Abstract
Platelet-derived microparticles (PMPs) are a group of micrometer-scale extracellular vesicles released by platelets upon activation that are responsible for the majority of microvesicles found in plasma. PMPs’ physiological properties and functions have long been investigated by researchers. In this regard, a noticeable area of studies has been devoted to evaluating the potential roles and effects of PMPs on cancer progression. Clinical and experimental evidence conflictingly implicates supportive and suppressive functions for PMPs regarding cancer. Many of these functions could be deemed as a cornerstone for future considerations of PMPs usage in cancer targeted therapy. This review discusses what is currently known about PMPs and provides insights for new and possible research directions for further grasping the intricate interplay between PMPs and cancer.
Keywords: PMP, Platelet, Microparticle, Cancer
Introduction
Cancer is the first cause of death globally followed by cardiovascular diseases, imposing high costs on the health system. Following recent medical breakthroughs, the researchers’ focus has shifted toward tumorigenic mechanisms, cancer management, effective treatments and reducing treatment side effects. Improvement of the current treatment strategies requires a deeper understanding of the tumor microenvironment and its effective elements, which will ultimately lead to the use of combination therapies. Platelets as a blood component, are capable of playing a key role in tumorigenesis. In order to grow, tumors require a network of blood supply and the platelets floating within this network attach to the tumor cells, get activated, accumulate and might become part of the tumor microenvironment, potentially affecting parenchyma and tumor-dependent stroma.1 Increasing data are proving platelets as a key element bridging between thrombotic events and inflammatory pathways, leading to systemic inflammatory and immune processes.2 Not only platelets provide secreted, pleiotropic inflammatory mediators and factors orchestrating heterotypic interactions with endothelial cells, neutrophils, and monocytes, but they also produce microparticles.3 Microparticles (MPs) are a heterogeneous group of mainly spherical vesicles which contrary to exosomes, form through a process of membrane budding (exocytosis) and are basically present in all body fluids and maintained at a concentration of >106/mL in blood under normal conditions, and reportedly increase during tissue hypoxia, oxidative stress, cell activation and a variety of diseases such as heparin-induced thrombocytopenia, thrombosis, idiopathic thrombocytopenic purpura, sickle cell disease, uremia, cancer, multiple sclerosis, rheumatoid arthritis, antiphospholipid syndrome and systemic lupus erythematosus.4-6 The first clues of a potential involvement of platelet MPs (PMPs) in cancer were provided when their high plasma levels were found in a variety of malignancies such as gastric and lung cancers, decreasing following therapy. Such findings are suggestive of a possible indicator of clinical prognosis.7-9 Initially, Chargaff and West10 identified PMPs as a precipitable factor in platelet-free plasma potentially capable of promoting thrombin generation. PMPs are currently known to comprise the majority of MP population in peripheral blood and account for over 70% of all extracellular vesicles.11,12
PMP characterization is generally based on electron and atomic microscopy, and analyzing protein markers, and single particle analyzers. Size distribution of PMPs varies in a wide range between 50 to 2000 nm, but is mainly within the 100-800 nm range.13-15
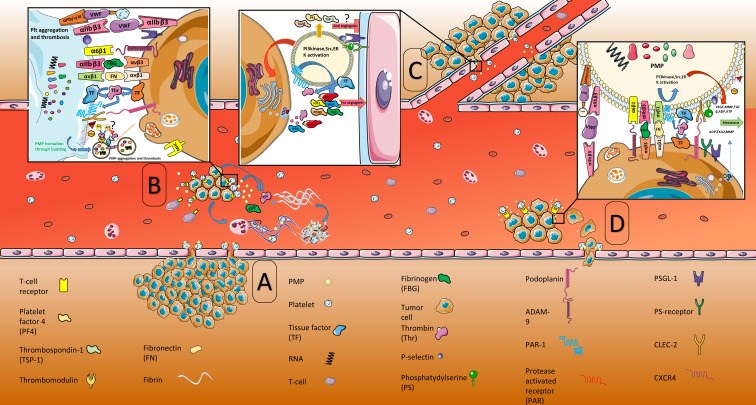
Means by which platelet microparticles get involved in tumorigenesis include shrouding tumor cells in circulation, allowing immune invasion, inducing a pro-coagulant state, aiding metastatic dissemination through establishing niches for the anchorage of circulating tumor cells, as well as anti-inflammatory, anticoagulant, antiangiogenic and apoptosis-inducing mechanisms (Figure 1). However, PMPs’ mechanisms of action after contacting the tumor cells is still a matter of debate.16 The present review will discuss how the PMPs influence tumorigenesis and their potential supportive and suppressive function in cancer progression.
Figure 1.
PMPs in cancer progression. (A) Endothelial dysfunction and poor coverage by pericytes lead to tumor cell intravasation. (B) Cancer cells promptly bind to platelets and activate them in bloodstream through adhesion molecules expressed on both cells. These interactions protect tumor cells against immune surveillance (platelet binding to tumor cells prevents tumor MHC molecule presentation to T-cells) and lead to the release of PMPs and activation of biomolecules participating in thrombosis, angiogenesis and metastasis. Tumor cell-PMP interactions increase the procoagulant activity of PMPs, providing a procoagulant membrane surface for thrombin activation and forming a prothrombinase complex which travels in the circulation, causing distant clot formation. PMPs can externalize tissue factor pathway inhibitor (TFPI) on their surface. The TF: FVIIa complex is regulated by TFPI, thrombomodulin, protein S or endothelial protein C receptor, conveying their ultimate participation in anticoagulant pathways. (C) Tumor cell-PMP interactions stimulate tumor cell expression of proangiogenic factors. The TF expression on PMPs initiates thrombin generation, subsequently boosting angiogenesis. PMPs may promote a switch to antiangiogenic state in endothelial cells. PMPs secrete PF4, TSP-1 and TGFβ which prompt a switch to anti-angiogenic state in endothelial cells. (D) Tumor cell-PMP interactions lead to metastasis. GPIIb/IIIa and TF play critical roles in metastases formation. GPIIb/IIIa supports stable adhesion of PMPs to tumor cells through binding to fibrinogen or vWF. GPIIb/IIIa (αIIbβ3) activation also initiates signaling which is responsible for the secretion of VEGF, ATP, ADP, TXA2, TGFβ and MMPs from PMPs. Presence of TF on the surface of PMPs provides a procoagulant membrane surface for thrombin generation, subsequently activating PAR-1 and signaling pathways mediated by PI3K, Src, and ERK, resulting in VEGF and MMPs secretion. PMPs also induce tumor cells to secrete ADP, TXA2 and MMPs. These mediators trigger tumor cell-induced platelet (and PMP) aggregation (TCIPA) which facilitates the microvascular arrest of tumor cells at distal sites during the metastasis process, tumor cell invasion, EMT and angiogenesis, all of which subsequently aid anchoring of metastatic tumor cells to distant sites, thereof assisting the establishment of new nodes. Moreover, ATP released from PMPs promotes tumor metastasis through relaxing endothelial barrier function upon binding the endothelial P2Y2 receptor and permitting extravasation of tumor cells. This figure was obtained using Servier Medical Art. (http://smart.servier.com/).
PMP
PMP formation, structure and components
PMP formation through cell membrane budding is tightly linked to surface exposure of phosphatidylserine on platelets. Cell membrane phospholipids are asymmetrically arranged under physiological conditions; sphingomyelin (SM) and phosphatidylcholine (PC) are present in the outer layer while phosphatidylethanolamine (PE) and phosphatidylserine (PS) lie in the inner layer. Membrane asymmetry is controlled by the “flip-flop” mechanism which is regulated by phospholipid transporters including scramblase, flippase and floppase.17 flippase, directed toward the cytosol and ATP-dependent transporters; (ii) floppases, directed toward the extracellular environment and ATP-dependent transporters; and (iii) scramblases, bidirectional and ATP-independent transporters. Scramblases allow for a random distribution of lipids between the membrane bilayers. The flippases are very selective for PS, and their action is responsible for maintaining this phospholipid mainly sequestered at the inner leaflet of the cell membrane.18,19 Platelet activation by agonists such as collagen, ADP, thrombin, and Ca2+ ionophore, activates resting platelets and increases intracellular calcium, which in turn, inactivates flippase and induces floppase and scramblase activation, resulting in immediate exposure of negatively charged phospholipid PS.17,20 The energy required for this translocation is supplied from the ATP provided by Ca2+-dependent proteolysis degradation.21 As intracellular calcium flush occurs, cell blebbing can happen through cysteine protease and μ calpain, which in turn leads to disaggregation of cytoskeleton constituents, as well as α-actinin and talin. In platelets though, μ calpain inhibition is reported to prevent PMP shedding and its activation to be mediated by elevated cyclic AMP levels. As a result of activation of μ calpain and subsequently protein kinase A, cytoskeleton proteolytic degradation is triggered, which results in membrane blebbing and PMP release.19 Transmembrane protein 16F) TMEM16F) has been suggested to be necessary for phospholipid scrambling and PMP release.22 Some studies have been identified that there are some other specific molecular events to explain the connection between the increase of intracellular calcium after platelet activation and PS externalization. It has been suggested that PS externalization is another proposed cause of influx in the calcium channels, leading to calcium stores depletion, also known as store-operated calcium entry (SOCE), shown to be regulated by actin cytoskeleton. Through rearranging actin molecules of the cytoskeleton, GTPase Rho A acts in SOCE regulation and the subsequent PS exposure.19,23
While membrane scrambling and PS exposure are generally considered to be essential for PMP release, a considerable share of PMPs do not expose surface PS,However, we still cannot comprehend the intricacies of shedding of non-PS-exposing PMPs, implicating further research to grasp involved cellular mechanisms.12,19 Other processes which have also been implicated in PMP formation are proteasome function, protein tyrosine dephosphorylation, and calmodulin activation, the influence of which is not completely distinct.12,24,25 Detailed studies on PMPs have revealed noticeable complexity and heterogeneity of surface markers, content and size distribution.25,26 They are also different from megakaryocyte derived MPs based on surface markers. Table 1 presents the differences between platelet and megakaryocyte derived MPs. Platelet Microparticles are affected by the stimulus of their generation and their structural heterogeneity tightly depends on the mechanism resulting in their generation.15,27 Based on structural variations, PMPs can be categorized into three groups of single-layered PMPs, multi-vesicular PMPs, and organelle-containing PMPs. For instance, PMPs formed as a result of platelet stimulation by thrombin are comparatively smaller in size and contain cytoplasm, cellular components and organelles such as a mitochondrion, alpha- and glycogen granules.15
Table 1. Diversity of MPs markers based on cell of origin .
| MP Source | Specific Markers | References |
| Megakaryocyte | GPVI | 23,25,34 |
| αIIbβ3 (CD41), CD42b | ||
| Filamin A | ||
| Activated platelet | P-selectin(CD62P) | 23,25,35 |
| LAMP-1 | ||
| CD31, CD42b,CD36,CD61, αIIbβ3 (CD41) | ||
| PS+/- | ||
| Apoptotic platelet | CD31, CD42b | 19,23,35 |
| Histones | ||
| Fragmented DNA | ||
| High levels of phosphatidylserine |
Abbreviations: MP: Microparticle; GP: Glycoprotein; CD: Cluster of Differentiation; LAMP-1: Lysosomal-associated membrane protein 1; PS: Phosphatidylserine.
