Abstract
BACKGROUND AND PURPOSE:
The trochlear groove and trochlear cistern are anatomic landmarks closely associated with the tentorial segment of cranial nerve IV. The purposes of this study were to describe the MR imaging appearances of the trochlear groove and trochlear cistern and to test our hypothesis that knowledge of these anatomic landmarks facilitates identification of cranial nerve IV in routine clinical practice.
MATERIALS AND METHODS:
For this retrospective study, consecutive MR imaging examinations of the sinuses performed in 25 patients (50 sides) at our institution were reviewed. Patient characteristics and study indications were recorded. Three readers performed independent assessments of trochlear groove, cistern, and nerve visibility on coronal images obtained by using a T2-weighted driven equilibrium radiofrequency reset pulse sequence.
RESULTS:
Interobserver agreement was 78% for visibility of the trochlear groove, 56% for the trochlear cistern, and 68% for cranial nerve IV. Following consensus review, the trochlear groove was present in 44/50 sides (88%), the trochlear cistern was present in 25/50 sides (50%), and cranial nerve IV was identified in 36/50 sides (72%). When the trochlear groove was present, cranial nerve IV was identified in 35/44 sides (80%), in contrast to 1/6 sides (17%) with no groove (P = .0013). When the trochlear cistern was present, cranial nerve IV was identified in 23/25 sides (92%), in contrast to 13/25 sides (52%) with no cistern (P = .0016).
CONCLUSIONS:
The trochlear groove and trochlear cistern are anatomic landmarks that facilitate identification of cranial nerve IV in routine clinical practice.
Historically, imaging of cranial nerve IV has been difficult.1,2 These difficulties likely relate to the small size of the nerve and the presence of numerous adjacent blood vessels in the quadrigeminal and ambient cisterns.3,4 These difficulties are compounded by the fact that MR images are often acquired in the axial plane, nearly parallel to the cisternal course of the nerve.
In research settings, high-resolution MR images have reliably demonstrated cranial nerve IV in healthy volunteers; however, long acquisition times ranging from 7 to 26 minutes make these sequences impractical for routine clinical use.3,5,6 Acknowledging the perceived impracticality of consistently identifying cranial nerve IV in routine practice, more recently published work has proposed using volumetric analyses of the superior oblique muscles as a correlate for the presence or absence of cranial nerve IV in patients with congenital superior oblique palsy.7 However, the ability to reliably identify the nerve itself can be important in identifying underlying pathology and can aid in treatment and surgical planning.3,8
Various segments and subsegments have been proposed to describe the course of cranial nerve IV distal to its exit from the dorsal midbrain and proximal to its entrance into the cavernous sinus.3,4,6,9–11 Some authors consider the tentorial segment to be the distal subdivision of the cisternal segment,3,6,9,10 and others describe the tentorial segment as distinct from the cisternal segment of cranial nerve IV.4,11 However, there is generally agreement that the tentorial segment of cranial nerve IV begins when the nerve becomes closely associated with the inferior aspect of the cerebellar tentorium and ends at the entrance of the nerve to the cavernous sinus.
Cadaveric dissections have shown that the tentorial segment of cranial nerve IV travels within a shallow groove (Fig 1) inferolateral to the free tentorial edge en route to the cavernous sinus, and this shallow groove has been referred to as the “trochlear groove.”4,9,10,12 After passing through the trochlear groove but before entering the cavernous sinus, the tentorial segment of cranial nerve IV pierces the tentorium to course a short distance through the posterior petroclinoid fold.4,13 The space through which cranial nerve IV passes in the posterior petroclinoid fold may contain CSF and has been referred to as the “trochlear cistern” (Fig 2).4 These findings are consistent with the common progression of the cranial nerves through a transitional “dural cave segment” in their course from the intracranial to the extracranial compartment.14
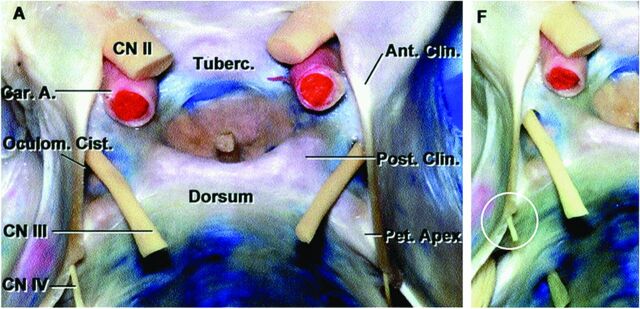
Fig 1.
