Abstract
BACKGROUND AND PURPOSE:
Widening of the occipital condyle-C1 interval is the most specific and sensitive means of detecting atlanto-occipital dislocation. Recent studies attempting to define normal measurements of the condyle-C1 interval in children have varied substantially. This study was performed to test the null hypothesis that condyle-C1 interval morphology and joint measurements do not change as a function of age.
MATERIALS AND METHODS:
Imaging review of subjects undergoing CT of the upper cervical spine for reasons unrelated to trauma or developmental abnormality was performed. Four equidistant measurements were obtained for each bilateral condyle-C1 interval on sagittal and coronal images. The cohort was divided into 7 age groups to calculate the mean, SD, and 95% CIs for the average condyle-C1 interval in both planes. The prevalence of a medial occipital condyle notch was calculated.
RESULTS:
Two hundred forty-eight joints were measured in 124 subjects with an age range of 2 days to 22 years. The condyle-C1 interval varies substantially by age. Average coronal measurements are larger and more variable than sagittal measurements. The medial occipital condyle notch is most prevalent from 1 to 12 years and is uncommon in older adolescents and young adults.
CONCLUSIONS:
The condyle-C1 interval increases during the first several years of life, is largest in the 2- to 4-year age range, and then decreases through late childhood and adolescence. A single threshold value to detect atlanto-occipital dissociation may not be sensitive and specific for all age groups. Application of this normative data to documented cases of atlanto-occipital injury is needed to determine clinical utility.
Widening or asymmetry of the occipital condyle-C1 interval (CCI) on CT has been shown to be the most specific and sensitive means of detecting atlanto-occipital dislocation in the pediatric population.1 A prior study of the normal CCI measurements in children suggested that CCI joint measurements do not differ substantially from birth to early adulthood.2 However, more recent studies evaluating the CCI by using different measurement techniques3,4 and our own experience at a large tertiary care children's hospital suggest otherwise. The purpose of this study was to assess normative CCI measurements in the largest nontraumatic cohort to date and test the null hypothesis that CCI morphology and joint space measurements do not change with age.
Materials and Methods
Subject Identification
This retrospective study was approved by our institutional review board and was performed at a tertiary care children's hospital. A retrospective review was performed of subjects undergoing imaging of the cervical spine for reasons unrelated to trauma or developmental abnormality of the spine. Using a radiology data base search engine (Softek Illuminate; https://www.softekinc.com/illuminate/), we searched for imaging modalities that included postprocessed true sagittal and coronal reconstructions of the craniocervical junction, including sinus, temporal bone, and head CT.
Criteria for inclusion in the study were age younger than 23 years and subjects who had undergone CT that included the occipital condyle-C1 joint in its entirety. Clinical exclusion criteria included a history of recent head/neck trauma, genetic/syndromic diagnosis, or connective tissue disorder. Exclusion criteria based on imaging included the following: developmental abnormalities of the craniocervical junction or cervical spine, craniosynostosis, or other evidence of genetic/syndromic abnormalities. Patient demographics and clinical indications for the examination were tabulated.
Imaging
All CT examinations were performed on either an Aquilion 64 or Aquilion ONE CT scanner (Toshiba Medical Systems, Tokyo, Japan) with detector widths of 0.375 mm. The kilovolt(peak) was between 80 and 120 mA and was age-dependent. All sinus, head, and temporal bone CT examinations were performed by using a helical acquisition. 3D head examinations were performed by using a volume acquisition on the Aquilion ONE or a helical acquisition on the Aquilion 64. Sagittal and coronal reconstructions were performed by the CT technologist at section thicknesses of ≤2 mm.
Image Analysis
Each imaging examination was reviewed by 1 of 2 examiners. The first investigator (L.L.L.) had 7 years of experience reviewing CT and is an attending pediatric neuroradiologist. The second investigator (P.S.) was a postgraduate year 1 resident who received detailed instructions and initial supervision in the appropriate measurements. Each investigator examined approximately two-thirds of all the subjects, with 45 subjects (36%) being examined by both examiners to calculate interobserver variance. For those 45 subjects evaluated by both investigators, the measurements were averaged in the final analysis. The investigators were included in the multiple regression analysis to detect any independent association of the investigator with average CCI measurements.
