Abstract
Introduction
Cervical cancer is the most common cancer in India. Screening for cervical cancer helps in marked reduction of invasive cervical cancers. The low sensitivity of Papanicolaou cytology (Pap smear) and high-risk human papillomavirus (HR-HPV) in excluding high-grade intraepithelial lesion (ASC-H) leads to unnecessary referrals to colposcopy-guided biopsy. The combined cervical cytology screening and HR-HPV have its own limitations and still need further standardization. Using additional biomarkers like staining with p16 and Ki-67 might help in triaging abnormal pap smear.
Materials and Methods
A prospective, cross-sectional study was performed over a period of 16 months in the Department of Obstetrics and Gynaecology, in collaboration with Department of Pathology. Study was conducted to know the efficacy of immunostaining with p16/Ki-67 in predicting the presence of significant lesion in cases of mild cytological atypia. PAP smears (conventional and LBC) along with P16, Ki-67 and available biopsies were correlated.
Results
Liquid-based cytology (LBC) was done in 2134 cases, out of which 46 cases showed abnormal cytological findings such as [22 atypical squamous cells of undetermined significance (ASCUS), 3 low-grade squamous intraepithelial lesion (LSIL), 8 atypical squamous cells cannot exclude high-grade lesion (ASC-H), 6 high-grade squamous intraepithelial lesion (HSIL), 5 squamous cell carcinoma (SCC), 2 adenocarcinoma, 1 atypical glandular cells of undetermined significance (AGUS)]. Immunostaining with p16 and Ki-67 was performed on 38 cases of abnormal cytological smears. Out of 38 abnormal cytology cases, 28 cases had shown co-staining for both p16 and Ki-67, suggestive of true HPV infection of the cells. Of the 38 cases, 07/14 ASCUS, 06/06 HSIL, 07/08 ASC-H, 05/05 squamous cell carcinoma and 02/02 adenocarcinoma also showed dual positivity for p16 and Ki-67. One case of AGUS was diagnosed, but the smear was unsatisfactory for immunocytochemical evaluation and excluded from the study. Three cases of LSIL were also diagnosed on cytological evaluation, and 1 of them however showed positivity for p16 and Ki-67 on immunocytochemistry (ICC). In the ASC-US group, the sensitivity and specificity of the immunostaining in diagnosing CIN2 + lesions were 87.51%, and in LSIL group, the sensitivity and specificity of the immunostaining in diagnosing CIN2 + lesions were 100%. p16/Ki-67 positivity also increased with cytological severity which in turn corresponded with histological findings: it reached from 50% in ASC-US to 100% in both HSIL and SCC categories.
Conclusion
This immunostaining with p16 and Ki67 can be a useful method in the triaging of the ASC-US and the LSIL group as considering the high sensitivity and specificity values.
Keywords: p16, Ki67, ASC-US, ICC, Liquid-based cytology
Introduction
Cervical cancer is the second most common cancer after breast and colorectal cancer worldwide. Despite having a national cancer program since 1975, it still leads the cancer-related cause of death in India and many other developing countries and is one of the major public health problems. Screening program for cervical cancer helps in detection of precancerous lesions of cervix, ultimately leading to marked reduction in the incidence and mortality [1]. For cervical cancer development, high-risk human papillomavirus infection is necessary. Most HPV infections are asymptomatic, transient and self-limiting with a very low incidence of viral infection converting into cancer. It has become very crucial to develop new techniques to diagnose these cancer transforming HPV infections [2]. In ninety percent of cases, HPV disappears in 2 years. Less than 10% HPV infections progress to high-grade lesions or cancer. As no significant precursor lesion is found, many of the women undergo unnecessary additional procedures like a repeat Papanicolaou smear, colposcopy or cervical biopsies [3]. The Papanicolaou (Pap) smear was introduced in 1941. Screening with Pap smears and high-risk human papillomavirus (hr-HPV) testing has become the standard of care. The overall sensitivity in the detection of premalignant lesions like high-grade squamous intraepithelial lesion is 70–80%, and specificity is between 60 and 95% cases. About 5–20% of results are false negative, and in almost 30% of newly diagnosed cases of carcinoma cervix, patient usually has at least one false-negative Papanicolaou test. Neither of the screening tests would tell which precursor lesion will progress to invasive cancer [4]. HPV oncogenes affect the expressions of host gene that is involved in cell cycle regulation and proliferation. p16 and Ki67 biomarkers are involved in cell proliferation. So these additional markers of dysplasia will potentially increase the positive predictive value for the diagnoses. p16 is a cyclin-dependent kinase inhibitor, a cell cycle regulator protein that induces cell cycle arrest under normal physiological conditions. Due to functional inactivation of the retinoblastoma gene by HPV E7, there is abnormal overexpression of p16 which makes it a potential immunohistochemical screening marker for dysplasia arising from an HPV infection [5]. Ki-67 is a proliferation marker expressed in all phases of the cell cycle except G0 that is resting cells.
