Abstract
Background:
Treatment of first-time shoulder dislocation (FSD) is a topic of debate. After high rates of recurrent instability after nonoperative management were reported in the literature, primary repair of FSD significantly increased. At the same time, new concepts were proposed that had promising results for immobilization in external rotation (ER) and abduction (ABD).
Purpose:
The aim of this study was to evaluate the recurrence rates (primary outcome) and clinical outcomes (secondary outcome parameters) of immobilization in ER+ABD versus arthroscopic primary stabilization after FSD.
Study Design:
Randomized controlled trial; Level of evidence, 1.
Methods:
In a multicenter randomized controlled trial, patients with FSD were randomized to either treatment with immobilization in 60° of ER plus 30° of ABD (group 1) or surgical treatment with arthroscopic Bankart repair (group 2). Clinical evaluation was performed 1, 3, and 6 weeks as well as 6, 12, and 24 months postoperatively or after reduction, including range of motion, instability testing, subjective shoulder value, Constant-Murley score, Rowe score, and Western Ontario Shoulder Instability Index. Recurrent instability events were prospectively recorded.
Results:
Between 2011 and 2017, a total of 112 patients were included in this study. Of these, 60 patients were allocated to group 1 and 52 to group 2. At the 24-month follow-up, 91 patients (81.3%) were available for clinical examination. The recurrence rate was 19.1% in group 1 and 2.3% in group 2 (P = .016). No significant differences were found between groups regarding clinical shoulder scores (P > .05). Due to noncompliance with the immobilization treatment protocol, 4 patients (6.7%) were excluded.
Conclusion:
Immobilization in ER+ABD versus primary arthroscopic shoulder stabilization for the treatment of FSD showed no differences in clinical shoulder scores. However, recurrent instability was significantly higher after nonoperative treatment.
Keywords: first-time shoulder dislocation, shoulder instability, shoulder stabilization, immobilization in external rotation and abduction
Anterior shoulder instability is common in the general population, especially in young and physically active persons. Males and athletes are especially affected by glenohumeral instability.8,28,37 The rate of recurrence varies in different studies and different groups of patients. Wasserstein et al47 found a pooled rate of recurrence for nonoperative management of first-time anterior shoulder instability of 21% (range, 19%-88%) at a minimum follow-up of 2 years. Other authors reported even higher failure rates with a nonoperative approach, with recurrence rates up to 92% especially in patients younger than 30 years.21,39,45,48 As such, there has been growing interest in the role of surgical stabilization after first-time shoulder dislocation (FSD). Studies from Great Britain and Germany have shown a significant increase of primary repair surgery in cases of FSD in the last 2 decades.3,33 With the rise of minimally invasive arthroscopic techniques, several authors suggest early surgical treatment for FSD, predominantly in a young and active population.3,33
For the nonoperative management of FSD, a standardized treatment algorithm has not been established, and different kinds of rehabilitation regimens exist. In particular, no consensus is available regarding position and duration of immobilization. Historically, shoulder immobilization after FSD was performed in the so-called safe position in internal rotation (IR). In 2001, Itoi et al25 introduced the idea of immobilization in external rotation (ER). The concept is based on observations made in a magnetic resonance imaging (MRI) controlled study that a reduction of the labrum to the glenoid rim can be reached in an ER position of the shoulder. Several clinical studies comparing IR and ER immobilization for nonoperative management of FSD were performed.13,22,23,32,44,49 In a recent Cochrane review, Braun et al6 concluded that there is insufficient evidence as to whether immobilization in ER confers any benefit over immobilization in IR. However, it must be kept in mind that all of these studies used different angles of ER between 0° and 30°. Miller et al35 showed that the contact force between the labrum and anterior glenoid increased in ER and reached its maximum above 45° of ER. Moreover, in an arthroscopic controlled study, Hart and Kelly18 proved that the best in vivo position of the labrum could be reached in 60° of ER and an additional 30° of abduction (ABD). In a later biomechanical study, Itoi et al24 showed that abducting the arm during immobilization in ER improved reduction of the Bankart lesion. It remains unclear whether nonoperative treatment using immobilization in ER+ABD achieves similar outcomes compared with primary arthroscopic shoulder stabilization.
The aim of the current study was to evaluate the recurrence rates (primary outcome) and clinical outcomes (secondary outcome parameters) of immobilization in ER+ABD versus arthroscopic primary stabilization after FSD in a multicenter prospective randomized controlled trial (RCT). We hypothesized that there would be no significant differences regarding recurrence rates and clinical outcomes between the 2 interventions and that both would lead to satisfying results.
Methods
Study Design
The study was designed as a multicenter prospective RCT, initiated and conducted by the German Society for Shoulder and Elbow Surgery (DVSE). A total of 7 departments specializing in shoulder and elbow surgery throughout Germany participated in this trial. The patient inclusion criteria were (1) first-time traumatic anterior shoulder dislocation, (2) inclusion and randomization 3 days or less after dislocation, (3) type B2 (unidirectional without hyperlaxity) or B3 (unidirectional with hyperlaxity) instability according to Gerber and Nyffeler,15 and (4) age between 18 and 40 years. The exclusion criteria were (1) recurrent shoulder instability, (2) posterior and multidirectional shoulder instability, (3) any concomitant shoulder pathology (eg, cuff tear, bony Bankart lesion, dislocation fracture including greater tuberosity fracture, engaging Hill-Sachs lesion, nerve lesion), (4) noncompliance especially in wearing the brace for immobilization in ER and ABD, and (5) unwillingness to participate in the study. Patients were assigned to the nonoperative treatment with immobilization or the surgical treatment with shoulder stabilization within 3 days after trauma and dislocation at a 1:1 allocation ratio based on an allocation sequence that was generated on a computer and internet-based randomization tool. The recruitment period was between October 2011 and October 2017. In all patients, standardized radiography and MRI of the affected shoulder were performed to rule out any concomitant pathologies. After baseline assessment, patients underwent the assigned treatment. Longitudinal follow-up included clinical evaluation.
