This systematic review and meta-analysis evaluates the risks and outcomes associated with 14 corticosteroid interventions administered to preterm infants.
Key Points
Question
Which is the most appropriate postnatal corticosteroid regimen for preventing mortality or bronchopulmonary dysplasia (BPD) in preterm neonates at 36 weeks’ postmenstrual age?
Findings
In this systematic review and network meta-analysis of 62 studies with 5559 neonates, a moderately early-initiated, medium cumulative dose of systemic dexamethasone had the highest relative risk reduction of mortality or BPD among 14 regimens, with a low confidence in the evidence.
Meaning
Results of this study suggested that a moderately early-initiated, medium cumulative dose of systemic dexamethasone appeared to be the best regimen for preventing mortality or BPD at 36 weeks’ postmenstrual age.
Abstract
Importance
The safety of postnatal corticosteroids used for prevention of bronchopulmonary dysplasia (BPD) in preterm neonates is a controversial matter, and a risk-benefit balance needs to be struck.
Objective
To evaluate 14 corticosteroid regimens used to prevent BPD: moderately early-initiated, low cumulative dose of systemic dexamethasone (MoLdDX); moderately early-initiated, medium cumulative dose of systemic dexamethasone (MoMdDX); moderately early-initiated, high cumulative dose of systemic dexamethasone (MoHdDX); late-initiated, low cumulative dose of systemic dexamethasone (LaLdDX); late-initiated, medium cumulative dose of systemic dexamethasone (LaMdDX); late-initiated, high cumulative dose of systemic dexamethasone (LaHdDX); early-initiated systemic hydrocortisone (EHC); late-initiated systemic hydrocortisone (LHC); early-initiated inhaled budesonide (EIBUD); early-initiated inhaled beclomethasone (EIBEC); early-initiated inhaled fluticasone (EIFLUT); late-initiated inhaled budesonide (LIBUD); late-initiated inhaled beclomethasone (LIBEC); and intratracheal budesonide (ITBUD).
Data Sources
PubMed, Cochrane Central Register of Controlled Trials (CENTRAL), Embase, World Health Organization’s International Clinical Trials Registry Platform (ICTRP), and CINAHL were searched from inception through August 25, 2020.
Study Selection
In this systematic review and network meta-analysis, the randomized clinical trials selected included preterm neonates with a gestational age of 32 weeks or younger and for whom a corticosteroid regimen was initiated within 4 weeks of postnatal age. Peer-reviewed articles and abstracts in all languages were included.
Data Extraction and Synthesis
Two independent authors extracted data in duplicate. Network meta-analysis used a bayesian model.
Main Outcomes and Measures
Primary combined outcome was BPD, defined as oxygen requirement at 36 weeks’ postmenstrual age (PMA), or mortality at 36 weeks’ PMA. The secondary outcomes included 15 safety outcomes.
Results
A total of 62 studies involving 5559 neonates (mean [SD] gestational age, 26 [1] weeks) were included. Several regimens were associated with a decreased risk of BPD or mortality, including EHC (risk ratio [RR], 0.82; 95% credible interval [CrI], 0.68-0.97); EIFLUT (RR, 0.75; 95% CrI, 0.55-0.98); LaHdDX (RR, 0.70; 95% CrI, 0.54-0.87); MoHdDX (RR, 0.64; 95% CrI, 0.48-0.82); ITBUD (RR, 0.73; 95% CrI, 0.57-0.91); and MoMdDX (RR, 0.61; 95% CrI, 0.45-0.79). Surface under the cumulative ranking curve (SUCRA) value ranking showed that MoMdDX (SUCRA, 0.91), MoHdDX (SUCRA, 0.86), and LaHdDX (SUCRA, 0.76) were the 3 most beneficial interventions. ITBUD (RR, 4.36; 95% CrI, 1.04-12.90); LaHdDX (RR, 11.91; 95% CrI, 1.64-44.49); LaLdDX (RR, 6.33; 95% CrI, 1.62-18.56); MoHdDX (RR, 4.96; 95% CrI, 1.14-14.75); and MoMdDX (RR, 3.16; 95% CrI, 1.35-6.82) were associated with more successful extubation from invasive mechanical ventilation. EHC was associated with a higher risk of gastrointestinal perforation (RR, 2.77; 95% CrI, 1.09-9.32). MoMdDX showed a higher risk of hypertension (RR, 3.96; 95% CrI, 1.10-30.91). MoHdDX had a higher risk of hypertrophic cardiomyopathy (RR, 5.94; 95% CrI, 1.95-18.11).
Conclusions and Relevance
This study suggested that MoMdDX may be the most appropriate postnatal corticosteroid regimen for preventing BPD or mortality at a PMA of 36 weeks, albeit with a risk of hypertension. The quality of evidence was low.
Introduction
Bronchopulmonary dysplasia (BPD) remains one of the most common, complex, and intriguing diseases among preterm neonates. Bronchopulmonary dysplasia is associated with an increased risk of mortality as well as short- and long-term morbidity, especially in extremely low-gestational-age neonates (ELGANs).1,2,3 Although the pathogenesis of BPD has yet to be fully deciphered, an imbalance between ongoing pulmonary inflammation and simultaneous repair seems to play a major role.4,5 In ELGANs, postnatal corticosteroids (PNCs) have been used for both the prevention and treatment of BPD. The anti-inflammatory action of PNCs on the pulmonary system has been postulated to improve gas exchange and lung mechanics, thus facilitating weaning from invasive mechanical ventilation.6 However, the use of PNCs in ELGANs remains controversial because of fear of adverse neurodevelopmental effects.7
Multiple studies have indicated that BPD is associated with risk of poor long-term neurological outcomes, such as cerebral palsy, as well as cognitive, visual, speech, and learning impairments and behavioral problems.1 Doyle et al,2 in their follow-up to a longitudinal study of extremely preterm infants born during the past 3 decades, found that the rates of BPD did not decrease despite an increase in the use of noninvasive respiratory support in the latter years. Doyle et al2 postulated that less use of PNCs, even in infants who were at the highest risk of BPD, might be a contributing factor. As such, clinicians often have to negotiate between the risks of adverse outcomes associated with long-term ventilation and the potential adverse outcomes of PNCs.
Field studies report a varying prevalence of PNC use (3%-50%).8,9 Appreciating the chasm, different academic bodies provide advice on the use of both systemic and inhaled PNCs for preterm neonates who are at risk of BPD.10,11,12 As a common denominator, the recommendations unanimously warn against the early use of systemic dexamethasone at fewer than 8 days of life. However, the policy statements for other regimens of systemic dexamethasone or different corticosteroids, including hydrocortisone and inhaled corticosteroids, differ widely among advisory bodies.10,11,12
An abundance of systematic reviews and meta-analyses that compare different PNCs using pairwise comparisons are available.13,14,15,16,17,18 However, evaluating such a complex intervention in a network meta-analysis would ease interpretation and enable the ranking of PNCs according to improved outcomes and safety.19 To our knowledge, only a single network meta-analysis has covered this subject.20 To guide safe clinical practice, we performed a comprehensive systematic review and network meta-analysis to scrutinize the existing body of evidence as well as to evaluate and compare treatments that have not been compared against each other in randomized clinical trials (RCTs).
Methods
The study protocol was registered with PROSPERO (CRD42020205685).21 We followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline.22
Interventions and Studies
This systematic review and network meta-analysis evaluated 14 interventions for BPD: (1) moderately early-initiated (8-14 days), low cumulative dose (<2 mg/kg) of systemic dexamethasone (MoLdDX); (2) moderately early-initiated, medium cumulative dose (2-4 mg/kg) of systemic dexamethasone (MoMdDX); (3) moderately early-initiated, high cumulative dose (>4 mg/kg) of systemic dexamethasone (MoHdDX); (4) late-initiated (15-27 days), low cumulative dose of systemic dexamethasone (LaLdDX); (5) late-initiated, medium cumulative dose of systemic dexamethasone (LaMdDX); (6) late-initiated, high cumulative dose of systemic dexamethasone (LaHdDX); (7) early-initiated (<8 days) systemic hydrocortisone (EHC); (8) late-initiated (≥8 days) systemic hydrocortisone (LHC); (9) early-initiated (<8 days) inhaled budesonide (EIBUD); (10) early-initiated inhaled beclomethasone (EIBEC); (11) early-initiated inhaled fluticasone (EIFLUT); (12) late-initiated (≥8 days) inhaled budesonide (LIBUD); (13) late-initiated inhaled beclomethasone (LIBEC); and (14) intratracheal budesonide (ITBUD; using surfactant as a vehicle). The cumulative dose and duration of systemic dexamethasone were categorized on the basis of previously published systematic reviews.14
We included studies of preterm neonates with a gestational age of 32 weeks or younger that compared any of the previously mentioned interventions in an RCT. Published and peer-reviewed full-text articles and abstracts in all languages were included. The characteristics of the included studies are provided in Table 1.23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83 Studies that evaluated early-initiated dexamethasone (<8 days of postnatal age) or dexamethasone in established cases of BPD (≥28 days) were excluded.
Table 1. Characteristics of the Included Studies.
| Source (study location) | Birth weight, mean or median, g | Gestational age, mean (SD), wk | Intervention 1 (No.) | Intervention 2 (No.) | Time of randomization | Dose, mg/kg | Ventilated at enrollment? | Open-label systemic corticosteroid used? | ANS, % | Other comments |
|---|---|---|---|---|---|---|---|---|---|---|
| LIBUD vs late-initiated systemic dexamethasone | ||||||||||
| Dimitriou et al,23 1997 (United Kingdom) | 833 |
|
LaMdMcDX (20)a | LIBUD (20) | 27 d | 2.8 | Yes | No | 55-60 | LIBUD: 100 μg 4 times daily; 10 d |
| Halliday et al,24 2001 (Ireland) | 1007 |
|
LaMdMcDX (150)a | EIBUD (143) (LIBUD) (142) | >15 d | 2.7 | Yes | No | 55-63 |
|
| EIBEC | ||||||||||
| Cole et al,25 1999 (United States) | 800 |
|
EIBEC (123) | Placebo (130) | 5 d | NA | Yes | Yes | 68-77 |
|
| Zimmerman et al,26 2000 (United States) | 828 |
|
EIBEC (20) | Placebo (19) | <8 h | NA | Yes | Yes | 70-79 | Tapering dose; exact dose not mentioned; 12 d |
| Jangaard et al,27 2002 (Canada) | 900 |
|
EIBEC (30) | Placebo (30) | <96 h | NA | Yes | Yes | 50-53 | 200 μg/kg/d; 28 d |
| ITBUD + surfactant | ||||||||||
| Lin et al,28 2001 (China) | 953 | NA (mean: 27) | EIBUD (44) | Placebo (42) | <12 h | NA | NA | NA | NA | ITBUD: 500 μg/kg |
| Yeh et al,29 2008 (Taiwan); Kuo et al,30 2010 (Taiwan) | 900 |
|
ITBUD + surfactant (60) | Surfactant (56) | <2 h | NA | Yes | Yes | 42-46 | ITBUD: 0.25 mg/kg with 100 mg/kg Survanta, repeated administration every 8 h until FiO2 < 0.4 |
| Yeh et al,31 2016 (United States and Taiwan) | 908 |
|
ITBUD + surfactant (131) | Surfactant (134) | <4 h | NA | Yes | Yes | 79-85 | ITBUD: 0.25 mg/kg with 100 mg/kg Survanta, repeated administration every 8 h until FiO2 < 0.3 or extubated, maximum dose: 6 |
| Ke et al,32 2016 (China) | NA | NA |
|
Surfactant (46) | 4 h | NA | Yes | NA | NA |
|
| Pan et al,33 2017 (China) | 1310 |
|
ITBUD + surfactant (15) | Surfactant (15) | 4 h | NA | Yes | NA | 60-67 | ITBUD: mean (SD), 0.25 (70) mg pulmonary surfactant; surfactant dose of 70 mg/kg, repeated once if FiO2 > 0.4 or MAP >8 cm water |
| EIBUD | ||||||||||
| Merz et al,34 1999 (Germany) | 1114 |
|
EIBUD (12) | Placebo (11) | 3 d | NA | Yes | Yes | 58-63 | 1600 μg/d; 10 d |
| Bassler et al,35,36 2015, 2018 (multicenter Europe) | 800 |
|
EIBUD (437) | Placebo (419) | <24 h | NA | Yes | No | 88-90 | 200 μg Twice daily; 14 d followed by 200 μg once daily until withdrawal of oxygen or positive pressure or 32 wk’ PMA |
