Abstract
Osteoarthritis (OA) is a degenerative and chronic joint disease characterized by clinical symptoms and distortion of joint tissues. It primarily damages joint cartilage, causing pain, swelling, and stiffness around the joint. It is the major cause of disability and pain. The prevalence of OA is expected to increase gradually with the aging population and increasing prevalence of obesity. Many potential therapeutic advances have been made in recent years due to the improved understanding of the underlying mechanisms, diagnosis, and management of OA. Embryonic stem cells and induced pluripotent stem cells differentiate into chondrocytes or mesenchymal stem cells (MSCs) and can be used as a source of injectable treatments in the OA joint cavity. MSCs are known to be the most studied cell therapy products in cell-based OA therapy owing to their ability to differentiate into chondrocytes and their immunomodulatory properties. They have the potential to improve cartilage recovery and ultimately restore healthy joints. However, despite currently available therapies and advances in research, unfulfilled medical needs persist for OA treatment. In this review, we focused on the contents of non-cellular and cellular therapies for OA, and briefly summarized the results of clinical trials for cell-based OA therapy to lay a solid application basis for clinical research.
Keywords: osteoarthritis, diagnosis, management, surgery, cell therapy, embryonic stem cells, induced pluripotent stem cells, mesenchymal stem cells
1. Introduction
Osteoarthritis (OA) is the most common chronic articular disease and remains one of the few chronic aging disorders with few effective treatments, none of which have been proven to delay disease progression. It can affect small, medium, and large joints, although in terms of a painful disease, the knee is most frequently affected in up to 10% of men and 13% of women aged above 60 years, with evidence of symptomatic OA of the knee in the United States [1].
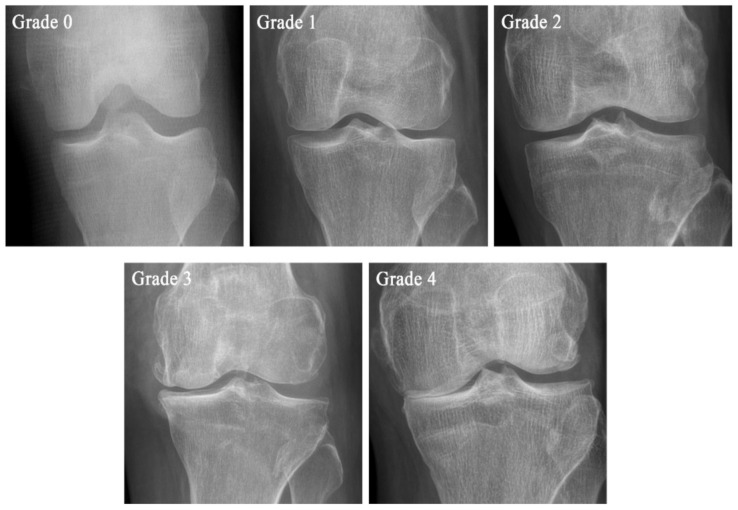
OA can be defined pathologically, radiographically, and clinically. The most common method for radiographic definition is the Kellgren–Lawrence (KL) radiographic grading system and atlas, which has been used for more than 40 years. This overall joint scoring system grades OA into five levels from 0 to 4, defining OA by the presence of a definite osteophyte (Grade ≥ 2), and more severe grades by the presumed successive appearance of joint space narrowing, sclerosis, cysts, and deformity [1,2]. However, all patients with radiographic OA do not have a clinical condition, and all patients with joint symptoms do not demonstrate radiographic OA [1]. Therefore, OA must be diagnosed using a variety of pathological, clinical, and radiological methods [3].
2. Osteoarthritis of the Knee
The knee is the largest synovial joint in humans and consists of bone structures (distal femur, proximal tibia, and patella); cartilage (meniscus and free cartilage); ligaments; infrapatellar fat pad; and synovium. The synovium is responsible for the production of synovial fluid that lubricates and nourishes the vascular cartilage. However, considering the frequent use and high stress on this joint, it is a frequent site of painful conditions, particularly OA [4,5]. Disease evaluation of OA is generally slow and can take years. Successively, the disease can also go through stages or show gradual evolution over time, making the severity and symptoms of the disease worse [6].
3. Mechanisms/Pathophysiology
The diarthrodial joint connects two adjacent bones, covered with a special articular cartilage layer, and wrapped in a synovial bursa [7]. The articular cartilage is composed of water (>70%) and organic extracellular matrix components, mainly type II collagen, aggrecan, or other proteoglycans [6]. Chondrocytes detect mechanical stress and changes in the pericellular matrix primarily through receptors on the components of the extracellular matrix. The change in response to mechanical or inflammatory stimulation results in the upregulation of aggrecanase and collagenase. Moreover, receptors on resting chondrocytes are protected from interacting with certain matrix components by the unique composition of the pericellular matrix. Type II collagen-containing networks in the interregional regions are generally not degraded as they are coated with proteoglycans [8].
The main cartilage matrix-degrading enzymes are zinc-dependent metalloproteinases (MMPs) belonging to the MMP and A Disintegrin and Metalloproteinase with Thrombospondin motifs (ADAMTS) families. MMPs include the collagenases MMP-1 and MMP-13 (highly efficient against type II collagen as a substrate), MMP-3 (a potent aggrecanase), and MMP activator [9].
The importance of proteoglycan depletion in cartilage erosion has been demonstrated in ADAMT5 (the primary aggrecanase) knockout mice protected from progression using a surgical OA model [10]. However, aggrecan depletion, by itself, does not drive OA progression, as suggested by studies wherein MMP13 knockout mice exhibited inhibition of cartilage erosion; however, it does not prevent aggrecan depletion [11]. When the collagen network begins to break down, irreversible cartilage breakdown proceeds [8]. Partly, overloading and inflammation leading to cartilage degradation can cause OA. Prostaglandin E2 is one of the major catabolic factors associated with OA, where MMP is crucial for cartilage degeneration. Thus, the mechanosensitive microsomal prostaglandin E synthase type 1 enzyme represents a potential therapeutic target in OA [12].
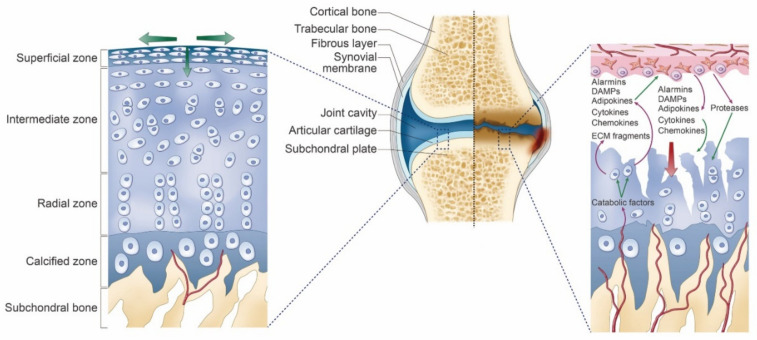
In OA, there is a gradual disappearance of cartilage associated with chondrocyte loss and phenotypic transformation, including cluster formation and activation of catabolic phenotypic and hypertrophic differentiation. Remodeling of subchondral bone occurs with the development of blood vessels located in structures (vascular channels) that contain osteoblasts and sensory nerves. Vascular channels should facilitate biochemical communication between the bone and cartilage. In response to multiple stimulations, chondrocytes modify the phenotype and express a subset of factors (such as cytokines, chemokines, alarmins, damage-associated molecular pattern, and adipokines). All these mediators act as paracrine factors, begin a vicious cycle of cartilage breakdown, reach the synovial fluid, and trigger an inflammatory process with the production of synovial macrophages and fibroblasts of the factor [8]. Vascular channels have sensory nerve terminations, and the associated innervation of articular cartilage may contribute to tibiofemoral pain in OA across a wide range of structural disease severities [13]. Figure 1 illustrates the associated mechanism [6,8].
Figure 1.
Mechanisms for the osteoarthritis of the knee. Healthy articular cartilage (Left)—Because of absence of vessels within cartilage, chondrocytes can live in a hypoxic environment. Hypoxia is important for chondrocyte function and survival. The main function of cartilage is the absorption and the removal of mechanical load, which is necessary to maintain cartilage homeostasis. Osteoarthritis articular cartilage (Right)—Development of vessels (called vascular channels) are supposed to facilitate biochemical communication between the bone and the cartilage (such as cytokines, chemokines, alarmins). It initiates a vicious cycle of cartilage degradation.
