Abstract
The International Classification of Diseases–11th revision (ICD-11) classification of personality disorders is the official diagnostic system that is used all over the world, and it has recently been renewed. However, as yet very few data are available on its performance. This study examines the Personality Inventory for ICD-11 (PiCD), which assesses the personality domains of the system, and the Standardized Assessment of Severity of Personality Disorder (SASPD), which determines severity. The Spanish versions of the questionnaires were administered to a community (n = 2,522) and a clinical sample (n = 797). Internal consistency was adequate in the PiCD (α = .75 to .84) but less so in the SASPD (α = .64 and .73). Factor analyses suggested a unidimensional or bidimensional structure for severity, while revealing that the personality trait qualifiers are organized into four factors: negative affectivity, detachment, dissociality, and a bipolar domain of disinhibition–anankastia. The mutual relationships between traits and severity were analyzed, as well as the ability of the whole system to identify clinical subjects. Although further improvements are required, the results generally support the use of the PiCD and the SASPD and help substantiate the new ICD-11 taxonomy that underlies them.
Keywords: personality disorder, personality pathology, ICD-11, severity, PiCD, SASPD
The two main diagnostic systems for personality disorders have started a journey toward an evidence-based dimensional taxonomy. The Diagnostic and Statistical Manual of Mental Disorders–Fifth edition (DSM-5; American Psychiatric Association, 2013) fell far short of this target: The new taxonomic system was left pending until more evidence becomes available, and it still merged dimensions and categories in equal proportions. In contrast, the International Classification of Diseases–11th revision (ICD-11) classification has gone much farther by offering a wholly dimensional system and by discarding traditional categories almost completely (World Health Organization, 2018). The exception is the retention of the borderline specifier, which is not part of the evidence-based model but whose removal was deemed a huge loss by a portion of clinicians (Tyrer et al., 2019). In view of the fact that the ICD is the official diagnostic system in use all over the world, it is surprising that these substantial reforms have not prompted more attention.
The ICD-11 personality disorder taxonomy encompasses a trait part, composed of five domains of personality psychopathology plus the borderline specifier, and a severity part which determines whether the subject is or not disordered. The trait part is based on a broad revision of the literature which identified the main features contributing to personality disturbance (Mulder et al., 2011; Tyrer et al., 2011). These features were finally established as negative affectivity, detachment, dissociality, disinhibition, and anankastia. Although the last two domains are presented separately in the classification, they have generally been conceived in the literature as the two poles of a single construct (Tyrer et al., 2014). The ICD trait part is similar to the DSM-5, except that it does not consider psychoticism as a personality trait. Although there are no official instruments that measure this model, the Personality Inventory for ICD-11 (PiCD) is the first published measure specifically designed for this purpose. The PiCD has shown adequate reliability and structural validity in its original version (Oltmanns & Widiger, 2018, 2019), as well as good concurrent validity with the Big Five, the DSM-5, and other personality psychopathology models (Crego & Widiger, 2019; Oltmanns & Widiger, 2019, 2020; Somma et al., 2020). As for the borderline specifier, it was only recently added and so is not included in most studies, including this one (Reed, 2018).
The severity part consists of a single dimension that qualifies the subject as having a normal personality or as suffering a mild, moderate, or severe personality disorder. That is to say that, in the ICD-11, it is severity that determines personality disorder diagnosis, whereas traits are optional qualifiers with a more secondary role. The idea of a general severity continuum has been under investigation for some time, and its central role in the taxonomy is thought to simplify the diagnostic process and to emphasize the degree of disturbance (Crawford et al., 2011; Tyrer & Johnson, 1996). As of yet, the Standardized Assessment of Severity of Personality Disorder (SASPD) is the only instrument that has been developed to measure this continuum (Olajide et al., 2018). However, this self-reporting tool is more aligned with the initial emphasis of the ICD on harm to others and to occupational roles (Tyrer et al., 2015) than with the DSM-5, in which the focus was on problems with the self and interpersonal bonds. Despite this, the SASPD correlates by between .58 and .73 with measures of DSM-5 level of functioning, indicating significant overlap (Bach & Anderson, 2018; McCabe & Widiger, 2020; Oltmanns & Widiger, 2019), and it has proved capable of predicting expert judgment on personality disorder severity, as well as various measures of well-being and maladaptation (Bach & Anderson, 2018).
Overall, this is an entirely new taxonomy that, as its authors state, “has to be tested critically and thoroughly” (Mulder & Tyrer, 2018, p. 30). However, because of the short time interval since their publication, only a dozen studies are available on the properties of the PiCD or the SASPD, and further evidence is urgently needed. For example, the PiCD has been studied in nonclinical subjects (Carnovale et al., 2020; McCabe & Widiger, 2020; Somma et al., 2020) and in patients assessed via the Internet (Oltmanns & Widiger, 2018, 2019, 2020), and thus additional examination of its reliability and validity in clinical samples is required. The structure of the model also needs closer scrutiny. On the one hand, although domains are allegedly based on the literature (Mulder et al., 2011; Tyrer et al., 2011), they have undergone nontrivial changes since then in their number and nature (Crego & Widiger, 2019; Kleindienst et al., 2017): The early traits “emotional/unstable” and “anxious/dependent” were collapsed into negative affectivity around 2014, disinhibition did not appear until 2015, and borderline was added at the very last moment (Reed, 2018; Tyrer et al., 2014; Tyrer et al., 2015). On the other hand, the original structure (Oltmanns & Widiger, 2018) has only been replicated in students (Carnovale et al., 2020) or using an informant version (Bach et al., 2020), and in no case were five independent domains found. All three studies instead supported a four-factor solution with disinhibition and anankastia located at the opposite poles of a single dimension.
A paucity of data is also true for severity, as the properties of the SASPD have only been studied in one community sample (McCabe & Widiger, 2020) and in a few small or mid-sized clinical samples (Bach & Anderson, 2018; Olajide et al., 2018; Oltmanns & Widiger, 2019). Thus, we do not know whether the SASPD, which seeks to reflect the combined impact of five different traits, really forms a single dimension or in fact forms several. Thus far, neither the only study on its structure (Rek et al., 2019) nor the evidence on its predecessor, the Standardized Assessment of Personality–Abbreviated Scale (Bach et al., 2019), have particularly supported unidimensionality. We also need to test in larger community and clinical samples how far severity overlaps with personality traits, as the evidence available up to now suggests blurred boundaries (McCabe & Widiger, 2020; Oltmanns & Widiger, 2019). It is even unclear whether severity works differently for each trait, and whether measuring severity provides any advantage over simply assessing domains. Finally, the diagnostic utility of the joint trait and severity parts also needs to be tested in studies that directly compare community and clinical samples. In this process, population norms have to be established, and nonarbitrary diagnostic thresholds should be set based on the prediction of maladaptive outcomes (Bagby & Widiger, 2020; Herpertz et al., 2017).
We expect to find a four-factor personality structure with good psychometric properties, and a partly independent, unidimensional severity continuum able to accurately detect participants with mental health problems. Given that validation in other languages and cultures is what gives the classification a truly universal scope, and that only an Italian PiCD (Somma et al., 2020) and a Danish and a German SASPD (Bach & Anderson, 2018; Rek et al., 2019) are available currently, we hope our study will further our knowledge of the ICD-11 system and help make it available to a wider range of researchers.
Method
Participants
The community sample consisted of 2,522 volunteers, 59.2% women, with mean age 39.8 years (SD = 19.0, range 16 to 92). Participants were undergraduates and their relatives and acquaintances recruited from three different universities in Catalonia and Madrid, Spain. They answered anonymously and did not receive any compensation for participating. This sample was representative of the general Spanish population in terms of age (43.4 years; www.ine.es) and level of education: In a subsample of 801 participants, about one third had completed primary and lower secondary education, one quarter upper secondary and post-secondary education, and the remaining 40% tertiary education. The clinical sample consisted of 797 outpatients, 70.7% women, with mean age 41.7 years (SD = 13.6, range 15 to 82). They were consecutively referred to the mental health units of six hospitals in Catalonia, Spain. Patients were clinically diagnosed at their respective centers, with the main diagnoses including mild to moderate affective disorders (37.0%), anxiety or phobic disorder (22.1%), mixed affective and anxious disorder (8.7%), substance-related disorder (8.1%), eating disorder (5.8%), and other disorders (4.3%) each with a frequency below 3%. No categorical diagnoses of personality disorder were made. Based on the proposed cutoffs for the SASPD, calibrated against expert judgment (Olajide et al., 2018), 23.4% of our clinical sample would have at least a mild personality disorder (SASPD ≥ 8), of whom 10.1% would also exceed the threshold for a moderate or severe personality disorder (SASPD ≥ 10). Combined sample size allowed a rate of 55.3 participants per trait in factor analysis. The study was approved by the ethical committees of the respective centers.
