Abstract
Analysis of a nationally representative sample of emergency department visits revealed that children from lower-income neighborhoods were more likely to receive care in emergency departments with lower pediatric volume, an association largely driven by urban-rural differences in access to emergency care.
Keywords: access, emergency department, geographic access, pediatric, socioeconomic status
Introduction
Disparities by socioeconomic status (SES) exist in the delivery and outcomes of emergency care for children. In the emergency department (ED), children who are publicly insured or uninsured, receive less diagnostic testing than privately insured children.(1–3) Children who live in low-income neighborhoods and those who lack insurance also experience worse outcomes and higher mortality rates in the ED.(4,5)
ED characteristics are also a major determinant of outcomes for children. The majority of ED visits by children in the United States are made to general EDs, with only approximately 10% occurring in pediatric EDs.(6) Many general EDs care for low volumes of children, limiting the experience and comfort of providers with diagnosing and managing pediatric-specific conditions.(7,8) Lower-pediatric-volume EDs are also less likely to have pediatric-specific resources and policies to facilitate readiness to provide emergency care for children when compared to high-pediatric-volume EDs.(9) Less experience in caring for pediatric patients may result in reduced capability to provide definitive care for common pediatric complaints resulting in higher rates of transfers to children’s hospitals,(10–12) more frequent misdiagnosis of emergent conditions,(13) and poorer health outcomes among critically ill children.(14)
Prior studies demonstrate that racial and ethnic minority adults are significantly less likely to visit hospitals with high patient volumes,(15,16) with their care concentrated in hospitals with generally worse performance.(17) However, how demographic factors influence care-seeking patterns among children is less well understood. Understanding where children of different SES backgrounds receive emergency care may provide insight into the underlying causes of differences in care and disparities in outcomes among children in the ED. Therefore, we sought to determine the association of neighborhood income and insurance type, two markers of socioeconomic status, with characteristics of the EDs children visit.
Methods
We conducted a cross-sectional analysis of ED visits among patients less than 18 years of age from 2014 to 2017 using the Nationwide Emergency Department Sample (NEDS).(18) The NEDS is a nationally representative, weighted sample of ED visits that includes all visits to an annually varying 20% stratified sample of hospital-owned EDs nationwide. We excluded visits for psychiatric conditions (Healthcare Cost and Utilization Project Clinical Classifications Software codes 650–670).(11)
The exposure variables were quartile of neighborhood income and insurance type. Neighborhood income was defined by the quartile of median household income for ZIP code. Household incomes for each quartile varied by year with the following ranges: poorest quartile ≤$39,999–43,999, second quartile $40,000–44,000 to $50,999–55,999, third quartile $51,000–56,000 to $65,999–73,999, and wealthiest quartile ≥$66,000–74,000. Insurance type was categorized by primary payer as public, private, or uninsured.
The primary outcome was the proportion of visits made to EDs of low (<1,800 visits per year), medium (1,800–4,999 visits per year), medium-high (5,000–9,999 visits per year), and high (≥10,000 visits per year) pediatric volume.(9) A secondary outcome was the proportion of visits by ED type, defined as pediatric (≥70% of visits by patients less than 18 years of age) or general (<70% of visits by patients less than 18 years of age).(11)
We determined the unadjusted associations of neighborhood income and insurance type with the distribution of visits to EDs by pediatric volume and type with chi square tests. For the primary outcome of ED volume, we stratified the associations by the urban-rural status of patient residence, a known determinant of access to emergency care.(19) We also used a partial proportional odds model to assess the extent to which neighborhood income and insurance status influenced ED visits by pediatric volume after adjusting for potential patient-level confounders including urban-rural status, age, and presence of a complex chronic condition.(20) All results were weighted to account for the complex survey design of the NEDS. This study was deemed exempt by the Boston Children’s Hospital Institutional Review Board.
Results
From 2014 to 2017, there were 107.6 million ED visits by children after 2.7 million (2.4%) psychiatric visits were excluded. By neighborhood income, there were 39.2 million ED visits by children in the poorest quartile, 28.7 million by children in the second quartile, 22.3 million by children in the third quartile, and 16.0 million by children in the wealthiest quartile. Children with private insurance made 30.2 million ED visits, children with public insurance 70.6 million, and uninsured children 6.6 million.
