Abstract
We summarize in this article the development, roll out, and preliminary outcomes of a large-scale proactive mental health support model for frontline healthcare workers during the early stages of the COVID-19 pandemic, specifically during New York City's initial case surge in March through June of 2020. This paper summarizes the program design and output for two types of dedicated teams of behavioral health clinicians: 1) Mental Health Liaisons, who provided preventative support to COVID-19 hospital units and Emergency Departments, and 2) Mental Health Crisis Response Teams, who staffed 24/7 crisis response lines to support and mitigate staff crises as needed. In addition to the specifics of this model, we discuss the strategies, rewards, and difficulties of rapidly staging and evaluating such a model in the context of an ongoing disaster situation. We also offer recommendations for how this multi-dimensional model may be replicated in other settings.
Keywords: Emergency psychiatry, Disaster psychiatry, Crisis, Stress, Intervention, Occupational mental health, Trauma psychiatry
1. Introduction
It is March 17th and the Mount Sinai Health System (MSHS), which includes over 3,000 licensed hospital beds spanning three boroughs of New York City, is already treating 2,500 patients with a presumptive or definitive diagnosis of COVID-19. The surge peak has not fully hit yet, but the impact of the pandemic on our health care system is already profound, and there is tremendous concern about the emotional and psychological toll on our employees. We needed to rapidly build up and scale out a robust set of support services for our 42,000 employees, particularly those at the frontlines of caring for patients with COVID. The mission was to create a spectrum of services that was substantial in content and proactive, basing it around the concept of “Mental Health PPE”—that protective equipment and tools for our employees’ mental and emotional health were just as important as physical protective equipment. We report here on a multipronged approach to support the mental health needs of front-line workers in a large healthcare system at the epicenter of the COVID crisis, with a focus on two specific interventions.
1.1. Five-tier model of employee emotional support
There is significant potential for mental health consequences in medical responders to disasters (Naushad et al., 2019). In the face of a limited evidence base for how to minister to the acute mental health needs of disaster affected communities, including responders (Katz, 2011; Birur et al., 2017; North and Pfefferbaum, 2013), various departments across Mount Sinai rapidly collaborated to create and coordinate a five-tier model of emotional support for MSHS employees. This model was based on the following key principles: 1) interventions should be interconnected and part of a continuum of need; 2) the model must have a proactive component, promoting personal and communal well-being and resilience; and 3) the model should account for limitations on in-person support due to COVID-19. The model was part of a larger overall effort to address employees’ needs (Ripp et al., 2020).
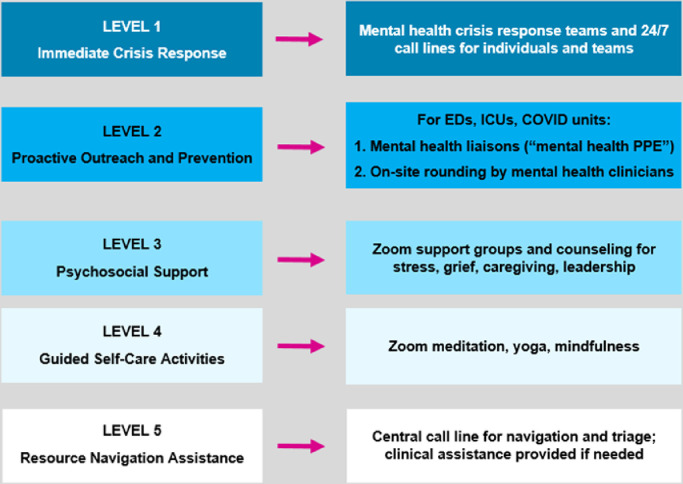
The model, as shown in Fig. 1 , included five levels based on acuity and baseline need. We will focus on an operational overview and preliminary analysis of the most acute interventions, Levels 1 and 2, which were led by the Mount Sinai Behavioral Health service line.
Fig. 1.
Five-tier model of employee wellness support.
On April 3rd, we went live with the Mental Health Liaison (MHL) and Mental Health Crisis Response Team (MHCRT) interventions. We completed the model, operationalization and rollout of both programs within 2 weeks of conception and were based on principles of psychological first aid (Substance Abuse and Mental Health Services Administration, 2005).