Instruments
The PiCD (Oltmanns & Widiger, 2018) is a 60-item self-report measuring the five domains of the dimensional ICD-11 personality model (World Health Organization, 2018): negative affectivity, detachment, dissociality, disinhibition, and anankastia. Each domain has 12 items rated from 1 (strongly disagree) to 5 (strongly agree). The PiCD was translated by three Spanish native speakers who were familiar with the constructs being measured and worked independently. Semantic and conceptual equivalence were given priority throughout the adaptation process. The translators then agreed on a common version, which was blindly back-translated by an English native speaker and compared with the original. Discrepancies were consensually resolved by the translators and the original authors of the instrument. Before final approval, a pilot study was undertaken in 20 participants from the target population to ensure understandability and feasibility. The above procedures followed the standard recommendations for adapting questionnaires (Epstein et al., 2015).
The SASPD (Olajide et al., 2018) was modeled after the Standardized Assessment of Personality–Abbreviated Scale (Moran et al., 2003). Its nine items reflect possible undesired consequences of each of the five ICD-11 domains: Items 4, 6, and 9 are linked to negative affectivity (losing temper, worrying, and feeling helpless); Items 1 and 3 to detachment (avoiding people and lacking friends); Items 2 and 8 to dissociality (distrusting others and being callous); Item 7 to anankastia (being excessively organized); and Item 5 to disinhibition (being impulsive). The translation procedures described above were applied to the SASPD.
Data Analysis
Descriptive statistics for the PiCD and the SASPD were obtained in the clinical and community samples separately. Internal reliability was examined through Cronbach’s alphas (α) and corrected item-scale correlations (ri-s). To determine whether similar amounts of information are provided along the scales, we conducted an item response theory (IRT) analysis using Samejima’s graded response model (Toland, 2014).
The structure of the PiCD was examined at the item level using a range of factor analytical methods in line with current recommendations (Hopwood & Donnellan, 2010; McCrae et al., 1996; Osborne, 2014). Given that the PiCD structure has been defined previously, confirmatory factor analysis (CFA) was conducted first. Model fit was examined through the comparative fit index (CFI), Tucker–Lewis index (TLI), root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR). Values above .95 for CFI and TLI, below .06 for RMSEA, and below .08 for SRMR, were considered a good fit (Brown, 2015). As a significant number of items showed at least moderate skewness (>|1|) or kurtosis (>1), all analyses were based on the polychoric correlation matrix (Flora et al., 2012) and the robust diagonally weighted least squares estimator.
Fit eventually proved to be poor, so we moved on to an exploratory factor analysis (EFA) approach. Solutions with different numbers of factors from one to seven were successively retained. We used the Hull method (Lorenzo-Seva et al., 2011) and parallel analysis based on minimum rank factor analysis (Timmerman & Lorenzo-Seva, 2011) to decide on the most appropriate number of factors. Solutions were rotated to direct oblimin except the four- and five-factor solutions, which were rotated to Procrustes targeted at the previously published solutions (Oltmanns & Widiger, 2018). Additionally, these solutions were independently obtained in two random partitions of the sample, and then used as targets in an exploratory structural equation model (ESEM) analysis to examine fit in a cross-validation design. Target loadings <.10 were freely estimated. In a more demanding design, the same procedure was applied to the community and clinical samples. Replicability between solutions was additionally examined through Tucker’s congruence coefficients (Φ), with Φ ≥ .85 indicating fair similarity and Φ ≥ .95 equivalence (Lorenzo-Seva & ten Berge, 2006).
We examined the mutual relationships between the PiCD domains and the SASPD through Pearson’s correlations (r) and multiple linear regression. We also studied the ability of the PiCD and SASPD to predict in a logistic regression whether the subject belongs to the clinical sample (caseness). Sensitivity (Se) and specificity (Sp) were calculated for the most predictive dimensions, and the best cutoff points were estimated through receiver operating characteristic curves. SPSS 22 was used for all analyses except Factor 10.9.02 (Ferrando & Lorenzo-Seva, 2017) for EFA, and R 3.6.0 (R Core Team, 2018) for IRT analysis (package “ltm”; Rizopoulos, 2006), CFA, and ESEM (package “lavaan”; Rosseel, 2012). We report how we determined our sample size, all data exclusions, all manipulations, and all measures in the study.
Results
Descriptives, Distribution, and Reliability of the PiCD and the SASPD
Descriptive statistics of the PiCD and the SASPD in the community and clinical samples are provided in Table 1. When calculated for each sex (Supplementary Table S1, available online), raw scores in the community sample can be taken as the population norms for computing T scores. Under this metric, the clinical sample was 1 SD above the mean in negative affectivity and the SASPD, around ½ a SD in detachment, disinhibition, and dissociality, and on a par in anankastia. Comparisons with the previous literature suggested that the Spanish population, either clinical or nonclinical, was slightly lower than others in detachment and dissociality, and that our clinical sample was somewhat higher in negative affectivity (Supplementary Figure S1; Supplementary Tables S2 and S3, available online). Distributions of all the scales were within the commonly accepted limits of ±2 regarding skewness and zero-centered kurtosis (frequency distributions in Supplementary Figure S2, available online).
Table 1.
Mean (SD), Distribution Shape, Internal Reliability, Item-Scale Correlations, and Group Differences Between the Community and Clinical Samples.
| Community sample (n = 2,522) |
Clinical sample (n = 797) |
Student’s t |
Cohen’s d | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | Skew | Kurt | α |
r
i-s
|
M | SD | Skew | Kurt | α |
r
i-s
|
t | p | ||||
| M | Range | M | Range | ||||||||||||||
| Negative affectivity | 31.9 | 8.1 | 0.298 | −0.206 | .83 | 0.49 | 0.09-0.69 | 42.3 | 8.4 | −0.313 | −0.391 | .83 | 0.49 | 0.10-0.66 | −31.2 | <.001 | 1.27 |
| Detachment | 25.7 | 7.5 | 0.535 | −0.008 | .82 | 0.48 | 0.10-0.65 | 29.4 | 8.8 | 0.282 | −0.417 | .82 | 0.48 | 0.11-0.63 | −11.8 | <.001 | 0.47 |
| Dissociality | 21.8 | 6.9 | 1.150 | 1.810 | .82 | 0.47 | 0.32-0.64 | 23.8 | 7.5 | 0.560 | 0.136 | .79 | 0.44 | 0.27-0.58 | −7.0 | <.001 | 0.28 |
| Disinhibition | 24.2 | 7.5 | 0.665 | 0.263 | .84 | 0.49 | 0.30-0.62 | 27.8 | 8.5 | 0.902 | 0.607 | .83 | 0.48 | 0.29-0.60 | −11.7 | <.001 | 0.46 |
| Anankastia | 39.5 | 7.2 | −0.208 | 0.074 | .80 | 0.44 | 0.28-0.60 | 40.1 | 7.2 | −0.204 | 0.340 | .75 | 0.39 | 0.24-0.54 | −2.2 | .030 | 0.08 |
| SASPD total | 5.7 | 3.2 | 1.297 | 2.942 | .64 | 0.32 | 0.23-0.42 | 8.8 | 4.4 | 0.681 | 0.179 | .73 | 0.40 | 0.21-0.52 | −21.2 | <.001 | 0.88 |
Note. Skew = skewness; Kurt = zero-centered kurtosis; ri-s = corrected item-scale correlations; SASPD = Standardized Assessment of Severity of Personality Disorder.
