Abstract
BACKGROUND AND PURPOSE:
Although blood pressure reduction has been postulated to result in a fall in cerebral perfusion pressure in patients with intracerebral hemorrhage, the latter is rarely measured. We assessed regional cerebral perfusion pressure in patients with intracerebral hemorrhage by using CT perfusion source data.
MATERIALS AND METHODS:
Patients with acute primary intracerebral hemorrhage were randomized to target systolic blood pressures of <150 mm Hg (n = 37) or <180 mm Hg (n = 36). Regional maps of cerebral blood flow, cerebral perfusion pressure, and cerebrovascular resistance were generated by using CT perfusion source data, obtained 2 hours after randomization.
RESULTS:
Perihematoma cerebral blood flow (38.7 ± 11.9 mL/100 g/min) was reduced relative to contralateral regions (44.1 ± 11.1 mL/100 g/min, P = .001), but cerebral perfusion pressure was not (14.4 ± 4.6 minutes−1 versus 14.3 ± 4.8 minutes−1, P = .93). Perihematoma cerebrovascular resistance (0.34 ± 0.11 g/mL) was higher than that in the contralateral region (0.30 ± 0.10 g/mL, P < .001). Ipsilateral and contralateral cerebral perfusion pressure in the external (15.0 ± 4.6 versus 15.6 ± 5.3 minutes−1, P = .15) and internal (15.0 ± 4.8 versus 15.0 ± 4.8 minutes−1, P = .90) borderzone regions were all similar. Borderzone cerebral perfusion pressure was similar to mean global cerebral perfusion pressure (14.7 ± 4.7 minutes−1, P ≥ .29). Perihematoma cerebral perfusion pressure did not differ between blood pressure treatment groups (13.9 ± 5.5 minutes−1 versus 14.8 ± 3.4 minutes−1, P = .38) or vary with mean arterial pressure (r = −0.08, [−0.10, 0.05]).
CONCLUSIONS:
Perihematoma cerebral perfusion pressure is maintained despite increased cerebrovascular resistance and reduced cerebral blood flow. Aggressive antihypertensive therapy does not affect perihematoma or borderzone cerebral perfusion pressure. Maintenance of cerebral perfusion pressure provides physiologic support for the safety of blood pressure reduction in intracerebral hemorrhage.
Patients with intracerebral hemorrhage (ICH) most often present with elevated blood pressure (BP), but acute treatment remains controversial.1,2 Despite the results of recent randomized controlled trials of BP management demonstrating no excess of adverse clinical events,3,4 many physicians are reluctant to aggressively use antihypertensive agents in the acute phase of ICH. This relucence is primarily based on persisting theoretic concerns that there is a zone of tissue at risk for ischemic injury surrounding the acute hematoma.5 In addition, more recent MR imaging studies have suggested that subacute ischemic injury occurs in areas remote from the hematoma, including borderzone (BZ, also known as watershed) regions.6–11 The etiology of these ischemic injuries has been postulated to be hemodynamic compromise secondary to BP reduction.10 Studies of CBF in the perihematoma region indicate that this region is relatively hypoperfused, but not severely enough to result in ischemia.12–14 Previous PET studies have demonstrated that the perihematoma region is, in fact, hypometabolic, likely secondary to the primary brain injury, and that the oxygen extraction fraction is not elevated, indicating the absence of misery perfusion.12,15 Nonetheless, it is possible that reduction of BP will result in a fall in cerebral perfusion pressure (CPP), subsequently precipitating ischemia.16 In the Intracerebral Hemorrhage Acutely Decreasing Arterial Pressure Trial (ICH ADAPT), we demonstrated that acute BP reduction is not associated with a significant fall in CBF.17 It has been demonstrated, however, that CPP is more sensitive than CBF or CBV to changes in blood pressure.18 The relationship between CPP and BP reduction in patients with intracerebral hemorrhage is unknown.
Global CPP is normally calculated as the difference between the mean arterial pressure and intracranial pressure, which requires insertion of an intraventricular manometer. Monitoring of intracranial pressure and CPP is generally reserved for patients with a decreased level of consciousness and/or obstructive hydrocephalus requiring ventricular drainage. In these cases, current consensus guidelines recommend that BP be titrated to ensure that CPP is between 50 and 70 mm Hg.19,20 In addition, global CPP may not reflect local variations in intracranial pressure due to the mass effect of a hematoma, particularly in small hematomas.21 Measurements of regional CPP might inform clinical BP management decisions. With PET, it has been demonstrated that CPP can be calculated as a ratio of CBF to CBV.18 We adapted this technique by using CTP source data from ICH ADAPT to assess local CPP in acute ICH. We tested the hypothesis that aggressive antihypertensive therapy reduces CPP in the perihematoma and borderzone regions.
Materials and Methods
Patients
The ICH ADAPT protocol (clinicaltrials.gov, NCT00963976) has been published previously.4 Briefly, patients 18 years of age or older presenting with acute primary (spontaneous) ICH diagnosed on noncontrast CT within 24 hours of symptom onset were prospectively enrolled. Exclusion criteria included evidence of secondary ICH (ie, related to underlying tumors, arteriovenous malformations, or drug use), planned surgical resection, contraindications to BP reduction or an indication for urgent reduction, or inability to undergo CTP imaging. A standardized antihypertensive treatment protocol was applied with the sequential use of labetalol, hydralazine, and IV enalapril. Informed consent was obtained from each patient or an authorized representative, and the human ethics committees at each site approved the study protocol.