1.2. Program descriptions
1.2.1. Level 1 - MHCRT
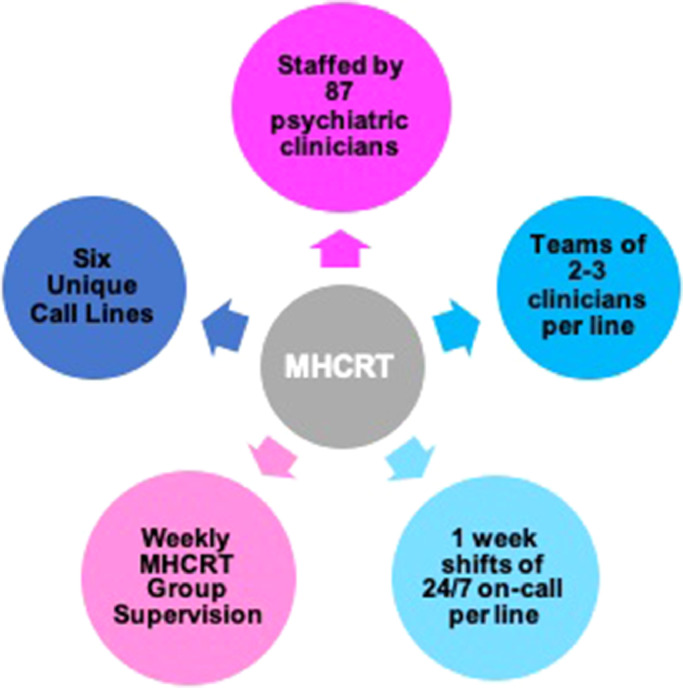
The MHCRT, Fig. 2 , staffed six distinct hospital-based 24/7 crisis call lines. Employees could call for any urgent or crisis level emotional support needs, both individual and group. The latter piece proved critical as often entire clinical units or services would collectively experience acute crises due to numerous and frequent patient deaths, as well as deaths of colleagues. MHCRT members themselves engaged in weekly supervision with program leadership to debrief, process, and problem-solve.
Fig. 2.
MHCRT program model.
1.2.2. Level 2 - MHL
While the MHCRT and other interventions in the 5-tier model primarily relied on employees reaching out for help, it was also critical to have interventions that proactively engaged employees. The Mental Health Liaison program was comprised of psychiatrists, psychologists, social workers, and mental health counselors in the Mount Sinai Behavioral Health service line and Department of Social Work. The program was targeted to staff in direct frontline care activities in COVID units, ICU's and emergency services. Each team was initially assigned to cover 1-3 units. The MHLs were available to all employees on their assigned units by text, phone, and email during weekdays. Once contacted by an employee, the MHL would routinely check back in with the employee primarily via text/email. MHLs also worked with unit leadership to proactively schedule regular group support sessions for their units.
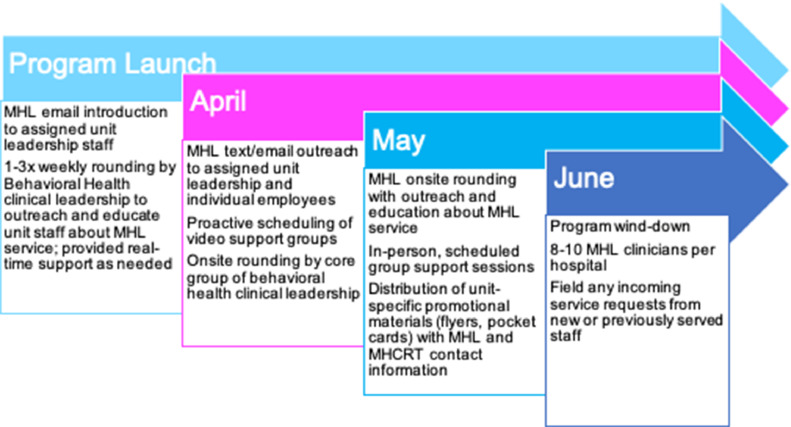
Most MHLs continued for the full 3-month duration of the program, with 129 unique individuals staffing 103 positions. Fig. 3, Fig. 4 demonstrate the initial structure of the MHL program in April, and its evolution to the final model to include additional units, emphasis of on-site rounding, as well as coverage of ancillary services and medical staff who were not assigned to any sole unit/service.
Fig. 3.
MHL model – initial.
Fig. 4.
MHL model – final.
