and hospitalizations for COVID-19 [4]. Among aging minoritized persons, Black and Hispanic persons over the age of 65 years, the risk of severe illness or death from COVID-19 is especially high.
In response to nationwide increases in COVID-19 cases, local and state governments have implemented temporary restrictions and regulations to decrease person-to-person contact and prevent the spread of COVID-19. Such regulations include stay-at-home orders, non-essential business curfews, and business closures [7]. Despite these efforts, COVID-19 continues to spread, with the number of confirmed infections rising by the thousands daily in the USA [3]. Widening disparities further illustrate that government efforts may not be addressing key factors associated with the spread of this disease. Understanding the factors that contribute to existing disparities is essential to preventing further spread and further mortality, particularly among high-risk groups.
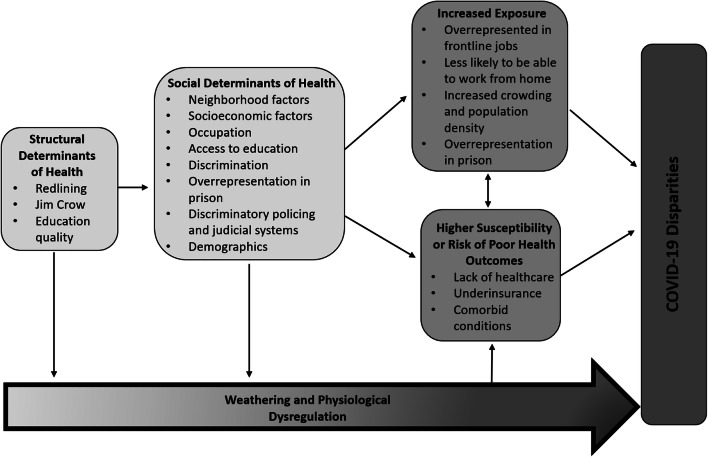
In the current review, we examine factors that make aging minoritized persons susceptible to both increased risk of exposure to COVID-19 and severe COVID-19 infection or death. We propose a biopsychosocial model in which we hypothesize that social inequality contributes to observed disparities in COVID-19 morbidity and mortality. Specifically, we define the weathering hypothesis as it relates to aging minoritized populations and discuss the role of weathering in explaining increased risk of exposure and severe infection. Next, we discuss the social and behavioral factors that may contribute to the biological risk factors exhibited for COVID-19. We follow with an exploration of those biological risk factors. Finally, we conclude with some recommendations to mitigate the burden of COVID-19 in these populations.
Weathering
The weathering hypothesis, first coined by Arline Geronimus, is defined as the physiological impact of social inequality compounded with age that leads to health inequities [8]. Understanding how accumulated stress and other social disadvantages over the lifecourse can produce premature biological aging can help elucidate the effects of social inequality, racial discrimination, or bias in exposures to psychosocial or environmental hazards on health [8]. The hypothesis posits that marginalized racial and ethnic groups, such as Black and Hispanic populations, experience early health deterioration by way of cumulative exposure to socio-political inequality [8, 9••].
Currently, literature suggests that the consequences of social inequality may manifest physically through expedited biological aging. Biological age is an abstract concept to express the “true global state” of aging and life expectancy using biomarkers and an algorithm as compared to a person’s chronological age [10]. Allostatic load scores, which operationalize the physiological burden imposed by stress, are higher in Black persons ages 35–64 years old when compared to White persons in the same age range [11]. Other measures of biological aging, such as telomere length, have also indicated greater degrees of weathering in marginalized groups when compared to non-marginalized groups. For example, short telomeres, which indicate more advanced biological age, have been shown to be more prevalent in Black women in comparison to their White counterparts due to unique social, political, and racial indicators of stress [12]. Often by way of this accelerated biological aging, older minoritized individuals are also more likely to develop severe forms and chronic sequelae of conditions like cardiovascular diseases (CVD), metabolic disorders, and certain cancers [13, 14]. As with COVID-19, Black and Hispanic populations exhibit higher rates of hospitalizations and mortality, which is attributable to bearing a disproportionate burden of underlying comorbidities such as CVD [9••]. As comorbidities and accelerated aging are compounded with persistent inequity over the lifespan, the likelihood of experiencing severe illness and/or death due to COVID-19 increases.
Emerging research has shown that social inequity also plays a major role in increasing one’s risk of exposure to COVID-19. Social determinants of health, including childhood and adult socioeconomic status, neighborhood and physical environment, housing, and access to healthcare and resources, disproportionately affect Black and Hispanic groups and are known to influence risk of exposure to COVID-19 [4, 15]. For example, crowded living environments and overrepresentation in “essential worker” occupations put Black and Hispanic individuals at greater risk for exposure to COVID-19 by limiting ability to social distance [16, 17]. The socially linked factors that increase COVID-19 risk of exposure and severe health outcomes for aging minoritized persons lead us to hypothesize that weathering may have an association with observed COVID-19 disparities (Fig. 1).
Fig. 1.
