Abstract
Introduction/Objectives:
Uncontrolled diabetes can lead to major health complications, and significantly contributes to diabetes-related morbidity, mortality, and healthcare costs. Few studies have examined the relationship between unmet social needs and diabetes control among predominantly Black and Hispanic patient populations.
Methods:
In a large urban hospital system in the Bronx, NY, 5846 unique patients with diabetes seen at a primary care visit between April 2018 and December 2019 completed a social needs screener. Measures included diabetes control (categorized as Hemoglobin (Hb) A1c <9.0 as controlled and Hb A1C ≥9.0 as uncontrolled), social needs (10-item screen), and demographic covariates, including age, sex, race/ethnicity, insurance status, percentage of block-group poverty, patient’s preferred language, and the Elixhauser Comorbidity Index.
Results:
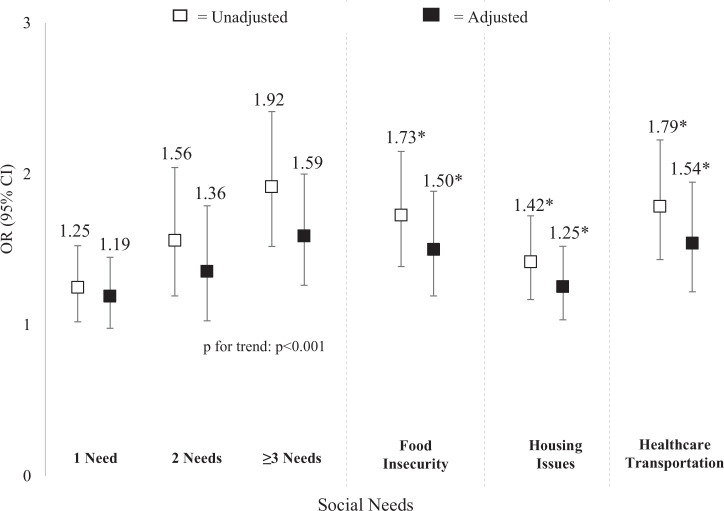
Twenty-two percent (22%) of the patient sample had at least 1 unmet social need, and the most prevalent unmet social needs were housing issues (including housing quality and insecurity), food insecurity, and lack of healthcare transportation. Logistic regression analysis showed a significant relationship between social needs and uncontrolled diabetes, with more social needs indicating a greater likelihood of uncontrolled diabetes (Adjusted Odds Ratio (AOR) for ≥3 needs: 1.59, 95% CI: 1.26, 2.00). Of the patients with most frequently occurring unmet social needs, lack of healthcare transportation (AOR: 1.54, 95% CI: 1.22, 1.95) and food insecurity (AOR: 1.50, 95% CI: 1.19, 1.89) had the greatest likelihood of having uncontrolled diabetes, after adjusting for covariates.
Conclusion:
Unmet social needs appear to be linked to a greater likelihood of uncontrolled diabetes. Implications for healthcare systems to screen and address social needs for patients with diabetes are discussed.