The density of PMPs largely depends on the quantity and quality of the glycoproteins, which mostly consist of membrane transporters and adhesion receptors. PMPs carry over forty different glycoproteins including IIb/IIIa, Ib/IX, P-selectin and gp53, as well as receptors for a number of coagulation factors. A variety of molecules are found in PMPs including coagulation, transcription and growth factors, enzymes, adhesion molecules, cytokines, chemokines, complement proteins, bioactive lipids, lipid mediators factors, apoptosis regulators and miRNAs.28,29 A comprehensive summary of PMP’s content and surface markers and their functions is outlined in Table 2. Many bioactive substances are released during platelet activation, which are typically stored in their α and dense granules. The fact that PMPs have a higher content of PS and P-selectin compared to their cell of origin, suggests either the existence of a dynamic process for content selection or that the PMPs arise from particular regions of platelet membrane rich in such factors, while the findings regarding flow-induced protrusions also promote the hypothesis that the budding might occur in specific regions.30,31 A proportion of PMPs may also transfer their mitochondria, while there are studies speculating the role of PMPs as a source of circulating nucleic acids. Size seems to be another factor influencing PMPs constitution, as size distribution and content have been revealed to be correlated with one another.32,33
Table 2. PMP’s content and surface markers and their functions .
| PMP surface marker and content | Function | References |
| CD42b (GPIb) | Adhesion to vWF | 36-38 |
| Neutrophil activation | ||
| CD62P (P-Selectin) | Binding to PSGL-1 | 33,34,38-40 |
| CD42a (GPIbIX) | Adhesion | 41,42 |
| CD61 (GPIIIa) | Adhesion | 43-45 |
| Aggregation | ||
| CD41/61 (GPIIb/IIIa, αIIbβ3) | Adhesion | 46-48 |
| Aggregation | ||
| Tumor cells metastasis | ||
| Binding to fibrinogen | ||
| Lysosomal-associated membrane protein-3 (LAMP3, CD63, gp53) | Adhesion | 49 |
| Inflammation | ||
| Receptors for coagulation factors | Binding to FVa and FVIIIa | 33 |
| Anionic phospholipids | Passive procoagulant activity | 50 |
| MMPs | Degrading ECM | 11 |
| CXCR4 | Inflammatory response | 47,51 |
| Cytokine receptors: TNFR-I, TNFR-II | TNFα-induced CD40L expression | 40,52 |
| TF | Activating coagulation | 50 |
| PAR-1 (protease-activated receptor) | Procoagulant activity | 47,53 |
| MHC1 (probable) | Presenting antigens to T cells | 54,55 |
| CD40L (CD154) | Activating B Cells | 33,56 |
| C-type lectin-like receptor (CLEC-2) | Probably binding to Podoplanin (PDPN) | 57 |
| LPC (probable) | Platelet activation, spread, aggregation and migration | 58 |
| Vascular inflammation | ||
| Complement activator (gC1qR , IgG) | Complement activation | 59 |
| Inflammation | ||
| Complement regulators (C1-INH, CD55, CD59) | Regulating complement system | 59 |
| Enzymes (cyclooxygenase-1,12-lipoxygenase, caspases 3 and 9, Heparanase, NO synthase) | Pro/anti-inflammatory response | 25,33,60,61 |
| Apoptosis | ||
| Tumorgenesis | ||
| Growth factors (VEGF, PDGF, TGFβ, bFGF, IGF1) |
Angiogenesis | 33,62 |
| Metastasis | ||
| Cytokines (IL1b, IL-6, IL-8) |
Inflammation | 33,62-64 |
| Angiogenesis | ||
| Megakaryopoiesis | ||
| Chemokines (CCL5, CCL23, CXCL7, CXCL4) |
Monocytic arrest on ECs | 33,49,62,65 |
| Negative angiogenesis factor | ||
| Suppressing neutrophil apoptosis | ||
| S1P, AA, Thromboxane A2 | AA delivery to cells | 65,66 |
| Transcription factors | Regulating inflammation and immunity | 33,67 |
| MicroRNAs | RNA transfer to target cells | 30,68,69 |
| Mitochondria | Producing inflammatory mediators | 25 |
| Inducing leukocyte activation | ||
| Thrombospondin | Antiangiogenesis factor | 70 |
| Platelet-activating factor | Activating neutrophils and macrophages | 71 |
Abbreviations: PMP, Platelet microparticle; vWF, von Willebrand factor; PSGL-1, P-selectin glycoprotein ligand-1; ECM, Extracellular matrix; CXCR4, C-X-C chemokine receptor type 4; TNFR, Tumor necrosis factor receptor; MHC, major histocompatibility complex; FasL, Fas ligand; VEGF, Vascular endothelial growth factor; PDGF, Platelet derived growth factor; TGFβ, Transforming growth factor beta; bFGF, basic fibroblast growth factor; IGF1, Insulin-like growth factor 1; IL, interleukin; EC, Endothelial cell; AA, Arachidonic acid; S1P, Sphingosine-1-phosphate; MMPs, Metalloproteinases; TF, Tissue factor; LPC, Lysophosphatidylcholine.
Platelet activation mechanisms
Factors triggering PMP formation in circulation include platelets apoptosis, platelets exposure to complement component C5b9, physiological or pathological elements resulting in cell activation (thrombin, collagen, ADP, Ca2+ ionophore) or infectious agents (e.g. bacterial lipopolysaccharide or influenza virus H1N1), shear stress, blood processing and storage (PMP counts double over 5 days of storage in apheresis concentrates) and mediators released by tumor cells.25,72 Dual stimulation with thrombin and collagen or a single agonist mixed with shear stress has been reported to cause maximal PMP production. For instance, the requirement of von Willebrand factor (vWF) for shear-generated PMP is supported by the evidence that antibodies blocking the vWF receptor (CD42b) inhibit PMP production.73-76
PMPs function
PMP and intercellular communication
Due to their potency as intercellular communication mediators, PMPs have recently been considered of particular interest by researchers. PMPs interact with many cells such as neutrophils, monocytes, endothelial and tumor cells to induce phenotypic changes or new functions in these cells by delivering a variety of factors including bioactive proteins, lipids, enzymes, surface receptors, growth factors, transcription factors and miRNAs and are even capable of transferring infectious agents such as HIV and prion. PMPs transfer CXCR4 receptor to cells lacking it and make them vulnerable to X4-HIV. Plasma and platelets account for the main source of cell-associated prion proteins in human blood. Studies alike also report this protein to be released by apheresis-obtained platelets.1,30,77 Although several poorly understood modes of interactions have been reported, three modes have been hypothesized through which the PMPs interact with the other cells. One is signaling proteins and bioactive lipids present on PMP surface stimulating the receptors on the target cells.78 Another hypothesis is the fusion of PMPs with the target cells to transfer the membrane integral proteins, while the third suggestion is PMP internalization and unpacking for the delivery of miRNAs and cytosolic enzymes.16 Membrane fusion between PMPs and cells leads to PMP content deposition in the recipient cell’s cytosol. This fusion process seems to be dependent on PS. However, PMPs find another way to interact with the target cell.79 Gas6 is a secretory protein which binds to the membrane PS and then functions as a ligand for tyrosine receptor kinases Axl, Tyro3, and MERtk.80 A recent study demonstrated that extracellular vesicles (including platelet microvesicle or PMP) are sorted into the endosomal pathway, moving quickly through the cytoplasm and then stalling at the endoplasmic reticulum, before eventually fusing with lysosomes for degradation inside the target cell.81 However, further studies are still required to clearly perceive the regulation of PMPs uptake. Mechanisms concerned in PMP adhesion as well as its internalization within tumor cells are yet to be elucidated, though are hypothesized to involve interactions with various receptors like GP1b, p-selectin and PS receptors on the surface of tumor cell, alongside other interactions such as phagocytosis or fusion.82,83
PMP, inflammation and metastasis
Several mechanisms have been known for activated platelets to signal their target cells involved in inflammatory interactions, some of which occur through secreting mediators which might involve PMPs.84 PMPs are also reportedly increased in several other disease states with a recognized inflammatory component involved.85-87 Particular effects of PMP molecular transfer might be dependent on the type of target cells as well as the underlying inflammatory disease and certain patient factors.88 They might also exert anti-inflammatory effects, the mechanisms of which remain to be known. An overview of PMP involvement in inflammation is provided in Table 3.
Table 3. PMP involvement in inflammation .
| PMP’s inflammatory mediator | Target cell | Outcome of interaction | References |
| RANTES (CCL5) | Monocytes Activated endothelial cells |
Vascular wall infiltration | 16,96 |
| Stimulating chemotactic motility | |||
| Inducing monocytic arrest on endothelial cells | |||
| AA | Monocyte – Endothelial cells | Activation of PKC | 97 |
| Increased adherence between monocytes and endothelial cells | |||
| Increased chemotaxis of U-937 promonocytic cell line | |||
| CD41 and CD62P | Endothelial cells | Endothelial cell activation | 11 |
| PS | Macrophages Dendritic cells |
Neutralizing dendritic cells and macrophages phagocytic activity | 98 |
| Phosphatidylserine, GPIIb/IIIa, P-selectin | Monocytes | Activating monocytes | 99 |
| Protumorigenic effect | |||
| Upregulating phagocyte markers expression | |||
| PPARγ/RXR complex | THP-1 monocytic cell line | Aggregation of THP-1 cells | 100 |
| Producing TF+ monocytic MVs | |||
| Modifying gene expression | |||
| miR 126-3p | Macrophages | Inducing phagocytic phenotype | 101 |
| Downregulation of cytokine/chemokine secretion | |||
| Induced monocyte differentiation to M2 macrophage | |||
| PS? | Macrophages | Reduced release of TNF-ɑ and IL-10 | 98 |
| Immediately induced release of TGF-β from macrophage | |||
| AA | U-937 (promonocytic cell line) | Increased Mac-1 and ITGAL (integrin subunit alpha L) expression | 66,102,103 |
| Increased chemotaxis | |||
| AA | Endothelial cells Monocytes |
Expression of thromboxane A2 and COX-2 in endothelial cells | 66,102 |
| Facilitating platelet aggregation | |||
| Facilitating monocyte-EC interaction | |||
| Mitochondria | Leukocytes | Hydrolysis of mitochondrial membrane by sPLA2-IIA producing inflammatory mediators which promote leukocyte activation | 32,84 |
| CD154 (CD40 L) | B cells | Switch of antigen-specific IgG secretion | 56 |
| CD154 (CD40 L) | Monocytes | Increased inflammatory signals (IL1β, TNFα, MCP1) | 49,104,105 |
| Stimulating monocyte-derived dendritic cells maturation | |||
| miR-183 | NK cells | Knockdown of NK activation adapter DAP12 | 91,106,107 |
| Suppressing NK cell inflammatory response to tumor | |||
| TGFβ1 | CD4+ T Cells | Increased TGFβ1 production | 108 |
| Increased differentiation of CD4+ naive Tcells to FOXP3+ regulatory Tcells | |||
| PF4(CXCL4) | CD4+ T Cells | Anti-inflammatory effect through reducing IFNγ, IL6, TNFα expression | 109 |
| PF4(CXCL4) | Treg cells | Treg stability in an inflammatory environment | 110 |
| CXCR3-mediated signaling in activated T cells | |||
| Negative regulator of TH17 differentiation | |||
| P-selectin | Treg cells | Treg stability in an inflammatory environment | 110 |
| PMP adhesion to Tregs through PSGL-1 | |||
| Prevention of peripheral blood–derived Tregs differentiation into IL-17– and IFN-γ producing cells | |||
| P-Selectin | Neutrophils | Triggering neutrophil activation, aggregation and phagocytosis | 111 |
| Inducing adhesion to the endothelium | |||
| GPIbα | Neutrophils (β2 integrin Mac 1 (CD11b/CD18) | Neutrophil activation | 49,111 |
| GPIIb/IIIa receptors | Neutrophils | Transferring GPIIb/IIIA to neutrophils participating in NFkB activation of neutrophils | 112 |
| sPLA2-IIA and 12-lipoxygenase | Neutrophils | Promoting PMP internalization | 113,114 |
| Enhancing inflammation | |||
| β defensin 1 | Neutrophils | NETosis (neutrophil extracellular traps) Cancer associated thrombosis |
49,115 |
| PMP-miRNAs | Neutrophils | Not clear | 16 |
| PMPs miRNAs released from collagen-activated platelets | Leukocytes | Stimulating cytokine responses | 115,116 |
| Regulating cytokines release | |||
| 12-lipoxygenase | Mast cells | Negative inflammatory regulator | 60 |
Abbreviations: PMP, platelet microparticles; N/A ,Not applicable; MVs, microvesicles; AA, Arachidonic acid; COX-2, cyclooxygenase-2; EC, Endothelial cell; sPLA2-IIA, secretory Phospholipase A2 group IIA; IgG, Immunoglobulin G; TNFα, tumor necrosis factor alpha; MCP1, monocyte chemoattractant protein-1; NK cells, Natural killer cells; IFNγ, Interferon gamma; Treg cells, T regulatory cells; TH, T helper cells.