The study protocol was confirmed by the research committee of the DVSE, and reports of the current status of the study were provided at the annual meetings of the committee and society. This trial has not been registered, because registering an RCT online (eg, at ClinicalTrials.gov or a similar database recognized by the International Committee of Medical Journal Editors) was not mandatory when the study was started in 2011. Apart from that, reporting of the clinical trial was accomplished according to the CONSORT (Consolidated Standards of Reporting Trials) guidelines for reporting RCTs. This study was approved by the local ethics committee (EA4/030/11).
Interventions
Patients were assigned to receive either a nonoperative treatment with immobilization in 60° of ER and 30° of ABD (group 1) or surgical treatment with arthroscopic shoulder stabilization (group 2). For immobilization in the ER+ABD position, a Bledsoe ARC XR (Bledsoe Brace System) orthosis was used (Figure 1). In a previous study, this brace was tested and compared with 3 other available braces for immobilization in the ER+ABD position.46 With regard to functionality and comfort, this orthosis achieved the best results and was found to be most effective for immobilization of the shoulder in an ER+ABD position after first-time traumatic shoulder instability.46 The immobilization treatment began at least 3 days after trauma and was initiated directly after the patient provided written consent to participate in the study. Correct positioning of the brace and shoulder in 60° of ER and 30° of ABD was determined by an orthopaedic technician and a physician. Patients were instructed to wear the brace 24 hours a day, for 3 weeks in total. The patients could take off the brace for a maximum of 1 hour per day only for showering and personal hygiene. After completion of the immobilization treatment, physical therapy treatment was initiated, which was comparable to a standardized rehabilitation protocol of patients being treated by a surgical stabilization procedure (Appendix). Patients assigned to group 2 underwent surgery within 3 weeks after trauma. Surgeries were performed with patients in the lateral decubitus position, and 3 portals were used. A standardized arthroscopic shoulder stabilization procedure was performed with labral repair and capsular shift using a knotless technique. For refixation of the labrum, at least 3 PEEK anchors (Arthrex) with a FiberWire loop (Arthrex) were used. Postoperatively, the patients were immobilized in IR in a sling for 3 weeks, and a standardized rehabilitation protocol was performed. Free passive and active range of motion exercises were allowed 6 weeks after FSD (and the start of immobilization treatment) for group 1 and 6 weeks after surgical stabilization for group 2. In both groups, sport-specific exercises were prohibited for 3 months and return to sports for 6 months.
Figure 1.

Immobilization in 60° of external rotation and 30° of abduction in the Bledsoe ARC XR brace.
Clinical Evaluation
Baseline examination was performed at the time of randomization, before any treatment began, and included a pathology-specific medical history and anamnesis (mechanism and severity of trauma leading to shoulder dislocation, time since dislocation, previous treatment, type of profession, and level of activity in profession and sports) and determination of the type of shoulder instability according to Gerber and Nyffeler (type B2 or B3).15 General laxity, a positive sulcus sign,2 a positive hyperabduction test according to Gagey and Gagey,14 and a positive Coudane-Walch sign11 with >85° of ER in neutral position were criteria for a type B3 instability.
Longitudinal follow-up examinations were performed 6 weeks and 6, 12, and 24 months after randomization in both groups, always by the same examiner at the individual centers. In group 1, two additional appointments were performed 1 and 3 weeks after the immobilization treatment began. The aim of these 2 examinations was to check the correct position of immobilization and the brace and the compliance of the patient. Follow-up examinations at 6 weeks included numeric pain scale (from 0 to 10) and assessment of active range of motion using a goniometer. Follow-up examinations at 6, 12, and 24 months included the following: assessment of active range of motion using a goniometer; instability testing including the apprehension test43 and relocation test27; hyperlaxity assessment including the sulcus sign,2 hyperabduction test,14 and Coudane-Walch sign11; scapular dyskinesis evaluation according to Kibler29; and standardized objective and subjective clinical shoulder scores including the subjective shoulder value (SSV),16 Constant-Murley score (CS),10 Rowe score (RS),42 and Western Ontario Shoulder Instability Index (WOSI).20,30 Abduction strength for determination of the CS was measured using a dynamometer. Furthermore, any adverse events including recurrent instability were assessed. Recurrent instability included any traumatic or atraumatic dislocation or subluxation event reported by the patient. A positive apprehension or relocation test was recorded and rated as a persisting shoulder instability symptom, not as a recurrent instability event. The absence or occurrence of a recurrent instability event was defined as the primary outcome parameter. Clinical outcomes including range of motion and shoulder scores (SSV, CS, RS, WOSI) were secondary outcome parameters.
Statistical Analysis
Before the beginning of the study, a power analysis for sample size calculation was performed based on a P value of .05, a power of 80% for stating the difference in recurrence, and an expected follow-up rate of 80%. A sample size of 110 patients was calculated. During the trial, data were collected on report forms and later converted into spreadsheets for statistical analysis. Group characteristics and outcome variables were tested for normal distribution using the Kolmogorov-Smirnov test. For group comparisons, the Mann-Whitney U test, t test, chi-square test, or Fisher exact test was used. All reported tests were 2-tailed, and a P value <.05 was considered statistically significant. All patients enrolled in this randomized trial were allocated according to the randomization sequence and received the assigned intervention along with the rehabilitation treatment. An intention-to-treat analysis for patients who underwent surgical stabilization secondarily was not performed.