Keywords: disease management, underserved communities, primary care, community health, health outcomes
Introduction
In 2017, the total cost of diabetes, which include medical expenditures and lost productivity, were estimated to be $327 billion.1 Diabetes is the leading cause of kidney failure, lower-limb amputation, and adult-onset blindness.2 There are significant racial disparities in both diabetes risk and diabetes control,3 with epidemiologic studies observing Hemoglobin (Hb) A1C increasing over time for non-Hispanic Blacks and Mexican Americans, but decreasing over time for non-Hispanic Whites.4 Not only is diabetes more prevalent in African-American and Latino populations, risk factors, including obesity, physical inactivity, and unhealthy diet, are also more common.5 Racial disparities in adverse health outcomes may exist due to structural and systemic inequalities that result in unmet social needs like housing, transportation, and food insecurity.6 The awareness of social needs among patients is considered a necessary step in advancing health equity in primary care.7
Diabetes accounts for 11% of ambulatory care visits in the United States.8 The range of topics addressed in an office visit among adults with diabetes are diverse and include health-related issues as well as social environment conditions and social needs.9 Research suggests that health behaviors and adequate access to health care required to ensure good control of diabetes can be undermined by unmet social needs.10,11 Individuals with severe food insecurity are at greater risk for both developing diabetes and having uncontrolled diabetes.12-14 A recent study in a rural population of mostly white patients demonstrated several social needs, including difficulties paying bills, rationing medication due to cost, race, food insecurity, and loneliness were associated with poor glycemic control over time.15 Maintaining a healthy diet, physical activity, and having a healthy body mass index (BMI) can be challenging for individuals facing multiple social needs.16,17 In prior work, patients experiencing more social needs were more likely to miss follow-up appointments.18 Other studies have shown that individuals experiencing housing insecurity, for example, were more likely to report worse health and delays in medical care.19 Food insecurity is linked to worse diabetes-related symptoms and medication rationing,20 and deciding between buying food or buying medication.10 However, health systems, are not typically equipped to identify nor to address social needs of patients seen in the clinical setting. As a result, few studies15,20-22 have examined the association of unmet social needs and diabetes control among predominantly Black and Latino patients seen in primary care and servicing predominantly low-income areas.
Data from a large urban hospital system of predominantly Black and Hispanic patients shows that approximately 20% of screened patients have one or more unmet social needs.18 The objective of this study was to examine whether unmet social needs, and specific social need categories, were associated with uncontrolled diabetes among adults in a large urban health system.
Methods
Between April 2018 and December 2019, 54 854 unique patients from a Bronx, NY-based hospital system completed a 10-item social needs screener at participating primary care sites in the Bronx and Westchester counties, NY. After excluding patients less than 18 years old (n = 19 686), patients who did not complete every screener question (n = 1532) and patients with missing preferred language (n = 25), we identified those that had both a Type 2 diabetes diagnosis (E11.X) in the 2 years prior to the screener and an Hb A1c test result in the 3 months prior to the completed screener, which resulted in a final sample size of 5846. The primary outcome was diabetes control (categorized as Hb A1c <9.0 as controlled, Hb A1C ≥9.0 as uncontrolled) within the 3 months prior to social needs assessment.
The main independent variables were frequency of unmet social needs (the number of social needs categorized as 0, 1, 2, ≥3) and the 3 most prevalent unmet social need category for the sample, which included housing issues (housing instability and housing quality needs), food insecurity, and healthcare transportation. Unmet social needs were measured using a 10-item screening tool adapted from the Health Leads’ instrument (described elsewhere.)18 Briefly, the 10 items focused on actionable items which could be addressed by connecting patients to resources. Social needs data were only available for patients who visited clinics where screening practices were implemented. The decision to screen patients for unmet social needs was clinic-specific, and was influenced by multiple factors, including the overall risk of the population, the number of patients who visited the clinic, and staff availability to administer the screening. Additional covariates measured included age (continuous), sex (male and female), race/ethnicity (Hispanic, non-Hispanic Black, non-Hispanic other, and a missing indicator), insurance status (Medicaid, Medicare, commercial, and a missing indicator), percentage of block-group poverty (categorized into 5 quintiles and a missing indicator), the patient’s preferred language (English and non-English), and the Elixhauser Comorbidity Index (categorized as 0, 1-2, or ≥3). The Elixhauser Comorbidity Index excluded Type 2 diabetes. All data was extracted using Microsoft SQL Server, version 18, to query data from the Epic Electronic Health Record Data Warehouse and Looking Glass Clinical Analytics, version 4.4.2 (Streamline Health, Atlanta, GA), an online application supporting extraction of clinical data. To estimate area-based poverty level, the addresses of all patients living in NY, CT, PA, and NJ were geocoded using the New York State Street and Address Composite tool for NY addresses and the US Census Bureau geocoder for non-NY addresses. Those residing outside of these 4 states or reporting PO Box addresses were excluded (n = 467). After 97.7% of patients were successfully geocoded, their addresses were joined to block-group poverty data from the 2014 to 2018 American Community Survey, the latest year for which data was available. The prevalence of controlled and uncontrolled diabetes as well as all covariates were estimated by category of unmet social needs. To determine the relationship between social needs and diabetes control, a 2-stepped analytic approach was used. First, unadjusted, bivariate logistic regressions were estimated for number of social needs and each independent variable. Next, a fully-adjusted logistic regression model was estimated for the number of unmet social needs and also by each independent unmet social need, adjusting for all covariates. All models that included block-group poverty accounted for clustering of individuals. Tests for trend used the number of unmet social needs as a group linear variable. Statistical analyses used Stata 16.0 (StataCorp, College Station, TX) and mapping used ArcGIS 10.3.1 (ESRI, Redlands, CA). The study was approved by the Albert Einstein College of Medicine IRB. Data were analyzed in the spring of 2020.