Labeled (A) and unlabeled (F) anterosuperior views of the sella and suprasellar region demonstrate cranial nerve IV passing into the trochlear groove (circle, F). Car.A. indicates carotid artery; Oculom., oculomotor; Post., posterior; Ant., anterior; Cist., cistern; Tuberc., tuberculum; Clin., clinoid; Pet. Apex, petrous apex. Modified with permission from Rhoton AL Jr. The sellar region. Neurosurgery 2002;51(4 suppl):S335–74.12
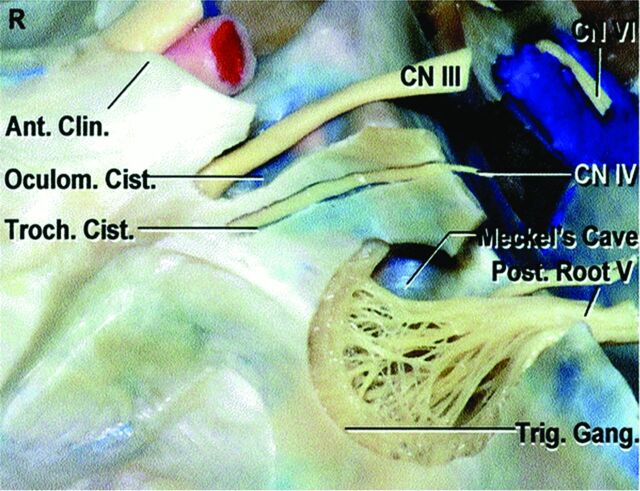
Fig 2.
Lateral view of the right cavernous sinus demonstrates cranial nerve IV traveling within the trochlear cistern immediately proximal to entering the cavernous sinus. The trochlear cistern is located inferior to the oculomotor cistern and superior to the Meckel cave. Troch. indicates trochlear; Trig. Gang., trigeminal ganglion. Modified with permission from Rhoton AL Jr. The cavernous sinus, the cavernous venous plexus, and the carotid collar. Neurosurgery 2002;51(4 suppl):S375–410.16
Coronal 2D T2-weighted driven equilibrium radiofrequency reset pulse (coronal T2 DRIVE) is a fluid-sensitive MR sequence commonly performed during sinus MR imaging examinations at our institution. We have observed cranial nerve IV within both the trochlear groove (Fig 3) and the trochlear cistern (Fig 4) on clinical images obtained with this sequence. With respect to the more easily identifiable cranial nerve V, the trochlear groove is typically seen on coronal images at the level of the trigeminal nerve cisternal segment and the trochlear cistern is seen at the level of the Meckel cave.
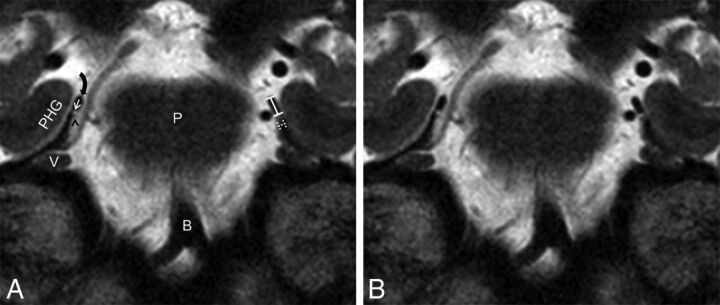
Fig 3.