Results
Patient Population
A total of 112 consecutive patients fulfilling the inclusion and exclusion criteria were enrolled and randomized among the 7 centers involved in this trial. Of these, 60 patients were allocated to the immobilization treatment (group 1) and 52 patients to the surgical treatment (group 2). The majority of the patients were male (n = 103; 92%) and the distribution did not differ between the 2 groups (P = .90). The mean age of the total patient cohort was 26.2 ± 5.9 years; age was similar in both groups with no significant difference (P = .29). In group 1, we found that 86.7% (n = 52) of the patients had a type B2 shoulder instability and 13.3% (n = 8) had a type B3 shoulder instability. The distribution in group 2 was similar (P = .39), with 80.8% (n = 42) of patients classified as type B2 and 19.2% (n = 10) as type B3 instability. Regarding professions and level of activity in profession and sports, no significant differences between the 2 groups were found. Most patients had a non–physically demanding job but were active in contact and/or overhead sports (eg, soccer, team handball, martial arts). The groups showed no significant differences regarding baseline characteristics, as shown in Table 1.
Table 1.
Comparison of Baseline Group Characteristics a
| Group 1 | Group 2 | P Value | |
|---|---|---|---|
| Age, y, mean ± SD | 26.7 ± 5.8 | 25.7 ± 6.2 | .29 |
| Sex | |||
| Female | 8.3 (5) | 7.7 (4) | .90 |
| Male | 91.6 (55) | 92.3 (48) | |
| Instability (Gerber b classification) | |||
| B2 | 86.7 (52) | 80.8 (42) | .39 |
| B3 | 13.3 (8) | 19.2 (10) | |
| Job | |||
| Physically demanding | 41.7 (25) | 32.7 (17) | .33 |
| Not physically demanding | 58.3 (35) | 67.3 (35) | |
| Sports | |||
| None | 26.7 (16) | 17.3 (9) | .43 |
| No overhead or contact | 18.3 (11) | 25 (13) | |
| Contact and/or overhead | 55 (33) | 57.7 (30) |
Values are expressed as % (n) unless otherwise noted.
Gerber and Nyffeler.15
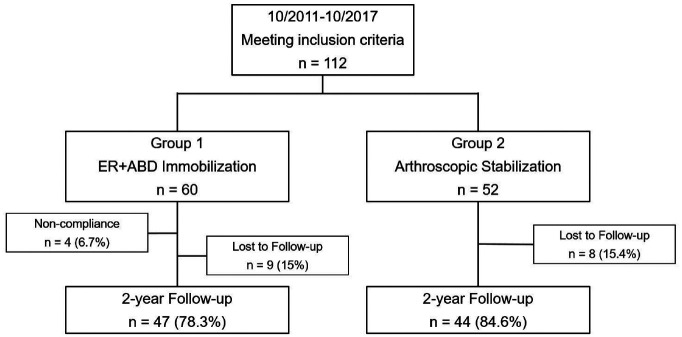
At the 24-month follow-up, 91 (81.3%) patients were available for the final clinical examination (47/60 in group 1 and 44/52 in group 2). A total of 9 patients from group 1 and 8 patients from group 2 were lost to follow-up because contact information changed without notice. Further, 4 patients (6.7%) allocated to the ER+ABD immobilization were secondarily excluded from the study because of noncompliance (ie, they interrupted the immobilization treatment) (Figure 2). Baseline characteristics of the patients lost to follow-up or excluded due to noncompliance did not differ from the characteristics of the other patients.
Figure 2.
Flowchart of trial. ER+ABD = 60° of external rotation and 30° of abduction.
Rate of Recurrence—Primary Outcome Parameter
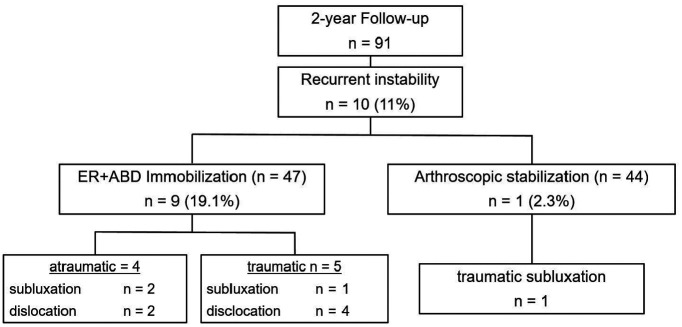
The overall recurrence rate was 11% (n = 10). Among the 47 patients treated nonoperatively with immobilization in ER+ABD, 9 patients reported a recurrent instability event. In 5 cases, these were traumatic dislocations (n = 4) or subluxations (n = 1). Atraumatic recurrent instability events were reported by 4 patients, with dislocation in 2 cases and subluxation in another 2 cases within the 24-month observation time. All traumatic subluxation or dislocation events were due to a collision or a fall during sports activities (n = 1 collision during rugby, n = 2 collision during soccer, n = 2 bicycle fall). Atraumatic events were recorded in cases of no trauma or inadequate trauma. For example, 1 patient had recurrent instability after reaching for something high in a wardrobe, which was considered an atraumatic dislocation. Another patient was lying on his bed while holding his arms behind his head when he was startled and moved quickly, leading to a dislocation, which was considered an inadequate trauma. These events resulted in a recurrence rate of 19.1% after nonoperative treatment with immobilization in ER+ABD after FSD.