Results
Bivariate analysis shows that patients with diabetes with more social needs are more likely to have uncontrolled diabetes (see Table 1). Approximately, 22% of the sample had at least 1 unmet social need. Patients with more unmet social needs were more likely to be younger, Hispanic, and insured through Medicaid. Overall, patients with more unmet social needs were more likely to live in poverty-dense neighborhoods and have more comorbidities. Housing issues (including housing quality and insecurity) were the most frequently occurring unmet social need (10.1%), followed by food insecurity (7.1%), and healthcare transportation (6.9%). Patients with unmet social needs were more likely to have uncontrolled diabetes when compared to individuals with no unmet social needs (see Figure 1). There was a dose-response relationship between the number of unmet social needs and risk of uncontrolled diabetes. Housing insecurity, food insecurity, and healthcare transportation were all linked to a higher likelihood of uncontrolled diabetes (see Figure 1). Of these unmet social needs, patients with unmet healthcare transportation had the highest risk of uncontrolled diabetes (Adjusted Odds-Ratio: 1.54 (95% CI: 1.22, 1.95) adjusting for covariates.
Table 1.
Summary of Demographic Variables for Patients With Social Risk Assessments Conducted Between April 2018 and December 2019: Bronx NY (n = 5846).
| Social needs | |||||
|---|---|---|---|---|---|
| None | 1 need | 2 needs | ≥3 needs | ||
| n | % | % | % | % | |
| Total | 5846 | 78.2 (77.15, 79.26) | 10.6 (9.81, 11.39) | 4.9 (4.38, 5.49) | 6.3 (5.70, 6.95) |
| Controlled diabetes (Hb A1C <9) | 4611 | 80.4 (79.3, 81.6) | 76.7 (73.2, 79.9) | 72.5 (67.0, 77.3) | 68.2 (63.3, 72.8) |
| Uncontrolled diabetes (Hb A1C ≥9) | 1235 | 19.6 (18.4, 20.7) | 23.3 (20.1, 26.8) | 27.5 (22.7, 33.0) | 31.8 (27.2, 36.7) |
| Age, y | |||||
| Mean (SD) | 63.2 (13.8) | 64.1 (13.7) | 62.4 (13.4) | 58.7 (14.1) | 57.6 (13.0) |
| Sex | |||||
| Male | 2238 | 39.0 (37.6, 40.4) | 36.9 (33.2, 40.8) | 29.3 (24.3, 34.8) | 38.6 (33.7, 43.7) |
| Female | 3608 | 61.0 (59.6, 62.4) | 63.1 (59.2, 66.8) | 70.7 (65.2, 75.7) | 61.4 (56.3, 66.3) |