Weathering and physiological dysregulation
Social and Behavioral Factors
A complex web of social and behavioral factors likely contributes to weathering and thus plays a role in the observed disparities in COVID-19 morbidity and mortality for aging minoritized populations. Understanding this web requires attending to the longstanding structural inequities in employment, housing, healthcare, and other critical social determinants of health that shape both infection exposure and treatment access differentially along racial/ethnic lines and across the lifecourse [18]. Furthermore, adopting an intersectional perspective can help shed light on risk heterogeneity within aging minoritized populations by socioeconomic status and gender/sex (among other dimensions of social identity and/or position) as a result of multiple and oftentimes compounding axes of structural inequity [19]. In this section, we review some social and behavioral determinants that may be contributing to COVID-19 morbidity and mortality disparities.
Discrimination
To fully understand the effects of COVID-19, the past and current context of discrimination and racism in the USA on the interpersonal and structural levels must be considered. During their lifecourse, older Black individuals have experienced legal discrimination via Jim Crow laws as well as ensuing and current discriminatory policies which are cultivated through structural racism. In relation to COVID-19, policies such as redlining may contribute to inequities as minoritized individuals are more likely to live in areas of high population density and with less resources leaving them vulnerable to infection spread [20]. Similarly, mass incarceration has resulted in overrepresentation of these populations in the US prison system where infection rates have been found to be over 5 times greater than rates in the general population [21]. Moreover, the experience of racial discrimination at the interpersonal level may be contributing to severe COVID-19 illness and mortality in aging minoritized persons through accelerated biological aging and the process of weathering [12].
Cultural Norms and Religion
Culture and religion are critical and often overlooked aspects which may inadvertently contribute to COVID-19 spread. Among others, large family size and close contact greetings are common among Hispanic persons and are cultural norms that may challenge the feasibility of social distancing and increase the risk of COVID-19 infection and transmission [22]. Furthermore, the closure of churches, which play an important role in Black communities often serving as sources of information, resources, social interaction, and emotional support, may disproportionately affect Black communities [23]. The uniqueness of these factors and their potential to exacerbate the reach and effects of COVID-19 underscore the need for culturally appropriate public health measures and communication. Especially given the historical mistreatment, efforts to empower minoritized populations through appropriate dissemination of information and supportive resources are crucial.
Healthcare and Historical Context
Minoritized persons in the USA experience a fraught relationship with the healthcare system that may exacerbate COVID-19-related risks. Because of centuries of experimentation, mistreatment, discrimination, and dehumanization from the healthcare system and research, many Black and Hispanic people are, understandably, hesitant to trust the system. This may be heightened in aging minoritized persons who acutely remember or experienced overt offenses, though these atrocities continue to this day [24, 25••]. An illustration of these effects is the distrust of the COVID-19 vaccination efforts: though skepticism is present across racial and ethnic lines, if vaccination trends continue [26], marginalized communities may be vaccinated at lower rates, leaving aging minoritized persons at particular risk [27, 28]. Furthermore, immigrants that are undocumented may be largely barred from treatment and prevention efforts, given the poor dissemination of information regarding COVID-19 to non-English speaking populations and rational fears that interaction with the healthcare system may result in detention, punishment, and/or deportation [29]. Additionally, similar to incarcerated populations, COVID-19 infection rates are growing faster in immigration detention centers than elsewhere in the USA [30].
Minoritized persons are un- or underinsured at higher rates than White people [31, 32], such that healthcare utilization may present insurmountable costs. Federal legislation has been enacted to cover many of the COVID-19-related costs for those uninsured [33], but few people likely know about this [34]. Given the complexity of our multi-payer system, it is often unclear what is covered and can be particularly difficult to navigate as an older person. Finally, access presents another barrier to healthcare for aging minoritized populations, who tend to have less access to transportation, are unable to take time off from work, and have other difficulties [31, 32].
Socioeconomic Status
Socioeconomic status is often a proxy for social determinants of health. It represents a critical array of factors that impact acute and chronic disease risk; here, we will discuss housing and employment. Populations that live in lower-quality or hazardous housing, are homeless or have housing instability, live in multigenerational homes, and/or tightly packed public housing complexes are among the highest risk for coronavirus transmission and COVID-19 for a multitude of reasons [32, 35]. These also tend to be disproportionately made up of minoritized communities. Minoritized communities are less likely to receive financial deferments for housing payments and, thus, face eviction [36]. A particularly poignant illustration of how this intersects with and compounds health inequities in aging minoritized populations is in short- and long-term care facilities, where people are contracting and dying of COVID-19 at extraordinary rates [37, 38]. In particular, nursing homes that have greater proportions of minoritized persons are some of those that are experiencing the most severe outbreaks [38–41].
Employment inequities are also exacerbating COVID-19-related morbidity and mortality. Aging persons and minoritized persons are among groups that may be more likely to be laid off or are already living at or below the poverty line [32], which itself is linked to health outcomes. Black and Hispanic persons are also much more likely to be essential workers in the service industry [16, 32, 35], where social distancing is difficult and working from home is not an option. Many live paycheck-to-paycheck or without paid sick leave [32], eliminating ability to take time off if sick and effectively encouraging coronavirus spread through no fault of their own.