The investigators tabulated the following measurements and imaging features: clivus-dens angle; coronal, axial, and sagittal plane reconstruction angle; CCI in the sagittal and coronal planes; and the presence of a medial occipital condyle notch in the midjoint on sagittal images.
The clivus-dens angle was calculated as the angle between lines drawn along the dorsal cortex of the clivus and the posterior cortex of the dens. This angle was calculated to test whether the degree of flexion or extension of the joint was associated with differences in joint space measurements. The coronal reconstruction plane angulation was calculated to evaluate whether differences in reconstruction angulation between varying types of examinations were associated with differences in CCI measurements. The coronal reconstruction plane angulation was calculated from sagittal images as the angle between the coronal reconstruction plane and a line drawn along the posterior aspect of the dens. To reduce measurement variation secondary to rotation and tilt of the head in relation to the upper cervical spine, axial and sagittal plane angulations were calculated. The axial plane angulation was calculated as the angle between the skull base (drawn along the midline skull base) and a line drawn between the midline anterior and posterior arches of C1. Examinations with axial angulation >10° were excluded. The sagittal reconstruction plane angulation was calculated from the coronal images as the angle between a vertical plumb line and a line drawn through the center of the C2 body and the dens. Examinations with sagittal reconstruction plane angulation of >5° were excluded.
To calculate the average CCI, the investigators used the method of Pang et al,2 except that localizer lines were used in the sagittal plane rather than the axial plane to select coronal images to allow confident exclusion of the medial occipital condyle notch in younger children. Four equidistant measurements were made for each bilateral CCI in both the sagittal and coronal planes perpendicular to the articular surfaces (Fig 1). In the coronal plane, measurements from a section localized to the midjoint on sagittal images were obtained, taking special care to avoid the medial occipital condyle notch, if present. The medialmost measurement was taken beginning at the margin of the foramen magnum, and the lateralmost measurement was taken where the superior aspect of the C1 lateral mass goes from a rounded contour to a flat articular plane. In the sagittal plane, measurements were obtained from a section localized to the midjoint on coronal images. When measuring the CCI on sagittal images with the medial occipital condyle notch present, the examiners took special care to avoid measurements within the medial occipital notch. The anteriormost measurement was taken beginning at the anterior margin of the C1 joint, and the posteriormost measurement was taken beginning at the posterior margin of the C1 joint. These 4 measurements for each joint space were then averaged, giving 2 average coronal and 2 average sagittal CCI values for each patient.
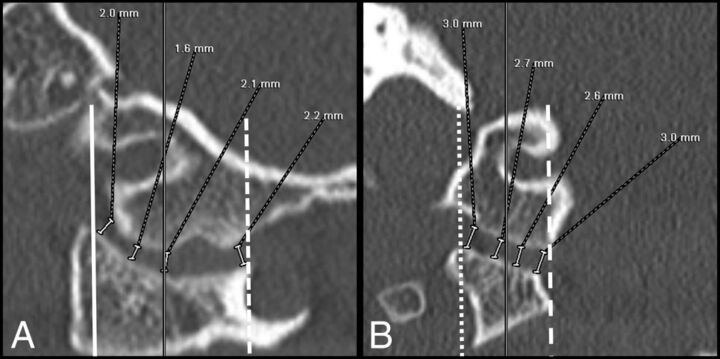
Fig 1.
Method used to make sagittal (A) and coronal (B) CCI measurements in an 8-year-old boy. Note the use of localizer lines (solid black lines midjoint) to avoid the notch when selecting the appropriate coronal image from which to obtain measurements. On sagittal images (A), the anteriormost measurement is taken beginning at the anterior margin of the C1 joint (solid white line) and the posteriormost measurement is taken beginning at the posterior margin of the C1 joint (dashed line). On coronal images, the medialmost measurement is taken beginning at the margin of the foramen magnum (dashed white line) and the lateralmost measurement is taken where the superior aspect of the C1 lateral mass goes from a rounded contour to a flat articular plane (dotted line).