| Sadeghnia et al,37 2018 (Iran) | 915 |
|
EIBUD (35) | Placebo (35) | 2 h | NA | No | NA | 38-49 | 500 μg Every 12 h; 7 d |
| Cao et al,38 2018 (China) | NA | NA (inclusion ≤32 w) | EIBUD (40) | Placebo (40) | NA | NA | NA | NA | NA | 250 μg/kg, Duration not mentioned |
| EIFLUT | ||||||||||
| Fok et al,39 1999 (China) | 987 |
|
EIFLUT (27) | Placebo (26) | <24 h | NA | Yes | Yes | 50-55 | 250 μg Twice daily every 12 d |
| Yong et al,40 1999 (NA) | 972 |
|
EIFLUT (20) | Placebo (20) | <18 h | NA | Yes | NA | NA | 500 μg/d; 14 d |
| Nakamura et al,41 2016 (Japan) | 784 |
|
EIFLUT (107) | Placebo (104) | <24 h | NA | Yes | NA | 40-42 | 50 μg Twice daily; 6 wk or until extubation |
| EHC | ||||||||||
| Watterberg et al,42 1999 (United States) | 746 |
|
EHC (20) | Placebo (20) | <48 h | 10.5 | Yes | Yes | 85 | 1 mg/kg/d for 9 d; 0.5 mg/kg/d for 3 d |
| Efird et al,43 2005 (United States) | 783 |
|
EHC (16) | Placebo (18) | <3 h | 5.8 | NA | No | >94 |
|
| Watterberg et al,44,45 2004, 2007 (United States) | 733 |
|
EHC (180) | Placebo (180) | 12-48 h | 13.5 | Yes | Yes | 77-81 | 1 mg/kg/d for 12 d; 0.5 mg/kg/d for 3 d |
| Peltoniemi et al,46,47 2005, 2009 (Finland) | 895 |
|
EHC (25) | Placebo (26) | <36 h | 11.5 | Yes | No | 92-96 | 2 mg/kg/d for 2 d; 1.5 mg/kg/d for 2 d; 0.75 mg/kg/d for 6 d |
| Bonsante et al,48 2007 (Italy) | 860 |
|
EHC (25) | Placebo (25) | <48 h | 10.5 | Yes | Yes | 52-68 | 1 mg/kg/d for 9 d; 0.5 mg/kg/d for 3 d |
| Ng et al,49 2006 (Hong Kong) | 919 |
|
EHC (24) | Placebo (24) | 12 h | 15 | NA | Yes | NA | 1 mg/kg 3 Times daily; 5 d |
| Hochwald et al,50 2014 (United States) | 844 |
|
EHC (11) | Placebo (11) | ≤48 h | 7 | NA | NA | 63 |
|
| Baud et al,51,52 2016, 2019 (France) | 850 |
|
EHC (255) | Placebo (266) | 16 h | 8.5 | Yes | No | 88-95 | 1 mg/kg/d for 7 d; 0.5 mg/kg/d for 3 d |
| LIBEC | ||||||||||
| LaForce and Brudno,53 1993 (United States) | <1500 | NA | LIBEC (6) | Placebo (7) | ≥14 d | NA | Yes | NA | NA | 50 μg 3 Times daily; 28 d |
| Giep et al,54 1996 (United States) | 768 |
|
LIBEC (10) | Placebo (9) | 19 d | NA | Yes | Yes | 22-40 | 1000 μg/kg/d |
| Denjean et al,55 1998 (France) | 1050 |
|
LIBEC (43) | Placebo (43) | 10 d | NA | Yes | Yes | 14-26 | 250 μg 4 Times daily; 28 d |
| LIBEC vs late-initiated systemic dexamethasone | ||||||||||
| Suchomski and Cummings,56 2002 (United States) | 845 |
|
LIBEC (51) | LaHdLcDX (27)a | 17 d | 7.6 | Yes | Yes | 48-84 |
|
| Rozycki et al,57 2003 (United States) | 760 |
|
LIBEC (15) | LaHdLcDX (15)a | >14 d | 7.6 | Yes | Yes | 59-67 |
|
| LIBUD | ||||||||||
| Arnon et al,58 1996 (United Kingdom) | 1024 |
|
LIBUD (9) | Placebo (11) | 14 d | NA | Yes | NA | 73-78 | 600 μg Twice daily for 7 d or until extubation |
| Jónsson et al,59 2000 (Sweden) | 806 |
|
LIBUD (15) | Placebo (15) | 7 d | NA | Yes | Yes | 67-80 |
|
| LHC | ||||||||||
| Parikh et al,60,61 2013, 2015 (United States) | 666 |
|
LHC (31) | Placebo (33) | 16 d | 17 | Yes | Yes | 61-81 | 3 mg/kg/d for 3 d; 2 mg/kg/d for 2 d; 1 mg/kg/d for 1 d |
| Onland et al,62 2019 (Netherlands) | 742 |
|
LHC (181) | Placebo (190) | 10 d | 72.5 | Yes | NA | 87-91 |
|
| Late-initiated systemic dexamethasone | ||||||||||
| Cummings et al,63 1989 (United States) | 827 |
|
LaHdLcDX (13)a | LaMdLcDX (12)a Placebo (11) | 15 d | 3 vs 7.98 | Yes | NA | 25-38 | Course duration: 18 and 42 d |
| Kothadia et al,64 1999 (United States) | 750 |
|
LaHdLcDX (50)a | Placebo (45) | 19 d | 7.98 | Yes | NA | 16-48 | 0.5 mg/kg/d for 3 d; 0.3 mg/kg/d for 3 d; dose reduced by 10% every 3rd d to reach 0.1 mg/kg/d on 34th d;, same dose on alternate d for 1 wk |
| Malloy et al,65 2005 (United States) | 770 |
|
LaMdScDX (8)a | LaLdScDX (8)a | 15 d | 2.7 vs 0.56 | Yes | Yes | 63-75 |
|
| Doyle et al,66,67 2006, 2007 (Australia) | 676 |
|
LaLdMcDX (35)a | Placebo (35) | 4 wk | 0.89 | Yes | Yes | 89 | 0.15 mg/kg/d for 3 d; 0.10 mg/kg/d for 3 d; 0.05 mg/kg/d for 2 d; 0.02 mg/kg/d for 2 d |
| Moderately early-initiated systemic dexamethasone | ||||||||||
| Kari et al,68 1993 (Finland) | 880 |
|
MoMdScDX (17)a | Placebo (24) | 14 d | 3.5 | Yes | Yes | 4-6 | 0.5 mg/kg/d; 7 d |
| Ramanathan et al,69 1994 (United States) | NA | NA (mean, 27 wk) | MoMdScDX (15)a | MoLdScDX (13)a | 10-14 d | 1.9 vs 1 | NA | NA | NA |
|
| Brozanski et al,70 1995 (United States) | 804 |
|
MoHdLcDX (39)a | Placebo (39) | 7 d | 3-10.5 | Yes | NA | 20-23 |
|
| Durand et al,71 1995 (United States) | <1500 | NA | MoMdScDX (23)a | Placebo (20) | 7-14 d | 2.35 | Yes | NA | NA | 0.5 mg/kg/d for 3 d and then 0.25 mg/kg/d for 3 d and 0.10 mg/kg for 1 d |
| Scott et al,72 1997 (United States) | NA | NA | MoMdScDX (10)a | Placebo (5) | 11-14 d | 1.9 | Yes | NA | NA | 0.5 mg/kg/d for 2 d and then 0.3 mg/kg/d for 3 d |
| Bloomfield et al,73 1998 (New Zealand); Armstrong et al,74 2002 (New Zealand) | 782.5 |
|
MoHdMcDX (19)a | LaHdLcDX (21)a | 14 d | 5.3 vs 7.1 | Yes | NA | 62-68 |
|
| Kovács et al,75 1998 (Canada) | 763 |
|
MoLdScDX (30)a | Placebo (30) | 7 d | 1.5 | Yes | Yes | 73 | 0.25 mg/kg Twice daily for 3 d |
| Merz et al,34 1999 (Germany) | 960 |
|
MoMdLcDX (15)a | LaMdLcDX (15)a | 7 d vs 14 d | 2.9 | Yes | NA | 73-87 | 0.5 mg/kg/d for 3 d; 0.3 mg/kg/d for 3 d; 0.1 mg/kg/d, followed by this dose alternatively every 2nd d until day 16 |
| Romagnoli et al,76,77 1999, 2002 (Italy) | 899 |
|
MoHdMcDX (15)a | Placebo (15) | 10 d | 4.75 | Yes | NA | 40-47 | 0.5 mg/kg/d for 6 d; 0.25 mg/kg/d for 6 d; 0.125 mg/kg/d for 2 d |
| Durand et al,78 2002 (United States) | 895 |
|
MoMdScDX (23)a | MoLdScDX (24)a | NA | 2.35 vs 1 | Yes | Yes (after study period) | 50-52 |
|
| Walther et al,79 2003 (United States) | 1011 |
|
MoMdMcDX (17)a | Placebo (19) | 7-14 d | 1.9 | Yes | Yes | 42-76 | 0.2 mg/kg/d for 4 d; 0.15 mg/kg/d for 4 d; 0.10 mg/kg/d for 4 d; 0.05 mg/kg/d for 2 d |
| McEvoy et al,80 2004 (United States) | 834.5 |
|
MoMdMcDX (29)a | MoLdScDX (33)a | 7-14 d | 2.35 vs 1 | Yes | Yes (after study period) | 34-48 |
|
| Odd et al,81 2004 (New Zealand) | 695 |
|
MoMdLcDX (17)a | MoHdLcDX (16)a | 10-12 d | 3.8 vs 6.5 | Yes | Yes | NA |
|
| Alishiri and Mosavi,82 2015 (Iran) | 1456 |
|
MoMdScDX (27)a | Placebo (31) | 8 d | 3.5 | No | Yes | 33-39 | 0.25 mg/kg Twice daily from 7 d |
| Marr et al,83 2019 (United States) | 777 |
|
MoHdLcDX (30)a | MoMdMcDX (29)a | 14 d | 7.98 vs 4 | Yes | NA | 62-63 |
|
Abbreviations: ANS, antenatal corticosteroids; EHC, early-initiated systemic hydrocortisone; EIBEC, early-initiated inhaled beclomethasone; EIBUD, early-initiated inhaled budesonide; EIFLUT, early-initated inhaled fluticasone; IQR, interquartile range; ITBUD, intratracheal budesonide; LaHdLcDX, late-initiated, high cumulative dose, long course of systemic dexamethasone; LaLdMcDX, late-initiated, low cumulative dose, medium course of systemic dexamethasone; LaLdScDX, late-initiated, low cumulative dose, short course of systemic dexamethasone; LaMdLcDX, late-initiated, medium cumulative dose, long course of systemic dexamethasone; LaMdMcDX, late-initiated, medium cumulative dose, medium course of systemic dexamethasone; LaMdScDX, late-initiated, medium cumulative dose, short course of systemic dexamethasone; LHC, late-initiated systemic hydrocortisone; LIBEC, late-initated inhaled beclomethasone; LIBUD, late initiated inhaled budesonide; MAP, mean arterial pressure; MoHdLcDX, moderately early-initiated, high cumulative dose, long course of systemic dexamethasone; MoHdMcDX, moderately early-initiated, high cumulative dose, medium course of systemic dexamethasone; MoLdScDX, moderately early-initiated, low cumulative dose, short course of systemic dexamethasone; MoMdLcDX, moderately early-initiated, medium cumulative dose, long course of systemic dexamethasone; MoMdMcDX, moderately early-initiated, medium cumulative dose, medium course of systemic dexamethasone; MoMdScDX, moderately early-initiated, medium cumulative dose, short course of systemic dexamethasone; NA, not applicable; Pco2, partial pressure of carbon dioxide; PMA, postmenstrual age.
Early-initiated: less than 8 days of postnatal age; late-initiated: 15 to 27 days of postnatal age; moderately early-initiated: 8 to 14 days of postnatal age; long course: more than 14 days; medium course: 8 to 14 days; short course: less than 8 days; high cumulative dose: greater than 4 mg/kg and low cumulative dose: less than 2 mg/kg; medium cumulative dose: 2 to 4 mg/kg.
Primary and Secondary Outcomes
The primary combined outcome was mortality or BPD, which was defined as oxygen dependency, at a postmenstrual age (PMA) of 36 weeks. The secondary outcomes were incidences of BPD at a PMA of 36 weeks, BPD at 28 days of age, successful extubation from invasive mechanical ventilation, mortality before discharge, an intraventricular hemorrhage grade of III or IV,84 periventricular leukomalacia, hyperglycemia, hypertension (defined as systolic or diastolic blood pressure >2 SDs above the mean for neonates’ gestational and postnatal age), necrotizing enterocolitis (stage ≥II per Bell et al85), gastrointestinal perforation, retinopathy of prematurity stage 3 or higher,86 blood culture–proven sepsis, hypertrophic cardiomyopathy, cerebral palsy or neurodevelopmental impairment (NDI) at 18 to 24 months (cerebral palsy or mental development index <70 per Bayley Scales of Infant Development II), or visual or hearing impairment.
Literature Search, Study Selection, and Risk-of-Bias Assessment
We searched the online databases MEDLINE (via PubMed), Cochrane Central Register of Controlled Trials (CENTRAL), Embase, World Health Organization’s International Clinical Trials Registry Platform (ICTRP), and CINAHL (via CENTRAL) from inception through August 25, 2020. The citations from previously published systematic reviews on PNCs for prevention and treatment of BPD were also searched. The search strategy used is shown in eTable 1 in the Supplement.
Two of us (T.B. and J.A.) independently screened titles, abstracts, and full-text articles. Full-text articles of relevant RCTs were selected and evaluated for inclusion. In case of differences of opinion between the 2 reviewers, we consulted a third author (V.V.R.).
The risk of bias for the included studies was assessed by 2 of us (T.B. and V.V.R.) using the Cochrane Collaboration risk-of-bias tool.87 The domains of selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias were evaluated. Disagreements between the 2 assessors were resolved by consulting a third reviewer (C.C.R.).
Quality of Evidence
The quality of evidence for the primary and secondary outcomes was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) Working Group approach for network meta-analysis.88 The direct evidence from pairwise comparisons was first evaluated on risk of bias, inconsistency (heterogeneity), imprecision, indirectness, and publication bias. The quality of indirect evidence was evaluated from the lowest quality of direct evidence (of pairwise comparisons) from the first-order loops. When 2 or more first-order loops were detected, the highest quality of evidence among them was used. If no first-order loops were present, the quality of indirect evidence was inferred from the lowest quality of direct evidence from the higher-order loops. The highest quality of evidence between direct and indirect evidence was adjudged to be the quality of the evidence for the final network estimate. The quality of evidence was ranked as follows: high (high confidence in the evidence), moderate (moderate confidence), low (some confidence), and very low (little confidence) (Table 2).
