Abstract
This cross-sectional study uses data from the Ontario Drug Benefit database to assess prescribing patterns of psychotropic drugs among nursing home residents in Ontario, Canada during the coronavirus disease 2019 pandemic.
A notable feature of the coronavirus disease 2019 (COVID-19) pandemic is the sizeable number of outbreaks and deaths in nursing homes. To limit the introduction of the virus in this setting, strict and lengthy lockdowns were imposed on nursing homes worldwide, resulting in concerns about the mental health of nursing home residents and increases in the use of psychotropic medications, which were frequently overprescribed before the pandemic.1,2
Methods
In this cross-sectional study, we examined the monthly proportion of nursing home residents who were prescribed psychotropic drugs as a proportion of the monthly number of residents filling a prescription for any drug in Ontario, Canada, from April 2018 to September 2020. As of March 1, 2020, 77 291 residents were living in the province’s 623 licensed nursing homes, in which they received personal and nursing care, subsidized accommodations, and prescription medications through a publicly funded long-term care program. Restrictions on visitation, absences (ie, leaving the nursing home), congregate dining, and group activities began in all Ontario nursing homes on March 14, 2020. The study was approved by the research ethics board of the University of Toronto, which waived the need for informed consent because there was no contact with nursing home residents, and anonymity was assured. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cross-sectional studies.
We examined the prescribing patterns of 4 classes of psychotropic medications: antipsychotics (first and second generation), antidepressants (selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, bupropion, and mirtazapine), benzodiazepines, and trazodone. We also assessed the prescribing of 2 negative tracer drugs (metformin and statins) for which prescribing patterns were not expected to change during the pandemic. Data were obtained from the Ontario Drug Benefit database through the Ministry of Health.
An interrupted time series analysis without external controls was used to examine changes in prescribing compared with expected prescribing based on the linear secular trend of prescribing from April 2018 to February 2020. We calculated absolute changes in the proportion of residents receiving a psychotropic drug prescription during the first 7 months of the COVID-19 pandemic (March to September 2020) compared with the most recent prepandemic months (January to February 2020). Data were analyzed from October to November 2020.
Results
From March to September 2020, absolute increases were found in the mean monthly proportion of nursing home residents who received prescriptions for antipsychotic medications, antidepressant medications, and trazodone compared with January to February 2020 (Table). A comparison of the January to February 2020 period with the month of September 2020 alone indicated absolute increases in the proportion of residents receiving prescriptions for antipsychotic drugs (1.6%; 95% CI, 0.9%-2.4%), antidepressant drugs (1.6%; 95% CI, 1.0%-2.2%), and trazodone (1.0%; 95% CI, 0.3%-1.8%). While prescribing for benzodiazepine medications decreased slightly (−0.2%; 95% CI, −1.0% to 0.6%), the interrupted time series analysis (Figure) revealed an increase in prescribing (0.3%; 95% CI, −0.3% to 0.9%) compared with decreases in secular prescribing trends between April 2018 and February 2020. This analysis also indicated that deviations higher than increasing secular prescribing trends were present for all other psychotropic medications, including antipsychotics (1.7%; 95% CI, 1.1%-2.2%), antidepressants (1.4%; 95% CI, 0.9%-1.8%), and trazodone (1.1%; 95% CI, 0.6%-1.7%). Decreases were observed in the proportion of residents who received prescriptions for metformin (−0.3%; 95% CI, −1.1% to 0.5%) and statins (−0.7%; 95% CI, −1.4% to 0.1%), and these decreases were more substantial compared with secular trends for the April 2018 to February 2020 period (for metformin, −0.6%; 95% CI, −1.2% to 0%; for statins, −1.4%; 95% CI, −1.9% to −0.8%).
Table. Changes in Psychotropic Drug Prescribing Among Nursing Home Residents in Ontario, Canada From January to September 2020.