Statistical Analysis
The cohort was divided into 7 age groups to calculate the mean, SD, and 95% confidence intervals for average coronal and sagittal CCIs. Multivariate logistic regression models were used to evaluate the independent effects of subject age, sex, investigator (L.L.L. and P.S.), coronal reconstruction angle, and the clivus-dens angle on average CCIs. Model selection under a stepwise criterion was performed to avoid multicollinearity. The mean absolute difference between left and right coronal and sagittal average CCI was calculated. The variance in measurements at different locations within the joint was calculated for the entire population to determine whether some locations within the joint are more reliable measures from one subject to the next. Stepwise comparison between the variance of the most lateral CCI measurement and the 3 more medial CCI measurements (coronal plane) and the most anterior CCI measurement and the 3 more posterior measurements (sagittal plane) was performed. Quantitative morphologic changes with time in the coronal plane were investigated by measuring the mean difference between the lateralmost and medialmost coronal occipital condyle-C1 joint space measurements for each age group. The mean absolute variance in joint space measurement by the investigator was calculated by using measurements for the 45 subjects examined by both investigators. A subset analysis of investigator variance for those subjects 14 years and older and a second group younger than 14 years was also performed. A χ2 or Fisher exact test was used to assess the relationship between subject age and the presence of the medial occipital condyle notch. P < .05 was considered significant. All analyses were performed by using SAS statistical software, Version 9.3 (SAS Institute, Cary, North Carolina).
Results
One hundred twenty-four subjects (248 joint spaces) were identified as appropriate according to inclusion and exclusion criteria. The mean age of the cohort was 7.8 years (range, 2 months to 22 years). The cohort included 62 females and 62 males. CT examination types were as follows: routine sinus (n = 90), routine head (n = 21), 3D head (n = 6), and temporal bone (n = 7). Clinical indications for the examinations were sinusitis (n = 53), abnormal head shape (n = 13), fever (n = 10), mass/tumor (n = 9), cough (n = 8), seizure (n = 8), headache (n = 3), leukemia (n = 3), hearing loss (n = 2), and other (n = 15).
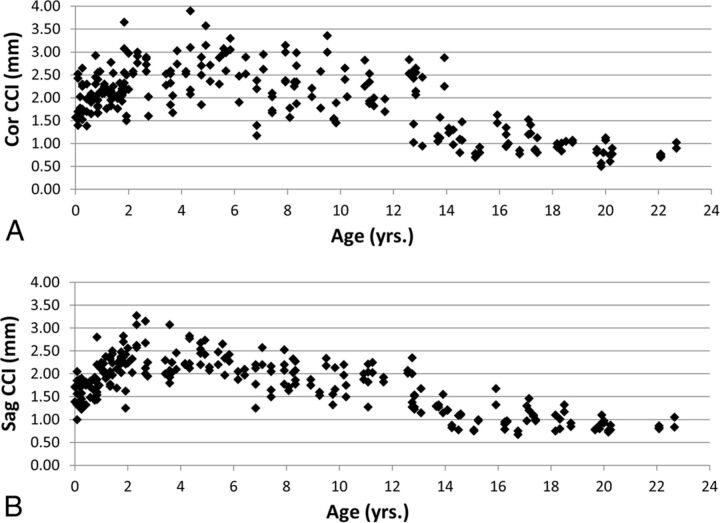
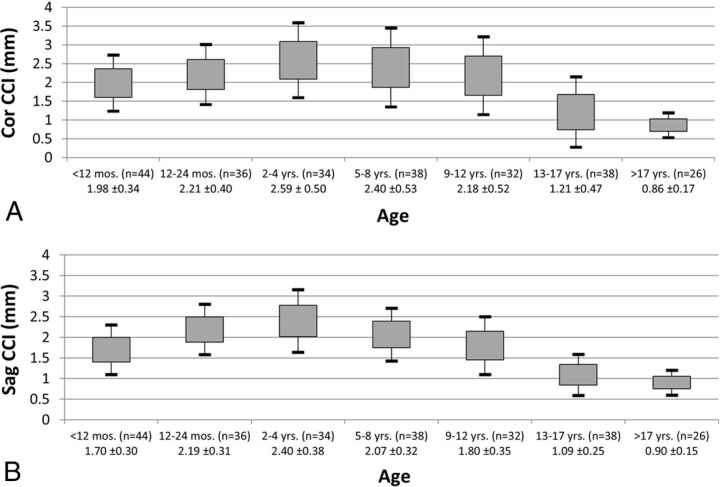
Scatterplots reveal the distribution of all data by age for the 248 joints in the sagittal and coronal planes (Fig 2). Results were aggregated into 7 age groups, with a range of 26–44 joint spaces in each age group. With a multivariate logistic regression, subject age was found to be statistically associated with average coronal and sagittal CCIs (Fig 3). The mean sagittal and coronal CCIs increased during the first 2 years of life and were largest in the 2- to 4-year age group at 2.4 mm (95% CI, 2.26–2.53 mm) in the sagittal plane and 2.59 mm (95% CI, 2.41–2.76 mm) in the coronal plane. Beyond the 2- to 4-year age group, CCI decreased throughout development. In the 17-years of age and older group, CCI was 0.90 mm (95% CI, 0.84–0.96 mm) in the sagittal plane and 0.86 mm (95% CI, 0.80–0.93 mm) in the coronal plane. This age-dependent change in CCI was statistically significant with a quadratic relationship (P < .001) (Figs 2 and 3). The mean clival-dens angle was 30°(1° to 58°). The mean coronal reconstruction plane angle was 5.6° (−17° to 54°). Multivariate logistic regression analysis revealed no significant relationship between mean sagittal/coronal CCI and subject sex, investigator, clival-dens angle, or coronal reconstruction angle.