Children living in the poorest, second, and third neighborhood income quartile had lower proportions of visits to high-pediatric-volume EDs compared to children living in the wealthiest neighborhood income quartile (57.1% poorest quartile, 51.5% second, 56.6% third, 63.5% wealthiest) and greater proportions of visits to low-pediatric-volume EDs (4.4% poorest quartile, 6.4% second, 4.6% third, and 2.3% wealthiest) (p < 0.01). However, within each urban-rural group except for smaller metropolitan, children in lower-income neighborhoods were more likely to visit EDs with higher pediatric volume (p = 0.57 for metropolitan with population 50,000–1 million, p < 0.01 for all other groups). Children who were publicly insured more commonly visited high-pediatric-volume EDs than privately insured and uninsured children (54.3% private, 57.3% public, 55.8% uninsured) and less commonly visited low-pediatric-volume EDs (5.8% private, 4.2% public, 4.7% uninsured) (p < 0.01). This pattern was true within each urban-rural group except for rural children, for whom there was no significant difference across insurance groups (p = 0.24 for rural, p < 0.01 for all other groups) (Figure 1).
Figure 1:
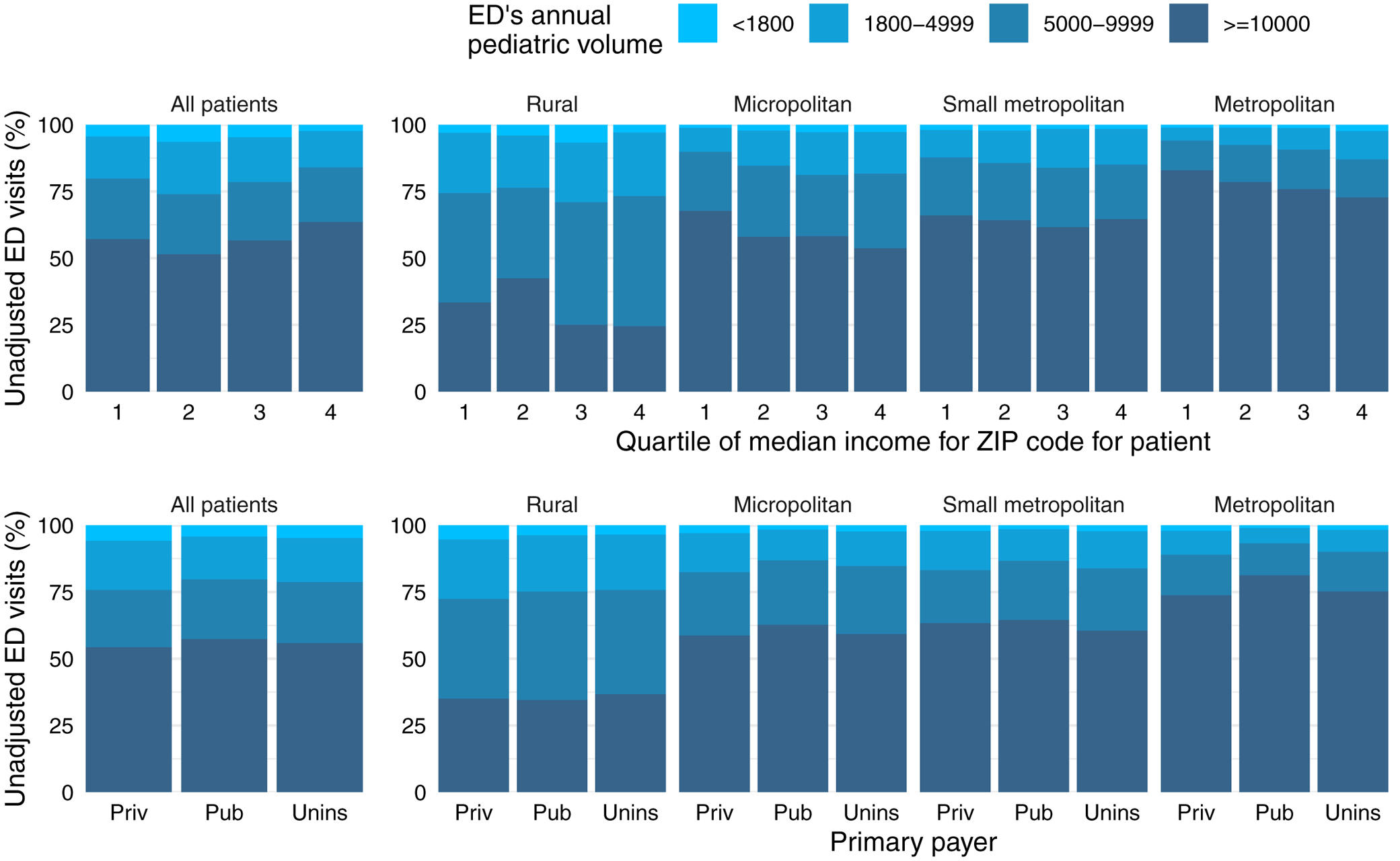
Unadjusted proportions of pediatric visits to EDs by annual pediatric volume overall and stratified by urban-rural status of residence a) by quartile of median household income of ZIP code of residence b) by insurance type
Adjustment for patient-level factors in the partial proportional odds model revealed that lower neighborhood income quartile was independently associated with receipt of emergency care in higher-pediatric-volume EDs (Figure 2). Publicly insured children were more likely than privately insured and uninsured children to receive care in higher-pediatric-volume EDs.
Figure 2:
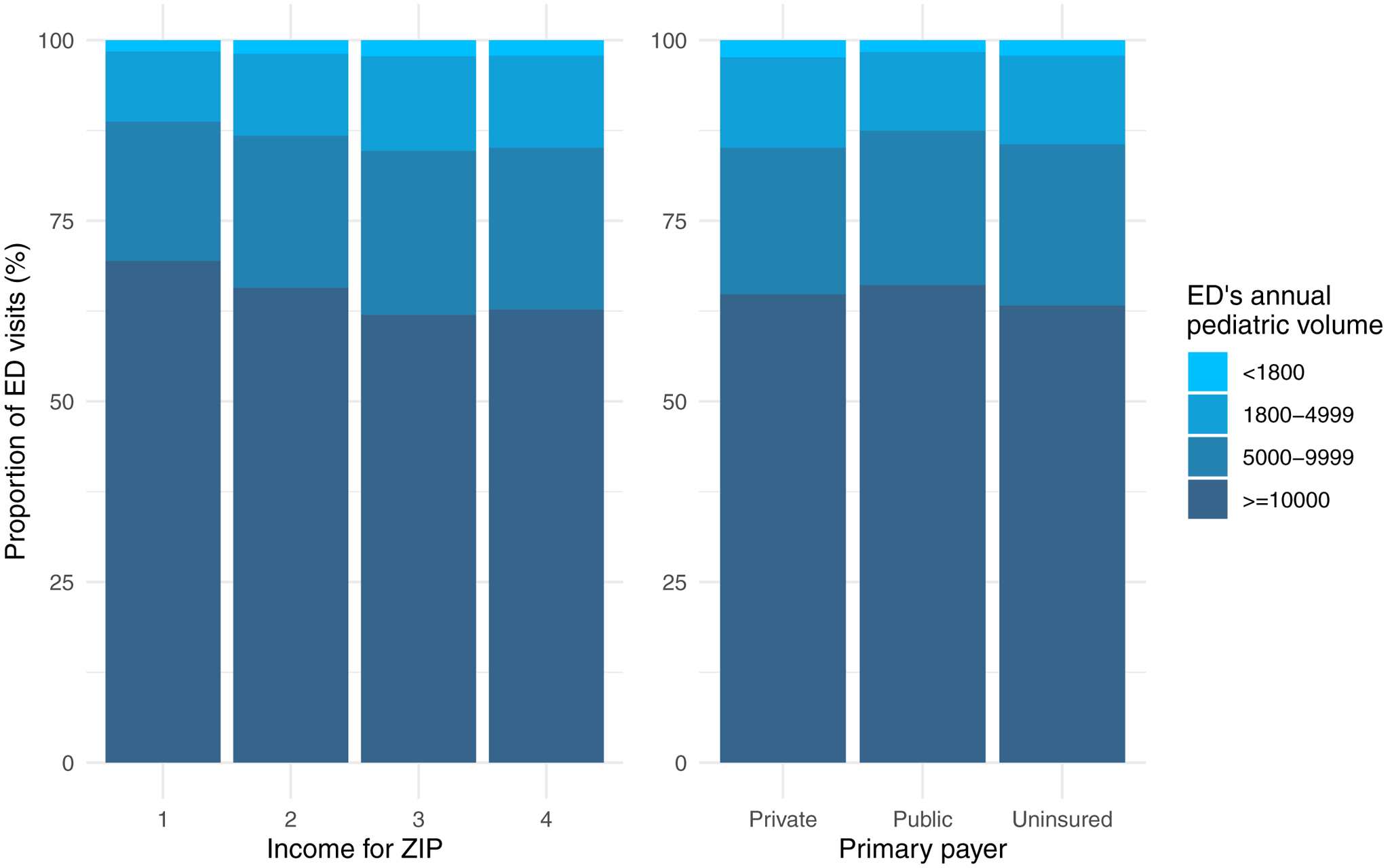