Labeled (A) and unlabeled (B) coronal T2 DRIVE images demonstrate cranial nerve IV (black arrowhead on the patient's right) in cross-section traveling along the bilateral trochlear grooves (straight white arrow on the patient's right). The right tentorial free edge (curved black arrow), right cranial nerve V (V), right parahippocampal gyrus (PHG), belly of the pons (P), and basilar artery (B) are labeled for orientation. The dashed lines on the patient's left illustrate the measurement of the maximum trochlear groove depth, and the solid lines on the patient's left illustrate the measurement of the shortest distance between the free tentorial edge and the medial border of the trochlear groove.
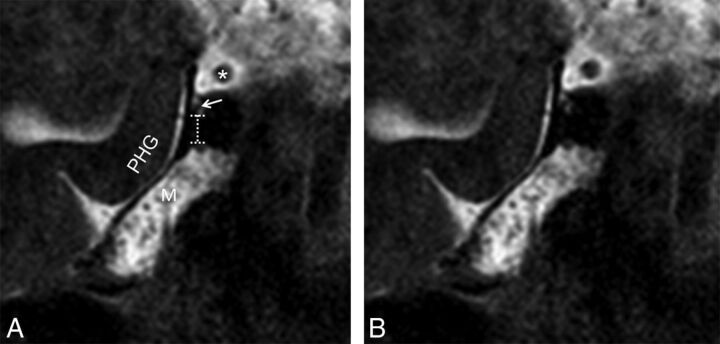
Fig 4.
Labeled (A) and unlabeled (B) coronal T2 DRIVE images demonstrate cranial nerve IV (white arrow) in cross-section within the right trochlear cistern. The right cranial nerve III (asterisk), right Meckel cave (M), and right parahippocampal gyrus (PHG) are labeled for orientation. The dashed lines illustrate the measurement of the vertical distance between the inferior margin of the trochlear cistern and the superior margin of the Meckel cave.
We hypothesized that knowledge of these anatomic landmarks will facilitate identification of the tentorial segment of cranial nerve IV in routine clinical practice.
The purposes of this study were to describe the MR imaging appearances of the trochlear groove and trochlear cistern and to test our hypothesis regarding the utility of these landmarks for identifying cranial nerve IV.
Materials and Methods
Subjects
For this Health Insurance Portability and Accountability Act–compliant, institutional review board–approved study, all sinus MR imaging examinations performed at Massachusetts Eye and Ear between December 1, 2015, and April 1, 2016, were retrospectively reviewed. Inclusion criteria were the following: 1) older than 18 years of age, 2) coronal T2 DRIVE sequence performed, and 3) no superior oblique palsy documented in the patient's electronic medical record. Twenty-five MR imaging examinations in 25 patients met the inclusion criteria and were included in the study. Patient characteristics and study indications were recorded.
To maximize generalizability and to best simulate routine clinical practice, we did not exclude examinations containing motion, pulsation, and other MR imaging artifacts from our study.
Image Acquisition
All examinations were performed on a 3T scanner (Achieva; Philips Healthcare, Best, the Netherlands) by using an 8-channel head coil (SENSE Flex M coil; Philips Healthcare).
The coronal T2 DRIVE sequence acquisition parameters for the study group were as follows: TR, 3369–6355 ms; TE, 100 ms; echo-train length, 11; FOV, 120–160 mm; matrix, 324 × 300 to 456 × 454; voxel size, from 0.3 × 0.35 × 3.0 to 0.4 × 0.44 × 3.0; gap, 0.3 (n = 12) or 1 mm (n = 13); NEX, 1 (n = 15) or 2 (n = 10). These acquisition parameters resulted in a mean sequence acquisition time of 3 minutes 54 seconds ± 37 seconds (range, 2 minutes 54 seconds–5 minutes).
Reader Assessment
Anatomic Structures.