| Medication type | Jan-Feb 2020 | Mar-Sep 2020 | Sep 2020 | ||||
|---|---|---|---|---|---|---|---|
| Mean monthly proportion of residents receiving prescription, %a | Mean monthly proportion of residents receiving prescription, % | Difference, % (95% CI) | Mean proportion of residents receiving prescription, %a | Difference, % (95% CI) | |||
| From Jan-Feb 2020b | From expected secular trend for Apr 2018-Feb 2020 c | From Jan-Feb 2020b | From expected secular trend for Apr 2018-Feb 2020c | ||||
| Psychotropic | |||||||
| Antidepressants | 51.3 | 52.3 | 1.0 (0.6 to 1.4) | 0.8 (0.5 to 1.1) | 52.9 | 1.6 (1.0 to 2.2) | 1.4 (0.9 to 1.8) |
| Trazodone | 25.4 | 26.1 | 0.7 (0.2 to 1.2) | 0.7 (0.3 to 1.0) | 26.5 | 1.0 (0.3 to 1.8) | 1.1 (0.6 to 1.7) |
| Antipsychotics | 28.4 | 29.5 | 1.1 (0.6 to 1.6) | 1.0 (0.7 to 1.3) | 30.0 | 1.6 (0.9 to 2.4) | 1.7 (1.1 to 2.2) |
| Benzodiazepines | 11.3 | 11.2 | −0.1 (−0.6 to 0.5) | 0.2 (−0.2 to 0.5) | 11.1 | −0.2 (−1.0 to 0.6) | 0.3 (−0.3 to 0.9) |
| Negative tracer | |||||||
| Metformin | 12.7 | 12.5 | −0.2 (−0.7 to 0.3) | −0.3 (−0.7 to 0.0) | 12.4 | −0.3 (−1.1 to 0.5) | −0.6 (−1.2 to 0.0) |
| Statins | 31.0 | 30.3 | −0.7 (−1.2 to −0.2) | −0.8 (−1.1 to −0.5) | 30.3 | −0.7 (−1.4 to 0.1) | −1.4 (−1.9 to −0.8) |
Mean monthly number of residents filling a prescription of interest as a proportion of the monthly number of residents filling a prescription for any drug. As of March 1, 2020, 77 291 residents were living in 623 licensed nursing homes in Ontario, Canada.
Absolute differences with 95% CIs compared with January to February 2020.
Adjusted absolute differences with 95% CIs compared with expected prescribing rates based on linear secular trends from April 2018 to February 2020.
Figure. Changes in Psychotropic Drug Prescribing Among Nursing Home Residents in Ontario, Canada, From April 2018 to September 2020.
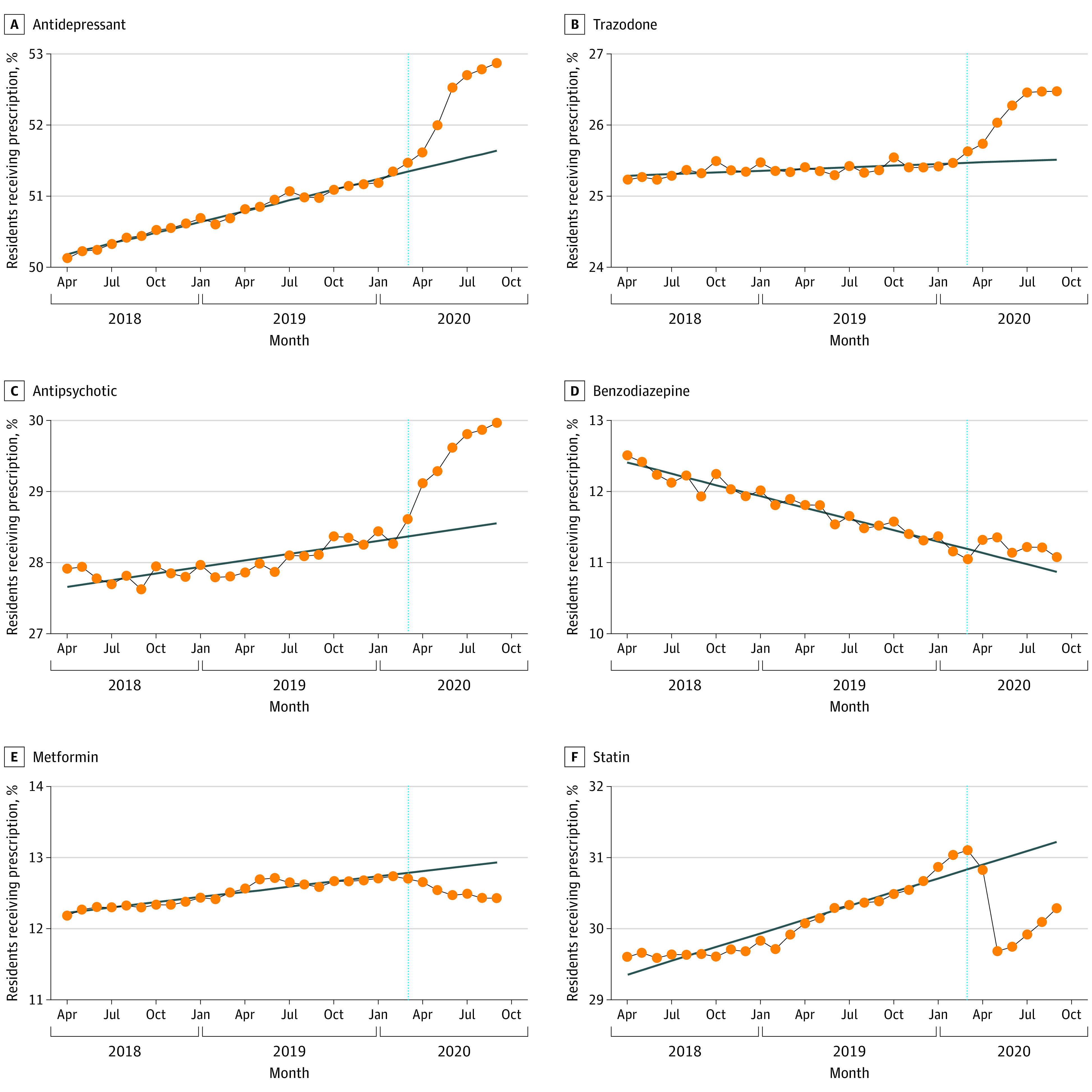
Monthly proportion of residents filling a prescription for each drug class from April 2018 to September 2020. As of March 1, 2020, 77 291 residents were living in 623 licensed nursing homes in Ontario. Expected prescribing was based on secular trends before the onset of the coronavirus disease 2019 (COVID-19) lockdown. The blue vertical dotted line represents the beginning of the lockdown (March 2020) in Ontario.
Discussion
This population-based study of all nursing home residents in Ontario, Canada, found increased prescribing of psychotropic drugs at the onset of the COVID-19 pandemic that persisted through September 2020. Although absolute increases in prescribing were small, they were disproportionate to expected secular prescribing trends from April 2018 to February 2020, and they were distinct from observed prescribing changes for other drugs during the pandemic.
