SUMMARY:
Talimogene laherparepvec is an oncolytic virus recently approved for targeted treatment of advanced melanoma. Because of an inflammatory reaction, treated lesions may increase in size and develop infiltrative margins that can be construed as disease progression or extracapsular spread. In this report, we describe our initial experience imaging the response of metastatic nodes injected with talimogene laherparepvec. Six of 12 nodes (50%) showed growth from baseline followed by decreased size, 5 of 12 nodes (42%) showed a downward size trend, and 1 node showed continued increase in size. Seven of 9 nodes (78%) developed infiltrative margins at a median of 79 days, and 6 of 9 (67%) nodes became necrotic at a median of 76 days after injection, all showing decreased size at final follow-up. An increase in the size of nodes injected with talimogene laherparepvec does not necessarily indicate progression. Infiltrative margins are also frequently seen and may be confused with extracapsular disease.
Talimogene laherparepvec (T-VEC) is a second-generation oncolytic virus that was approved for the treatment of unresectable melanoma in the United States and Europe in 2015. This is the first intralesional immunotherapeutic agent approved by the FDA and the European Commission as well as the first such drug to show an increased durable response rate and overall survival in a Phase III clinical trial in patients with melanoma.1 T-VEC is a herpes simplex virus type 1 that has been genetically modified to selectively replicate in tumoral tissue. It results in direct lysis of tumor cells, which is followed and enhanced by a systemic immune response against viral and tumoral antigens.2 Data so far suggest that T-VEC is effective at achieving local control, though treatment of systemic disease may necessitate combination therapy.3
Histopathology shows that T-VEC elicits a prominent local inflammatory reaction and, in many cases, an increase in the size of the lesion followed by subsequent response.4,5 In our institution, in addition to an increase in size, we have noted the development of infiltrative margins and necrosis on CT in several T-VEC–injected nodes that ultimately decreased in size, mimicking extracapsular spread or progression of disease at some point during follow-up. The purpose of this report is to describe the imaging manifestations of nodes injected with T-VEC and correlate these findings with final nodal size and patient outcome.
Case Series
This post hoc analysis was approved by our institutional review board and was derived from a Phase Ib clinical trial assessing the safety of combined intratumoral T-VEC injection and intravenous ipilimumab in adult patients with histologically confirmed stage IIIB/IV melanoma. After the first injection with T-VEC, nodes were re-injected after 4 weeks and then every 2 weeks until complete response, disappearance, or disease progression per the immune response–related criteria.6 Amenable nodes were injected by using palpation or sonography guidance. The initial dose was 106 plaque-forming units/mL followed by 108 plaque-forming units/mL thereafter,4 with injected volumes ranging between 0.5–2 mL. Ipilimumab was administered a total of 4 times, every 3 weeks starting at week 6 from the first T-VEC injection.
We included a total of 12 nodes from 7 patients. The following imaging features were recorded on serial contrast-enhanced CT by a single radiologist and compared with baseline CT before injection: average size (cross-sectional dimensions), margins (well circumscribed or infiltrative), and necrosis. The median follow-up was 277 days (interquartile range, 221–348).
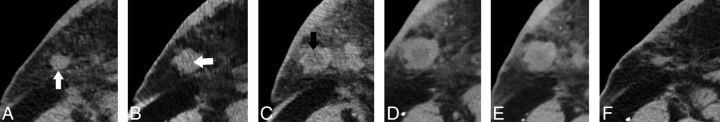
Two major growth patterns were observed. Six of 12 nodes (50%) showed an increase in size relative to the baseline followed by decreased size, with the size at final follow-up smaller than baseline (Fig 1A). Peak nodal size was reached at a median of 93 days (interquartile range, 79–104) after the first T-VEC injection and ranged from 29%–106% increase in size, with a median of 41%. Five of 12 nodes (42%) showed a downward trend in size (Fig 1B). Two of these showed minor increases in size during follow-up, but never larger than baseline. Two of 5 nodes were nonmeasurable at last follow-up CT. The remainder node (1 of 12; 8%) showed an upward trend (Fig 1A), but could not be followed after 184 days because the patient was placed under hospice care because of systemic disease progression. Except for this node, the sizes of all other nodes at last follow-up were smaller than baseline.