| Race/ethnicity | |||||
| Hispanic | 2466 | 40.0 (38.6, 41.4) | 48.5 (44.6, 52.5) | 51.9 (46.1, 57.6) | 51.1 (46.0, 56.2) |
| Non-Hispanic black | 1768 | 31.1 (29.7, 32.4) | 29.1 (25.7, 32.8) | 24.7 (20.1, 30.1) | 26.1 (21.9, 30.8) |
| Other | 449 | 8.1 (7.3, 8.9) | 6.0 (4.4, 8.2) | 7.7 (5.1, 11.4) | 5.4 (3.5, 8.3) |
| Missing | 1163 | 20.8 (19.7, 22.0) | 16.3 (13.6, 19.5) | 15.7 (11.9, 20.4) | 17.4 (13.9, 21.6) |
| Preferred language | |||||
| English | 4374 | 75.3 (74.1, 76.6) | 73.1 (69.5, 76.5) | 71.4 (65.9, 76.4) | 73.9 (69.2, 78.1) |
| Non-English | 1472 | 24.7 (23.4, 25.9) | 26.9 (23.5, 30.5) | 28.6 (23.6, 34.1) | 26.1 (21.9, 30.8) |
| Payer | |||||
| Medicaid | 1431 | 21.4 (20.3, 22.6) | 27.8 (24.4, 31.5) | 42.9 (37.2, 48.7) | 42.4 (37.4, 47.5) |
| Medicare | 2918 | 51.1 (49.7, 52.6) | 52.6 (48.6, 56.5) | 39.4 (33.9, 45.1) | 38.6 (33.7, 43.7) |
| Commercial | 1238 | 23.3 (22.1, 24.5) | 14.4 (11.8, 17.4) | 13.2 (9.8, 17.7) | 12.8 (9.7, 16.6) |
| Missing | 259 | 4.2 (3.6, 4.8) | 5.2 (3.7, 7.2) | 4.5 (2.6, 7.6) | 6.3 (4.2, 9.2) |
| Block-group poverty, % | |||||
| Q1: 0-9.6 | 1205 | 22.4 (21.2, 23.6) | 16.8 (14.1, 20.0) | 11.5 (8.3, 15.7) | 12.0 (9.0, 15.7) |
| Q2: 9.7-19.6 | 1053 | 18.7 (17.5, 19.8) | 16.2 (13.5, 19.3) | 18.1 (14.1, 23.0) | 13.0 (10.0, 16.9) |
| Q3: 19.7-29.4 | 1131 | 19.6 (18.5, 20.8) | 17.8 (15.0, 21.0) | 20.6 (16.3, 25.6) | 17.7 (14.1, 21.9) |
| Q4: 29.5-41.3 | 1111 | 18.1 (17.0, 19.2) | 21.2 (18.2, 24.6) | 20.2 (16.0, 25.3) | 25.5 (21.3, 30.2) |
| Q5: 41.4-78.9 | 1128 | 17.5 (16.4, 18.6) | 25.1 (21.8, 28.7) | 26.8 (22.0, 32.3) | 26.1 (21.9, 30.8) |
| Missing | 218 | 3.7 (3.2, 4.3) | 2.9 (1.8, 4.6) | 2.8 (1.4, 5.5) | 5.7 (3.7, 8.6) |
| Elixhauser comorbidity index | |||||
| 0 | 128 | 2.1 (1.7, 2.6) | 2.3 (1.3, 3.8) | 3.8 (2.1, 6.8) | 1.9 (0.9, 3.9) |
| 1 | 808 | 14.3 (13.3, 15.3) | 10.7 (8.5, 13.4) | 16.4 (12.5, 21.1) | 11.1 (8.3, 14.8) |
| 2 | 948 | 16.8 (15.7, 17.9) | 13.4 (11.0, 16.4) | 13.9 (10.4, 18.4) | 15.8 (12.4, 19.9) |
| ≥3 | 3962 | 66.8 (65.4, 68.2) | 73.6 (70.0, 77.0) | 65.9 (60.2, 71.1) | 71.2 (66.4, 75.6) |
Figure 1.