Fig 2.
Scatterplots representing each of the 248 joint spaces in the coronal (A) and sagittal (B) planes.
Fig 3.
Average CCI by age group in the coronal (A) and sagittal (B) planes. The gray box represents ±1 SD, and the bars represent ±2 SDs from the mean.
The mean absolute variance in measurement between the investigators for the 45 subjects measured by both investigators was 0.19 ± 0.17 mm in the sagittal plane and 0.27 ± 0.28 mm in the coronal plane. Subset analysis of measurement variance in younger (13 years or younger) versus older (14 years and older) subjects revealed an SD of 0.18 versus 0.09 mm (P = .001) in the sagittal plane and 0.30 versus 0.09 mm (P = < .001) in the coronal plane, respectively.
Across all subjects, the mean absolute difference (ie, asymmetry) between the right and left CCI in the sagittal plane was 0.218 mm (95% CI, 0.186–0.249 mm) and the mean difference between the right and left CCI in the coronal plane was 0.252 mm (95% CI, 0.208–0.296 mm).
Analysis of measurement variance based on measurement location within the joint space in the sagittal plane showed a trend toward greater variability in the posterior measurement (0.56 mm) compared with the anterior measurement (0.39 mm), but the trend was not statistically significant (P = .06). The same analysis in the coronal plane showed significantly greater variability of the medial measurements (1.53 mm) compared with the lateral measurements (0.32 mm) in the coronal plane (P = .001).
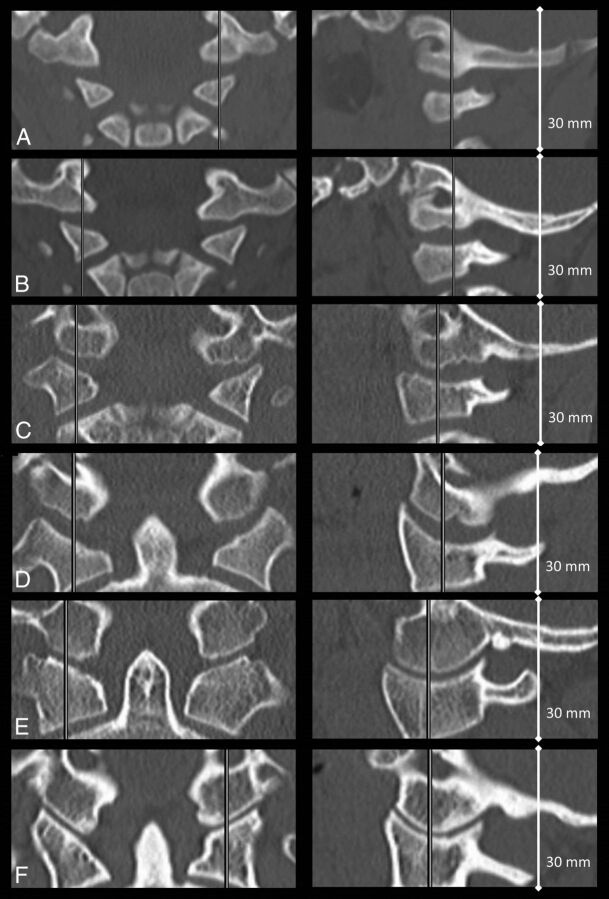
To evaluate the morphologic changes that occur in the coronal plane, the examiners calculated the difference between lateralmost and medialmost measurements by age group and revealed the following: <12 months (1.39 mm, P < .001), 12–24 months (1.84 mm, P < .001), 2–4 years (2.07 mm, P < .001), 5–8 years (1.56 mm, P < .001), 9–12 years (1.21 mm, P < .001), 13–17 years (0.42 mm, P < .001), and older than 17 years (0.115 mm; P = .078). Examples from this study of the age-related changes in the morphology of the occipital condyle and occipital condyle-C1 articulation throughout childhood and young adulthood are given in Fig 4.