Among the 44 patients treated surgically with arthroscopic shoulder stabilization, only 1 patient (2.3%) reported a traumatic subluxation, which occurred during a bicycle accident 12 months postoperatively (Figure 3). Regarding the main outcome parameter, the rate of recurrent instability events, a significant difference (P = .016) was found between the 2 groups. The majority (n = 9; 90%) of patients who experienced recurrent shoulder instability were younger than 30 years: the mean age was 25 ± 4.8 years (range, 20-37 years). All of them were male. A total of 9 patients (90%) were active in sports on a regular basis, and 8 of them (80%) performed overhead and/or contact sports. The majority (n = 9; 90%) had a type B2 instability according to the Gerber and Nyffeler15 classification. The recurrent dislocation event occurred at a mean of 9.8 ± 4.4 months after FSD (range, 3-16 months). There were 5 patients (10.6%) who required secondary arthroscopic shoulder stabilization due to recurrent shoulder instability at a mean of 12.2 months (range, 5-21 months) after initial dislocation. All patients requiring surgery had been treated with ER+ABD immobilization previously, reported a subjective feeling of instability, and showed clinical signs of shoulder instability. No clinical scores were obtained before surgery. The remaining patients who experienced recurrent instability were treated nonoperatively because either they experienced only a single instability event or they refused surgical stabilization due to subjective well-being. Among the patients who did not have a recurrent instability episode, the apprehension and relocation tests were positive in 3 patients (7.9%) in the ER+ABD immobilization group and 2 patients (4.7%) in the arthroscopic stabilization group (P = .67). Positive apprehension and relocation tests were considered persisting shoulder instability symptoms, not recurrent instability events. No statistically significant differences were observed regarding instability symptoms among the patients who did not have recurrent dislocation or subluxation. Apart from recurrent instability events, no further complications were noted in this study, either after immobilization treatment or after surgical shoulder stabilization.
Figure 3.
Comparison of recurrent instability events at 24-month follow-up between patients treated nonoperatively with immobilization in external rotation and abduction (ER+ABD) (group 1) and patients treated surgically with arthroscopic shoulder stabilization (group 2).
Clinical Outcome—Secondary Outcome Parameter
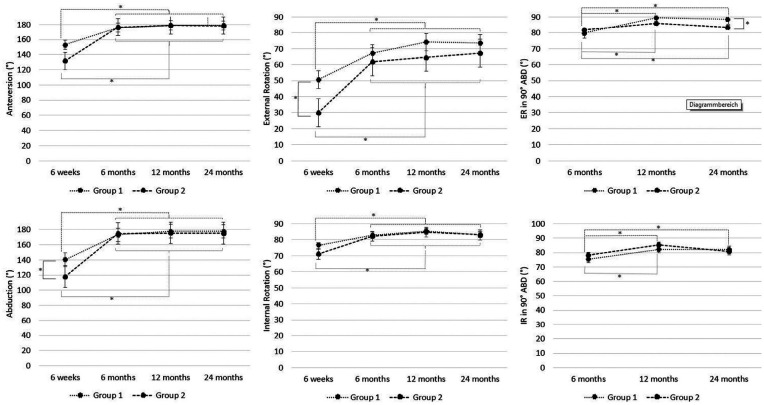
Regarding anteversion, IR, and IR at 90° of ABD, no significant differences between the 2 groups were noted at any of the follow-up time points. At the 6-week follow-up examination, significant differences in ER and ABD became evident between the 2 groups. Patients treated nonoperatively showed significantly better ER (52°± 21°) and ABD (139°± 34°) compared with patients treated surgically with shoulder stabilization (ER, 29°± 18°; ABD, 115°± 35°; P < .01 and P = .03, respectively). This difference equalized over time. At the 24-month follow-up, a small but significant difference became evident regarding the ER capacity at 90° of ABD; patients in group 1 reached 86°± 9° and those in group 2 reached 80°± 12° (P = .02). In both groups, the range of motion significantly improved over time, especially compared with the 6-week follow-up examination (Figure 4).
Figure 4.
Comparison of range of motion at 24-month follow-up between patients treated nonoperatively with immobilization in external rotation and abduction (ER+ABD) (group 1) and patients treated surgically with arthroscopic shoulder stabilization (group 2). Significant differences in external rotation and abduction were found between the 2 groups at 6 weeks after reduction (group 1) or postoperatively (group 2) and in external rotation in 90° of abduction at 24-month follow-up. *Significant differences between the different time points and between the 2 groups.
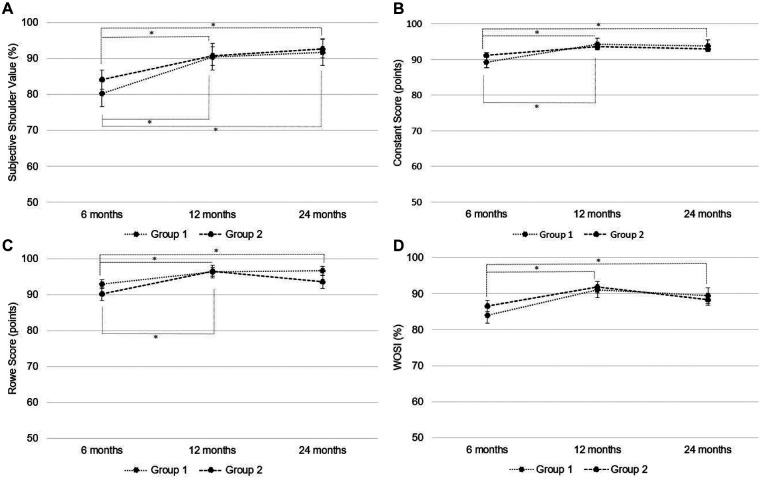
At no follow-up point did any of the clinical scores show a statistically significant difference between the 2 groups (Figure 5). In group 1, the SSV reached 93.6% ± 4.4%, the CS 96.9 ± 4.7 points, the RS 89.1 ± 7.1 points, and the WOSI 91.5% ± 7.9% at the 2-year follow-up. In group 2, the SSV reached 93.1% ± 6.5%, the CS 93.9 ± 10.1 points, the RS 88.5 ± 11.2 points, and the WOSI 92.7% ± 8.1% at the 2-year follow-up. Differences between follow-up examinations were found in both groups. Significant improvements in the SSV, CS, RS, and WOSI were found at the 12- and 24-month follow-up compared with the 6-month examinations in group 1. In group 2, the difference was significant in the SSV, CS, and RS predominantly from the 6-month follow-up compared with the 12-month follow-up examination. Overall, the clinical scores were satisfactory in both groups. No significant differences in ABD strength were noted between the 2 groups.