Adjusted proportions of pediatric visits to EDs by annual pediatric volume overall controlling for age, presence of a complex chronic condition, and urban-rural status of residence a) by quartile of median household income of ZIP code of residence b) by insurance type
No consistent association in unadjusted analyses with visits by ED type was observed across neighborhood income quartiles (12.1% poorest quartile, 8.1% second, 10.3% third, and 11.3% wealthiest to pediatric EDs, p = 0.03) or insurance types (9.7% private, 10.9% public, 9.2% uninsured to pediatric EDs, p = 0.29).
Discussion
Across the United States, children in lower-income neighborhoods tended to receive care in EDs with lower pediatric volume. Adjustment for patient-level factors including urban-rural residence status, however, revealed that lower neighborhood income was independently associated with receiving care in higher-pediatric-volume EDs. Publicly insured children were more likely to visit higher-pediatric-volume EDs than privately insured and uninsured children in both unadjusted and adjusted analyses.
A critical question for understanding socioeconomic disparities in healthcare quality is how they are driven by differences between hospitals where patients receive care versus differences in the quality of care between patients within the same hospitals. While between-hospital differences largely account for such disparities among adult patients,(21,22) this is less likely to be the case for children in the ED given how modest differences in care-seeking patterns are by neighborhood income and insurance status. The worse emergency outcomes experienced by children of lower SES may be influenced more by systematic variation and bias in care within institutions,(23) as evidenced by patient-level care disparities identified in studies exclusively examining pediatric EDs.(24,25) Disparities in outcomes may also reflect differences in patient-level characteristics including their severity of illness upon presentation, representing a need for measures that more specifically reflect the quality of healthcare delivery in the pediatric setting.(5,26,27)