Platelets assist cancer progression in a number of levels, especially at the late stages of primary tumors and metastasis.89,90 Formation of platelet–tumor-PMP aggregates, might facilitate tumor cells microvascular arrest at distal sites during the metastasis process.91 Distant metastasis needs tumor cells to undergo the following: crossing the vessel wall, remaining in circulation, angiogenesis, and ultimately proliferation at a new metastasis site.7,92 The interactions between tumor cells and platelets which lead to metastasis depend on platelet capacity to bind to the injured vascular endothelium, its capability of paracrine regulation of tumor cell growth and proliferation, and its ability to protect neoplastic cells in circulation against immune cells, and PMPs are likely to contribute to metastasis in a similar fashion.11 Bakewell et al. suggested that integrin β3 (heterodimer of αVβ3 and αIIbβ5) plays a critical role in metastasis, while platelet receptor (GP IIb/IIIa) antagonist serves as a protective factor against bone and other organs metastases.93 PMPs induced by certain breast cancer cell lines have been shown to strongly potentiate invasion and migration of these cells, though how PMPs bind to these cells remains a mystery and contrary to previous assumption that integrin αIIbβ3 and P selectin are involved in the process, it is now demonstrated that neither are. Such findings, suggest the existence of a positive feedback mechanism, by which cancer cells magnify their aggressiveness through PMP release induction.94 Tissue factor (TF) has been well proven to function in tumor growth, angiogenesis and metastasis. Thereby, it is not a surprising finding that its presence on the surface of PMPs facilitates metastasis.11,93 The role of metalloproteinases has been proven in advancing tumor invasion and angiogenesis. PMPs not only secrete metalloproteinases but also induce prostate cancer cells to do so. Furthermore, the procoagulant PMP surface aids anchoring of metastatic tumor cells to distant sites, establishing new nodes.90,95 PMPs also increase proliferation of A549 human lung carcinoma cell line, leading to expression of abnormal cyclin D2 and formation of distal lung metastases in mice 7. The delivery of PMP-coated cells into mice increases distal metastasis to the bone marrow and lung, compared to the control group only treated with the murine lewis lung carcinoma cells.7,93 Moreover, ATP generated by tumor-associated platelets in the process of PMP formation in blood promotes tumor metastasis through relaxing endothelial barrier function.91
PMP and thrombosis
Cancer-related venous thromboembolism (VTE) was firstly described in the mid-19th century. Since then, the ever-growing risk of VTE has been the subject of intense research. VTE is described as the formation of blood clots in deeper veins of arm, leg, or groin that travel in circulation or lodging in the lungs (Pulmonary Embolism). This phenomenon occurs in 15 to 20% of cancerous patients.117,118 An increased level of platelet-, monocyte-, and endothelial-derived MPs are correlated with thrombotic events occurred in arterial and venous vessels42,119 In cancer patients suffering from VTE, the increased procoagulant activity of MPs including PMP is already observed at baseline, implying that it might be considered as a prognostic marker for VTE.117,118 Sinauridze et al applied two in vitro models (i.e., spatial clot formation and thrombin generation assays) to investigate PMP membranes enrichment with CD62, PS, and factor X binding sites. They reported that PMPs show a 100-fold greater specific procoagulant activity compared to activated platelets.31 In another study, Zhao et al. showed that PMP plasma levels correlate with procoagulant activity of colon cancer and increase along with the advancement of cancer stage.8 Furthermore, PMPs might prove a source of “blood-borne” TF inherited from platelets.119 As TF plays an important role in thrombosis and is promoted by tumor cells, the TF-bearing PMPs are of significance in tumor cell-induced platelet aggregation (TCIPA).63 Campello et al showed that patients with unprovoked VTE and those with various cancers with or without VTE have remarkably higher PMP and TF-MP levels compared to the controls.120 Tesselar et al examined TF co-expression with CD61 through confocal immunofluorescence microscopy. They reported that these TF positive-PMPs may be formed by the fusion of PMPs and malignant epithelial cell-derived MPs.121 In line with the above study, Hron et al. observed a significantly higher TF positive-PMP level in advanced colorectal cancer patients than that of healthy individuals. This result can be explained by the considerable increase in TF positive-PMPs. They also speculated that colorectal cancer cells might transfer the TFs onto PMPs.122 Another result of this study was the considerably higher PS content on PMPs compared with leukocyte-derived MPs, which justifies the direct relationship between D-dimer levels and TF positive-PMPs.122 A meta-analysis covering four cohorts and two case-control studies reports that TF-bearing MPs (including PMPs) are associated with a higher risk of VTE in cancer patients, particularly in patients of pancreatic cancer.23,118 Toth et al observed that CD62-positive PMP levels are highly associated with the level of prothrombin. Moreover, using electron microscopy, they found that the number of PMPs adherent to vWF is 3.5 times higher in breast cancer patients compared to controls. PMPs are the most copious source of MPs and demonstrate an increased number of vWF-binding receptors including integrin αIIbβ3 or GPIb, which may have a possible role in thrombosis.123 PMPs bear a wide range of surface receptors, including integrin GPIbα-IX-V receptor complex, GPIIb/IIIa, CXCR4, and P-selectin. As a result, they provide a procoagulant membrane surface for thrombin activation and forming a prothrombinase complex that travels in the circulation. Hence, distant clots are formed that often exhibits a procoagulant effect outlasting the activated platelets that generated them75. Morel et al124 showed that anionic phospholipids on PMPs surface induce accumulation of procoagulant and protein C anticoagulant enzyme complexes. Here, depending on the cell of origin, PMPs are able to expose tissue factor pathway inhibitor (TFPI), thrombomodulin, endothelial protein C receptor or protein S and lead to their ultimate participation in anticoagulant pathways.They are capable of facilitating FVa inhibition by activated protein C (APC) while APC, dependent on protein S, can inhibit coagulation on MPs.75,125
Under particular conditions, anticoagulant properties of PMPs have been proven as beneficial for their potential role in the progress of the anticoagulant process in cancer. For example, in early sepsis, they can retain APC as an inhibitor of VIIIa and Va factors.125,126 Several studies have revealed that CD41-positive PMPs can promote the generation of small amounts of thrombin. Thus, an anticoagulant process along with the protein C system may be activated by Va and VIIIa inactivation.5,21 Knowing CD41-positive PMPs can prompt the generation of minute amounts of thrombin. However, it is disputable whether PMPs are a cause or a result of thrombosis 30. In this regard, no data is available about the PMP-associated anticoagulant effect on cancer cells. Furthermore, it is not clear whether platelet activation and thrombocytosis are ultimately the causative agents or the result of tumor progression.127 Overall, PMPs which were once explained as inert “cellular dust” are thereby no less than “thrombotic dynamite”, specifically in the state of malignancy, while they show anticoagulant properties as well.91
PMP and angiogenesis
Growth, tumorigenesis and metastasis all depend on abnormal angiogenesis, which is characterized by the new blood vessels forming capillaries to sustain an adequate level of oxygen delivery.128 This procedure is dependent on extracellular matrix degradation, disruption of cell-cell contact and the proliferation, migration and capillary tube forming of endothelial cells. Imbalance between many proangiogenic (signaling pathways and growth factors) and antiangiogenic factors (endostatin, angiostatin, thrombospondin-1) regulates angiogenesis. Among notable proangiogenic factors are vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF), basic fibroblast growth factor (bFGF), insulin-like growth factor 1 (IGF-1), epidermal growth factor (EGF), transforming growth factor beta 1 (TGF-β-1), regulated on activation normal T-cell expressed and secreted (RANTES), matrix metalloproteinases (MMP1, MMP2 and MMP9), angiopoietins (1, 2 and 4) and cytokines such as interleukin 6 (IL-6) and interleukin8 (IL-8).62,70 All these pro- and antiangiogenic factors are secreted by platelets, tumor cells and PMPs, and take part in various stages of angiogenesis, including migration, proliferation and adhesion of endothelial cells.129,130 PMPs stimulate formation of network capillary tubes and stimulate tumor cell expression of proangiogenic factors.7,78,84,131 They are loaded with proangiogenic factors (PDGF, FGF, VEGF) released from α granules of the platelets of origin. Interaction of PMPs with endothelial cells may prompt a switch to a proangiogenic state, a phenomenon which could be extended by PMPs’ capacity to induce expression of kinase-dependent protein (MAPK p42/44 andAKT) and matrix metalloproteinase type 1 (MT1-MMP), as well as MMP-9,2 mRNA, interleukin 8 and VEGF in tumor cells.132 CXCR4 transfer to early outgrowth cells by PMPs amplifies the proangiogenic properties such as extracellular matrix adhesion or enhanced migration, proliferation and tube formation.133 The TF on PMPs initiates thrombin generation, resulting in VEGF secretion and prompting angiogenesis.134 Kim et al firstly demonstrated that PMPs raise in vitro proliferation, chemotactic migration and formation of capillary-like tubes of human umbilical vein endothelial cells (HUVECs). The fundamental mechanisms are depended on the protein growth factors such as FGF-2 and VEGF, and lipid growth factors such as S1P, all of which were inhibited by PI3K and Gi protein inhibitors.78,128,134 Prokopi et al demonstrated that PMPs can influence the angiogenic function of endothelial progenitor cells and endothelial tube formation is prompted by endothelial progenitor cell culture conditioned medium. Such outcome was reduced by PMPs removal from the conditioned medium by filtration, ultracentrifugation or prohibition of the platelet GPIIb-IIIa integrin complex formation.131 Studies show that ADP-mediated platelet activation induces VEGF release (not endostatin), while thromboxane A2 stimulates endostatin release but not VEGF. Platelets’ releasate generated by ADP-mediated activation, has been also shown to promote migration and formation of EC tubules in angiogenesis in vitro models.84 The proangiogenic influence of platelets and PMPs raises the question of what their mechanism is in light of angiogenic inhibitors presence besides the activators in platelets α granules. A possible explanation was proposed by Italiano et al who revealed various localizations of angiogenic cytokines among different granules.135 This hypothesis was further noted by another group who reported that the α granules are morphologically heterogeneous by 3D analysis and electron tomography.136
PMP and apoptosis
Human platelets retain considerable quantities of FasL in their α-granules, which is either released into the medium or expressed on the surface once the platelet is activated.137 CD95 (Fas) expression is increased in cancer cells treated with platelets or its derivatives. This phenomenon could induce apoptosis in cancer cells through platelets interaction, which is in line with Bykovskaya and Yaftian et al findings.138,139 Although the presence of FasL on PMP surface has not been evidenced, the transmission of this receptor from platelets to PMPs is not far-fetched.140,141 sphingosine-1-phosphate which is a lipid component of PMP seems to mediate the anti-apoptotic effects of PMP on ECs.84 Human platelets also bear considerable amounts of CD40L in their alpha granules, which they either release to the medium or express on their surface once they are activated.142 CD40L expression on PMPs’ surface has been evidenced. The interaction between CD40L on platelets and PMPs’ surface with CD40 on pre-B ALL cells has also resulted in increased Fas expression in tumor cells which in turn induces apoptosis.143,144 Yet another study demonstrated that CD95L and CD95 possess several cancer related tumor-promoting and non-apoptotic functions, protecting and promoting cancer stem cells.145
PMP and miRNAs
miRNAs are 22-nucleotide-long regulatory RNAs expressed in multicellular organisms. MiRNAs control most (>60%) of mammalian protein-coding genes.146 While some miRNAs are universally expressed, many are specific to tissue or developmental stage.147 The RNA-induced silencing complex (RISC) directed by the miRNA sequence leads to translational inhibition and mRNA degradation by Argonaute nucleases. miRNA role in gene expression is mostly fine-tuning and lowering noise in protein expression.148 Platelets are rich in pre-miRNAs as well as mature miRNAs. Platelet-derived miRNAs are packed into PMPs and account for a major share of platelet content released in PMPs.16,28 miRNA content of PMPs seems to form a subgroup of platelet miRNAs, suggesting active selection and incorporation of miRNAs into PMPs rather than simply random integration 68. Purified PMPs can regulate gene expression and transfer some miRNA content to cells such as leukocytes and endothelium following co-culture in vitro.149-152 New potentials of PMPs have recently begun to emerge, mainly presenting their capability to transfer miRNA content and regulate gene expression in target cells, which allows them to impact cancer development at different stages.16 Studies have proved that the content of circulating PMP miRNA is modified in different pathologies suggesting their potential as biomarkers for the disease along with platelet activation.68,153 Many miRNAs abundant in PMPs target both oncogenes and tumor suppressor genes in different cancers, and have been considered as prognostic markers for malignancies and implicated in therapy resistance. Similar to platelets, PMPs may be rich in variant isoforms of miRNA (isomiRs) with base-shifted seed sites.82 Next-generation sequencing of RNA expression as well as expanded mapping for miRNA targets are required to clarify the full extent of platelet miRNA impact.16 While PMPs have formerly been considered as cancer-promoting agents, their potential in transmission of miRNA and gene expression downregulation in different cell types implies the possible tumor-suppressive and apoptosis-inductive properties of PMPs.16,82 PMPs interaction with tumor cells in solid tumors via direct transfer of platelet-derived miRNAs also modulates tumor cell gene expression, resulting in tumor cell apoptosis, and inhibits growth of colon and lung carcinoma ectopic tumors, whereas miR-24 blockade in tumor cells accelerates tumor growth in vivo.82 In another study on the effect of PMPs on HUVECs, it was revealed that released PMPs after platelet thrombin-mediated activation are rich in miR-223. PMPs internalization by HUVECs and subsequent transmission of Argonaute 2-miR-223 complexes lead to downregulation of miR-223 targets inside the recipient endothelial cells, which might occasionally cause endothelial apoptosis.82,83,150,154 In presence of PMPs, anti-angiogenic modulators such as thrombospondin-1 (THBS-1) are substantially downregulated in HUVECs. Transfer of miRNA let-7a which targets THBS-1 in HUVECs, explains the neovascularization effect of PMP.155,156 Results of several studies emphasize the potential of PMP-mediated miRNA delivery to affect gene expression in target cells. Such findings provide unprecedented insight into mechanisms underlying horizontal RNA transfer and unveil several regulatory roles for PMP miRNAs in cancer progression. Platelet miRNAs transfer might also alter other sides of tumor biology including multi-drug resistance, known to be controlled by MPs.157-160 Thereby, platelets both positively and negatively affect cancer progression using different fashions and at several stages.16,82,161
Table 4 summarizes some studies on PMP miRNAs and their possible involvement in cancer fate.