When the volume of COVID 19 admissions began to decrease, June programming was scaled down to one larger team per hospital to maintain continuity of service for units previously outreached. As with MHCRT, weekly group supervision was conducted by program leadership throughout the duration of the program. When indicated, MHCRT team members communicated with MHL team members regarding particular patients or units that were experiencing high levels of distress. Fig. 5 summarizes key operational characteristics for the MHL program as the months progressed.
Fig. 5.
MHL operationalization and roll out.
2. Methods
2.1. Data collection
MHCRT staff submitted weekly data logs, including total number of: 1) calls received, 2) overnight calls received between 5 pm and 8 am, 3) calls requiring emergency referral, 4) calls requiring group crisis debrief, 5) outpatient mental health care referrals, and 6) comments on content and themes of interactions. Similarly, MHL teams submitted data weekly, including number and content of individual and group level interactions, outpatient mental health referrals, and themes of interactions. This analysis utilized MHCRT data collected over 13 weeks and MHL data collected over 12 weeks.
2.2. Data analysis
Analysis utilized a two-pronged approach. The first, a quantitative analysis, included descriptive statistics of all MHL and MHCRT data operational output metrics. The second utilized Braun and Clarke's (2012) method for content analysis to search for themes that arose in interactions between the MHL/MHCRT and the staff member engaging in the service (Braun and Clarke, 2012).
3. Results
3.1. MHCRT
The MHCRT program received a total 77 calls from April 7 – July 6, as presented in Fig. 6 . The majority of both overnight (5PM- 8AM) and daytime (8AM – 5PM) contacts occurred in April (n = 35), followed by May (n = 22) and then June (n = 20). Overnight calls constituted a minority of contacts (n = 17), both month over month and overall.
Fig. 6.
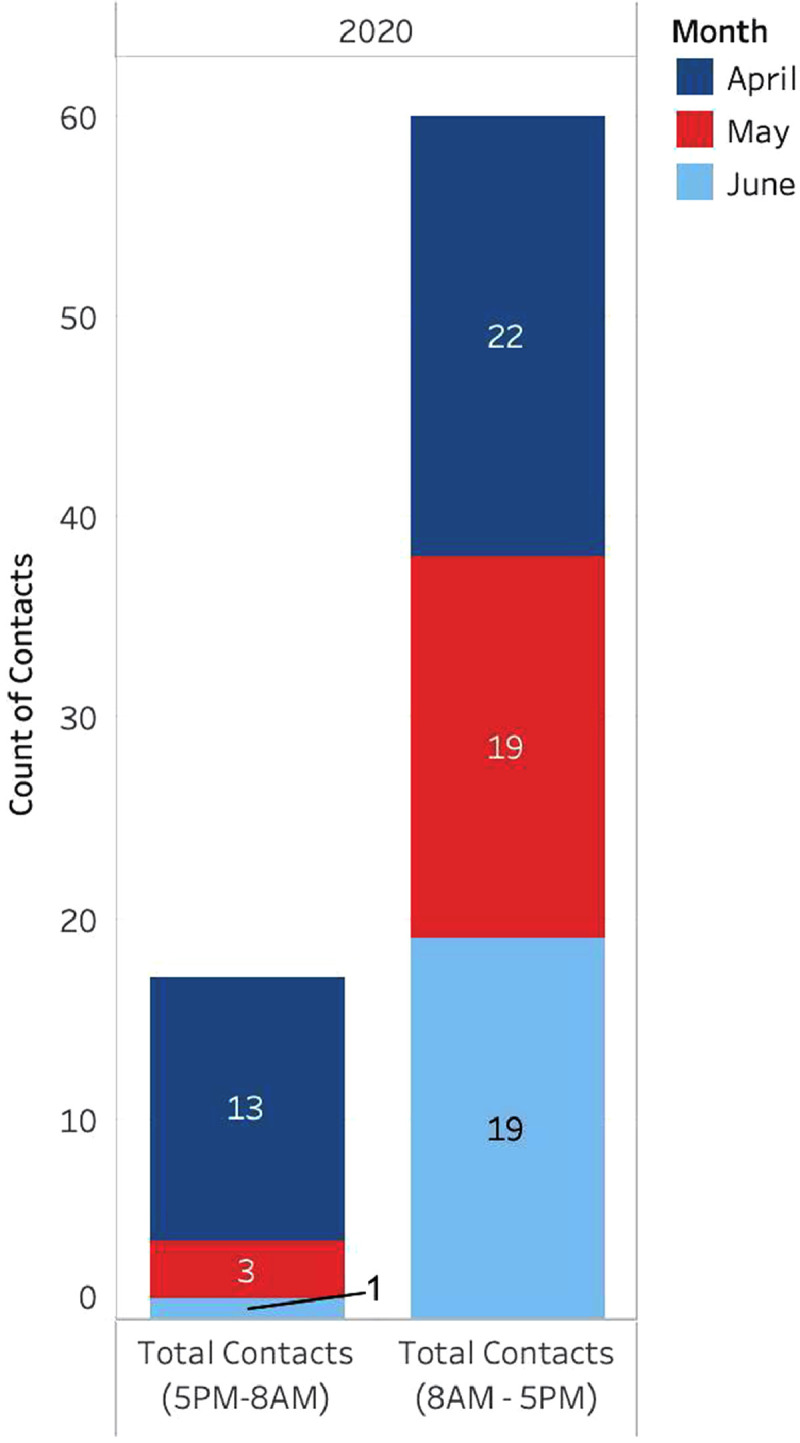
MHCRT program outputs.