Table 2. Assessment of the Quality of Evidence for the Different Comparisons for Bronchopulmonary Dysplasia (BPD) or Mortality at Postmenstrual Age (PMA) of 36 Weeks.
| Regimen comparison | Quality of evidence (reason for downgrading)a | Network meta-analysis | ||
|---|---|---|---|---|
| Indirect evidence | Direct evidence | RR (95% CrI) | Quality of evidencea | |
| Primary outcome: BPD or mortality at 36 wk’ PMA | ||||
| EHC:EIBEC | Low (risk of bias, imprecision) | NA | 0.90 (0.59-1.30) | Low |
| EHC:EIBUD | Moderate (imprecision) | NA | 1.01 (0.75-1.35) | Moderate |
| EHC:EIFLUT | Moderate (imprecision) | NA | 1.12 (0.79-1.54) | Moderate |
| EHC:ITBUD | Low (imprecision, heterogeneity) | NA | 1.15 (0.84-1.52) | Low |
| EHC:LaHdDXb | Moderate (imprecision) | NA | 1.20 (0.87-1.59) | Moderate |
| EHC:LaLdDXb | Low (severe imprecision) | NA | 0.93 (0.63-1.29) | Low |
| EHC:LaMdDXb | Low (severe imprecision) | NA | 0.90 (0.64-1.21) | Low |
| EHC:LHC | Moderate (imprecision) | NA | 0.83 (0.59-1.09) | Moderate |
| EHC:LIBEC | Very low (risk of bias, severe imprecision) | NA | 1.09 (0.71-1.51) | Very low |
| EHC:LIBUD | Very low (risk of bias, imprecision) | NA | 0.94 (0.62-1.36) | Very low |
| EHC:MoHdDXb | Moderate (imprecision) | NA | 1.31 (0.94-1.77) | Moderate |
| EHC:MoLdDXb | Very low (risk of bias, severe imprecision) | NA | 1.00 (0.62-1.53) | Very low |
| EHC:MoMdDXb | Low (risk of bias, imprecision) | NA | 1.38 (0.98-1.89) | Low |
| EHC:Placebo | NA | Moderate (imprecision) | 0.82 (0.68-0.97)c | Moderate |
| EIBEC:EIBUD | Low (risk of bias, imprecision) | NA | 1.16 (0.75-1.77) | Low |
| EIBEC:EIFLUT | Low (risk of bias, imprecision) | NA | 1.29 (0.80-2.00) | Low |
| EIBEC:ITBUD | Low (risk of bias, imprecision) | NA | 1.32 (0.84-1.99) | Low |
| EIBEC:LaHdDXb | Low (risk of bias, imprecision) | NA | 1.38 (0.88-2.08) | Low |
| EIBEC:LaLdDXb | Low (risk of bias, imprecision) | NA | 1.07 (0.65-1.67) | Low |
| EIBEC:LaMdDXb | Low (risk of bias, imprecision) | NA | 1.04 (0.65-1.57) | Low |
| EIBEC:LHC | Low (risk of bias, imprecision) | NA | 0.95 (0.61-1.43) | Low |
| EIBEC:LIBEC | Very low (risk of bias, severe imprecision) | NA | 1.25 (0.74-1.94) | Very low |
| EIBEC:LIBUD | Very low (risk of bias, imprecision) | NA | 1.08 (0.64-1.74) | Very low |
| EIBEC:MoHdDXb | Low (risk of bias, imprecision) | NA | 1.51 (0.95-2.30) | Low |
| EIBEC:MoLdDXb | Very low (risk of bias, severe imprecision) | NA | 1.15 (0.64-1.91) | Very low |
| EIBEC:MoMdDXb | Low (risk of bias, imprecision) | NA | 1.59 (0.99-2.45) | Low |
| EIBEC:Placebo | NA | Low (risk of bias, imprecision) | 0.95 (0.65-1.33) | Low |
| EIBUD:EIFLUT | Moderate (imprecision) | NA | 1.12 (0.76-1.59) | Moderate |
| EIBUD:ITBUD | Low (imprecision, heterogeneity) | NA | 1.15 (0.80-1.57) | Low |
| EIBUD:LaHdDXb | Moderate (imprecision) | NA | 1.20 (0.84-1.63) | Moderate |
| EIBUD:LaLdDXb | Low (severe imprecision) | NA | 0.93 (0.62-1.30) | Low |
| EIBUD:LaMdDXb | Low (severe imprecision) | Very low (risk of bias, imprecision) | 0.90 (0.66-1.15) | Low |
| EIBUD:LHC | Moderate (imprecision) | NA | 0.83 (0.57-1.13) | Moderate |
| EIBUD:LIBEC | Very low (risk of bias, severe imprecision) | NA | 1.09 (0.68-1.55) | Very low |
| EIBUD:LIBUD | Very low (risk of bias, imprecision) | Very low (risk of bias, imprecision) | 0.93 (0.66-1.26) | Very low |
| EIBUD:MoHdDXb | Moderate (imprecision) | NA | 1.31 (0.90-1.83) | Moderate |
| EIBUD:MoLdDXb | Very low (risk of bias, severe imprecision) | NA | 1.00 (0.60-1.57) | Very low |
| EIBUD:MoMdDXb | Low (risk of bias, imprecision) | NA | 1.38 (0.95-1.94) | Low |
| EIBUD:Placebo | Very low (risk of bias, imprecision) | Moderate (imprecision) | 0.83 (0.63-1.02) | Moderate |
| EIFLUT:ITBUD | Low (imprecision, heterogeneity) | NA | 1.05 (0.70-1.49) | Low |
| EIFLUT:LaHdDXb | Moderate (imprecision) | NA | 1.09 (0.74-1.56) | Moderate |
| EIFLUT:LaLdDXb | Low (severe imprecision) | NA | 0.84 (0.54-1.25) | Low |
| EIFLUT:LaMdDXb | Low (severe imprecision) | NA | 0.82 (0.54-1.18) | Low |
| EIFLUT:LHC | Moderate (imprecision) | NA | 0.76 (0.50-1.07) | Moderate |
| EIFLUT:LIBEC | Very low (risk of bias, severe imprecision) | NA | 0.99 (0.61-1.46) | Very low |
| EIFLUT:LIBUD | Low (severe imprecision) | NA | 0.86 (0.53-1.31) | Low |
| EIFLUT:MoHdDXb | Moderate (imprecision) | NA | 1.19 (0.79-1.73) | Moderate |
| EIFLUT:MoLdDXb | Very low (risk of bias, severe imprecision) | NA | 0.91 (0.53-1.47) | Very low |
| EIFLUT:MoMdDXb | Low (risk of bias, imprecision) | NA | 1.26 (0.83-1.84) | Low |
| EIFLUT:Placebo | NA | Moderate (imprecision) | 0.75 (0.55-0.98)c | Moderate |
| ITBUD:LaHdDXb | Low (imprecision, heterogeneity) | NA | 1.06 (0.75-1.47) | Low |
| ITBUD:LaLdDXb | Low (imprecision, heterogeneity) | NA | 0.82 (0.54-1.18) | Low |
| ITBUD:LaMdDXb | Low (imprecision, heterogeneity) | NA | 0.80 (0.55-1.11) | Low |
| ITBUD:LHC | Low (imprecision, heterogeneity) | NA | 0.73 (0.51-1.01) | Low |
| ITBUD:LIBEC | Very low (risk of bias, severe imprecision) | NA | 0.96 (0.61-1.38) | Very low |
| ITBUD:LIBUD | Low (risk of bias, imprecision) | NA | 0.83 (0.53-1.24) | Low |
| ITBUD:MoHdDXb | Low (imprecision, heterogeneity) | NA | 1.16 (0.80-1.63) | Low |
| ITBUD:MoLdDXb | Very low (risk of bias, severe imprecision) | NA | 0.88 (0.53-1.39) | Very low |
| ITBUD:MoMdDXb | Low (risk of bias, imprecision) | NA | 1.22 (0.84-1.74) | Low |
| ITBUD:Placebo | NA | Low (imprecision, heterogeneity) | 0.73 (0.57-0.91)c | Low |
| LaHdDX:LaLdDXb | Low (severe imprecision) | NA | 0.78 (0.52-1.13) | Low |
| LaHdDX:LaMdDXb | Low (severe imprecision) | Low (severe imprecision) | 0.76 (0.53-1.04) | Low |
| LaHdDX:LHC | Moderate (imprecision) | NA | 0.70 (0.49-0.96)c | Moderate |
| LaHdDX:LIBEC | Very low (risk of bias, severe imprecision) | Low (risk of bias, imprecision) | 0.91 (0.67-1.15) | Low |
| LaHdDX:LIBUD | Low (severe imprecision) | NA | 0.79 (0.52-1.18) | Low |
| LaHdDX:MoHdDXb | Moderate (imprecision) | Low (risk of bias, imprecision) | 1.10 (0.79-1.51) | Moderate |
| LaHdDX:MoLdDXb | Very low (risk of bias, severe imprecision) | NA | 0.84 (0.51-1.32) | Very low |
| LaHdDX:MoMdDXb | Low (risk of bias, imprecision) | NA | 1.16 (0.81-1.64) | Low |
| LaHdDX:Placebo | Low (severe imprecision) | Moderate (imprecision) | 0.70 (0.54-0.87)c | Moderate |
| LaLdDX:LaMdDXb | Low (severe imprecision) | Low (severe imprecision) | 0.99 (0.69-1.38) | Low |
| LaLdDX:LHC | Low (severe imprecision) | NA | 0.92 (0.60-1.32) | Low |
| LaLdDX:LIBEC | Very low (risk of bias, severe imprecision) | NA | 1.20 (0.73-1.78) | Very low |
| LaLdDX:LIBUD | Low (severe imprecision) | NA | 1.03 (0.66-1.57) | Low |
| LaLdDX:MoHdDXb | Low (severe imprecision) | NA | 1.45 (0.95-2.13) | Low |
| LaLdDX:MoLdDXb | Very low (risk of bias, severe imprecision) | NA | 1.10 (0.64-1.80) | Very low |
| LaLdDX:MoMdDXb | Low (severe imprecision) | NA | 1.52 (1.00-2.27) | Low |
| LaLdDX:Placebo | Low (severe imprecision) | Low (severe imprecision) | 0.91 (0.66-1.21) | Low |
| LaMdDX:LHC | Low (severe imprecision) | NA | 0.92 (0.60-1.32) | Low |
| LaMdDX:LIBEC | Low (risk of bias, imprecision) | NA | 1.03 (0.66-1.57) | Low |
| LaMdDX:LIBUD | Very low (risk of bias, imprecision) | Low (risk of bias, imprecision) | 1.05 (0.78-1.42) | Low |
| LaMdDX:MoHdDXb | Low (severe imprecision) | NA | 1.48 (1.01-2.10)c | Low |
| LaMdDX:MoLdDXb | Low (severe imprecision) | NA | 1.12 (0.67-1.79) | Low |
| LaMdDX:MoMdDXb | Low (severe imprecision) | Low (severe imprecision) | 1.55 (1.06-2.24)c | Low |
| LaMdDX:Placebo | Very low (risk of bias, imprecision) | Low (severe imprecision) | 0.93 (0.71-1.19) | Low |
| LHC:LIBEC | Very low (risk of bias, severe imprecision) | NA | 1.33 (0.85-1.92) | Very low |
| LHC:LIBUD | Low (severe imprecision) | NA | 1.15 (0.74-1.75) | Low |
| LHC:MoHdDXb | Moderate (imprecision) | NA | 1.60 (1.11-2.28)c | Moderate |
| LHC:MoLdDXb | Very low (risk of bias, severe imprecision) | NA | 1.22 (0.74-1.95) | Very low |
| LHC:MoMdDXb | Low (risk of bias, imprecision) | NA | 1.69 (1.16-2.45)c | Low |
| LHC:Placebo | NA | Moderate (imprecision) | 1.01 (0.79-1.28) | Moderate |
| LIBEC:LIBUD | Very low (risk of bias, imprecision) | NA | 0.89 (0.55-1.43) | Very low |
| LIBEC:MoHdDXb | Low (risk of bias, imprecision) | NA | 1.24 (0.83-1.86) | Low |
| LIBEC:MoLdDXb | Very low (risk of bias, severe imprecision) | NA | 0.94 (0.55-1.58) | Very low |
| LIBEC:MoMdDXb | Very low (risk of bias, severe imprecision) | NA | 1.30 (0.86-2.01) | Very low |
| LIBEC:Placebo | Low (risk of bias, imprecision) | Very low (risk of bias, severe imprecision) | 0.78 (0.57-1.09) | Low |
| LIBUD:MoHdDXb | Low (risk of bias, imprecision) | NA | 1.44 (0.91-2.16) | Low |
| LIBUD:MoLdDXb | Low (risk of bias, imprecision) | NA | 1.09 (0.61-1.82) | Low |
| LIBUD:MoMdDXb | Low (risk of bias, imprecision) | NA | 1.51 (0.95-2.30) | Low |
| LIBUD:Placebo | Low (severe imprecision) | NA | 0.91 (0.62-1.25) | Low |
| MoHdDX:MoLdDXb | Low (severe imprecision) | NA | 0.77 (0.47-1.20) | Low |
| MoHdDX:MoMdDXb | Low (risk of bias, imprecision) | Low (severe imprecision) | 1.06 (0.83-1.35) | Low |
| MoHdDX:Placebo | Low (severe imprecision) | Moderate (imprecision) | 0.64 (0.48-0.82)c | Moderate |
| MoLdDX:MoMdDXb | Very low (risk of bias, severe imprecision) | Low (severe imprecision) | 1.44 (0.90-2.19) | Low |
| MoLdDX:Placebo | Low (severe imprecision) | Very low (risk of bias, severe imprecision) | 0.87 (0.55-1.27) | Low |
| MoMdDX:Placebo | Low (severe imprecision) | Low (risk of bias, imprecision) | 0.61 (0.45-0.79)c | Low |
Abbreviations: CrI, credible interval; EHC, early-initiated systemic hydrocortisone; EIBEC, early-initiated inhaled beclomethasone; EIBUD, early-initiated inhaled budesonide; EIFLUT, early-initiated inhaled fluticasone; ITBUD, intratracheal budesonide; LaHdDX, late-initiated, high cumulative dose of systemic dexamethasone; LaLdDX, late-initiated, low cumulative dose of systemic dexamethasone; LaMdDX, late-initiated, medium cumulative dose of systemic dexamethasone; LHC, late-initiated systemic hydrocortisone; LIBEC, late-initiated inhaled beclomethasone; LIBUD, late-initiated inhaled budesonide; MoHdDX, moderately early-initiated, high cumulative dose of systemic dexamethasone; MoLdDX, moderately early-initiated low cumulative dose of systemic dexamethasone; MoMdDX, moderately early-initiated, medium cumulative dose of systemic dexamethasone; NA, not applicable; PMA, postmenstrual age; RR, risk ratio.
Quality of evidence was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) Working Group approach: high (high confidence in the evidence: the true effect [or the reality, as defined by the GRADE group] is close to the estimated effect), moderate (moderate confidence: the true effect is likely close to but likely substantially different from the estimated effect), low (some confidence: the true effect is likely substantially different from the estimated effect), and very low (little confidence: the true effect is substantially different from the estimated effect).
Early-initiated: <8 days of postnatal age; late-initiated: 15 to 27 days of postnatal age; moderately early-initiated: 8 to 14 days of postnatal age; long course: more than 14 days; medium course: 8 to 14 days; short course: less than 8 days; high cumulative dose: greater than 4 mg/kg; low cumulative dose: less than 2 mg/kg; medium cumulative dose: 2 to 4 mg/kg.
Values are statistically significant.
Statistical Analysis
Network meta-analysis using bayesian and frequentist approaches was performed using R, version 3.6.2; netmeta; BUGSnet; and gemtc packages (R Foundation for Statistical Computing).89,90 The bayesian network meta-analysis was performed with Markov chain Monte Carlo simulation using vague priors. We used generalized linear models with 4 chains, burn-in of 50 000 iterations followed by 100 000 iterations, and 10 000 adaptations.90 Network geometry was evaluated with network plots. Model fit was assessed with leverage plots, total residual deviance, and deviance information criterion. Gelman-Rubin as well as trace and density plots were inspected for model convergence.91 Node-splitting and inconsistency model method in the bayesian approach as well as net-splitting in the frequentist approach were used to look for any inconsistency between the direct and indirect evidence.92 A P < .05 was considered as statistically significant. The sensitivity of the bayesian results was assessed by comparing them with the results of the frequentist approach.