Our findings do suggest there may be less access to EDs with more pediatric experience among children living in lower-income areas. This may reflect the greater proportion of lower-income households in rural areas, where EDs tend to have lower pediatric volume and less pediatric readiness.(28) Thus, urban-rural differences in emergency care access may contribute to income-based disparities nationally. Significant gaps exist in geographic accessibility of pediatric-ready EDs,(29) which may be widened further by increasing regionalization of pediatric emergency care. As pediatric care becomes more concentrated, pediatric volume may decline further in lower-volume hospitals that serve rural, disproportionately lower-income patient populations.(11,30) Thus, efforts to increase readiness broadly across EDs,(29) particularly those in rural areas, take on greater importance to protect equity of emergency care access for children across socioeconomic strata.
Despite using a large, nationally representative sample of ED visits, our study has limitations. The NEDS does not include data on patient race and ethnicity, which have been associated with differences in care-seeking patterns among adults(15) and disparities in health outcomes for children.(31) Thus, the influence of race and ethnicity on where children receive emergency care could not be assessed. Information on EDs was de-identified by the NEDS, which precluded an assessment of characteristics of individual EDs beyond those ascertainable from the NEDS. Although pediatric volume and type are well-established determinants of the quality of emergency care provided to children, examining SES-related access to EDs by pediatric readiness as a more direct indicator of quality represents a potential avenue for future research.