This study examined the prescribing patterns of multiple classes of psychotropic drugs as well as drugs for which prescribing patterns were not expected to change during the pandemic. The results thus expand on those of a study in the United Kingdom, which reported increased prescribing of antipsychotic medications among patients with dementia during the pandemic.3 Our study is limited by a lack of data on prescribing indications. Although psychotropic medications may have been prescribed for residents who were dying of COVID-19, drugs such as antidepressants and trazodone are not typically used for acute palliative management. Therefore, it is likely that prescribing increases were also associated with the consequences of prolonged social isolation produced by infection prevention and control measures.4,5 Furthermore, clinicians may have been less likely to prioritize favorable nonpharmacological management for common issues, such as responsive behaviors, because of diminished resources, including lack of staffing.
Overall, the study’s findings highlight the importance of balancing infection prevention and control measures in nursing homes with the well-being of residents during the COVID-19 pandemic. Further studies are warranted to characterize additional factors that may be associated with drug prescribing during the pandemic, including prescriber and nursing home characteristics.6
References
- 1.Abbasi J. Social isolation—the other COVID-19 threat in nursing homes. JAMA. 2020;324(7):619-620. [DOI] [PubMed] [Google Scholar]
- 2.Rochon PA, Stukel TA, Bronskill SE, et al. Variation in nursing home antipsychotic prescribing rates. Arch Intern Med. 2007;167(7):676-683. doi: 10.1001/archinte.167.7.676 [DOI] [PubMed] [Google Scholar]
- 3.Howard R, Burns A, Schneider L. Antipsychotic prescribing to people with dementia during COVID-19. Lancet Neurol. 2020;19(11):892. doi: 10.1016/S1474-4422(20)30370-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van der Roest HG, Prins M, van der Velden C, et al. The impact of COVID-19 measures on well-being of older long-term care facility residents in the Netherlands. J Am Med Dir Assoc. 2020;21(11):1569-1570. doi: 10.1016/j.jamda.2020.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cagnin A, Di Lorenzo R, Marra C, et al. ; SINdem COVID-19 Study Group . Behavioral and psychological effects of coronavirus disease-19 quarantine in patients with dementia. Front Psychiatry. 2020;11:578015. doi: 10.3389/fpsyt.2020.578015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bergman C, Stall NM, Haimowitz D, et al. Recommendations for welcoming back nursing home visitors during the COVID-19 pandemic: results of a Delphi panel. J Am Med Dir Assoc. 2020;21(12):1759-1766. doi: 10.1016/j.jamda.2020.09.036 [DOI] [PMC free article] [PubMed] [Google Scholar]