Fig 4.
Coronal (left) and sagittal (right) images of the CCI in subjects of the following ages: 3 months (A), 1.5 years (B), 4 years (C), 9 years (D), 17 years (E), and 22 years (F).
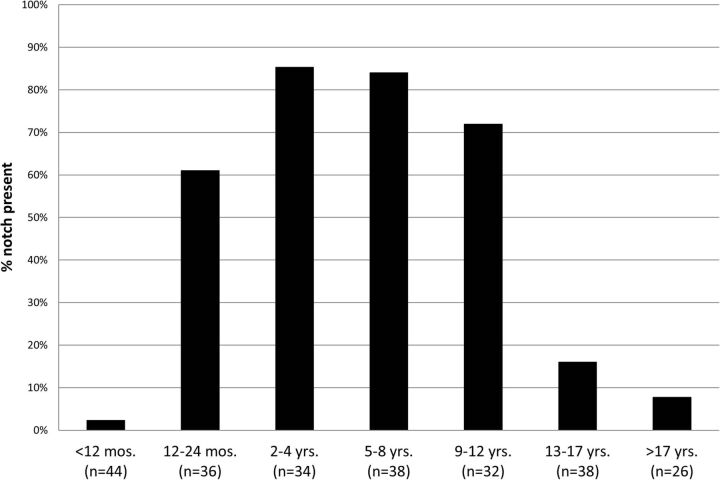
The medial occipital condyle notch (Fig 5) was first detected in a subject at 12 months of age and was very uncommon after 13 years of age. The prevalence of the notch peaked in the 2- to 4-year (85.3%) and 5- to 8-year age groups (84%) and became less frequent throughout life (Fig 6). The prevalence of the notch was age-dependent (P < .001).
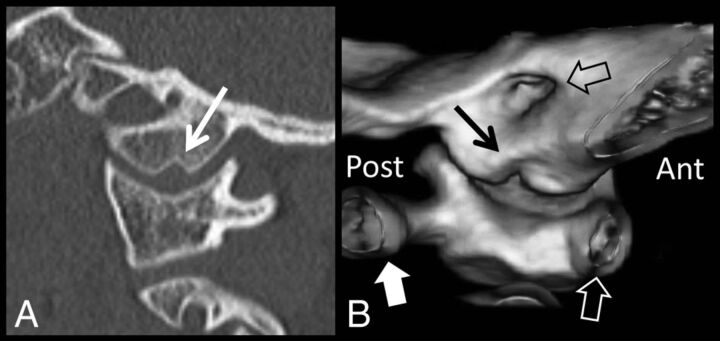
Fig 5.
Sagittal CT (A) demonstrates the medial occipital condyle notch (white arrow) in an 8-year-old boy. A 3D surface-rendered reconstruction image (B) with a medial-to-lateral perspective demonstrates the 3D contour of the occipital condyle notch (black arrow). For orientation, the anterior arch of C1 (white hollow arrow) is to the right and the posterior arch of C1 (white block arrow) is to the left. The internal auditory canal is shown by a hollow black arrow. Note how the notch is wider at its medial aspect compared with the lateral aspect. Ant indicates anterior; post, posterior.
Fig 6.
Prevalence of the medial occipital condyle notch by age group.
Discussion
In our clinical practice, we have been frequently asked by our neurosurgical colleagues to evaluate the CCI in patients with trauma and have often identified joint spaces in young subjects that were much larger than those in older patients, contradicting prior studies.2 In addition, we noted that the occipital condyle and CCI interval undergo significant morphologic changes throughout development (Fig 4), making it challenging to apply previously published normative data. All prior investigations into the normative values and age-related changes in the CCI in the pediatric population2–4 have some limitations (Table), decreasing widespread applicability in children.