It can provide an index of the cell growth fraction. In this study, we have studied the role of Pap smear/liquid-based cytology (LBC) and immunostaining for p16 and Ki-67 in allowing identification of abnormal cells in cytology smears, and we also investigated whether p16/Ki-67 immunostaining can be used to triage abnormal Pap smears.
Material and Methods
This was a prospective, cross-sectional study performed in the Department of Obstetrics and Gynaecology, in collaboration with Department of Pathology over a period of 16 months (July 2017–Nov 2018). Informed consent was obtained, and only the cases above the age of 21 were included in the study presenting with symptoms like postcoital bleeding, contact bleeding, excitation pain, excessive or offensive smelling vaginal discharge, dyspareunia and pelvic pain syndrome were included in the study. Patients younger than 21 years were excluded from the study. Also if the samples were obtained in women with hysterectomies, or if there was insufficient residual fluid to prepare an additional slide, diagnosed cervical cancer, pregnancy, prior therapy for cervical neoplasia and inability to give informed consent such cases were not included in the study. Institutional review board approval for this study was obtained bearing no: AIIMS/RES(03)/2016/126.
In total, 2134 patients met the inclusion criteria and gave consent to participate in the study. Liquid-based cytology was done in these patients. Out of 2134 patients, 46 cases showed abnormal cytological findings. In total, 38 abnormal cytology cases were subjected to immunocytochemistry and colposcopy-guided biopsy.
Sample Collection and Processing
For reporting the cervical cytology, liquid-based cytology (LBC) was used. LBC samples were collected using a Wallach broom device and transferred to BD Sure Path Preservative Solution. All samples were collected by a trained health provider. The samples were then transported to the laboratory and processed the following day. Final diagnosis was made according to the guidelines made by the Bethesda System of Reporting Cervical Cytology (2014) by pathologist after proper evaluation according to the guidelines made by the Bethesda System of Reporting Cervical Cytology (2014). LBC sample of abnormal smears was preserved.
Immunocytochemistry for p16 and ki-67
Two unstained slides were prepared from the preserved LBC sample of the cases with abnormal cytology. Immunocytochemical (ICC) analysis was performed on 38 cases. Antigen retrieval was performed by heat-mediated method following which they were subjected to immunostaining. The antibodies used in this study were anti-CDKN2A/p16INK4a antibody at a dilution of 1:100 (Abcam) and ready-to-use prediluted Ki-67 monoclonal antibody from Thermo scientific. Both were amplified by labelled streptavidin–biotin-peroxidase system using Leica Bond-Max. The colour of immunostaining was developed by chromogenic substrate diaminobenzidine and hydrogen peroxide. After light counterstaining in Harry’s haematoxylin, the slides were mounted and analysed using light microscopy.
Evaluation of ICC staining was performed as positive and negative reaction. For p16 it was evaluated as positive nuclear or cytoplasmic staining. For Ki-67, only nuclear positivity was taken into consideration.
Colposcopy-guided biopsy was performed in the patient with abnormal cytological smear. Any histopathological abnormality ASCUS, LSIL, HSIL were considered as positive histopathological correlation.
Statistical Analysis
All statistical analyses were performed using SPSS version Chi-square test for independence for evaluating association of p16/Ki-67 staining with cervical epithelial abnormality. All the categorical data were compared by Fisher’s exact test. A P value < 0.05 was taken as statistically significant.