Pairwise comparisons were depicted using forest plots and the I2 statistic to detect heterogeneity. Estimates were reported as risk ratios (RRs, with 95% credible intervals [CrIs] or 95% CIs). Forest plots, league plots, and matrix plots were used to illustrate the network estimates of various comparisons. Ranking of the interventions was performed with the surface under the cumulative ranking curve (SUCRA) plots.93 Caution is warranted when interpreting the SUCRA. The SUCRA values can vary across outcomes for the same regimen, and the differences might be attributed to chance alone; the values should be interpreted along with the quality of evidence and do not capture the magnitude of differences in outcomes between 2 regimens.93
In addition, we performed the following sensitivity analyses: (1) excluding RCTs that enrolled neonates on noninvasive respiratory support; (2) subdividing dexamethasone therapy according to the total duration of the treatment course into short course (<8 days), medium course (8-14 days) and long course (>14 days); (3) excluding RCTs with antenatal corticosteroid coverage of less than 70%; (4) excluding RCTs with a high risk of bias; (5) excluding RCTs that evaluated intratracheal budesonide; and (6) combining the different types of inhaled corticosteroids.
Results
Of the 2211 studies screened, 62 studies (involving 5559 neonates) were included in the final analysis23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83 (Table 1 and eFigure 1 in the Supplement). The mean (SD) gestational age of the enrolled neonates was 26 (1) weeks (eFigure 2 in the Supplement). We contacted 19 authors for additional information regarding their studies, and 2 responded. The included studies consisted of two 3-group RCTs,24,63 and 41 had enrolled ventilated neonates,23,24,25,26,27,28,29,31,34,35,38,39,40,41,42,44,46,48,51,55,56,57,59,60,62,63,64,65,66,68,69,70,71,74,75,76,78,79,80,81,83 but only 18 had included neonates with an antenatal corticosteroid coverage of more than 70%.25,26,28,29,31,34,42,43,44,46,51,59,60,62,65,66,75,79 Excluded studies are listed in eTable 2 in the Supplement.
Thirteen studies were judged to have a high risk of bias.25,32,33,37,50,54,55,58,65,68,75,81,82 Three studies were classified as having variable risk of bias,24,28,69 and 45 studies had a low risk of bias.23,26,27,29,30,31,34,35,36,38,39,40,41,42,43,44,45,46,47,48,49,51,52,53,56,57,59,60,61,62,63,64,66,67,70,71,72,73,74,76,77,78,79,80,83 The RCTs with a high risk of bias predominantly had concerns regarding random sequence generation and allocation concealment. The risk-of-bias summary and graph are shown in eFigure 3 in the Supplement.
Primary Outcome
A total of 45 studies with 5236 neonates and 2768 events (53% event rate) were included for the assessment of the primary outcome (Figure 1 and eTable 3 in the Supplement).23,24,25,26,27,28,29,31,34,35,38,39,40,41,42,43,44,46,59,49,50,51,55,56,57,60,62,63,64,65,66,68,69,70,71,74,75,76,78,79,80,81,83 When compared with placebo, EHC (RR, 0.82; 95% CrI, 0.68-0.97); EIFLUT (RR, 0.75; 95% CrI, 0.55-0.98); LaHdDX (RR, 0.70; 95% CrI, 0.54-0.87); MoHdDX (GRADE: moderate) (RR, 0.64; 95% CrI, 0.48-0.82); ITBUD (RR, 0.73; 95% CrI, 0.57-0.91); and MoMdDX (GRADE: low) (RR, 0.61; 95% CrI, 0.45-0.79) decreased the risk of the primary outcome, mortality or BPD at 36 weeks’ PMA (Figure 1). Furthermore, MoMdDX was better than LaMdDX (GRADE: low) (RR, 0.67; 95% CrI, 0.45-0.94), and MoHdDX was better than LaMdDX (GRADE: low) (RR, 0.70; 95% CrI, 0.48-0.99) (Figure 2).
Figure 1. Network, Surface Under the Cumulative Ranking Curve (SUCRA), and Forest Plots for Bronchopulmonary Dysplasia or Mortality at Postmenstrual Age of 36 Weeks .
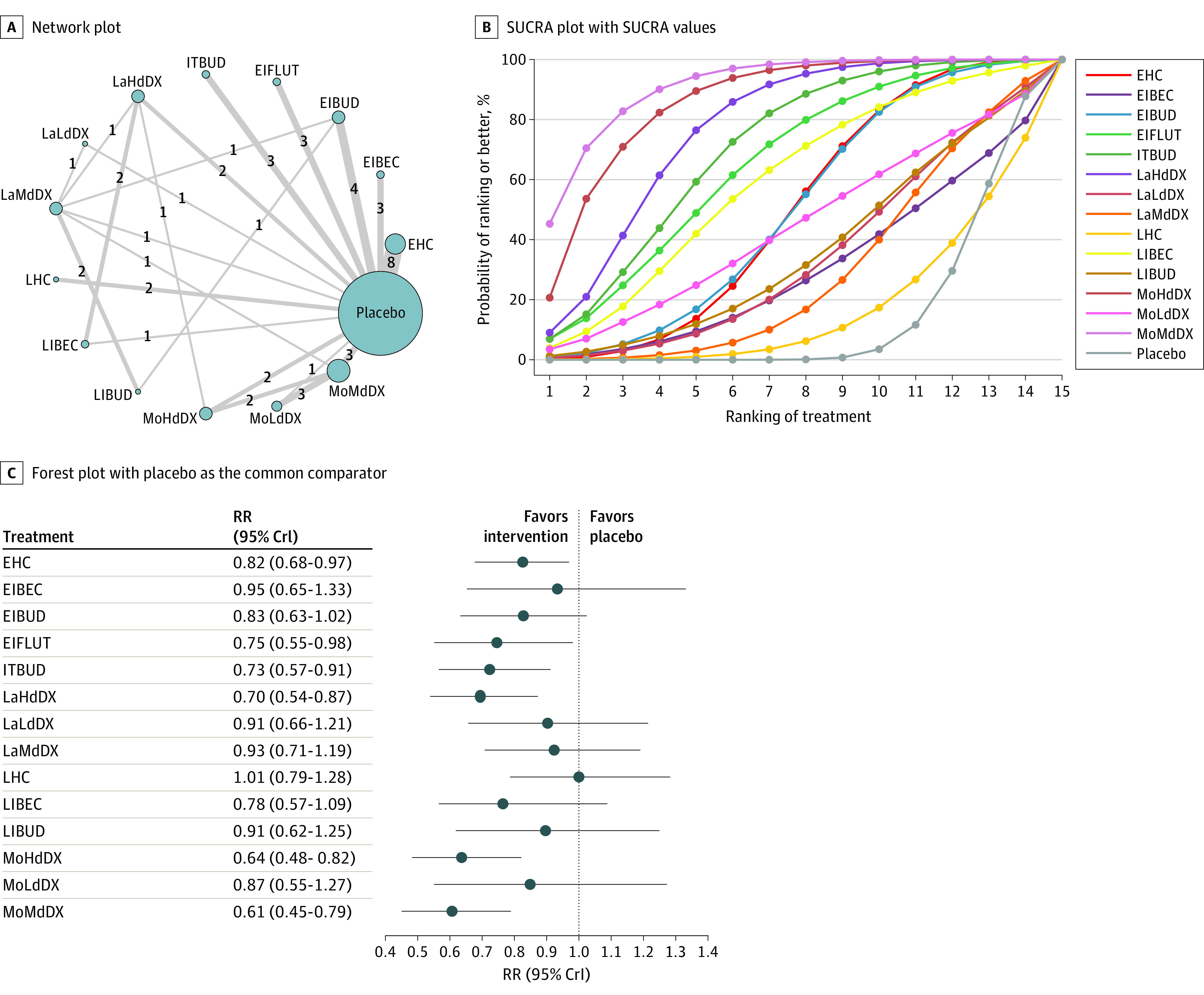
A, Different nodes represent the postnatal corticosteroid interventions. The size of the nodes is proportional to the number of patients who were assigned to the intervention. The thickness of the lines connecting the nodes is proportional to the number of pairwise trials that evaluated the interventions, which are shown as numbers along the lines. B, Higher ranking of treatment was associated with smaller outcome value. The SUCRA values (%) for each treatment were as follows: 49 for early-initiated systemic hydrocortisone (EHC); 30, early-initiated inhaled beclomethasone (EIBEC); 50, early-initiated inhaled budesonide (EIBUD); 65, early-initiated inhaled fluticasone (EIFLUT); 70, intratracheal budesonide (ITBUD); 76, late-initiated, high cumulative dose of systemic dexamethasone (LaHdDX); 34, late-initiated, low cumulative dose of systemic dexamethasone (LaLdDX); 29, late-initiated, medium cumulative dose of systemic dexamethasone (LaMdDX); 17, late-initiated systemic hydrocortisone (LHC); 59, late-initiated inhaled beclomethasone (LIBEC); 35, late-initiated inhaled budesonide (LIBUD); 86, moderately early-initiated, high cumulative dose of systemic dexamethasone (MoHdDX); 44, moderately early-initiated, low cumulative dose of systemic dexamethasone (MoLdDX); 91, moderately early-initiated, medium cumulative dose of systemic dexamethasone (MoMdDX); and 14, placebo. C, The forest plot shows the risk ratio (RR) relative to placebo. CrI indicates credible interval.
Figure 2. League Plot of the Network Estimates of Postnatal Corticosteroid Comparisons for Bronchopulmonary Dysplasia or Mortality at a Postmenstrual Age of 36 Weeks .
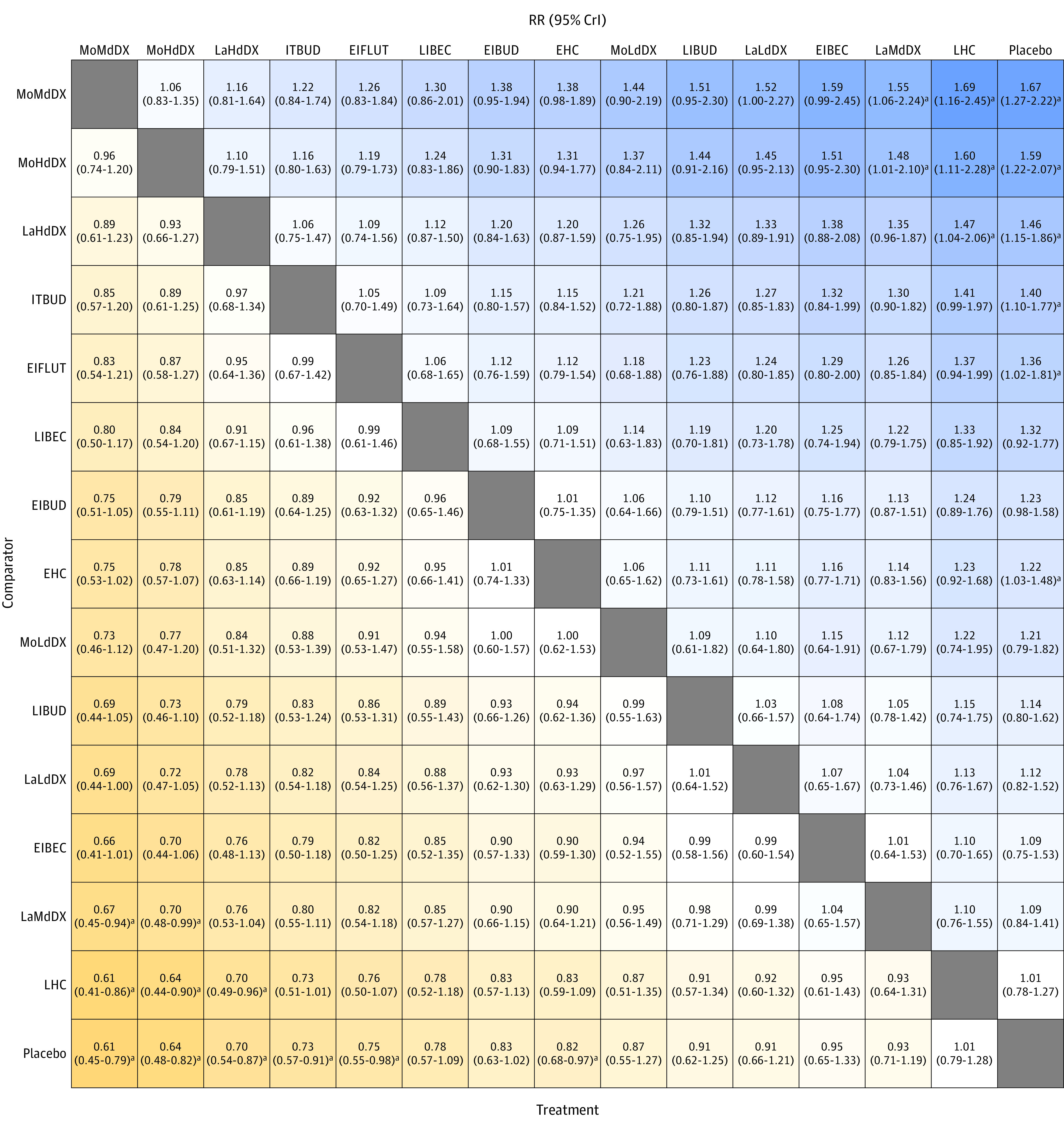
Network estimates are depicted as risk ratio (RR) with 95% credible interval (CrI). EHC indicates early-initiated systemic hydrocortisone; EIBEC, early-initiated inhaled beclomethasone; EIBUD, early-initiated inhaled budesonide; EIFLUT, early-initiated inhaled fluticasone; ITBUD, intratracheal budesonide; LaHdDX, late-initiated, high cumulative dose of systemic dexamethasone; LaLdDX, late-initiated, low cumulative dose of systemic dexamethasone; LaMdDX, late-initiated, medium cumulative dose of systemic dexamethasone; LHC, late-initiated systemic hydrocortisone; LIBEC, late-initiated inhaled beclomethasone; LIBUD, late-initiated inhaled budesonide; MoHdDX, moderately early-initiated, high cumulative dose of systemic dexamethasone; MoMdDX, moderately early-initiated, medium cumulative dose of systemic dexamethasone; MoLdDX, moderately early-initiated, low cumulative dose of systemic dexamethasone.
aValues are statistically significant.