The infrapatellar fat pad (IFP) is in close contact with the synovial membrane, and due to the metabolic properties of adipose tissue, IFP may affect the functioning of the synovial membrane [14]. In a recent study, it was found that IFP in OA patients of the knee was more inflamed and vascularized compared to the IFP in anterior cruciate ligament reconstruction patients [15]. It has been recognized that IFP secretes adipocytokines and has more inflammation and fibrotic changes than control group [15]. All of these studies could support the new idea that the IFP and the synovial membrane could be considered a morpho-functional unit [14].
Cartilage is a highly specialized connective tissue, and its damage is the main feature of OA. The primary determinants of OA are namely, aging, genetic predisposition, metabolic syndrome, or trauma, and activation of the inflammatory pathways occurs in cartilage [16]. Chondrocytes form a vicious cycle leading to the progression of OA by producing inflammatory mediators that can lead to cartilage damage and changes in adjacent joint tissue. Therefore, the components of inflammatory pathways to discover disease-modifying OA drugs should be known [8].
4. Diagnosis
Although OA is an extremely common illness, its diagnosis may be difficult. Diagnostic criteria were developed for OA of the knee. The primary goal of the diagnostic criteria is to differentiate OA from other arthritis, such as rheumatoid arthritis and ankylosing spondylitis [6].
The American College of Rheumatology (ACR) classification criteria for OA of the knee were used widely [17]. One study demonstrated that crepitus is specific for patellofemoral joint OA rather than tibiofemoral joint OA, as suggested by the magnetic resonance imaging definition [18]. Another arthroscopy-based study reported an association between crepitus and cartilage pathology in both compartments of the knee [19].
Cartilage degeneration and other skeletal changes can be examined radiographically and quantified using the semi-quantitative grading scale known as the KL scale [20], Ahlbäck classification [21], and knee osteoarthritis grading system (KOGS) [22]. The original definitions of the KL scale, Ahlbäck classification, and KOGS are shown in Table 1. A KL grade picture is shown in Figure 2 [21].
Table 1.
Comparison of the original definitions of the Kellgren–Lawrence (KL) scale, Ahlbäck clasScheme 20.
| Grade | KL Scale | Ahlbäck Classification | KOGS |
|---|---|---|---|
| Grade 0 | No pathological features of osteoarthritis (OA) | ||
| Grade 1 | Suspicious narrowing of the joint space and possible osseous lip | Joint space narrowing, with or without subchondral sclerosis. Joint space narrowing is defined by this system as a joint space <3 mm, or less than half of the space in the other compartment, or less than half of the space of the homologous compartment of the other knee | An isolated medial, lateral tibiofemoral, or patella-femoral joint OA with ligament stability and two functionally intact compartments |
| Grade 2 | Clear bone tissue and possible stenosis of the joint space | Obliteration of the joint space | Deteriorating isolated lesion with ligament stability and a correctible coronal subluxation |
| Grade 3 | Moderate multiple bone tissue, clear narrowing of the joint space, slight sclerosis, and possible deformity of the ends of the bones | Bone defect/loss < 5 mm | Includes an isolated medial or lateral tibiofemoral OA and concomitant pathologies such as anterior cruciate ligament deficiency (3A) or grooving of patella-femoral joint or patellectomy (3B) |
| Grade 4 | Large bone tissue, marked narrowing of the joint space, severe sclerosis, and clear deformities of the ends of the bones | Bone defect/loss between 5 mm and 10 mm | Includes cases of bi-compartmental tibiofemoral OA without concomitant ligament instability (4A) and with ligament instability (4B) |
| Grade 5 | Bone defect/loss >10 mm, often with subluxation and arthritis of the other compartment |
Figure 2.
The example of the Kellgren–Lawrence (KL) scale. KL classification is the most widely used radiographic scale. The radiograph was recorded at St. Mary’s Hospital in Seoul.
5. Risk Factor
Previous knee trauma increases the risk of osteoarthritis of the knee by 3.86 times [23]. Old age, female, overweight and obesity, repetitive use of joints, bone density, muscle weakness, and joint relaxation all play an important role in the development of knee OA [23]. Also, frequent squatting is a risk factor for knee OA [23].
6. Current Point-of-Care Treatment
Conventional Management
Currently, various guidelines have been developed to standardize and recommend available treatments by academic and professional societies. Table 2 shows the available treatment options from the Osteoarthritis Research Society International (OARSI), ACR, and the American Academy of Orthopedic Surgeons (AAOS) publications [24,25,26].
Table 2.
Osteoarthritis of the knee management recommendations from the three societies.
| Treatment | OARSI | ACR | AAOS |
|---|---|---|---|
| Exercise (Land-based) | Appropriate | Strong recommendation | Strong recommendation |
| Exercise (Water-based) | Appropriate | Strong recommendation | Strong recommendation |
| Transcutaneous electrical nerve stimulation | Uncertain | Strong recommendation against use | Inconclusive |
| Cane (Walking stick) | Appropriate | Strong recommendation | |
| Weight control | Appropriate | Strong recommendation | Moderate recommendation |
| Chondroitin or Glucosamine | Not appropriate for disease modification, Uncertain (Sx relief) | Strong recommendation against use | Recommendation against use |
| Acetaminophen | Without comorbidities: appropriate | Conditional recommendation | Inconclusive |
| Duloxetine | Appropriate | Conditional recommendation | No recommendation |
| Oral NSAIDs | Without comorbidities: appropriate; With comorbidities: Uncertain |
Strong recommendation | Strong recommendation |
| Topical NSAIDs | Appropriate | Conditional recommendation against use | Strong recommendation |
| Opioids | Uncertain | No recommendation | Recommended (only tramadol) |
| Intra-articular corticosteroids | Appropriate | Strong recommendation | Inconclusive |
| Intra-articular viscosupplementation | Uncertain | Conditional recommendation against use | Recommendation against use |
OARSI: Osteoarthritis Research Society International; ACR: American College of Rheumatology; AAOS: American Academy of Orthopedic Surgeons; NSAIDs: non-steroidal anti-inflammatory drugs.
7. Interventional Management
Multiple substances that are delivered through intra-articular (IA) injections have been explored. The idea is that local treatments (IA injection) will have less systemic side effects and placing the drug inside the joint will have a more direct effect. Studies have shown that IA therapy is more effective than oral non-steroidal anti-inflammatory drugs and other systemic pharmacological treatments; however, it has also revealed that some of its benefits may be secondary to the IA placebo effect [27,28].
Also, injectable drug delivery alone, including new treatments, may not provide significant benefits for OA treatment. Because IA injections cannot target the complexity of the pathological mechanisms [29]. It means that relatively new concept is the multimodal approach to the IA injections, which is needed to significant effect on the entire knee.
7.1. Intra-Articular Corticosteroid Injection
In the knee joint of OA, IA corticosteroid injections are usually conditionally recommended over other forms of IA injection. There are few one-to-one comparisons; however, the evidence for the efficacy of glucocorticoid injections is significantly higher than that of other drugs [25]. Corticoids act directly on nuclear receptors, disrupting the inflammatory cascade at several levels, causing immunosuppressive and anti-inflammatory effects. They are part of the pain relief mechanism and reduce the action and production of interleukin-1, prostaglandins, leukotriene, MMP9, and MMP-11, which are believed to increase joint mobility in the knee OA [4]. The clinical anti-inflammatory effects of these actions include decrease in erythema, heat, swelling, and tenderness of the inflammatory joints, and increases in relative viscosity with an increase in hyaluronic acid (HA) concentration [28]. Therefore, IA corticosteroid injections reduce acute pain episodes and increase joint mobility, particularly when there is evidence of inflammation and joint effusion during OA redness [30].
The current Food and Drug Administration approved immediate release corticosteroids for IA usages namely, methylprednisolone acetate, triamcinolone acetate, triamcinolone hexacetonide, betamethasone acetate, betamethasone sodium phosphate, and dexamethasone [28].
In summary, research evidence shows that IA corticosteroid injections provide a short-term reduction in OA pain and act as an adjunct to key therapy for moderate to severe pain relief in patients with OA [31].