Table 4. PMP’s miRNAs and their functions .
| PMP miRNA(s) | Target cell | Physiological outcome | References |
| miR-223 | A549 human lung carcinoma cell line |
Downregulation of EPB41L3 | 152 |
| Improvement of cell invasion | |||
| miR-223 | HUVEC | Downregulation of EFNA1 and FBXW7 RNA | 162 |
| miR-223 | HUVEC | Downregulation of IGF-1R | 154 |
| Apoptosis | |||
| miRNA let-7a | HUVEC | Downregulation of thrombospondin-1 (THBS-1) | 155 |
| miR-22 miR-185 miR-320b miR-423-5p |
HMEC-1 human microvascular endothelial cell line |
Downregulation of ICAM-1 | 151 |
| miR-126-3p | Macrophage | Downregulation of ATF3, ATP1B1, ATP9A and RAI14 | 163 |
| Downregulation of CCL4, CSF1, TNFα | |||
| Enhanced phagocytic capacity | |||
| miR-24 | Colon and lung carcinoma cells | Mitochondrial depolarization | 82 |
| Increased caspase 3 activity | |||
| Induced apoptosis | |||
| Inhibited tumor growth | |||
| miR-183 | Natural killer cell | Suppressed cytolytic function of tumor-associated NK cell | 16 |
| miR-939 | Epithelial ovarian cancer cell | Inducing epithelial to mesenchymal transition | 164 |
Abbreviation: HUVEC, Human umbilical vein endothelial cell.
PMP, tumorigenesis and clinical evidence
Human cancer cells are able to promptly bind to platelets and activate them through α3-integrins on the cells or surface molecules such as glycoprotein IIb/IIIa on platelets, or via releasing mediators such as thromboxaneA2, ADP or tumor-associated proteinases.121 Such interactions result in increased expression of adhesion molecules, induced cytokine secretion, facilitated metastasis and angiogenesis, protection of tumor cells against immune surveillance, increased proliferation, migration and invasiveness of tumor cells, and activation of intracellular signaling pathways, wherein downstream signaling ultimately alters tumor cells reactivity with the endothelial cells.129 PMPs possess cytoplasmic proteins and chemokine receptors that strengthen tumor cell adhesion to endothelial cells, induce chemotaxis, upregulate matrix metalloproteinase production, and hence facilitate tumor cell invasiveness, which can also be prompted by the PS on the outer membrane of PMPs that coat tumor cells.1,129 Permeability of tumor neo-vasculature allows circulating PMPs immediate access to tumor cells, PMP infiltration, delivery of platelet-derived miRNAs to the tumor cells, growth suppression and gene regulatory effects, together expanding the reach and abilities of platelets and their microparticles to impact cancer progression beyond the intravascular area.165 Goldfinger et al noticed infiltration of PMPs in numerous solid tumor types and various tumor grades, though not in unaffected tissues. PMP exposure caused by vascular leak is hence likely limited to solid tumors distinguished from normal tissues.82 PMPs and platelets relationship with vascular leakage has recently been defined in ischemia and post-ischemic tissue repair, cardiovascular diseases, sepsis, diabetesand wound healing, indicating the impact of PMPs and miRNA transfer beyond the extent of solid tumor progression as a potential mediator of physiological responses to vascular leakage.166-172 Considering the critical role of platelets in cancer progression, PMPs could be involved in cancer cells proliferation, metastatic progression, inflammation, angiogenesis, apoptosis, immune evasion, extracellular matrix degradation, tumor growth and chemo-resistance.173 While an increased level of total PMPs in circulation has been observed in various types of malignancies such as gastric, ovarian, breast and lung cancer, high levels of PMPs have been correlated with tumor aggressiveness and poor clinical outcome.172,173 PMPs have been demonstrated to be capable of transferring CD41 to lung cancer cells, therefore triggering signaling molecules phosphorylation and promoting expression of MMPs and chemoinvasion. Moreover, PMPs which contain a certain epidermal growth factor receptor (EGFRvlll) typically expressed by gliomas cells, can transfer this oncogenic receptor to cancer cells lacking it, promoting their oncogenic activity.174 Nevertheless, Mege et al reported a decrease in PMP concentration in colorectal cancer patients compared to healthy individuals, which does not agree with Hron et al study122 showing higher TF positive-PMP levels in advanced colorectal cancer patients in comparison with healthy subjects.174
Independent of the tumor stage and under high shear stress conditions, platelet activation and aggregation as well as PMP formation are observed to increase. Although these increases vary by tumor type, they mostly appear to occur concurrently with cancer stage advancing and the highest levels are associated with advanced stages and distal metastasis of cancers.175-179
Table 5 outlines studies providing data on PMPs involvement in cancer.
Table 5. Clinical evidences of PMP involvement in tumorigenesis .
| Cancer type | PMP level increase | PMP influence | References |
| Myeloproliferative neoplasm | 2 fold | Thromboinflammation | 180,181 |
| Colorectal cancer | Up to 4 fold | Lymph node metastasis | 122,176 |
| Breast cancer | 3.5 fold | Improved cancer invasiveness | 7,11,123,182,183 |
| Induction of angiogenesis and metastasis | |||
| Raised number of vWF-binding receptors | |||
| P-glycoprotein transfer to tumor cells | |||
| Induction of HER2 | |||
| Gastric cancer | Up to 35 fold in stage IV compared to stage I, II, III |
Prediction of metastasis with sensitivity and specificity rates over 90% | 129,174,179 |
| Plasma levels of PMPs higher in patients than healthy control | |||
| Non-small cell Lung cancer | N/A | Induced expression of MMP9, MMP2 and angiogenic factors (VEGF, HGF, IL8) | 7,11,173 |
| Activation of signaling molecules phosphorylation (MAPK p42/44 and AKY) | |||
| Induced chemoinvasion, adhesion to endothelium and fibrinogen, tumor progression, metastasis and angiogenesis | |||
| Prostate cancer and HRPC | N/A | Increased adhesion of cancer cells to endothelium and ECM | 84,184,185 |
| Assisted tumor invasion by increased metalloproteinases production and secretion | |||
| Increased cancer cells accumulation | |||
| Increased IL-8 secretion | |||
| Neurogenerative disease | >N/A | Tumor development and metastasis | > 186 |
| Increased survival and proliferation of embryonic neural stem cells | |||
| Improved potential to differentiate to glia and neurons |
Abbreviations: PMP, Platelet microparticles; N/A, Not applicable; vWF, von Willebrand factor; HER2, Human epidermal growth factor receptor 2; MMP, Matrix metalloproteinase; VEGF, Vascular endothelial growth factor; HGF, hepatocyte growth factor; ECM, Extracellular matrix; HPRC, hormone-refractory prostate cancer
Conclusion and Perspectives
In this review, we explain the activation, formation, component and structure of PMPs. Next, we describe their participation in cancer development. Despite the limited number of works on the role of PMPs in cancer, it is very important to characterize PMPs as a potential biomarker in cancer. The fluctuations of MPs during a cancer may suggest the significant role of microparticles as a cellular transporter, which plays a key role in cancer physiopathology. While PMPs involvement in metastasis and immune evasion of tumor cells are not fully understood, they have been demonstrated to mediate horizontal transfer of RNAs, leading to further ambiguities. Considering their ability to inhibit tumor growth, PMPs might counteract the platelets immediate impact on promoting cancer progression. However, findings are also suggestive of their indirect role in cancer promotion through certain platelet miRNAs’ transfer.161 Such contrasting data propose a possible dual-phase impact, whereby PMPs play anticancer roles in primary stages of tumor growth to encourage cancer progression mainly through miRNA-independent mechanisms.16 Further studies are required to comprehensively understand the interactions between PMPs and tumor cells influencing cancer progression. What appears to be undisputed thus far is that PMPs can serve as signaling molecules, passing on regulatory miRNAs to a variety of cells, yet tumor-specific miRNAs, as well as their target mRNAs, need to be determined alongside different phenotypic outcomes of mRNA silencing by tumor types. Inasmuch as circulating PMPs and their platelet-derived regulatory miRNAs are unequivocally involved throughout cancer progression, explicating concerned mechanisms will not only be of keen interest to researchers but will also represent a potential major breakthrough in cancer therapeutic targeting.
Ethical Issues
Not applicable.
Conflict of Interest
None.