Unadjusted and adjusted odds ratios and 95% confidence intervals (95%CI) of diabetes control by unmet social needs (n = 5846). Adjusted models include age, sex, race/ethnicity, preferred language, payer, area-based poverty and Elixhauser comorbidity score.
*P < .05.
Discussion
Uncontrolled diabetes leads to costly complications in terms of related morbidity and healthcare costs.23 There is a growing body of evidence from our group and others that unmet social needs are associated with increased chronic conditions and poorer health care access.24,25 In our patient sample, approximately 10% of patients have 2 or more unmet social needs (similar prevalence in a larger hospital system sample18). The dose-response relationship of multiple unmet social needs on diabetes control shown in this study suggests a compounding effect of social needs on diabetes control. There are few studies examining the relationship between food and housing insecurity and uncontrolled diabetes in clinical populations.14,17,20,21,26 However, the results of our study are consistent with other population-based reports suggesting food insecurity and unstable housing undermine disease prevention efforts and management of chronic conditions.26,27 Programs that link patients experiencing unmet social needs with services to address those unmet needs both within and outside of the clinical setting show various degrees of success.21,28,29 For example, Housing First has demonstrated success among individuals who are managing chronic conditions, including improved disease management, improved linkage to care through case management, and offering clients a sense of stability that enables them to manage other aspects of their life.30,31 However, more recent review of the evidence shows some potential limitations to the program’s effectiveness, including voluntary engagement with case management services (leading to various levels of resident/patient engagement) and a lack of implementation fidelity to the Housing First model.32 Programs to address hunger and food insecurity among patients typically consist of linking to federal food programs like WIC (Women, Infant, Children) and SNAP (Supplemental Nutrition Assistance Program). The relationship between healthcare-related transportation and diabetes control is less often examined. Recent advances in the implementation and scaling of telemedicine has emerged primarily due to the current COVID-19 pandemic.33,34 Telehealth visits have increased exponentially since the start of the pandemic.35 The potential for telehealth visits to address some of the barriers to care due to transportation are important to explore further particularly during this time of healthcare delivery during a viral pandemic.
A few limitations of the study design should be considered when interpreting the results. This study was cross-sectional, so it was not possible to determine causation or the longitudinal impact of social needs (including the type of social needs that change over time, and how social needs impact diabetes control over time.) The social needs screening tool was not universally implemented across all healthcare clinics in our healthcare system, decisions to implement the screening tools might include staff capacity to administer the screening, perceptions of patients (including their likelihood of having social needs), clinic volume, and patient health risk, therefore, there may be a selection bias of patients screened. However, despite these limitations, the results add to other existing evidence suggesting unmet social needs can undermine health and wellbeing of patients. Added strengths of this study that augment current research is the predominantly Black and Hispanic clinical sample from a large urban hospital system. Additionally, analyses included both the type and number of unmet social needs, highlighting the potential impact of various unmet social needs on diabetes control.
Conclusion
The results of this study show unmet social needs are associated with uncontrolled diabetes. In addition, healthcare-related transportation was the most strongly associated unmet social need with uncontrolled diabetes followed by food insecurity and housing issues. Prior research has shown that food insecurity and low-quality housing as well as limited access to healthcare can influence chronic health conditions.36-38 Our results are consistent with these reports but also show a dose-response relationship of unmet social needs on diabetes control where the risk was highest among patients with more unmet social needs. Within hospital systems, the capacity to systematically screen and connect patients with support resources is a necessary first step, but it is likely not sufficient to completely mitigate this complex issue. Health systems are beginning to invest in the resources needed to address unmet social needs but more research is needed to identify which patients to target and what interventions work to address these needs.
Footnotes
Authors’s Note: Earle C. Chambers is also affiliated with Montefiore Health System, Bronx, NY, USA and Nicole Hollingsworth is now affiliated with Hackensack Meridian Health, Edison, NJ, USA.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: ECC received funding from the following NIH grants: R01 DK121896, P30 DK111022. KF received funding from Doris Duke Charitable Foundation (grant #2018169) and Agency for Healthcare Research and Quality (K12 HS026396).