Gender/Sex
Another important dimension of social identity/position potentially contributing to heterogeneity in COVID-19 morbidity and mortality risk within aging minoritized populations is gender/sex. It is now well-described that, relative to cisgender men, cisgender women are less likely to have severe cases and/or die yet may be more likely to experience long-term or chronic symptoms of the disease (i.e., “long COVID”) [42, 43]. Furthermore, researchers have postulated that there are important interactions between gender/sex and age, given the non-uniformity of the observed gender/sex morbidity and mortality ratios across age groups [44]. Unfortunately, COVID-19 data is rarely disaggregated by gender/sex, race/ethnicity, and age simultaneously [45], and thus, how these dimensions of social identity/position intersect to shape risk across the lifecourse is largely unknown. However, research into the unique forms of structural disadvantage experienced by populations marginalized by sexism, racism, and ageism is suggestive of meaningful intersectionality. For example, minoritized women (especially Black, Hispanic, and Indigenous women) are disproportionately represented among frontline workers and in occupations that do not provide paid sick days [46, 47], which may contribute to a higher risk of COVID-19 exposure. Minoritized women are also more likely than their male and/or White counterparts to suffer from conditions associated with severe COVID-19 symptoms (e.g., asthma, diabetes) and experience considerable medical discrimination [48, 49•], potentially leading to poor outcomes once infected. Collectively, these social and health inequities, in addition to the biological impacts of weathering, suggest that aging minoritized women may experience distinctive disparities in COVID-19 morbidity and mortality. More research in this area, especially research that includes gender minority populations who have been largely excluded from extant surveillance efforts, is critically needed.
Health-Related and Biological Factors
Only a subset of those infected with COVID-19 develop severe infection, characterized by hypoxemia, progressive respiratory failure, systemic organ failure, and/or death [50]. Pre-existing chronic conditions including hypertension, diabetes, elevated body mass index (BMI), chronic kidney disease (CKD), and cardiovascular disease have been consistently associated with severe COVID-19 infection [51, 52]. These pre-existing conditions disproportionately impact Black and Hispanic populations as a consequence of social, economic, and historic factors, including the marginalization and abuse of these populations by the medical community [6••]. As proposed above, the weathering hypothesis may help to explain why marginalized populations bear a disproportionate share of the chronic health disease burden: exposure to racial discrimination results in persistent exposure to stress and a chronic inflammatory state. Consistent with this hypothesis, aging minoritized populations have higher levels of inflammatory markers, and elevated inflammatory markers strongly predict hypertension, diabetes, and cardiovascular disease [53]. It is also important to acknowledge the interrelated nature and co-occurrence of these conditions. Indeed, multimorbidity (the coexistence of two or more chronic conditions) is the norm in adults over age 65 years, with a prevalence of 55–98% [54, 55].
Hypertension, Cardiovascular Disease, and Chronic Kidney Disease
COVID-19 patients with hypertension or cardiovascular disease are 3–4 times more likely to develop severe disease compared to those without pre-existing conditions [56, 57•]. Additionally, patients with chronic kidney disease (CKD) have COVID-19 hospitalization and mortality rates 11 and 14 times higher than the general population, respectively [58, 59]. Black individuals have the highest prevalence of hypertension and CKD of any racial and ethnic group in the USA, with 57.1% of Black adults reporting hypertension in 2018 [60–62]. Hypertension is a significant risk factor for cardiovascular disease and CKD, and Black patients are twice as likely to die of preventable heart disease and kidney failure than white individuals [63, 64]. Consistent with our understanding of weathering, Black populations have been shown to develop hypertension and cardiovascular disease on average 10 years before White populations, even after accounting for differences in demographic and health-related factors [65]. Lifetime discrimination has also been associated with hypertension among Black women in the USA, and income inequality and neighborhood racial segregation are associated with increased mortality among Black patients with advanced CKD [64, 66]. The increased risk of severe COVID-19 infection among individuals with hypertension, cardiovascular disease, and/or CKD demonstrates another way COVID-19 is sharpening pre-existing disparities.
Diabetes
Individuals with COVID-19 and diabetes have twofold and threefold increased risks of intensive care unit (ICU) admission and mortality respectively, after adjusting for confounders [57, 67]. Racial minority groups are disproportionately impacted by diabetes compared to Whites, and Native Americans have the highest prevalence of diabetes of any racial or ethnic group [68]. Minority populations also experience more diabetes-related complications and worse diabetes outcomes [69]. Diabetes risk and control has been associated with low socioeconomic status and lower educational attainment, which emphasizes the important role of social factors on diabetes risk and management [70, 71]. Food insecurity, a phenomenon more than twice as common in Black and Hispanic households than white households, is also linked to poor glycemic control [72]. Interestingly, Bello-Chavolla et al. found that while diabetes predicted COVID-19 mortality, high BMI mediated 49.5% of this effect, underscoring the relationship between many pre-existing conditions [73].
Body Mass Index and Weight Stigma
High body mass index (BMI) has also been associated with severe disease and death among COVID-19 patients [52, 74]. In 2018, Black adults had the highest age-adjusted prevalence of BMI > 30 k/m2, and Hispanic adults also had age-adjusted prevalence above the national average [75]. In a review on racial disparities in BMI, Byrd and colleagues point to factors related to food deserts and the associated consumption of calorically dense but nutritionally poor foods, residence in neighborhoods with inadequate access to places to be physically active, decreased access to medical care, stress, income, sleep, and racism as drivers of the observed differences among racial and ethnic groups in both the prevalence and management of obesity [76].