References
- 1.Ratajczak J, Wysoczynski M, Hayek F, Janowska-Wieczorek A, Ratajczak MZ. Membrane-derived microvesicles: important and underappreciated mediators of cell-to-cell communication. Leukemia. 2006;20(9):1487–95. doi: 10.1038/sj.leu.2404296. [DOI] [PubMed] [Google Scholar]
- 2.Morrell CN, Aggrey AA, Chapman LM, Modjeski KL. Emerging roles for platelets as immune and inflammatory cells. Blood. 2014;123(18):2759–67. doi: 10.1182/blood-2013-11-462432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Semple JW, Italiano JE Jr, Freedman J. Platelets and the immune continuum. Nat Rev Immunol. 2011;11(4):264–74. doi: 10.1038/nri2956. [DOI] [PubMed] [Google Scholar]
- 4.Flaumenhaft R. Formation and fate of platelet microparticles. Blood Cells Mol Dis. 2006;36(2):182–7. doi: 10.1016/j.bcmd.2005.12.019. [DOI] [PubMed] [Google Scholar]
- 5.Berckmans RJ, Nieuwland R, Böing AN, Romijn FP, Hack CE, Sturk A. Cell-derived microparticles circulate in healthy humans and support low grade thrombin generation. Thromb Haemost. 2001;85(4):639–46. [PubMed] [Google Scholar]
- 6.Headland SE, Jones HR, D’Sa AS, Perretti M, Norling LV. Cutting-edge analysis of extracellular microparticles using ImageStream(X) imaging flow cytometry. Sci Rep. 2014;4:5237. doi: 10.1038/srep05237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Janowska-Wieczorek A, Wysoczynski M, Kijowski J, Marquez-Curtis L, Machalinski B, Ratajczak J. et al. Microvesicles derived from activated platelets induce metastasis and angiogenesis in lung cancer. Int J Cancer. 2005;113(5):752–60. doi: 10.1002/ijc.20657. [DOI] [PubMed] [Google Scholar]
- 8.Zhao L, Bi Y, Kou J, Shi J, Piao D. Phosphatidylserine exposing-platelets and microparticles promote procoagulant activity in colon cancer patients. J Exp Clin Cancer Res. 2016;35:54. doi: 10.1186/s13046-016-0328-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dovizio M, Bruno A, Contursi A, Grande R, Patrignani P. Platelets and extracellular vesicles in cancer: diagnostic and therapeutic implications. Cancer Metastasis Rev. 2018;37(2-3):455–67. doi: 10.1007/s10555-018-9730-4. [DOI] [PubMed] [Google Scholar]
- 10.Chargaff E, West R. The biological significance of the thromboplastic protein of blood. J Biol Chem. 1946;166(1):189–97. [PubMed] [Google Scholar]
- 11.Żmigrodzka M, Guzera M, Miśkiewicz A, Jagielski D, Winnicka A. The biology of extracellular vesicles with focus on platelet microparticles and their role in cancer development and progression. Tumour Biol. 2016;37(11):14391–401. doi: 10.1007/s13277-016-5358-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arraud N, Linares R, Tan S, Gounou C, Pasquet JM, Mornet S. et al. Extracellular vesicles from blood plasma: determination of their morphology, size, phenotype and concentration. J Thromb Haemost. 2014;12(5):614–27. doi: 10.1111/jth.12554. [DOI] [PubMed] [Google Scholar]
- 13.Théry C, Witwer KW, Aikawa E, Alcaraz MJ, Anderson JD, Andriantsitohaina R. et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): a position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J Extracell Vesicles. 2018;7(1):1535750. doi: 10.1080/20013078.2018.1535750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nolan JP, Jones JC. Detection of platelet vesicles by flow cytometry. Platelets. 2017;28(3):256–62. doi: 10.1080/09537104.2017.1280602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ponomareva AA, Nevzorova TA, Mordakhanova ER, Andrianova IA, Rauova L, Litvinov RI. et al. Intracellular origin and ultrastructure of platelet-derived microparticles. J Thromb Haemost. 2017;15(8):1655–67. doi: 10.1111/jth.13745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lazar S, Goldfinger LE. Platelet microparticles and miRNA transfer in cancer progression: many targets, modes of action, and effects across cancer stages. Front Cardiovasc Med. 2018;5:13. doi: 10.3389/fcvm.2018.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bobrie A, Colombo M, Raposo G, Théry C. Exosome secretion: molecular mechanisms and roles in immune responses. Traffic. 2011;12(12):1659–68. doi: 10.1111/j.1600-0854.2011.01225.x. [DOI] [PubMed] [Google Scholar]
- 18.Nagata S, Sakuragi T, Segawa K. Flippase and scramblase for phosphatidylserine exposure. Curr Opin Immunol. 2020;62:31–8. doi: 10.1016/j.coi.2019.11.009. [DOI] [PubMed] [Google Scholar]
- 19.Benameur T, Osman A, Parray A, Ait Hssain A, Munusamy S, Agouni A. Molecular mechanisms underpinning microparticle-mediated cellular injury in cardiovascular complications associated with diabetes. Oxid Med Cell Longev. 2019;2019:6475187. doi: 10.1155/2019/6475187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morel O, Morel N, Jesel L, Freyssinet JM, Toti F. Microparticles: a critical component in the nexus between inflammation, immunity, and thrombosis. Semin Immunopathol. 2011;33(5):469–86. doi: 10.1007/s00281-010-0239-3. [DOI] [PubMed] [Google Scholar]
- 21.Freyssinet JM, Toti F. Formation of procoagulant microparticles and properties. Thromb Res. 2010;125 Suppl 1:S46–8. doi: 10.1016/j.thromres.2010.01.036. [DOI] [PubMed] [Google Scholar]
- 22.Fujii T, Sakata A, Nishimura S, Eto K, Nagata S. TMEM16F is required for phosphatidylserine exposure and microparticle release in activated mouse platelets. Proc Natl Acad Sci U S A. 2015;112(41):12800–5. doi: 10.1073/pnas.1516594112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zarà M, Guidetti GF, Camera M, Canobbio I, Amadio P, Torti M. et al. Biology and role of extracellular vesicles (EVs) in the pathogenesis of thrombosis. Int J Mol Sci. 2019;20(11) doi: 10.3390/ijms20112840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gupta N, Li W, Willard B, Silverstein RL, McIntyre TM. Proteasome proteolysis supports stimulated platelet function and thrombosis. Arterioscler Thromb Vasc Biol. 2014;34(1):160–8. doi: 10.1161/atvbaha.113.302116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boilard E, Duchez AC, Brisson A. The diversity of platelet microparticles. Curr Opin Hematol. 2015;22(5):437–44. doi: 10.1097/moh.0000000000000166. [DOI] [PubMed] [Google Scholar]
- 26.Marcoux G, Duchez AC, Cloutier N, Provost P, Nigrovic PA, Boilard E. Revealing the diversity of extracellular vesicles using high-dimensional flow cytometry analyses. Sci Rep. 2016;6:35928. doi: 10.1038/srep35928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shai E, Rosa I, Parguiña AF, Motahedeh S, Varon D, García Á. Comparative analysis of platelet-derived microparticles reveals differences in their amount and proteome depending on the platelet stimulus. J Proteomics. 2012;76 Spec No:287–96. doi: 10.1016/j.jprot.2012.02.030. [DOI] [PubMed] [Google Scholar]
- 28.Hunter MP, Ismail N, Zhang X, Aguda BD, Lee EJ, Yu L. et al. Detection of microRNA expression in human peripheral blood microvesicles. PLoS One. 2008;3(11):e3694. doi: 10.1371/journal.pone.0003694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aatonen M, Grönholm M, Siljander PR. Platelet-derived microvesicles: multitalented participants in intercellular communication. Semin Thromb Hemost. 2012;38(1):102–13. doi: 10.1055/s-0031-1300956. [DOI] [PubMed] [Google Scholar]
- 30.Edelstein LC. The role of platelet microvesicles in intercellular communication. Platelets. 2017;28(3):222–7. doi: 10.1080/09537104.2016.1257114. [DOI] [PubMed] [Google Scholar]
- 31.Sinauridze EI, Kireev DA, Popenko NY, Pichugin AV, Panteleev MA, Krymskaya OV. et al. Platelet microparticle membranes have 50- to 100-fold higher specific procoagulant activity than activated platelets. Thromb Haemost. 2007;97(3):425–34. [PubMed] [Google Scholar]
- 32.Boudreau LH, Duchez AC, Cloutier N, Soulet D, Martin N, Bollinger J. et al. Platelets release mitochondria serving as substrate for bactericidal group IIA-secreted phospholipase A2 to promote inflammation. Blood. 2014;124(14):2173–83. doi: 10.1182/blood-2014-05-573543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Melki I, Tessandier N, Zufferey A, Boilard E. Platelet microvesicles in health and disease. Platelets. 2017;28(3):214–21. doi: 10.1080/09537104.2016.1265924. [DOI] [PubMed] [Google Scholar]
- 34.Flaumenhaft R, Dilks JR, Richardson J, Alden E, Patel-Hett SR, Battinelli E. et al. Megakaryocyte-derived microparticles: direct visualization and distinction from platelet-derived microparticles. Blood. 2009;113(5):1112–21. doi: 10.1182/blood-2008-06-163832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zuwala-Jagiello J, Pazgan-Simon M, Murawska-Cialowicz E, Simon K. Influence of diabetes on circulating apoptotic microparticles in patients with chronic hepatitis C. In Vivo. 2017;31(5):1027–34. doi: 10.21873/invivo.11165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chirinos JA, Heresi GA, Velasquez H, Jy W, Jimenez JJ, Ahn E. et al. Elevation of endothelial microparticles, platelets, and leukocyte activation in patients with venous thromboembolism. J Am Coll Cardiol. 2005;45(9):1467–71. doi: 10.1016/j.jacc.2004.12.075. [DOI] [PubMed] [Google Scholar]
- 37.Sun C, Zhao WB, Chen Y, Hu HY. Higher plasma concentrations of platelet microparticles in patients with acute coronary syndrome: a systematic review and meta-analysis. Can J Cardiol. 2016;32(11):1325 e1–e10. doi: 10.1016/j.cjca.2016.02.052. [DOI] [PubMed] [Google Scholar]
- 38.Villmow T, Kemkes-Matthes B, Matzdorff AC. Markers of platelet activation and platelet-leukocyte interaction in patients with myeloproliferative syndromes. Thromb Res. 2002;108(2-3):139–45. doi: 10.1016/s0049-3848(02)00354-7. [DOI] [PubMed] [Google Scholar]
- 39.Nomura S, Ishii K, Kanazawa S, Inami N, Uoshima N, Ishida H. et al. Significance of elevation in cell-derived microparticles after allogeneic stem cell transplantation: transient elevation of platelet-derived microparticles in TMA/TTP. Bone Marrow Transplant. 2005;36(10):921–2. doi: 10.1038/sj.bmt.1705150. [DOI] [PubMed] [Google Scholar]
- 40.Baj-Krzyworzeka M, Majka M, Pratico D, Ratajczak J, Vilaire G, Kijowski J. et al. Platelet-derived microparticles stimulate proliferation, survival, adhesion, and chemotaxis of hematopoietic cells. Exp Hematol. 2002;30(5):450–9. doi: 10.1016/s0301-472x(02)00791-9. [DOI] [PubMed] [Google Scholar]
- 41.Ogata N, Imaizumi M, Nomura S, Shozu A, Arichi M, Matsuoka M. et al. Increased levels of platelet-derived microparticles in patients with diabetic retinopathy. Diabetes Res Clin Pract. 2005;68(3):193–201. doi: 10.1016/j.diabres.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 42.Bernal-Mizrachi L, Jy W, Jimenez JJ, Pastor J, Mauro LM, Horstman LL. et al. High levels of circulating endothelial microparticles in patients with acute coronary syndromes. Am Heart J. 2003;145(6):962–70. doi: 10.1016/s0002-8703(03)00103-0. [DOI] [PubMed] [Google Scholar]
- 43.VanWijk MJ, Boer K, Berckmans RJ, Meijers JC, van der Post JA, Sturk A. et al. Enhanced coagulation activation in preeclampsia: the role of APC resistance, microparticles and other plasma constituents. Thromb Haemost. 2002;88(3):415–20. [PubMed] [Google Scholar]
- 44.Pereira J, Alfaro G, Goycoolea M, Quiroga T, Ocqueteau M, Massardo L. et al. Circulating platelet-derived microparticles in systemic lupus erythematosus Association with increased thrombin generation and procoagulant state. Thromb Haemost. 2006;95(1):94–9. [PubMed] [Google Scholar]
- 45.Harlow FH, Brown MA, Brighton TA, Smith SL, Trickett AE, Kwan YL. et al. Platelet activation in the hypertensive disorders of pregnancy. Am J Obstet Gynecol. 2002;187(3):688–95. doi: 10.1067/mob.2002.125766. [DOI] [PubMed] [Google Scholar]