ORCID iDs: Kathleen E. McAuliff  https://orcid.org/0000-0001-6540-9729
https://orcid.org/0000-0001-6540-9729
Kevin Fiori  https://orcid.org/0000-0003-1370-7366
https://orcid.org/0000-0003-1370-7366
References
- 1. American Diabetes Association. Economic costs of diabetes in the US in 2017. Diabetes Care. 2018;41:917-928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chertman LS, Neuman D, Vendrame F. Update on diabetes medical management: epidemiology and treatment. In: Delamater A, Marrero D, eds. Behavioral Diabetes. Springer; 2020: 261-275. doi: 10.1007/978-3-030-33286-0_18 [DOI] [Google Scholar]
- 3. Smalls BL, Ritchwood TD, Bishu KG, Egede LE. Racial/ethnic differences in glycemic control in older adults with type 2 diabetes: United States 2003-2014. Int J Environ Res Public Health. 2020;17:950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Saydah S, Cowie C, Eberhardt MS, De Rekeneire N, Narayan KM. Race and ethnic differences in glycemic control among adults with diagnosed diabetes in the United States. Ethn Dis. 2007;17:529-535. [PubMed] [Google Scholar]
- 5. Katzmarzyk PT, Staiano AE. New race and ethnicity standards: elucidating health disparities in diabetes. BMC Med. 2012;10:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38:976-993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. O’Neill B, Ferrer R, O’Brien P, et al. Improving equity through primary care: proceedings of the 2019 Toronto international conference on quality in primary care. Ann Fam Med. 2020;18:364-369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. National Ambulatory Medical Care Survey: 2016 National Summary Tables. Accessed October 19, 2020. https://www.cdc.gov/nchs/data/ahcd/namcs_summary/2016_namcs_web_tables.pdf
- 9. Bolen SD, Sage P, Perzynski AT, Stange KC. No moment wasted: the primary-care visit for adults with diabetes and low socio-economic status. Prim Health Care Res Dev. 2016;17:18-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gucciardi E, Vahabi M, Norris N, Del Monte JP, Farnum C. The intersection between food insecurity and diabetes: a review. Curr Nutr Rep. 2014;3:324-332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Haire-Joshu D, Hill-Briggs F. The next generation of diabetes translation: a path to health equity. Annu Rev Public Health. 2019;40:391-410. [DOI] [PubMed] [Google Scholar]
- 12. Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999-2002. J Gen Intern Med. 2007;22:1018-1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Seligman HK, Jacobs EA, Lopez A, Tschann J, Fernandez A. Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care. 2012;35:233-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Vijayaraghavan M, Jacobs EA, Seligman H, Fernandez A. The association between housing instability, food insecurity, and diabetes self-efficacy in low-income adults. J Health Care Poor Underserved. 2011;22:1279-1291. [DOI] [PubMed] [Google Scholar]
- 15. Walker RJ, Garacci E, Palatnik A, Ozieh MN, Egede LE. The longitudinal influence of social determinants of health on glycemic control in elderly adults with diabetes. Diabetes Care. 2020;43:759-766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kumanyika SK. A framework for increasing equity impact in obesity prevention. Am J Public Health. 2019;109:1350-1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Patel MR, Piette JD, Resnicow K, Kowalski-Dobson T, Heisler M. Social determinants of health, cost-related nonadherence, and cost-reducing behaviors among adults with diabetes: findings from the National Health Interview Survey. Med Care. 2016;54:796-803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Heller CG, Parsons AS, Chambers EC, Fiori KP, Rehm CD. Social risks among primary care patients in a large urban health system. Am J Prev Med. 2020;58:514-525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stahre M, VanEenwyk J, Siegel P, Njai R. Housing insecurity and the association with health outcomes and unhealthy behaviors, Washington State, 2011. Prev Chronic Dis. 2015;12:E109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Berkowitz SA, Meigs JB, DeWalt D, et al. Material need