With media coverage emphasizing high BMI as a risk factor for severe COVID-19, larger bodied individuals are likely to experience increased weight stigma within and outside of the medical system [77]. Approximately 19–42% of individuals with high BMI report experiencing weight discrimination and 40–50% report internalizing weight bias [78]. Conscious and unconscious bias from medical professionals can create an unwelcoming and at times hostile environment for larger bodied individuals, leading to delays in both COVID and non-COVID-related care due to weight concerns [79]. Weight stigma, which can be internalized as chronic stress, may exacerbate the underlying predisposition toward inflammation and dysregulated immune response, which has been proposed as a mechanism of severe COVID-19 among people with elevated BMI [80–82]. Since minority populations bear a disproportionate burden of the incidence and subsequent health consequences of elevated BMI, it is likely that there is significant intersectionality between race, ethnicity, BMI, and weight stigma with COVID-19 infection and outcomes.
Conclusion
The observed disparities in COVID-19 risk, morbidity, and mortality mirror prior inequalities in disease burden that continue to negatively impact Black and Hispanic persons, particularly those who are older adults. Per the weathering hypothesis, increased exposure to social inequality over the lifecourse places these older minoritized individuals at greater risk for physiological “wear and tear” [9••]. As these physiological disruptions continue, diseases, including COVID-19, can disproportionately harm those who are already vulnerable to poor health outcomes [15, 83]. Understanding the role that structural racism has in shaping the impact of the COVID-19 pandemic is necessary if addressing disparities and preventing further infection and death is the goal for COVID-19 stakeholders. This review highlights the unique challenges that aging minoritized populations face and presents opportunities for addressing the needs of those populations.
Rather than proposing behavioral changes that often fail to address the true sources of population health inequity, we provide local- and state-level recommendations to mitigate the burden of COVID-19 in older Black and Hispanic populations. First, a key to preventing not only the spread but also the fatal impacts of COVID-19 is having proper access to testing, as individuals are made aware of their ability to infect others and are able to seek medical care before symptoms worsen [1]. This could include increasing the number of COVID-19 testing sites in minority communities, creating targeted dissemination efforts to make communities aware of available resources and testing sites, and providing testing to individuals while also limiting barriers such as the cost, the need for health insurance, and the accessibility of results. Second, and related to the issue of testing, is the need for governments to continue to observe COVID-19 disparities through extensive data on the number of confirmed COVID-19 cases, hospitalizations, and deaths across a wide range of sociodemographic categories, while emphasizing that tracking will not result in penalization for persons such as undocumented immigrants [84]. Third, policymakers must recognize that universal policies may not be as universally beneficial as they intend to be. For instance, while Stay-at-Home orders may be issued to prevent further disease spread, some Black and Hispanic individuals, many of whom comprise the frontline and essential workforce, are unable to simply stay at home or socially distance [17]. Policymakers must also ensure that policies do not have inimical effects on older minoritized populations [84, 85]. Fourth, it is imperative that local and state governments address the financial inequalities that existed prior to COVID-19 and have since been exacerbated. These economic challenges may be addressed with adequate and consistent economic relief efforts, which would be especially beneficial to older Black and Hispanic individuals who have lower median wealth than older Whites [86]. Additionally, as vaccines continue to be dispensed throughout the USA, a pattern of disproportionate vaccination has emerged, as Black and Hispanic populations are getting vaccinated at lower rates than White populations, despite having higher rates of cases, hospitalizations, and deaths from COVID-19 [87, 88•]. To ensure that the most at-risk individuals receive the vaccine, equitable vaccine distribution must be prioritized, and efforts must be made to address challenges with vaccine hesitancy and access in these populations.
As researchers, we can support state and local governments in their efforts to address growing racial and ethnic disparities in COVID-19 morbidity and mortality. One approach could be expanding current research on the process of weathering and the health effects of experiencing social inequality over the lifecourse. Such studies would be helpful in illustrating that current COVID-19 disparities are the consequence of inequities that can be at least partially mitigated through policy changes. Moreover, researchers can continue to do research that explores and highlights disparities in COVID-19 morbidity, mortality, and vaccination to further identify at-risk groups and provide support for currently identified at-risk groups. Other efforts could include publishing more data on COVID-19 that is accessible to minoritized and older minoritized populations to help increase knowledge and awareness of COVID-19 while possibly increasing trust and addressing vaccine hesitancy.
Compliance with Ethical Standards
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.COVID-19 overview and infection prevention and control priorities in non-US healthcare settings | CDC. https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/overview/index.html#background. Accessed 4 Feb 2021.
- 2.COVID-19 map - Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/map.html. Accessed 4 Feb 2021.
- 3.COVID-19 provisional counts - weekly updates by select demographic and geographic characteristics. https://www.cdc.gov/nchs/nvss/vsrr/covid_weekly/index.htm. Accessed 4 Feb 2021.
- 4.COVID-19 hospitalization and death by race/ethnicity | CDC. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html. Accessed 4 Feb 2021.
- 5.COVID-19 provisional counts - health disparities. https://www.cdc.gov/nchs/nvss/vsrr/covid19/health_disparities.htm. Accessed 4 Feb 2021.