- 46.Nomura S, Suzuki M, Kido H, Yamaguchi K, Fukuroi T, Yanabu M. et al. Differences between platelet and microparticle glycoprotein IIb/IIIa. Cytometry. 1992;13(6):621–9. doi: 10.1002/cyto.990130610. [DOI] [PubMed] [Google Scholar]
- 47.Janowska-Wieczorek A, Majka M, Kijowski J, Baj-Krzyworzeka M, Reca R, Turner AR. et al. Platelet-derived microparticles bind to hematopoietic stem/progenitor cells and enhance their engraftment. Blood. 2001;98(10):3143–9. doi: 10.1182/blood.v98.10.3143. [DOI] [PubMed] [Google Scholar]
- 48.Gremmel T, Frelinger AL 3rd, Michelson AD. Platelet physiology. Semin Thromb Hemost. 2016;42(3):191–204. doi: 10.1055/s-0035-1564835. [DOI] [PubMed] [Google Scholar]
- 49.Lam FW, Vijayan KV, Rumbaut RE. Platelets and their interactions with other immune cells. Compr Physiol. 2015;5(3):1265–80. doi: 10.1002/cphy.c140074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Owens AP 3rd, Mackman N. Microparticles in hemostasis and thrombosis. Circ Res. 2011;108(10):1284–97. doi: 10.1161/circresaha.110.233056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Contento RL, Molon B, Boularan C, Pozzan T, Manes S, Marullo S. et al. CXCR4-CCR5: a couple modulating T cell functions. Proc Natl Acad Sci U S A. 2008;105(29):10101–6. doi: 10.1073/pnas.0804286105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pignatelli P, Cangemi R, Celestini A, Carnevale R, Polimeni L, Martini A. et al. Tumour necrosis factor alpha upregulates platelet CD40L in patients with heart failure. Cardiovasc Res. 2008;78(3):515–22. doi: 10.1093/cvr/cvn040. [DOI] [PubMed] [Google Scholar]
- 53.Kahner BN, Dorsam RT, Kunapuli SP. Role of P2Y receptor subtypes in platelet-derived microparticle generation. Front Biosci. 2008;13:433–9. doi: 10.2741/2690. [DOI] [PubMed] [Google Scholar]
- 54.Zufferey A, Schvartz D, Nolli S, Reny JL, Sanchez JC, Fontana P. Characterization of the platelet granule proteome: evidence of the presence of MHC1 in alpha-granules. J Proteomics. 2014;101:130–40. doi: 10.1016/j.jprot.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 55.Chapman LM, Aggrey AA, Field DJ, Srivastava K, Ture S, Yui K. et al. Platelets present antigen in the context of MHC class I. J Immunol. 2012;189(2):916–23. doi: 10.4049/jimmunol.1200580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sprague DL, Elzey BD, Crist SA, Waldschmidt TJ, Jensen RJ, Ratliff TL. Platelet-mediated modulation of adaptive immunity: unique delivery of CD154 signal by platelet-derived membrane vesicles. Blood. 2008;111(10):5028–36. doi: 10.1182/blood-2007-06-097410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tsukiji N, Inoue O, Morimoto M, Tatsumi N, Nagatomo H, Ueta K. et al. Platelets play an essential role in murine lung development through Clec-2/podoplanin interaction. Blood. 2018;132(11):1167–79. doi: 10.1182/blood-2017-12-823369. [DOI] [PubMed] [Google Scholar]
- 58.Diehl P, Nienaber F, Zaldivia MTK, Stamm J, Siegel PM, Mellett NA. et al. Lysophosphatidylcholine is a major component of platelet microvesicles promoting platelet activation and reporting atherosclerotic plaque instability. Thromb Haemost. 2019;119(8):1295–310. doi: 10.1055/s-0039-1683409. [DOI] [PubMed] [Google Scholar]
- 59.Yin W, Ghebrehiwet B, Peerschke EI. Expression of complement components and inhibitors on platelet microparticles. Platelets. 2008;19(3):225–33. doi: 10.1080/09537100701777311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tang K, Liu J, Yang Z, Zhang B, Zhang H, Huang C. et al. Microparticles mediate enzyme transfer from platelets to mast cells: a new pathway for lipoxin A4 biosynthesis. Biochem Biophys Res Commun. 2010;400(3):432–6. doi: 10.1016/j.bbrc.2010.08.095. [DOI] [PubMed] [Google Scholar]
- 61.Cui H, Tan YX, Österholm C, Zhang X, Hedin U, Vlodavsky I. et al. Heparanase expression upregulates platelet adhesion activity and thrombogenicity. Oncotarget. 2016;7(26):39486–96. doi: 10.18632/oncotarget.8960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Goubran HA, Kotb RR, Stakiw J, Emara ME, Burnouf T. Regulation of tumor growth and metastasis: the role of tumor microenvironment. Cancer Growth Metastasis. 2014;7:9–18. doi: 10.4137/cgm.s11285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Plantureux L, Mège D, Crescence L, Dignat-George F, Dubois C, Panicot-Dubois L. Impacts of cancer on platelet production, activation and education and mechanisms of cancer-associated thrombosis. Cancers (Basel) 2018;10(11) doi: 10.3390/cancers10110441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Beaulieu LM, Lin E, Mick E, Koupenova M, Weinberg EO, Kramer CD. et al. Interleukin 1 receptor 1 and interleukin 1β regulate megakaryocyte maturation, platelet activation, and transcript profile during inflammation in mice and humans. Arterioscler Thromb Vasc Biol. 2014;34(3):552–64. doi: 10.1161/atvbaha.113.302700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dean WL, Lee MJ, Cummins TD, Schultz DJ, Powell DW. Proteomic and functional characterisation of platelet microparticle size classes. Thromb Haemost. 2009;102(4):711–8. doi: 10.1160/th09-04-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Boilard E, Larabee K, Shnayder R, Jacobs K, Farndale RW, Ware J. et al. Platelets participate in synovitis via Cox-1-dependent synthesis of prostacyclin independently of microparticle generation. J Immunol. 2011;186(7):4361–6. doi: 10.4049/jimmunol.1002857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lannan KL, Sahler J, Kim N, Spinelli SL, Maggirwar SB, Garraud O. et al. Breaking the mold: transcription factors in the anucleate platelet and platelet-derived microparticles. Front Immunol. 2015;6:48. doi: 10.3389/fimmu.2015.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Diehl P, Fricke A, Sander L, Stamm J, Bassler N, Htun N. et al. Microparticles: major transport vehicles for distinct microRNAs in circulation. Cardiovasc Res. 2012;93(4):633–44. doi: 10.1093/cvr/cvs007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Xia L, Zeng Z, Tang WH. The role of platelet microparticle associated microRNAs in cellular crosstalk. Front Cardiovasc Med. 2018;5:29. doi: 10.3389/fcvm.2018.00029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gaetani E, Del Zompo F, Marcantoni M, Gatto I, Giarretta I, Porfidia A. et al. Microparticles produced by activated platelets carry a potent and functionally active angiogenic signal in subjects with Crohn’s disease. Int J Mol Sci. 2018;19(10) doi: 10.3390/ijms19102921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kuijpers TW, van den Berg JM, Tool AT, Roos D. The impact of platelet-activating factor (PAF)-like mediators on the functional activity of neutrophils: anti-inflammatory effects of human PAF-acetylhydrolase. Clin Exp Immunol. 2001;123(3):412–20. doi: 10.1046/j.1365-2249.2001.01483.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Falanga A, Tartari CJ, Marchetti M. Microparticles in tumor progression. Thromb Res. 2012;129 Suppl 1:S132–6. doi: 10.1016/s0049-3848(12)70033-6. [DOI] [PubMed] [Google Scholar]
- 73.Heemskerk JW, Bevers EM, Lindhout T. Platelet activation and blood coagulation. Thromb Haemost. 2002;88(2):186–93. [PubMed] [Google Scholar]
- 74.Morel O, Jesel L, Freyssinet JM, Toti F. Cellular mechanisms underlying the formation of circulating microparticles. Arterioscler Thromb Vasc Biol. 2011;31(1):15–26. doi: 10.1161/atvbaha.109.200956. [DOI] [PubMed] [Google Scholar]
- 75.Nomura S, Shimizu M. Clinical significance of procoagulant microparticles. J Intensive Care. 2015;3(1):2. doi: 10.1186/s40560-014-0066-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pontiggia L, Steiner B, Ulrichts H, Deckmyn H, Forestier M, Beer JH. Platelet microparticle formation and thrombin generation under high shear are effectively suppressed by a monoclonal antibody against GPIba. Thromb Haemost. 2006;96(6):774–80. [PubMed] [Google Scholar]
- 77.Goubran HA, Burnouf T, Stakiw J, Seghatchian J. Platelet microparticle: a sensitive physiological “fine tuning” balancing factor in health and disease. Transfus Apher Sci. 2015;52(1):12–8. doi: 10.1016/j.transci.2014.12.015. [DOI] [PubMed] [Google Scholar]
- 78.Kim HK, Song KS, Chung JH, Lee KR, Lee SN. Platelet microparticles induce angiogenesis in vitro. Br J Haematol. 2004;124(3):376–84. doi: 10.1046/j.1365-2141.2003.04773.x. [DOI] [PubMed] [Google Scholar]
- 79.Del Conde I, Shrimpton CN, Thiagarajan P, López JA. Tissue-factor-bearing microvesicles arise from lipid rafts and fuse with activated platelets to initiate coagulation. Blood. 2005;106(5):1604–11. doi: 10.1182/blood-2004-03-1095. [DOI] [PubMed] [Google Scholar]
- 80.Happonen KE, Tran S, Mörgelin M, Prince R, Calzavarini S, Angelillo-Scherrer A. et al. The Gas6-Axl protein interaction mediates endothelial uptake of platelet microparticles. J Biol Chem. 2016;291(20):10586–601. doi: 10.1074/jbc.M115.699058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Butler JT, Abdelhamed S, Kurre P. Extracellular vesicles in the hematopoietic microenvironment. Haematologica. 2018;103(3):382–94. doi: 10.3324/haematol.2017.183335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Michael JV, Wurtzel JGT, Mao GF, Rao AK, Kolpakov MA, Sabri A. et al. Platelet microparticles infiltrating solid tumors transfer miRNAs that suppress tumor growth. Blood. 2017;130(5):567–80. doi: 10.1182/blood-2016-11-751099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Jansen F, Yang X, Hoyer FF, Paul K, Heiermann N, Becher MU. et al. Endothelial microparticle uptake in target cells is annexin I/phosphatidylserine receptor dependent and prevents apoptosis. Arterioscler Thromb Vasc Biol. 2012;32(8):1925–35. doi: 10.1161/atvbaha.112.253229. [DOI] [PubMed] [Google Scholar]
- 84.Varon D, Shai E. Platelets and their microparticles as key players in pathophysiological responses. J Thromb Haemost. 2015;13 Suppl 1:S40–6. doi: 10.1111/jth.12976. [DOI] [PubMed] [Google Scholar]
- 85.Shantsila E, Kamphuisen PW, Lip GY. Circulating microparticles in cardiovascular disease: implications for atherogenesis and atherothrombosis. J Thromb Haemost. 2010;8(11):2358–68. doi: 10.1111/j.1538-7836.2010.04007.x. [DOI] [PubMed] [Google Scholar]
- 86.Siljander PR. Platelet-derived microparticles - an updated perspective. Thromb Res. 2011;127 Suppl 2:S30–3. doi: 10.1016/s0049-3848(10)70152-3. [DOI] [PubMed] [Google Scholar]
- 87.Goubran HA, Burnouf T, Radosevic M, El-Ekiaby M. The platelet-cancer loop. Eur J Intern Med. 2013;24(5):393–400. doi: 10.1016/j.ejim.2013.01.017. [DOI] [PubMed] [Google Scholar]
- 88.Schwertz H, Rondina MT. Platelets and their Microparticles go hand in hand. Thromb Res. 2018;168:164–5. doi: 10.1016/j.thromres.2018.07.018. [DOI] [PubMed] [Google Scholar]
- 89.Sharma D, Brummel-Ziedins KE, Bouchard BA, Holmes CE. Platelets in tumor progression: a host factor that offers multiple potential targets in the treatment of cancer. J Cell Physiol. 2014;229(8):1005–15. doi: 10.1002/jcp.24539. [DOI] [PubMed] [Google Scholar]
- 90.Varon D, Hayon Y, Dashevsky O, Shai E. Involvement of platelet derived microparticles in tumor metastasis and tissue regeneration. Thromb Res. 2012;130 Suppl 1:S98–9. doi: 10.1016/j.thromres.2012.08.289. [DOI] [PubMed] [Google Scholar]
- 91.Goubran H, Sabry W, Kotb R, Seghatchian J, Burnouf T. Platelet microparticles and cancer: an intimate cross-talk. Transfus Apher Sci. 2015;53(2):168–72. doi: 10.1016/j.transci.2015.10.014. [DOI] [PubMed] [Google Scholar]
- 92. Metastatic Cancer - National Cancer Institute. Available from: https://www.cancer.gov/types/metastatic-cancer.