After a brief self-guided training session based on 10 sinus MR imaging examinations not included in the study group, 3 radiologists independently reviewed the coronal T2-DRIVE sequences for the 25 patients in the study group with the Massachusetts Eye and Ear PACS. The radiologists included 2 fellowship-trained neuroradiologists (6 and 3 years' subspecialty experience) and 1 neuroradiology fellow. They were asked to determine whether the trochlear groove, trochlear cistern, and cranial nerve IV were identifiable on each side in all patients, and discrepancies were resolved by consensus review. To be considered “identifiable,” the tentorial segment of cranial nerve IV had to be identified by the radiologist on at least 2 images for a given side, though the images did not have to be contiguous.
Artifacts.
Potential confounding effects of MR imaging artifacts (motion, pulsation, and so forth) on cranial nerve IV visibility were assessed by consensus. Sequences were designated as containing artifacts that would “not preclude nerve identification,” “possibly preclude nerve identification,” or “likely preclude nerve identification.” This consensus review was performed 3 weeks following the anatomic structure identification consensus review to minimize potential for recall bias.
Measurements
When the anatomic structures of interest were identified, related measurements were obtained. For the trochlear groove, the maximum groove depth and the shortest distance between the free tentorial edge and the medial border of the groove were measured (Fig 3A). For the trochlear cistern, the vertical distance between the inferior margin of the trochlear cistern and the superior margin of the Meckel cave was measured (Fig 4A). For the tentorial segment of cranial nerve IV, the cross-sectional nerve diameter was measured.
Statistical Analysis
Mean, SD, and range are reported for continuous variables. Absolute and relative frequencies are reported for categoric variables. The Pearson χ2 test was used to compare proportions. For statistical analysis, consensus opinion regarding the identification of the trochlear groove and trochlear cistern was taken to indicate the “presence” or “absence” of these landmarks. Consensus opinion regarding identification of cranial nerve IV indicated whether the nerve was “identifiable” or “not identifiable.” JMP Pro, Version 12 (SAS Institute, Cary, North Carolina) was used for all analyses, and a P value < .05 indicated a statistically significant difference.
Results
Subjects
To reach a study group of 25 patients and 50 sides, we reviewed 32 examinations. Seven examinations were excluded for not containing the coronal T2 DRIVE sequence of interest. Patient age and sex and study indication data are provided in the Table.
Characteristics of the study group
| Characteristics | No. (%) |
|---|---|
| Sex | |
| Male | 9 (36%) |
| Female | 16 (64%) |
| Age (yr) | |
| Mean | 56.2 |
| SD | 13.8 |
| Max | 85 |
| Min | 30 |
| Indication | |
| Sinonasal carcinoma | 6 |
| Inverted papilloma | 4 |
| Adenoid cystic carcinoma | 2 |
| Other (n = 1 each) | 13 |
Note:—Max indicates maximum; Min, minimum.
Reader Assessment
Anatomic Structures.
Interobserver agreement was 78% for identification of the trochlear groove, 56% for the trochlear cistern, and 68% for cranial nerve IV.
Following consensus review, the trochlear groove was present in 44/50 sides (88%), and the trochlear cistern was present in 25/50 sides (50%). In 46/50 sides (92%), either the trochlear groove or trochlear cistern was present. The tentorial segment of cranial nerve IV was identified in 36/50 sides (72%). When the trochlear groove was present, cranial nerve IV was identified in 35/44 sides (80%), in contrast to 1/6 sides (17%) with no groove. This observed difference in proportions was statistically significant (P = .0013). When the trochlear cistern was present, cranial nerve IV was identified in 23/25 sides (92%), in contrast to 13/25 sides (52%) with no cistern. This observed difference in proportions was also statistically significant (P = .0016).
When neither the trochlear groove nor trochlear cistern was present, cranial nerve IV was identified in 0/4 sides (0%), in contrast to 36/46 sides (78%) with at least 1 landmark present (P = .0008).
Artifacts.