The PiCD domains showed acceptable internal reliabilities of α = .80 to .86 in the community and .75 to .83 in the clinical sample. Corrected item-scale (ri-s) correlations were good overall, but reflected the presence of some less consistent items. For example, Item 26 (“Changes in my mood are unrelated to what is happening in my life”) was poorly correlated with its corresponding negative affectivity domain in both samples (ri-s = .09 and .10, respectively; Supplementary Table S4, available online), and Item 23 (“I feel pretty much the same all the time”) showed ri-s = .10 and .11 with detachment. With regard to the SASPD, internal reliability was lower (α = .64 in the community and .73 in the clinical sample, respectively), with Items 5 to 9 showing ri-s below .30 in either sample. Furthermore, 12 items of the PiCD and the SASPD showed skewness and/or kurtosis greater than ±2 (Supplementary Table S4, available online). For the most part, these were items of pathological content that obtained low scores as expected only in the community sample. Four items, however, showed skewed distributions in both samples (PiCD Items 9, 24, and 54, and SASPD Item 8). They all reflected extreme forms of dissociality, such as indifference or amusement about others’ suffering, which were not common in either sample.
Graded response model analyses indicated that the SASPD and three PiCD domains—detachment, dissociality, and disinhibition—provided much more information at higher levels of the latent trait: 62.8% in the upper half versus 28.2% in the lower half, on average (Supplementary Figure S3, available online). By contrast, negative affectivity showed the opposite pattern in the clinical sample, and anankastia in both samples.
Factor Structure of the PiCD
The PiCD domains were not orthogonal, as shown by the Pearson’s intercorrelations in Table 2. In the community sample, the highest associations were between disinhibition and negative affectivity (r = .36), dissociality (.44), and anankastia (−.46). In the clinical sample, the highest correlations were between disinhibition and negative affectivity (.47), detachment (.33), dissociality (.50), and anankastia (−.46), while negative affectivity also correlated with detachment (.36) and dissociality (.33).
Table 2.
Intercorrelations Between the PiCD and the SASPD in the Community (Below the Diagonal, n = 2,522) and the Clinical Sample (Above the Diagonal, n = 797).
| Negative affectivity | Detachment | Dissociality | Disinhibition | Anankastia | PiCD total | SASPD | |
|---|---|---|---|---|---|---|---|
| Negative affectivity | — | .36 ** | .33 ** | .47 ** | .02 | .76 ** | .63 ** |
| Detachment | .21** | — | .23** | .33 ** | .08* | .71 ** | .48 ** |
| Dissociality | .18** | .26** | — | .50 ** | −.14** | .65 ** | .43 ** |
| Disinhibition | .36 ** | .22** | .44 ** | — | −.46** | .65 ** | .49 ** |
| Anankastia | .20** | .15** | −.09* | −.46** | — | .13** | −.13** |
| PiCD total | .71 ** | .66 ** | .61 ** | .56 ** | .28** | — | .66 ** |
| SASPD | .44 ** | .30 ** | .27** | .26** | .02 | .46 ** | — |
Note. Correlations ≥|.30| are in bold type. PiCD = Personality Inventory for ICD-11; SASPD = Standardized Assessment of Severity of Personality Disorder.
p < .05. **p < .01.
The Kaiser–Meyer–Olkin (KMO) index of sampling adequacy was .93 (very good) in the whole sample, and the Bartlett’s test of sphericity was highly significant (69565.9, degrees of freedom = 1,770, p < .001). Given that the PiCD structure had been examined before, CFA was applied first. However, neither the five-factor solution with 12 items per domain nor the previously reported four- and five-factor solutions (Oltmanns & Widiger, 2018) produced an optimal fit: CFI = .77 to .83, TLI = .76 to .82, RMSEA = .10 to .11, and SRMR = .10 to .11. This was also true when the community and the clinical samples were analyzed separately (Supplementary Table S5, available online).
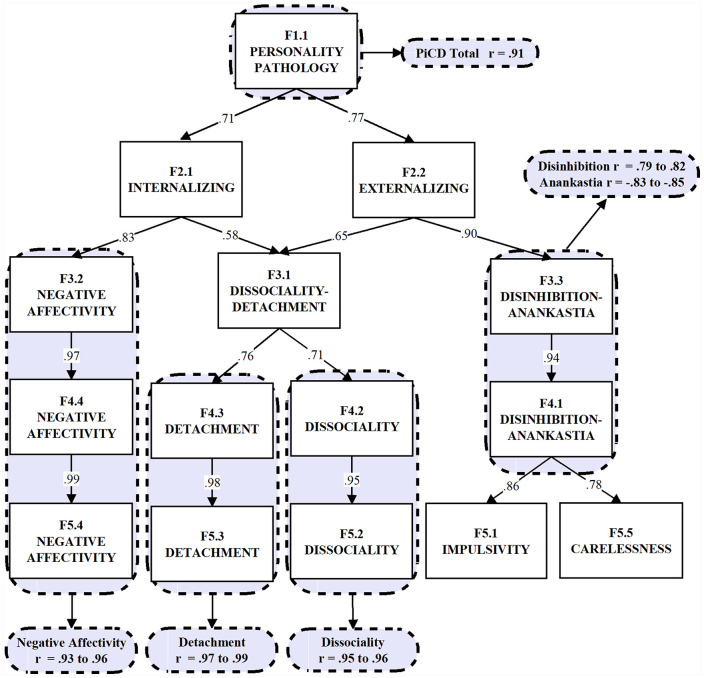
Poor fit is common when applying CFA to personality structures, due to the strict requirement of simple structures and zero cross-loadings (Ferrando & Lorenzo-Seva, 2017; Hopwood & Donnellan, 2010). Therefore, following current recommendations, we applied an EFA approach (McCrae et al., 1996; Osborne, 2014). In order to examine the entire hierarchical structure, solutions with different numbers of factors from one to seven were successively retained and rotated to direct oblimin. The exceptions were the four- and five-factor structures, which underwent Procrustean rotations targeted at the originally published solutions (Tables 6 and S1 in Oltmanns & Widiger, 2018). Hull and parallel tests suggested four and five factors respectively. The four-factor solution (Table 3, left) explained 45% of the variance. The second to fourth factors faithfully reproduced the dissociality, detachment, and negative affectivity domains (r = .95, .97, and .93 respectively), whereas the first factor was a bipolar dimension with disinhibition (.82) and anankastia (−.85) at opposite poles. Absolute intercorrelations between factors ranged from .02 to .36, with mean .23. As for the five-factor solution, the second to fourth factors also reproduced the dissociality, detachment, and negative affectivity domains (r = .96 to .99), but anankastia and disinhibition could not be recovered as separate domains (Table 3, right). Instead, the disinhibition–anankastia factor split into two dimensions which may be called “impulsivity versus caution” and “carelessness versus perfectionism,” and showed a poorer replicability between samples than the bipolar factor (Φ = .93 and .86). Targeting the original structure with 12 items per domain instead of the empirically based solution did not produce different results. Figure 1 represents the complete hierarchical structure from one to five factors and the correspondence of each factor with the five original PiCD domains (one- to three-factor solutions in Supplementary Table S6; correlations in Supplementary Table S7, available online). Additional factors beyond the fifth were moderately replicable but barely interpretable (Supplementary Table S8, available online).
Table 3.