Figure 5.
Longitudinal comparison of (A) subjective shoulder value (SSV), (B) Constant-Murley score, (C) Rowe score, and (D) Western Ontario Shoulder Instability Index (WOSI) at different time points between patients treated nonoperatively with immobilization in external rotation and abduction (ER+ABD) (group 1) and patients treated surgically with arthroscopic shoulder stabilization (group 2). No significant differences were noted at any time point between the 2 groups. *Significant differences between the different time points.
Discussion
In this multicenter RCT, which compared immobilization in ER+ABD versus primary arthroscopic shoulder stabilization for the treatment of FSD, we found no statistically significant differences regarding the clinical shoulder scores between the 2 groups. However, a significant difference was found regarding the main outcome parameter, as recurrent instability events were more common in the nonoperatively treated group. Secondary shoulder stabilization surgery was required in 10.6% (5/47) of these patients. Almost all patients who had recurrent shoulder instability were younger than 30 years and were active in contact and/or overhead sports. Only regarding ER at 90° of ABD did a significant difference become evident at 2-year follow-up. However, this small difference was clinically negligible and generally not noticeable for the patient. At 6-week follow-up, a significant difference was found regarding ABD and ER. This might be due to a partial postoperative stiffness in patients treated by surgical shoulder stabilization and subsequent immobilization in IR. Additionally, patients treated by immobilization are passively forced into an ER position and lose less capacity for range of motion within the first couple of weeks. A total of 4 patients allocated to the nonoperative treatment group were secondarily excluded because of noncompliance, as they did not tolerate the immobilization treatment. The ER+ABD position might be uncomfortable for the patient, which is a disadvantage of this kind of treatment. However, most of the patients tolerated the immobilization well. To our knowledge, we have presented the first RCT comparing immobilization in ER+ABD with the commonly performed arthroscopic shoulder stabilization in patients with first-time traumatic anterior shoulder instability.
The concept of immobilization in ER was introduced by Itoi et al25 in 2001, and since then multiple studies have been performed comparing different kinds of immobilization. In their Cochrane review, Braun and McRobert6 concluded that the evidence was insufficient regarding whether immobilization in ER confers any benefit compared with immobilization in IR after FSD with regard to recurrent instability. The pooled recurrence rate was 22.4% for immobilization in ER versus 30% for immobilization in IR.6 None of the studies used an immobilization of 60° of ER plus 30° of ABD, which, according to biomechanical and arthroscopic data, is the best position for reduction of the labrum to allow healing in an anatomic position.18,24 The degree of ER used varied from 0° to 30°, and in only 2 trials was the arm additionally immobilized in ABD.6,9,13,19,23,32,44,49 Heidari et al19 presented the first RCT comparing the risk of recurrent instability after immobilization in IR versus ER+ABD. In their study, the shoulder was stabilized in 10° of ER and 15° of ABD or was immobilized in IR in a conventional sling. At 24-month follow-up, the investigators found a significant difference, with a recurrence rate of 33.3% in the IR group and 3.9% in the ER+ABD group. Chan et al,9 using 30° of ER and 30° of ABD, found a 30% rate of recurrent dislocation for their conventional sling group and 24% for their ER+ABD bracing group. In our study, the rate of recurrent instability was 19.1% after immobilization in ER+ABD. Although this number is significantly higher compared with the rate of recurrent instability after surgical stabilization, the clinical outcome in patients without recurrent instability was almost equal in both groups.
The tendency to use early surgical stabilization has increased in the last few decades, especially for young and active patients.3,4,33 This might be due to the use of sophisticated, minimally invasive techniques and patients’ requests for treatments options with the lowest risk for recurrent instability. The rate of recurrence after primary repair for FSD reported in the literature ranges between 7% and 29% at a minimum follow-up of 2 years.1,12,17,34,36,38,40,41 Several authors concluded that initial shoulder stabilization is the treatment of choice for FSD in younger patients who are active in overhead, contact, or collision sports.