insecurities, control of diabetes mellitus, and use of health care resources: results of the Measuring Economic Insecurity in Diabetes study. JAMA Intern Med. 2015;175:257-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Berkowitz SA, Hulberg AC, Standish S, Reznor G, Atlas SJ. Addressing unmet basic resource needs as part of chronic cardiometabolic disease management. JAMA Intern Med. 2017;177:244-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Blitstein JL, Lazar D, Gregory K, et al. Foods for health: an integrated social medical approach to food insecurity among patients with diabetes. Am J Health Promot. Published online October 12, 2020. doi: 10.1177/0890117120964144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Centers for Disease Control Prevention. National diabetes statistics report, 2020. Centers for Disease Control and Prevention, US Department of Health and Human Services; 2020: 12-15. [Google Scholar]
- 24. Fiori KP, Heller CG, Rehm CD, et al. Unmet social needs and no-show visits in primary care in a US Northeastern Urban Health System, 2018-2019. Am J Public Health. 2020;110(S2):S242-S250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Alcantara C, Diaz SV, Cosenzo LG, Loucks EB, Penedo FJ, Williams NJ. Social determinants as moderators of the effectiveness of health behavior change interventions: scientific gaps and opportunities. Health Psychol Rev. 2020;14:132-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Berkowitz SA, Kalkhoran S, Edwards ST, Essien UR, Baggett TP. Unstable housing and diabetes-related emergency department visits and hospitalization: a nationally representative study of safety-net clinic patients. Diabetes Care. 2018;41:933-939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Keene DE, Henry M, Gormley C, Ndumele C. ‘Then I found housing and everything changed’: transitions to rent-assisted housing and diabetes self-management. Cityscape. 2018;20:107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gucciardi E, Yang A, Cohen-Olivenstein K, Parmentier B, Wegener J, Pais V. Emerging practices supporting diabetes self-management among food insecure adults and families: a scoping review. PloS One. 2019;14:e0223998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Vold L, Lynch M, Martin W. A review of housing and food intersections: implications for nurses and nursing research. Can J Nurs Res. 2019;51:221-232. [DOI] [PubMed] [Google Scholar]
- 30. Chhabra M, Spector E, Demuynck S, Wiest D, Buckley L, Shea JA. Assessing the relationship between housing and health among medically complex, chronically homeless individuals experiencing frequent hospital use in the United States. Health Soc Care Community. 2020;28:91-99. [DOI] [PubMed] [Google Scholar]
- 31. Srebnik D, Connor T, Sylla L. A pilot study of the impact of housing first-supported housing for intensive users of medical hospitalization and sobering services. Am J Public Health. 2013;103:316-321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Tsai J. Is the housing first model effective? Different evidence for different outcomes. Am J Public Health. 2020;110:1376-1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Anjana RM, Pradeepa R, Deepa M, et al. Acceptability and utilization of newer technologies and effects on glycemic control in type 2 diabetes: lessons learnt from lockdown. Diabetes Technol Ther. 2020;22:527-534. [DOI] [PubMed] [Google Scholar]
- 34. Tulenko K, Vervoort D. Cracks in the system: the effects of the coronavirus pandemic on public health systems. Am Rev Public Adm. 2020;50:455-466. [Google Scholar]
- 35. Short JB, Mammen A. A pandemic application of creative destruction in healthcare. Front Health Serv Manage. 2020;37:4-9. [DOI] [PubMed] [Google Scholar]
- 36. Caswell KJ, Zuckerman S. Food Insecurity, Housing Hardship, and Medical Care Utilization. Urban Institute; 2018. [Google Scholar]
- 37. Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21:71-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pollack CE, Griffin BA, Lynch J. Housing affordability and health among homeowners and renters. Am J Prev Med. 2010;39:515-521. [DOI] [PubMed] [Google Scholar]