SUCRA values ranked MoMdDX (SUCRA, 0.91); MoHdDX (SUCRA, 0.86); and LaHdDX (SUCRA, 0.76) as the 3 most beneficial interventions. The least beneficial intervention was LHC (SUCRA, 0.17) (Figure 1). Direct evidence from the pairwise comparisons and the split between direct and indirect evidence are shown in eFigures 4 and 5 in the Supplement. The quality of evidence for the various comparisons for the primary outcome is described in Table 2.
Secondary Outcomes
The network characteristics for all 15 secondary outcomes are provided in eTable 3 in the Supplement. The network plots; SUCRA plots; forest plots depicting the network estimate compared with placebo, split between direct and indirect evidence, and direct pairwise comparisons; and the league plots or matrix plots are shown in eFigures 6 to 56 in the Supplement. The quality-of-evidence assessment is outlined in eTable 4 in the Supplement. Because of the sparseness of some of the networks, node-splitting to assess inconsistency was not possible for some of the 15 outcomes (intraventricular hemorrhage, periventricular leukomalacia, necrotizing enterocolitis, hypertrophic cardiomyopathy, and cerebral palsy at 18-24 months).
EIBUD was associated with decreased incidence of BPD at a PMA of 36 weeks (GRADE: moderate) (RR, 0.71; 95% CrI, 0.51-0.94). Furthermore, EHC showed a pattern of lesser incidence of BPD at 36 weeks’ PMA but did not reach statistical significance (RR, 0.86; 95% CrI, 0.71-1.02).
When compared with placebo, MoMdDX (GRADE: low) (RR, 0.43; 95% CrI, 0.18-0.82) and EHC (GRADE: moderate) (RR, 0.69; 95% CrI, 0.44-0.98) were associated with reduced mortality before discharge. EIBUD did not show any significant difference in the incidence of mortality compared with placebo (RR, 0.89; 95% CrI, 0.46-1.36).
The following regimens were associated with more extubations: ITBUD (RR, 4.36; 95% CrI, 1.04-12.90); LaHdDX (RR, 11.91; 95% CrI, 1.64-44.49); LaLdDX (RR, 6.33; 95% CrI, 1.62-18.56); MoHdDX (RR, 4.96; 95% CrI, 1.14-14.75); and MoMdDX (GRADE: very low to low) (RR, 3.16; 95% CrI, 1.35-6.82). According to SUCRA ranking, LaHdDX was the best intervention.
None of the interventions were associated with either a decreased or an increased risk of NDI. In addition, LaHdDX showed a lower incidence of NDI at 18 to 24 months compared with LaMdDX (GRADE: low) (RR, 0.31; 95% CrI, 0.03-0.90).
Compared with placebo, EHC was associated with a higher risk of gastrointestinal perforation (GRADE: moderate) (RR, 2.77; 95% CrI, 1.09-9.32). The network was sparse, and inconsistency assessment was not possible. The direct pairwise analysis revealed a higher risk of hypertrophic cardiomyopathy with MoHdDX compared with placebo (GRADE: low) (RR, 5.94; 95% CrI, 1.95-18.11).
Compared with placebo, MoMdDX was associated with higher risk of hypertension (GRADE: low) (RR, 3.96; 95% CrI, 1.10-30.91). Inconsistency was detected in the network meta-analysis.
Sensitivity Analyses
Moderately early-initiated, medium cumulative dose, short course of systemic dexamethasone (RR, 0.54; 95% CrI, 0.30-0.86); moderately early-initiated, high cumulative dose, long course of systemic dexamethasone (RR, 0.65; 95% CrI, 0.42-0.95); and late-initiated, high cumulative dose, long course of systemic dexamethasone (RR, 0.71; 95% CrI, 0.52-0.94) were associated with decreased risk of the primary outcome, mortality or BPD at PMA of 36 weeks (Figure 3). On the basis of SUCRA values, a moderately early-initiated, medium cumulative dose, short course of systemic dexamethasone was found to be the best intervention (SUCRA, 0.82). The network characteristics for all of the sensitivity analyses are shown in eTable 3 in the Supplement. Inconsistency assessment by splitting direct and indirect evidence as well as the league plot depicting the network estimates for the different comparisons are given in eFigures 57 and 58 in the Supplement.
Figure 3. Subdividing Dexamethasone Therapy by Total Duration of the Course.
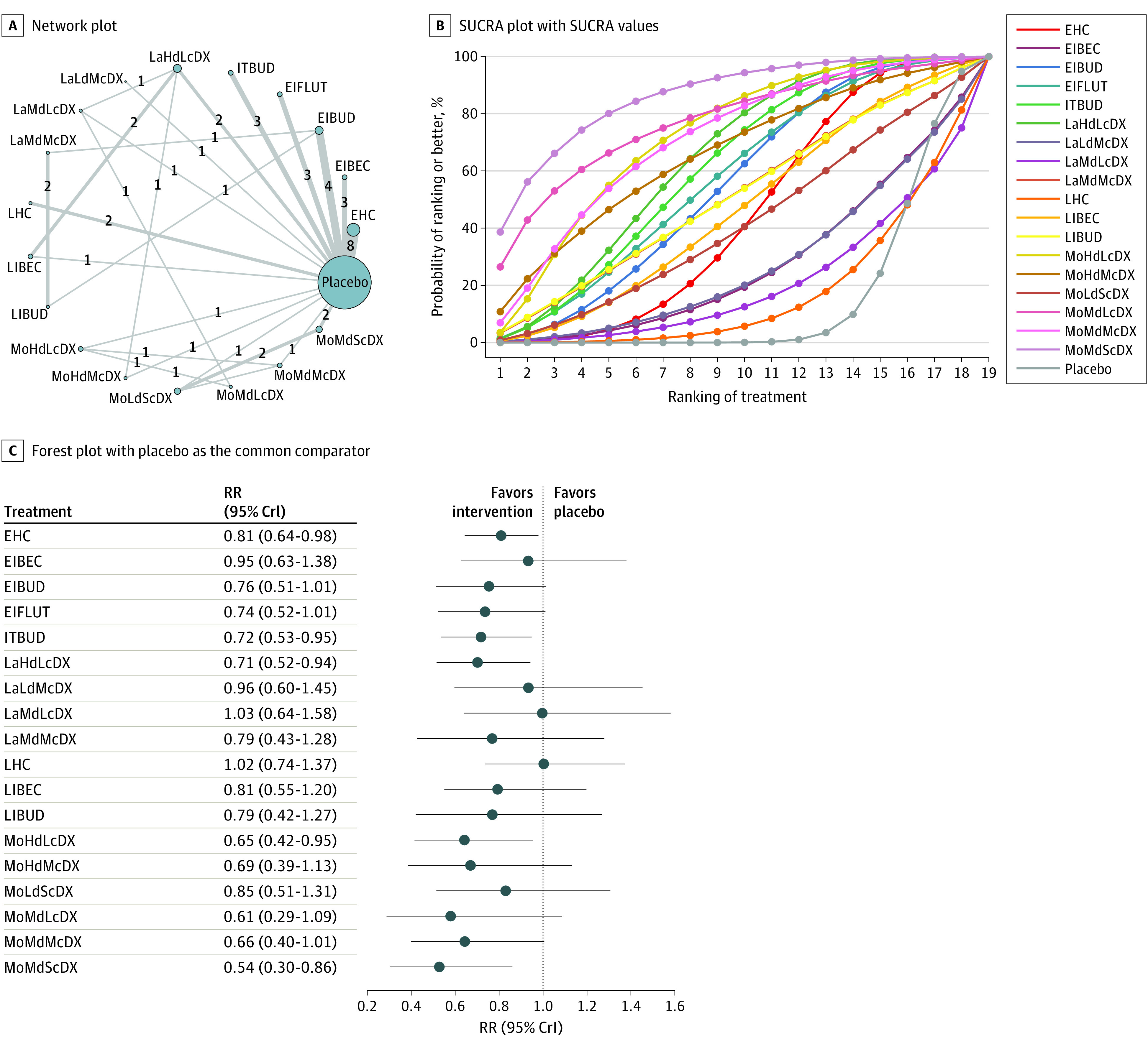
A, Different nodes represent the postnatal corticosteroid interventions. The size of the nodes is proportional to the number of patients who were assigned to the intervention. The thickness of the lines connecting the nodes is proportional to the number of pairwise trials that evaluated the interventions, which are shown as numbers along the lines. B, Higher ranking of treatment was associated with smaller outcome value. The surface under the cumulative ranking curve (SUCRA) values (%) for each treatment were as follows: 44 for early-initiated systemic hydrocortisone (EHC); 29, early-initiated inhaled beclomethasone (EIBEC); 53, early-initiated inhaled budesonide (EIBUD); 56, early-initiated inhaled fluticasone (EIFLUT); 59, intratracheal budesonide (ITBUD); 62, late-initiated, high cumulative dose, long course of systemic dexamethasone (LaHdLcDX); 29, late-initiated, low cumulative dose, medium course of systemic dexamethasone (LaLdMcDX); 58, late-initiated, low cumulative dose, short course of systemic dexamethasone (LaLdScDX); 22, late-initiated, medium cumulative dose, long course of systemic dexamethasone (LaMdLcDX); 50, late-initiated, medium cumulative dose, medium course of systemic dexamethasone (LaMdMcDX); 56, late-initiated, medium cumulative dose, short course of systemic dexamethasone (LaMdScDX); 19, late-initiated systemic hydrocortisone (LHC); 46, late-initiated inhaled beclomethasone (LIBEC); 50, late-initiated inhaled budesonide (LIBUD); 69, moderately early-initiated, high cumulative dose, long course of systemic dexamethasone (MoHdLcDX); 63, moderately early-initiated, high cumulative dose, medium course of systemic dexamethasone (MoHdMcDX); 41, moderately early-initiated, low cumulative dose, short course of systemic dexamethasone (MoLdScDX); 74, moderately early-initiated, medium cumulative dose, long course of systemic dexamethasone (MoMdLcDX); 68, moderately early-initiated, medium cumulative dose, medium course of systemic dexamethasone (MoMdMcDX); 82, moderately early-initiated, medium cumulative dose, short course of systemic dexamethasone (MoMdScDX); and 17, placebo. C, The forest plot shows the risk ratio (RR) relative to placebo. CrI indicates credible interval; RR, risk ratio.
In excluding RCTs that enrolled neonates on noninvasive respiratory support, we found that the results for the primary outcome were similar to those of the primary analysis. When RCTs with antenatal corticosteroid coverage of less than 70% were excluded, only ITBUD showed a significant decrease in the incidence of the primary outcome (RR, 0.64; 95% CrI, 0.44-0.89) (eFigures 59-61 in the Supplement).
The results for the primary outcome were similar to those of the primary analysis when RCTs that evaluated ITBUD were excluded. When trials with a high risk of bias were excluded, the network estimates for both EHC (RR, 0.75; 95% CrI, 0.53-1.01) and EIFLUT (RR, 0.84; 95% CrI, 0.67-1.02) compared with placebo did not show any significant decrease in the mortality or BPD at a PMA of 36 weeks (eFigures 62-64 in the Supplement).
By combining the different types of inhaled corticosteroids, we found that early-initiated inhaled corticosteroid was associated with a decreased risk of the primary outcome measure when compared with placebo (RR, 0.81; 95% CrI, 0.69-0.94). All of the other results for different comparisons were similar to those of the primary analysis (eFigures 65-67 in the Supplement).
Discussion
This systematic review and network meta-analysis included 62 RCTs that evaluated the outcomes and safety of different regimens of PNCs administered through various routes (systemic, inhaled, and intratracheal). The primary outcome measure was the combined outcome of BPD or mortality at a PMA of 36 weeks.
These results indicate that moderately early initiation (8-14 days of postnatal age) of systemic dexamethasone with a medium cumulative dose (2-4 mg/kg) appeared to be the most successful intervention in preventing mortality or BPD. In contrast, Zeng et al20 in their network meta-analysis found the early initiation (<8 days) of systemic dexamethasone in a high dose (>3 mg/kg/d) to be the most successful in preventing BPD at 36 weeks. Substantial differences exist between the present network meta-analysis and that of Zeng et al.20 First, we excluded studies that had evaluated early systemic dexamethasone because this therapy is unanimously touted as an unsafe intervention by different academic bodies and by authors of several systematic reviews.7,8,10,94 Second, the interventions that we evaluated were different with the addition of LHC and ITBUD, as well as splitting inhaled corticosteroids (EIBUD, EIBEC, EIFLUT, LIBEC, and LIBUD) and subdividing systemic dexamethasone into different regimens based on a previously published Cochrane review.14 Third, although Zeng et al20 had evaluated safety by assessing cerebral palsy alone, we assessed 11 short- and long-term adverse effects. Fourth, we included 25 trials28,29,30,31,32,33,34,36,37,40,41,43,49,52,53,54,57,58,62,72,75,78,80,82,83 that were not evaluated by Zeng et al20 because of the different inclusion criteria.
The 2020 Canadian Paediatric Society recommendation advises initiating systemic dexamethasone at a dose of 0.15 to 0.2 mg/kg/d for a total duration of 7 to10 days in preterm neonates who require continued invasive mechanical ventilation beyond the first week of life.12 In keeping with this recommendation, our findings also suggested that moderately early initiation (8-14 days) of dexamethasone is better than late initiation (>14 days). However, the cumulative dose suggested by the Canadian Paediatric Society is anywhere between 1 and 2 mg/kg, whereas findings in the present study favored a dose of 2 to 4 mg/kg. The 2020 Canadian Paediatric Society recommendation relied on evidence from pairwise meta-analyses. In addition, a guidelines panel takes into consideration multiple other parameters when moving from evidence to recommendation, such as clinician and parental preference, adverse effects profile, and cost-benefit ratio.95
In this study, the quality of evidence for MoMdDX or MoLdDX compared with placebo was low, implying that the true effect (or the reality, as defined by the GRADE group) might be substantially different from the estimated outcome. Risk of bias and imprecision were the reasons for downgrading the quality of evidence for MoMdDX vs placebo. The sensitivity analysis that evaluated the duration of dexamethasone course indicated that a moderately early-initiated, medium dose, and short course (<8 days) of systemic dexamethasone might be the best intervention. A short course has also been advocated in the 2019 update of the European Consensus Guidelines on the Management of Respiratory Distress Syndrome.11
Of the different regimens with late initiation, only LaHdDX was associated with a significant decrease in risk of the primary outcome. Although LaLdDX appeared to be a good intervention to facilitate extubation, it did not translate into better clinical outcomes (GRADE: low). Thus, late initiation might warrant a relatively high dose for a better outcome than moderately early initiation. In their prediction model of the various risk factors of BPD, Laughon et al96 concluded that, with advancing age, the risk of BPD of all severity increased with continued mechanical ventilation. This risk might be secondary to the ongoing pulmonary inflammation from a ventilator-induced lung injury and hence requiring a higher dose of systemic dexamethasone in the third rather than the second week of life. This analysis of long-term outcomes indicated that none of the interventions were associated with an increased risk of NDI when compared with placebo (GRADE: low). We also found that LaHdDX had a lower incidence of NDI compared with LaMdDX. In a sparse network, the evidence was derived from a single study published 3 decades ago, and the overall quality of evidence was judged to be low.63
This study showed that, although LHC did not have any benefits for short-term outcomes, EHC had a decreased risk of the combined outcome of BPD or mortality at 36 weeks that was attributable to a decreased risk of mortality. These findings are in agreement with the 2010 American Academy of Paediatrics and 2020 Canadian Paediatric Society policy statements.10,12 In addition, EHC was associated with higher rates of gastrointestinal perforation. It was suggested that this increased risk of perforation was associated with concomitant indomethacin use.12 The present analysis also indicated that EIFLUT might be associated with a decreased risk of mortality or BPD. Moderate-quality evidence points toward a decreased risk of BPD at a PMA of 36 weeks associated with EIBUD. However, EIBUD was not found to have a lower risk of the competing outcome of BPD or mortality at a PMA of 36 weeks. The possibility of this finding being associated with an increase in the risk of mortality could not be ruled out.