7.2. Intra-Articular Hyaluronic Acid Injection (Viscosupplementation)
HA, a viscoelastic mucopolysaccharide component of synovial fluid, is produced from harvested rooster combs or through in vitro bacterial fermentation [32]. HA is a high-molecular-weight glycosaminoglycan that consists of a repeating sequence of disaccharide units composed of N-acetyl glucosamine and glucuronic acid [33]. Viscous supplementation through an IA injection of HA is aimed at restoring the beneficial environment present in non-arthritic joints. Additionally, the safety profile of such injections for painful knee OA is well established [32].
Previous studies demonstrated obvious benefits of intra-articular HA injection; however, according to the 2019 ACR/European League Against Rheumatism study, the benefit was restricted to studies with a higher risk of bias compared to saline injection. Therefore, in recent years, HA injection has been conditionally recommended to control joint symptoms when glucocorticoid injection or other interventions fail [25].
7.3. Intra-Articular Platelet-Rich Plasma Injection
The IA platelet-rich plasma (PRP) injection has emerged as a good treatment for knee OA. Several randomized controlled trials have been shown that PRP is a safe and effective treatment. At this time, IA PRP is not a standard treatment of the knee OA, but it is similar in efficacy to HA, and appears to be more effective than HA in young, active patients with low-grade OA [34].
8. Surgery
The goals of surgery for patients with OA are to reduce pain, minimize disability, and improve quality of life. Treatment should be individualized according to the functional condition of the patients, severity of the disease, and nature of the underlying disease. Surgical intervention for patients with OA is generally performed when a less invasive treatment is unsuccessful.
8.1. Total Knee Replacement Surgery (Total Knee Arthroplasty)
Total knee replacement (TKR) surgery involves excising the damaged ends of the tibia and femur and capping both using a prosthesis. Both prostheses comprise durable plastic. These new surfaces move smoothly with each other. Partial recovery takes 6 weeks and complete recovery takes up to 1 year [35].
A randomized, controlled trial of TKR demonstrated that non-surgical treatment after TKR is superior to non-surgical treatment alone in providing pain relief in patients with moderate to severe OA of the knee and improving function and quality of life after 1 year. However, clinically relevant improvements were seen in both groups, and patients who received TKR had more severe side effects [36].
In addition, IFP resection during TKR is the subject of an ongoing debate without clear consensus [37].
8.2. Partial Knee Replacement Surgery (Unicompartmental Knee Arthroplasty)
Unicompartmental knee arthroplasty is an alternative to TKR for patients whose disease is limited to a single area of the knee, particularly the isolated tibiofemoral compartment (medial or lateral). As partial knee replacement is performed using smaller incisions, patients can generally be discharged earlier than those who undergo TKR and can return sooner to normal activities, including work and sports [38].
8.3. Knee Osteotomy (High Tibial Osteotomy or Femoral Osteotomy)
High tibial osteotomy is a surgery to realign the knee joint. It is more important for the treatment of cartilage damage or OA of the medial compartment with varus deformity. High tibial osteotomy creates a postoperative valgus limb alignment by lateral movement of the load-bearing axis of the lower limb [39].
8.4. Knee Arthroscopy
Knee arthroscopy is most commonly performed to treat OA or meniscus problems. An arthroscopy requires a small incision in the skin with the insertion of a camera on a stick. Another incision is needed to insert other instruments and treat the disease [40].
8.5. Knee Cartilage Repair and Cartilage Restoration
Many surgical techniques have been developed to address focal cartilage defects. Cartilage surgery strategies include palliative (chondroplasty and debris removal); repair (perforation and microfracture); or restoration (auto chondral cell transplant, osteochondral autograft, and bone cartilage allograft) [41].
9. Cellular & Experimental Therapy
9.1. Cellular Therapy
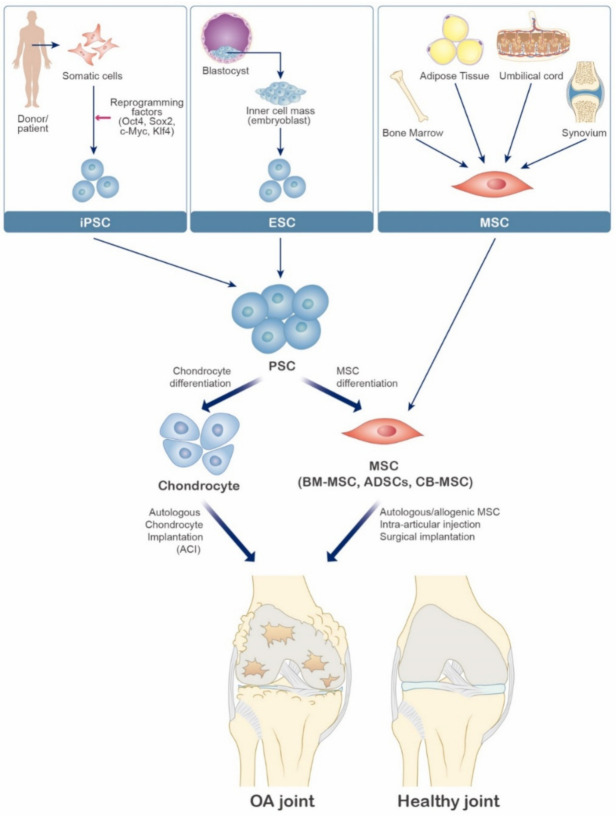
Several cell therapeutic attempts have been made to regenerate damaged joint cartilage. Autologous chondrocyte implantation (ACI) has been proposed as a surgical technique for partial cartilage lesions [42]. ACI is known as the most traditional cell-based therapy that has evolved with a high success rate. However, since it is limited to the damaged cartilage area, it is difficult to use in general OA treatment [43,44,45]. Mechanical, biological, and chemical scaffold-based approaches have also been developed to allow autologous chondrocytes to fill the cartilage lesions. With the scaffold, chondrocytes are less prone to dedifferentiation, and more favorable cartilage can be produced [46]. However, the limited number of primary chondrocytes has shown therapeutic limitations. Consequently, stem cell-based therapies have been developed to compensate for these shortcomings (Figure 3). Stem cells are undifferentiated cells capable of differentiating into various specialized cells such as bone cells, chondrocytes, and adipocytes [47]. Additionally, stem cells are characterized by the ability to release cytokine secretions that can downregulate several important inflammations [48]. Three other types of stem cells, embryonic stem cells (ESCs), induced pluripotent stem cells (iPSCs), and mesenchymal stem cells (MSCs) are also potential candidates for cartilage regeneration for the OA treatment. Both ESCs and iPSCs have intrinsically pluripotent features and can differentiate into other cell types, including chondrocytes. Several studies have shown that chondrocytes can be differentiated using ESCs and iPSCs [49,50]. However, there is a risk that both stem cells can form teratoma and immunogenicity [51].
Figure 3.
Schematic diagram of various cell-based therapy for osteoarthritis. Embryonic stem cells (ESC), induced pluripotent stem cells (iPSC), and mesenchymal stem cells (MSC) are potential candidates for cartilage regeneration for the OA treatment. MSC can be isolated from bone marrow, adipose tissue, umbilical cord, synovium. Pluripotent stem cells (PSC), including ESC and iPSC, are considered sources for the derivation of chondrocytes and MSC.
Mesenchymal stem cells (MSCs) are not as pluripotent as ESCs and iPSCs; however, may be considered the most ideal among the various types of stem cells for OA treatment [52]. MSCs have advantages that can be obtained in various ways such as bone marrow [53], adipose tissue [54], and umbilical cord [55]. As MSCs express and secrete various growth factors and cytokines and have anti-inflammatory activity, numerous studies have been conducted for the treatment of OA [56,57,58]. In addition to these sources of stem cells, infrapatellar fat pad (IFP) have been recently considered as a source of stem cells for cartilage regeneration in OA due to their increased chondrogenic capacity [59,60]. However, IFP-derived stem cells seem to be primed by the pathological environment and exert a protective role in the inflammatory environment [60]. Thus, further research is needed to clarify this point.