3.2. MHL
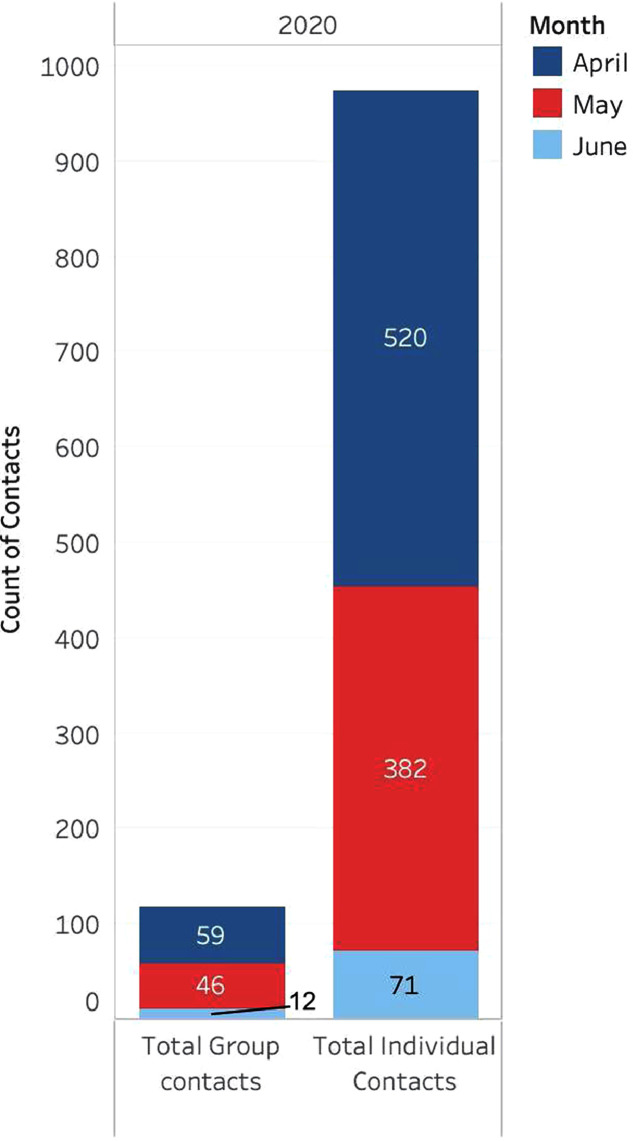
MHL staff conducted a total of 1,090 total contacts, as demonstrated in Fig. 7 , including individual- and group-level interactions. The large majority of these contacts consisted of individual-level outreach (n = 973), while group-level outreach accounted for 117 contacts.
Fig. 7.
MHL program outputs.
Volume peaked in April, much of which was proactive outreach to unit leadership. However, May (post-peak of surge), yielded the highest volume of on-site visits to the unit and the highest numbers of referrals to outpatient mental health treatment.
3.3. Outpatient mental health referrals
Altogether, as shown in Fig. 8 , MHL and MHCRT contacts led to a total of 38 referrals for staff members to outpatient mental health care. MHLs generated the majority of such referrals (n = 24) to formal mental health care. By month, both MHL and MHCRT referrals peaked in the month of May (n = 24).