Imaging Protocol
Two hours after randomization, all patients underwent a standard repeat noncontrast CT scan of the brain. The scan consisted of 5-mm sections (120 KV[peak], 300 mA per section) through the entire brain (18–20 sections with a 512 × 512 matrix). Due to differences in CT scanner capabilities between sites, a variable 38- to 80-mm-thick section was selected to assess perfusion (CTP) centered over the section where the hematoma had the greatest diameter on noncontrast CT. Intravenous iodinated contrast (40 mL) was administered at 4–7 mL/s via an 18-ga angiocatheter in an antecubital vein. CTP images were acquired every 1 second for 50 seconds (80 KV[p], 200 mA per image), and all sections were 5-mm-thick. All patients had a repeat NCCT scan at 24 ± 3 hours.
Image Processing and Analysis
Raw contrast-enhanced CT images were imported into the PerfScape analysis package (2.0 CT Edition; Olea Medical, La Ciotat, France) software. An arterial input function was manually selected over the contralateral anterior cerebral artery, while the venous output function was obtained over the confluence of the sinuses. Perfusion maps were derived from the tissue time-attenuation curve on the basis of the change in x-ray attenuation, which is linearly related to iodinated contrast concentration on a per-voxel basis with time. Errors introduced by delay and dispersion of the contrast bolus before arrival in the cerebral circulation were corrected for by using a block-circulant deconvolution algorithm.22 Quantitative perfusion indices, including CBF and CBV, were calculated on a voxelwise basis and used to generate color-coded maps.
All perfusion maps were transferred to the Analyze 11.0 software package (AnalyzeDirect, Overland Park, Kansas).23 Maps of CPP and cerebrovascular resistance (CVR) were generated by using a voxelwise calculation of CBF/CBV and 1/CBV, respectively (Fig 1), as previously described.18 The perimeter of the hematoma was outlined on the precontrast arrival CT source image by using a semiautomated intensity Hounsfield unit threshold technique, as previously described.24 Internal and external BZ and 7-mm perihematoma ROIs were manually outlined (Fig 1). In cases in which the hematoma itself involved a BZ, the latter was not outlined. All voxels containing blood vessels were removed from the ROI by using an intensity-threshold function. On the basis of previous studies, voxels with CBF of >100 mL/100 g/min or CBV of >8 mL/100 g were assumed to contain vessels and removed from the ROI.25–27 Mean perfusion indices were measured in all ROIs, contralateral homologous regions, and the entire hemispheres (excluding the hematoma) ipsilateral and contralateral to the hematoma.
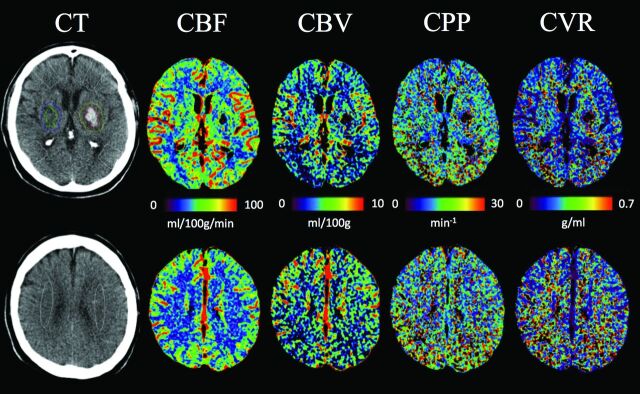
Fig 1.
Examples of CT perfusion source data with perihematoma and external and internal borderzone ROIs. Maps of cerebral blood flow, cerebral blood volume, cerebral perfusion pressure, and cerebrovascular reserve at 2 different sections from a patient in the <180-mm Hg treatment group.
Statistical Analysis
Statistical analysis was performed by using SPSS Statistics 21.0 2008 (IBM, Armonk, New York). Differences in perfusion parameters were assessed with paired t tests. Linear regression was used to assess the relationship between the perfusion parameters and blood pressure. Differences in perfusion parameters between treatment groups were assessed with independent-samples t tests.
Results
Patient Characteristics and Outcomes
Seventy-five patients were randomized in ICH ADAPT.17 Two patients were excluded from this analysis due to inadequate quality of raw CTP data required to complete CPP and CVR calculations. This study, therefore, included 73 patients (54 men), with a median age of 70 years (interquartile range, 60–80 years). Hematoma locations were as follows: 55 basal ganglia, 17 lobar, and 1 posterior fossa. Median time from symptom onset to CTP imaging was 9.8 hours (interquartile range, 6.0–19.2 hours), and from the acute diagnostic CT to the CTP study, it was 4.8 hours (interquartile range, 3.4–14.5 hours). The delay between the diagnostic CT and randomization was variable with a median of 2.3 hours (interquartile range, 1.0–11.6 hours). Four patients in each treatment arm had antithrombotic-associated ICH (either antiplatelet or anticoagulant; Table 1).