Differences in access to EDs with higher pediatric experience between urban and rural children translate into income-related access disparities at the national level, an important health equity-related consideration as pediatric care becomes increasingly regionalized. Further research into reasons underlying disparities in pediatric emergency outcomes should explore ED characteristics beyond pediatric volume as well as individual-level variation in care provided to children.
Funding Sources:
No funding was received for this research.
Abbreviations:
- SES
socioeconomic status
- ED
emergency department
- NEDS
Nationwide Emergency Department Sample
Footnotes
Conflicts of Interest: The authors declare no conflicts of interest. Lawrence Chang wrote the first draft of the manuscript. No honorarium, grant, or other form of payment was given to anyone to produce the manuscript.
Data Sharing: All data used for this research are publicly available.
References:
- 1.Mannix R, Chiang V, Stack AM. Insurance status and the care of children in the emergency department. Journal of Pediatrics. 2012;161(3):536–41. [DOI] [PubMed] [Google Scholar]
- 2.Hambrook JT, Kimball TR, Khoury P, Cnota J. Disparities Exist in the Emergency Department Evaluation of Pediatric Chest Pain. Congenital Heart Disease. 2010. May;5(3):285–91. [DOI] [PubMed] [Google Scholar]
- 3.Smink DS, Fishman SJ, Kleinman K, Finkelstein JA. Effects of race, insurance status, and hospital volume on perforated appendicitis in children. Pediatrics. 2005. April;115(4):920–5. [DOI] [PubMed] [Google Scholar]
- 4.Wang L, Haberland C, Thurm C, Bhattacharya J, Park KT, Abe T. Health outcomes in US children with abdominal pain at major emergency departments associated with race and socioeconomic status. PLoS ONE. 2015. August 12;10(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rees CA, Monuteaux MC, Raphael JL, Michelson KA. Disparities in Pediatric Mortality by Neighborhood Income in United States Emergency Departments. Journal of Pediatrics. 2020;219(3):209–215. [DOI] [PubMed] [Google Scholar]
- 6.Bourgeois FT, Shannon MW. Emergency Care for Children in Pediatric and General Emergency Departments. Pediatric Emergency Care. 2007. February 1;23(2):94–102. [DOI] [PubMed] [Google Scholar]
- 7.Chamberlain JM, Krug S, Shaw KN. Emergency care for children in the United States. Health Affairs. 2013;32(12):2109–15. [DOI] [PubMed] [Google Scholar]
- 8.Jain PN, Choi J, Katyal C. Pediatric Care in the Nonpediatric Emergency Department: Provider Perspectives. Hospital Pediatrics. 2019. March;9(3):216–9. [DOI] [PubMed] [Google Scholar]
- 9.Gausche-Hill M, Ely M, Schmuhl P, Telford R, Remick KE, Edgerton EA, et al. A national assessment of pediatric readiness of emergency departments. JAMA Pediatrics. 2015. June 1;169(6):527–34. [DOI] [PubMed] [Google Scholar]
- 10.Walls TA, Chamberlain JM, Klein BL. Factors Associated With Emergency Department Discharge After Pediatric Interhospital Transport A Role for Outreach Education? Pediatric Emergency Care. 2015;31(1). [DOI] [PubMed] [Google Scholar]
- 11.Michelson KA, Hudgins JD, Lyons TW, Monuteaux MC, Bachur RG, Finkelstein JA. Trends in Capability of Hospitals to Provide Definitive Acute Care for Children: 2008 to 2016. Pediatrics. 2020. January 1;145(1). [DOI] [PubMed] [Google Scholar]
- 12.Cushing AM, Bucholz E, Michelson KA. Trends in regionalization of emergency care for common pediatric conditions. Pediatrics. 2020. April 1;145(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smink DS, Finkelstein JA, Kleinman K, Fishman SJ. The Effect of Hospital Volume of Pediatric Appendectomies on the Misdiagnosis of Appendicitis in Children. Vol. 113, Pediatrics. 2004. January 1;113(1):18–23. [DOI] [PubMed] [Google Scholar]
- 14.Ames SG, Davis BS, Marin JR, Fink EL, Olson LM, Gausche-Hill M, et al. Emergency Department Pediatric Readiness and Mortality in Critically Ill Children. Pediatrics. 2019. September 1;144(3):e20190568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gray BH, Schlesinger M, Mitchell S, Horowitz SE. Racial and Ethnic Disparities in the Use of High-Volume Hospitals. Inquiry: The Journal of Health Care Organization, Provision, and Financing. 2009. August;46(3):322–38. [DOI] [PubMed] [Google Scholar]
- 16.Kronebusch K, Gray BH, Schlesinger M. Explaining racial/ethnic disparities in use of high-volume hospitals: Decision-making complexity and local hospital environments. Inquiry: The Journal of Health Care Organization, Provision, and Financing. 2014;51(1):1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jha AK, John Orav E, Epstein AM. Low-quality, high-cost hospitals, mainly in South, care for sharply higher shares of elderly black, Hispanic, and Medicaid patients. Health Affairs. 2011. October;30(10):1904–11. [DOI] [PubMed] [Google Scholar]
- 18.Healthcare CostUtilization Project (HCUP). Introduction to the HCUP Nationwide Emergency Department Sample (NEDS). 2019. Available from: www.hcup-us.ahrq.gov.