Only a few studies have compared nonoperative management and early surgical stabilization after FSD.5,26,31 In a systematic review from 2009, Brophy and Marx7 compared RCTs that reported the results of nonoperative treatment versus primary surgical stabilization after FSD; those investigators concluded that the recurrence rate was reduced by surgical intervention, particularly in young, active, male patients. All studies found higher recurrence rates after nonoperative treatment (46%-75%) compared with primary stabilization (2.7%-18.7%) at a minimum follow-up of 2 years.5,7,26,31 None of these studies used immobilization of the shoulder in ER or ER+ABD. The 2.3% recurrence rate after surgical stabilization that we found is low but comparable to those reported in the literature and might rise to a small extent after a longer follow-up period. We found a recurrence rate of 19.1% after nonoperative treatment with immobilization in ER+ABD, which is considerably lower than rates reported by other RCTs using immobilization in IR. Thus, even if the recurrence rate after surgical stabilization is lower compared with nonoperative treatment, immobilization in ER+ABD seems to be beneficial compared with other nonoperative treatment options. In our study, the clinical results were similar in both groups. Patients who are affected by FSD should be informed about the different treatment options. We believe that immobilization in ER+ABD is a reasonable therapy for FSD that leads to satisfactory clinical outcomes with an acceptable recurrence rate. However, the risk for recurrence is lower when primary surgical stabilization is performed. Additionally, patient-specific risk factors such as age and level of activity should be considered in the treatment decision. Patients performing high-risk sports might benefit from primary surgical stabilization, as it shows better outcomes regarding recurrence rate.
Limitations
The recruitment period of 6 years seems to be long for a study that includes 6 referral centers for shoulder surgery and the common pathology of shoulder instability. However, we chose strict inclusion and exclusion criteria, which made recruitment of patients difficult. In our experience, patient acquisition for a randomized clinical trial that includes a surgical treatment group and a nonoperative treatment is challenging and demands extensive explanations to the prospective patients before they can be included. Multiple patients were not eligible for the study for predominantly 2 reasons: either they refused to participate in the study or they visited the outpatient departments >3 days after trauma, which was too late for enrollment and randomization. Due to organizational burdens in the different departments and the multicenter study design, we were not able to record all of the patients with FSD who would possibly have been eligible for the trial. The number of patients who were lost because they refused to participate, sought treatment >3 days after dislocation, or had concomitant lesions listed under the exclusion criteria is unclear, leading to a potential selection bias. Owing to the nature of both interventions, blinding of the patients was not possible and blinding of the outcome examiners was not feasible. This lack of blinding also creates a risk of bias. However, this risk is reduced by the fact that most of the outcome measurements are patient reported and subjective. We believe that a follow-up period of 2 years is generally enough to judge the efficiency and outcome of a nonoperative or surgical treatment in cases of shoulder instability. According to the literature, the risk of recurrent instability is highest within the first year after FSD and decreases over time.17,47 However, it is possible that the current results might change in a mid- to long-term follow-up. Unfortunately, we were not able to conduct follow-up examinations of the patients who experienced a recurrent instability and had to be excluded because of noncompliance. This compromises the analysis of clinical outcomes between the 2 groups because only patients who were successfully treated are considered in the 24-month follow-up results. An intention-to-treat analysis for patients who underwent surgical stabilization secondarily was not performed. No radiographic or MRI evaluation was conducted at the latest follow-up, and follow-up times were not long enough to determine long-term problems such as arthropathy. Return to sports was not evaluated in detail, which is another limitation.
Conclusion
Immobilization in ER+ABD versus primary arthroscopic shoulder stabilization for the treatment of FSD showed no differences in clinical shoulder scores. However, recurrent instability was significantly higher after nonoperative treatment. Traumatic as well as atraumatic recurrent instability events can be observed, which mainly affect patients younger than 30 years who are active in sports. Primary surgical stabilization might be preferred for this group if the patient desires the lowest risk for recurrent dislocation.
Supplemental Material
Supplemental material, sj-pdf-1-ajs-10.1177_0363546520987823 for Immobilization in External Rotation and Abduction Versus Arthroscopic Stabilization After First-Time Anterior Shoulder Dislocation: A Multicenter Randomized Controlled Trial by Marvin Minkus, Matthias Königshausen, Dirk Maier, Frieder Mauch, Thomas Stein, Stefan Greiner, Mohamed Moursy and Markus Scheibel in The American Journal of Sports Medicine
Footnotes