Results
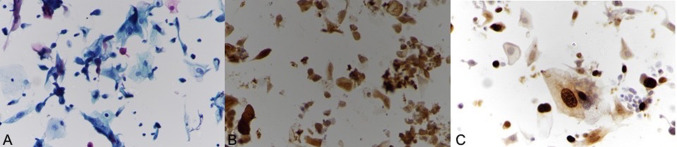
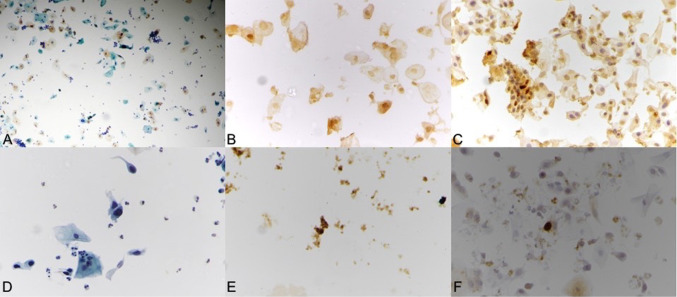
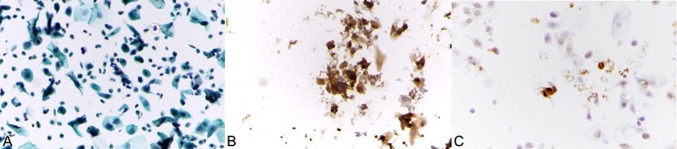
The study included 2134 women who met the inclusion criteria. The patients age ranged from 31 to 70 years, with a mean age of 41 years. Out of the 2134 women, 170 smears were unsatisfactory for evaluation. Of the rest, 1856 (86.95%) patients were diagnosed as negative for intraepithelial lesion and malignancy. In abnormal smear, 22 (47.8%) had ASC-US, 8 (17%) had ASC-H, 3 cases (6.5%) had LSIL, 6 (13%) had HSIL, 5 (10%) had invasive squamous cell carcinoma, 2 (4.34%) cases were of adenocarcinoma, and 1 (2.17%) case had atypical glandular cells of undetermined significance [AGUS] (Table 1). Out of the 46 cases of epithelial abnormality, immunostaining followed by colposcopy-guided cervical biopsy was performed on 38 cases. On histological evaluation of each of the diagnostic categories, 14 ASCUS cases were biopsied showing negative results in 5 (35.71%), CIN1 was seen in 4 cases (28.57%), CIN2/3 in 3 cases (21.42%) and chronic cervicitis in 2 cases (14.28%); 0.3 LSIL cases were biopsied showing negative results in 1 case (33.33%), chronic cervicitis in 1 case (33.33%), CIN1 in none (0%), and CIN2/3 in 1 case (33.33%); 0.8 ASC-H cases were biopsied showing negative results in 1 case ( 12.5%), chronic cervicitis in 1 case (12.58%), CIN1 in 1 case (12.58%), CIN2 + in 4 cases (50%) and invasive carcinoma in 1(12.5%) case. Six HSIL cases were biopsied showing negative results in 1 (16.66%), CIN1 in 0 (0%), CIN2/3 in 4 (66.66%) and invasive carcinoma in 1 patient (16.16%). Squamous cell carcinoma was detected in 5 (100%) and adenocarcinoma in 2 (100%) cases (Table 2). Out of 38, abnormal cytology cases, 28 cases displayed co-staining for both p16 and Ki-67, suggestive of true HPV infection of the cells. Of the 38 positive cases, 07/14 ASCUS (Fig. 1), 06/06 HSIL (Fig. 2), 07/08 ASC-H, 05/05 squamous cell carcinoma (Fig. 3), 02/02 adenocarcinoma showed positivity for both p16 and Ki-67. One AGUS was diagnosed, but the smear was unsatisfactory for immunocytochemical evaluation and was excluded from the study (Table 3).
Table 1.
Cytology
| NILM | 1856 |
| ASCUS | 22 |
| LSIL | 3 |
| HSIL | 6 |
| ASC-H | 8 |
| SCC | 5 |
| ADENOCARCINOMA | 2 |
| AGUS | 1 |
| UNSATISFACTORY | 170 |
| INFLAMMATION | 54 |
| ATROPHIC | 7 |
| Total | 2134 |
Table 2.