- 6.•• Alcendor DJ. Racial disparities-associated COVID-19 mortality among minority populations in the US. J Clin Med. 2020;9. 10.3390/jcm9082442An in-depth review and exploration of the potential causes of the observed racial disparities in COVID-19 morbidity and mortality. Medical predisposition and societal and cultural barriers to adequate care among racial and ethnic minorities are highlighted, and comprehensive changes in government policies are recommended to address these health inequities. [DOI] [PMC free article] [PubMed]
- 7.Czeisler MÉ, Tynan MA, Howard ME, et al. Public attitudes, behaviors, and beliefs related to COVID-19, stay-at-home orders, nonessential business closures, and public health guidance — United States, New York City, and Los Angeles, May 5–12, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:751–758. doi: 10.15585/mmwr.mm6924e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Geronimus AT. Black/white differences in the relationship of maternal age to birthweight: a population-based test of the weathering hypothesis. Soc Sci Med. 1996;42. 10.1016/0277-9536(95)00159-X. [DOI] [PubMed]
- 9.Geronimus AT, Hicken M, Keene D, et al. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health. 2006;96:826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klemera P, Doubal S. A new approach to the concept and computation of biological age. Mech Ageing Dev. 2006;127. 10.1016/j.mad.2005.10.004. [DOI] [PubMed]
- 11.McEwen BS, Seeman T. Protective and damaging effects of mediators of stress. Elaborating and testing the concepts of allostasis and allostatic load. In: Annals of the New York Academy of Sciences; 1999. 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed]
- 12.Geronimus AT, Hicken MT, Pearson JA, et al. Do US black women experience stress-related accelerated biological aging?: a novel theory and first population-based test of black-white differences in telomere length. Hum Nat. 2010;21. 10.1007/s12110-010-9078-0. [DOI] [PMC free article] [PubMed]
- 13.Juster RP, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci Biobehav Rev 2010;35:2–16. doi:10.1016/j.neubiorev.2009.10.002 [DOI] [PubMed]
- 14.Quiñones AR, Botoseneanu A, Markwardt S, et al. Racial/ethnic differences in multimorbidity development and chronic disease accumulation for middle-aged adults. PLoS ONE. 2019;14. 10.1371/journal.pone.0218462. [DOI] [PMC free article] [PubMed]
- 15.Garcia MA, Homan PA, García C, et al. The color of COVID-19: structural racism and the disproportionate impact of the pandemic on older Black and Latinx adults. The Journals of Gerontology: Series B Published Online First. 2020. 10.1093/geronb/gbaa114. [DOI] [PMC free article] [PubMed]
- 16.Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. J Am Med Assoc. 2020;323:2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The Lancet. The plight of essential workers during the COVID-19 pandemic. Lancet. 2020;395. 10.1016/S0140-6736(20)31200-9. [DOI] [PMC free article] [PubMed]
- 18.Chowkwanyun M, Reed AL. Racial health disparities and Covid-19 — caution and context. N Engl J Med. 2020;383. 10.1056/nejmp2012910. [DOI] [PubMed]
- 19.Bowleg L. We’re not all in this together: on COVID-19, intersectionality, and structural inequality. Am J Public Health. 2020. 10.2105/AJPH.2020.305766. [DOI] [PMC free article] [PubMed]
- 20.Egede LE, Walker RJ. Structural racism, social risk factors, and Covid-19 — a dangerous convergence for Black Americans. N Engl J Med. 2020;383. 10.1056/nejmp2023616. [DOI] [PMC free article] [PubMed]
- 21.Macmadu A, Berk J, Kaplowitz E, et al. COVID-19 and mass incarceration: a call for urgent action. Lancet Public Health. 2020;5. 10.1016/S2468-2667(20)30231-0. [DOI] [PMC free article] [PubMed]
- 22.Spanish professor describes how COVID-19 has affected area’s Hispanic community. http://ocm.auburn.edu/experts/2020/05/261019-hispanic-community.php. Accessed 4 Feb 2021.
- 23.DeSouza F, Parker CB, Spearman-McCarthy EV, et al. Coping with racism: a perspective of COVID-19 church closures on the mental health of African Americans. J Racial Ethn Health Disparities. 2020;8:7–11. doi: 10.1007/s40615-020-00887-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Scharf DP, Mathews KJ, Jackson P, et al. More than Tuskegee: understanding mistrust about research participation. J Health Care Poor Underserved. 2010;21. 10.1353/hpu.0.0323. [DOI] [PMC free article] [PubMed]
- 25.•• Smedley BD, Stith AY, Nelson AR. Unequal treatment: confronting racial and ethnic disparities in health care (with CD). 2003. 10.17226/12875An important and comprehensive review on the inequities in the healthcare system faced by persons of color and their downstream effects, as well as suggestions for education, policy, and research for the future.
- 26.Hughes MM, Saiyed NS, Chen TS. Local-level adult influenza and pneumococcal vaccination disparities: Chicago, Illinois, 2015–2016. Am J Public Health. 2018;108. 10.2105/AJPH.2017.304257. [DOI] [PMC free article] [PubMed]
- 27.Coronavirus vaccine hesitancy in Black and Latinx communities | 2020-12-11 | Relias Media - Continuing Medical Education Publishing. https://www.reliasmedia.com/articles/147327-coronavirus-vaccine-hesitancy-in-black-and-latinx-communities. Accessed 4 Feb 2021.