Submitted March 18, 2020; accepted October 11, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: Financial support was provided by the Wilhelm Julius Teufel Company, which assisted this study. M.S., D.M., F.M., T.S., and S.G. received consultant payments from Arthrex that were not related to this work. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Aboalata M, Plath JE, Seppel G, Juretzko J, Vogt S, Imhoff AB. Results of arthroscopic Bankart repair for anterior-inferior shoulder instability at 13-year follow-up. Am J Sports Med. 2017;45(4):782-787. [DOI] [PubMed] [Google Scholar]
- 2. Altchek DW, Warren RF, Skyhar MJ, Ortiz G. T-plasty modification of the Bankart procedure for multidirectional instability of the anterior and inferior types. J Bone Joint Surg Am. 1991;73(1):105-112. [PubMed] [Google Scholar]
- 3. Balke M, Shafizadeh S, Bouillon B, Banerjee M. Management of shoulder instability: the current state of treatment among German orthopaedic surgeons. Arch Orthop Trauma Surg. 2016;136(12):1717-1721. [DOI] [PubMed] [Google Scholar]
- 4. Berendes TD, Pilot P, Nagels J, Vochteloo AJ, Nelissen RG. Survey on the management of acute first-time anterior shoulder dislocation amongst Dutch public hospitals. Arch Orthop Trauma Surg. 2015;135(4):447-454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bottoni CR, Wilckens JH, DeBerardino TM, et al. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med. 2002;30(4):576-580. [DOI] [PubMed] [Google Scholar]
- 6. Braun C, McRobert CJ. Conservative management following closed reduction of traumatic anterior dislocation of the shoulder. Cochrane Database Syst Rev. 2019;(5):CD004962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brophy RH, Marx RG. The treatment of traumatic anterior instability of the shoulder: nonoperative and surgical treatment. Arthroscopy. 2009;25(3):298-304. [DOI] [PubMed] [Google Scholar]
- 8. Cameron KL, Mauntel TC, Owens BD. The epidemiology of glenohumeral joint instability: incidence, burden, and long-term consequences. Sports Med Arthrosc Rev. 2017;25(3):144-149. [DOI] [PubMed] [Google Scholar]
- 9. Chan SK, Bentick KR, Kuiper JH, Kelly CP. External rotation bracing for first-time anterior dislocation of the shoulder: a discontinued randomised controlled trial comparing external rotation bracing with conventional sling. Shoulder Elbow. 2019;11(4):256-264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160-164. [PubMed] [Google Scholar]
- 11. Coudane H, Walch G, Sebesta A. Chronic anterior instability of the shoulder in adults: methodology [in French]. Rev Chir Orthop Reparatrice Appar Mot. 2000;86(suppl 1):94-95. [PubMed] [Google Scholar]
- 12. De Carli A, Vadala AP, Lanzetti R, et al. Early surgical treatment of first-time anterior glenohumeral dislocation in a young, active population is superior to conservative management at long-term follow-up. Int Orthop. 2019;43(12):2799-2805. [DOI] [PubMed] [Google Scholar]
- 13. Finestone A, Milgrom C, Radeva-Petrova DR, et al. Bracing in external rotation for traumatic anterior dislocation of the shoulder. J Bone Joint Surg Br. 2009;91(7):918-921. [DOI] [PubMed] [Google Scholar]
- 14. Gagey OJ, Gagey N. The hyperabduction test. J Bone Joint Surg Br. 2001;83(1):69-74. [DOI] [PubMed] [Google Scholar]
- 15. Gerber C, Nyffeler RW. Classification of glenohumeral joint instability. Clin Orthop Relat Res. 2002;400:65-76. [DOI] [PubMed] [Google Scholar]
- 16. Gilbart MK, Gerber C. Comparison of the subjective shoulder value and the Constant score. J Shoulder Elbow Surg. 2007;16(6):717-721. [DOI] [PubMed] [Google Scholar]
- 17. Grumet RC, Bach BR, Jr, Provencher MT. Arthroscopic stabilization for first-time versus dislocation recurrent shoulder instability. Arthroscopy. 2010;26(2):239-248. [DOI] [PubMed] [Google Scholar]
- 18. Hart WJ, Kelly CP. Arthroscopic observation of capsulolabral reduction after shoulder dislocation. J Shoulder Elbow Surg. 2005;14(2):134-137. [DOI] [PubMed] [Google Scholar]
- 19. Heidari K, Asadollahi S, Vafaee R, et al. Immobilization in external rotation combined with abduction reduces the risk of recurrence after primary anterior shoulder dislocation. J Shoulder Elbow Surg. 2014;23(6):759-766. [DOI] [PubMed] [Google Scholar]
- 20. Hofstaetter JG, Hanslik-Schnabel B, Hofstaetter SG, Wurnig C, Huber W. Cross-cultural adaptation and validation of the German version of the Western Ontario Shoulder Instability index. Arch Orthop Trauma Surg. 2010;130(6):787-796. [DOI] [PubMed] [Google Scholar]
- 21. Hovelius L, Olofsson A, Sandstrom B, et al. Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger. a prospective twenty-five-year follow-up. J Bone Joint Surg Am. 2008;90(5):945-952. [DOI] [PubMed] [Google Scholar]
- 22. Itoi E, Hatakeyama Y, Kido T, et al. A new method of immobilization after traumatic anterior dislocation of the shoulder: a preliminary study. J Shoulder Elbow Surg. 2003;12(5):413-415. [DOI] [PubMed] [Google Scholar]
- 23. Itoi E, Hatakeyama Y, Sato T, et al. Immobilization in external rotation after shoulder dislocation reduces the risk of recurrence: a randomized controlled trial. J Bone Joint Surg Am. 2007;89(10):2124-2131. [DOI] [PubMed] [Google Scholar]
- 24. Itoi E, Kitamura T, Hitachi S, Hatta T, Yamamoto N, Sano H. Arm abduction provides a better reduction of the Bankart lesion during immobilization in external rotation after an initial shoulder dislocation. Am J Sports Med. 2015;43(7):1731-1736. [DOI] [PubMed] [Google Scholar]
- 25. Itoi E, Sashi R, Minagawa H, Shimizu T, Wakabayashi I, Sato K. Position of immobilization after dislocation of the glenohumeral joint: a study with use of magnetic resonance imaging. J Bone Joint Surg Am. 2001;83(5):661-667. [DOI] [PubMed] [Google Scholar]
- 26. Jakobsen BW, Johannsen HV, Suder P, Sojbjerg JO. Primary repair versus conservative treatment of first-time traumatic anterior dislocation of the shoulder: a randomized study with 10-year follow-up. Arthroscopy. 2007;23(2):118-123. [DOI] [PubMed] [Google Scholar]