Cytology and histopathology correlation
| Cytology | Normal | Chronic cervicitis | LSIL (CIN1) | HSIL (CIN2 +) | Malignancy | Total |
|---|---|---|---|---|---|---|
| ASCUS | 5 | 2 | 4 | 3 | 0 | 14 |
| ASC-H | 1 | 1 | 1 | 4 | 1 | 8 |
| LSIL | 1 | 1 | 0 | 1 | 0 | 3 |
| HSIL | 1 | 0 | 0 | 4 | 1 | 6 |
| MALIGNANCY | 0 | 0 | 0 | 0 | 7 | 7 |
| Total | 8 | 4 | 6 | 12 | 9 | 38 |
Fig. 1.
a Low power view of liquid-based cytology of ASCUS displaying relatively mature squamous cells with increased nuclear size along with few cells showing koilocytosis (Papanicolaou × 100). b Positive immunostaining for p16 (× 100). c Positive immunostaining
Fig. 2.
a Liquid-based cytology smear shows immature squamous cells with increased nuclear size representing ASC-H ((Papanicolaou × 100). b Positive immunostaining for p16 (× 400). c Positive immunostaining for Ki-67 (× 400). d Liquid-based cytology smear of HSIL showing isolated small cells with high nuclear to cytoplasmic ratio (Papanicolaou × 100). e Positive immunostaining for p16 (× 100)
Fig. 3.
a Squamous cell carcinoma composed of round to oval nuclei with considerable variation in size and membrane shape with fibrillar cytoplasmic strands (Papanicolaou × 100). b Positive immunostaining for p16 (× 400). c Positive immunostaining for Ki-67 (× 400)
Table 3.
Cytology/staining/histopathological correlation
| Cytology finding | p16/Ki‐67 co-positivity in cytology | Histopathological correlation |
|---|---|---|
| ASCUS (14 cases) | 7 (50%) | 6 (42%) |
| ASC-H (8 cases) | 7 (87.5%) | 6 (75%) |
| LSIL (3 cases) | 1 (33.33%) | 1 (33.33%) |
| HSIL (6 cases) | 6 (100%) | 5 (83%) |
| SCC (5 cases) | 5 (100%) | 5 (100%) |
| Adenocarcinoma (2 cases) | 2 (100%) | 2 (100%) |
| Total-38 | 28 | 25 |
Three cases of LSIL were also diagnosed on cytological evaluation, and 1 of them showed positivity for p16 and Ki-67 on immunocytochemistry (ICC). For Ki-67 (× 400)p16/Ki-67 positivity also increased with cytological severity which in turn corresponded with histological findings: it reached from 50% in ASC-US to 100% in both HSIL and SCC categories. In the ASC-US category, 7 cases (50%) showed positive immunostaining, 4 were found to be CIN1, and 3 were found to be CIN2/CIN3 on histopathology, whereas 7 (50%) cases showed negative staining despite having CIN1 in 1 case. In the LSIL cases 1 (33.33%) case showed positive immunostaining, which confirmed to have a diagnosis of CIN2/CIN3. Two cases which were negative for immunostaining were found to have no dysplastic changes in the histopathology.
In diagnosed cytological cases of ASC-US and LSIL, comparative values of sensitivity, specificity, PPV, NPV and two-sided P value of the immunostaining with co-positivity for p16/Ki67 in detecting significant histological lesion (CIN2/CIN3) were calculated. For ASCUS, the sensitivity and specificity of the dual immunostaining in detecting CIN2/CIN3 were found to be 85.71%, whereas for LSIL the values were 100%. The positive and negative predicative value for ASCUS and LSIL was 85.71% and 100%, respectively.
Discussion
Screening for cervical cancer has led to marked reduction in the incidence of invasive cervical cancers. Despite these screening programs and HPV testing, 30% of newly diagnosed cancers are found in the women who followed the recommended guidelines for screening [2]. HPV infection is very common in young girls, but the infection is usually transient, and in maximum cases, spontaneous resolution occurs in a few years. The integration of the viral genome with the host genome is the most significant factor in the development of invasive carcinoma [6].