Table 1:
Baseline characteristics and outcomes of randomized patientsa
| Characteristic | <150-mm Hg Target (n = 37) | <180-mm Hg Target (n = 36) | P Value |
|---|---|---|---|
| Age (yr) | 71.0 ± 12.5 | 68.7 ± 11.1 | .40 |
| Male | 26 (70%) | 28 (78%) | .47 |
| Symptom onset to randomization (hr) | 10.5 ± 7.4 | 9.7 ± 7.0 | .65 |
| Medical history | |||
| Hypertension | 26 (70%) | 27 (75%) | .71 |
| Previous ICH | 4 (11%) | 1 (3%) | .19 |
| Antiplatelet/anticoagulation | 4 (11%) | 4 (11%) | .74 |
| Ischemic stroke | 6 (16%) | 2 (6%) | .17 |
| Clinical characteristics | |||
| Systolic BP (mm Hg) | 182 ± 20 | 184 ± 25 | .66 |
| Diastolic BP (mm Hg) | 94 ± 19 | 97 ± 23 | .53 |
| Mean arterial pressure (mm Hg) | 123 ± 17 | 126 ± 22 | .54 |
| Glasgow Coma Scale | 13.3 ± 2.7 | 13.9 ± 1.9 | .27 |
| NIHSS score | 12.3 ± 7.7 | 11.5 ± 6.3 | .64 |
| Hematoma characteristics | |||
| Basal ganglia | 28 (76%) | 27 (75%) | .99 |
| Lobar | 9 (24%) | 8 (22%) | |
| Cerebellum | 0 (0%) | 1 (3%) | |
| Intraparenchymal volume (mL) | 24.5 ± 28.9 | 22.61 ± 21.35 | .75 |
| Intraventricular volume (mL) | 2.20 ± 6.26 | 4.25 ± 8.78 | .26 |
| Total ICH volume (mL) | 26.68 ± 31.50 | 26.86 ± 25.24 | .98 |
| Antihypertensive therapyb | |||
| Labetalol (No.) (mean dose ± SD in mg) | 34 (38 ± 25) | 16 (29 ± 25) | |
| Hydralazine (No.) (mean dose ± SD in mg) | 18 (22 ± 14) | 5 (14 ± 8) | |
| IV enalapril (No.) (mean dose ± SD in mg) | 9 (1.25 ± 0) | 3 (1.25 ± 0) | |
| Outcomes | |||
| Mortality (No.) (%) | 7 (19) | 4 (11) | .52 |
| Modified Rankin Scale score (median) (IQR) | 3 (1.5–5.5) | 4 (2–5) | .43 |
| Hematoma growth >6 mL (No.) (%) | 8 (21) | 8 (22) | .86 |
Note:—IQR indicates interquartile range.
Data are means unless otherwise specified.
Nineteen patients in the <150-mm Hg group and 2 patients in the <180-mm Hg group received multiple antihypertensives.
The mean systolic and diastolic BP at the time of the CTP scan was 150 ± 20 and 77 ± 15 mm Hg, respectively. The number of patients receiving each of the 3 antihypertensive therapies along with the mean dose is recorded in Table 1. The median acute Glasgow Coma Scale and NIHSS scores were 15 (range, 4–15; interquartile range, 13–15) and 10 (range, 1–35; interquartile range, 6–17), respectively.
The mean intraparenchymal hematoma volume at the time of CTP imaging was 23.9 ± 28.3 mL. Follow-up imaging was performed at a median of 21.8 hours (interquartile range, 21–23.7 hours) later. Mean hematoma volume at that time was 25.5 ± 27.3 mL. Eleven patients (15%) had large-volume ICHs, with hematoma volumes of >40 mL. Hematoma expansion of >6 mL was seen in 16 patients (8 in each treatment group, P = .86). Thirty-seven patients were randomized to a target BP of <150 mm Hg, and 36, to a target BP of <180 mm Hg. No significant differences in patient characteristics were seen between the treatment groups (Table 1).
There were no differences in any clinical outcome events between the 2 groups (Table 1). Mortality was 19% in the 150-mm Hg treatment group and 11% in the 180-mm Hg treatment group (P = .52). Functional disability as measured by the modified Rankin Scale score was comparable between the 150-mm Hg (median, 3 mm Hg; interquartile range, 1.5–5.5 mm Hg) and 180-mm Hg (median, 4 mm Hg; interquartile range, 2–5 mm Hg) treatment groups (P = .43). No patient in the trial had an ischemic lesion on 24-hour follow-up CT.
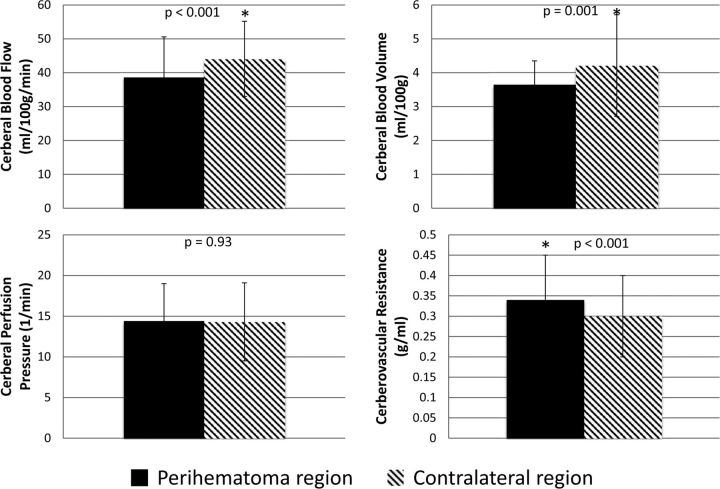
Cerebral Blood Flow and Volume
Mean perihematoma CBF in all 73 patients (38.7 ± 11.9 mL/100 g/min; Fig 2) was significantly lower than that in contralateral homologous regions (44.1 ± 11.1 mL/100 g/min, P < .001). Mean ipsilateral hemispheric CBF (42.1 ± 10.5 mL/100 g/min) was lower than that in the contralateral hemisphere (43.4 ± 10.5 mL/100 g/min, P < .001).
Fig 2.
Mean (±SD) perihematoma and contralateral homologous region cerebral blood flow, cerebral blood volume, cerebral perfusion pressure, and cerebrovascular reserve.
