Abstract
Major consequences of untreated severe mitral regurgitation (MR) includes heart failure, ventricular remodeling and pulmonary hypertension leading to significant morbidity and mortality. MitraClip is the most widely used device for treatment of severe MR. To overcome some of the shortcomings of MitraClip, novel devices like PASCAL mitral valve repair system are developed. We performed a single arm meta-analysis for patients with severe mitral regurgitation (MR) undergoing PASCAL mitral valve repair system. The results showed that 93.8% patients had reduction in MR grade, with an average operative time of 88 min and an average increase of 86.33 m in 6-min walk test.
Keywords: PASCAL mitral valve repair system, Mitral valve repair, Mitral regurgitation
1. Short communication
Left untreated, severe mitral regurgitation (MR) leads to sequel including heart failure, left ventricular remodeling and pulmonary hypertension.1 Despite the significant morbidity and mortality associated with untreated MR, there are a significant amount of patients not treated due to the perceived risk of surgery.2 For the high-risk surgical patient, the only Food and Drug administration (FDA) approved transcatheter repair system, the Mitraclip (Abbott Vascular, Santa Clara, California, USA), reduces MR via a mechanism based off the Alfieri stitch. Because of its inherent limitations, several novel transcatheter devices are in development to overcome the shortcomings of MitraClip; the PASCAL mitral valve repair system (Edwards LiveScience, Irvine, California, USA) is among them. In contrast to previous generation MitraClip devices, PASCAL allows for independent leaflet capture, and contains a nitinol spacer in between the clasping arms to reduce tension on the leaflets. Additionally, the PASCAL device offers a more user-friendly method for steering. The first-in-man study was published in 2017. Till date, less than 200 patients have been reported to have undergone mitral valve repair using the PASCAL system.
We searched PubMed, EMBASE, Web of Science and Google Scholar for original articles of patients undergoing PASCAL mitral valve repair system through September 1st, 2020. Search queries included “PASCAL mitral” and “mitral valve repair system”. We performed a single arm meta-analysis of included studies reporting mitral regurgitation grades at follow-up operated with PASCAL mitral valve repair system. Inverse variance method with empirical Bayes estimator of Tau2 was used to pool proportions.
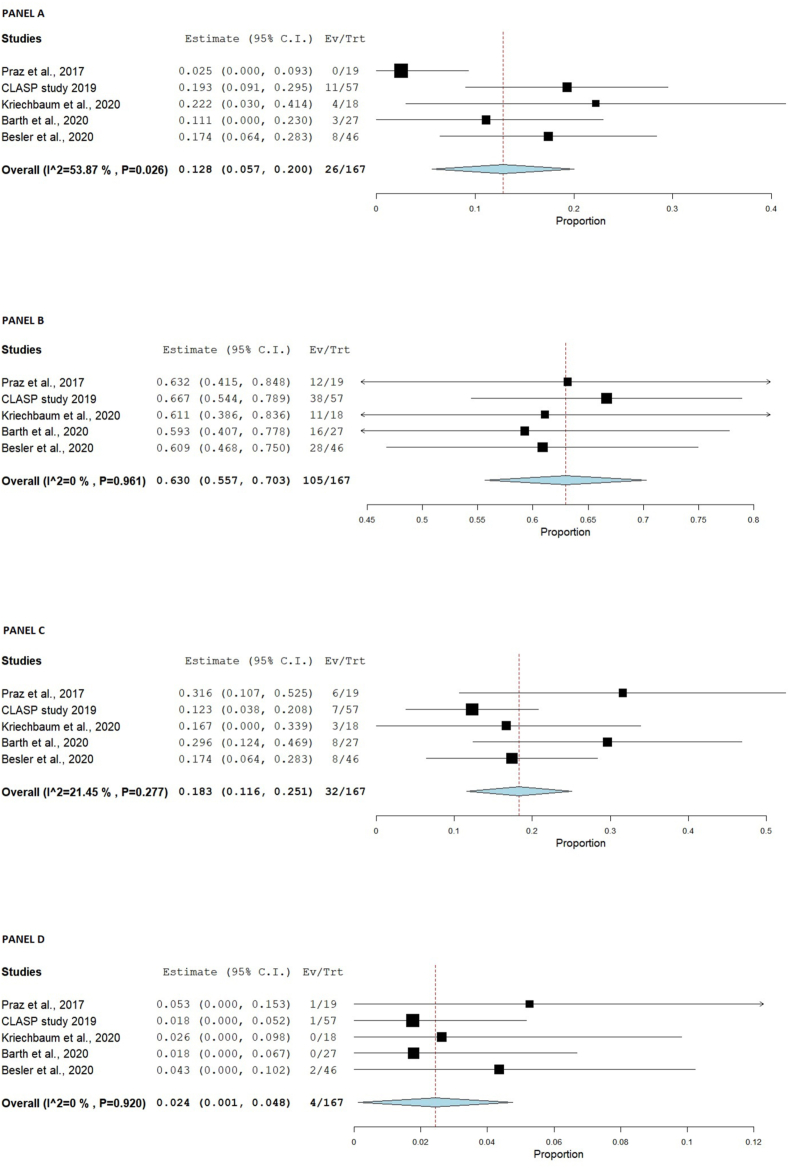
In total, 5 studies were included, comprising 184 patients.1, 2, 3, 4, 5 Baseline characteristics are presented in Table 1. The average age was 77.2 years, 62.2% of patients were males. 82% patients had hypertension, 27% had diabetes mellitus and 67.6% patients had atrial fibrillation. 45.3% patients had functional MR, 34.04% patients had degenerative MR and 20.7% patients had mixed etiology. All patients had grade III, or IV MR. 3 studies had 30 days follow-up, one study had 5 months follow up and one study had only post-procedural outcomes available. The average time for device implantation was 88 min. Mean increase in 6-min walk test on follow up was 86.33 m. 12.8% (CI 5.7%–20%; I2 = 54%) of patients at follow up had grade 0 MR, 63% (CI 55.7%–70.3%; I2 = 0%) patients had grade I MR, 18% (CI 11.6%–25.1%; I2 = 21%) had grade II MR, and 2.4% (CI 0.1 %–4.8%; I2 = 0%) patients had a grade III MR (Fig. 1). With respect to adverse outcome 4/134 (3%) of the patients had severe bleeding and 30 days all-cause mortality was seen in 9/166 (5.42%) of the patients.