- 27. Jobe FW, Kvitne RS, Giangarra CE. Shoulder pain in the overhand or throwing athlete: the relationship of anterior instability and rotator cuff impingement. Orthop Rev. 1989;18(9):963-975. [PubMed] [Google Scholar]
- 28. Kerr ZY, Collins CL, Pommering TL, Fields SK, Comstock RD. Dislocation/separation injuries among US high school athletes in 9 selected sports: 2005-2009. Clin J Sport Med. 2011;21(2):101-108. [DOI] [PubMed] [Google Scholar]
- 29. Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26(2):325-337. [DOI] [PubMed] [Google Scholar]
- 30. Kirkley A, Griffin S, McLintock H, Ng L. The development and evaluation of a disease-specific quality of life measurement tool for shoulder instability. The Western Ontario Shoulder Instability Index (WOSI). Am J Sports Med. 1998;26(6):764-772. [DOI] [PubMed] [Google Scholar]
- 31. Kirkley A, Werstine R, Ratjek A, Griffin S. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: long-term evaluation. Arthroscopy. 2005;21(1):55-63. [DOI] [PubMed] [Google Scholar]
- 32. Liavaag S, Brox JI, Pripp AH, Enger M, Soldal LA, Svenningsen S. Immobilization in external rotation after primary shoulder dislocation did not reduce the risk of recurrence: a randomized controlled trial. J Bone Joint Surg Am. 2011;93(10):897-904. [DOI] [PubMed] [Google Scholar]
- 33. Malhotra A, Freudmann MS, Hay SM. Management of traumatic anterior shoulder dislocation in the 17- to 25-year age group: a dramatic evolution of practice. J Shoulder Elbow Surg. 2012;21(4):545-553. [DOI] [PubMed] [Google Scholar]
- 34. Marshall T, Vega J, Siqueira M, Cagle R, Gelber JD, Saluan P. Outcomes after arthroscopic Bankart repair: patients with first-time versus recurrent dislocations. Am J Sports Med. 2017;45(8):1776-1782. [DOI] [PubMed] [Google Scholar]
- 35. Miller BS, Sonnabend DH, Hatrick C, et al. Should acute anterior dislocations of the shoulder be immobilized in external rotation? A cadaveric study. J Shoulder Elbow Surg. 2004;13(6):589-592. [DOI] [PubMed] [Google Scholar]
- 36. Odenwald S, Lemke J, Bauer GJ, Mauch F, Brunner UH, Krackhard T. First traumatic anterior shoulder dislocation: postoperative results 6 months and 2 years after arthroscopic stabilization in young patients [in German]. Unfallchirurg. 2008;111(7):507-510, 512-503. [DOI] [PubMed] [Google Scholar]
- 37. Owens BD, Agel J, Mountcastle SB, Cameron KL, Nelson BJ. Incidence of glenohumeral instability in collegiate athletics. Am J Sports Med. 2009;37(9):1750-1754. [DOI] [PubMed] [Google Scholar]
- 38. Owens BD, DeBerardino TM, Nelson BJ, et al. Long-term follow-up of acute arthroscopic Bankart repair for initial anterior shoulder dislocations in young athletes. Am J Sports Med. 2009;37(4):669-673. [DOI] [PubMed] [Google Scholar]
- 39. Pogorzelski J, Fritz EM, Godin JA, Imhoff AB, Millett PJ. Nonoperative treatment of five common shoulder injuries. Obere Extremität. 2018;13(2):89-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ranalletta M, Rossi LA, Alonso Hidalgo I, et al. Arthroscopic stabilization after a first-time dislocation: collision versus contact athletes. Orthop J Sports Med. 2017;5(9):2325967117729321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Robinson CM, Jenkins PJ, White TO, Ker A, Will E. Primary arthroscopic stabilization for a first-time anterior dislocation of the shoulder: a randomized, double-blind trial. J Bone Joint Surg Am. 2008;90(4):708-721. [DOI] [PubMed] [Google Scholar]
- 42. Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am. 1978;60(1):1-16. [PubMed] [Google Scholar]
- 43. Rowe CR, Zarins B. Recurrent transient subluxation of the shoulder. J Bone Joint Surg Am. 1981;63(6):863-872. [PubMed] [Google Scholar]
- 44. Taskoparan H, Kilincoglu V, Tunay S, Bilgic S, Yurttas Y, Komurcu M. Immobilization of the shoulder in external rotation for prevention of recurrence in acute anterior dislocation. Acta Orthop Traumatol Turc. 2010;44(4):278-284. [DOI] [PubMed] [Google Scholar]
- 45. te Slaa RL, Wijffels MP, Brand R, Marti RK. The prognosis following acute primary glenohumeral dislocation. J Bone Joint Surg Br. 2004;86(1):58-64. [PubMed] [Google Scholar]
- 46. Thierbach A, Le DA, Uecker T, Gerhardt C, Scheibel M. Abduction/external rotation immobilization after primary traumatic anterior shoulder dislocation: which ortheses are suitable? [in German]. Unfallchirurg. 2014;117(12):1112-1117. [DOI] [PubMed] [Google Scholar]
- 47. Wasserstein DN, Sheth U, Colbenson K, et al. The true recurrence rate and factors predicting recurrent instability after nonsurgical management of traumatic primary anterior shoulder dislocation: a systematic review. Arthroscopy. 2016;32(12):2616-2625. [DOI] [PubMed] [Google Scholar]
- 48. Wheeler JH, Ryan JB, Arciero RA, Molinari RN. Arthroscopic versus nonoperative treatment of acute shoulder dislocations in young athletes. Arthroscopy. 1989;5(3):213-217. [DOI] [PubMed] [Google Scholar]
- 49. Whelan DB, Kletke SN, Schemitsch G, Chahal J. Immobilization in external rotation versus internal rotation after primary anterior shoulder dislocation: a meta-analysis of randomized controlled trials. Am J Sports Med. 2016;44(2):521-532. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-ajs-10.1177_0363546520987823 for Immobilization in External Rotation and Abduction Versus Arthroscopic Stabilization After First-Time Anterior Shoulder Dislocation: A Multicenter Randomized Controlled Trial by Marvin Minkus, Matthias Königshausen, Dirk Maier, Frieder Mauch, Thomas Stein, Stefan Greiner, Mohamed Moursy and Markus Scheibel in The American Journal of Sports Medicine