In some benign cases and low-grade squamous lesions high viral loads were found which could be due to increased episomal levels not related to the oncogenic potential of HPV. This factor supported the utility of cancer cell biomarker p16 instead of viral copy number as a better adjunct tool in determining which patient would show disease progression. To refine the risk in a patient with abnormal cytological smear currently available is hr-HPV testing of ASCUS smears. But in LSIL this was not cost-effective as 83.4% of the LSIL smears were positive of hr-HPV. Only a small number of both ASCUS/hr-HPV-positive and LSIL/hr-HPV-positive cases showed CIN2,3 on histopathology, suggesting that a large number of the population undergo unnecessary colposcopy referral. Colposcopy referral is further increased by the patients diagnosed as ASC-H or HSIL on cervical PAP smear screening [7]. The goal of our study was to demonstrate the role of p16 /Ki67 stains in identifying histopathological significant lesions in the patients with abnormal smear findings.
As our study had a small sample population for immunocytochemical testing with p16 and Ki67 in cases of ASCUS, LSIL and ASC-H, larger prospective studies are required to validate these findings. In our study, the prevalence of CIN2 or worse lesions in ASC-US patients was 21.42%. Other studies showed the prevalence to be 5–22% [8]. The prevalence of CIN2-positive lesions in the patients with cytological diagnosis of LSIL was found to be high and reached 33.3%. Other studies have found it to be around 9–30% [9].
In our study, 73.68% of all women with epithelial abnormality showed co-positivity with p16/Ki-67 immunostaining suggestive of true infection. For ASC-US, the sensitivity and specificity of p16/Ki-67 immunostaining in detecting CIN2/CIN3 were found to be 85.71%, whereas for LSIL the values were 100%. The positive and negative predictive values for ASCUS and LSIL were 85.71% and 100%, respectively. Other studies showed the sensitivity between 64 and 98% and the specificity of 43% and 81% in detecting high-grade lesions in ASCUS [10]. The limitation of our study was a small population of patients with abnormal smears, lack of availability of concurrent HPV testing and the use of residual fluid for immunostaining.
Screening of cervical cancer helps in the detection of precancerous lesions of the cervix and ultimately leads to a marked reduction in incidence and mortality due to invasive cervical cancers. Cytological examination by PAP smears has been established as a standard method for cancer screening. The diagnostic protocols still need to be standardized, especially for the management of diagnoses such as ASC-US and LSIL where the risk to progress to malignancy is high. The simultaneous expression of a proliferation-associated protein (Ki-67) and a protein associated with tumour suppression (p16) should grant a high specificity in the detection of dysplastic cells in which the neoplastic process has been initiated [11].
Conclusion
P16 and Ki67, being the INK4A tumour markers, have a lot of significance in ascertaining the progressive lesions. This also clears the ambiguity grey zone of low-grade and high-grade lesions. Mainly they indicate progressive HPV infections with manifestation of E6 and E7. As E6 is responsible for degradation of P53 tumour-suppressive gene, E7 causes the RB protein to get phosphorylated, thus releasing the E2F transcription factor leading to cell divisions and immortalizations. As most of the studies are suggestive of high sensitivity with p16/Ki-67 immunostaining for detecting high-grade precursor lesions in the patients with abnormal cytological smears, it can be used as an adjunct in triaging of the ASCUS and the LSIL group. With the use of p16/Ki-67 immunostaining, the number of referrals to colposcopy centres can be reduced to half. In low-resource countries, the cost of HPV testing, p16/Ki-67 immunostaining and the referral to colposcopy centres protocols need to be further explored to determine the most favourable strategy.
Dr. Meenakshi Gothwal
is currently working as an Associate Professor in the Department of Obstetrics and Gynaecology at All India Institute of Medical Sciences, Jodhpur. She is actively involved in the research activities of the department with her areas of interest being high-risk pregnancy and gynaecological oncology. She is also working on various intramural funded projects as a primary investigator in the project entitled “Cancer-cell biomarkers p16 and Ki67 in abnormal cervical cytological smear” as well as co-investigator in various projects focussing on contraception, sexually transmitted diseases, prediction of preterm labour using utero-cervical angle, prevention of surgical site infections and correlation of intrapartum electronic foetal surveillance with adverse neonatal outcomes, etc. She has a keen interest in undergraduate as well as postgraduate teaching and is also guiding undergraduate students for short-term student projects funded by ICMR and attends various workshops for the same. She has also presented various papers in both national and international conferences.
Funding
Yes (AIIMS, Jodhpur).
Compliance with Ethical Standards
Conflict of interest
None declared.
Informed Consent
Informed consent was taken.