Comparison of investigations of the normal CCI to date, including this study
| Investigator | Cohort Size | Mean CCI (mm) | Mean Age (Range) | Age-Dependent? | Sag/Cor Measure | Subjects with Trauma |
|---|---|---|---|---|---|---|
| Pang et al1 (2007) | 89 | 1.28 | 56 Months (6 months to 17.1 years) | No | Sag/Cor (avg. 4 measures) | 80% |
| Bertozzi et al3 (2009) | 117 | 1.6 | 56 Months (2 months to 10 years) | Not examined | Sag (avg. 5 measures) | 100% |
| Vachhrajani et al4 (2014) | 42 | 2.38 | 100 Months (1 month to 17.8 years) | Yes | Cor (1 measure) | 86% |
| Current study (2015) | 124 | 0.90–2.4 | 94 Months (2 months to 22 years) | Yes | Sag/Cor (avg. 4 measures) | 0% |
Note:—Sag indicates sagittal; cor, coronal; avg., average.
Prior studies of the CCI interval have primarily assessed patients with trauma,2–4 leaving whether these are truly representative of a normative population up to debate. Bertozzi et al3 and Vachhrajani et al4 both focused on myriad craniocervical junction anatomic measurements, with less focus on the CCI. Both of these studies included measurements of the joint in only a single plane (Bertozzi et al, sagittal; Vachhrajani et al, coronal), and in the case of Vachhrajani et al, only a single measurement in the center of the joint was used. Pang et al2 had the most rigorous investigation of the CCI, with 4 measurements in each plane. The average CCI varied substantially among these 3 studies, with nearly a 2-fold difference between the results of Pang et al (1.28 mm) and Vachhrajani et al (2.4 mm).
We were unable to reproduce the findings of Pang et al,2 who demonstrated no significant age-related changes in the CCI. According to our findings, the CCI morphology and average measurements change substantially with development, with an increase in the first several years of life before a steady decline in the later childhood and early teenage years. The etiology of this initial increase is not completely understood but corresponds to increased prevalence of the medial occipital notch. Despite meticulous effort in our study to exclude the notch, its presence may contribute to this initial increase, particularly in the coronal plane. We hypothesize that the notch has a fanlike shape, with the more medial part of the notch having a greater anteroposterior dimension than the lateral aspect of the notch. This would explain the large difference between medialmost and lateralmost CCI joint space measurements in the coronal plane. The progressive decrease in average CCI joint space from the 2- to 4-year period until the later teenage years is a common trajectory for most joints of the human body.5–8 As with most synovial joint spaces in the body, the occipital condyle and C1 lateral mass components of the CCI undergo progressive ossification of cartilage, leading to a decrease in the “osseus” joint space detected on CT.
While the scatterplots and age group data give an overall sense of the change in average CCI with time, examination of specific parts of the joint (ie, medial versus lateral) is also very informative. Figure 4 shows the striking change in morphology of the CCI that occurs during the early months and years of human development. Anecdotally, one of the most apparent features of the CCI that changes with time is the difference between medial and lateral joint space in the coronal plane. Our measurement data bear this out, with the average medialmost coronal measurement being significantly greater and more variable than the lateralmost measurement in younger age groups. In contrast to the younger subjects, within the oldest age group, the variance and measurement difference between the medialmost and lateralmost joint spaces are small. With this understanding in mind, it is not surprising that Vachhrajani et al4 found this large mean CCI measurement with high variability, considering that they only made a single measurement in the coronal plane.
Prior work by Pang et al2 examining the clinical utility of the CCI measurement found it to be a specific and sensitive means for detecting atlanto-occipital dislocation, with a cutoff value of 4 mm. In their investigation, Pang et al assumed no change in the CCI measurements with age, which does not agree with the findings of our study. Most interesting, a more recent investigation by Gire et al9 advocated an even more aggressive abnormal CCI cutoff value of 2.5 mm to detect AOD in all age groups, but this study did not include any control subjects less than 18 years of age to define the false-positive rate in children. Our study would suggest a very high false-positive rate in the age range of 1–12 years by using a cutoff value of 2.5 mm, given that this value is within 1 or 2 SDs of the mean for these age groups. Our data would support using the more conservative abnormal cutoff of 4 mm (Pang et al) for infants and children younger than 13 years, to avoid false-positives, while in older teens and young adults, the more aggressive abnormal cutoff of 2.5 mm proposed by Gire et al may be valid.