Fig. 8.
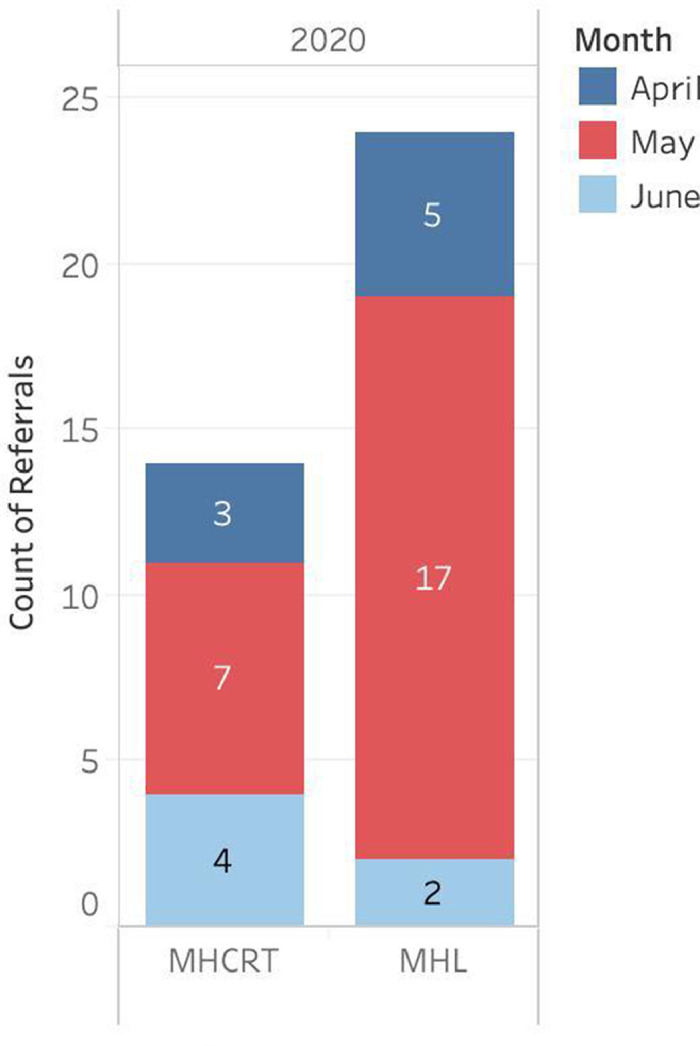
MHL and MHCRT outpatient mental health care referrals.
3.4. Qualitative results from both programs
Three categories containing associated themes emerged from the narrative section of the tracking sheets, which described the general summary of the exchange between the MHLs or MHCRT members. These include: Support Seeking Behaviors, Presenting Symptoms, and Triggering Events/Thoughts.
3.4.1. Support Seeking Behaviors
There was not a “one size fits all” approach that successfully engaged or encouraged staff to seek support. However, conversations between MHLs/MHCRTs and staff elicited feedback about what hindered seeking support. One such reason was simply logistical. Nursing leadership expressed that setting up video meetings was just “one more thing that has to get done”, and that when teams got to the unit, the crisis had resolved, the staff had dispersed, or nobody felt like talking any longer. As the surge passed, COVID units closed, staff often expressed that they had the desire to talk, but that they “needed to catch a breath” and would reach out when ready. And when they were ready, sometimes, stigma about seeking help inhibited seeking it. Several staff who did reach out to MHL/MHCRT expressed a desire to continue the intervention but worried that they would be looked down upon for doing so, or that their ability to do their job would be in question.
On-site presence was resoundingly the most well received form of the MHL intervention. Some units even asked MHLs to join morning huddles and change of shift. On-site support also seemed to enhance engagement in treatment seeking when there was a crisis on the unit, such as the death of a fellow staff member or a high volume of deaths in one shift.
Effective support techniques included mindfulness and breathing exercises, having the ability to text someone when they needed to check-in, and access to referrals for mental health treatment. Staff, including those that did not reach out for direct support, expressed that just knowing it was there was support within itself. One staff member relayed that she kept a pocket card explaining the MHL program on her refrigerator and in her actual pocket throughout the day so she could touch it and know that support was there if she needed it.