In the present analysis, ITBUD appeared to be beneficial, a finding that is in sync with other pairwise meta-analyses.15,16 However, intratracheal budesonide is used very early in postnatal life during the window of surfactant administration, when a higher proportion of the neonates are successfully extubated. Further studies are warranted to investigate this intervention’s benefits in neonates who remain ventilated beyond the first week of life.
Limitations
This study has several limitations. Most of the included RCTs had used open-label dexamethasone. Analysis of some of the postnatal systemic dexamethasone regimens (pulse, individualized, or based on daily dose) could not be performed. We could not conduct a meta-regression analysis similar to that of Doyle et al97 by assessing neonates according to their baseline risk of BPD. Some of the networks assessing the safety outcomes were sparse, with low to very low quality of evidence.
Conclusions
Although it presents a risk of hypertension, a moderately early-initiated (8-14 days), medium cumulative dose (2-4 mg/kg), short course (<8 days) of systemic dexamethasone might be the most appropriate PNC regimen for preventing the risk of BPD or mortality at PMA of 36 weeks, with a low quality of evidence. In view of this low confidence in the evidence, the successful outcome and safety of this regimen need to be confirmed by an adequately powered multicentric RCT.
Neither a moderately early-initiated nor late-initiated low dose of systemic dexamethasone (<2 mg/kg) appeared successful in decreasing the risk of BPD or mortality at a PMA of 36 weeks, with a low quality of evidence.
EHC might confer a survival advantage, with a moderate quality of evidence. EIFLUT might be a better alternative to EIBUD, especially in lieu of the possibility of increased risk of mortality with EIBUD, with a moderate quality of evidence. Although ITBUD appeared to be a good intervention with a low quality of evidence, further research is warranted in neonates who require continued mechanical ventilation beyond the first week of life.
eFigure 1. Literature Search/PRISMA Flow
eFigure 2. Mean Gestational Age of the Enrolled Neonates
eFigure 3. Risk of Bias Summary and Graph of the Included Trials
eFigure 4. Direct Evidence from the Pair Wise Comparisons for the Primary Outcome BPD or Mortality at 36 Weeks’ PMA
eFigure 5. Split Between Direct and Indirect Evidence for the Primary Outcome BPD or Mortality at 36 Weeks’ PMA
eFigure 6. Network Plot for BPD at 36 Weeks’ PMA (A), SUCRA Plot with SUCRA Values (%) for BPD at 36 Weeks’ PMA (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for BPD at 36 Weeks’ PMA (C)
eFigure 7. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for BPD at 36 Weeks’ PMA
eFigure 8. Direct Evidence from the Pair Wise Comparisons for BPD at 36 Weeks’ PMA
eFigure 9. Split Between Direct and Indirect Evidence for BPD at 36 Weeks’ PMA
eFigure 10. Network Plot for BPD at 28 Days (A), SUCRA Plot with SUCRA Values (%) for BPD at 28 Days (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for BPD at 28 Days (C)
eFigure 11. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for BPD at 28 Days
eFigure 12. Direct Evidence from the Pair Wise Comparisons for BPD at 28 Days
eFigure 13. Split Between Direct and Indirect Evidence for BPD at 28 Days
eFigure 14. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for Mortality (C)
eFigure 15. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Mortality
eFigure 16. Direct Evidence from the Pair Wise Comparisons for Mortality
eFigure 17. Split Between Direct and Indirect Evidence for Mortality
eFigure 18. Network Plot for BPD (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for Successful Extubation (C)
eFigure 19. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Successful Extubation
eFigure 20. Direct Evidence from the Pair Wise Comparisons for Successful Extubation
eFigure 21. Split Between Direct and Indirect Evidence for Successful Extubation
eFigure 22. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for NDI at 18-24 Months (C)
eFigure 23. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for NDI at 18-24 Months
eFigure 24. Direct Evidence from the Pair Wise Comparisons for NDI at 18-24 Months
eFigure 25. Split Between Direct and Indirect Evidence for NDI at 18-24 Months
eFigure 26. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for GI Perforation (C)
eFigure 27. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for GI Perforation
eFigure 28. Direct Evidence from the Pair Wise Comparisons for GI Perforation
eFigure 29. Split Between Direct and Indirect Evidence for GI Perforation
eFigure 30. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for Hypertrophic Cardiomyopathy (C)
eFigure 31. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Hypertrophic Cardiomyopathy
eFigure 32. Direct Evidence from the Pair Wise Comparisons for Hypertrophic Cardiomyopathy
eFigure 33. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for Hypertension (C)
eFigure 34. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Hypertension
eFigure 35. Direct Evidence from the Pair Wise Comparisons for Hypertension
eFigure 36. Split Between Direct and Indirect Evidence for Hypertension
eFigure 37. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for Sepsis (C)
eFigure 38. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Sepsis
eFigure 39. Direct Evidence from the Pair Wise Comparisons for Sepsis
eFigure 40. Split Between Direct and Indirect Evidence for Sepsis
eFigure 41. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for Severe ROP (C)
eFigure 42. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Severe ROP
eFigure 43. Direct Evidence from the Pair Wise Comparisons for Severe ROP
eFigure 44. Split Between Direct and Indirect Evidence for Severe ROP
eFigure 45. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for NEC (C)
eFigure 46. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for NEC
eFigure 47. Direct Evidence from the Pair Wise Comparisons for NEC
eFigure 48. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for IVH >II (C)
eFigure 49. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for IVH >II
eFigure 50. Direct Evidence from the Pair Wise Comparisons for IVH >II
eFigure 51. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for PVL (C)
eFigure 52. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for PVL
eFigure 53. Direct Evidence from the Pair Wise Comparisons for PVL
eFigure 54. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for CP (C)
eFigure 55. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for CP
eFigure 56. Direct Evidence from the Pair Wise Comparisons for CP
eFigure 57. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Sensitivity Analysis - Duration of Course of Dexamethasone
eFigure 58. Split Between Direct and Indirect Evidence for Duration of Course of Dexamethasone
eFigure 59. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for Sensitivity Analysis Excluding Trials with Antenatal Corticosteroid Coverage <70% (C)
eFigure 60. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Sensitivity Analysis Excluding Trials with Antenatal Corticosteroid Coverage <70%
eFigure 61. Split Between Direct and Indirect Evidence for Sensitivity Analysis Excluding Trials with Antenatal Corticosteroid Coverage <70%
eFigure 62. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for Sensitivity Analysis by Excluding Trials with High Risk of Bias (C)
eFigure 63. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Sensitivity Analysis by Excluding Trials with High Risk of Bias
eFigure 64. Split Between Direct and Indirect Evidence for Sensitivity Analysis by Excluding Trials with High Risk of Bias
eFigure 65. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for Sensitivity Analysis by Combining Different Types of Inhaled Corticosteroids (C)
eFigure 66. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Sensitivity Analysis by Combining Different Types of Inhaled Corticosteroids
eFigure 67. Split Between Direct and Indirect Evidence for Sensitivity Analysis by Combining Different Types of Inhaled Corticosteroids
eTable 1. Literature Search Strategy for Two Electronic Databases
eTable 2. Some of the Studies That Were Excluded for Valid Reasons
eTable 3. Network Characteristics for All the Outcomes and Sensitivity Analysis
eTable 4. GRADE/Quality of Evidence for Some of the Secondary Outcomes
References
- 1.Doyle LW, Anderson PJ. Long-term outcomes of bronchopulmonary dysplasia. Semin Fetal Neonatal Med. 2009;14(6):391-395. doi: 10.1016/j.siny.2009.08.004 [DOI] [PubMed] [Google Scholar]
- 2.Doyle LW, Carse E, Adams AM, Ranganathan S, Opie G, Cheong JLY; Victorian Infant Collaborative Study Group . Ventilation in extremely preterm infants and respiratory function at 8 years. N Engl J Med. 2017;377(4):329-337. doi: 10.1056/NEJMoa1700827 [DOI] [PubMed] [Google Scholar]
- 3.Schmidt B, Asztalos EV, Roberts RS, Robertson CM, Sauve RS, Whitfield MF; Trial of Indomethacin Prophylaxis in Preterms (TIPP) Investigators . Impact of bronchopulmonary dysplasia, brain injury, and severe retinopathy on the outcome of extremely low-birth-weight infants at 18 months: results from the Trial of Indomethacin Prophylaxis in Preterms. JAMA. 2003;289(9):1124-1129. doi: 10.1001/jama.289.9.1124 [DOI] [PubMed] [Google Scholar]
- 4.Kalikkot Thekkeveedu R, Guaman MC, Shivanna B. Bronchopulmonary dysplasia: a review of pathogenesis and pathophysiology. Respir Med. 2017;132:170-177. doi: 10.1016/j.rmed.2017.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Higgins RD, Jobe AH, Koso-Thomas M, et al. Bronchopulmonary dysplasia: executive summary of a workshop. J Pediatr. 2018;197:300-308. doi: 10.1016/j.jpeds.2018.01.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jobe AH. Postnatal corticosteroids for bronchopulmonary dysplasia. Clin Perinatol. 2009;36(1):177-188. doi: 10.1016/j.clp.2008.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barrington KJ. The adverse neuro-developmental effects of postnatal steroids in the preterm infant: a systematic review of RCTs. BMC Pediatr. 2001;1:1. doi: 10.1186/1471-2431-1-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nuytten A, Behal H, Duhamel A, et al. ; EPICE (Effective Perinatal Intensive Care in Europe) Research Group . Correction: evidence-based neonatal unit practices and determinants of postnatal corticosteroid-use in preterm births below 30 weeks GA in Europe: a population-based cohort study. PLoS One. 2017;12(2):e0172408. doi: 10.1371/journal.pone.0172408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gortner L, Misselwitz B, Milligan D, et al. ; Members of the MOSAIC Research Group . Rates of bronchopulmonary dysplasia in very preterm neonates in Europe: results from the MOSAIC cohort. Neonatology. 2011;99(2):112-117. doi: 10.1159/000313024 [DOI] [PubMed] [Google Scholar]
- 10.Watterberg KL; American Academy of Pediatrics, Committee on Fetus and Newborn . Policy statement—postnatal corticosteroids to prevent or treat bronchopulmonary dysplasia. Pediatrics. 2010;126(4):800-808. doi: 10.1542/peds.2010-1534 [DOI] [PubMed] [Google Scholar]
- 11.Sweet DG, Carnielli V, Greisen G, et al. European consensus guidelines on the management of respiratory distress syndrome - 2019 update. Neonatology. 2019;115(4):432-450. doi: 10.1159/000499361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lemyre B, Dunn M, Thebaud B. Postnatal corticosteroids to prevent or treat bronchopulmonary dysplasia in preterm infants. Paediatr Child Health. 2020;25(5):322-331. doi: 10.1093/pch/pxaa073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shinwell ES, Portnov I, Meerpohl JJ, Karen T, Bassler D. Inhaled corticosteroids for bronchopulmonary dysplasia: a meta-analysis. Pediatrics. 2016;138(6):e20162511. doi: 10.1542/peds.2016-2511 [DOI] [PubMed] [Google Scholar]
- 14.Onland W, De Jaegere AP, Offringa M, van Kaam A. Systemic corticosteroid regimens for prevention of bronchopulmonary dysplasia in preterm infants. Cochrane Database Syst Rev. 2017;1(1):CD010941. doi: 10.1002/14651858.CD010941.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Delara M, Chauhan BF, Le ML, Abou-Setta AM, Zarychanski R, 'tJong GW. Efficacy and safety of pulmonary application of corticosteroids in preterm infants with respiratory distress syndrome: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2019;104(2):F137-F144. doi: 10.1136/archdischild-2017-314046 [DOI] [PubMed] [Google Scholar]
- 16.Zhong YY, Li JC, Liu YL, et al. ; Intratracheal Administration of Corticosteroid and Pulmonary Surfactant for Preventing Bronchopulmonary Dysplasia in Preterm Infants With Neonatal Respiratory Distress Syndrome . Early intratracheal administration of corticosteroid and pulmonary surfactant for preventing bronchopulmonary dysplasia in preterm infants with neonatal respiratory distress syndrome: a meta-analysis. Curr Med Sci. 2019;39(3):493-499. doi: 10.1007/s11596-019-2064-9 [DOI] [PubMed] [Google Scholar]