- 28.U.S. public now divided over whether to get COVID-19 vaccine | Pew Research Center. https://www.pewresearch.org/science/2020/09/17/u-s-public-now-divided-over-whether-to-get-covid-19-vaccine/. Accessed 4 Feb 2021.
- 29.Page KR, Flores-Miller A. Lessons we’ve learned — Covid-19 and the undocumented Latinx community. N Engl J Med. 2021;384. 10.1056/nejmp2024897. [DOI] [PubMed]
- 30.Erfani P, Uppal N, Lee CH, et al. COVID-19 testing and cases in immigration detention centers, April-August 2020. JAMA - J Am Med Assoc. 2020. 10.1001/jama.2020.21473. [DOI] [PMC free article] [PubMed]
- 31.Communities of color at higher risk for health and economic challenges due to COVID-19 | KFF. https://www.kff.org/coronavirus-covid-19/issue-brief/communities-of-color-at-higher-risk-for-health-and-economic-challenges-due-to-covid-19/. Accessed 4 Feb 2021.
- 32.Center for Disease Control. Health equity considerations and racial and ethnic minority groups. In: e-conversion - proposal for a cluster of excellence; 2020.
- 33.COVID-19 claims reimbursement to health care providers and facilities for testing, treatment, and vaccine administration for the uninsured | Official web site of the U.S. Health Resources & Services Administration. https://www.hrsa.gov/CovidUninsuredClaim. Accessed 4 Feb 2021.
- 34.Limitations of the program for uninsured COVID-19 patients raise concerns | KFF. https://www.kff.org/policy-watch/limitations-of-the-program-for-uninsured-covid-19-patients-raise-concerns/. Accessed 4 Feb 2021.
- 35.Samhsa. Double jeopardy: COVID-19 and behavioral health disparities for Black and Latino communities in the U.S. (Submitted by OBHE) percentage of Blacks, Latinos, and people of color by state population, COVID-19 cases, and COVID-19 deaths (Kaiser Family Foundation, CDC, US Census Bureau).
- 36.A Triple Pandemic? The economic impacts of COVID-19 disproportionately affect Black and Hispanic households | Joint Center for Housing Studies. https://www.jchs.harvard.edu/blog/a-triple-pandemic-the-economic-impacts-of-covid-19-disproportionately-affect-black-and-hispanic-households. Accessed 4 Feb 2021.
- 37.Preparing for COVID-19 in nursing homes | CDC. https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care.html. Accessed 4 Feb 2021.
- 38.COVID-19 has claimed the lives of 100,000 long-term care residents and staff | KFF. https://www.kff.org/policy-watch/covid-19-has-claimed-the-lives-of-100000-long-term-care-residents-and-staff/. Accessed 4 Feb 2021.
- 39.Abrams HR, Loomer L, Gandhi A, et al. Characteristics of U.S. nursing homes with COVID-19 cases. J Am Geriatr Soc. 2020;68. 10.1111/jgs.16661. [DOI] [PMC free article] [PubMed]
- 40.He M, Li Y. Fang F. Is there a link between nursing home reported quality and COVID-19 cases? Evidence from California skilled nursing facilities. J Am Med Dir Assoc. 2020;21. 10.1016/j.jamda.2020.06.016. [DOI] [PMC free article] [PubMed]
- 41.Bui DP, See I, Hesse EM, et al. Association between CMS quality ratings and COVID-19 outbreaks in nursing homes — West Virginia, March 17–June 11, 2020. MMWR Morb Mortal Wkly Rep. 2020;69. 10.15585/mmwr.mm6937a5. [DOI] [PMC free article] [PubMed]
- 42.The sex, gender and COVID-19 project | Global Health 50/50. https://globalhealth5050.org/the-sex-gender-and-covid-19-project/. Accessed 4 Feb 2021.
- 43.Sudre CH, Murray B, Varsavsky T, et al. Attributes and predictors of Long-COVID: analysis of COVID cases and their symptoms 1 collected by the Covid Symptoms Study App 2 3 doi: medRxiv preprint. medRxiv. 2020.
- 44.Bhopal SS, Bhopal R. Sex differential in COVID-19 mortality varies markedly by age. Lancet. 2020;396. 10.1016/S0140-6736(20)31748-7. [DOI] [PMC free article] [PubMed]
- 45.Dehingia N, Raj A. Sex differences in COVID-19 case fatality: do we know enough? Lancet Glob Health. 2021;9. 10.1016/S2214-109X(20)30464-2. [DOI] [PMC free article] [PubMed]
- 46.Empower women - it’s 2020, and Black women aren’t even close to equal pay. https://www.empowerwomen.org/en/resources/documents/2020/08/its-2020-and-black-women-arent-even-close-to-equal-pay?lang=en. Accessed 4 Feb 2021.
- 47.On the frontlines at work and at home: the disproportionate economic effects of the coronavirus pandemic on women of color - Center for American Progress. https://www.americanprogress.org/issues/women/reports/2020/04/23/483846/frontlines-work-home/ (accessed 4 Feb 2021).