Fig 1.
Line graph showing change in size over time relative to baseline CT. A, Fifty percent of nodes showed initial growth followed by decreased size. One node (marked with an asterisk at last time point) demonstrated a continued increase in size, but could not be followed after 184 days. B, Forty-two percent of nodes showed a downward trend in size. The final size was smaller than baseline in all nodes except for the one indicated in A.
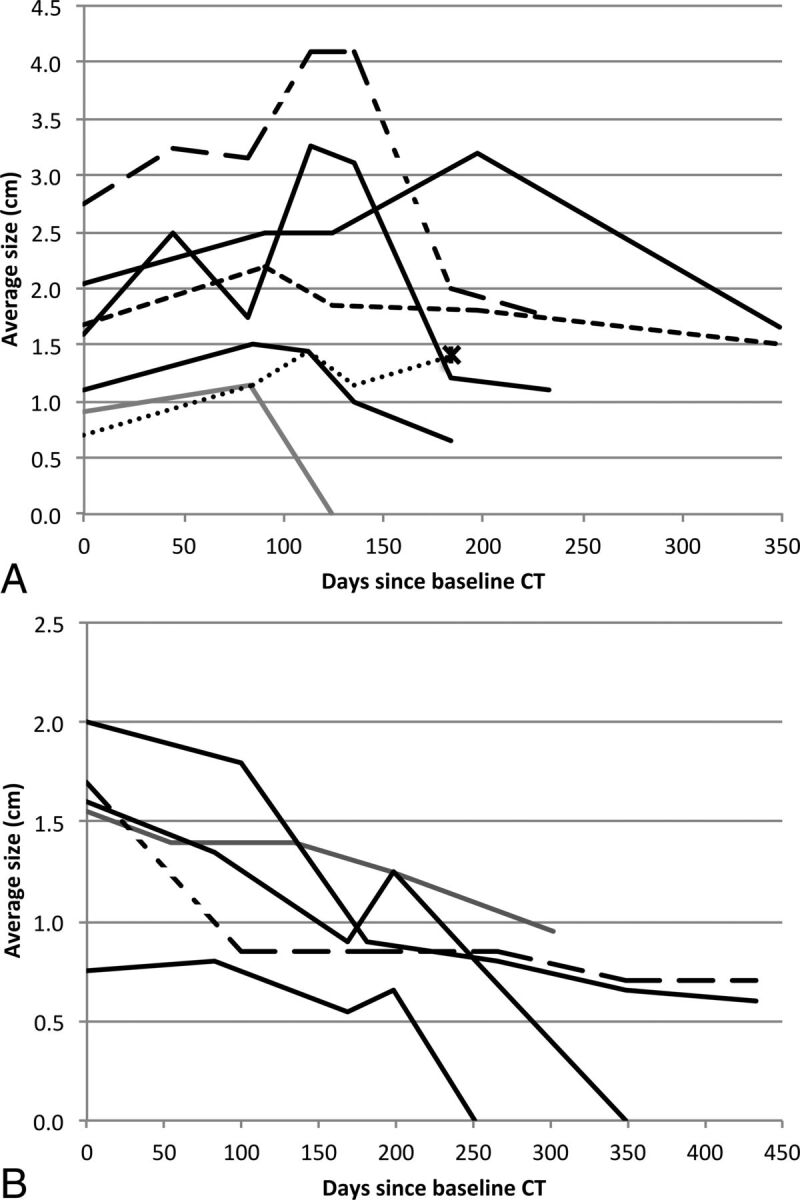
Regarding margins, these were well circumscribed at baseline in 9 of 12 nodes (75%), and the rest were infiltrative. Seven of the 9 nodes (78%) with initially well-circumscribed margins eventually became infiltrative at a median of 79 days (interquartile range 73–94) after the first T-VEC injection (Fig 2).