None of the coronal T2 DRIVE sequences were considered to contain artifacts that would “likely preclude nerve identification,” and 4 examinations (8 sides) were thought to contain artifacts that would “possibly preclude nerve identification.” Among these 4 examinations with artifacts that would possibly preclude nerve identification, cranial nerve IV was identified in 5/8 sides (63%). If these 8 sides had been initially excluded, the observed differences in proportions between cranial nerve IV identification in the presence and absence of the trochlear groove and trochlear cistern would have remained statistically significant (P = .0196 and .0082, respectively).
Measurements
When present, the trochlear groove was located a mean distance of 1.4 ± 0.44 mm inferolateral to the free tentorial edge (range, 0.7–2.4 mm), and the mean maximum groove depth was 0.5 ± 0.15 mm (range, 0.2–0.8 mm). When present, the trochlear cistern was located a mean distance of 3.7 ± 1.8 mm superior to the Meckel cave (range, 1.2–7.0 mm). When identified, the mean diameter of the tentorial segment of cranial nerve IV was 0.4 ± 0.07 mm (range. 0.2–0.6 mm).
Discussion
This study describes the MR imaging appearances of the trochlear groove and trochlear cistern on a fluid-sensitive sequence used in our routine clinical practice and demonstrates that successfully identifying these anatomic landmarks facilitates identification of the tentorial segment of cranial nerve IV.
Recent neurosurgical studies report that the trochlear groove and trochlear cistern are present in up to 100% of cadaver specimens and represent reliable anatomic landmarks for intraoperative nerve identification.9,11 We identified the trochlear groove in 88% of sides and the trochlear cistern in 50% of sides, with at least 1 of these landmarks seen in 92% of sides. The discrepancy in rates of landmark identification between the current MR imaging–based study and previous cadaveric studies likely reflects limitations of the coronal T2 DRIVE sequence for resolving these small structures, with the increased length of the trochlear groove relative to the trochlear cistern likely contributing to its relatively increased visibility.
We identified the tentorial segment of cranial nerve IV in 72% of total sides, 80% of sides in which the trochlear groove was present, and 92% of sides in which the trochlear cistern was present. Although these results for the tentorial segment of cranial nerve IV do not match those previously reported by Kanoto et al,6 who used a high-resolution motion-sensitized driven equilibrium sequence with a 26-minute acquisition time in a population of healthy volunteers, the coronal T2 DRIVE sequence investigated in our study with an average acquisition time of <4 minutes is more likely to be of practical benefit when daily MR imaging volume imposes sequence acquisition time constraints. Additionally, patients being evaluated for cranial nerve deficits may be less likely to remain motionless during longer sequence acquisitions than healthy volunteers; this scenario may result in image-quality degradation. Image-acquisition parameters were not the focus of this study, and it is possible that the coronal T2 DRIVE sequence or a similar fluid-sensitive sequence could be modified to improve visualization of the trochlear groove, trochlear cistern, and cranial nerve IV without meaningfully prolonging the acquisition.
Regardless of the particular sequence used, there are multiple clinical scenarios in which it is important for the radiologist to provide an accurate imaging assessment of cranial nerve IV, including suspected congenital absence of the nerve, involvement of the nerve by schwannoma or perineural spread of malignancy, trauma to the nerve related to penetrating injury or shear forces, and extrinsic compression of the nerve by a skull base mass, aneurysm, or crossing vessel.
Operative planning for skull base mass resection likely represents the scenario in which the radiologist has the greatest opportunity to positively impact patient care, because cranial nerve IV palsy is the most frequent complication following meningioma surgery in the region of the tentorial incisura.15 The frequency of this complication has been hypothesized to reflect difficulty in identifying and preserving the nerve at the time of the operation related to the small diameter of the nerve and displacement and distortion of the nerve along its lengthy intracranial course.9–11
The relatively low interobserver agreement for the presence of the trochlear groove, trochlear cistern, and cranial nerve IV likely reflects both the difficulty of confidently identifying these small structures noninvasively and the relatively limited self-guided training of the readers before completing the study interpretations. Interobserver agreement may have been improved with a more extensive group training session before performing the study, and given that consensus was easily reached in all discrepant cases, we expect interobserver agreement to improve with continued experience.