3.4.2. Presenting symptoms
The overwhelming emotional themes involved anxiety, fear, and panic. Sleeplessness was also common. Staff articulated secondary emotions such as anger over not having proper PPE, frustration at feeling helpless over their inability to save patients, and concerns about returning to work after recovering from COVID-19. Sheer disbelief over the COVID-19 crisis left some callers feeling stuck as they could not believe how many people were dying each day. This led some to feel hopeless about the situation, which in turn led to fear about a second wave, creating a cyclical pattern of ongoing anxiety.
3.4.3. Triggering events/thoughts
Triggering events and thoughts appeared to be related to presenting symptoms. The MHL service commonly received contacts about ongoing anxiety over not having enough PPE, worry about getting their family sick, or anxiety that was manifesting itself in all aspects of their daily life. The majority of MHCRT calls however were triggered by an acute crisis such as the death or intubation of a staff member or a young child.
Many staff expressed concerns for their family and children, particularly about infecting them with COVID, or that their absence to go and work on the frontlines was causing psychological distress. Other callers expressed extreme sadness over missing their kids and how spending time with them at the end of a difficult shift had been their “go-to coping mechanism”, but now it had become something they were fearful of engaging in.
4. Discussion
4.1. Impact and efficacy
We were not able to conduct a rigorous study of efficacy, which is a logistical and ethical challenge facing all acute responses to mass trauma. However, qualitatively there was a tremendous positive response from employees and hospital leadership, particularly for the MHL program. Many expressed a desire for the program to continue beyond the acute phase of the pandemic.
We deliberately did not ask MHL staff to separate out contacts that involved coordination with leadership, versus contacts with individual employees, because we conceived of the program as a whole, dynamic package. The value of the program was not just at the level of the frontline employee; it also emphasized the importance of engaging and supporting unit/service leadership, as they would likely have the most day-to-day impact on their staff. Sometimes it took over 10 attempts to engage leadership, and some were never engaged—but we inherently classified that as part of the overall process of support rather than as a failure.
4.2. Challenges
The primary challenge for both programs was the large size of our health system, and the scaling up services that normally would take months or years to develop and implement. Effective and rapid communication of the programs was a challenge, as identified above. For example, our initial plan was to have MHL's text each of the staff on their assigned units to introduce themselves and establish a personal connection. However, the logistics of acquiring all staff cell phone numbers proved too cumbersome, especially amid shifting staff re-assignments to new units. And, ironically, the robustness and diversity of the employee support services actually may have led to some confusion by employees about what exactly all the different services were.
It is also important to emphasize the operational oversight of these programs. Written procedures and FAQs were developed and refined recurrently to ensure standardization and to rapidly address unexpected issues. We focused heavily on effective communication and outreach about these programs, particularly in light of email and other electronic communication overload. We therefore deliberately included old-fashioned paper flyers, postings, and pocket cards to include tangible, “3D” objects of reference.
4.3. Replication
We believe that both the MHL and MHCRT programs can be replicated on a smaller scale in other hospitals/health systems. We were fortunate that all the clinicians volunteered for both programs and on top of their usual work (all of our behavioral health services remained open during the entire pandemic). There was tremendous goodwill by our clinicians, and the effort was characterized as a humanitarian mission for our own colleagues. Mount Sinai is one of the largest providers of behavioral health services in New York, and we therefore have a very large clinical workforce likely in comparison to others. However, we do not believe that the MHL teams need to solely consist of psychiatric clinicians. The most important qualities of the MHL members were to be empathic, nonjudgmental, and good communicators.
We initially assigned multiple clinicians to each MHL and MHCRT team to ensure that we had adequate numbers of staff and the ability to quickly respond. We believe now that we could have implemented this with a smaller number of people for the size of our system (approximately half the number). There was no clear ratio of # of units/services or number of employees that was optimal. We recommend that other hospitals interested in the MHL model start with 1 member for 3-5 units/services, depending on the number of employees. We also strongly recommend inclusion of an in -person rounding component.
Additional recommendations from our experience include: 1) underscoring to employees that these services are confidential and supportive; 2) an additional emphasis for employees that no one will force them to talk to a therapist or psychiatrist; and 3) active support by program leadership of MHL and MHCRT members themselves, in recognition of the emotional impact this work can have on them. This can be achieved by regular large group debriefs, as well as smaller support meetings led by various team leaders. Regarding the emphasis on confidential and supportive nature of these services, these recommendations directly respond to the continuing and significant stigma associated with mental health services, even among the healthcare workforce. In order to ensure rapid adoption, it may help to stress that this is a support service, not a treatment service.