Human ESCs can be used as a raw material for cell therapy for the treatment of OA. It has been demonstrated that MSCs differentiated from ESCs have similar efficacy to those extracted from somatic tissues, such as bone marrow, and can treat various autoimmune and inflammatory diseases [61,62,63]. ESC-derived MSCs are more advantageous for use as a cell therapy than natural MSCs extracted from bone marrow tissues (Table 3). ESCs can be produced on a large scale from human ESC raw materials that can be supplied endlessly.
Table 3.
Summary of advantages and disadvantages of ESCs, iPSCs, and MSCs.
| Advantages | Disadvantages | |
|---|---|---|
| Embryonic stem cells (ESCs) | Unlimited self-renewal | Ethical concerns |
| Unlimited proliferation | Tumorigenic potential | |
| Pluripotent | Difficulty in vitro work | |
| Potentially unlimited supply | Difficulty in controlling differentiation | |
| Induced pluripotent stem cells (iPSCs) | Autologous origin | Security |
| Extensive sources | Tumorigenic potential | |
| Unlimited self-renewal | Inefficiency | |
| Unlimited proliferation | Instability | |
| Pluripotent | Unclear mechanism | |
| No ethical issues | Difficulty in controlling differentiation | |
| Mesenchymal stem cells (MSCs) | High chondrogenic potential | A limited number of cells |
| Good expansion ability | More affected by donor age | |
| Easily accessible, reliable for isolation | Donor site pain |
Additionally, human ESCs may be a potential treatment option as a source of consistently homogeneous cells with high chondrogenic ability [49]. Sources of expandable cartilage precursors may have broad potential to advance articular cartilage therapy and disease modeling and act as therapeutics that can promote cartilage regeneration or prevent degeneration [64,65]. Although several studies have attempted to treat OA using specialized cells derived from human ESCs [66,67,68], clinical studies on effective human ESC-derived cell therapeutics in patients with OA are still needed.
9.2. Induced Pluripotent Stem Cells for Osteoarthritis
The general differences in ESCs and iPSCs and the use of human PSCs for disease modeling have been extensively discussed in the literature [69,70,71]. The development of iPSCs opens up new horizons for the development of new research tools for OA that do not yet have a clear treatment [72]. The iPSCs, reprogrammed from somatic cells [73,74], provided a new opportunity to create a virtually unlimited number of patient-specific stem cells for OA for drug discovery. Thus, chondrogenic differentiation of iPSCs from patients with symptoms of OA may enable many studies of cartilage tissue [42,50,75]. Clinical studies using iPSCs in cell therapy for OA are still in the basic stage with an understanding of the cartilage regeneration mechanisms. iPSCs have proliferative and differentiation capabilities similar to those of other stem cells; however, do not have immune rejection reactions and ethical problems [76]. Additionally, studies on a new method of producing iPSCs without the use of viral vectors have been actively conducted in recent years to reduce the risk of tumorigenicity [77,78]. Nevertheless, there is still limited data on the effects of iPSCs on cartilage formation and OA, and further studies are needed (Table 4).
Table 4.
Detailed clinical studies of ESCs, iPSCs, and MSCs in OA.
| Cell Source | No. of Participants | Mean Follow-Up (Months) | Delivery Methods | Clinical Outcome | Reference/NCT |
|---|---|---|---|---|---|
| ESCs | N/A | N/A | N/A | N/A | N/A |
| iPSCs | N/A | N/A | N/A | N/A | N/A |
| BMSCs | 45 | 75 | Two-stage surgical approaches | No risk of serious complications | [91] N/A |
| BMSCs | 4 | 12 | IA injection | Improved pain, walking, and stairs climbing | [92] 00550524 |
| BMSCs | 56 | 24 | IA injection | Better clinical outcomes and MRI in MSCs group | [93] N/A |
| BMSCs | 12 | 12 | IA injection | Improvement of cartilage quality on MRI | [94,95] 03956719 |
| BMSCs | 3 | 60 | IA injection | Better than the baseline level | [96] 00550524 |
| AMSCs (ASF) | 18 | 6 | IA injection | Better clinical outcomes | [97] 01300598 |
| AMSCs (ASF) | 100 | 26 | IA injection | Improved pain VAS scores | [98] N/A |
| AMSCs (GSF) | 40 | 29 | IA injection and surgical implantation | Improved clinical outcomes | [99] N/A |
| AMSCs (ASF) | 18 | 6 | IA injection | Improved clinical outcomes | [100] 01585857 |
| AMSCs (ASF) | 24 | 6 | IA injection | Improved clinical outcomes | [101] 02658344 |
ESCs; embryonic stem cells, iPSCs; induced pluripotent stem cells, BMSCs; bone-marrow-derived mesenchymal stem cells, AMSCs; adipose-derived mesenchymal stem cells, ASF; abdominal subcutaneous fat, GSF; gluteal subcutaneous fat, IA injection; intra-articular injection, MRI; magnetic resonance imaging, VAS; visual analog scale, NCT; The national clinical trial number, N/A; Not Assigned.
9.3. Mesenchymal Stem Cells for Osteoarthritis
MSCs are pluripotent progenitor cells derived from a population of adult stem cells that can be isolated from numerous tissues, including bone marrow, peripheral blood, adipose tissue, synovium, placenta, and umbilical cord [79,80]. Human MSCs are defined as cells that adhere to plastics; are positive for CD105, CD73 cell surface markers; negative for CD45, CD34 cell surface markers; and differentiate into osteoblasts, chondrocytes, and adipocytes [81]. Additionally, MSCs have unique immunomodulatory properties and can reduce inflammation and support other cells, enhancing angiogenesis, cell survival, and differentiation [82,83].
The primary isolated stromal cell represents the best option for OA treatment [84]. Bone marrow-derived stromal cells are the most common clinical source of MSC [85,86]. Although the main source has been on the use of bone marrow-derived stromal cells, some researchers have chosen to use adipose tissue-derived stromal cells as an alternative cell line [87,88]. These are harvested from bone marrow concentrate containing hematopoietic stem cells, endothelial progenitor cells, and related cytokines and growth factors [89]. Currently, translational medical research targeting MSCs for OA in the clinical trial database is promising. Clinical trials using MSCs in knee OA are actively underway. However, careful evaluation of clinical outcome data is necessary. The results appear to focus primarily on safety and efficacy [90]. Several studies have reported clinical trials for IA injection of MSCs in patients with OAs (Table 4) [91,92,93,94,95,96,97,98,99,100,101].
It has been suggested that the secretion of trophic factors, where exosomes play an important role, contributes to the MSC-based therapeutic mechanism of OA [102,103]. The paracrine secretion of MSC-derived exosomes may play a role in the repair of joint tissue as well as MSC-based treatments for other disorders. Recent studies have shown that MSC-derived exosomes may inhibit OA development and have summarized findings on exosomes derived from various MSCs and their effectiveness in OA therapy [104,105].
10. Noncellular Therapy
Gene Therapy
Gene therapy with genes encoding cartilage growth factor and anti-inflammatory cytokines is of interest in treating OA. Gene transfer was conducted in two ways: (1) In vivo injection/intravenous administration into the joint; (2) Ex vivo exposition/cell harvesting from the patient to the vector, and returning the modified cells to the joint [106].
In 2017, in vitro TGF-β1 gene therapy using retrovirus was approved for allogeneic chondrocytes [107]. In 2018, Kim et al. reported the clinical efficacy of TissueGene-C (TG-C), a cell and gene therapy for human knee OA consisting of non-transfected and transduced chondrocytes transduced using retrovirus to overexpress TGF-β1. They concluded that TG-C was associated with a statistically significant improvement in function and pain in patients with knee OA [108].
11. Conclusions
OA is the most common chronic joint disease, associated with obesity, aging, and socioeconomic impact. The mechanism works complex, local and systemic factors modulate clinical and structural representation, sometimes resulting in a common end-course of joint destruction. Treatment goals are to relieve symptoms and improve quality of life. Conventional management, surgery, and experimental therapy are summarized above.