- 17.Shah SS, Ohlsson A, Halliday HL, Shah VS. Inhaled versus systemic corticosteroids for preventing bronchopulmonary dysplasia in ventilated very low birth weight preterm neonates. Cochrane Database Syst Rev. 2017;10(10):CD002058. doi: 10.1002/14651858.CD002058.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Onland W, Offringa M, van Kaam A. Late (≥ 7 days) inhalation corticosteroids to reduce bronchopulmonary dysplasia in preterm infants. Cochrane Database Syst Rev. 2017;8(8):CD002311. doi: 10.1002/14651858.CD002311.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dias S, Caldwell DM. Network meta-analysis explained. Arch Dis Child Fetal Neonatal Ed. 2019;104(1):F8-F12. doi: 10.1136/archdischild-2018-315224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zeng L, Tian J, Song F, et al. Corticosteroids for the prevention of bronchopulmonary dysplasia in preterm infants: a network meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2018;103(6):F506-F511. doi: 10.1136/archdischild-2017-313759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ramaswamy VV, Bandyopadhyay T, Nanda D, et al. Efficacy and safety of postnatal corticosteroids for the prevention of bronchopulmonary dysplasia in preterm neonates: systematic review and network meta-analysis. Accessed September 8, 2020. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020205685 [DOI] [PMC free article] [PubMed]
- 22.Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777-784. doi: 10.7326/M14-2385 [DOI] [PubMed] [Google Scholar]
- 23.Dimitriou G, Greenough A, Giffin FJ, Kavadia V. Inhaled versus systemic steroids in chronic oxygen dependency of preterm infants. Eur J Pediatr. 1997;156(1):51-55. doi: 10.1007/s004310050552 [DOI] [PubMed] [Google Scholar]
- 24.Halliday HL, Patterson CC, Halahakoon CW; European Multicenter Steroid Study Group . A multicenter, randomized Open Study of Early Corticosteroid Treatment (OSECT) in preterm infants with respiratory illness: comparison of early and late treatment and of dexamethasone and inhaled budesonide. Pediatrics. 2001;107(2):232-240. doi: 10.1542/peds.107.2.232 [DOI] [PubMed] [Google Scholar]
- 25.Cole CH, Colton T, Shah BL, et al. Early inhaled glucocorticoid therapy to prevent bronchopulmonary dysplasia. N Engl J Med. 1999;340(13):1005-1010. doi: 10.1056/NEJM199904013401304 [DOI] [PubMed] [Google Scholar]
- 26.Zimmerman JJ, Gabbert D, Shivpuri C, Kayata S, Miller J, Ciesielski W. Meter-dosed, inhaled beclomethasone initiated at birth to prevent bronchopulmonary dysplasia. Pediatr Crit Care Med. 2000;1(2):140-145. doi: 10.1097/00130478-200010000-00009 [DOI] [PubMed] [Google Scholar]
- 27.Jangaard KA, Stinson DA, Allen AC, Vincer MJ. Early prophylactic inhaled beclomethasone in infants less than 1250 g for the prevention of chronic lung disease. Paediatr Child Health. 2002;7(1):13-19. doi: 10.1093/pch/7.1.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lin YJ, Lin HC, Lin CH, Su BH, Yeh TF. Early endotracheal instillation of budesonide (B) for prevention of CLD in preterm infant with RDS-a double blind clinical trial. Ped Res. 2001;21:278A. [Google Scholar]
- 29.Yeh TF, Lin HC, Chang CH, et al. Early intratracheal instillation of budesonide using surfactant as a vehicle to prevent chronic lung disease in preterm infants: a pilot study. Pediatrics. 2008;121(5):e1310-e1318. doi: 10.1542/peds.2007-1973 [DOI] [PubMed] [Google Scholar]
- 30.Kuo HT, Lin HC, Tsai CH, Chouc IC, Yeh TF. A follow-up study of preterm infants given budesonide using surfactant as a vehicle to prevent chronic lung disease in preterm infants. J Pediatr. 2010;156(4):537-541. doi: 10.1016/j.jpeds.2009.10.049 [DOI] [PubMed] [Google Scholar]
- 31.Yeh TF, Chen CM, Wu SY, et al. Intratracheal administration of budesonide/surfactant to prevent bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2016;193(1):86-95. doi: 10.1164/rccm.201505-0861OC [DOI] [PubMed] [Google Scholar]
- 32.Ke H, Li ZK, Yu XP, Guo JZ. Efficacy of different preparations of budesonide combined with pulmonary surfactant in the treatment of neonatal respiratory distress syndrome: a comparative analysis [in Chinese]. Zhongguo Dang Dai Er Ke Za Zhi. 2016;18(5):400-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pan J, Chen MW, Ni WQ, et al. Clinical efficacy of pulmonary surfactant combined with budesonide for preventing bronchopulmonary dysplasia in very low birth weight infants [in Chinese]. Zhongguo Dang Dai Er Ke Za Zhi. 2017;19(2):137-141. doi: 10.7499/j.issn.1008-8830.2017.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Merz U, Kusenbach G, Häusler M, Peschgens T, Hörnchen H. Inhaled budesonide in ventilator-dependent preterm infants: a randomized, double-blind pilot study. Biol Neonate. 1999;75(1):46-53. doi: 10.1159/000014076 [DOI] [PubMed] [Google Scholar]
- 35.Bassler D, Plavka R, Shinwell ES, et al. ; NEUROSIS Trial Group . Early inhaled budesonide for the prevention of bronchopulmonary dysplasia. N Engl J Med. 2015;373(16):1497-1506. doi: 10.1056/NEJMoa1501917 [DOI] [PubMed] [Google Scholar]
- 36.Bassler D, Shinwell ES, Hallman M, et al. ; Neonatal European Study of Inhaled Steroids Trial Group . Long-term effects of inhaled budesonide for bronchopulmonary dysplasia. N Engl J Med. 2018;378(2):148-157. doi: 10.1056/NEJMoa1708831 [DOI] [PubMed] [Google Scholar]
- 37.Sadeghnia A, Beheshti BK, Mohammadizadeh M. The effect of inhaled budesonide on the prevention of chronic lung disease in premature neonates with respiratory distress syndrome. Int J Prev Med. 2018;9:15. doi: 10.4103/ijpvm.IJPVM_336_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cao YY, Yao G, Wang Y, et al. Aerosol inhalation of budesonide and pulmonary surfactant to prevent bronchopulmonary dysplasia. J Pediatr Pharmacy. 2018;24(03):25-29. [Google Scholar]
- 39.Fok TF, Lam K, Dolovich M, et al. Randomised controlled study of early use of inhaled corticosteroid in preterm infants with respiratory distress syndrome. Arch Dis Child Fetal Neonatal Ed. 1999;80(3):F203-F208. doi: 10.1136/fn.80.3.F203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yong WSC, Carney S, Pearse RG, Gibson AT. The effect of inhaled fluticasone propionate (FP) on premature babies at risk for developing chronic lung disease of prematurity. Arch Dis Child Fetal Neonatal Ed. 1999;80:G64. [Google Scholar]
- 41.Nakamura T, Yonemoto N, Nakayama M, et al. ; The Neonatal Research Network, Japan . Early inhaled steroid use in extremely low birthweight infants: a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed. 2016;101(6):F552-F556. doi: 10.1136/archdischild-2015-309943 [DOI] [PubMed] [Google Scholar]
- 42.Watterberg KL, Gerdes JS, Gifford KL, Lin HM. Prophylaxis against early adrenal insufficiency to prevent chronic lung disease in premature infants. Pediatrics. 1999;104(6):1258-1263. doi: 10.1542/peds.104.6.1258 [DOI] [PubMed] [Google Scholar]
- 43.Efird MM, Heerens AT, Gordon PV, Bose CL, Young DA. A randomized-controlled trial of prophylactic hydrocortisone supplementation for the prevention of hypotension in extremely low birth weight infants. J Perinatol. 2005;25(2):119-124. doi: 10.1038/sj.jp.7211193 [DOI] [PubMed] [Google Scholar]
- 44.Watterberg KL, Gerdes JS, Cole CH, et al. Prophylaxis of early adrenal insufficiency to prevent bronchopulmonary dysplasia: a multicenter trial. Pediatrics. 2004;114(6):1649-1657. doi: 10.1542/peds.2004-1159 [DOI] [PubMed] [Google Scholar]
- 45.Watterberg KL, Shaffer ML, Mishefske MJ, et al. Growth and neurodevelopmental outcomes after early low-dose hydrocortisone treatment in extremely low birth weight infants. Pediatrics. 2007;120(1):40-48. doi: 10.1542/peds.2006-3158 [DOI] [PubMed] [Google Scholar]
- 46.Peltoniemi O, Kari MA, Heinonen K, et al. Pretreatment cortisol values may predict responses to hydrocortisone administration for the prevention of bronchopulmonary dysplasia in high-risk infants. J Pediatr. 2005;146(5):632-637. doi: 10.1016/j.jpeds.2004.12.040 [DOI] [PubMed] [Google Scholar]
- 47.Peltoniemi OM, Lano A, Puosi R, et al. ; Neonatal Hydrocortisone Working Group . Trial of early neonatal hydrocortisone: two-year follow-up. Neonatology. 2009;95(3):240-247. doi: 10.1159/000164150 [DOI] [PubMed] [Google Scholar]
- 48.Bonsante F, Latorre G, Iacobelli S, et al. Early low-dose hydrocortisone in very preterm infants: a randomized, placebo-controlled trial. Neonatology. 2007;91(4):217-221. doi: 10.1159/000098168 [DOI] [PubMed] [Google Scholar]
- 49.Ng PC, Lee CH, Bnur FL, et al. A double-blind, randomized, controlled study of a “stress dose” of hydrocortisone for rescue treatment of refractory hypotension in preterm infants. Pediatrics. 2006;117(2):367-375. doi: 10.1542/peds.2005-0869 [DOI] [PubMed] [Google Scholar]
- 50.Hochwald O, Palegra G, Osiovich H. Adding hydrocortisone as 1st line of inotropic treatment for hypotension in very low birth weight infants. Indian J Pediatr. 2014;81(8):808-810. doi: 10.1007/s12098-013-1151-3 [DOI] [PubMed] [Google Scholar]
- 51.Baud O, Maury L, Lebail F, et al. ; PREMILOC Trial Study Group . Effect of early low-dose hydrocortisone on survival without bronchopulmonary dysplasia in extremely preterm infants (PREMILOC): a double-blind, placebo-controlled, multicentre, randomised trial. Lancet. 2016;387(10030):1827-1836. doi: 10.1016/S0140-6736(16)00202-6 [DOI] [PubMed] [Google Scholar]
- 52.Baud O, Trousson C, Biran V, Leroy E, Mohamed D, Alberti C; PREMILOC Trial Group . Two-year neurodevelopmental outcomes of extremely preterm infants treated with early hydrocortisone: treatment effect according to gestational age at birth. Arch Dis Child Fetal Neonatal Ed. 2019;104(1):F30-F35. doi: 10.1136/archdischild-2017-313756 [DOI] [PubMed] [Google Scholar]
- 53.LaForce WR, Brudno DS. Controlled trial of beclomethasone dipropionate by nebulization in oxygen- and ventilator-dependent infants. J Pediatr. 1993;122(2):285-288. doi: 10.1016/S0022-3476(06)80134-4 [DOI] [PubMed] [Google Scholar]
- 54.Giep T, Raibble P, Zuerlein T, Schwartz ID. Trial of beclomethasone dipropionate by metered-dose inhaler in ventilator-dependent neonates less than 1500 grams. Am J Perinatol. 1996;13(1):5-9. doi: 10.1055/s-2007-994193 [DOI] [PubMed] [Google Scholar]
- 55.Denjean A, Paris-Llado J, Zupan V, et al. Inhaled salbutamol and beclomethasone for preventing broncho-pulmonary dysplasia: a randomised double-blind study. Eur J Pediatr. 1998;157(11):926-931. doi: 10.1007/s004310050969 [DOI] [PubMed] [Google Scholar]
- 56.Suchomski SJ, Cummings JJ. A randomized trial of inhaled versus intravenous steroids in ventilator-dependent preterm infants. J Perinatol. 2002;22(3):196-203. doi: 10.1038/sj.jp.7210705 [DOI] [PubMed] [Google Scholar]
- 57.Rozycki HJ, Byron PR, Elliott GR, Carroll T, Gutcher GR. Randomized controlled trial of three different doses of aerosol beclomethasone versus systemic dexamethasone to promote extubation in ventilated premature infants. Pediatr Pulmonol. 2003;35(5):375-383. doi: 10.1002/ppul.10269 [DOI] [PubMed] [Google Scholar]
- 58.Arnon S, Grigg J, Silverman M. Effectiveness of budesonide aerosol in ventilator-dependent preterm babies: a preliminary report. Pediatr Pulmonol. 1996;21(4):231-235. doi: [DOI] [PubMed] [Google Scholar]
- 59.Jónsson B, Eriksson M, Söder O, Broberger U, Lagercrantz H. Budesonide delivered by dosimetric jet nebulization to preterm very low birthweight infants at high risk for development of chronic lung disease. Acta Paediatr. 2000;89(12):1449-1455. doi: 10.1111/j.1651-2227.2000.tb02775.x [DOI] [PubMed] [Google Scholar]
- 60.Parikh NA, Kennedy KA, Lasky RE, McDavid GE, Tyson JE. Pilot randomized trial of hydrocortisone in ventilator-dependent extremely preterm infants: effects on regional brain volumes. J Pediatr. 2013;162(4):685-690.e1. doi: 10.1016/j.jpeds.2012.09.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Parikh NA, Kennedy KA, Lasky RE, Tyson JE. Neurodevelopmental outcomes of extremely preterm infants randomized to stress dose hydrocortisone. PLoS One. 2015;10(9):e0137051. doi: 10.1371/journal.pone.0137051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Onland W, Cools F, Kroon A, et al. ; STOP-BPD Study Group . Effect of hydrocortisone therapy initiated 7 to 14 days after birth on mortality or bronchopulmonary dysplasia among very preterm infants receiving mechanical ventilation: a randomized clinical trial. JAMA. 2019;321(4):354-363. doi: 10.1001/jama.2018.21443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cummings JJ, D’Eugenio DB, Gross SJ. A controlled trial of dexamethasone in preterm infants at high risk for bronchopulmonary dysplasia. N Engl J Med. 1989;320(23):1505-1510. doi: 10.1056/NEJM198906083202301 [DOI] [PubMed] [Google Scholar]
- 64.Kothadia JM, O’Shea TM, Roberts D, Auringer ST, Weaver RG III, Dillard RG. Randomized placebo-controlled trial of a 42-day tapering course of dexamethasone to reduce the duration of ventilator dependency in very low birth weight infants. Pediatrics. 1999;104(1, pt 1):22-27. doi: 10.1542/peds.104.1.22 [DOI] [PubMed] [Google Scholar]
- 65.Malloy CA, Hilal K, Rizvi Z, Weiss M, Muraskas JK. A prospective, randomized, double-masked trial comparing low dose to conventional dose dexamethasone in neonatal chronic lung disease. Internet J Pediat Neonatol. 2005;5(1):10473. [Google Scholar]
- 66.Doyle LW, Davis PG, Morley CJ, McPhee A, Carlin JB; DART Study Investigators . Low-dose dexamethasone facilitates extubation among chronically ventilator-dependent infants: a multicenter, international, randomized, controlled trial. Pediatrics. 2006;117(1):75-83. doi: 10.1542/peds.2004-2843 [DOI] [PubMed] [Google Scholar]
- 67.Doyle LW, Davis PG, Morley CJ, McPhee A, Carlin JB; DART Study Investigators . Outcome at 2 years of age of infants from the DART study: a multicenter, international, randomized, controlled trial of low-dose dexamethasone. Pediatrics. 2007;119(4):716-721. doi: 10.1542/peds.2006-2806 [DOI] [PubMed] [Google Scholar]
- 68.Kari MA, Heinonen K, Ikonen RS, Koivisto M, Raivio KO. Dexamethasone treatment in preterm infants at risk for bronchopulmonary dysplasia. Arch Dis Child. 1993;68(5 Spec No):566-569. doi: 10.1136/adc.68.5_Spec_No.566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ramanathan R, Siassi B, Sardesai S, deLemos RA. Comparison of two dosage regimens of dexamethasone for early treatment of chronic lung disease in very low birth weight (VLBW). Pediatric Research. 1994;34:250A. [Google Scholar]