A limitation of this study is that we were not able to confirm the presence of cranial nerve IV along its entire cisternal length, though the nerve had to be present on at least 2 images to be considered “identifiable.” In the evaluation of patients with trochlear nerve palsy at our institution, we have observed cases in which the nerve could be reliably identified along most of its course on the normal side but could not be seen within the trochlear groove or trochlear cistern on the contralateral, symptomatic side (Fig 5). Although anecdotal, the “empty” trochlear groove and “empty” trochlear cistern in such patients may represent important imaging findings.
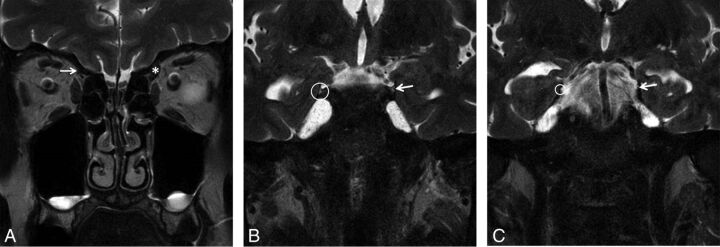
Fig 5.
A, Coronal T2 DRIVE image obtained in a 47-year-old woman with clinically suspected congenital right trochlear palsy demonstrates a markedly diminutive right superior oblique muscle (arrow). The left superior oblique muscle (asterisk) is normal. Coronal T2 DRIVE images obtained in the same patient demonstrate the presence of the trochlear nerve within the trochlear groove (arrow, B) and trochlear cistern (arrow, C) on the normal left side. On the symptomatic right side, the trochlear groove (circle, B) and trochlear cistern (circle, C) can be seen clearly; however, no nerve can be identified.
An additional weakness of this study is the exclusion of pediatric patients, who represent a substantial proportion of patients being evaluated for suspected cranial nerve IV pathology and most patients with suspected congenital palsy.
Additional work could optimize sequence acquisition parameters for the visualization of the trochlear groove, trochlear cistern, and tentorial segment of cranial nerve IV; determine whether the trochlear groove and trochlear cistern are present in patients with congenital absence of cranial nerve IV; and assess whether the trochlear groove and trochlear cistern in combination with the coronal T2 DRIVE sequence or a sequence similar to it could be used for the following: 1) to identify cranial nerve IV in pediatric patients, 2) to reliably determine the presence or absence of cranial nerve IV, 3) to facilitate preoperative identification of cranial nerve IV in patients with skull base masses, or 4) to have a measurable effect on the historically high cranial nerve IV palsy complication rate following resection of tentorial meningiomas.
Conclusions
The trochlear groove and trochlear cistern are anatomic landmarks with which the tentorial segment of cranial nerve IV is closely associated en route to the cavernous sinus. These landmarks can be reliably identified by using a fluid-sensitive MR sequence and may improve the chances of identifying cranial nerve IV in routine clinical practice. These findings are expected to improve diagnostic confidence and diagnostic accuracy in the MR imaging evaluation of patients with suspected cranial nerve IV pathology.
ABBREVIATION:
- coronal T2 DRIVE
coronal 2D T2-weighted driven equilibrium radiofrequency reset pulse
Footnotes
Paper previously represented, in part, as an oral scientific presentation entitled “The Trochlear Groove: A Useful Anatomic Landmark for Identifying Cranial Nerve IV” at: Annual Meeting of the American Society of Head and Neck Radiology, September 7–11, 2016; Washington, DC.