Table 1.
Baseline characteristics of patients undergoing PASCAL mitral valve repair system for treatment of grade III/IV mitral regurgitation.
| Baseline Characteristics | |
|---|---|
| Age (years) | 77.2 (184) |
| Female | 74 (37.82%) |
| NYHA Class III/IV | 143 (77.71%) |
| Comorbidities | |
| Hypertension | 138/166 (80.72%) |
| Diabetes Mellitus | 45/166 (27.12%) |
| Pulmonary Hypertension | 8/62 (12.9%) |
| Aortic aneurysm | 6/62 (10%) |
| Cardiomyopathy (ischemic/nonischemic) | 63/93 (67.74%) |
| Previous MI | 40/166 (24.10%) |
| Stroke/cerebrovascular event | 50/134 (37.31%) |
| Aortic Valve Disease | 23/62 (37.7%) |
| Pulmonary Valve Disease | 17/62 (27.4%) |
| Tricuspid Valve Disease | 35/62 (56.5%) |
| Coronary artery disease | 48/103 (46.60%) |
| Peripheral vascular disease | 6/93 (6.45%) |
| Heart Failure | 36/62(58.1%) |
| Renal Disease | 32/85 (37.64%) |
| Chronic lung disease | 33/166 (19.90%) |
| History of cardiac surgery | 21/72 (29.20%) |
| Euro Score II | 8.03 (72) |
| Cadiac device (pacemaker/defibrillator) | 25/122 (20.50%) |
| Atrial Fibrillation | 124 (67.39%) |
| Medications | |
| Beta blockers | 102/122 (83.61%) |
| ACE-I/ARBs | 100/122 (81.97%) |
| Aldosterone antagonist | 65/91 (71.43%) |
| Loop diuretics | 111/122 (90.98%) |
| Lab Investigations | |
| eGFR | 56.33 (161) |
| proBNP | 2825 (91) |
| BNP | 535 (82) |
| MR Etiology | |
| Functional | 83/184 (45.11%) |
| Degenerative | 73/184 (39.70%) |
| Mixed | 27/184 (14.67%) |
| Outcome | |
| Time of implantation | 88 min |
| Severe bleeding | 4/134 (3%) |
| 30 days mortality (all cause) | 9/166 (5.42%) |
| Myocardial Infarction | 0 |
| NYHA Class I | 34/108 (31.48%) |
| NYHA Class II | 77/126 (61.11%) |
| Mean increase in 6 min walk distance | 88.33 m |
Fig. 1.
Forest plots: PANEL A: MR grade 0; PANEL B: MR grade 1; PANEL C: MR grade 2; PANEL D: MR grade 3.
In conclusion, PASCAL mitral valve repair system leads to reduction in MR grade and improved 6-min walk test distance without any adverse outcomes.
Source of research support or funding
None.
Declaration of competing interest
The authors declare they have no conflict of interest.
References
- 1.Lim D.S., Kar S., Spargias K. Transcatheter valve repair for patients with mitral regurgitation: 30-day results of the CLASP study. JACC Cardiovasc Interv. 2019;12(14):1369–1378. doi: 10.1016/j.jcin.2019.04.034. [DOI] [PubMed] [Google Scholar]
- 2.Kriechbaum S.D., Boeder N.F., Gaede L. Mitral valve leaflet repair with the new PASCAL system: early real-world data from a German multicentre experience. Clin Res Cardiol. 2020;109(5):549–559. doi: 10.1007/s00392-019-01538-3. [DOI] [PubMed] [Google Scholar]
- 3.Barth S., Hautmann M.B., Arvaniti E. Mid-term hemodynamic and functional results after transcatheter mitral valve leaflet repair with the new PASCAL device. Clin Res Cardiol. 2020 doi: 10.1007/s00392-020-01733-7. [DOI] [PubMed] [Google Scholar]
- 4.Praz F., Spargias K., Chrissoheris M. Compassionate use of the PASCAL transcatheter mitral valve repair system for patients with severe mitral regurgitation: a multicentre, prospective, observational, first-in-man study. Lancet. 2017;390(10096):773–780. doi: 10.1016/S0140-6736(17)31600-8. [DOI] [PubMed] [Google Scholar]
- 5.Besler C., Noack T., von Roeder M. Transcatheter edge-to-edge mitral valve repair with the PASCAL System: early results from a real-world series. EuroIntervention. 2020 doi: 10.4244/EIJ-D-20-00216. [DOI] [PubMed] [Google Scholar]