There was a reduction in perihematoma CBV (3.65 ± 0.70 mL/100 g; Fig 2) compared with the contralateral regions (4.21 ± 1.53 mL/100 g, P = .001). Mean ipsilateral hemispheric CBV (3.83 ± 0.63 mL/100 g) was lower than that in the contralateral hemisphere (3.88 ± 0.64 mL/100 g, P = .033).
Cerebral Perfusion Pressure and Cerebrovascular Resistance
Perihematoma CPP (14.4 ± 4.6 minutes−1) was similar to that in contralateral homologous regions (14.3 ± 4.8 minutes−1, P = .93; Fig 2). Ipsilateral hemispheric CPP (14.6 ± 4.6 minutes−1) was also comparable with that in the contralateral hemispheric CPP (14.8 ± 4.9 minutes−1, P = .28). There were no differences in CPP within the ipsilateral and contralateral external (15.0 ± 4.6 and 15.6 ± 5.3 minutes−1, respectively; P = .15) or ipsilateral and contralateral internal (15.0 ± 4.8 and 15.0 ± 4.8 minutes−1, respectively; P = .90) BZ regions. Similarly, there were no significant differences when the CPP in the above ipsilateral and contralateral external and internal BZ regions was compared with the mean bilateral hemispheric CPP (14.7 ± 4.7 minutes−1, P ≥ .29; Table 2). On linear regression analysis, CPP was not related to intraparenchymal hematoma volume (β = −0.001 [−0.002, 0.001]).
Table 2:
Effect of BP reduction on perfusion parameters
| Perfusion Parameters and Region | Treatment Group |
P Value | |
|---|---|---|---|
| <150 mm Hg (n = 37) | <180 mm Hg (n = 36) | ||
| Absolute ipsilateral CPP | |||
| Perihematoma | 13.9 ± 5.5 | 14.8 ± 3.4 | .38 |
| Hemisphere | 14.0 ± 5.3 | 15.2 ± 3.9 | .27 |
| External BZ | 14.1 ± 4.6 | 15.8 ± 4.6 (n = 35) | .11 |
| Internal BZ | 13.5 ± 4.6 (n = 27) | 16.5 ± 4.7 (n = 29) | .02a |
| Absolute contralateral CPP | |||
| Perihematoma | 13.9 ± 5.5 | 14.8 ± 4.0 | .43 |
| Hemisphere | 14.3 ± 5.8 | 15.2 ± 3.8 | .45 |
| External BZ | 15.1 ± 6.5 | 16.0 ± 3.7 (n = 35) | .46 |
| Internal BZ | 15.0 ± 7.1 (n = 27) | 16.0 ± 4.6 (n = 29) | .48 |
| Absolute ipsilateral CVR | |||
| Perihematoma | 0.32 ± 0.10 | 0.36 ± 0.11 | .11 |
| Hemisphere | 0.29 ± 0.08 | 0.32 ± 0.08 | .14 |
| External BZ | 0.31 ± 0.11 | 0.37 ± 0.12 (n = 35) | .05a |
| Internal BZ | 0.37 ± 0.13 (n = 27) | 0.44 ± 0.16 (n = 29) | .08 |
| Absolute contralateral CVR | |||
| Perihematoma | 0.28 ± 0.09 | 0.33 ± 0.11 | .56 |
| Hemisphere | 0.28 ± 0.08 | 0.32 ± 0.09 | .09 |
| External BZ | 0.32 ± 0.11 | 0.38 ± 0.12 (n = 35) | .04a |
| Internal BZ | 0.36 ± 0.12 (n = 27) | 0.40 ± 0.14 (n = 29) | .16 |
| Relative CPP | |||
| Perihematoma | 1.02 ± 0.16 | 1.02 ± 0.15 | .96 |
| Hemisphere | 0.99 ± 0.09 | 1.00 ± 0.10 | .75 |
| External BZ | 0.99 ± 0.19 | 1.00 ± 0.26 (n = 35) | .76 |
| Internal BZ | 1.01 ± 0.17 (n = 27) | 1.01 ± 0.16 (n = 29) | .99 |
| Relative CVR | |||
| Perihematoma | 1.16 ± 0.23 | 1.11 ± 0.17 | .36 |
| Hemisphere | 1.04 ± 0.10 | 1.02 ± 0.08 | .32 |
| External BZ | 1.01 ± 0.18 | 1.01 ± 0.22 (n = 35) | .91 |
| Internal BZ | 1.02 ± 0.17 (n = 27) | 1.04 ± 0.15 (n = 29) | .52 |
Significant.
Mean perihematoma CVR (0.34 ± 0.11 g/mL) was slightly higher than that in contralateral homologous regions (0.30 ± 0.10 g/mL, P < .001; Fig 2). Ipsilateral hemispheric CVR was also elevated (0.31 ± 0.08) relative to the contralateral hemisphere (0.30 ± 0.09 g/mL, P = .04). There were no hemispheric differences in CVR within the external (0.34 ± 0.12 versus 0.35 ± 0.12 g/mL, P = .53) or internal (0.41 ± 0.15 versus 0.39 ± 0.14 g/mL, P = .17) BZ regions.
Effect of Blood Pressure Treatment on Cerebral Perfusion Pressure and Cerebrovascular Resistance
At the time of CTP imaging, systolic BP was significantly lower in the <150-mm Hg target group (140 ± 19 mm Hg) than that in the <180-mm Hg target group (162 ± 12 mm Hg, P < .001). Mean CPP and CVR in the perihematoma and most BZ regions was similar between BP treatment groups (Table 2). Mean CPP in the ipsilateral internal BZ (13.5 ± 4.6 minutes−1) in the <150-mm Hg group was lower than that in the <180-mm Hg group (16.5 ± 4.7 minutes−1, P = .02; Table 2). Mean CVR in the contralateral internal BZ (0.32 ± 0.11 g/mL) in the <150-mm Hg group was lower than that in the <180-mm Hg group (0.38 ± 0.12 g/mL, P = .04; Table 2).