Four- and Five-Factor Solutions of the PiCD in the Whole Sample (N = 3,319).
| Items | Four factors |
Five factors |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| F4.1 | F4.2 | F4.3 | F4.4 | F5.1 | F5.2 | F5.3 | F5.4 | F5.5 | |
| picd15_ak | −.71 | .09 | .25 | −.19 | −.79 | .15 | .00 | −.13 | .00 |
| picd35_ak | −.67 | .33 | −.15 | .25 | −.19 | .22 | .03 | .21 | −.60 |
| picd5_ak | −.66 | .25 | −.08 | .18 | −.26 | .16 | .06 | .16 | −.50 |
| picd55_ak | −.64 | −.14 | .20 | .04 | −.61 | −.13 | .07 | .08 | −.11 |
| picd20_ak | −.61 | .40 | −.09 | .24 | −.16 | .29 | .08 | .21 | −.56 |
| picd45_ak | −.61 | .06 | .22 | .18 | −.65 | .12 | −.01 | .24 | −.02 |
| picd12_dn | .58 | −.12 | .23 | .08 | .05 | .05 | −.08 | .14 | .66 |
| picd7_dn | .53 | .04 | .24 | .06 | .12 | .16 | .02 | .10 | .51 |
| picd27_dn | .53 | −.02 | .18 | .19 | .06 | .14 | −.10 | .24 | .58 |
| picd60_ak | −.53 | −.05 | .15 | −.02 | −.62 | −.01 | −.06 | .04 | −.01 |
| picd47_dn | .50 | .06 | −.09 | .50 | .58 | .04 | .07 | .45 | −.03 |
| picd25_ak | −.47 | −.09 | .28 | .02 | −.60 | −.02 | .04 | .09 | .10 |
| picd32_dn | .46 | .09 | −.11 | .34 | .55 | .06 | .06 | .29 | −.04 |
| picd57_dn | .44 | .00 | .28 | .12 | .06 | .12 | .06 | .16 | .46 |
| picd50_ak | −.44 | .10 | −.26 | .20 | −.20 | .07 | −.20 | .20 | −.32 |
| picd30_ak | −.40 | −.06 | .37 | −.33 | −.65 | .02 | .08 | −.26 | .23 |
| picd42_dn | .36 | .17 | .22 | .04 | −.01 | .29 | −.01 | .08 | .45 |
| picd40_ak | −.31 | .01 | .18 | .22 | −.41 | .08 | −.02 | .27 | .07 |
| picd52_dn | .30 | .30 | .09 | .11 | .15 | .35 | .02 | .12 | .19 |
| picd59_ds | .00 | .78 | −.07 | .00 | .00 | .81 | −.12 | .00 | −.02 |
| picd44_ds | −.06 | .76 | −.05 | .03 | −.06 | .79 | −.12 | .04 | −.02 |
| picd54_ds | .04 | .72 | .18 | −.26 | .02 | .72 | .16 | −.26 | .02 |
| picd14_ds | −.17 | .69 | −.22 | −.02 | −.08 | .70 | −.24 | −.02 | −.13 |
| picd49_ds | −.03 | .68 | −.07 | .05 | −.02 | .70 | −.11 | .05 | −.04 |
| picd19_ds | −.26 | .64 | −.09 | .07 | .00 | .58 | .03 | .04 | −.33 |
| picd34_ds | −.08 | .64 | −.03 | −.07 | −.01 | .63 | −.02 | −.08 | −.10 |
| picd9_ds | .05 | .60 | .18 | −.12 | .00 | .62 | .13 | −.12 | .05 |
| picd39_ds | .00 | .59 | .20 | −.10 | −.04 | .60 | .14 | −.10 | .04 |
| picd24_ds | −.02 | .55 | .27 | −.22 | −.13 | .57 | .17 | −.20 | .11 |
| picd4_ds | .09 | .46 | −.08 | .27 | .18 | .46 | −.03 | .25 | −.10 |
| picd29_ds | .05 | .31 | .01 | .20 | .03 | .34 | −.03 | .20 | .03 |
| picd37_dn | .27 | .31 | .11 | .05 | −.04 | .43 | −.11 | .09 | .37 |
| picd22_dn | .13 | .29 | .25 | .04 | −.02 | .34 | .14 | .06 | .18 |
| picd43_dt | −.07 | −.15 | .75 | .01 | −.04 | −.22 | .81 | .00 | −.02 |
| picd13_dt | −.07 | −.19 | .74 | .07 | −.04 | −.25 | .79 | .06 | −.02 |
| picd33_dt | −.05 | .12 | .68 | .06 | .02 | .06 | .75 | .04 | −.07 |
| picd28_dt | −.07 | −.28 | .67 | .08 | −.07 | −.32 | .69 | .09 | .02 |
| picd58_dt | .01 | −.02 | .63 | .23 | −.01 | −.04 | .63 | .24 | .03 |
| picd3_dt | −.02 | .08 | .57 | .21 | .10 | .01 | .68 | .19 | −.12 |
| picd8_dt | −.06 | .26 | .51 | −.12 | .02 | .20 | .59 | −.14 | −.08 |
| picd38_dt | .04 | .03 | .51 | .17 | −.06 | .05 | .44 | .18 | .12 |
| picd53_dt | .00 | .30 | .47 | −.18 | .01 | .26 | .49 | −.19 | −.00 |
| picd18_dt | .06 | .21 | .45 | .07 | .05 | .19 | .46 | .07 | .03 |
| picd48_dt | .03 | .27 | .39 | −.02 | .10 | .22 | .47 | −.04 | −.06 |
| picd10_ak | −.26 | −.20 | .31 | .04 | −.43 | −.14 | .10 | .09 | .16 |
| picd26_na | .04 | .06 | .25 | .05 | .00 | .06 | .23 | .05 | .05 |
| picd41_na | .06 | −.09 | .13 | .78 | .01 | −.02 | .03 | .80 | .07 |
| picd16_na | −.16 | −.09 | .13 | .76 | −.09 | −.06 | .07 | .77 | −.08 |
| picd56_na | .00 | .07 | .03 | .75 | .05 | .11 | −.01 | .75 | −.05 |
| picd1_na | −.03 | .04 | −.11 | .72 | .11 | .05 | −.07 | .70 | −.16 |
| picd11_na | .05 | .01 | .02 | .72 | .07 | .06 | −.02 | .72 | −.01 |
| picd46_na | .00 | −.14 | .17 | .69 | −.05 | −.08 | .07 | .71 | .06 |
| picd21_na | −.08 | −.13 | .20 | .68 | −.07 | −.09 | .13 | .69 | −.01 |
| picd36_na | −.10 | −.40 | −.17 | .65 | −.10 | −.34 | −.25 | .67 | −.00 |
| picd2_dn | .39 | .11 | −.25 | .61 | .65 | .05 | .01 | .54 | −.24 |
| picd51_na | .08 | −.07 | .25 | .60 | .02 | −.02 | .17 | .61 | .08 |
| picd31_na | .00 | −.09 | .02 | .56 | .08 | −.09 | .05 | .55 | −.08 |
| picd17_dn | .46 | .06 | −.15 | .55 | .62 | .02 | .06 | .49 | −.12 |
| picd6_na | −.39 | .24 | −.05 | .50 | −.15 | .22 | −.02 | .50 | −.30 |
| picd23_dt | −.13 | .08 | .24 | −.39 | −.16 | .06 | .21 | −.37 | .03 |
| McDonald’s ω | .87 | .86 | .85 | .89 | .87 | .85 | .87 | .89 | .68 |
| Φwhole-comm | 1.00 | 1.00 | 1.00 | .99 | .98 | 1.00 | .99 | .99 | .97 |
| Φwhole-clin | .98 | .99 | .99 | .99 | .96 | .99 | .97 | .99 | .94 |
| Φcomm-clin | .97 | .98 | .97 | .97 | .93 | .98 | .94 | .97 | .86 |
| Φwhole-Oltmanns | .82 | .92 | .93 | .95 | .84 | .91 | .91 | .90 | .29 |
| Φwhole-Bach | .94 | .86 | .69 | .67 | .72 | .87 | .92 | .71 | .80 |
| Φwhole-Carnovale | .96 | .89 | .89 | .96 | — | — | — | — | — |
Note. Loadings λ ≥ |.30|, McDonald’s Omega coefficients ω ≥ .70, and Tucker’s coefficients Φ ≥ .95 are in bold type. Items are sorted following the four-factor solution. na = negative affectivity; dt = detachment; ds = dissociality; dn = disinhibition; ak = anankastia; comm = community sample; clin = clinical sample; Oltmanns = Oltmanns and Widiger (2018); Bach = Bach et al. (2019); Carnovale = Carnovale et al. (2020).
Figure 1.
Hierarchical structure of the PiCD.
Note. All between-level correlations ≥.50 are reported. Grey-shaded areas indicate the correspondence with the originally proposed domains. The complete correlation matrix is provided in Supplementary Table S7 (available online). PiCD = Personality Inventory for ICD-11.