- 48.Chang MH, Moonesinghe R, Athar HM, et al. Trends in disparity by sex and race/ethnicity for the leading causes of death in the United States-1999-2010. J Public Health Manag Pract. 2016;22. 10.1097/PHH.0000000000000267. [DOI] [PubMed]
- 49.• Obinna DN. Essential and undervalued: health disparities of African American women in the COVID-19 era. Ethnicity and Health Published Online First. 2020. 10.1080/13557858.2020.1843604Review of the structural inequities faced by African American women and the impacts such inequities have on COVID-19 vulnerability, as informed by intersectionality theory. [DOI] [PubMed]
- 50.Berlin DA, Gulick RM, Martinez FJ. Severe Covid-19. N Engl J Med. 2020;383:2451–2460. doi: 10.1056/NEJMcp2009575. [DOI] [PubMed] [Google Scholar]
- 51.Sanyaolu A, Okorie C, Marinkovic A, et al. Comorbidity and its impact on patients with COVID-19. SN Comprehensive Clinical Medicine. 2020;2. 10.1007/s42399-020-00363-4. [DOI] [PMC free article] [PubMed]
- 52.Ong SWX, Young BE, Leo YS, et al. Association of higher body mass index with severe coronavirus disease 2019 (COVID-19) in younger patients. Clin Infect Dis. 2020;71. 10.1093/cid/ciaa548. [DOI] [PMC free article] [PubMed]
- 53.Simons RL, Lei MK, Klopack E, et al. Racial discrimination, inflammation, and chronic illness among African American women at midlife: support for the weathering perspective. Journal of Racial and Ethnic Health Disparities Published Online First. 2020. 10.1007/s40615-020-00786-8. [DOI] [PMC free article] [PubMed]
- 54.Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10. 10.1016/j.arr.2011.03.003. [DOI] [PubMed]
- 55.Salive ME. Multimorbidity in older adults. Epidemiol Rev. 2013;35. 10.1093/epirev/mxs009. [DOI] [PubMed]
- 56.Wang X, Fang X, Cai Z, et al. Comorbid chronic diseases and acute organ injuries are strongly correlated with disease severity and mortality among COVID-19 patients: a systemic review and meta-analysis. Research. 2020:2020. 10.34133/2020/2402961. [DOI] [PMC free article] [PubMed]
- 57.• Barrera FJ, Shekhar S, Wurth R, et al. Prevalence of diabetes and hypertension and their associated risks for poor outcomes in Covid-19 Patients. J Endoc Soc. 2020;4. 10.1210/jendso/bvaa102Thorough review of 65 observational studies examining the impact of diabetes and hypertension on Covid-19 patients. [DOI] [PMC free article] [PubMed]
- 58.Oetjens MT, Luo JZ, Chang A, et al. Electronic health record analysis identifies kidney disease as the leading risk factor for hospitalization in confirmed COVID-19 patients. PLoS ONE. 2020;15. 10.1371/journal.pone.0242182. [DOI] [PMC free article] [PubMed]
- 59.Henry BM, Lippi G. Chronic kidney disease is associated with severe coronavirus disease 2019 (COVID-19) infection. Int Urol Nephrol. 2020;52. 10.1007/s11255-020-02451-9. [DOI] [PMC free article] [PubMed]
- 60.Ferdinand KC, Yadav K, Nasser SA, et al. Disparities in hypertension and cardiovascular disease in blacks: the critical role of medication adherence. J Clin Hypertens. 2017;19. 10.1111/jch.13089. [DOI] [PMC free article] [PubMed]
- 61.Ostchega Y, Fryar CD, Nwankwo T, et al. Hypertension prevalence among adults aged 18 and over: United States, 2017-2018. NCHS data brief. 2020. [PubMed]
- 62.Novick TK, Rizzolo K, Cervantes L. COVID-19 and kidney disease disparities in the United States. Adv Chronic Kidney Dis. 2020;27. 10.1053/j.ackd.2020.06.005. [DOI] [PMC free article] [PubMed]
- 63.Lariscy JT, Tasmim S, Collins S. Racial and ethnic disparities in health. In: Encyclopedia of gerontology and population aging: Springer International Publishing; 2020. p. 1–9. 10.1007/978-3-319-69892-2_999-1.
- 64.Crews DC, Liu Y, Boulware LE. Disparities in the burden, outcomes, and care of chronic kidney disease. Curr Opin Nephrol Hypertens. 2014;23. 10.1097/01.mnh.0000444822.25991.f6. [DOI] [PMC free article] [PubMed]
- 65.Thorpe RJ, Fesahazion RG, Parker L, et al. Accelerated health declines among African Americans in the USA. J Urban Health. 2016;93. 10.1007/s11524-016-0075-4. [DOI] [PMC free article] [PubMed]
- 66.Forde AT, Sims M, Muntner P, et al. Discrimination and hypertension risk among African Americans in the Jackson Heart Study. Hypertension Published Online First. 2020. 10.1161/HYPERTENSIONAHA.119.14492. [DOI] [PMC free article] [PubMed]
- 67.Mantovani A, Byrne CD, Zheng MH, et al. Diabetes as a risk factor for greater COVID-19 severity and in-hospital death: a meta-analysis of observational studies. Nutr Metab Cardiovasc Dis. 2020;30. 10.1016/j.numecd.2020.05.014. [DOI] [PMC free article] [PubMed]
- 68.Addressing health disparities in diabetes | Diabetes | CDC. https://www.cdc.gov/diabetes/disparities.html. Accessed 4 Feb 2021.