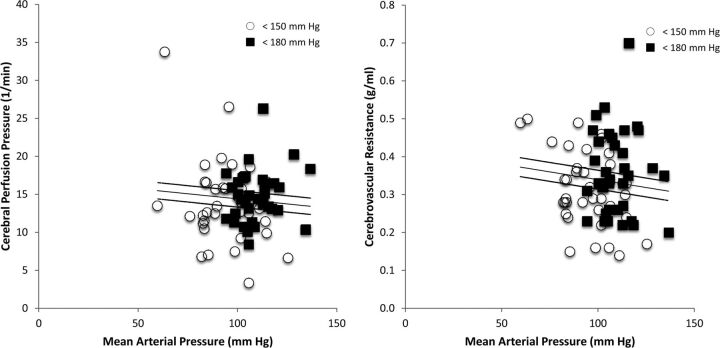
There was no relationship between perihematoma CPP and BP in all patients at the time of the CTP scan (systolic BP, β = −0.04 [−0.07, 0.05]; diastolic BP, β = −0.10 [−0.11, 0.04]); or mean arterial pressure, β = −0.08 [−0.10, 0.05]; Fig 3). Similarly, perihematoma CVR was unrelated to BP at the time of the CTP scan (systolic BP, β = −0.10 [−0.002, 0.001]; diastolic BP, β = −0.10 [−0.002, 0.001]); or mean arterial pressure (β = −0.11 [−0.003, 0.001], Fig 3).
Fig 3.
Plots of cerebral perfusion pressure and cerebrovascular resistance against mean arterial pressure. The open circles refer to the <150-mm Hg treatment group, while the filled squares represent the <180-mm Hg treatment group. There was no relationship between mean arterial pressure and CPP (β = −0.08 [−0.10, 0.05]) or CVR (β = −0.11 [−0.003, 0.001]).
Discussion
This assessment of local cerebral perfusion pressure and cerebrovascular resistance in patients with acute primary intracerebral hemorrhage indicates that CPP is maintained in all potentially hemodynamically vulnerable regions. There is also a slight increase in CVR within the perihematoma region. Neither CPP nor CVR appear to be affected by acute BP reduction.
Cerebral Perfusion Pressure Assessment
Changes in CPP are relevant to the management of BP in patients with acute ICH, though measurement of CPP in patients with ICH is challenging. In this study, we adapted the method originally described by Schumann et al (1998)18 to estimate regional CPP on the basis of positron-emission tomography–derived measurements of CBF. In a primate model of cerebral ischemia, these authors demonstrated that CPP is strongly correlated with mean arterial pressure, the major physiologic determinant of CPP in patients with vascular insults. In fact, CPP (or the CBF/CBV ratio) was shown to be more sensitive to slight variations in mean arterial pressure compared with individual measurements of CBF or CBV.18 These data indicated that blood pressure reduction did not have a subtle effect on CPP, which may not have been evident on the more conventional measures of CBF and CBV alone at this single point in time. Although PET and CTP differ with respect to tracer kinetics (diffusible versus nondiffusible), the physiologic data are comparable both qualitatively and quantitatively,28 permitting application of the method described by Schumann et al to both perfusion imaging modalities. Additionally, intermittent CTP studies in severe traumatic head injuries have been shown to provide additional information with respect to preservation of autoregulation compared with continuous CPP measurements.29 Thus, CPP measured by noninvasive imaging techniques may be of particular interest in patients with traumatic brain injuries.
Perihematoma Perfusion Pressure
Our results and those of a PET study completed in patients with acute ICH12 confirm that CBF and CBV are modestly reduced in the perihematoma region. Although estimates of CPP and CVR were not included in the PET studies, these parameters could, in fact, be derived from source data in the same manner as that described by Schumman et al (1998).18 The elevated CVR within the perihematoma region is presumably secondary to compression of the microvasculature by the space-occupying effect of the hematoma and edema. Maintenance of CPP suggests that this increase in CVR is not responsible for the reduction in CBF, however. Both direct (PET) and indirect (CTP) measurements of oxygen metabolism suggest that CBF reduction is related to decreased metabolic demand within the perihematoma region.12,15,30
Blood Pressure and Perihematoma Perfusion Pressure
We have previously demonstrated that acute BP reduction does not result in reduced perihematoma CBF in patients with acute ICH.15,17,31 In the present study, we found no relationship between BP treatment target or actual BP and perihematoma CPP. The maintenance of CPP despite marked reductions in BP in many of our patients suggests some preservation of autoregulation in patients with acute ICH. This is consistent with serial measurements of CBF pre- and post-BP reduction by using both PET and CTP.15,31
Borderzone Cerebral Perfusion Pressure
Our CPP measurements may be relevant to the results of diffusion-weighted MR imaging studies indicating that subacute ischemic injury occurs in areas remote from the hematoma, including BZ regions, in up to one-third of patients with acute ICH.6–11 The retrospective association shown between BP reduction in the setting of chronic hypertensive vasculopathy and these ischemic lesions raises the possibility that they are a consequence of hemodynamic compromise. Given that CPP has been shown to be more sensitive to slight variations in mean arterial pressure than individual measurements of CBF or CBV,18 we postulated that subtle perfusion changes in the BZ regions may only become apparent by using this analysis. External and internal BZ CPP was not different from that in surrounding hemispheric tissue and did not vary between the ipsilateral and contralateral hemispheres. The modest reduction in the absolute CPP in the ipsilateral internal BZ in the <150-mm Hg treatment group is of dubious clinical significance, particularly given the lack of difference in relative CPP. Furthermore, the slight decrease in ipsilateral CPP in our more aggressive BP target group is an unlikely mechanism for DWI lesion formation, which has been reported with equal frequency in both the ipsilateral and contralateral hemispheres.10 Very recent research suggests that the small DWI lesions outside the perihematoma region are associated with larger hematoma volumes. The precise etiology of these lesions is unknown, though they may represent an epiphenomenon with an underlying microvascular pathogenesis rather than a hemodynamic mechanism of ischemic injury after primary ICH.32 Nonetheless, the possibility that very localized hemodynamic changes, including variations in CPP, are related to the development of these small DWI lesions cannot be excluded on the basis of our results.