To cross-validate the four- and five-factor solutions, EFAs were repeated in two randomly split samples. Each solution was then used as a target for ESEM analysis in the complementary sample. Both the four-factor (CFI = .97, TLI = .97, RMSEA = .05, SRMR = .05) and the five-factor solutions (CFI = .98, TLI = .98, RMSEA = .04, SRMR = .04) showed a good fit. Replicability between samples was also good, with Φ = .99 across the four-factor solution and Φ = .97 to 99 in the five-factor solution. In a more demanding design, the same approach was applied to the community and clinical samples. Both the four- (CFI = .95, TLI = .94 to .95, RMSEA = .06, SRMR = .06, congruence Φ = .96 to .98) and the five-factor solutions (CFI = .97, TLI = .96 to .97, RMSEA = .04 to .05, SRMR = .05, congruence Φ = .90 to .97; Supplementary Table S9, available online) showed acceptable fit and replicability. An additional random-intercept analysis (Carnovale et al., 2020; Maydeu-Olivares & Coffman, 2006), aimed at controlling for acquiescent responding or other biases, barely improved fit. Furthermore, the method factor only explained 6.0% and 4.9% of the variance of the four- and five-factor solutions when added to the CFA models, and 2.5% and 2.6% in the case of ESEM models.
Factor Structure of the SASPD
CFA showed poor fit for the unidimensional structure of the SASPD in the whole sample (CFI = .88, TLI = .84, RMSEA = .12, SRMR = .09; Supplementary Table S5, available online). In the subsequent EFA, the KMO index was .75 indicating mediocre sample adequacy (Kaiser & Rice, 1974), but the Bartlett’s test of sphericity was highly significant (4414.5, degrees of freedom = 36, p < .001). Hull and parallel tests coincided in suggesting a one-factor solution, and only the one- and two-factor solutions showed good replicability between the community and clinical samples (Φ = .96 to .99; Table 4). The former included all items and gave support to a unidimensional construct, whereas the latter separated social maladaptation (dislike of being with others, lacking friends, mistrust, and indifference to other’s feelings) from nonsocial maladaptation (losing temper, acting impulsively, and worrying). However, the structure was problematic in some aspects: Two out of nine items, reflecting orderliness and neediness, did not load on any factor, and ESEM analyses favored two or three factors over one (Supplementary Table S9, available online).
Table 4.
One- to Three-Factor Solutions of the SASPD in the Whole Sample (N = 3,292).
| Items | One factor |
Two factors |
Three factors |
|||
|---|---|---|---|---|---|---|
| F1.1 | F2.1 | F2.2 | F3.1 | F3.2 | F3.3 | |
| saspd1_dt | .68 | .80 | −.01 | .05 | .78 | −.03 |
| saspd2_ds | .62 | .53 | .16 | .06 | .53 | .14 |
| saspd3_dt | .67 | .83 | −.04 | .05 | .81 | −.06 |
| saspd4_na | .62 | .04 | .82 | .06 | .05 | .78 |
| saspd5_dn | .45 | −.08 | .72 | .03 | −.09 | .73 |
| saspd6_na | .44 | .16 | .36 | .98 | .03 | .04 |
| saspd7_ak | .33 | .18 | .21 | .18 | .16 | .12 |
| saspd8_ds | .50 | .43 | .13 | −.29 | .50 | .28 |
| saspd9_na | .35 | .14 | .28 | .10 | .13 | .24 |
| McDonald’s ω | .77 | .75 | .68 | — | .76 | .73 |
| Φwhole-comm | .99 | 1.00 | .98 | .93 | .99 | .97 |
| Φwhole-clin | .99 | .98 | .98 | .99 | .98 | .98 |
| Φcomm-clin | .96 | .97 | .99 | .94 | .96 | .99 |
Note. Loadings λ ≥ |.30|, McDonald’s Omega coefficients ω ≥ .70, and Tucker’s coefficients Φ ≥ .95 are in bold type. na = negative affectivity; dt = detachment; ds = dissociality; dn = disinhibition; ak = anankastia; comm = community sample; clin = clinical sample.
Criterion Validity
Concerning the mutual relationships between personality traits and severity, all PiCD domains significantly correlated with the SASPD, in both the community (range r = .26 to .44) and the clinical samples (.43 to .63). The exception was anankastia, which showed nil (.02) or negative (−.13) correlation with severity respectively (Table 2). When we predicted the SASPD from the PiCD through linear regression, the higher coefficients were found for negative affectivity in both samples (b = .406 and .456, respectively, p < .001; Supplementary Table S10, available online). The contribution of detachment and dissociality was smaller, that of disinhibition was negligible, and anankastia rather acted as a protective factor (−.101 and −.116, respectively, p < .001).
Next, caseness (i.e., belonging to the clinical sample) was used as an external criterion to examine whether severity was able to predict maladaptation better than and beyond personality traits. Although all variables differed to some extent between the community and clinical samples (Table 1, right), only negative affectivity and the SASPD (odds ratio = 1.15 and 1.06, respectively, p < .001) were substantially predictive in logistic regression (Supplementary Table S10, available online). Introducing the disinhibition–anankastia bipolar factor instead of its constituent domains did not change the results, as their maladaptive potential seems marginal in this case. Nor did quadratic terms make any important contribution to the prediction, indicating that the domains are unipolar with regard to maladaptation. Finally, the interactions between traits and severity, represented by the product of each domain multiplied by the SASPD, barely contributed at all to the prediction of caseness when added to the original variables, and did not improve the prediction when used instead of them.
Receiver operating characteristic curves gave similar results (Supplementary Figure S4, available online). Areas under the curve were .81 for negative affectivity and .72 for the SASPD, with all other variables having limited predictive ability. The best cutoffs for these two variables were obtained by applying Youden’s index (Se + Sp − 1 = max). The resulting thresholds were ≥37 for negative affectivity, which gave Se = .76 and Sp = .73, and ≥7 for the SASPD, which gave Se = .66, Sp = .68 (Supplementary Table S10, available online).
Discussion
In this study, we describe Spanish adaptations of the PiCD and the SASPD, which assess the trait and severity parts of the ICD-11 classification of personality disorders, respectively. The PiCD proved to be reliable and showed a consistent factorial structure, whereas the SASPD seems to require some psychometric refinement. Even so, both instruments were able to detect the clinical cases with reasonable accuracy. The general conclusions are that they can be used for diagnosis in clinical settings with due caution, and that the underlying ICD-11 taxonomy is supported. Some points deserve further comment.
During their development both the DSM-5 and the ICD-11 have wavered with regard to whether disinhibition and anankastia should be kept together or apart (Skodol, 2011; Tyrer et al., 2014), but it is the former option which is supported by the evidence (Mulder et al., 2011; Wright et al., 2012). Our results also confirm this view, given that negative affectivity, detachment, and dissociality are reproduced as they appear in the taxonomy, whereas disinhibition and anankastia form the opposite extremes of a single bipolar dimension, resulting in a four-factor structure. The attempt to retain five factors does not bring us any closer to a meaningful five-factor system, because disinhibition and anankastia cannot be recovered as separate domains. Instead, two narrower bipolar domains emerge, reflecting “impulsivity” and “carelessness.” Furthermore, although both models fit the data about equally well in ESEM, the four-factor solution was more congruent between the samples and with the literature: Whereas the bipolar domain of disinhibition–anankastia showed at least partial agreement with prior solutions (Φ = .82 with Oltmanns & Widiger, 2018; .94 with Bach et al., 2019; .96 with Carnovale et al., 2020), impulsivity and carelessness did not (.29 to .86; Table 3). The PiCD has also resulted in a four-factor structure whenever it has been analyzed together with other questionnaires (Crego & Widiger, 2019; McCabe & Widiger, 2020; Oltmanns & Widiger, 2018, 2020; Somma et al., 2020). It is of note that whereas a bipolar construct of disinhibition–anankastia has found support beyond the PiCD (Harkness et al., 2012; Widiger & Simonsen, 2005; Wright et al., 2012), other models with a broader or simply a different definition of anankastia have identified it as a separate factor (De Clercq et al., 2006; Gutiérrez et al., 2014; Kushner et al., 2011).