REFERENCES
- 1. Fischbach F, Müller M, Bruhn H. High-resolution depiction of the cranial nerves in the posterior fossa (N III-N XII) with 2D fast spin echo and 3D gradient echo sequences at 3.0 T. Clin Imaging 2009;33:169–74 10.1016/j.clinimag.2008.09.012 [DOI] [PubMed] [Google Scholar]
- 2. Yousry I, Camelio S, Schmid UD, et al. Visualization of cranial nerves I-XII: value of 3D CISS and T2-weighted FSE sequences. Eur Radiol 2000;10:1061–67 10.1007/s003300000452 [DOI] [PubMed] [Google Scholar]
- 3. Yousry I, Moriggl B, Dieterich M, et al. MR anatomy of the proximal cisternal segment of the trochlear nerve: neurovascular relationships and landmarks. Radiology 2002;223:31–38 10.1148/radiol.2231010612 [DOI] [PubMed] [Google Scholar]
- 4. Joo W, Rhoton AL. Microsurgical anatomy of the trochlear nerve. Clin Anat 2015;28:857–64 10.1002/ca.22602 [DOI] [PubMed] [Google Scholar]
- 5. Choi BS, Kim JH, Jung C, et al. High-resolution 3D MR imaging of the trochlear nerve. AJNR Am J Neuroradiol 2010;31:1076–79 10.3174/ajnr.A1992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kanoto M, Toyoguchi Y, Hosoya T, et al. Visualization of the trochlear nerve in the cistern with use of high-resolution turbo spin-echo multisection motion-sensitized driven equilibrium. AJNR Am J Neuroradiol 2013;34:1434–37 10.3174/ajnr.A3403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yang HK, Lee DS, Kim JH, et al. Association of superior oblique muscle volumes with the presence or absence of the trochlear nerve on high-resolution MR imaging in congenital superior oblique palsy. AJNR Am J Neuroradiol 2015;36:774–78 10.3174/ajnr.A4202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Blitz AM, Macedo LL, Chonka ZD, et al. High-resolution CISS MR imaging with and without contrast for evaluation of the upper cranial nerves: segmental anatomy and selected pathologic conditions of the cisternal through extraforaminal segments. Neuroimaging Clin N Am 2014;24:17–34 10.1016/j.nic.2013.03.021 [DOI] [PubMed] [Google Scholar]
- 9. Herlan S, Hirt B, Tatagiba M, et al. Focus on the lateral incisural space: where is the trochlear nerve? J Neurol Surg B Skull Base 2013;74:271–73 10.1055/s-0033-1347899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ammirati M, Musumeci A, Bernardo A, et al. The microsurgical anatomy of the cisternal segment of the trochlear nerve, as seen through different neurosurgical operative windows. Acta Neurochir (Wien) 2002;144:1323–27 10.1007/s00701-002-1017-3 [DOI] [PubMed] [Google Scholar]
- 11. Gupta T, Gupta SK, Sahni D. Anatomy of the tentorial segment of the trochlear nerve in reference to its preservation during surgery for skull base lesions. Surg Radiol Anat SRA 2014;36:967–71 10.1007/s00276-014-1278-6 [DOI] [PubMed] [Google Scholar]
- 12. Rhoton AL Jr. The sellar region. Neurosurgery 2002;51(4 suppl):S335–74 [PubMed] [Google Scholar]
- 13. Iaconetta G, de Notaris M, Benet A, et al. The trochlear nerve: microanatomic and endoscopic study. Neurosurg Rev 2013;36:227–37; discussion 237–38 10.1007/s10143-012-0426-x [DOI] [PubMed] [Google Scholar]
- 14. Blitz AM, Choudhri AF, Chonka ZD, et al. Anatomic considerations, nomenclature, and advanced cross-sectional imaging techniques for visualization of the cranial nerve segments by MR imaging. Neuroimaging Clin N Am 2014;24:1–15 10.1016/j.nic.2013.03.020 [DOI] [PubMed] [Google Scholar]
- 15. Samii M, Carvalho GA, Tatagiba M, et al. Meningiomas of the tentorial notch: surgical anatomy and management. J Neurosurg 1996;84:375–81 10.3171/jns.1996.84.3.0375 [DOI] [PubMed] [Google Scholar]
- 16. Rhoton AL Jr. The cavernous sinus, the cavernous venous plexus, and the carotid collar. Neurosurgery 2002;51(4 suppl):S375–410 [PubMed] [Google Scholar]