Clinical Implications
Our findings are consistent with those in previous studies of perfusion in patients with acute ICH, suggesting that acute BP reduction is safe. These data are also consistent with the lack of indicators of clinical harm in randomized trials of BP reduction after ICH.17,33,34 Although concerns persist that BZ regions may be hemodynamically vulnerable to rapid BP reduction, we can find no objective evidence to support this hypothesis. We are currently testing the hypothesis that BP reduction is associated with the development of MR imaging ischemic lesions as part of an ongoing randomized trial (NCT02281838).
Limitations
This study has a number of limitations. Regional CPP was measured indirectly, but noninvasively, by using the ratio of CBF to CBV maps. Global CPP has been correlated with the CBF/CBV ratio,18 but regional evaluation of CPP by using CTP has not been confirmed with direct measurements of intracranial pressure. Invasive intracranial pressure measurements were not included in this study; consequently, our noninvasive, indirect measurements of CPP cannot be validated. Furthermore, CTP studies are single-time-point assessments in a potentially dynamic process. This study cannot exclude the possibility that CPP does, in fact, drop transiently after BP reduction either before or after the CTP study. Finally, these data are from a relatively small sample of patients with ICH with predominately small-to-moderate hematoma volumes. In our study, only 15% of patients had ICH volumes of >40 mL. This is consistent with other ICH trials.33,35 Patients with large-volume ICH are less likely to be enrolled in trials because they are treated either conservatively or alternatively with surgical resection from the onset; consequently, these patients make up the minority in this clinical trial. All patients in our study were stable enough and lacked contraindications to CTP scanning 2 hours after randomization, which certainly introduced a selection bias. Nonetheless, these results provide further insight into cerebral perfusion patterns in acute ICH.
Conclusions
Perihematoma CPP is maintained, despite a modest increase in CVR, in acute primary ICH. Vascular borderzone CPP and CVR are normal in patients with ICH. Reduction of BP does not affect CPP in perihematoma or borderzone regions. These results provide further physiologic support for the safety of BP reduction in ICH.
ABBREVIATIONS:
- BP
blood pressure
- BZ
borderzone
- CPP
cerebral perfusion pressure
- CVR
cerebrovascular resistance
- ICH
intracerebral hemorrhage
- ICH ADAPT
Intracerebral Hemorrhage Acutely Decreasing Arterial Pressure Trial
Footnotes
Disclosures: Bronwen Gould—RELATED: Grant: Alberta Innovates Health Solutions (summer studentship). Thomas Jeerakathil—RELATED: Grant: Canadian Institutes for Health Research,* Comments: I am a collaborator on the grant that funded this research project. This was a peer-reviewed grant from a government funding agency. There is no conflict of interest. Dariush Dowlatshahi—UNRELATED: Expert Testimony: Canadian Medical Protective Association (medicolegal consultation for ischemic stroke); Grants/Grants Pending: Heart and Stroke Foundation, Comments: grant funding to study CTA, spot sign, and ICH; Patents (planned, pending or issued: patent on CT imaging software for the ICH spot sign; Travel/Accommodations/Meeting Expenses Unrelated to Activities Listed: BI Worldwide (travel grant to the meeting). Michael D. Hill—UNRELATED: Board Membership: Heart and Stroke Foundation of Alberta Board (volunteer charity board); Consultancy: Merck, Comments: Adjudication Committee for clinical trials in diabetes; Grants/Grants Pending: Covidien,* Comments: grant for clinical trial. Shelagh B. Coutts—UNRELATED: Canadian Institutes of Health Research,* Genome Canada,* Heart and Stroke Foundation of Canada,* Comments: grant funding for research not related to this article. Kenneth S. Butcher—RELATED: Grant: Alberta Institutes of Health Research and Heart and Stroke Foundation of Canada,* Comments: A grant-in-aid supported the ICH ADAPT trial; UNRELATED: Grants/Grants Pending: Canadian Institutes of Health Research,* Comments: Two grants-in-aid for unrelated work (blood pressure reduction in ischemic stroke and novel anticoagulant therapy in acute noncardioembolic stroke); Payment for Lectures (including service on Speakers Bureaus): speaker fees for new oral anticoagulants use by Boehringer Ingelheim, Bayer, and Pfizer/Bristol-Myers Squibb Canada. *Money paid to the institution.