- 70.Brozanski BS, Jones JG, Gilmour CH, et al. Effect of pulse dexamethasone therapy on the incidence and severity of chronic lung disease in the very low birth weight infant. J Pediatr. 1995;126(5, pt 1):769-776. doi: 10.1016/S0022-3476(95)70410-8 [DOI] [PubMed] [Google Scholar]
- 71.Durand M, Sardesai S, McEvoy C. Effects of early dexamethasone therapy on pulmonary mechanics and chronic lung disease in very low birth weight infants: a randomized, controlled trial. Pediatrics. 1995;95(4):584-590. [PubMed] [Google Scholar]
- 72.Scott SM, Backstrom C, Bessman S. Effect of five days of dexamethasone therapy on ventilator dependence and adrenocorticotropic hormone-stimulated cortisol concentrations. J Perinatol. 1997;17(1):24-28. [PubMed] [Google Scholar]
- 73.Bloomfield FH, Knight DB, Harding JE. Side effects of 2 different dexamethasone courses for preterm infants at risk of chronic lung disease: a randomized trial. J Pediatr. 1998;133(3):395-400. doi: 10.1016/S0022-3476(98)70277-X [DOI] [PubMed] [Google Scholar]
- 74.Armstrong DL, Penrice J, Bloomfield FH, Knight DB, Dezoete JA, Harding JE. Follow up of a randomised trial of two different courses of dexamethasone for preterm babies at risk of chronic lung disease. Arch Dis Child Fetal Neonatal Ed. 2002;86(2):F102-F107. doi: 10.1136/fn.86.2.F102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kovács L, Davis GM, Faucher D, Papageorgiou A. Efficacy of sequential early systemic and inhaled corticosteroid therapy in the prevention of chronic lung disease of prematurity. Acta Paediatr. 1998;87(7):792-798. doi: 10.1111/j.1651-2227.1998.tb01749.x [DOI] [PubMed] [Google Scholar]
- 76.Romagnoli C, Zecca E, Vento G, De Carolis MP, Papacci P, Tortorolo G. Early postnatal dexamethasone for the prevention of chronic lung disease in high-risk preterm infants. Intensive Care Med. 1999;25(7):717-721. doi: 10.1007/s001340050935 [DOI] [PubMed] [Google Scholar]
- 77.Romagnoli C, Zecca E, Luciano R, Torrioli G, Tortorolo G. A three year follow up of preterm infants after moderately early treatment with dexamethasone. Arch Dis Child Fetal Neonatal Ed. 2002;87(1):F55-F58. doi: 10.1136/fn.87.1.F55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Durand M, Mendoza ME, Tantivit P, Kugelman A, McEvoy C. A randomized trial of moderately early low-dose dexamethasone therapy in very low birth weight infants: dynamic pulmonary mechanics, oxygenation, and ventilation. Pediatrics. 2002;109(2):262-268. doi: 10.1542/peds.109.2.262 [DOI] [PubMed] [Google Scholar]
- 79.Walther FJ, Findlay RD, Durand M. Adrenal suppression and extubation rate after moderately early low-dose dexamethasone therapy in very preterm infants. Early Hum Dev. 2003;74(1):37-45. doi: 10.1016/S0378-3782(03)00082-3 [DOI] [PubMed] [Google Scholar]
- 80.McEvoy C, Bowling S, Williamson K, McGaw P, Durand M. Randomized, double-blinded trial of low-dose dexamethasone: II. functional residual capacity and pulmonary outcome in very low birth weight infants at risk for bronchopulmonary dysplasia. Pediatr Pulmonol. 2004;38(1):55-63. doi: 10.1002/ppul.20037 [DOI] [PubMed] [Google Scholar]
- 81.Odd DE, Armstrong DL, Teele RL, Kuschel CA, Harding JE. A randomized trial of two dexamethasone regimens to reduce side-effects in infants treated for chronic lung disease of prematurity. J Paediatr Child Health. 2004;40(5-6):282-289. doi: 10.1111/j.1440-1754.2004.00364.x [DOI] [PubMed] [Google Scholar]
- 82.Alishiri A, Mosavi SA. Association of postnatal dexamethasone use in the development of retinopathy of prematurity in low birth weight infants. Int Eye Sci. 2015;15(3):386-389. doi: 10.3980/j.issn.1672-5123.2015.3.02 [DOI] [Google Scholar]
- 83.Marr BL, Mettelman BB, Bode MM, Gross SJ. Randomized trial of 42-day compared with 9-day courses of dexamethasone for the treatment of evolving bronchopulmonary dysplasia in extremely preterm infants. J Pediatr. 2019;211:20-26.e1. doi: 10.1016/j.jpeds.2019.04.047 [DOI] [PubMed] [Google Scholar]
- 84.Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92(4):529-534. doi: 10.1016/S0022-3476(78)80282-0 [DOI] [PubMed] [Google Scholar]
- 85.Bell MJ, Ternberg JL, Feigin RD, et al. Neonatal necrotizing enterocolitis: therapeutic decisions based upon clinical staging. Ann Surg. 1978;187(1):1-7. doi: 10.1097/00000658-197801000-00001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.International Committee for the Classification of Retinopathy of Prematurity . The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol. 2005;123(7):991-999. doi: 10.1001/archopht.123.7.991 [DOI] [PubMed] [Google Scholar]
- 87.Higgins JPT, Thomas J, Chandler J, et al, eds. Cochrane Handbook for Systematic Reviews of Interventions. Version 6.0. Updated July 2019. Accessed August 25, 2020. http://www.training.cochrane.org/handbook.
- 88.Puhan MA, Schünemann HJ, Murad MH, et al. ; GRADE Working Group . A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. 2014;349:g5630. doi: 10.1136/bmj.g5630 [DOI] [PubMed] [Google Scholar]
- 89.Shim SR, Kim SJ, Lee J, Rücker G. Network meta-analysis: application and practice using R software. Epidemiol Health. 2019;41:e2019013. doi: 10.4178/epih.e2019013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Béliveau A, Boyne DJ, Slater J, Brenner D, Arora P. BUGSnet: an R package to facilitate the conduct and reporting of bayesian network meta-analyses. BMC Med Res Methodol. 2019;19(1):196. doi: 10.1186/s12874-019-0829-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Brooks S, Gelman A. General methods for monitoring convergence of iterative simulations. J Comput Graph Stat. 1998;7(4):434-455. [Google Scholar]
- 92.Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. 2010;29(7-8):932-944. doi: 10.1002/sim.3767 [DOI] [PubMed] [Google Scholar]
- 93.Mbuagbaw L, Rochwerg B, Jaeschke R, et al. Approaches to interpreting and choosing the best treatments in network meta-analyses. Syst Rev. 2017;6(1):79. doi: 10.1186/s13643-017-0473-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Doyle LW, Cheong JL, Ehrenkranz RA, Halliday HL. Early (< 8 days) systemic postnatal corticosteroids for prevention of bronchopulmonary dysplasia in preterm infants. Cochrane Database Syst Rev. 2017;10(10):CD001146. doi: 10.1002/14651858.CD001146.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Atkins D, Best D, Briss PA, et al. ; GRADE Working Group . Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490. doi: 10.1136/bmj.328.7454.1490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Laughon MM, Langer JC, Bose CL, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network . Prediction of bronchopulmonary dysplasia by postnatal age in extremely premature infants. Am J Respir Crit Care Med. 2011;183(12):1715-1722. doi: 10.1164/rccm.201101-0055OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Doyle LW, Halliday HL, Ehrenkranz RA, Davis PG, Sinclair JC. An update on the impact of postnatal systemic corticosteroids on mortality and cerebral palsy in preterm infants: effect modification by risk of bronchopulmonary dysplasia. J Pediatr. 2014;165(6):1258-1260. doi: 10.1016/j.jpeds.2014.07.049 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Literature Search/PRISMA Flow
eFigure 2. Mean Gestational Age of the Enrolled Neonates
eFigure 3. Risk of Bias Summary and Graph of the Included Trials
eFigure 4. Direct Evidence from the Pair Wise Comparisons for the Primary Outcome BPD or Mortality at 36 Weeks’ PMA
eFigure 5. Split Between Direct and Indirect Evidence for the Primary Outcome BPD or Mortality at 36 Weeks’ PMA
eFigure 6. Network Plot for BPD at 36 Weeks’ PMA (A), SUCRA Plot with SUCRA Values (%) for BPD at 36 Weeks’ PMA (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for BPD at 36 Weeks’ PMA (C)
eFigure 7. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for BPD at 36 Weeks’ PMA
eFigure 8. Direct Evidence from the Pair Wise Comparisons for BPD at 36 Weeks’ PMA
eFigure 9. Split Between Direct and Indirect Evidence for BPD at 36 Weeks’ PMA
eFigure 10. Network Plot for BPD at 28 Days (A), SUCRA Plot with SUCRA Values (%) for BPD at 28 Days (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for BPD at 28 Days (C)
eFigure 11. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for BPD at 28 Days
eFigure 12. Direct Evidence from the Pair Wise Comparisons for BPD at 28 Days
eFigure 13. Split Between Direct and Indirect Evidence for BPD at 28 Days
eFigure 14. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for Mortality (C)
eFigure 15. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Mortality
eFigure 16. Direct Evidence from the Pair Wise Comparisons for Mortality
eFigure 17. Split Between Direct and Indirect Evidence for Mortality
eFigure 18. Network Plot for BPD (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for Successful Extubation (C)
eFigure 19. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Successful Extubation
eFigure 20. Direct Evidence from the Pair Wise Comparisons for Successful Extubation
eFigure 21. Split Between Direct and Indirect Evidence for Successful Extubation
eFigure 22. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for NDI at 18-24 Months (C)
eFigure 23. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for NDI at 18-24 Months
eFigure 24. Direct Evidence from the Pair Wise Comparisons for NDI at 18-24 Months
eFigure 25. Split Between Direct and Indirect Evidence for NDI at 18-24 Months
eFigure 26. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for GI Perforation (C)
eFigure 27. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for GI Perforation
eFigure 28. Direct Evidence from the Pair Wise Comparisons for GI Perforation
eFigure 29. Split Between Direct and Indirect Evidence for GI Perforation
eFigure 30. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for Hypertrophic Cardiomyopathy (C)
eFigure 31. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Hypertrophic Cardiomyopathy
eFigure 32. Direct Evidence from the Pair Wise Comparisons for Hypertrophic Cardiomyopathy
eFigure 33. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for Hypertension (C)
eFigure 34. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Hypertension
eFigure 35. Direct Evidence from the Pair Wise Comparisons for Hypertension
eFigure 36. Split Between Direct and Indirect Evidence for Hypertension
eFigure 37. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for Sepsis (C)
eFigure 38. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Sepsis
eFigure 39. Direct Evidence from the Pair Wise Comparisons for Sepsis
eFigure 40. Split Between Direct and Indirect Evidence for Sepsis
eFigure 41. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for Severe ROP (C)
eFigure 42. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Severe ROP
eFigure 43. Direct Evidence from the Pair Wise Comparisons for Severe ROP
eFigure 44. Split Between Direct and Indirect Evidence for Severe ROP
eFigure 45. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for NEC (C)
eFigure 46. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for NEC
eFigure 47. Direct Evidence from the Pair Wise Comparisons for NEC
eFigure 48. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for IVH >II (C)
eFigure 49. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for IVH >II
eFigure 50. Direct Evidence from the Pair Wise Comparisons for IVH >II
eFigure 51. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for PVL (C)
eFigure 52. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for PVL
eFigure 53. Direct Evidence from the Pair Wise Comparisons for PVL
eFigure 54. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for CP (C)
eFigure 55. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for CP
eFigure 56. Direct Evidence from the Pair Wise Comparisons for CP
eFigure 57. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Sensitivity Analysis - Duration of Course of Dexamethasone
eFigure 58. Split Between Direct and Indirect Evidence for Duration of Course of Dexamethasone
eFigure 59. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for Sensitivity Analysis Excluding Trials with Antenatal Corticosteroid Coverage <70% (C)
eFigure 60. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Sensitivity Analysis Excluding Trials with Antenatal Corticosteroid Coverage <70%
eFigure 61. Split Between Direct and Indirect Evidence for Sensitivity Analysis Excluding Trials with Antenatal Corticosteroid Coverage <70%
eFigure 62. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for Sensitivity Analysis by Excluding Trials with High Risk of Bias (C)
eFigure 63. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Sensitivity Analysis by Excluding Trials with High Risk of Bias
eFigure 64. Split Between Direct and Indirect Evidence for Sensitivity Analysis by Excluding Trials with High Risk of Bias
eFigure 65. Network Plot (A), SUCRA Plot with SUCRA Values (%) (B), and Forest Plot Depicting the Network Estimates [RR (95% CrI)] of the Various Interventions with “Placebo” as the Common Comparator for Sensitivity Analysis by Combining Different Types of Inhaled Corticosteroids (C)
eFigure 66. League Plot Depicting the Network Estimates [RR (95% CrI)] of Postnatal Corticosteroids Comparisons for Sensitivity Analysis by Combining Different Types of Inhaled Corticosteroids
eFigure 67. Split Between Direct and Indirect Evidence for Sensitivity Analysis by Combining Different Types of Inhaled Corticosteroids
eTable 1. Literature Search Strategy for Two Electronic Databases
eTable 2. Some of the Studies That Were Excluded for Valid Reasons
eTable 3. Network Characteristics for All the Outcomes and Sensitivity Analysis
eTable 4. GRADE/Quality of Evidence for Some of the Secondary Outcomes