This study underscores the need for surgeons and imaging professionals to understand the normal dynamic changes that the occipital condyle-C1 joint space undergoes in the early years of life. Using medial occipital condyle-C1 joint space measurements in the coronal plane in young children will inevitably result in false-positives if the aforementioned cutoff values of 2.5 and 4 mm are applied. We recommend using multiple measurements obtained in the sagittal plane at the midjoint, with special care to exclude the medial occipital condyle notch to avoid such false-positives.
Additionally, an understanding of medial occipital condyle notch prevalence can help the imaging professional avoid falsely identifying asymmetry between the joint spaces on coronal images. In young subjects in whom the prevalence of a notch is high, on any given coronal image, one side may be located within the notch while the other is not. In this scenario, an apparent asymmetry between the joint spaces will inevitably be present. When assessing for asymmetry, one should pay careful attention to the location of the medial occipital condyle notch for each joint space to prevent a false-positive result.
We hope that these normative data will be applied to patient populations with documented atlanto-occipital injury to assess the clinical utility and establish more age-appropriate abnormal cutoff values.
Conclusions
The null hypothesis is rejected. The average CCI increases during the first several years of life, is largest in the 2–4 year range, and then decreases through late childhood and adolescence. Average coronal measurements are larger and more variable than sagittal measurements, especially in younger patients, an age when the prevalence of the medial occipital notch is highest. These dynamic changes suggest that a single threshold value to detect atlanto-occipital dissociation may not be sensitive and specific for all age groups. Application of these normative data to documented cases of atlanto-occipital injury is needed to determine clinical utility.
ABBREVIATION:
- CCI
occipital condyle-C1 interval
Footnotes
Paper previously presented as an oral presentation at: American Society of Neuroradiology Annual Meeting and the Foundation of the ASNR Symposium, April 25–30, 2015; Chicago, Illinois.
References
- 1. Pang D, Nemzek WR, Zovickian J. Atlanto-occipital dislocation, part 2: the clinical use of (occipital) condyle-C1 interval, comparison with other diagnostic methods, and the manifestation, management, and outcome of atlanto-occipital dislocation in children. Neurosurgery 2007;61:995–1015; discussion 1015 10.1227/01.neu.0000303196.87672.78 [DOI] [PubMed] [Google Scholar]
- 2. Pang D, Nemzek WR, Zovickian J. Atlanto-occipital dislocation: part 1–normal occipital condyle-C1 interval in 89 children. Neurosurgery 2007;61:514–21; discussion 521 10.1227/01.NEU.0000290897.77448.1F [DOI] [PubMed] [Google Scholar]
- 3. Bertozzi JC, Rojas CA, Martinez CR. Evaluation of the pediatric craniocervical junction on MDCT. AJR Am J Roentgenol 2009;192:26–31 10.2214/AJR.08.1058 [DOI] [PubMed] [Google Scholar]
- 4. Vachhrajani S, Sen AN, Satyan K, et al. Estimation of normal computed tomography measurements for the upper cervical spine in the pediatric age group. J Neurosurg Pediatr 2014;14:425–33 10.3171/2014.7.PEDS13591 [DOI] [PubMed] [Google Scholar]
- 5. Greulich WW, Pyle SI. Radiographic Atlas of Skeletal Development of the Hand and Wrist. Stanford: Stanford University Press; 1959 [Google Scholar]
- 6. Santiago RC, de Miranda Costa LF, Vitral RW, et al. Cervical vertebral maturation as a biologic indicator of skeletal maturity. Angle Orthod 2012;82:1123–31 10.2319/103111-673.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wientroub S, Tardiman R, Green I, et al. The development of the normal infantile hip as expressed by radiological measurements. Int Orthop 1981;4:239–41 [DOI] [PubMed] [Google Scholar]
- 8. Kaawach W, Ecklund K, Di Canzio J, et al. Normal ranges of scapholunate distance in children 6 to 14 years old. J Pediatr Orthop 2001;21:464–67 10.1097/01241398-200107000-00010 [DOI] [PubMed] [Google Scholar]
- 9. Gire JD, Roberto RF, Bobinski M, et al. The utility and accuracy of computed tomography in the diagnosis of occipitocervical dissociation. Spine J 2013;13:510–19 10.1016/j.spinee.2013.01.023 [DOI] [PubMed] [Google Scholar]