This work was supported by a grant-in-aid from Alberta Innovates Health Solutions (G513000128) and the Heart and Stroke Foundation of Canada (G220170180). K.S.B holds a Canada Research Chair in Cerebrovascular Disease, a Heart and Stroke Foundation of Alberta Professorship in Stroke Medicine, and a New Investigator Award from Alberta Innovates Health Solutions. M.D.H. has a Heart and Stroke Foundation of Alberta Professorship in Stroke Medicine. A.M.D. has a Chair in Stroke Medicine (Heart and Stroke Foundation of Alberta). S.B.C. has an Alberta Innovates Health Solutions New Investigator award. B.G. and R.M. were supported by Alberta Innovates Health Solutions studentships.
Preliminary data previously presented at: International Stroke Congress, February 9–11, 2011; Los Angeles, California.
References
- 1. Fogelholm R, Avikainen S, Murros K. Prognostic value and determinants of first-day mean arterial pressure in spontaneous supratentorial intracerebral hemorrhage. Stroke 1997;28:1396–400 10.1161/01.STR.28.7.1396 [DOI] [PubMed] [Google Scholar]
- 2. Okumura K, Ohya Y, Maehara A, et al. Effects of blood pressure levels on case fatality after acute stroke. J Hypertens 2005;23:1217–23 10.1097/01.hjh.0000170385.76826.4a [DOI] [PubMed] [Google Scholar]
- 3. Anderson CS, Huang Y, Wang JG, et al. ; INTERACT Investigators. Intensive blood pressure reduction in acute cerebral haemorrhage trial (INTERACT): a randomised pilot trial. Lancet Neurol 2008;7:391–99 10.1016/S1474-4422(08)70069-3 [DOI] [PubMed] [Google Scholar]
- 4. Butcher K, Jeerakathil T, Emery D, et al. The Intracerebral Haemorrhage Acutely Decreasing Arterial Pressure Trial: ICH ADAPT. Int J Stroke 2010;5:227–33 10.1111/j.1747-4949.2010.00431.x [DOI] [PubMed] [Google Scholar]
- 5. Mendelow AD. Mechanisms of ischemic brain damage with intracerebral hemorrhage. Stroke 1993;24(12 suppl):I115–17; discussion I118–19 [PubMed] [Google Scholar]
- 6. Brazzelli M, Sandercock PA, Chappell FM, et al. Magnetic resonance imaging versus computed tomography for detection of acute vascular lesions in patients presenting with stroke symptoms. Cochrane Database Syst Rev 2009;CD007424 10.1002/14651858.CD007424.pub2 [DOI] [PubMed] [Google Scholar]
- 7. Kimberly WT, Gilson A, Rost NS, et al. Silent ischemic infarcts are associated with hemorrhage burden in cerebral amyloid angiopathy. Neurology 2009;72:1230–35 10.1212/01.wnl.0000345666.83318.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Singer OC, Kurre W, Humpich MC, et al. ; MR Stroke Study Group Investigators. Risk assessment of symptomatic intracerebral hemorrhage after thrombolysis using DWI-ASPECTS. Stroke 2009;40:2743–48 10.1161/STROKEAHA.109.550111 [DOI] [PubMed] [Google Scholar]
- 9. Singer OC, Berkefeld J, Lorenz MW, et al. ; MR Stroke Study Group Investigators. Risk of symptomatic intracerebral hemorrhage in patients treated with intra-arterial thrombolysis. Cerebrovasc Dis 2009;27:368–74 10.1159/000202427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Menon RS, Burgess RE, Wing JJ, et al. Predictors of highly prevalent brain ischemia in intracerebral hemorrhage. Ann Neurol 2012;71:199–205 10.1002/ana.22668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Arsava EM, Kayim-Yildiz O, Oguz KK, et al. Elevated admission blood pressure and acute ischemic lesions in spontaneous intracerebral hemorrhage. J Stroke Cerebrovasc Dis 2013;22:250–54 10.1016/j.jstrokecerebrovasdis.2011.08.006 [DOI] [PubMed] [Google Scholar]
- 12. Zazulia AR, Diringer MN, Videen TO, et al. Hypoperfusion without ischemia surrounding acute intracerebral hemorrhage. J Cereb Blood Flow Metab 2001;21:804–10 10.1097/00004647-200107000-00005 [DOI] [PubMed] [Google Scholar]
- 13. Schellinger PD, Fiebach JB, Hoffmann K, et al. Stroke MRI in intracerebral hemorrhage: is there a perihemorrhagic penumbra? Stroke 2003;34:1674–79 10.1161/01.STR.0000076010.10696.55 [DOI] [PubMed] [Google Scholar]
- 14. Butcher K, Baird T, MacGregor L, et al. Perihematomal edema in primary intracerebral hemorrhage is plasma derived. Stroke 2004;35:1879–85 10.1161/01.STR.0000131807.54742.1a [DOI] [PubMed] [Google Scholar]
- 15. Powers WJ, Zazulia AR, Videen TO, et al. Autoregulation of cerebral blood flow surrounding acute (6 to 22 hours) intracerebral hemorrhage. Neurology 2001;57:18–24 10.1212/WNL.57.1.18 [DOI] [PubMed] [Google Scholar]
- 16. Adams RE, Powers WJ. Management of hypertension in acute intracerebral hemorrhage. Crit Care Clin 1997;13:131–61 10.1016/S0749-0704(05)70299-2 [DOI] [PubMed] [Google Scholar]
- 17. Butcher KS, Jeerakathil T, Hill M, et al. ; ICH ADAPT Investigators. The Intracerebral Hemorrhage Acutely Decreasing Arterial Pressure Trial. Stroke 2013;44:620–26 10.1161/STROKEAHA.111.000188 [DOI] [PubMed] [Google Scholar]