Fig 2.
A, Coronal contrast-enhanced CT shows a round, well-circumscribed necrotic lesion (black arrow) at the inferior aspect of the right parotid gland. B, The lesion has increased in size and developed infiltrative margins (white arrow) 72 days after injection. Follow-up at 111 days (C) and 184 days (D) after injection demonstrates further growth and marked increase in central necrosis. E, The lesion shows decreased size after 337 days.
Three of 12 nodes (25%) showed necrosis at baseline CT. Necrosis eventually developed in 6 of the remaining 9 nodes (67%) at a median of 76 days (interquartile range, 72–81) since the first T-VEC injection (Figs 2 and 3). All nodes that became infiltrative or developed necrosis during follow-up showed a final size that was smaller than baseline. All nodes that were initially necrotic also showed a decreased final size compared with baseline. Clinical features and patient outcomes are summarized in the Table.
Fig 3.
A, Axial contrast-enhanced CT shows a small nodule in the deep right breast/axillary region (white arrow). The lesion shows slight central hypoattenuation and increased size at 34 days after injection (white arrow, B) with the development of frank central necrosis after 72 days (black arrow, C). There is a mild further increase in size at 104 days (D), followed by decreased size at 125 days (E) and near complete resolution at 174 days (F).
Clinical features, disease stage, final nodal size (relative to baseline CT), and patient outcome
| Patient No. | Lesion No. | Age, yr | Sex | Stage | BRAF Status | Location | Final Lesion Size | Patient Outcome |
|---|---|---|---|---|---|---|---|---|
| 1 | 1 | 63 | F | T3bN3M1a | Negative | Left supraclavicular | Decreased | Remission. |
| 2 | 2 | 66 | M | TxNxM1c | Wild type | Right supraclavicular | Decreased | T-VEC discontinued after disease progression in ribs. Placed on nivolumab with partial response. |
| 3 | Right supraclavicular | Decreased | ||||||
| 3 | 4 | 40 | M | pT1bN3M1c | Positive | Right preauricular | Decreased | IL-2 followed by BRAF and MEK inhibitors after ipilimumab/T-VEC treatment. Deceased. |
| 5 | Right submandibular | Decreased | ||||||
| 4 | 6 | 44 | M | T3bN3M1b | Positive | Right axillary | Decreased | BRAF and MEK inhibitors after ipilimumab/T-VEC treatment, followed by disease progression. Deceased. |
| 7 | Right axillary | Decreased | ||||||
| 5 | 8 | 58 | F | T3bN2M1a | Wild type | Left upper back | Decreased | Complete response for 21 months, followed by axillary recurrence. Placed on nivolumab. |
| 9 | Left breast | Decreased | ||||||
| 6 | 10 | 32 | M | T4bN3M1a | Negative | Left retroauricular | Decreased | Partial response for 6 months. Placed on nivolumab. |
| 7 | 11 | 63 | M | T3aN3M1c | Negative | Right chest wall | Increased | Rapid deterioration after brain metastases. Deceased. |
| 12 | Right axilla | Decreased |
Note:—IL-2 indicates interleukin 2.