Author Contributions
All authors were involved in drafting the manuscript or revising it critically for important intellectual content, and all authors approved the final version to be published. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by a grant from the Korea Healthcare Technology R&D project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (HI20C0495). This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 2020R1A2C3004123).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhang Y., Jordan J.M. Epidemiology of osteoarthritis. Clin. Geriatr. Med. 2010;26:355–369. doi: 10.1016/j.cger.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kellgren J.H., Jeffrey M.R., Ball J. The Epidemiology of Chronic Rheumatism: A Symposium. Blackwell Scientific Publications; Oxford, UK: 1963. [Google Scholar]
- 3.Hannan M.T., Felson D.T., Pincus T. Analysis of the discordance between radiographic changes and knee pain in osteoarthritis of the knee. J. Rheumatol. 2000;27:1513–1517. [PubMed] [Google Scholar]
- 4.Mora J.C., Przkora R., Cruz-Almeida Y. Knee osteoarthritis: Pathophysiology and current treatment modalities. J. Pain Res. 2018;11:2189–2196. doi: 10.2147/JPR.S154002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rubin B.R. Management of osteoarthritic knee pain. J. Am. Osteopath. Assoc. 2005;105:S23–S28. [PubMed] [Google Scholar]
- 6.Martel-Pelletier J., Barr A.J., Cicuttini F.M., Conaghan P.G., Cooper C., Goldring M.B., Goldring S.R., Jones G., Teichtahl A.J., Pelletier J.P. Osteoarthritis. Nat. Rev. Dis. Primers. 2016;2:16072. doi: 10.1038/nrdp.2016.72. [DOI] [PubMed] [Google Scholar]
- 7.Netter F.H., Hansen J.T. Atlas of Human Anatomy. 3rd ed. Icon Learning Systems; Teterboro, NJ, USA: 2003. [Google Scholar]
- 8.Houard X., Goldring M.B., Berenbaum F. Homeostatic mechanisms in articular cartilage and role of inflammation in osteoarthritis. Curr. Rheumatol. Rep. 2013;15:375. doi: 10.1007/s11926-013-0375-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Troeberg L., Nagase H. Proteases involved in cartilage matrix degradation in osteoarthritis. Biochim. Biophys. Acta. 2012;1824:133–145. doi: 10.1016/j.bbapap.2011.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glasson S.S., Askew R., Sheppard B., Carito B., Blanchet T., Ma H.L., Flannery C.R., Peluso D., Kanki K., Yang Z., et al. Deletion of active ADAMTS5 prevents cartilage degradation in a murine model of osteoarthritis. Nature. 2005;434:644–648. doi: 10.1038/nature03369. [DOI] [PubMed] [Google Scholar]
- 11.Little C.B., Barai A., Burkhardt D., Smith S.M., Fosang A.J., Werb Z., Shah M., Thompson E.W. Matrix metalloproteinase 13-deficient mice are resistant to osteoarthritic cartilage erosion but not chondrocyte hypertrophy or osteophyte development. Arthritis Rheum. 2009;60:3723–3733. doi: 10.1002/art.25002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gosset M., Berenbaum F., Levy A., Pigenet A., Thirion S., Cavadias S., Jacques C. Mechanical stress and prostaglandin E2 synthesis in cartilage. Biorheology. 2008;45:301–320. doi: 10.3233/BIR-2008-0494. [DOI] [PubMed] [Google Scholar]
- 13.Suri S., Gill S.E., Massena de Camin S., Wilson D., McWilliams D.F., Walsh D.A. Neurovascular invasion at the osteochondral junction and in osteophytes in osteoarthritis. Ann. Rheum. Dis. 2007;66:1423–1428. doi: 10.1136/ard.2006.063354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Macchi V., Stocco E., Stecco C., Belluzzi E., Favero M., Porzionato A., De Caro R. The infrapatellar fat pad and the synovial membrane: An anatomo-functional unit. J. Anat. 2018;233:146–154. doi: 10.1111/joa.12820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Belluzzi E., Macchi V., Fontanella C.G., Carniel E.L., Olivotto E., Filardo G., Sarasin G., Porzionato A., Granzotto M., Pozzuoli A., et al. Infrapatellar Fat Pad Gene Expression and Protein Production in Patients with and without Osteoarthritis. Int. J. Mol. Sci. 2020;21:6016. doi: 10.3390/ijms21176016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim H.A., Cho M.L., Choi H.Y., Yoon C.S., Jhun J.Y., Oh H.J., Kim H.Y. The catabolic pathway mediated by Toll-like receptors in human osteoarthritic chondrocytes. Arthritis Rheumatol. 2006;54:2152–2163. doi: 10.1002/art.21951. [DOI] [PubMed] [Google Scholar]
- 17.Wu C.W., Morrell M.R., Heinze E., Concoff A.L., Wollaston S.J., Arnold E.L., Singh R., Charles C., Skovrun M.L., FitzGerald J.D., et al. Validation of American College of Rheumatology classification criteria for knee osteoarthritis using arthroscopically defined cartilage damage scores. Semin. Arthritis Rheum. 2005;35:197–201. doi: 10.1016/j.semarthrit.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 18.Schiphof D., van Middelkoop M., de Klerk B.M., Oei E.H., Hofman A., Koes B.W., Weinans H., Bierma-Zeinstra S.M. Crepitus is a first indication of patellofemoral osteoarthritis (and not of tibiofemoral osteoarthritis) Osteoarthr. Cartil. 2014;22:631–638. doi: 10.1016/j.joca.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 19.Ike R., O’Rourke K.S. Compartment-directed physical examination of the knee can predict articular cartilage abnormalities disclosed by needle arthroscopy. Arthritis Rheumatol. 1995;38:917–925. doi: 10.1002/art.1780380707. [DOI] [PubMed] [Google Scholar]
- 20.Kohn M.D., Sassoon A.A., Fernando N.D. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin. Orthop. Relat. Res. 2016;474:1886–1893. doi: 10.1007/s11999-016-4732-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hernandez-Vaquero D., Fernandez-Carreira J.M. Relationship between radiological grading and clinical status in knee osteoarthritis. A multicentric study. BMC Musculoskelet Disord. 2012;13:194. doi: 10.1186/1471-2474-13-194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oosthuizen C.R., Takahashi T., Rogan M., Snyckers C.H., Vermaak D.P., Jones G.G., Porteous A., Maposa I., Pandit H. The Knee Osteoarthritis Grading System for Arthroplasty. J. Arthroplast. 2019;34:450–455. doi: 10.1016/j.arth.2018.11.011. [DOI] [PubMed] [Google Scholar]
- 23.Heidari B. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Casp. J. Intern. Med. 2011;2:205–212. [PMC free article] [PubMed] [Google Scholar]
- 24.McAlindon T.E., Bannuru R.R., Sullivan M.C., Arden N.K., Berenbaum F., Bierma-Zeinstra S.M., Hawker G.A., Henrotin Y., Hunter D.J., Kawaguchi H., et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthr. Cartil. 2014;22:363–388. doi: 10.1016/j.joca.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 25.Kolasinski S.L., Neogi T., Hochberg M.C., Oatis C., Guyatt G., Block J., Callahan L., Copenhaver C., Dodge C., Felson D., et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheumatol. 2020;72:220–233. doi: 10.1002/art.41142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jevsevar D.S., Brown G.A., Jones D.L., Matzkin E.G., Manner P.A., Mooar P., Schousboe J.T., Stovitz S., Sanders J.O., Bozic K.J., et al. The American Academy of Orthopaedic Surgeons evidence-based guideline on: Treatment of osteoarthritis of the knee, 2nd edition. J. Bone Jt. Surg. Am. 2013;95:1885–1886. doi: 10.2106/00004623-201310160-00010. [DOI] [PubMed] [Google Scholar]
- 27.Bannuru R.R., Schmid C.H., Kent D.M., Vaysbrot E.E., Wong J.B., McAlindon T.E. Comparative effectiveness of pharmacologic interventions for knee osteoarthritis: A systematic review and network meta-analysis. Ann. Intern. Med. 2015;162:46–54. doi: 10.7326/M14-1231. [DOI] [PubMed] [Google Scholar]