- 93.Bakewell SJ, Nestor P, Prasad S, Tomasson MH, Dowland N, Mehrotra M. et al. Platelet and osteoclast beta3 integrins are critical for bone metastasis. Proc Natl Acad Sci U S A. 2003;100(24):14205–10. doi: 10.1073/pnas.2234372100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zarà M, Guidetti GF, Boselli D, Villa C, Canobbio I, Seppi C. et al. Release of prometastatic platelet-derived microparticles induced by breast cancer cells: a novel positive feedback mechanism for metastasis. TH Open. 2017;1(2):e155–e63. doi: 10.1055/s-0037-1613674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Labelle M, Begum S, Hynes RO. Platelets guide the formation of early metastatic niches. Proc Natl Acad Sci U S A. 2014;111(30):E3053–61. doi: 10.1073/pnas.1411082111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mause SF, von Hundelshausen P, Zernecke A, Koenen RR, Weber C. Platelet microparticles: a transcellular delivery system for RANTES promoting monocyte recruitment on endothelium. Arterioscler Thromb Vasc Biol. 2005;25(7):1512–8. doi: 10.1161/01.atv.0000170133.43608.37. [DOI] [PubMed] [Google Scholar]
- 97.Distler JH, Pisetsky DS, Huber LC, Kalden JR, Gay S, Distler O. Microparticles as regulators of inflammation: novel players of cellular crosstalk in the rheumatic diseases. Arthritis Rheum. 2005;52(11):3337–48. doi: 10.1002/art.21350. [DOI] [PubMed] [Google Scholar]
- 98.Sadallah S, Eken C, Martin PJ, Schifferli JA. Microparticles (ectosomes) shed by stored human platelets downregulate macrophages and modify the development of dendritic cells. J Immunol. 2011;186(11):6543–52. doi: 10.4049/jimmunol.1002788. [DOI] [PubMed] [Google Scholar]
- 99.Vasina EM, Cauwenberghs S, Feijge MA, Heemskerk JW, Weber C, Koenen RR. Microparticles from apoptotic platelets promote resident macrophage differentiation. Cell Death Dis. 2011;2(9):e211. doi: 10.1038/cddis.2011.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lin HC, Chang HW, Hsiao SH, Chou ML, Seghatchian J, Burnouf T. Platelet-derived microparticles trigger THP-1 monocytic cell aggregation and release of pro-coagulant tissue factor-expressing microparticles in vitro. Transfus Apher Sci. 2015;53(2):246–52. doi: 10.1016/j.transci.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 101.Laffont B, Corduan A, Rousseau M, Duchez AC, Lee CH, Boilard E. et al. Platelet microparticles reprogram macrophage gene expression and function. Thromb Haemost. 2016;115(2):311–23. doi: 10.1160/th15-05-0389. [DOI] [PubMed] [Google Scholar]
- 102.Barry OP, Pratico D, Lawson JA, FitzGerald GA. Transcellular activation of platelets and endothelial cells by bioactive lipids in platelet microparticles. J Clin Invest. 1997;99(9):2118–27. doi: 10.1172/jci119385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Barry OP, Praticò D, Savani RC, FitzGerald GA. Modulation of monocyte-endothelial cell interactions by platelet microparticles. J Clin Invest. 1998;102(1):136–44. doi: 10.1172/jci2592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kaneider NC, Kaser A, Tilg H, Ricevuti G, Wiedermann CJ. CD40 ligand-dependent maturation of human monocyte-derived dendritic cells by activated platelets. Int J Immunopathol Pharmacol. 2003;16(3):225–31. doi: 10.1177/039463200301600307. [DOI] [PubMed] [Google Scholar]
- 105.Bei JJ, Liu C, Peng S, Liu CH, Zhao WB, Qu XL. et al. Staphylococcal SSL5-induced platelet microparticles provoke proinflammatory responses via the CD40/TRAF6/NFκB signalling pathway in monocytes. Thromb Haemost. 2016;115(3):632–45. doi: 10.1160/th15-04-0322. [DOI] [PubMed] [Google Scholar]
- 106.Sadallah S, Schmied L, Eken C, Charoudeh HN, Amicarella F, Schifferli JA. Platelet-derived ectosomes reduce NK cell function. J Immunol. 2016;197(5):1663–71. doi: 10.4049/jimmunol.1502658. [DOI] [PubMed] [Google Scholar]
- 107.Donatelli SS, Zhou JM, Gilvary DL, Eksioglu EA, Chen X, Cress WD. et al. TGF-β-inducible microRNA-183 silences tumor-associated natural killer cells. Proc Natl Acad Sci U S A. 2014;111(11):4203–8. doi: 10.1073/pnas.1319269111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Haribhai D, Luo X, Chen J, Jia S, Shi L, Schroeder JA. et al. TGF-β1 along with other platelet contents augments Treg cells to suppress anti-FVIII immune responses in hemophilia A mice. Blood Adv. 2016;1(2):139–51. doi: 10.1182/bloodadvances.2016001453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sadallah S, Amicarella F, Eken C, Iezzi G, Schifferli JA. Ectosomes released by platelets induce differentiation of CD4+T cells into T regulatory cells. Thromb Haemost. 2014;112(6):1219–29. doi: 10.1160/th14-03-0281. [DOI] [PubMed] [Google Scholar]
- 110.Dinkla S, van Cranenbroek B, van der Heijden WA, He X, Wallbrecher R, Dumitriu IE. et al. Platelet microparticles inhibit IL-17 production by regulatory T cells through P-selectin. Blood. 2016;127(16):1976–86. doi: 10.1182/blood-2015-04-640300. [DOI] [PubMed] [Google Scholar]
- 111.Lo SC, Hung CY, Lin DT, Peng HC, Huang TF. Involvement of platelet glycoprotein Ib in platelet microparticle mediated neutrophil activation. J Biomed Sci. 2006;13(6):787–96. doi: 10.1007/s11373-006-9107-5. [DOI] [PubMed] [Google Scholar]
- 112.Li X, Cong H. Platelet-derived microparticles and the potential of glycoprotein IIb/IIIa antagonists in treating acute coronary syndrome. Tex Heart Inst J. 2009;36(2):134–9. [PMC free article] [PubMed] [Google Scholar]
- 113.Duchez AC, Boudreau LH, Naika GS, Bollinger J, Belleannée C, Cloutier N. et al. Platelet microparticles are internalized in neutrophils via the concerted activity of 12-lipoxygenase and secreted phospholipase A2-IIA. Proc Natl Acad Sci U S A. 2015;112(27):E3564–73. doi: 10.1073/pnas.1507905112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Rousseau M, Belleannee C, Duchez AC, Cloutier N, Levesque T, Jacques F. et al. Detection and quantification of microparticles from different cellular lineages using flow cytometry Evaluation of the impact of secreted phospholipase A2 on microparticle assessment. PLoS One. 2015;10(1):e0116812. doi: 10.1371/journal.pone.0116812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Scherlinger M, Sisirak V, Richez C, Lazaro E, Duffau P, Blanco P. New insights on platelets and platelet-derived microparticles in systemic lupus erythematosus. Curr Rheumatol Rep. 2017;19(8):48. doi: 10.1007/s11926-017-0678-0. [DOI] [PubMed] [Google Scholar]
- 116.Boilard E, Nigrovic PA, Larabee K, Watts GF, Coblyn JS, Weinblatt ME. et al. Platelets amplify inflammation in arthritis via collagen-dependent microparticle production. Science. 2010;327(5965):580–3. doi: 10.1126/science.1181928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.van Doormaal F, Kleinjan A, Berckmans RJ, Mackman N, Manly D, Kamphuisen PW. et al. Coagulation activation and microparticle-associated coagulant activity in cancer patients An exploratory prospective study. Thromb Haemost. 2012;108(1):160–5. doi: 10.1160/th12-02-0099. [DOI] [PubMed] [Google Scholar]
- 118.Cui CJ, Wang GJ, Yang S, Huang SK, Qiao R, Cui W. Tissue Factor-bearing MPs and the risk of venous thrombosis in cancer patients: a meta-analysis. Sci Rep. 2018;8(1):1675. doi: 10.1038/s41598-018-19889-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Khaspekova SG, Antonova OA, Shustova ON, Yakushkin VV, Golubeva NV, Titaeva EV. et al. Activity of tissue factor in microparticles produced in vitro by endothelial cells, monocytes, granulocytes, and platelets. Biochemistry (Mosc) 2016;81(2):114–21. doi: 10.1134/s000629791602005x. [DOI] [PubMed] [Google Scholar]
- 120.Campello E, Spiezia L, Radu CM, Bulato C, Castelli M, Gavasso S. et al. Endothelial, platelet, and tissue factor-bearing microparticles in cancer patients with and without venous thromboembolism. Thromb Res. 2011;127(5):473–7. doi: 10.1016/j.thromres.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 121.Tesselaar ME, Romijn FP, Van Der Linden IK, Prins FA, Bertina RM, Osanto S. Microparticle-associated tissue factor activity: a link between cancer and thrombosis? J Thromb Haemost. 2007;5(3):520–7. doi: 10.1111/j.1538-7836.2007.02369.x. [DOI] [PubMed] [Google Scholar]
- 122.Hron G, Kollars M, Weber H, Sagaster V, Quehenberger P, Eichinger S. et al. Tissue factor-positive microparticles: cellular origin and association with coagulation activation in patients with colorectal cancer. Thromb Haemost. 2007;97(1):119–23. [PubMed] [Google Scholar]
- 123.Toth B, Liebhardt S, Steinig K, Ditsch N, Rank A, Bauerfeind I. et al. Platelet-derived microparticles and coagulation activation in breast cancer patients. Thromb Haemost. 2008;100(4):663–9. [PubMed] [Google Scholar]
- 124.Morel O, Morel N, Freyssinet JM, Toti F. Platelet microparticles and vascular cells interactions: a checkpoint between the haemostatic and thrombotic responses. Platelets. 2008;19(1):9–23. doi: 10.1080/09537100701817232. [DOI] [PubMed] [Google Scholar]
- 125.Somajo S, Koshiar RL, Norström E, Dahlbäck B. Protein S and factor V in regulation of coagulation on platelet microparticles by activated protein C. Thromb Res. 2014;134(1):144–52. doi: 10.1016/j.thromres.2014.04.031. [DOI] [PubMed] [Google Scholar]
- 126.Reid VL, Webster NR. Role of microparticles in sepsis. Br J Anaesth. 2012;109(4):503–13. doi: 10.1093/bja/aes321. [DOI] [PubMed] [Google Scholar]
- 127.Meikle CK, Kelly CA, Garg P, Wuescher LM, Ali RA, Worth RG. Cancer and thrombosis: the platelet perspective. Front Cell Dev Biol. 2016;4:147. doi: 10.3389/fcell.2016.00147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zuazo-Gaztelu I, Casanovas O. Unraveling the role of angiogenesis in cancer ecosystems. Front Oncol. 2018;8:248. doi: 10.3389/fonc.2018.00248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Varon D, Shai E. Role of platelet-derived microparticles in angiogenesis and tumor progression. Discov Med. 2009;8(43):237–41. [PubMed] [Google Scholar]
- 130.Wang ZT, Wang Z, Hu YW. Possible roles of platelet-derived microparticles in atherosclerosis. Atherosclerosis. 2016;248:10–6. doi: 10.1016/j.atherosclerosis.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 131.Prokopi M, Pula G, Mayr U, Devue C, Gallagher J, Xiao Q. et al. Proteomic analysis reveals presence of platelet microparticles in endothelial progenitor cell cultures. Blood. 2009;114(3):723–32. doi: 10.1182/blood-2009-02-205930. [DOI] [PubMed] [Google Scholar]
- 132.Sun C, Feng SB, Cao ZW, Bei JJ, Chen Q, Zhao WB. et al. Up-regulated expression of matrix metalloproteinases in endothelial cells mediates platelet microvesicle-induced angiogenesis. Cell Physiol Biochem. 2017;41(6):2319–32. doi: 10.1159/000475651. [DOI] [PubMed] [Google Scholar]
- 133.Mause SF, Ritzel E, Liehn EA, Hristov M, Bidzhekov K, Müller-Newen G. et al. Platelet microparticles enhance the vasoregenerative potential of angiogenic early outgrowth cells after vascular injury. Circulation. 2010;122(5):495–506. doi: 10.1161/circulationaha.109.909473. [DOI] [PubMed] [Google Scholar]
- 134.Wojtukiewicz MZ, Sierko E, Hempel D, Tucker SC, Honn KV. Platelets and cancer angiogenesis nexus. Cancer Metastasis Rev. 2017;36(2):249–62. doi: 10.1007/s10555-017-9673-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Italiano JE Jr, Richardson JL, Patel-Hett S, Battinelli E, Zaslavsky A, Short S. et al. Angiogenesis is regulated by a novel mechanism: pro- and antiangiogenic proteins are organized into separate platelet alpha granules and differentially released. Blood. 2008;111(3):1227–33. doi: 10.1182/blood-2007-09-113837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.van Nispen tot Pannerden H , de Haas F, Geerts W, Posthuma G, van Dijk S, Heijnen HF. The platelet interior revisited: electron tomography reveals tubular alpha-granule subtypes. Blood. 2010;116(7):1147–56. doi: 10.1182/blood-2010-02-268680. [DOI] [PubMed] [Google Scholar]
- 137.Schleicher RI, Reichenbach F, Kraft P, Kumar A, Lescan M, Todt F. et al. Platelets induce apoptosis via membrane-bound FasL. Blood. 2015;126(12):1483–93. doi: 10.1182/blood-2013-12-544445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Bykovskaya SN, Bolvacheva AV, Kiselevsky MV, Khaylenko VA, Bykovsky AF. Platelet-mediated cytotoxicity and its enhancement by platelet activating factor. Biomed Pharmacother. 1991;45(7):279–88. doi: 10.1016/0753-3322(91)90082-5. [DOI] [PubMed] [Google Scholar]