Discussion
The potential antitumoral effects of viral infection have been recognized for many years.7 Although the affinity of certain viruses for tumor cells has long been established, the main issue until recently has been achieving control of viral replication in normal tissues. Genetic engineering has made it possible to design organisms that will selectively replicate in tumoral tissue while minimizing damage to the host. Deletion of the γ34.5 gene in T-VEC and other oncolytic viruses reduces their pathogenicity by inhibiting replication in normal tissue, whereas inactivation of the α47 gene promotes their replication in cancer cells.4 In addition, T-VEC has been modified to express granulocyte-macrophage colony-stimulating factor, which amplifies an immune response against the tumor.5 In essence, T-VEC's mechanism of action is 2-fold: a direct oncolytic effect after viral infection of the tumor and a secondary systemic response mounted by the host. The virus is the treatment agent rather than a drug delivery carrier. Notably, regional and systemic antitumor responses can be delayed for several weeks after the initiation of treatment and are most prominent in injected nodes, but nodes that were not injected are also affected to a lesser extent.8
On histopathologic analysis, Hu et al4 showed inflammatory changes in nearly all tumors injected with T-VEC. They found that necrosis was present in most treated tumors and was frequently extensive, with sparing of normal tissue. Although the prognostic significance of necrosis in melanoma nodes injected with T-VEC is established, the development of necrosis in solid tumors is generally accepted as a marker of tumor lysis and cell death.9 In a Phase II trial of patients with melanoma metastases treated with bevacizumab, the development of marked decreased attenuation or central necrosis (as part of the modified Morphology, Attenuation, Size, and Structure [MASS] criteria) was rare, but constituted a strong predictor of favorable response, with such changes deemed to be secondary to devascularization.10 A different study where bevacizumab was administered in combination with ipilimumab, an immunotherapeutic agent, also showed that necrosis was rare.11 In contradistinction to these studies, but consistent with the histopathologic description of T-VEC-injected nodes by Hu and colleagues,4 the development of necrosis was common in our cohort, and all such nodes showed a subsequent decrease in size. Therefore, it is reasonable to speculate that this phenomenon may be more of a function of the oncolytic properties of the virus rather than a systemic response and, therefore, more likely to be seen in patients injected with T-VEC and similar agents than in those receiving systemic immunotherapies or antiangiogenic drugs.
Most nodes in our study developed infiltrative margins at some point during follow-up, and all of these demonstrated a decreased final size. Although in the appropriate setting, ill-defined nodal margins suggest an inflammatory or infectious process, the imaging appearance of extracapsular tumor spread is indistinguishable. This finding has important treatment implications in a variety of head and neck tumors, where it conveys a poor prognosis.12,13 In melanoma, extracapsular spread in metastatic nodes also has prognostic implications and has been associated with failure after regional lymphadenectomy and potential benefit from more aggressive therapies.14,15 Thus, it is critical not to confuse these inflammatory changes with tumor progression because this could lead to the discontinuation of an effective therapy.
In our patients, 50% of all injected nodes showed initial growth before subsequently decreasing in size. This is consistent with the results from a Phase III trial in which more than half of the patients had lesions that initially increased in size or developed new lesions before achieving a response.1 This phenomenon of pseudoprogression has been described with other immunotherapies and is probably related to a flare reaction in the setting of inflammatory changes with or without edema, whereby established lesions can show a transient increase in size and microscopic disease may become inflamed and detectable as a “new” lesion on posttreatment imaging.6,16 It is also possible that in at least some of these cases, there is continued tumor growth until a considerable immunologic response is developed.6 In our study, extensive necrosis accounted for the increase in size of some nodes. Again, transient lesion growth and the development of “new” lesions can lead to patients being classified as having disease progression when some of them may actually benefit from continuation of treatment. Conventional criteria for objective treatment response, such as the Response Evaluation Criteria in Solid Tumors (RECIST) or the World Health Organization criteria, have inherent limitations in patients receiving immunotherapeutic agents. Prior studies using conventional criteria have documented tumor regression in patients initially thought to have stable or progressive disease.17 Newer criteria such as the immune response–related criteria are more inclusive of the expected patterns of disease activity in patients receiving these agents and may be better suited to evaluate response in such circumstances.6
This study has several limitations, the most notable being the small sample size and the retrospective nature of the analysis. The timing of the development of necrosis and infiltrative margins is a broad estimate because we do not know the exact time point when these changes occurred before the imaging study where they became evident. Depending on individual clinical need, CT studies were performed at different times after injection, and that introduced some variability. In addition, it is difficult to account for effects that ipilimumab may have had on individual nodal response, either by itself or through synergism. It is well established that ipilimumab may incite an inflammatory response and, in some cases, a temporary increase in tumor size can be observed during the first few weeks of treatment.18 Data from Phase II clinical trials in patients with advanced melanoma treated with ipilimumab show that close to 10% of them would have been misclassified as having progression of disease by World Health Organization criteria based on an increase in lesion size or the development of new lesions alone.6,19 The greatest increase in nodal size in our study occurred between 9 and 20 weeks after ipilimumab was initiated. We do not know to what extent the presumed inflammatory effects of T-VEC and ipilimumab may have overlapped.