- 28.Ayhan E., Kesmezacar H., Akgun I. Intraarticular injections (corticosteroid, hyaluronic acid, platelet rich plasma) for the knee osteoarthritis. World J. Orthop. 2014;5:351–361. doi: 10.5312/wjo.v5.i3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Georgiev T. Multimodal approach to intraarticular drug delivery in knee osteoarthritis. Rheumatol. Int. 2020;40:1763–1769. doi: 10.1007/s00296-020-04681-7. [DOI] [PubMed] [Google Scholar]
- 30.Rozental T.D., Sculco T.P. Intra-articular corticosteroids: An updated overview. Am. J. Orthop. 2000;29:18–23. [PubMed] [Google Scholar]
- 31.Osteoarthritis: National Clinical Guideline for Care and Management in Adults, London. [(accessed on 3 March 2021)];2008 Available online: https://www.ncbi.nlm.nih.gov/books/NBK48984/ [PubMed]
- 32.McArthur B.A., Dy C.J., Fabricant P.D., Valle A.G. Long term safety, efficacy, and patient acceptability of hyaluronic acid injection in patients with painful osteoarthritis of the knee. Patient Prefer. Adherence. 2012;6:905–910. doi: 10.2147/PPA.S27783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Strauss E.J., Hart J.A., Miller M.D., Altman R.D., Rosen J.E. Hyaluronic acid viscosupplementation and osteoarthritis: Current uses and future directions. Am. J. Sports Med. 2009;37:1636–1644. doi: 10.1177/0363546508326984. [DOI] [PubMed] [Google Scholar]
- 34.Pourcho A.M., Smith J., Wisniewski S.J., Sellon J.L. Intraarticular platelet-rich plasma injection in the treatment of knee osteoarthritis: Review and recommendations. Am. J. Phys. Med. Rehabil. 2014;93:S108–S121. doi: 10.1097/PHM.0000000000000115. [DOI] [PubMed] [Google Scholar]
- 35.Leopold S.S. Minimally invasive total knee arthroplasty for osteoarthritis. N. Engl. J. Med. 2009;360:1749–1758. doi: 10.1056/NEJMct0806027. [DOI] [PubMed] [Google Scholar]
- 36.Skou S.T., Roos E.M., Laursen M.B., Rathleff M.S., Arendt-Nielsen L., Simonsen O., Rasmussen S. A Randomized, Controlled Trial of Total Knee Replacement. N. Engl. J. Med. 2015;373:1597–1606. doi: 10.1056/NEJMoa1505467. [DOI] [PubMed] [Google Scholar]
- 37.Sun C., Zhang X., Lee W.G., Tu Y., Li H., Cai X., Yang H. Infrapatellar fat pad resection or preservation during total knee arthroplasty: A meta-analysis of randomized controlled trials. J. Orthop. Surg. Res. 2020;15:297. doi: 10.1186/s13018-020-01823-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rodriguez-Merchan E.C., Gomez-Cardero P. Unicompartmental knee arthroplasty: Current indications, technical issues and results. Efort Open Rev. 2018;3:363–373. doi: 10.1302/2058-5241.3.170048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu X., Chen Z., Gao Y., Zhang J., Jin Z. High Tibial Osteotomy: Review of Techniques and Biomechanics. J. Healthc. Eng. 2019;2019:8363128. doi: 10.1155/2019/8363128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chua M.J., Hart A.J., Mittal R., Harris I.A., Xuan W., Naylor J.M. Early mobilisation after total hip or knee arthroplasty: A multicentre prospective observational study. PLoS ONE. 2017;12:e0179820. doi: 10.1371/journal.pone.0179820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Richter D.L., Schenck R.C., Jr., Wascher D.C., Treme G. Knee Articular Cartilage Repair and Restoration Techniques: A Review of the Literature. Sports Health. 2016;8:153–160. doi: 10.1177/1941738115611350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nam Y., Rim Y.A., Lee J., Ju J.H. Current Therapeutic Strategies for Stem Cell-Based Cartilage Regeneration. Stem Cells Int. 2018;2018:8490489. doi: 10.1155/2018/8490489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nazempour A., Van Wie B.J. Chondrocytes, Mesenchymal Stem Cells, and Their Combination in Articular Cartilage Regenerative Medicine. Ann. Biomed. Eng. 2016;44:1325–1354. doi: 10.1007/s10439-016-1575-9. [DOI] [PubMed] [Google Scholar]
- 44.Mobasheri A., Kalamegam G., Musumeci G., Batt M.E. Chondrocyte and mesenchymal stem cell-based therapies for cartilage repair in osteoarthritis and related orthopaedic conditions. Maturitas. 2014;78:188–198. doi: 10.1016/j.maturitas.2014.04.017. [DOI] [PubMed] [Google Scholar]
- 45.Viste A., Piperno M., Desmarchelier R., Grosclaude S., Moyen B., Fessy M.H. Autologous chondrocyte implantation for traumatic full-thickness cartilage defects of the knee in 14 patients: 6-year functional outcomes. Orthop. Traumatol. Surg. Res. 2012;98:737–743. doi: 10.1016/j.otsr.2012.04.019. [DOI] [PubMed] [Google Scholar]
- 46.Caron M.M., Emans P.J., Coolsen M.M., Voss L., Surtel D.A., Cremers A., van Rhijn L.W., Welting T.J. Redifferentiation of dedifferentiated human articular chondrocytes: Comparison of 2D and 3D cultures. Osteoarthr. Cartil. 2012;20:1170–1178. doi: 10.1016/j.joca.2012.06.016. [DOI] [PubMed] [Google Scholar]
- 47.Zakrzewski W., Dobrzynski M., Szymonowicz M., Rybak Z. Stem cells: Past, present, and future. Stem Cell Res. Ther. 2019;10:68. doi: 10.1186/s13287-019-1165-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Siegel G., Schafer R., Dazzi F. The immunosuppressive properties of mesenchymal stem cells. Transplantation. 2009;87:S45–S49. doi: 10.1097/TP.0b013e3181a285b0. [DOI] [PubMed] [Google Scholar]
- 49.Craft A.M., Ahmed N., Rockel J.S., Baht G.S., Alman B.A., Kandel R.A., Grigoriadis A.E., Keller G.M. Specification of chondrocytes and cartilage tissues from embryonic stem cells. Development. 2013;140:2597–2610. doi: 10.1242/dev.087890. [DOI] [PubMed] [Google Scholar]
- 50.Lach M., Trzeciak T., Richter M., Pawlicz J., Suchorska W.M. Directed differentiation of induced pluripotent stem cells into chondrogenic lineages for articular cartilage treatment. J. Tissue Eng. 2014;5:2041731414552701. doi: 10.1177/2041731414552701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.de Almeida P.E., Ransohoff J.D., Nahid A., Wu J.C. Immunogenicity of pluripotent stem cells and their derivatives. Circ. Res. 2013;112:549–561. doi: 10.1161/CIRCRESAHA.111.249243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kim S.H., Ha C.W., Park Y.B., Nam E., Lee J.E., Lee H.J. Intra-articular injection of mesenchymal stem cells for clinical outcomes and cartilage repair in osteoarthritis of the knee: A meta-analysis of randomized controlled trials. Arch. Orthop. Trauma Surg. 2019;139:971–980. doi: 10.1007/s00402-019-03140-8. [DOI] [PubMed] [Google Scholar]
- 53.Gnecchi M., Melo L.G. Bone marrow-derived mesenchymal stem cells: Isolation, expansion, characterization, viral transduction, and production of conditioned medium. Methods Mol. Biol. 2009;482:281–294. doi: 10.1007/978-1-59745-060-7_18. [DOI] [PubMed] [Google Scholar]
- 54.Gruber H.E., Deepe R., Hoelscher G.L., Ingram J.A., Norton H.J., Scannell B., Loeffler B.J., Zinchenko N., Hanley E.N., Tapp H. Human adipose-derived mesenchymal stem cells: Direction to a phenotype sharing similarities with the disc, gene expression profiling, and coculture with human annulus cells. Tissue Eng. Part. A. 2010;16:2843–2860. doi: 10.1089/ten.tea.2009.0709. [DOI] [PubMed] [Google Scholar]
- 55.Ishige I., Nagamura-Inoue T., Honda M.J., Harnprasopwat R., Kido M., Sugimoto M., Nakauchi H., Tojo A. Comparison of mesenchymal stem cells derived from arterial, venous, and Wharton’s jelly explants of human umbilical cord. Int. J. Hematol. 2009;90:261–269. doi: 10.1007/s12185-009-0377-3. [DOI] [PubMed] [Google Scholar]