Another point is that the PiCD domains are far from being orthogonal. This may be a drawback, as the massive overlap between traditional diagnostic categories was a leading cause of their replacement by the current classification. However, the two cases differ in essential respects. On the one hand, a moderate overlap appears to reflect the true nature of personality traits, and typically results in broader superordinate factors forming hierarchical structures (Condon & Mroczek, 2016; Markon et al., 2005). For example, average intercorrelations of .19 have been reported in Livesley’s personality model, .36 in the DSM-5 dimensional taxonomy, and .20 in the Big Five (Gutiérrez et al., 2020; Saucier, 2002). This means that the PiCD domains are well within the usual range (average r = .28) but the DSM categories are not (.63; Lenzenweger et al., 2007). On the other hand, overlap between personality domains forms an integral part of a repeatedly replicated structure (Markon et al., 2005), whereas categories are arbitrary conglomerates of traits whose structure has never been confirmed (Muñoz-Champel et al., 2018).
Finally, not all PiCD domains appear equally maladaptive at first sight. Only negative affectivity, and to a lesser extent detachment and dissociality, can predict the SASPD, and only negative affectivity substantially predicts caseness. Disinhibition and anankastia play little or no role in either case. These differences between domains are not obvious when the correlations are examined (Table 2; Oltmanns & Widiger, 2019; Somma et al., 2020) but emerge in multiple regression (Supplementary Table S9, available online). There are several possible explanations for these results. They may indeed indicate that some domains are far less maladaptive than others, or that their harmfulness is partly due to their association with negative affectivity (Vall et al., 2015). Certainly, the pervasive presence of negative affectivity in most psychopathology has long been known (Claridge & Davis, 2001; Widiger & Oltmanns, 2017). However, the results may also highlight that the SASPD gives more weight to negative affectivity than to any other domain, particularly disinhibition and anankastia, as mentioned in the Method section. They may also reflect that caseness does not specifically identify personality disorders. Even if we assume that needing clinical care is a common complication of maladapted personalities, and that many of our patients probably present a personality disorder (Beckwith et al., 2014), our clinical sample was actually seeking professional help for a variety of mental problems; as these problems are predominantly depressive and anxiety disorders, negative emotionality must have been favored over all other domains (Claridge & Davis, 2001; Vall et al., 2015). This bias may also explain why severity, as defined by the SASPD, is a worse predictor of caseness than negative affectivity, even if the poor reliability of the SASPD may also have played a nontrivial role. Nevertheless, all the above should not obscure the fact that constructs such as “severity” or “dysfunction,” which increasingly form the basis for diagnosis, are still poorly understood and riddled with ambiguities. For example, whereas the trait parts of the ICD-11 and DSM-5 have a strong empirical basis and are quite similar with each other (Crego & Widiger, 2019; Somma et al., 2020), the severity/dysfunction parts still need considerable research investment (Bach & Anderson, 2018; Oltmanns & Widiger, 2019). This means that careful consideration is in order before we can completely trust the new systems.
Our results should be interpreted in the light of several limitations. First, we lack the borderline specifier, which was incorporated to the system as a sixth domain after this study began. Even if this decision might be more pragmatic than scientific (Mulder & Tyrer, 2018; Tyrer et al., 2019), the role and possible redundancies of borderline traits within the system warrant examination. Second, this study would have benefited from assessing other dimensional models (Ofrat et al., 2018) to investigate the concurrent validity of the ICD-11 classification. This task is currently underway. Finally, as stated above, caseness is a useful but not particularly specific criterion of personality disorder, and it should be taken as an indicator of general psychopathological morbidity. More varied and specific indicators of personality pathology need to be tested in future studies. Insofar as depression and anxiety symptoms may be overrepresented in our clinical sample, the results also need replication in other clinical populations.
In sum, the PiCD and—with some reservations—the SASPD proved to be adequate in their Spanish versions, and can be used with confidence in clinical and research settings. Even so, the current ICD-11 classification is “on probation only” (Tyrer et al., 2019, p. 496) and needs further refinement. Minor inconsistencies in the exact number and nature of personality domains need to be solved; however, evidence on this point is rapidly accumulating and it is unlikely to be a problem. Contrarily, the most consequential issue—who has a disorder and how severe—seems as elusive as ever. There is still disagreement on whether diagnosis should be based on the intensity of traits, the impact on functioning, the decline in well-being, or the probability of psychopathology, disability, or death (Zimmerman et al., 2018). It is not even clear whether different domains might require distinct definitions of severity. We hope that making the PiCD and the SASPD available to a broader range of researchers will promote much-needed conceptual and empirical advances in this area.
Supplemental Material
Supplemental material, Figure_S1_Hierarchical_Structure_of_the_PiCD for Personality Disorders in the ICD-11: Spanish Validation of the PiCD and the SASPD in a Mixed Community and Clinical Sample by Fernando Gutiérrez, Anton Aluja, José Ruiz, Luis F. García, Miguel Gárriz, Alfonso Gutiérrez-Zotes, David Gallardo-Pujol, Maria V. Navarro-Haro, Miquel Alabèrnia-Segura, Joan Ignasi Mestre-Pintó, Marta Torrens, Josep M. Peri, Bárbara Sureda, Joaquim Soler, Juan Carlos Pascual, Gemma Vall, Natalia Calvo, Marc Ferrer, Joshua R. Oltmanns and Thomas A. Widiger in Assessment
Supplemental material, Suppl.Mat._-_PiCD_and_SASPD_revision for Personality Disorders in the ICD-11: Spanish Validation of the PiCD and the SASPD in a Mixed Community and Clinical Sample by Fernando Gutiérrez, Anton Aluja, José Ruiz, Luis F. García, Miguel Gárriz, Alfonso Gutiérrez-Zotes, David Gallardo-Pujol, Maria V. Navarro-Haro, Miquel Alabèrnia-Segura, Joan Ignasi Mestre-Pintó, Marta Torrens, Josep M. Peri, Bárbara Sureda, Joaquim Soler, Juan Carlos Pascual, Gemma Vall, Natalia Calvo, Marc Ferrer, Joshua R. Oltmanns and Thomas A. Widiger in Assessment
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by project PI15/00536, part of the Plan Estatal de Investigación Científica y Técnica y de Innovación 2013-2016, financed by the ISCIII Subdirección General de Evaluación and the cofinanced by the European Regional Development Fund (ERDF, “A way to build Europe”; PI: F. Gutiérrez).