Lastly, although final smaller nodal size may represent successful treatment, the presence of viable disease cannot be excluded because the nodes in our series were not biopsied. In addition, although FDG-PET may have some utility in monitoring the response to T-VEC and other immunotherapies, data from both animal models and patients with cancer suggest that avid uptake could in some cases represent an inflammatory response to the virus and should not be automatically interpreted as progression of disease.20,21 The patients in our small cohort did not consistently have an FDG-PET scan after T-VEC injection during the time that these nodes were followed, and therefore, correlation with the morphologic changes that we observed was not possible.
CONCLUSIONS
In summary, half of the nodes in our patients showed an initial increase (pseudoprogression) in size after T-VEC injection followed by decreased size and, in some cases, resolution of the lesion. The development of infiltrative margins and necrosis was frequent, and all such nodes showed a final size that was smaller than baseline, a presumed measure of success. These imaging manifestations are concordant with the expected biologic behavior of lesions treated with immunotherapeutic agents, and necrosis appears to be common and prominent after T-VEC injection. Increased size per se is not necessarily indicative of progression or an indication to stop treatment in clinically stable patients. Additional studies with a larger number of patients are needed to fully understand the radiographic progression and magnitude of these changes and the relative contribution of both targeted and systemic immunotherapies. Because the use of targeted agents is a fairly new development and not as of yet widespread, many head and neck radiologists may not be aware of these potential imaging findings. The recognition that a patient may be undergoing such treatments is paramount to avoid diagnostic pitfalls and confusion with extracapsular spread or progression of disease. Our preliminary results highlight the importance of being cognizant of specific treatments before image interpretation.
ABBREVIATION:
- T-VEC
talimogene laherparepvec
Footnotes
Disclosures: Frances Collichio—UNRELATED: Consulting Fee or Honorarium: Amgen*; Other: Professional Development Committee of ASCO. *Money paid to the institution.
Paper previously presented at: 102nd Scientific Assembly and Annual Meeting of the Radiological Society of North America, November 27–December 2, 2016; Chicago, Illinois.
References
- 1. Andtbacka RH, Kaufman HL, Collichio F, et al. Talimogene laherparepvec improves durable response rate in patients with advanced melanoma. J Clin Oncol 2015;33:2780–88 10.1200/JCO.2014.58.3377 [DOI] [PubMed] [Google Scholar]
- 2. Ott PA, Hodi FS. Talimogene laherparepvec for the treatment of advanced melanoma. Clin Cancer Res 2016;22:3127–31 10.1158/1078-0432.CCR-15-2709 [DOI] [PubMed] [Google Scholar]
- 3. Rehman H, Silk AW, Kane MP, et al. Into the clinic: talimogene laherparepvec (T-VEC), a first-in-class intratumoral oncolytic viral therapy. J Immunother Cancer 2016;4:53 10.1186/s40425-016-0158-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hu JC, Coffin RS, Davis CJ, et al. A phase I study of OncoVEXGM-CSF, a second-generation oncolytic herpes simplex virus expressing granulocyte macrophage colony-stimulating factor. Clin Cancer Res 2006;12:6737–47 10.1158/1078-0432.CCR-06-0759 [DOI] [PubMed] [Google Scholar]
- 5. Appleton ES, Turnbull S, Ralph C, et al. Talimogene laherparepvec in the treatment of melanoma. Expert Opin Biol Ther 2015;15:1517–30 10.1517/14712598.2015.1084280 [DOI] [PubMed] [Google Scholar]