- 56.Shariatzadeh M., Song J., Wilson S.L. The efficacy of different sources of mesenchymal stem cells for the treatment of knee osteoarthritis. Cell Tissue Res. 2019;378:399–410. doi: 10.1007/s00441-019-03069-9. [DOI] [PubMed] [Google Scholar]
- 57.Iijima H., Isho T., Kuroki H., Takahashi M., Aoyama T. Effectiveness of mesenchymal stem cells for treating patients with knee osteoarthritis: A meta-analysis toward the establishment of effective regenerative rehabilitation. NPJ Regen. Med. 2018;3:15. doi: 10.1038/s41536-018-0041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang A.T., Feng Y., Jia H.H., Zhao M., Yu H. Application of mesenchymal stem cell therapy for the treatment of osteoarthritis of the knee: A concise review. World J. Stem Cells. 2019;11:222–235. doi: 10.4252/wjsc.v11.i4.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.do Amaral R., Almeida H.V., Kelly D.J., O’Brien F.J., Kearney C.J. Infrapatellar Fat Pad Stem Cells: From Developmental Biology to Cell Therapy. Stem Cells Int. 2017;2017:6843727. doi: 10.1155/2017/6843727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Stocco E., Barbon S., Piccione M., Belluzzi E., Petrelli L., Pozzuoli A., Ramonda R., Rossato M., Favero M., Ruggieri P., et al. Infrapatellar Fat Pad Stem Cells Responsiveness to Microenvironment in Osteoarthritis: From Morphology to Function. Front. Cell Dev. Biol. 2019;7:323. doi: 10.3389/fcell.2019.00323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kim S., Kim T.M. Generation of mesenchymal stem-like cells for producing extracellular vesicles. World J. Stem Cells. 2019;11:270–280. doi: 10.4252/wjsc.v11.i5.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lian Q., Lye E., Suan Yeo K., Khia Way Tan E., Salto-Tellez M., Liu T.M., Palanisamy N., El Oakley R.M., Lee E.H., Lim B., et al. Derivation of clinically compliant MSCs from CD105+, CD24- differentiated human ESCs. Stem Cells. 2007;25:425–436. doi: 10.1634/stemcells.2006-0420. [DOI] [PubMed] [Google Scholar]
- 63.Hwang N.S., Varghese S., Lee H.J., Zhang Z., Ye Z., Bae J., Cheng L., Elisseeff J. In vivo commitment and functional tissue regeneration using human embryonic stem cell-derived mesenchymal cells. Proc. Natl. Acad. Sci. USA. 2008;105:20641–20646. doi: 10.1073/pnas.0809680106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hwang N.S., Varghese S., Zhang Z., Elisseeff J. Chondrogenic differentiation of human embryonic stem cell-derived cells in arginine-glycine-aspartate-modified hydrogels. Tissue Eng. 2006;12:2695–2706. doi: 10.1089/ten.2006.12.2695. [DOI] [PubMed] [Google Scholar]
- 65.Toh W.S., Lee E.H., Guo X.M., Chan J.K., Yeow C.H., Choo A.B., Cao T. Cartilage repair using hyaluronan hydrogel-encapsulated human embryonic stem cell-derived chondrogenic cells. Biomaterials. 2010;31:6968–6980. doi: 10.1016/j.biomaterials.2010.05.064. [DOI] [PubMed] [Google Scholar]
- 66.Jiang B., Fu X., Yan L., Li S., Zhao D., Wang X., Duan Y., Yan Y., Li E., Wu K., et al. Transplantation of human ESC-derived mesenchymal stem cell spheroids ameliorates spontaneous osteoarthritis in rhesus macaques. Theranostics. 2019;9:6587–6600. doi: 10.7150/thno.35391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gibson J.D., O’Sullivan M.B., Alaee F., Paglia D.N., Yoshida R., Guzzo R.M., Drissi H. Regeneration of Articular Cartilage by Human ESC-Derived Mesenchymal Progenitors Treated Sequentially with BMP-2 and Wnt5a. Stem Cells Transl. Med. 2017;6:40–50. doi: 10.5966/sctm.2016-0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang Y., Yu D., Liu Z., Zhou F., Dai J., Wu B., Zhou J., Heng B.C., Zou X.H., Ouyang H., et al. Exosomes from embryonic mesenchymal stem cells alleviate osteoarthritis through balancing synthesis and degradation of cartilage extracellular matrix. Stem Cell Res. Ther. 2017;8:189. doi: 10.1186/s13287-017-0632-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Narsinh K.H., Plews J., Wu J.C. Comparison of human induced pluripotent and embryonic stem cells: Fraternal or identical twins? Mol. Ther. 2011;19:635–638. doi: 10.1038/mt.2011.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chin M.H., Mason M.J., Xie W., Volinia S., Singer M., Peterson C., Ambartsumyan G., Aimiuwu O., Richter L., Zhang J., et al. Induced pluripotent stem cells and embryonic stem cells are distinguished by gene expression signatures. Cell Stem Cell. 2009;5:111–123. doi: 10.1016/j.stem.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Puri M.C., Nagy A. Concise review: Embryonic stem cells versus induced pluripotent stem cells: The game is on. Stem Cells. 2012;30:10–14. doi: 10.1002/stem.788. [DOI] [PubMed] [Google Scholar]
- 72.Lietman S.A. Induced pluripotent stem cells in cartilage repair. World J. Orthop. 2016;7:149–155. doi: 10.5312/wjo.v7.i3.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Takahashi K., Tanabe K., Ohnuki M., Narita M., Ichisaka T., Tomoda K., Yamanaka S. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007;131:861–872. doi: 10.1016/j.cell.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 74.Yu J., Vodyanik M.A., Smuga-Otto K., Antosiewicz-Bourget J., Frane J.L., Tian S., Nie J., Jonsdottir G.A., Ruotti V., Stewart R., et al. Induced pluripotent stem cell lines derived from human somatic cells. Science. 2007;318:1917–1920. doi: 10.1126/science.1151526. [DOI] [PubMed] [Google Scholar]
- 75.Wei Y., Zeng W., Wan R., Wang J., Zhou Q., Qiu S., Singh S.R. Chondrogenic differentiation of induced pluripotent stem cells from osteoarthritic chondrocytes in alginate matrix. Eur. Cell Mater. 2012;23:1–12. doi: 10.22203/eCM.v023a01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Moradi S., Mahdizadeh H., Saric T., Kim J., Harati J., Shahsavarani H., Greber B., Moore J.B., IV. Research and therapy with induced pluripotent stem cells (iPSCs): Social, legal, and ethical considerations. Stem Cell Res. Ther. 2019;10:341. doi: 10.1186/s13287-019-1455-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Deng X.Y., Wang H., Wang T., Fang X.T., Zou L.L., Li Z.Y., Liu C.B. Non-viral methods for generating integration-free, induced pluripotent stem cells. Curr. Stem Cell Res. Ther. 2015;10:153–158. doi: 10.2174/1574888X09666140923101914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Stadtfeld M., Nagaya M., Utikal J., Weir G., Hochedlinger K. Induced pluripotent stem cells generated without viral integration. Science. 2008;322:945–949. doi: 10.1126/science.1162494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pittenger M.F., Mackay A.M., Beck S.C., Jaiswal R.K., Douglas R., Mosca J.D., Moorman M.A., Simonetti D.W., Craig S., Marshak D.R. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–147. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- 80.Friedenstein A.J., Chailakhyan R.K., Gerasimov U.V. Bone marrow osteogenic stem cells: In vitro cultivation and transplantation in diffusion chambers. Cell Tissue Kinet. 1987;20:263–272. doi: 10.1111/j.1365-2184.1987.tb01309.x. [DOI] [PubMed] [Google Scholar]
- 81.Lv F.J., Tuan R.S., Cheung K.M., Leung V.Y. Concise review: The surface markers and identity of human mesenchymal stem cells. Stem Cells. 2014;32:1408–1419. doi: 10.1002/stem.1681. [DOI] [PubMed] [Google Scholar]