Finally, for any employee support service to work well, employees must routinely see and hear from the highest levels of leadership about these services. We were very fortunate to have this support from our health system and hospital-specific leaders, and their support greatly contributed to the success of our programs. In particular, their support included such things as frequent broadcast email notifications, mention of services during on-site rounding by hospital leadership; and on-site rounding by behavioral health leadership at all campuses. At the same time, behavioral health leadership must have regular, robust representation at the highest level of emergency operations management to best advocate for inclusion of programs like the MHL and MHCRT in an organizational disaster response.
4.4. The long term
The pandemic has posed an extraordinary, once in a century challenge to our hospitals and communities. Healthcare workers also work under varying levels of stress and with varying levels of exposure to trauma in “normal times.” The model, which addressed the immediate, acute mental health needs of our colleagues in the pandemic, can and should be transitioned into lower-intensity programming that can both address the ordinary challenges of working in healthcare and be scaled up during extraordinary times. In fact, these services gave way to the founding of Mount Sinai's Center for Stress, Resilience, and Personal Growth (CSRPG) in July 2020. The CSRPG has dedicated full time mental health clinicians focused on longer term services for Mount Sinai's healthcare workers impacted by the pandemic through a wellness app, a series of resilience-promoting workshops, targeted outreach to clinical units, and trauma-informed mental health treatment services. Finally, a modified MHL program known as WARMTH (Wellness and Resilience through Mental Health) provides routine in-person rounding by a select group of clinicians and leaders from the Department of Psychiatry on key clinical units.
Contributors
Conceptualization, methodology, resources, supervision, writing, review and editing were conducted by SL, CK, and KK. Project administration, formal analysis, and original draft writing were led jointly by KM and MG. Data curation and visualization by MG. All authors contributed to and have approved the final manuscript. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Declaration of Competing Interest
Declaration of competing interest: On behalf of all authors I declare no conflict of interest.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. MHL and MHCRT, conducted by SL, KK, CK, KM, and MG, were financed internally by the Mount Sinai Health System and all participating clinical staff contributed voluntarily without extra pay, in the context of a humanitarian response. SL, KK, KM, and MG declare no conflict of interest. CK declares two potential conflicts of interest: 1) Consultant, Advanced Recovery Systems; and 2) Consultant, Rane Crisis Network.
References
- Naushad V.A., Bierens J.J., Nishan K.P., Firjeeth C.P., Mohammad O.H., Maliyakkal A.M., ChaliHadan S., Schreiber M.D. A systematic review of the impact of disaster on the mental health of medical responders. Prehospital Disaster Med. 2019 Dec;34(6):632–643. doi: 10.1017/S1049023X19004874. [DOI] [PubMed] [Google Scholar]
- Katz C.L. Disaster psychiatry: good intentions seeking science and sustainability. Adolesc. Psychiatry. 2011 Jul 1;1(3):187–196. [Google Scholar]
- Birur B., Math S.B., Fargason R.E. A review of psychopharmacological interventions post-disaster to prevent psychiatric sequelae. Psychopharmacol. Bull. 2017 Jan 26;47(1):8. doi: 10.64719/pb.4352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- North C.S., Pfefferbaum B. Mental health response to community disasters: a systematic review. JAMA. 2013 Aug 7;310(5):507–518. doi: 10.1001/jama.2013.107799. [DOI] [PubMed] [Google Scholar]
- Ripp J., Peccoralo L., Charney D. Attending to the emotional well-being of the health care workforce in a New York city health system during the COVID-19 Pandemic. Acad. Med. 2020;95(8):1136–1139. doi: 10.1097/ACM.0000000000003414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . US Department of Health and Human Services; Washington, DC, USA: 2005. (SAMHSA). Psychological First Aid – A Guide for Emergency and Disaster Response Workers (Fact Sheet) [Google Scholar]
- Braun V, Clarke V. In: APA Handbook of Research Methods in Psychology: vol 2, Research Designs. Cooper H, editor. APA; 2012. Thematic analysis; pp. 59–71. [Google Scholar]