- 6. Wolchok JD, Hoos A, O'Day S, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin Cancer Res 2009;15:7412–20 10.1158/1078-0432.CCR-09-1624 [DOI] [PubMed] [Google Scholar]
- 7. Fukuhara H, Ino Y, Todo T. Oncolytic virus therapy: a new era of cancer treatment at dawn. Cancer Sci 2016;107:1373–79 10.1111/cas.13027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kaufman HL, Amatruda T, Reid T, et al. Systemic versus local responses in melanoma patients treated with talimogene laherparepvec from a multi-institutional phase II study. J Immunother Cancer 2016;4:12 10.1186/s40425-016-0116-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kaufman HL, Kohlhapp FJ, Zloza A. Oncolytic viruses: a new class of immunotherapy drugs. Nat Rev Drug Discov 2015;14:642–62 10.1038/nrd4663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gray MR, Martin del Campo S, Zhang X, et al. Metastatic melanoma: lactate dehydrogenase levels and CT imaging findings of tumor devascularization allow accurate prediction of survival in patients treated with bevacizumab. Radiology 2014;270:425–34 10.1148/radiol.13130776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Nishino M, Giobbie-Hurder A, Ramaiya NH, et al. Response assessment in metastatic melanoma treated with ipilimumab and bevacizumab: CT tumor size and density as markers for response and outcome. J Immunother Cancer 2014;2:40 10.1186/s40425-014-0040-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mermod M, Tolstonog G, Simon C, et al. Extracapsular spread in head and neck squamous cell carcinoma: a systematic review and meta-analysis. Oral Oncol 2016;62:60–71 10.1016/j.oraloncology.2016.10.003 [DOI] [PubMed] [Google Scholar]
- 13. Maxwell JH, Ferris RL, Gooding W, et al. Extracapsular spread in head and neck carcinoma: impact of site and human papillomavirus status. Cancer 2013;119:3302–08 10.1002/cncr.28169 [DOI] [PubMed] [Google Scholar]
- 14. Bibault JE, Dewas S, Mirabel X, et al. Adjuvant radiation therapy in metastatic lymph nodes from melanoma. Radiat Oncol 2011;6:12 10.1186/1748-717X-6-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nathansohn N, Schachter J, Gutman H. Patterns of recurrence in patients with melanoma after radical lymph node dissection. Arch Surg 2005;140:1172–77 10.1001/archsurg.140.12.1172 [DOI] [PubMed] [Google Scholar]
- 16. Brahmer JR, Tykodi SS, Chow LQ, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med 2012;366:2455–65 10.1056/NEJMoa1200694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. van Baren N, Bonnet MC, Dréno B, et al. Tumoral and immunologic response after vaccination of melanoma patients with an ALVAC virus encoding MAGE antigens recognized by T cells. J Clin Oncol 2005;23:9008–21 10.1200/JCO.2005.08.375 [DOI] [PubMed] [Google Scholar]
- 18. Saenger YM, Wolchok JD. The heterogeneity of the kinetics of response to ipilimumab in metastatic melanoma: patient cases. Cancer Immun 2008;8:1 [PMC free article] [PubMed] [Google Scholar]
- 19. Chiou VL, Burotto M. Pseudoprogression and immune-related response in solid tumors. J Clin Oncol 2015;33:3541–43 10.1200/JCO.2015.61.6870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Covington MF, Curiel CN, Lattimore L, et al. FDG-PET/CT for monitoring response of melanoma to the novel oncolytic viral therapy talimogene laherparepvec. Clin Nucl Med 2017;42:114–15 10.1097/RLU.0000000000001456 [DOI] [PubMed] [Google Scholar]
- 21. Koski A, Ahtinen H, Liljenback H, et al. [(18)F]-fluorodeoxyglucose positron emission tomography and computed tomography in response evaluation of oncolytic adenovirus treatments of patients with advanced cancer. Hum Gene Ther 2013;24:1029–41 10.1089/hum.2013.123 [DOI] [PubMed] [Google Scholar]