- 69.Walker RJ, Strom Williams J, Egede LE. Influence of race, ethnicity and social determinants of health on diabetes outcomes. Am J Med Sci. 2016;351. 10.1016/j.amjms.2016.01.008. [DOI] [PMC free article] [PubMed]
- 70.Agardh E, Allebeck P, Hallqvist J, et al. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 2011;40. 10.1093/ije/dyr029. [DOI] [PubMed]
- 71.Saydah S, Lochner K. Socioeconomic status and risk of diabetes-related mortality in the U. S Public Health Reports. 2010;125. 10.1177/003335491012500306. [DOI] [PMC free article] [PubMed]
- 72.USDA ERS - household food security in the United States in 2016. https://www.ers.usda.gov/publications/pub-details/?pubid=84972. Accessed 4 Feb 2021.
- 73.Bello-Chavolla OY, Bahena-López JP, Antonio-Villa NE, et al. Predicting mortality due to SARS-CoV-2: a mechanistic score relating obesity and diabetes to COVID-19 outcomes in Mexico. J Clin Endocrinol Metab. 2020;105. 10.1210/clinem/dgaa346. [DOI] [PMC free article] [PubMed]
- 74.Garibaldi BT, Fiksel J, Muschelli J, et al. Patient trajectories among persons hospitalized for COVID-19. Ann Intern Med. 2021:174. 10.7326/m20-3905. [DOI] [PMC free article] [PubMed]
- 75.Hales CM, Carroll MD, Fryar CD, et al. Prevalence of obesity and severe obesity among adults: United States, 2017-2018. NCHS data brief. 2020. [PubMed]
- 76.Byrd AS, Toth AT, Stanford FC. Racial disparities in obesity treatment. Curr Obes Rep. 2018;7. 10.1007/s13679-018-0301-3. [DOI] [PMC free article] [PubMed]
- 77.Covid-19 does not discriminate by body weight | WIRED. https://www.wired.com/story/covid-19-does-not-discriminate-by-body-weight/. Accessed 4 Feb 2021.
- 78.Rubino F, Puhl RM, Cummings DE, et al. Joint international consensus statement for ending stigma of obesity. Nat Med. 2020;26:485–497. doi: 10.1038/s41591-020-0803-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Olson CL, Schumaker HD, Yawn BP. Overweight women delay medical care. Arch Fam Med. 1994;3. 10.1001/archfami.3.10.888. [DOI] [PubMed]
- 80.Sanchis-Gomar F, Lavie CJ, Mehra MR, et al. Obesity and outcomes in COVID-19: when an epidemic and pandemic collide. Mayo Clin Proc. 2020;95. 10.1016/j.mayocp.2020.05.006. [DOI] [PMC free article] [PubMed]
- 81.Sattar N, McInnes IB, McMurray JJV. Obesity is a risk factor for severe COVID-19 infection: multiple potential mechanisms. Circulation. 2020. 10.1161/CIRCULATIONAHA.120.047659. [DOI] [PubMed]
- 82.Chiappetta S, Sharma AM, Bottino V, et al. COVID-19 and the role of chronic inflammation in patients with obesity. Int J Obes. 2020;44. 10.1038/s41366-020-0597-4. [DOI] [PMC free article] [PubMed]
- 83.Ajilore O, Thames AD. The fire this time: the stress of racism, inflammation and COVID-19. Brain Behav Immun. 2020;88:66–67. doi: 10.1016/j.bbi.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Poteat T, Millett GA, Nelson LRE, et al. Understanding COVID-19 risks and vulnerabilities among black communities in America: the lethal force of syndemics. Ann Epidemiol. 2020;47:1–3. doi: 10.1016/j.annepidem.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Turner-Musa J, Ajayi O, Kemp L. Examining social determinants of health, stigma, and COVID-19 disparities. Healthcare. 2020;8:168. doi: 10.3390/healthcare8020168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.The Fed - disparities in wealth by race and ethnicity in the 2019 survey of consumer finances. https://www.federalreserve.gov/econres/notes/feds-notes/disparities-in-wealth-by-race-and-ethnicity-in-the-2019-survey-of-consumer-finances-20200928.htm. Accessed 4 Feb 2021.
- 87.Painter EM, Ussery EN, Patel A, et al. Demographic characteristics of persons vaccinated during the first month of the COVID-19 vaccination program — United States, December 14, 2020–January 14, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:174–177. doi: 10.15585/mmwr.mm7005e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.• Latest data on COVID-19 vaccinations race/ethnicity | KFF. https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-covid-19-vaccinations-cases-deaths-race-ethnicity/. Accessed 5 Feb 2021. Important report showing emerging disparities in COVID-19 vaccination rates by race/ethnicity, with Black and Hispanic individuals receiving less vaccinations than Whites. The report acknowledges limitations including a large amount of missing data.