- 18. Schumann P, Touzani O, Young A, et al. Evaluation of the ratio of cerebral blood flow to cerebral blood volume as an index of local cerebral perfusion pressure. Brain 1998;121:1369–79 10.1093/brain/121.7.1369 [DOI] [PubMed] [Google Scholar]
- 19. Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons; Joint Section on Neurotrauma and Critical Care, AANS/CNS, Carney NA, Ghajar J. Guidelines for the management of severe traumatic brain injury. J Neurotrauma 2007;24(suppl 1):S1–106. 10.1089/neu.2007.9976 17511535 [DOI] [Google Scholar]
- 20. Kirkman MA, Smith M. Intracranial pressure monitoring, cerebral perfusion pressure estimation, and ICP/CPP-guided therapy: a standard of care or optional extra after brain injury? Br J Anaesth 2014;112:35–46 10.1093/bja/aet418 [DOI] [PubMed] [Google Scholar]
- 21. Mayer SA, Lignelli A, Fink ME, et al. Perilesional blood flow and edema formation in acute intracerebral haemorrhage: a SPECT study. Stroke 1998;29:1791–98 10.1161/01.STR.29.9.1791 [DOI] [PubMed] [Google Scholar]
- 22. Wu O, Ostergaard L, Weisskoff RM, et al. Tracer arrival timing-insensitive technique for estimating flow in MR perfusion-weighted imaging using singular value decomposition with a block-circulant deconvolution matrix. Magn Reson Med 2003;50:164–74 10.1002/mrm.10522 [DOI] [PubMed] [Google Scholar]
- 23. Robb RA. The biomedical imaging resource at Mayo Clinic. IEEE Trans Med Imaging 2001;20:854–67 10.1109/42.952724 [DOI] [PubMed] [Google Scholar]
- 24. McCourt R, Gould B, Gioia L, et al. ; ICH ADAPT Investigators. Cerebral perfusion and blood pressure do not affect perihematoma edema growth in acute intracerebral hemorrhage. Stroke 2014;45:1292–98 10.1161/STROKEAHA.113.003194 [DOI] [PubMed] [Google Scholar]
- 25. Wintermark M, Thiran JP, Maeder P, et al. Simultaneous measurement of regional cerebral blood flow by perfusion CT and stable xenon CT: a validation study. AJNR Am J Neuroradiol 2001;22:905–14 [PMC free article] [PubMed] [Google Scholar]
- 26. Kudo K, Terae S, Katoh C, et al. Quantitative cerebral blood flow measurement with dynamic perfusion CT using the vascular-pixel elimination method: comparison with H2(15)O positron emission tomography. AJNR Am J Neuroradiol 2003;24:419–26 [PMC free article] [PubMed] [Google Scholar]
- 27. Murphy BD, Fox AJ, Lee DH, et al. Identification of penumbra and infarct in acute ischemic stroke using computed tomography perfusion-derived blood flow and blood volume measurements. Stroke 2006;37:1771–77 10.1161/01.STR.0000227243.96808.53 [DOI] [PubMed] [Google Scholar]
- 28. Gillard JH, Minhas PS, Harball MP, et al. Assessment of quantitative computed tomographic cerebral perfusion imaging with H2(15)O positron emission tomography. Neurol Res 2000;22:457–64 [DOI] [PubMed] [Google Scholar]
- 29. Wintermark M, Chioléro R, van Melle G, et al. Relationship between brain perfusion computed tomography variables and cerebral perfusion pressure in severe head trauma patients. Crit Care Med 2004;32:1579–87 10.1097/01.CCM.0000130171.08842.72 [DOI] [PubMed] [Google Scholar]
- 30. Kate MP, Hansen MB, Mouridsen K, et al. Blood pressure reduction does not reduce perihematoma oxygenation: a CT perfusion study. J Cereb Blood Flow Metab 2014;34:81–86 10.1038/jcbfm.2013.164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gould B, McCourt R, Asdaghi N, et al. ; ICH ADAPT investigators. Autoregulation of cerebral blood flow is preserved in primary intracerebral hemorrhage. Stroke 2013;44:1726–28 10.1161/STROKEAHA.113.001306 [DOI] [PubMed] [Google Scholar]
- 32. Gioia LC, Kate M, Choi V, et al. Ischemia in intracerebral hemorrhage is associated with leukoaraiosis and hematoma volume, not blood pressure reduction. Stroke 2015;46:1541–47 10.1161/STROKEAHA.114.008304 [DOI] [PubMed] [Google Scholar]
- 33. Qureshi AI, Palesch YY, Martin R, et al. ; Antihypertensive Treatment of Acute Cerebral Hemorrhage Study Investigators. Effect of systolic blood pressure reduction on hematoma expansion, perihematomal edema, and 3-month outcome among patients with intracerebral hemorrhage: results from the antihypertensive treatment of acute cerebral hemorrhage study. Arch Neurol 2010;67:570–76 10.1001/archneurol.2010.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Anderson CS, Heeley E, Huang Y, et al. ; INTERACT2 Investigators. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med 2013;368:2355–65 10.1056/NEJMoa1214609 [DOI] [PubMed] [Google Scholar]
- 35. Arima H, Anderson CS, Wang JG, et al. ; Intensive Blood Pressure Reduction in Acute Cerebral Haemorrhage Trial Investigators. Lower treatment blood pressure is associated with greatest reduction in hematoma growth after acute intracerebral hemorrhage. Hypertension 2010;56:852–58 10.1161/HYPERTENSIONAHA.110.154328 [DOI] [PubMed] [Google Scholar]