- 82.Pittenger M.F., Discher D.E., Peault B.M., Phinney D.G., Hare J.M., Caplan A.I. Mesenchymal stem cell perspective: Cell biology to clinical progress. NPJ Regen. Med. 2019;4:22. doi: 10.1038/s41536-019-0083-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wang M., Yuan Q., Xie L. Mesenchymal Stem Cell-Based Immunomodulation: Properties and Clinical Application. Stem Cells Int. 2018;2018:3057624. doi: 10.1155/2018/3057624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kim C., Keating A. Cell Therapy for Knee Osteoarthritis: Mesenchymal Stromal Cells. Gerontology. 2019;65:294–298. doi: 10.1159/000496605. [DOI] [PubMed] [Google Scholar]
- 85.Berebichez-Fridman R., Montero-Olvera P.R. Sources and Clinical Applications of Mesenchymal Stem Cells: State-of-the-art review. Sultan Qaboos Univ. Med. J. 2018;18:e264–e277. doi: 10.18295/squmj.2018.18.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ramakrishnan A., Torok-Storb B., Pillai M.M. Primary marrow-derived stromal cells: Isolation and manipulation. Methods Mol. Biol. 2013;1035:75–101. doi: 10.1007/978-1-62703-508-8_8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Koh Y.G., Choi Y.J. Infrapatellar fat pad-derived mesenchymal stem cell therapy for knee osteoarthritis. Knee. 2012;19:902–907. doi: 10.1016/j.knee.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 88.Koh Y.G., Jo S.B., Kwon O.R., Suh D.S., Lee S.W., Park S.H., Choi Y.J. Mesenchymal stem cell injections improve symptoms of knee osteoarthritis. Arthroscopy. 2013;29:748–755. doi: 10.1016/j.arthro.2012.11.017. [DOI] [PubMed] [Google Scholar]
- 89.Cianca J.C., Jayaram P. Musculoskeletal Injuries and Regenerative Medicine in the Elderly Patient. Phys. Med. Rehabil. Clin. N. Am. 2017;28:777–794. doi: 10.1016/j.pmr.2017.06.010. [DOI] [PubMed] [Google Scholar]
- 90.Shah K., Zhao A.G., Sumer H. New Approaches to Treat Osteoarthritis with Mesenchymal Stem Cells. Stem Cells Int. 2018;2018:5373294. doi: 10.1155/2018/5373294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wakitani S., Okabe T., Horibe S., Mitsuoka T., Saito M., Koyama T., Nawata M., Tensho K., Kato H., Uematsu K., et al. Safety of autologous bone marrow-derived mesenchymal stem cell transplantation for cartilage repair in 41 patients with 45 joints followed for up to 11 years and 5 months. J. Tissue Eng. Regen. Med. 2011;5:146–150. doi: 10.1002/term.299. [DOI] [PubMed] [Google Scholar]
- 92.Davatchi F., Abdollahi B.S., Mohyeddin M., Shahram F., Nikbin B. Mesenchymal stem cell therapy for knee osteoarthritis. Preliminary report of four patients. Int. J. Rheum. Dis. 2011;14:211–215. doi: 10.1111/j.1756-185X.2011.01599.x. [DOI] [PubMed] [Google Scholar]
- 93.Wong K.L., Lee K.B., Tai B.C., Law P., Lee E.H., Hui J.H. Injectable cultured bone marrow-derived mesenchymal stem cells in varus knees with cartilage defects undergoing high tibial osteotomy: A prospective, randomized controlled clinical trial with 2 years follow-up. Arthroscopy. 2013;29:2020–2028. doi: 10.1016/j.arthro.2013.09.074. [DOI] [PubMed] [Google Scholar]
- 94.Orozco L., Munar A., Soler R., Alberca M., Soler F., Huguet M., Sentis J., Sanchez A., Garcia-Sancho J. Treatment of knee osteoarthritis with autologous mesenchymal stem cells: A pilot study. Transplantation. 2013;95:1535–1541. doi: 10.1097/TP.0b013e318291a2da. [DOI] [PubMed] [Google Scholar]
- 95.Orozco L., Munar A., Soler R., Alberca M., Soler F., Huguet M., Sentis J., Sanchez A., Garcia-Sancho J. Treatment of knee osteoarthritis with autologous mesenchymal stem cells: Two-year follow-up results. Transplantation. 2014;97:e66–e68. doi: 10.1097/TP.0000000000000167. [DOI] [PubMed] [Google Scholar]
- 96.Davatchi F., Sadeghi Abdollahi B., Mohyeddin M., Nikbin B. Mesenchymal stem cell therapy for knee osteoarthritis: 5 years follow-up of three patients. Int. J. Rheum. Dis. 2016;19:219–225. doi: 10.1111/1756-185X.12670. [DOI] [PubMed] [Google Scholar]
- 97.Jo C.H., Lee Y.G., Shin W.H., Kim H., Chai J.W., Jeong E.C., Kim J.E., Shim H., Shin J.S., Shin I.S., et al. Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: A proof-of-concept clinical trial. Stem Cells. 2014;32:1254–1266. doi: 10.1002/stem.1634. [DOI] [PubMed] [Google Scholar]
- 98.Pak J., Chang J.J., Lee J.H., Lee S.H. Safety reporting on implantation of autologous adipose tissue-derived stem cells with platelet-rich plasma into human articular joints. BMC Musculoskelet Disord. 2013;14:337. doi: 10.1186/1471-2474-14-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kim Y.S., Kwon O.R., Choi Y.J., Suh D.S., Heo D.B., Koh Y.G. Comparative Matched-Pair Analysis of the Injection Versus Implantation of Mesenchymal Stem Cells for Knee Osteoarthritis. Am. J. Sports Med. 2015;43:2738–2746. doi: 10.1177/0363546515599632. [DOI] [PubMed] [Google Scholar]
- 100.Pers Y.M., Rackwitz L., Ferreira R., Pullig O., Delfour C., Barry F., Sensebe L., Casteilla L., Fleury S., Bourin P., et al. Adipose Mesenchymal Stromal Cell-Based Therapy for Severe Osteoarthritis of the Knee: A Phase I Dose-Escalation Trial. Stem Cells Transl. Med. 2016;5:847–856. doi: 10.5966/sctm.2015-0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lee W.S., Kim H.J., Kim K.I., Kim G.B., Jin W. Intra-Articular Injection of Autologous Adipose Tissue-Derived Mesenchymal Stem Cells for the Treatment of Knee Osteoarthritis: A Phase IIb, Randomized, Placebo-Controlled Clinical Trial. Stem Cells Transl. Med. 2019;8:504–511. doi: 10.1002/sctm.18-0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Mianehsaz E., Mirzaei H.R., Mahjoubin-Tehran M., Rezaee A., Sahebnasagh R., Pourhanifeh M.H., Mirzaei H., Hamblin M.R. Mesenchymal stem cell-derived exosomes: A new therapeutic approach to osteoarthritis? Stem Cell Res. Ther. 2019;10:340. doi: 10.1186/s13287-019-1445-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ni Z., Zhou S., Li S., Kuang L., Chen H., Luo X., Ouyang J., He M., Du X., Chen L. Exosomes: Roles and therapeutic potential in osteoarthritis. Bone Res. 2020;8:25. doi: 10.1038/s41413-020-0100-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cosenza S., Ruiz M., Toupet K., Jorgensen C., Noel D. Mesenchymal stem cells derived exosomes and microparticles protect cartilage and bone from degradation in osteoarthritis. Sci. Rep. 2017;7:16214. doi: 10.1038/s41598-017-15376-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ha D.H., Kim H.K., Lee J., Kwon H.H., Park G.H., Yang S.H., Jung J.Y., Choi H., Lee J.H., Sung S., et al. Mesenchymal Stem/Stromal Cell-Derived Exosomes for Immunomodulatory Therapeutics and Skin Regeneration. Cells. 2020;9:1157. doi: 10.3390/cells9051157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Roseti L., Desando G., Cavallo C., Petretta M., Grigolo B. Articular Cartilage Regeneration in Osteoarthritis. Cells. 2019;8:1305. doi: 10.3390/cells8111305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Evans C.H., Ghivizzani S.C., Robbins P.D. Gene Delivery to Joints by Intra-Articular Injection. Hum. Gene Ther. 2018;29:2–14. doi: 10.1089/hum.2017.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kim M.K., Ha C.W., In Y., Cho S.D., Choi E.S., Ha J.K., Lee J.H., Yoo J.D., Bin S.I., Choi C.H., et al. A Multicenter, Double-Blind, Phase III Clinical Trial to Evaluate the Efficacy and Safety of a Cell and Gene Therapy in Knee Osteoarthritis Patients. Hum. Gene Ther. Clin. Dev. 2018;29:48–59. doi: 10.1089/humc.2017.249. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.