ORCID iDs: Fernando Gutiérrez  https://orcid.org/0000-0002-6662-1796
https://orcid.org/0000-0002-6662-1796
Anton Aluja  https://orcid.org/0000-0002-7865-0287
https://orcid.org/0000-0002-7865-0287
José Ruiz  https://orcid.org/0000-0002-8694-6176
https://orcid.org/0000-0002-8694-6176
Miguel Gárriz  https://orcid.org/0000-0002-0467-9490
https://orcid.org/0000-0002-0467-9490
Alfonso Gutiérrez-Zotes  https://orcid.org/0000-0002-4858-1487
https://orcid.org/0000-0002-4858-1487
Maria V. Navarro-Haro  https://orcid.org/0000-0001-9726-3250
https://orcid.org/0000-0001-9726-3250
Bárbara Sureda  https://orcid.org/0000-0001-8256-3613
https://orcid.org/0000-0001-8256-3613
Supplemental Material: Supplemental material for this article is available online.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders, 5th ed. Author. [Google Scholar]
- Bach B., Anderson J. L. (2018). Patient-reported ICD-11 personality disorder severity and DSM-5 level of personality functioning. Journal of Personality Disorders, 34(2), 231-249. 10.1521/pedi_2018_32_393 [DOI] [PubMed] [Google Scholar]
- Bach B., Christensen S., Kongerslev M. T., Sellbom M., Simonsen E. (2020). Structure of clinician-reported ICD-11 personality disorder trait qualifiers. Psychological Assessment, 2(1), 50-59. 10.1037/pas0000747 [DOI] [PubMed] [Google Scholar]
- Bach B., Kongerslev M. T., Simonsen E. (2019). Prevalence and structure of self-other problems in SAPAS screening for personality disorder in a national sample. Personality and Mental Health, 14(2), 175-185. 10.1002/pmh.1470 [DOI] [PubMed] [Google Scholar]
- Bagby R. M., Widiger T. A. (2020). Assessment of the ICD-11 dimensional trait model: An introduction to the special section. Psychological Assessment, 32(1), 1-7. 10.1037/pas0000785 [DOI] [PubMed] [Google Scholar]
- Beckwith H., Moran P. F., Reilly J. (2014). Personality disorder prevalence in psychiatric outpatients: A systematic literature review. Personality and Mental Health, 8(2), 91-101. 10.1002/pmh.1252 [DOI] [PubMed] [Google Scholar]
- Brown T. A. (2015). Confirmatory factor analysis for applied research (2nd ed.). Guilford Press. [Google Scholar]
- Carnovale M., Sellbom M., Bagby R. M. (2020). The Personality Inventory for ICD-11: Investigating reliability, structural and concurrent validity, and method variance. Psychological Assessment, 32(1), 8-17. 10.1037/pas0000776 [DOI] [PubMed] [Google Scholar]
- Claridge G., Davis C. (2001). What’s the use of neuroticism? Personality and Individual Differences, 31(3), 383-400. 10.1016/S0191-8869(00)00144-6 [DOI] [Google Scholar]
- Condon D. M., Mroczek D. K. (2016). Time to move beyond the Big Five? European Journal of Personality, 30(4), 311-312. 10.1002/per.2060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford M. J., Koldobsky N., Mulder R., Tyrer P. (2011). Classifying personality disorder according to severity. Journal of Personality Disorders, 25(3), 321-330. 10.1521/pedi.2011.25.3.321 [DOI] [PubMed] [Google Scholar]
- Crego C., Widiger T. A. (2019). The convergent, discriminant, and structural relationship of the DAPP-BQ and SNAP with the ICD-11, DSM-5, and FFM trait models. Psychological Assessment, 32(1), 18-28. 10.1037/pas0000757 [DOI] [PubMed] [Google Scholar]
- De Clercq B., De Fruyt F., Van Leeuwen K., Mervielde I. (2006). The structure of maladaptive personality traits in childhood: A step toward an integrative developmental perspective for DSM-V. Journal of Abnormal Psychology, 115(4), 639-657. 10.1037/0021-843X.115.4.639 [DOI] [PubMed] [Google Scholar]
- Epstein J., Santo R. M., Guillemin F. (2015). A review of guidelines for cross-cultural adaptation of questionnaires could not bring out a consensus. Journal of Clinical Epidemiology, 68(4), 435-441. 10.1016/j.jclinepi.2014.11.021 [DOI] [PubMed] [Google Scholar]
- Ferrando P. J., Lorenzo-Seva U. (2017). Program FACTOR at 10: Origins, development and future directions. Psicothema, 29(2), 236-240. 10.7334/psicothema2016.304 [DOI] [PubMed] [Google Scholar]
- Flora D. B., LaBrish C., Chalmers R. P. (2012). Old and new ideas for data screening and assumption testing for exploratory and confirmatory factor analysis. Frontiers in Psychology, 3, Article 55. 10.3389/fpsyg.2012.00055 [DOI] [PMC free article] [PubMed]
- Gutiérrez F., Ruiz J., Peri J. M., Gárriz M., Vall G., Cavero M. (2020). Toward an integrated model of pathological personality traits: Common hierarchical structure of the PID-5 and the DAPP-BQ. Journal of Personality Disorders, 34(Supplement C), 25-39. 10.1521/pedi_2019_33_431 [DOI] [PubMed] [Google Scholar]
- Gutiérrez F., Vall G., Peri J. M., Gárriz M., Garrido J. M. (2014). A hierarchical model of normal and abnormal personality up to seven factors. Comprehensive Psychiatry, 55(2), 326-335. 10.1016/j.comppsych.2013.08.022 [DOI] [PubMed] [Google Scholar]
- Harkness A. R., Finn J. A., McNulty J. L., Shields S. M. (2012). The Personality Psychopathology–Five (PSY-5): Recent constructive replication and assessment literature review. Psychological Assessment, 24(2), 432-443. 10.1037/a0025830 [DOI] [PubMed] [Google Scholar]
- Herpertz S. C., Huprich S. K., Bohus M., Chanen A., Goodman M., Mehlum L., Moran P., Newton-Howes G., Scott L., Sharp C. (2017). The challenge of transforming the diagnostic system of personality disorders. Journal of Personality Disorders, 31(5), 577-589. 10.1521/pedi_2017_31_338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood C. J., Donnellan M. B. (2010). How should the internal structure of personality inventories be evaluated? Personality and Social Psychology Review, 14(3), 332-346. 10.1177/1088868310361240 [DOI] [PubMed] [Google Scholar]
- Kaiser H. F., Rice J. (1974). Little Jiffy, Mark IV. Educational and Psychological Measurement, 34(1), 111-117. 10.1177/001316447403400115 [DOI] [Google Scholar]
- Kleindienst N., Lyssenko L., Bohus M. (2017). Validating the proposed ICD-11 domains: A comment on Mulder et al. (2016). Personality and Mental Health, 11(4), 211-212. 10.1002/pmh.1371 [DOI] [PubMed] [Google Scholar]
- Kushner S. C., Quilty L. C., Tackett J. L., Bagby R. M. (2011). The hierarchical structure of the Dimensional Assessment of Personality Pathology (DAPP-BQ). Journal of Personality Disorders, 25(4), 504-516. 10.1521/pedi.2011.25.4.504 [DOI] [PubMed] [Google Scholar]
- Lenzenweger M. F., Lane M. C., Loranger A. W., Kessler R. C. (2007). DSM-IV personality disorders in the national comorbidity survey replication. Biological Psychiatry, 62(6), 553-564. 10.1016/j.biopsych.2006.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorenzo-Seva U., ten Berge J. M. F. (2006). Tucker’s congruence coefficient as a meaningful index of factor similarity. Methodology, 2(2), 57-64. 10.1027/1614-2241.2.2.57 [DOI] [Google Scholar]
- Lorenzo-Seva U., Timmerman M. E., Kiers H. A. L. (2011). The Hull method for selecting the number of common factors. Multivariate Behavioral Research, 46(2), 340-364. 10.1080/00273171.2011.564527 [DOI] [PubMed] [Google Scholar]
- Markon K. E., Krueger R. F., Watson D. (2005). Delineating the structure of normal and abnormal personality: An integrative hierarchical approach. Journal of Personality and Social Psychology, 88(1), 139-157. 10.1037/0022-3514.88.1.139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maydeu-Olivares A., Coffman D. L. (2006). Random intercept item factor analysis. Psychological Methods, 11(4), 344-362. 10.1037/1082-989X.11.4.344 [DOI] [PubMed] [Google Scholar]
- McCabe G. A., Widiger T. A. (2020). A comprehensive comparison of the ICD-11 and DSM-5 section III personality disorder models. Psychological Assessment, 32(1), 72-84. 10.1037/pas0000772 [DOI] [PubMed] [Google Scholar]
- McCrae R. R., Zonderman A. B., Costa P. T. J., Bond M. H., Paunonen S. V. (1996). Evaluating replicability of factors in the Revised NEO Personality Inventory: Confirmatory factor analysis versus Procrustes rotation. Journal of Personality and Social Psychology, 70(3), 552-566. 10.1037/0022-3514.70.3.552 [DOI] [Google Scholar]
- Moran P., Leese M., Lee T., Walters P., Thornicroft G., Mann A. (2003). Standardised Assessment of Personality–Abbreviated Scale (SAPAS): Preliminary validation of a brief screen for personality disorder. British Journal of Psychiatry, 183(3), 228-232. 10.1192/bjp.183.3.228 [DOI] [PubMed] [Google Scholar]