- 139.Yaftian M, Yari F, Ghasemzadeh M. Induction of apoptosis in human tumor cell lines by platelets. J Basic Res Med Sci. 2017;4(3):26–33. doi: 10.29252/jbrms.4.3.26. [DOI] [Google Scholar]
- 140.Distler JH, Huber LC, Gay S, Distler O, Pisetsky DS. Microparticles as mediators of cellular cross-talk in inflammatory disease. Autoimmunity. 2006;39(8):683–90. doi: 10.1080/08916930601061538. [DOI] [PubMed] [Google Scholar]
- 141.Aharon A, Brenner B. Microparticles, thrombosis and cancer. Best Pract Res Clin Haematol. 2009;22(1):61–9. doi: 10.1016/j.beha.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 142.Aloui C, Prigent A, Sut C, Tariket S, Hamzeh-Cognasse H, Pozzetto B. et al. The signaling role of CD40 ligand in platelet biology and in platelet component transfusion. Int J Mol Sci. 2014;15(12):22342–64. doi: 10.3390/ijms151222342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Yaftian M, Yari F, Ghasemzadeh M, Fallah Azad V, Haghighi M. Induction of apoptosis in cancer cells of pre-B ALL patients after exposure to platelets, platelet-derived microparticles and soluble CD40 ligand. Cell J. 2018;20(1):120–6. doi: 10.22074/cellj.2018.5032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Shigeta A, Tada Y, Wang JY, Ishizaki S, Tsuyusaki J, Yamauchi K. et al. CD40 amplifies Fas-mediated apoptosis: a mechanism contributing to emphysema. Am J Physiol Lung Cell Mol Physiol. 2012;303(2):L141–51. doi: 10.1152/ajplung.00337.2011. [DOI] [PubMed] [Google Scholar]
- 145.Peter ME, Hadji A, Murmann AE, Brockway S, Putzbach W, Pattanayak A. et al. The role of CD95 and CD95 ligand in cancer. Cell Death Differ. 2015;22(4):549–59. doi: 10.1038/cdd.2015.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Javandoost E, Firoozi-Majd E, Rostamian H, Khakpoor-Koosheh M, Mirzaei HR. Role of microRNAs in chronic lymphocytic leukemia pathogenesis. Curr Med Chem. 2020;27(2):282–97. doi: 10.2174/0929867326666190911114842. [DOI] [PubMed] [Google Scholar]
- 147.Londin E, Loher P, Telonis AG, Quann K, Clark P, Jing Y. et al. Analysis of 13 cell types reveals evidence for the expression of numerous novel primate- and tissue-specific microRNAs. Proc Natl Acad Sci U S A. 2015;112(10):E1106–15. doi: 10.1073/pnas.1420955112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Oliveto S, Mancino M, Manfrini N, Biffo S. Role of microRNAs in translation regulation and cancer. World J Biol Chem. 2017;8(1):45–56. doi: 10.4331/wjbc.v8.i1.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Risitano A, Beaulieu LM, Vitseva O, Freedman JE. Platelets and platelet-like particles mediate intercellular RNA transfer. Blood. 2012;119(26):6288–95. doi: 10.1182/blood-2011-12-396440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Corduan A, Plé H, Laffont B, Wallon T, Plante I, Landry P. et al. Dissociation of SERPINE1 mRNA from the translational repressor proteins Ago2 and TIA-1 upon platelet activation. Thromb Haemost. 2015;113(5):1046–59. doi: 10.1160/TH14-07-0622. [DOI] [PubMed] [Google Scholar]
- 151.Gidlöf O, van der Brug M, Ohman J, Gilje P, Olde B, Wahlestedt C. et al. Platelets activated during myocardial infarction release functional miRNA, which can be taken up by endothelial cells and regulate ICAM1 expression. Blood. 2013;121(19):3908–17, s1. doi: 10.1182/blood-2012-10-461798. [DOI] [PubMed] [Google Scholar]
- 152.Liang H, Yan X, Pan Y, Wang Y, Wang N, Li L. et al. MicroRNA-223 delivered by platelet-derived microvesicles promotes lung cancer cell invasion via targeting tumor suppressor EPB41L3. Mol Cancer. 2015;14:58. doi: 10.1186/s12943-015-0327-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Willeit P, Zampetaki A, Dudek K, Kaudewitz D, King A, Kirkby NS. et al. Circulating microRNAs as novel biomarkers for platelet activation. Circ Res. 2013;112(4):595–600. doi: 10.1161/circresaha.111.300539. [DOI] [PubMed] [Google Scholar]
- 154.Pan Y, Liang H, Liu H, Li D, Chen X, Li L. et al. Platelet-secreted microRNA-223 promotes endothelial cell apoptosis induced by advanced glycation end products via targeting the insulin-like growth factor 1 receptor. J Immunol. 2014;192(1):437–46. doi: 10.4049/jimmunol.1301790. [DOI] [PubMed] [Google Scholar]
- 155.Huong PT, Nguyen LT, Nguyen XB, Lee SK, Bach DH. The role of platelets in the tumor-microenvironment and the drug resistance of cancer cells. Cancers (Basel) 2019;11(2) doi: 10.3390/cancers11020240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Anene C, Graham AM, Boyne J, Roberts W. Platelet microparticle delivered microRNA-Let-7a promotes the angiogenic switch. Biochim Biophys Acta Mol Basis Dis. 2018;1864(8):2633–43. doi: 10.1016/j.bbadis.2018.04.013. [DOI] [PubMed] [Google Scholar]
- 157.Bebawy M, Combes V, Lee E, Jaiswal R, Gong J, Bonhoure A. et al. Membrane microparticles mediate transfer of P-glycoprotein to drug sensitive cancer cells. Leukemia. 2009;23(9):1643–9. doi: 10.1038/leu.2009.76. [DOI] [PubMed] [Google Scholar]
- 158.Gong J, Jaiswal R, Dalla P, Luk F, Bebawy M. Microparticles in cancer: a review of recent developments and the potential for clinical application. Semin Cell Dev Biol. 2015;40:35–40. doi: 10.1016/j.semcdb.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 159.Gong J, Jaiswal R, Mathys JM, Combes V, Grau GE, Bebawy M. Microparticles and their emerging role in cancer multidrug resistance. Cancer Treat Rev. 2012;38(3):226–34. doi: 10.1016/j.ctrv.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 160.Jaiswal R, Raymond Grau GE, Bebawy M. Cellular communication via microparticles: role in transfer of multidrug resistance in cancer. Future Oncol. 2014;10(4):655–69. doi: 10.2217/fon.13.230. [DOI] [PubMed] [Google Scholar]
- 161.Boilard E. Platelet-derived nanomedicine targets cancer. Blood. 2017;130(5):561–2. doi: 10.1182/blood-2017-05-786327. [DOI] [PubMed] [Google Scholar]
- 162.Laffont B, Corduan A, Plé H, Duchez AC, Cloutier N, Boilard E. et al. Activated platelets can deliver mRNA regulatory Ago2•microRNA complexes to endothelial cells via microparticles. Blood. 2013;122(2):253–61. doi: 10.1182/blood-2013-03-492801. [DOI] [PubMed] [Google Scholar]
- 163.Laffont B, Corduan A, Rousseau M, Duchez AC, Lee CH, Boilard E. et al. Platelet microparticles reprogram macrophage gene expression and function. Thromb Haemost. 2016;115(2):311–23. doi: 10.1160/th15-05-0389. [DOI] [PubMed] [Google Scholar]
- 164.Tang M, Jiang L, Lin Y, Wu X, Wang K, He Q. et al. Platelet microparticle-mediated transfer of miR-939 to epithelial ovarian cancer cells promotes epithelial to mesenchymal transition. Oncotarget. 2017;8(57):97464–75. doi: 10.18632/oncotarget.22136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Baluk P, Hashizume H, McDonald DM. Cellular abnormalities of blood vessels as targets in cancer. Curr Opin Genet Dev. 2005;15(1):102–11. doi: 10.1016/j.gde.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 166.Hayon Y, Shai E, Varon D, Leker RR. The role of platelets and their microparticles in rehabilitation of ischemic brain tissue. CNS Neurol Disord Drug Targets. 2012;11(7):921–5. doi: 10.2174/1871527311201070921. [DOI] [PubMed] [Google Scholar]
- 167.Chistiakov DA, Orekhov AN, Bobryshev YV. Endothelial barrier and its abnormalities in cardiovascular disease. Front Physiol. 2015;6:365. doi: 10.3389/fphys.2015.00365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Opal SM, van der Poll T. Endothelial barrier dysfunction in septic shock. J Intern Med. 2015;277(3):277–93. doi: 10.1111/joim.12331. [DOI] [PubMed] [Google Scholar]
- 169.Meziani F, Delabranche X, Asfar P, Toti F. Bench-to-bedside review: circulating microparticles--a new player in sepsis? Crit Care. 2010;14(5):236. doi: 10.1186/cc9231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Shin ES, Sorenson CM, Sheibani N. Diabetes and retinal vascular dysfunction. J Ophthalmic Vis Res. 2014;9(3):362–73. doi: 10.4103/2008-322x.143378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Tetta C, Bruno S, Fonsato V, Deregibus MC, Camussi G. The role of microvesicles in tissue repair. Organogenesis. 2011;7(2):105–15. doi: 10.4161/org.7.2.15782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Brill A, Dashevsky O, Rivo J, Gozal Y, Varon D. Platelet-derived microparticles induce angiogenesis and stimulate post-ischemic revascularization. Cardiovasc Res. 2005;67(1):30–8. doi: 10.1016/j.cardiores.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 173.Mezouar S, Mege D, Darbousset R, Farge D, Debourdeau P, Dignat-George F. et al. Involvement of platelet-derived microparticles in tumor progression and thrombosis. Semin Oncol. 2014;41(3):346–58. doi: 10.1053/j.seminoncol.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 174.Mege D, Panicot-Dubois L, Ouaissi M, Robert S, Sielezneff I, Sastre B. et al. The origin and concentration of circulating microparticles differ according to cancer type and evolution: a prospective single-center study. Int J Cancer. 2016;138(4):939–48. doi: 10.1002/ijc.29837. [DOI] [PubMed] [Google Scholar]
- 175.Chaari M, Ayadi I, Rousseau A, Lefkou E, Van Dreden P, Sidibe F. et al. Impact of breast cancer stage, time from diagnosis and chemotherapy on plasma and cellular biomarkers of hypercoagulability. BMC Cancer. 2014;14:991. doi: 10.1186/1471-2407-14-991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Dymicka-Piekarska V, Gryko M, Lipska A, Korniluk A, Siergiejko E, Kemona H. Platelet-derived microparticles in patients with colorectal cancer. J Cancer Ther. 2012;3(6):898–901. doi: 10.4236/jct.2012.326115. [DOI] [Google Scholar]
- 177.Ren JG, Man QW, Zhang W, Li C, Xiong XP, Zhu JY. et al. Elevated level of circulating platelet-derived microparticles in oral cancer. J Dent Res. 2016;95(1):87–93. doi: 10.1177/0022034515592593. [DOI] [PubMed] [Google Scholar]
- 178.Zhang W, Qi J, Zhao S, Shen W, Dai L, Han W. et al. Clinical significance of circulating microparticles in Ph-myeloproliferative neoplasms. Oncol Lett. 2017;14(2):2531–6. doi: 10.3892/ol.2017.6459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Kim HK, Song KS, Park YS, Kang YH, Lee YJ, Lee KR. et al. Elevated levels of circulating platelet microparticles, VEGF, IL-6 and RANTES in patients with gastric cancer: possible role of a metastasis predictor. Eur J Cancer. 2003;39(2):184–91. doi: 10.1016/s0959-8049(02)00596-8. [DOI] [PubMed] [Google Scholar]
- 180.Stein BL, McMahon B, Weiss I, Kwaan HC. Tissue-factor bearing microparticles and thrombotic risk in the myeloproliferative neoplasms. Blood. 2012;120(21):1145. doi: 10.1182/blood.V120.21.1145.1145. [DOI] [Google Scholar]
- 181.Marin Oyarzún CP, Heller PG. Platelets as mediators of thromboinflammation in chronic myeloproliferative neoplasms. Front Immunol. 2019;10:1373. doi: 10.3389/fimmu.2019.01373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Trappenburg MC, van Schilfgaarde M, Bredewold EO, van Aalderen MC, Spronk HM, Ten Cate H. et al. Elevated numbers and altered subsets of procoagulant microparticles in breast cancer patients using endocrine therapy. Thromb Res. 2011;127(4):363–9. doi: 10.1016/j.thromres.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 183.Tesselaar ME, Osanto S. Risk of venous thromboembolism in lung cancer. Curr Opin Pulm Med. 2007;13(5):362–7. doi: 10.1097/MCP.0b013e328209413c. [DOI] [PubMed] [Google Scholar]
- 184.Helley D, Banu E, Bouziane A, Banu A, Scotte F, Fischer AM. et al. Platelet microparticles: a potential predictive factor of survival in hormone-refractory prostate cancer patients treated with docetaxel-based chemotherapy. Eur Urol. 2009;56(3):479–84. doi: 10.1016/j.eururo.2008.06.038. [DOI] [PubMed] [Google Scholar]
- 185.Dashevsky O, Varon D, Brill A. Platelet-derived microparticles promote invasiveness of prostate cancer cells via upregulation of MMP-2 production. Int J Cancer. 2009;124(8):1773–7. doi: 10.1002/ijc.24016. [DOI] [PubMed] [Google Scholar]
- 186.Hayon Y, Dashevsky O, Shai E, Brill A, Varon D, Leker RR. Platelet microparticles induce angiogenesis and neurogenesis after cerebral ischemia. Curr Neurovasc Res. 2012;9(3):185–92. doi: 10.2174/156720212801619018. [DOI] [PubMed] [Google Scholar]