Footnotes
Meenakshi Gothwal: M.B.BS, MD, Associate Professor in the Department of Obstetrics & Gynecology, AIIMS, Jodhpur, Rajasthan, 342005, India. Aasma Nalwa: M.B.B.S, M.D, Associate Professor in the Department of Pathology, AIIMS Jodhpur, Rajasthan, 342005, India. Pratibha Singh: M.B.B.S, MS, Professor & HOD in the Department of Obstetrics & Gynecology, AIIMS, Jodhpur, Rajasthan, 342005, India. Garima Yadav: M.B.B.S, MS, Associate Professor in the Department of Obstetrics & Gynecology, AIIMS, Jodhpur, Rajasthan, 342005, India. Meenal Bhati: M.B.B.S, Postgraduate in the Department of Obstetrics & Gynecology, AIIMS, Jodhpur, Rajasthan, 342005, India. Nitesh Samriya: M.B.BS, Postgraduate in the Department of Obstetrics & Gynecology, S.N.M.C Jodhpur, Rajasthan, India.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Byun SW, Lee A, Kim S, et al. Immunostaining of p16ink4a/Ki-67 and L1 capsid protein on liquid-based cytology specimens obtained from ASC-H and LSIL-H cases. Int J Med Sci. 2013;10(12):1602. doi: 10.7150/ijms.6526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Toll AD, Kelly D, Maleki Z. Utility of P16 expression and Ki-67 proliferation index in ASCUS and ASC-H pap tests. Diagn Cytopathol. 2014;42(7):576–581. doi: 10.1002/dc.23076. [DOI] [PubMed] [Google Scholar]
- 3.Killeen JL, Dye T, Grace C, et al. Improved abnormal Pap smear triage using cervical cancer biomarkers. J Lower Genit Tract Dis. 2014;18(1):1–7. doi: 10.1097/LGT.0b013e31828aeb39. [DOI] [PubMed] [Google Scholar]
- 4.Das D, Sengupta M, Basu K, et al. Role of p16/Ki-67 Dual immunostaining in detection of cervical cancer precursors. J Cytol. 2018;35(3):153. doi: 10.4103/JOC.JOC_4_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sun M, Shen Y, Ren ML, Dong YM, et al. Meta-analysis on the performance of p16/Ki-67 dual immunostaining in detecting high-grade cervical intraepithelial neoplasm. J Cancer Res Ther. 2018;14(10):587. doi: 10.4103/0973-1482.183216. [DOI] [PubMed] [Google Scholar]
- 6.Doorbar J. Papillomavirus life cycle organization and biomarker selection. Dis Markers. 2007;23(4):297–313. doi: 10.1155/2007/613150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones BA, Davey DD. Quality management in gynecologic cytology using interlaboratory comparison. Arch Pathol Lab Med. 2000;124:672Y81. doi: 10.5858/2000-124-0672-QMIGCU. [DOI] [PubMed] [Google Scholar]
- 8.Edgerton N, Cohen C, Siddiqui MT. Evaluation of CINtec PLUS® testing as an adjunctive test in ASC-US diagnosed SurePath® preparations. Diagn Cytopathol. 2013;41:35–40. doi: 10.1002/dc.21757. [DOI] [PubMed] [Google Scholar]
- 9.Possati-Resende JC, Fregnani JHTG, Kerr LM, et al. The accuracy of p16/Ki-67 and HPV test in the detection of CIN2/3 in women diagnosed with ASC-US or LSIL. PLoS ONE. 2015;10:e0134445. doi: 10.1371/journal.pone.0134445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Petry KU, Schmidt D, Scherbring S, et al. Triaging Pap cytology negative, HPV positive cervical cancer screening results with p16/Ki-67 Dual-stained cytology. Gynecol Oncol. 2011;121:505–509. doi: 10.1016/j.ygyno.2011.02.033. [DOI] [PubMed] [Google Scholar]
- 11.Schmidt D, Bergeron C, Denton KJ, et al. p16/ki-67 dual-stain cytology in the triage of ASCUS and LSIL Papanicolaou cytology: Results from the European equivocal or mildly abnormal Papanicolaou cytology study. Cancer Cytopathol. 2011;119:158–166. doi: 10.1002/cncy.20140. [DOI] [PubMed] [Google Scholar]