- Mulder R. T., Newton-Howes G., Crawford M. J., Tyrer P. J. (2011). The central domains of personality pathology in psychiatric patients. Journal of Personality Disorders, 25(3), 364-377. 10.1521/pedi.2011.25.3.364 [DOI] [PubMed] [Google Scholar]
- Mulder R. T., Tyrer P. (2018). Diagnosis and classification of personality disorders. Current Opinion in Psychiatry, 32(1), 27-31. 10.1097/YCO.0000000000000461 [DOI] [PubMed] [Google Scholar]
- Muñoz-Champel A., Gutiérrez F., Peri J. M., Torrubia R. (2018). Personality disorders are not as we thought: Hierarchical factor structure at the criterion level. Journal of Personality Assessment, 100(1), 16-29. 10.1080/00223891.2017.1278700 [DOI] [PubMed] [Google Scholar]
- Ofrat S., Krueger R. F., Clark L. A. (2018). Dimensional approaches to personality disorder classification. In Livesley W. J., Larstone R. (Eds.), Handbook of personality disorders. theory, research, and treatment (2nd ed., pp. 72-87). Guilford Press. [Google Scholar]
- Olajide K., Munjiza J., Moran P., O’Connell L., Newton-Howes G., Bassett P., Akintomide G., Ng N., Tyrer P., Mulder R., Crawford M. J. (2018). Development and psychometric properties of the Standardized Assessment of Severity of Personality Disorder (SASPD). Journal of Personality Disorders, 32(1), 44-56. 10.1521/pedi_2017_31_285 [DOI] [PubMed] [Google Scholar]
- Oltmanns J. R., Widiger T. A. (2018). A self-report measure for the ICD-11 dimensional trait model proposal: The Personality Inventory for ICD-11. Psychological Assessment, 30(2), 154-169. 10.1037/pas0000459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oltmanns J. R., Widiger T. A. (2019). Evaluating the assessment of the ICD-11 personality disorder diagnostic system. Psychological Assessment, 31(5), 674-684. 10.1037/pas0000693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oltmanns J. R., Widiger T. A. (2020). The Five-Factor Personality Inventory for ICD-11: A facet-level assessment of the ICD-11 trait model. Psychological Assessment, 32(1), 60-71. 10.1037/pas0000763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborne J. W. (2014). Best practices in exploratory factor analysis. CreateSpace Independent Publishing. [Google Scholar]
- R Core Team. (2018). R: A language and environment for statistical computing. R Foundation for Statistical Computing. http://www.R-project.org [Google Scholar]
- Reed G. M. (2018). Progress in developing a classification of personality disorders for ICD-11. World Psychiatry, 17(2), 227-229. 10.1002/wps.20533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rek K., Thielmann I., Henkel M., Crawford M., Piccirilli L., Graff A., Mestel R, Zimmermann J. (2019). A comprehensive evaluation of the Standardized Assessment of Severity of Personality Disorder (SASPD) in clinical and non-clinical German samples. Manuscript submitted for publication. https://psyarxiv.com/unqhm/ [DOI] [PubMed]
- Rizopoulos D. (2006). ltm: An R package for latent variable modeling and item response theory analyses. Journal of Statistical Software, 17(5), 1-25. 10.18637/jss.v017.i05 [DOI] [Google Scholar]
- Rosseel Y. (2012). lavaan: An R Package for structural equation modeling. Journal of Statistical Software, 48(2), 1-36. 10.18637/jss.v048.i02 [DOI] [Google Scholar]
- Saucier G. (2002). Orthogonal markers for orthogonal factors: The case of the Big Five. Journal of Research in Personality, 36(1), 1-31. 10.1006/jrpe.2001.2335 [DOI] [Google Scholar]
- Skodol A. E. (2011). Scientific issues in the revision of personality disorders for DSM-5. Personality and Mental Health, 5(2), 97-111. 10.1002/pmh.161 [DOI] [Google Scholar]
- Somma A., Gialdi G., Fossati A. (2020). Reliability and construct validity of the Personality Inventory for ICD-11 (PiCD) in Italian adult participants. Psychological Assessment, 32(1), 29-39. 10.1037/pas0000766 [DOI] [PubMed] [Google Scholar]
- Timmerman M. E., Lorenzo-Seva U. (2011). Dimensionality assessment of ordered polytomous items with parallel analysis. Psychological Methods, 16(2), 209-220. 10.1037/a0023353 [DOI] [PubMed] [Google Scholar]
- Toland M. D. (2014). Practical guide to conducting an item response theory analysis. Journal of Early Adolescence, 34(1), 120-151. 10.1177/0272431613511332 [DOI] [Google Scholar]
- Tyrer P., Crawford M., Mulder R., Blashfield R., Farnam A., Fossati A., Kim Y.-R., Koldobsky N., Lecic-Tosevski D., Ndetei D., Swales M., Clark L. A., Reed G. M. (2011). The rationale for the reclassification of personality disorder in the 11th revision of the International Classification of Diseases (ICD-11). Personality and Mental Health, 5(4), 246-259. 10.1002/pmh.190 [DOI] [Google Scholar]
- Tyrer P., Crawford M., Sanatinia R., Tyrer H., Cooper S., Muller-Pollard C., Christodoulou P., Zauter-Tutt M., Miloseska-Reid K., Loebenberg G., Guo B., Yang M., Wang D., Weich S. (2014). Preliminary studies of the ICD-11 classification of personality disorder in practice. Personality and Mental Health, 8(4), 254-263. 10.1002/pmh.1275 [DOI] [PubMed] [Google Scholar]
- Tyrer P., Johnson T. (1996). Establishing the severity of personality disorder. American Journal of Psychiatry, 153(12), 1593-1597. 10.1176/ajp.153.12.1593 [DOI] [PubMed] [Google Scholar]
- Tyrer P., Mulder R., Kim Y.-R., Crawford M. J. (2019). The development of the ICD-11 classification of personality disorders: An amalgam of science, pragmatism, and politics. Annual Review of Clinical Psychology, 15(1), 481-502. 10.1146/annurev-clinpsy-050718-095736 [DOI] [PubMed] [Google Scholar]
- Tyrer P., Reed G. M., Crawford M. (2015). Classification, assessment, prevalence, and effect of personality disorder. Lancet, 385, 717-726. 10.1016/S0140-6736(14)61995-4 [DOI] [PubMed] [Google Scholar]
- Vall G., Gutiérrez F., Peri J. M., Gárriz M., Ferraz L., Baillés E., Obiols J. E. (2015). Seven basic dimensions of personality pathology and their clinical consequences: Are all personalities equally harmful? British Journal of Clinical Psychology, 54(4), 450-468. 10.1111/bjc.12091 [DOI] [PubMed] [Google Scholar]
- Widiger T. A., Oltmanns J. R. (2017). Neuroticism is a fundamental domain of personality with enormous public health implications. World Psychiatry, 16(2), 144-145. 10.1002/wps.20411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widiger T. A., Simonsen E. (2005). Alternative dimensional models of personality disorder: Finding a common ground. Journal of Personality Disorders, 19(2), 110-130. 10.1521/pedi.19.2.110.62628 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2018). International statistical classification of diseases for mortality and morbidity statistics (11th Revision). https://icd.who.int/browse11/l-m/en
- Wright A. G. C., Thomas K. M., Hopwood C. J., Markon K. E., Pincus A. L., Krueger R. F. (2012). The hierarchical structure of DSM-5 pathological personality traits. Journal of Abnormal Psychology, 121(4), 951-957. 10.1037/a0027669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman M., Morgan T. A., Stanton K. (2018). The severity of psychiatric disorders. World Psychiatry, 17(3), 258-275. 10.1002/wps.20569 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Figure_S1_Hierarchical_Structure_of_the_PiCD for Personality Disorders in the ICD-11: Spanish Validation of the PiCD and the SASPD in a Mixed Community and Clinical Sample by Fernando Gutiérrez, Anton Aluja, José Ruiz, Luis F. García, Miguel Gárriz, Alfonso Gutiérrez-Zotes, David Gallardo-Pujol, Maria V. Navarro-Haro, Miquel Alabèrnia-Segura, Joan Ignasi Mestre-Pintó, Marta Torrens, Josep M. Peri, Bárbara Sureda, Joaquim Soler, Juan Carlos Pascual, Gemma Vall, Natalia Calvo, Marc Ferrer, Joshua R. Oltmanns and Thomas A. Widiger in Assessment
Supplemental material, Suppl.Mat._-_PiCD_and_SASPD_revision for Personality Disorders in the ICD-11: Spanish Validation of the PiCD and the SASPD in a Mixed Community and Clinical Sample by Fernando Gutiérrez, Anton Aluja, José Ruiz, Luis F. García, Miguel Gárriz, Alfonso Gutiérrez-Zotes, David Gallardo-Pujol, Maria V. Navarro-Haro, Miquel Alabèrnia-Segura, Joan Ignasi Mestre-Pintó, Marta Torrens, Josep M. Peri, Bárbara Sureda, Joaquim Soler, Juan Carlos Pascual, Gemma Vall, Natalia Calvo, Marc Ferrer, Joshua R. Oltmanns and Thomas A. Widiger in Assessment