- 19.Carr BG, Branas CC, Metlay JP, Sullivan AF, Camargo CA. Access to Emergency Care in the United States. Annals of Emergency Medicine. 2009. August;54(2):261–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: Updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatrics. 2014. August 8;14(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hasnain-Wynia R, Baker DW, Nerenz D, Feinglass J, Beal AC, Landrum MB, et al. Disparities in Health Care Are Driven by Where Minority Patients Seek Care Examination of the Hospital Quality Alliance Measures. Archives of Internal Medicine. 2007. June 25;167(12):1233–9. [DOI] [PubMed] [Google Scholar]
- 22.Hasnain-Wynia R, Kang R, Mary MA, Landrum B, Vogeli C, Baker DW, et al. Racial and Ethnic Disparities within and between Hospitals for Inpatient Quality of Care: An Examination of Patient-level Hospital Quality Alliance Measures. Journal of Health Care for the Poor and Underserved. 2010;21(2):629–48. [DOI] [PubMed] [Google Scholar]
- 23.Spencer CS, Gaskin DJ, Roberts ET. The quality of care delivered to patients within the same hospital varies by insurance type. Health Affairs. 2013;32(10):1731–9. [DOI] [PubMed] [Google Scholar]
- 24.Goyal MK, Kuppermann N, Cleary SD, Teach SJ, Chamberlain JM. Racial disparities in pain management of children with appendicitis in emergency departments. JAMA Pediatrics. 2015. November 1;169(11):996–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goyal MK, Johnson TJ, Chamberlain JM, Cook L, Webb M, Drendel AL, et al. Racial and Ethnic Differences in Emergency Department Pain Management of Children With Fractures. Pediatrics. 2020. May 1;145(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lopez AM, Tilford JM, Anand KJ, Jo CH, Green JW, Aitken ME, et al. Variation in pediatric intensive care therapies and outcomes by race, gender, and insurance status. Pediatric Critical Care Medicine. 2006. January 1;7(1):2–6. [DOI] [PubMed] [Google Scholar]
- 27.Dynan L, Goudie A, Smith RB, Fairbrother G, Simpson LA. Differences in quality of care among non-safety-net, safety-net, and children’s hospitals. Pediatrics. 2013. February;131(2):304–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pilkey D, Edwards C, Richards R, Olson LM, Ely M, Edgerton EA. Pediatric Readiness in Critical Access Hospital Emergency Departments. Journal of Rural Health. 2019. September 1;35(4):480–9. [DOI] [PubMed] [Google Scholar]
- 29.Ray KN, Olson LM, Edgerton EA, Ely M, Gausche-Hill M, Schmuhl P, et al. Access to High Pediatric-Readiness Emergency Care in the United States. Journal of Pediatrics. 2018. March 1;194:225–232.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leyenaar JAK, Kozhimannil KB. The costs and benefits of regionalized care for children. Vol. 145, Pediatrics. 2020. April 1;145(4). [DOI] [PubMed] [Google Scholar]
- 31.Cunningham RM, Walton MA, Carter PM. The Major Causes of Death in Children and Adolescents in the United States. New England Journal of Medicine. 2018. December 20;379(25):2468–75. [DOI] [PMC free article] [PubMed] [Google Scholar]


